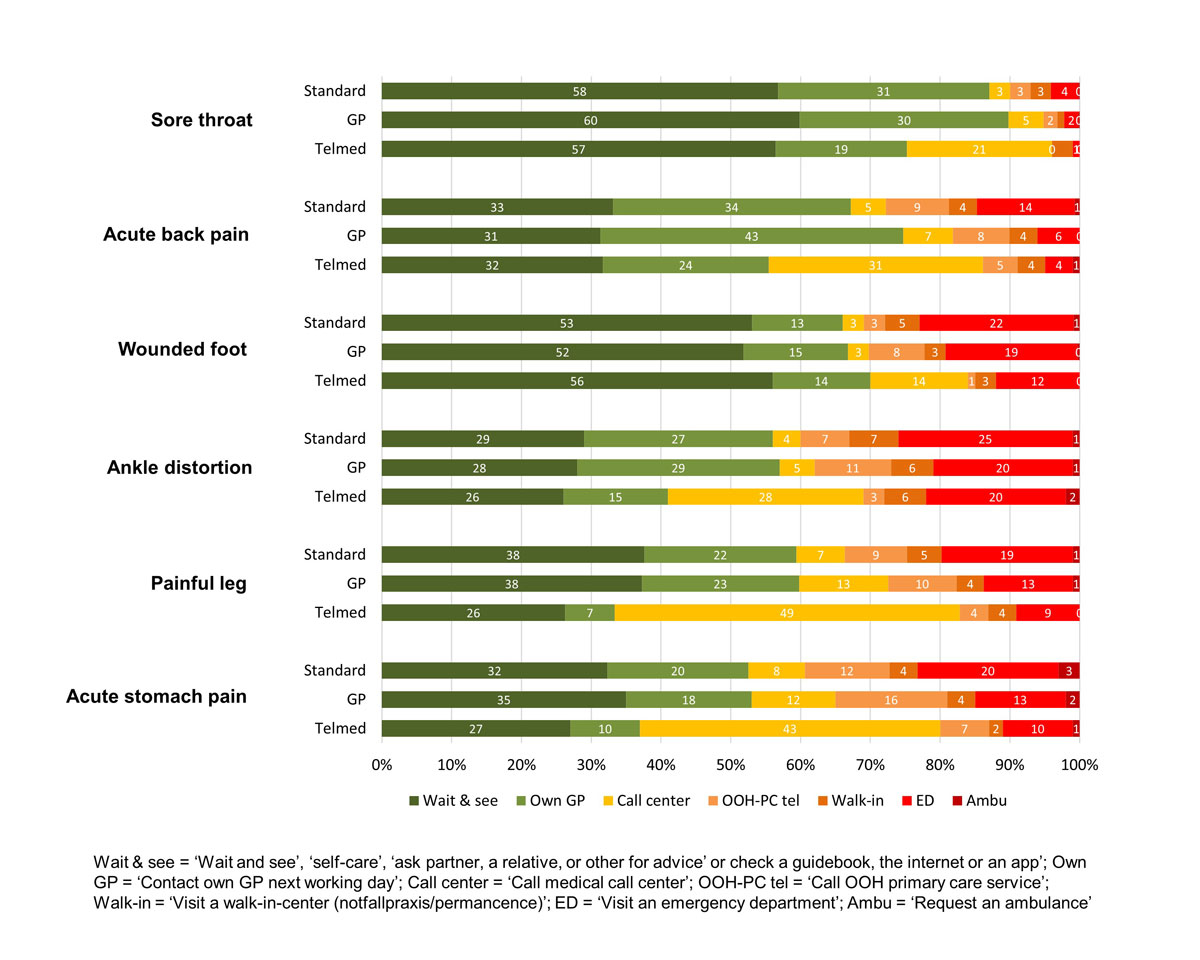
Figure 1 Intended help-seeking for the six cases, by HCP (n = 1126).
DOI: https://doi.org/10.4414/smw.2018.14686
Many European countries are dealing with overcrowding at emergency care services, such as emergency departments (EDs) of hospitals and out-of-hours (OOH) primary care services [1, 2]. This leads to high workload, long waiting times, patient dissatisfaction and increased costs, as well as to an increased risk of safety incidents [3–6]. Some of the medical problems presented at the ED or OOH healthcare services could have been treated by a general practitioner (GP) during daytime, or could have been handled by the patients themselves with self-care [7–10].
Switzerland also is dealing with crowding at the emergency care services, including medically irrelevant visits by self-referring patients who could have been treated by a GP [11, 12]. To reduce medically irrelevant use, EDs and health authorities have developed different models to reorganise emergency care services, including primary care centres integrated into hospitals’ EDs and telephone triage and advice services [8, 13].
Despite these initiatives in reorganising emergency care services, Swiss citizens can visit an ED whenever they want. Swiss primary care patients visit a hospital ED more often annually than patients from typical gatekeeping countries such as Denmark and the Netherlands (around 28% in Switzerland versus 18% in Denmark and the Netherlands) [14]. A previous study showed that, controlled for several population characteristics, Swiss citizens had a higher tendency to OOH help-seeking than Danish and Dutch citizens [15, 16]. Possible explanations for differences in healthcare use and help-seeking behaviour may be found in differences in organisation of the healthcare system.
In Switzerland, the mandatory health insurance offers free access to secondary care specialists and emergency care. However, in return for a lower premium, citizens can also choose alternative voluntary healthcare plans (HCPs), with various degrees of restriction, aiming to improve coordination and thus improve the quality of care [17]. Key elements of these alternative HCPs are coordination and gatekeeping: a GP or a medical call centre acts as gatekeeper to secondary care (table 1). There is growing interest in alternative HCPs. In 2004, 10% of Swiss citizens chose an alternative HCP, which increased to 64% in 2015 [21]. The alternative HCPs have been associated with a lower prevalence of potentially inappropriate medicine prescriptions in elderly patients and lower disease-specific hospitalisation rates in chronically ill patients [22, 23]. Relevant features of the Swiss OOH healthcare system are listed in table 1.
Table 1 Features of the Swiss healthcare system [18–20]
| Health insurance | ||||
| Citizens have to choose an HCP: | ||||
| HCP | First contact | First contact in the event of emergency | ||
| Standard | Doctor of the individual’s choice | Doctor of the individual’s choice | ||
| Voluntary alternative HCPs | GP models | Managed care model: aims to provide integrated care by coordination | GP (gatekeeper) in a medical network with capitation | Local OOH service or a dedicated telephone hotline. Gatekeeper should be informed as soon as possible about the emergency contact |
| List model | Fixed GP (gatekeeper) (the health insurance companies define which GPs can be chosen) | Local OOH service or a dedicated telephone hotline. Gatekeeper should be informed as soon as possible about the emergency contact | ||
| Call centre model (Telmed) | Medical call centre. Triage/counselling is provided by nurses, physicians and other trained healthcare professionals |
Medical call centre | ||
| Citizens with an alternative HCP get a premium reduction of around 15–25%. | ||||
| Citizens have to choose an annual deductible, ranging between CHF 300 and 2500 (€250–2000), and additionally have to pay 10% of all costs up to a maximum of CHF 700 (€600) per year (this cannot be covered by voluntary insurance). | ||||
| Lower income households can receive subsidies for paying their premium. | ||||
| At the end of the year, citizens can change their HCP and annual deductible for the next year. Citizens who have a standard HCP and the lowest possible deductible (CHF 300) can change every month. | ||||
| Organisation of OOH care | ||||
| OOH care is organised locally and models vary between regions. Most used services include: ‒ Rota systems run by GPs on duty; ‒ 24-hour telephone services (for example, Telmed, Medgate, Medi24); ‒ Walk-in-centres (e.g. group practices offering OOH care with extended opening hours); ‒ EDs of hospitals, at some places, general practices are integrated in the ED offer OOH care; ‒ Emergency medical services. |
||||
| There is no institutionalised information exchange between OOH services and general practices. However, individuals with an alternative HCP are obliged to inform their gatekeeper about an OOH contact. | ||||
| OOH primary care is delivered by GPs. Trained nurses, supervised by physicians, are involved in medical call centres providing triage and counselling. | ||||
ED = emergency department; GP = general practitioner; HCP = healthcare plan; OOH = out-of-hours
Most of the international and national literature on integrated healthcare models focuses on the elderly and patients with chronic diseases [22, 24]. However, data on the association between different HCPs and help-seeking behaviour OOH care are scant. The objective of our study was to examine the impact of HCPs on intended help-seeking behaviour in OOH care in Switzerland.
We performed a secondary analysis of Swiss data collected for the EurOOHnet survey study on help-seeking behaviour in Denmark, the Netherlands and Switzerland [15, 16, 25]. The aim of the larger study was to examine differences in help-seeking between the three countries and to identify factors that are associated with OOH help-seeking. For the present study, we focused only on the Swiss data to investigate the influence of HCPs. Swiss members of two consumer panels were invited to participate in a survey [26, 27]. These panel members represent the German-speaking part of the Swiss population (around 63% of all Swiss citizens). Due to the primary study aim, only Swiss individuals aged between 30–39 years and between 50–59 years were invited to participate. Based on a power calculation to detect differences in help-seeking between countries, we aimed to reach 600 individuals per age group. In December 2015, 6093 individuals were invited via e-mail to complete the online questionnaire. The data collection was ended after five days when 600 respondents in each age group completed the questionnaire.
A questionnaire consisting of six case scenarios and questions concerning factors related to help-seeking behaviour was developed, based on the Andersen’s Behavioural Model [28]. The case scenarios described medical problems with a potential need for seeking OOH care for a specific weekday and time (appendix 1). The cases varied in urgency, and some of them were based on cases from previous studies [29–31]. Also, new cases based on frequent reasons for encounter in the three countries were developed. Researchers, laypersons and an expert panel of GPs were involved in the development of the cases. A detailed description of the case development is available elsewhere [15].
Respondents were asked what choice they would make when facing the medical situation described in the case. In table 2, we present the possible answer categories and the two categorisations we made for each case as our two outcome measures: (1) intended help-seeking for OOH care and (2) intended help-seeking for OOH face-to-face care. When respondents gave more than one answer, we used the “highest” choice.
Table 2 Classification of intended out-of-hours (OOH) care.
| Answering categories: possible intended actions to take |
Classification:
OOH care |
Classification:
face-to-face OOH care |
|---|---|---|
| Wait and see | No OOH contact | No OOH face-to-face contact |
| Self-care | ||
| Ask partner, a relative, or other for advice | ||
| Check a guidebook, the internet or an app | ||
| Contact own GP next working day | ||
| Call medical call centre | OOH contact | |
| Call OOH primary care service | ||
| Visit a walk-in-centre (Notfallpraxis/permanence) | OOH face-to-face contact | |
| Visit an emergency department | ||
| Request an ambulance |
The other questions were used to identify factors that may be related to OOH help-seeking, based on Andersen’s Behavioural Model [28]. This is an acknowledged theoretical framework used to understand individuals’ healthcare use. According to this model, individual’s healthcare use is influenced by predisposing characteristics, enabling factors and need factors. Predisposing characteristics are demographic variables that make some individuals more likely to use healthcare than others (e.g., age or education). Enabling factors facilitate or obstruct healthcare use (e.g., income or telephone accessibility of healthcare service). Need factors refer to immediate reasons leading to healthcare use (e.g., actual health status). Also, environmental factors (e.g., healthcare system) and behavioural factors could influence access to healthcare services. For this paper, we used the healthcare system factor HCP as main factor of interest with the categories “standard”, “GP” or “Telmed”. The HCPs “managed care model” and “list model” (see table 1) are combined within the “GP model”, since from a patient perspective the steering mechanism of these models is very similar (GPs act as a gatekeeper).
The other factors used as potential confounders for the possible influence of HCP on intended help-seeking behaviour were: age, gender, education level, medical education, ethnicity, employment, living status, social support, health literacy (scales navigating the system and sufficient information), self-efficacy, anxiety, attitude towards use of OOH primary care (predisposing characteristics); travel time, problems with organising a consultation during the day (because of own work/private appointments, accessibility own GP and availability own GP), deductible, having an own GP (enabling factors); self-assessed health (need factor); and previous behaviour (contacts with GP and OOH care) (behavioural factors). A detailed operationalisation of these factors is to be elsewhere [16].
According to current Swiss law on human research, anonymously collected data require no approval by a regional ethics committee.
Descriptive statistics were used to describe the characteristics of the respondents. Differences in characteristics between HCPs were tested with ordinal regression analyses. We also presented the distribution of the answers given on the case scenarios, stratified for HCP. Univariate logistic regression analyses were performed to test differences in answers for each case scenario between individuals with the different HCPs, and are presented in appendix 2 . We conducted two binomial multiple regression analyses (generalised linear models) for testing the influence of HCP on the inclination to contact OOH care and to have a face-to-face contact with OOH care. We adjusted for the other factors based on Andersen’s Behavioural Model. Odds ratios (ORs) were presented with 95% confidence intervals (CIs). A sensitivity analysis investigated the consequences of excluding the respondents with missing values on the adjusted factors. Analyses were performed in R version 3.2.0 and SPSS version 25.
In total, 1200 Swiss individuals completed the questionnaire (600 for age group 30–39 and 600 for age group 50–59) (not in table). During data management, we found some questions with an open-text field that had identical written answers. Checking for duplicates between the two consumer panels (based on population characteristics and open answers), we revealed 16 potential duplicates. Although duplicates were checked by the consumer panels using IP-addresses, we still suspected that the questionnaire was filled in twice by some respondents. Therefore, we decided to exclude one of the completed questionnaires of these respondents.
Of the remaining 1184 respondents, 34.0% had a standard HCP, 51.4% a GP HCP and 14.6% a Telmed HCP; 4.9% did not know what kind of HCP they had (table 3). We excluded the last group (n = 58) from the analyses. The respondents of the three HCPs differed in some respects. Persons with a GP or Telmed HCP were younger, more often employed, assessed their health more often as good, and had more often a higher deductible, compared with persons with a standard HCP. Persons with a GP model had a higher score on health literacy regarding navigating the system and more often had an own GP than standard insured persons. They also reported having had fewer contacts with OOH care than standard insured persons. Telmed-insured persons were more highly educated, more often experienced problems contacting their own GP because of own working times or private appointments, less often had their own GP and had fewer contacts with their own GP than standard insured persons.
Table 3 Characteristics of the study population, stratified by healthcare plan (HCP).
| Factors† | Categories | HCP‡ | ||
|---|---|---|---|---|
|
Standard§
(nmax = 383) |
GP
(nmax = 579) |
Telmed
(nmax = 164) |
||
| Predisposing | ||||
| Age (years) | Mean, SD | 46.3 (10.2) | 44.6 (10.2)* | 42.4 (10.1)* |
| Gender | Male | 47.3 | 44.6 | 41.5 |
| Female | 52.7 | 55.4 | 58.5 | |
| Education level | Low | 9.1 | 6.2 | 1.8* |
| Middle | 59.3 | 65.6 | 63.4 | |
| High§ | 31.6 | 28.2 | 34.8 | |
| Medical education | None | 92.9 | 92.7 | 91.5 |
| Some/nurse/doctor | 7.1 | 7.3 | 8.5 | |
| Ethnicity | Native§ | 63.7 | 68.5 | 71.6 |
| Western migrant | 32.4 | 28.9 | 25.3 | |
| Non-western migrant | 3.9 | 2.6 | 3.1 | |
| Employment | Unemployed | 31.1 | 20.6 | 19.5 |
| Employed | 68.9 | 79.4 * | 80.5* | |
| Living status | Living alone | 27.2 | 25.0 | 26.8 |
| Living with another adult | 72.8 | 75.0 | 73.2 | |
| Social support | Lacking social support | 36.6 | 31.8 | 31.7 |
| Receiving social support | 63.4 | 68.2 | 68.3 | |
| Health literacy: navigating the system | Low ability | 4.7 | 1.6* | 2.4 |
| Middle ability | 23.0 | 19.5 | 18.9 | |
| High ability | 54.6 | 57.2 | 59.8 | |
| Highest ability§ | 17.8 | 21.8 | 18.9 | |
| Health literacy: sufficient information | Low ability | 7.6 | 6.6 | 4.9 |
| High ability | 66.8 | 66.8 | 65.9 | |
| Highest ability§ | 25.6 | 26.6 | 29.3 | |
| Self-efficacy | Low | 35.8 | 35.6 | 32.3 |
| High | 64.2 | 64.4 | 67.7 | |
| Anxiety | No anxiety | 84.3 | 88.1 | 87.2 |
| Anxiety | 15.7 | 11.9 | 12.8 | |
| Attitude towards use OOH primary care | Low barrier | 48.0 | 48.4 | 51.3 |
| High barrier | 52.0 | 51.6 | 48.7 | |
| Enabling | ||||
| Travel time | <15 minutes§ | 48.3 | 51.2 | 43.4 |
| 15–30 minutes | 43.2 | 40.9 | 47.8 | |
| >30 minutes | 8.6 | 7.9 | 8.8 | |
| Problems – own work or private appointments | No/few problems | 89.3 | 89.1 | 81.4 |
| Some/many problems | 10.7 | 10.9 | 18.6* | |
| Problems – accessibility own GP | No/few problems | 93.6 | 93.0 | 91.1 |
| Some/many problems | 6.4 | 7.0 | 8.9 | |
| Problems – availability own GP | No/few problems | 91.0 | 92.4 | 88.8 |
| Some/many problems | 9.0 | 7.6 | 11.2 | |
| Deductible | ≤1000 CHF | 66.6 | 49.5 | 44.6 |
| >1000 CHF | 33.4 | 50.5* | 55.4* | |
| Own GP | No | 9.4 | 3.5 | 22.6 |
| Yes | 90.6 | 96.5* | 77.4* | |
| Need | ||||
| Self-assessed health | Poor | 19.8 | 9.7 | 4.3 |
| Good | 80.2 | 90.3* | 95.7* | |
| Behaviour | ||||
| Frequency contacts own GP | None/one contact§ | 45.0 | 43.6 | 57.7 |
| Few contacts | 36.5 | 40.8 | 27.6* | |
| More contacts | 18.5 | 15.5 | 14.7 | |
| Frequency contacts OOH care | None§ | 64.8 | 71.9 | 70.7 |
| One contact | 19.2 | 17.1 | 17.1 | |
| More contacts | 16.0 | 11.0* | 12.2 | |
GP = general practitioner; OOH = out-of-hours; SD = standard deviation † Percentage of missing values factors ranged from 0% (age, gender, living situation, social support, health literacy, self-efficacy, anxiety, health status, having own GP) to 5.5% (deductible). ‡ Percentage of missing values HCP: 4.9% (don’t know, n = 58) § Used as reference group by comparison * Compared with standard insurance (reference) p <0.05, in bold
In figure 1, we present the answers given by the respondents on each of the six cases, divided by type of HCP. Overall, persons with a standard insurance more often intended to contact the ED than patients with an alternative HCP (mean six cases: standard 17%, GP 12%, Telmed 9%). Compared with persons with a standard or GP HCP, persons with a Telmed insurance more often chose to call the medical call centre (mean six cases: standard 5%, GP 8%, Telmed 31%). Detailed results of the association between intended OOH help-seeking and the various HCPs, stratified according to the six case scenarios, are given in appendix 2.
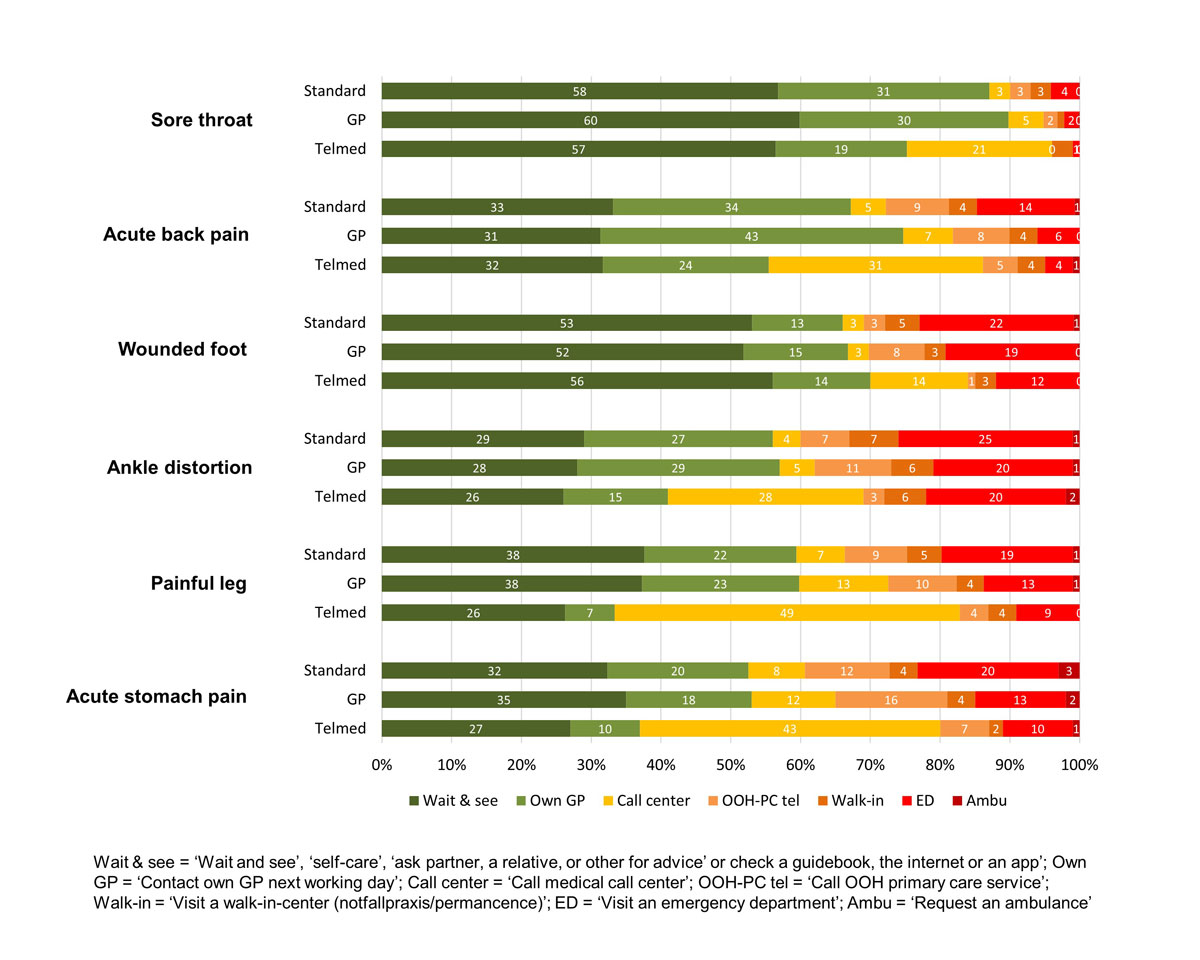
Figure 1 Intended help-seeking for the six cases, by HCP (n = 1126).
In table 4 , we present the results of the multiple binomial regression analyses, for the six cases combined and controlled for other factors. We excluded 158 respondents from these analyses, owing to one or more missing answers on the combined score for help-seeking (n = 3) and on the questions we used for the adjusted factors (n = 155). Our sensitivity analysis showed that excluding respondents with missing answers on the adjusted factors would not alter our results.
Table 4 Binomial regression analyses for impact of healthcare plan on (face-to-face) out-of-hours help-seeking.
| Healthcare plan |
Outcome: OOH care
(n = 968) |
Outcome: face-to-face OOH care
(n = 968) |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Standard (ref.) | ||||
| GP | 1.02 | 0.91-1.16 | 0.74* | 0.63-0.86 |
| Telmed | 2.28* | 1.91-2.72 | 0.69* | 0.55-0.87 |
Ref. = reference category; GP = general practitioner; OOH = out-of-hours; OR = Odds Ratio; CI = Confidence Interval; * p<0.05, in bold Adjusted for age, gender, education, medical education, ethnicity, employment, live status, social support, health literacy (navigating the system and information), self-efficacy, anxiety, attitude towards use OOH primary care, distance, problems (own work / private appointments, accessibility and availability own GP), self-assessed health, frequently contacts own GP, frequency contact OOH care, deductible and having an own GP
Persons with a Telmed HCP had a higher inclination to contact OOH care than persons with a standard HCP (OR 2.28, 95% CI 1.91–2.72). We found no differences in intended help-seeking between persons with a GP or a standard HCP. Regarding the influence of HCP on the intention to use face-to-face OOH care, we found opposite results. Both GP- and Telmed-insured persons were less inclined to have a face-to-face contact than standard insured persons (GP: OR 0.74, 95% CI 0.63–0.86; Telmed: OR 0.69, 95% CI 0.55–0.87).
Individuals with the alternative HCPs differed from individuals having a standard HCP in a number of ways. They seemed to be younger, more highly educated, more often employed and healthier, and to have a higher deductible. Despite these differences, for which we controlled in our analyses, we found that type of HCP is associated with individuals’ intention to seek OOH care help. Individuals insured via the Telmed HCP were more inclined to seek help OOH care than persons with a standard HCP. However, they were less inclined to choose a face-to-face OOH contact. They chose to call the medical call centre of their insurer when they experienced a medical problem, something that they were expected to do according to the policy. Persons with a GP HCP were also less likely to have an OOH face-to-face contact than persons with a standard HCP, although they are not restricted by the HCP to contact their gatekeeper in the event of an acute health problem.
A possible explanation could be that they are not used to visit a walk-in-clinic or ED during office hours, and consequently that they also prefer less to do so outside office hours, in comparison to persons with a standard HCP. Another explanation could be that persons of the three HCPs differ in factors other than those we included as control factors in our analyses. Individuals who decide to enrol in a standard HCP may have different ideas about using care. They are paying for unrestricted access to the ED and specialists and want to use this “benefit”. This might also explain why they choose to have a standard HCP in the first place. Other studies have discussed whether persons enrolled in an alternative plan would be healthier [32, 33], which is also probable in Switzerland. We controlled for the factor self-assessed health, which may not totally reflect the actual health status of individuals. Also need factors, such as having a chronic disease or medical history could be related to help-seeking.
As we wrote in the introduction, chronic patients enrolled in alternative GP HCPs had a lower probability of disease-related hospitalisation than those enrolled in a standard care model, and elderly patients had a lower prevalence of potentially inappropriate medication prescriptions [22, 23]. We are not aware of previous research that specifically studied the impact of alternative HCPs on the use of OOH care, but an integrated healthcare system in the United States – Kaiser Permanente – showed similar results for ED utilisation. In California, ED use was lower at hospitals affiliated with Kaiser Permanente than at other hospitals [34]. Members of this system are encouraged to use the tele-medical service and to schedule appointments for ED visits.
Several studies found a relation between accessibility of primary care and the number of ED visits, both in and outside office hours. For example, patients with a regular doctor who knows them personally were less likely to attend EDs [14]. A review of reviews showed that co-location of GP posts and EDs seems, together with the introduction of telephone triage systems, the preferred intervention to reduce inappropriate ED visits [35].
A strength of this study is that we also included individuals who may never contact an OOH care service, unlike many other studies focusing on patients who had already contacted a healthcare provider.
Our procedure of data collection could have introduced a risk of selection bias, on the one hand caused by the short period of data collection and on the other hand by a biased selection of participants using consumer panels. To check the representativeness of our respondents, we compared our respondents on the characteristics HCP, gender, education and ethnicity with the general population (data not shown) [21, 36]. Compared with the general population, we included fewer individuals with a Telmed HCP. However, this was not expected to have influenced our results, as we focused on the association of HCP with intended help-seeking. The other characteristics reflect the general population. Another limitation is the use of hypothetical case scenarios to measure intended help-seeking behaviour. Respondents could have made other choices in real life, especially when emotions are involved. Nevertheless, intended help-seeking seems to be a good predictor for measuring actual help-seeking [37].
Implementing alternative HCPs may not only influence healthcare use during daytime (focusing on chronic care), but could also have a positive influence on OOH face-to-face care use. It could reduce medically inappropriate use and therefore costs of emergency and OOH care services. On the other hand, Telmed-insured individuals often chose to call the medical call centre –more than people with other HCP insurance – which involves extra costs. However, these extra costs probably do not outweigh the savings of face-to-face care costs, although, this behaviour may have a negative influence on the self-reliance of the callers. Studies from other European countries have also shown the attraction of telephone services. Many contacts are handled on the phone instead of a face-to-face contact, but the total number of contacts may increase [38–40]. Our outcomes could be relevant for other countries who are organising their healthcare system. The impact of HCP on healthcare use is not only influenced by choices of patients, but the organisation of triage is essential for the final number of OOH (face-to-face) contacts. Future research could focus on motives of individuals in choosing a certain HCP, and on which individuals change their HCP including reasons for this change. We also recommend studying the impact of HCPs on actual OOH healthcare use, instead of intended help-seeking.
Alternative HCPs seem to influence the use of OOH care, although patients are not restricted by the HCP to contact their gatekeeper in case of emergency. These results could be relevant for policy makers, especially from non-gatekeeping countries, in order to reduce inappropriate use and costs of emergency and OOH care services.
The appendices are available in a separate file at: https://smw.ch/en/article/doi/smw.2018.14686/
The authors want to thank all GPs and individuals who participated in this study.
This study was supported by the Danish foundation TrygFonden. Trygfonden had no role in the study design, data collection, analysis, and interpretation of data, in the writing of the manuscript, and in the decision to submit the article for publication.
The authors have no competing interests to declare.
1 Pines JM , Hilton JA , Weber EJ , Alkemade AJ , Al Shabanah H , Anderson PD , et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011;18(12):1358–70. doi:.https://doi.org/10.1111/j.1553-2712.2011.01235.x
2 Carter EJ , Pouch SM , Larson EL . The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106–15. doi:.https://doi.org/10.1111/jnu.12055
3 Smits M , Keizer E , Huibers L , Giesen P . GPs’ experiences with out-of-hours GP cooperatives: a survey study from the Netherlands. Eur J Gen Pract. 2014;20(3):196–201. doi:.https://doi.org/10.3109/13814788.2013.839652
4 Johnson KD , Winkelman C . The effect of emergency department crowding on patient outcomes: a literature review. Adv Emerg Nurs J. 2011;33(1):39–54. doi:.https://doi.org/10.1097/TME.0b013e318207e86a
5 Hoot NR , Aronsky D . Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–36.e1. doi:.https://doi.org/10.1016/j.annemergmed.2008.03.014
6 Tekwani KL , Kerem Y , Mistry CD , Sayger BM , Kulstad EB . Emergency Department Crowding is Associated with Reduced Satisfaction Scores in Patients Discharged from the Emergency Department. West J Emerg Med. 2013;14(1):11–5. doi:.https://doi.org/10.5811/westjem.2011.11.11456
7 Durand AC , Gentile S , Devictor B , Palazzolo S , Vignally P , Gerbeaux P , et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med. 2011;29(3):333–45. doi:.https://doi.org/10.1016/j.ajem.2010.01.003
8 Chmiel C , Wang M , Sidler P , Eichler K , Rosemann T , Senn O . Implementation of a hospital-integrated general practice--a successful way to reduce the burden of inappropriate emergency-department use. Swiss Med Wkly. 2016;146:w14284. doi:.https://doi.org/10.4414/smw.2016.14284
9 Thijssen WA , van Mierlo E , Willekens M , Rebel J , Sandel MH , Giesen P , et al. Complaints and Diagnoses of Emergency Department Patients in the Netherlands: A Comparative Study of Integrated Primary and Emergency Care. PLoS One. 2015;10(7):e0129739. doi:.https://doi.org/10.1371/journal.pone.0129739
10 Keizer E , Smits M , Peters Y , Huibers L , Giesen P , Wensing M . Contacts with out-of-hours primary care for nonurgent problems: patients’ beliefs or deficiencies in healthcare? BMC Fam Pract. 2015;16(1):157. doi:.https://doi.org/10.1186/s12875-015-0376-9
11 Sanchez B , Hirzel AH , Bingisser R , Ciurea A , Exadaktylos A , Lehmann B , et al. State of Emergency Medicine in Switzerland: a national profile of emergency departments in 2006. Int J Emerg Med. 2013;6(1):23. doi:.https://doi.org/10.1186/1865-1380-6-23
12 Diserens L , Egli L , Fustinoni S , Santos-Eggimann B , Staeger P , Hugli O . Emergency department visits for non-life-threatening conditions: evolution over 13 years in a Swiss urban teaching hospital. Swiss Med Wkly. 2015;145:w14123. doi:.https://doi.org/10.4414/smw.2015.14123
13 Niemann S , Meer A , Simonin C , Abel T . Medical telephone triage and patient behaviour: How do they compare? Swiss Med Wkly. 2004;134(9-10):126–31. doi:.https://doi.org/10.4414/smw.2004.10276
14 van den Berg MJ , van Loenen T , Westert GP . Accessible and continuous primary care may help reduce rates of emergency department use. An international survey in 34 countries. Fam Pract. 2016;33(1):42–50. doi:.https://doi.org/10.1093/fampra/cmv082
15 Huibers L , Keizer E , Helles Carlsen A , Moth G , Smits M , Senn O , et al. Help-seeking behaviour outside office hours in Denmark, the Netherlands, and Switzerland: : a questionnaire study exploring responses to hypothetical cases. BMJ Open. 2018;8:e019295. doi:.https://doi.org/10.1136/bmjopen-2017-019295
16 Keizer E , Bondo Christensen M , Helles Carlsen A , Smits M , Wensing M , Senn O , et al. Factors related to out-of-hours help-seeking for acute health problems: a survey study using case scenarios. 2018. (Submitted)
17Berchtold P, Peytremann-Bridevaux I. Integrated care organizations in Switzerland. Int J Integr Care. 2011;11 Spec Ed:e010.
18 De Pietro C , Camenzind P , Sturny I , Crivelli L , Edwards-Garavoglia S , Spranger A , et al. Switzerland: Health System Review. Health Syst Transit. 2015;17(4):1–288, xix.
19Mossialos E, Wenzl M, Osborn R, Anderson C. International Profiles Of Health Care Systems, 2014. The Commonwealth Fund; 2015.
20Berchet C, Nader C. The organisation of out-of-hours primary care in OECD countries”, OECD Health Working Papers, No. 89. Paris: OECD Publishing; 2016.
21Forum Managesd Care. Erhebung Ärztenetze in der Schweiz [Collection of medical networks in Switzerland] 2015 [18-11-2017]. Available from: http://fmc.ch/infothek/erhebung-aerztenetze.
22 Huber CA , Reich O , Früh M , Rosemann T . Effects of Integrated Care on Disease-Related Hospitalisation and Healthcare Costs in Patients with Diabetes, Cardiovascular Diseases and Respiratory Illnesses: A Propensity-Matched Cohort Study in Switzerland. Int J Integr Care. 2016;16(1):11. doi:.https://doi.org/10.5334/ijic.2455
23 Reich O , Rosemann T , Rapold R , Blozik E , Senn O . Potentially inappropriate medication use in older patients in Swiss managed care plans: prevalence, determinants and association with hospitalization. PLoS One. 2014;9(8):e105425. doi:.https://doi.org/10.1371/journal.pone.0105425
24 Damery S , Flanagan S , Combes G . Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open. 2016;6(11):e011952. doi:.https://doi.org/10.1136/bmjopen-2016-011952
25European research network for out-of-hours primary health care. Available from: www.euroohnet.eu.
26Respondi consumer panel [Available from: www.respondi.com.
27Bilendi consumer panel [Available from: www.bilendi.co.uk/static/studymarket.
28 Andersen RM . Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi:.https://doi.org/10.2307/2137284
29 Smits M , Hanssen S , Huibers L , Giesen P . Telephone triage in general practices: A written case scenario study in the Netherlands. Scand J Prim Health Care. 2016;34(1):28–36. doi:.https://doi.org/10.3109/02813432.2016.1144431
30 Giesen P , Ferwerda R , Tijssen R , Mokkink H , Drijver R , van den Bosch W , et al. Safety of telephone triage in general practitioner cooperatives: do triage nurses correctly estimate urgency? Qual Saf Health Care. 2007;16(3):181–4. doi:.https://doi.org/10.1136/qshc.2006.018846
31Huibers L, Sloot S, Giesen P, van Veen M, van Ierland Y, Moll H. Wetenschappelijk onderzoek Nederlands Triage Systeem [Scientific Research Netherlands Triage System]. Nijmegen, Rotterdam: IQ healthcare Radboudumc, Erasmus MC Sophia Kinderziekenhuis; 2009.
32 Bes RE , Curfs EC , Groenewegen PP , de Jong JD . Health plan choice in the Netherlands: restrictive health plans preferred by young and healthy individuals. Health Econ Policy Law. 2017;12(3):345–62. doi:.https://doi.org/10.1017/S1744133116000517
33 Nicholas LH . Better Quality of Care or Healthier Patients? Hospital Utilization by Medicare Advantage and Fee-for-Service Enrollees. Forum Health Econ Policy. 2013;16(1):137–61. doi:.https://doi.org/10.1515/fhep-2012-0037
34 Selevan J , Kindermann D , Pines JM , Fields WW . What Accountable Care Organizations Can Learn from Kaiser Permanente California’s Acute Care Strategy. Popul Health Manag. 2015;18(4):233–6. doi:.https://doi.org/10.1089/pop.2014.0157
35 Van den Heede K , Van de Voorde C . Interventions to reduce emergency department utilisation: A review of reviews. Health Policy. 2016;120(12):1337–49. doi:.https://doi.org/10.1016/j.healthpol.2016.10.002
36 Federal Statistical Office. [Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/population.html.
37 Armitage CJ , Conner M . Efficacy of the Theory of Planned Behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–99. doi:.https://doi.org/10.1348/014466601164939
38 Newbould J , Abel G , Ball S , Corbett J , Elliott M , Exley J , et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ. 2017;358:j4197. doi:.https://doi.org/10.1136/bmj.j4197
39 Giesen P , Hammink A , Mulders A , Oude Bos A . Te snel naar de huisartsenpost [Too easy to go to the GP cooperative]. Med Contact (Bussum). 2009;06:239–42.
40 Huibers L , Moth G , Andersen M , van Grunsven P , Giesen P , Christensen MB , et al. Consumption in out-of-hours health care: Danes double Dutch? Scand J Prim Health Care. 2014;32(1):44–50. doi:.https://doi.org/10.3109/02813432.2014.898974
This study was supported by the Danish foundation TrygFonden. Trygfonden had no role in the study design, data collection, analysis, and interpretation of data, in the writing of the manuscript, and in the decision to submit the article for publication.
The authors have no competing interests to declare.