The “Sarner Code” for COVID-19 patients and triage during resource scarcity in Switzerland
Noé Brasier, Lucia Schuler, Christa Pintelon, Robert Einsle, Thomas Kaeslin, Philippe Stocker
Introduction
The COVID-19 pandemic has stretched healthcare systems to their limits. Discussing a patient’s preference concerning resuscitation and/or admission to the intensive care unit (ICU) has to be addressed at hospital admission, as enshrined in Swiss law. Involving patients in the healthcare decision-making process is of utmost importance and demanded [1]. Patients can participate by thinking about and discussing a patient decree with their close relatives and their family doctor in advance. The patient decree will help the patient to decide how far medical treatment should go.
Triage in times of resource scarcity in Switzerland
In the context of the current COVID-19 pandemic, the Swiss Academy of Medical Science (SAMS) and Swiss Society of Intensive Care Medicine (SSICM) amended the existing guideline for intensive care interventions from 2013, offering support and guidance for decision making in resource scarcity [2]. They discussed two stages (stage A with remaining ICU beds and stage B no ICU beds remaining), which are built on one another. The execution of the guidelines takes place through the ICU specialists, together with an interdisciplinary consortium if needed, and is always a case-by-case decision. If ICU capacity is exhausted (stage B) and not all patients requiring intensive care can be admitted, the short-term survival prognosis is decisive for triage. An additional specific parameter that is applied is frailty, assessed by means of the Clinical Frailty Score, which is an important prognostic marker in the elderly. Importantly, age, disability and dementia are principally not criteria to be used.
The Cantonal Hospital Obwalden
The Cantonal Hospital Obwalden is a Swiss HBase hospital (cantonal hospital without an ICU) [3]. Patients in need of ICU treatment are transferred to Lucerne Cantonal Hospital, among others. Up to March 2021, 148 patients were treated in-house during the first and second waves of the COVID-19 pandemic, of whom 10 were transferred to an ICU and 9 patients died in-house [4].
A classification code for treatment preference
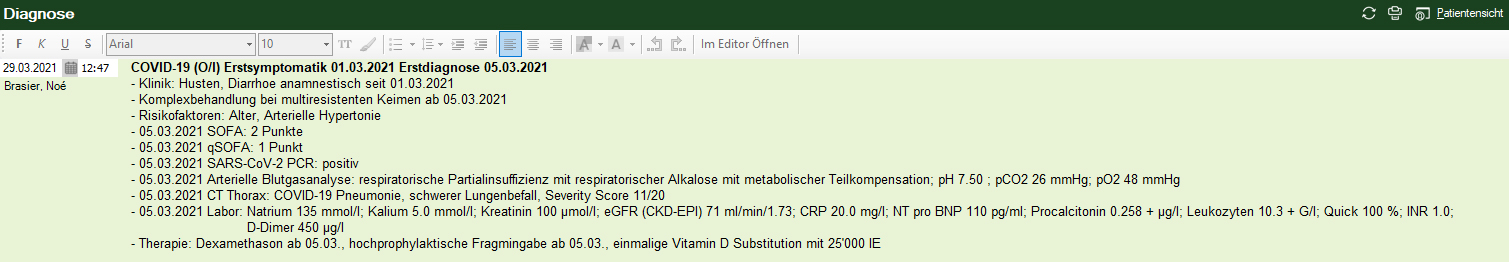
Based on the SAMS recommendation for triage in resource scarcity, we developed a simple code to classify patients according to their treatment preferences. We created five classes for COVID-19 patients, which are assigned after a personal discussion upon presentation to the emergency department: outpatient setting (A), outpatient palliative setting (P), in-house treatment with observation and assigning to ICU if indicated (O/I), in-house treatment with observation and change into palliative setting if indicated (O/P) and direct transfer to ICU if indicated (I). The code is marked on the top, next to the COVID-19 diagnosis as shown in figure 1.
Upon admission, the physician in charge leads a discussion with the patient on the currently indicated treatment and possible options in the case of health deterioration. The decision is made accordingly to informed consent rules. If this is not applicable as the patient cannot decide, family members, the family doctor and healthcare providers will have to decide in the best interest of the patient. The classification code is dynamic and reassessed during hospital treatment.
Figure 1: Fictional patient record including the code for treatment preference.
Noé Brasier, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland, noe.brasier[at]ksow.ch
Lucia Schuler, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland
Christa Pintelon, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland
Robert Einsle, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland
Thomas Kaeslin, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland
Philippe Stocker, Department of Internal Medicine, Cantonal Hospital Obwalden, Sarnen, Switzerland
References
- Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Arch Intern Med. 1996;156(13):1414–20.
- Swiss Academy of Medical Science. Guideline COVID-19 pandemic: Triage for intensive-care treatment under resource scarcity, V3.1.
- Swiss Society of Emergency and Rescue Medicine. Guideline for prehospital triage and care under resource scarcity in the hospital sector during the COVID-19 pandemic. V2.0 from 2020 April 6.
- Patient flow at Cantonhospital Obwalden (CH) during 2nd wave of COVID-19 pandemic, unpublished, data accessible on reasonable request from corresponding author.
