Swiss recommendations on driving ability in patients with diabetes mellitus
DOI: https://doi.org/https://doi.org/10.57187/s.4665
Endorsed by the Traffic Medicine Section of the Swiss Society of Legal Medicine (SSLM)
and the Executive Board of Swiss Society of Endocrinology and Diabetology (SSED)
Roger Lehmanna,
Sandrina Bervinib,
Vojtech Pavlicekc,
Regula Wickd,
Barbara Lucchinie,
Ulrike Itenf,
Lia Ballyg
a Department
of Endocrinology, Diabetes and Clinical Nutrition, University Hospital Zurich, Zurich,
Switzerland
b EndoDia Centre, Biel,
Switzerland
c Hospital Thurgau,
Kreuzlingen, Switzerland
d Institute for Legal Medicine, University of Zurich, Zurich, Switzerland
e Hospital Bellinzona, Bellinzona, Switzerland
f Swiss Society of Endocrinology and Diabetology (SGED-SSED), Baden, Switzerland
g Department of Endocrinology, Diabetes and Clinical Nutrition, University
Hospital Bern, Bern, Switzerland
Summary
Most people with diabetes mellitus operate
motor vehicles safely without creating any meaningful risk on the road for
themselves or others. A diagnosis of diabetes is, in itself, inadequate for
determining a person’s driving capability or safety. Diabetes-related traffic
accidents are rare for most drivers with diabetes mellitus and occur less
frequently than for many other diseases that can impair driving performance and
that are tolerated by society. The incidence of hypoglycaemia, which impairs
the ability to drive, severe retinopathy (including macular oedema) or cataract
formation affecting visual acuity required to drive a motor vehicle, and
peripheral neuropathy, which can severely impair sensation in the feet, is not so
common as to justify restricting driving privileges for all drivers with
diabetes mellitus.
In recent years, several pharmacological
and technological innovations have revolutionised diabetes care. Continuous glucose
monitoring system
(CGMS) technology has only recently become increasingly integrated into
diabetes therapy. Today, except for insulin, none of the treatments recommended
for type 2 diabetes mellitus causes hypoglycaemia, and the risk of hypoglycaemia
with ultra-long-acting insulins is lower. As a result, recommendations for
driving motor vehicles have had to be adjusted. Since hypoglycaemia is the
greatest risk factor for impaired driving ability, the latest technology (CGMS
coupled with hybrid closed-loop insulin pumps) can reduce the number of hypoglycaemic
events and blood glucose fluctuations. In addition, HbA1c and time in target
range can be improved. Patients with type 1 diabetes mellitus are now, in
exceptional cases, allowed to be licensed in higher vehicle categories. With
the analysis of CGMS data, an objective assessment of the frequency of hypoglycaemia
is now possible; this was previously only partially possible with blood glucose
logs. Patients who are treated with insulin should use a CGMS. This also
applies to gestational diabetes and diabetes during pregnancy. Since these
systems warn of impending hypoglycaemia, they will also improve road safety,
and the safety margin for blood glucose, previously set at 5 mmol/l, can be
lowered to 4 mmol/l. For CGMS users, blood glucose measurements every 2 hours
while driving are no longer necessary.
Introduction
The prevalence of diabetes mellitus in
Switzerland is 6.3% [1] and most of these people operate motor vehicles safely without
creating any meaningful risk on the road for themselves or others. A diagnosis
of diabetes is, in itself, inadequate for determining a person’s driving
capability or safety. In addition, diabetes mellitus is only recorded on the driver’s
licence if the diagnosis already existed at the time the licence was issued (this
applies in particular to young patients with type 1 diabetes mellitus or
monogenetic forms of diabetes). Otherwise, the diagnosis of diabetes is only recorded
on the driver’s licence in the event of a motor vehicle accident; for drivers
aged over 75, all of whom undergo assessment of fitness to drive; for people who drive
a motor vehicle professionally (cab,
truck, bus driver). The majority of people with diabetes mellitus are, therefore,
never registered by road traffic authorities. The treating physician has the
right, but no obligation, to report patients with diabetes mellitus with
reduced fitness to drive to the relevant authorities.
Diabetes-related traffic accidents are rare
for most drivers with diabetes mellitus and occur less frequently than for many
other diseases that can impair driving performance and are tolerated by society.
The incidence of hypoglycaemia, which impairs the ability to drive, severe
retinopathy (including macular oedema) or cataract formation affecting visual
acuity required to drive a motor vehicle, and peripheral neuropathy, which can
severely impair sensation in the feet, is not so common as to justify
restricting driving privileges for all drivers with diabetes mellitus.
Accident risk in
patients with diabetes mellitus
Although the above-mentioned complications
of diabetes mellitus can increase the risk of motor vehicle accidents, incapacitation
from hypoglycaemia poses the highest risk of accidents. The risk exists in
people who are treated with insulin, sulfonylureas or glinides. A study in drivers
treated with insulin concluded that 13% had developed hypoglycaemia while
driving in the previous year [1]. The analysis of various studies has shown
that there is an increased risk of traffic accidents, but it is very modest [2].
A meta-analysis showed that the risk of traffic accidents among drivers with
diabetes mellitus was not higher than among drivers without diabetes mellitus.
Elderly people [3] and those on insulin therapy showed a trend towards an
increased risk, but statistical significance was clearly missed [4]. Some
published studies suggest that drivers with type 1 diabetes have a slightly
higher risk of traffic accidents compared to drivers with type 2 diabetes
(insulin and/or sulfonylureas). A driver with type 2 diabetes has the same risk
as a driver without diabetes [5], but this has not been confirmed by other
studies [6]. Case-control studies have shown that drivers with diabetes
mellitus have only a slightly increased and, therefore, acceptable risk of
motor vehicle accidents compared to drivers without diabetes, but many studies
have significant limitations or are of poor quality. In particular, severe hypoglycaemia
is very common in a very small percentage of patients (especially those with
longstanding diabetes and under insulin therapy) and thus increases the risk of
accidents in the entire group. Older studies may no longer be up-to-date due to
changes in road conditions, motor vehicles and, above all, advances in the
treatment of diabetes mellitus: more and more continuous blood glucose
monitoring [7] in type 1 and type 2 diabetes, hybrid closed-loop insulin
pumps in type 1 diabetes mellitus, no more use of sulfonylureas and much better
ultra-long-acting insulins with a lower risk of hypoglycaemia. However, one
question remains: How frequently does blood glucose need to be measured? An
observational study with a continuous glucose monitoring system (CGMS) has
shown that with a blood or sensor glucose level ≥5 mmol/l at the start of
driving, a blood glucose level <3.9 mmol/l is reached within two hours in
13.8% of patients with type 1 and in 4.4% with type 2 diabetes mellitus treated
with insulin. After 4 hours it is even 22% and 8.4%, respectively [7].
In summary, most drivers with diabetes
safely operate motor vehicles without creating any meaningful risk of injury to
themselves or others. Diabetes mellitus alone is, therefore, not synonymous
with impaired fitness to drive, and the increasing adoption of diabetes technologies
and improved medications are likely to further reduce or prevent the frequency
of hypoglycaemia [8].
Legal basis of guidelines on fitness to drive in
patients with diabetes mellitus compared to other diseases
For other diseases, specific requirements
have been defined by traffic medicine and the relevant professional
associations, and such an approach has also been chosen for diabetes mellitus.
Legal basis
According to Art. 14 of the Road Traffic
Act (SVG), anyone who fulfills the following criteria is allowed to drive a
motor vehicle: is above the minimum age; has the necessary physical and mental
capacity to drive motor vehicles safely; does not have an addiction; and has
the capacity, judged by their previous behaviour, to follow the regulations as
a motor vehicle driver. Fitness to drive describes the general, non-temporal
and non-event-related suitability to drive a vehicle safely. On the other hand,
ability to drive
describes the event-related and time-limited ability to drive a vehicle safely,
based on current physical and mental capacity.
Furthermore, Art. 7 Para. 1 of the Traffic
Licencing Ordinance (VZV) states that anyone wishing to obtain a learner’s permit,
driver’s licence or a permit for professional passenger transport has to meet
the minimum medical requirements
set out in VZV Annex 1.
In the first medical group (categories A,
B, A1, B1, F, G, M and subcategory D1 if acquired under old law [entry 106] and
limited to 3.5 tons), the
minimum requirement mandates that in the presence of diabetes mellitus there
must be stable blood glucose control without hypoglycaemia or hyperglycaemia affecting
driving ability (VZV Annex 1).
In the second medical group (categories C,
D, C1, D1 if not acquired under old law, the permit for professional passenger
transport, traffic experts), the VZV mandates that drivers
are excluded from category D or subcategory D1 if hypoglycaemia may occur as a
side effect of treatment or in which hyperglycaemia may impair the ability to
drive. A permit to drive for category C or subcategory C1, for professional
passenger transport and for traffic experts, may be given under favourable
circumstances (VZV Annex 1).
The local authority may, as an exception, deviate from the
minimum medical requirements according to VZV Art. 7 Para. 3 if the applicant meets
the driving suitability
requirements under SVG Art. 14 Para. 2 and a doctor with level 4 recognition
(Traffic Medicine Specialist of the Swiss Society of Legal Medicine [SSLM])
confirms this. This is always an individual case assessment by the authorities.
According to the reporting right under SVG Art. 15d Para. 3, doctors may report
individuals with a reduced fitness to drive to the local road traffic authority
without violating medical confidentiality.
In summary, there is a legal basis for fitness
to drive, minimum medical requirements for driver’s licence categories and the
possibility of obtaining an exemption-based permit when deviating from the
minimum medical requirements. Hypoglycaemia is
the most important factor that leads to a restriction of driving ability.
Exceptions can be made for drivers with diabetes who can avoid hypoglycaemia
using the most advanced technological methods. Regardless of the reporting
right, a doctor is obliged to inform their patients about driving suitability.
The medical duty of disclosure and pointing out measures for reducing hypoglycaemia
is part of the safety counselling.
Hypoglycaemia and driving ability
The most important factor in diabetes
mellitus that leads to a restriction of driving ability is hypoglycaemia. Hypoglycaemia
only occurs when patients are treated with insulin, sulfonylureas or glinides.
The risk of hypoglycaemia is higher for sulfonylureas with a longer half-life
or with active metabolites. Short-acting glinides and gliclazide, which has no
active metabolites and a relatively short half-life, have the lowest rate of hypoglycaemia.
The same applies to the ultra-long-acting insulins, degludec (Tresiba®)
and glargine 300 (Toujeo®) with more stable pharmacodynamic profiles
[8].
A noticeable change in driving behaviour
was seen in the latest trials examining the influence of hypoglycaemia (both in
simulators and real cars). The lower the glucose concentration (venous blood
sugar <2.5 mmol/l and lasting more than 15 minutes), the more pronounced the
reduction of driving ability. Hypoglycaemia in the range of 3.0 to 3.5 mmol/l
reduced driving ability to a lesser degree. Typical changes include less
proactive driving behaviour, reduced fine motor skills and more-abrupt
reactions. It can be indirectly concluded that blood sugar levels above
this range, and especially above 3.9 mmol/l with stable values, are unlikely to
have a significant impact on driving behaviour [9, 10]. This aligns with
earlier research findings and corresponding international guidelines.
In England and Canada, a blood sugar level
of 4.0 mmol/l before driving is considered safe for patients treated with
insulin. For blood sugar <4.0 mmol/l, it is recommended to immediately stop
the vehicle, remove the ignition key, switch from the driver’s seat to the
passenger seat, correct the low blood sugar with rapidly acting carbohydrates
and wait 45 minutes before resuming the drive [11]. It should also be noted
that when hypoglycaemia is corrected, there may be a lag before a CGMS displays
normal blood sugar values (in case of doubt, a capillary blood glucose
measurement is recommended).
Factors in diabetes mellitus that impair fitness
to drive
Some micro- and macrovascular complications
can lead to impaired driving ability over a prolonged period. The best
predictive factor for development of these complications is glycaemic exposure, expressed
as HbA1c-years (the annual average of
HbA1c values is accumulated and every HbA1c value >6.0% is counted. A
similar approach is used for smoking with “pack-years”). When 50–70 HbA1c-years
are reached, practically all microvascular complications are present [12, 13]. Untreated
arterial hypertension, hypercholesterolaemia, smoking and visceral obesity exacerbate
these
effects. Severe impairment of visual acuity and the visual field due to proliferative
retinopathy and/or macular oedema, or severe peripheral neuropathy of the lower
extremities with loss of sensation, results in inability to properly perceive
and operate the accelerator, brake or clutch pedals. Severe chronic kidney disease
(eGFR <30
ml/min) increases the risk of hypoglycaemia when taking a sulfonylurea or
insulin.
Pregnancy and diabetes (gestational diabetes and
pre-existing diabetes)
Gestational
diabetes is now screened for in all pregnant women
between the 24th and 28th week of pregnancy using a 75 g oral glucose tolerance
test [14, 15]. If the fasting glucose is ≥5.1 mmol/l or the 1-hour value is ≥10.0
mmol/l or the 2-hour value is ≥8.5 mmol/l, gestational
diabetes is diagnosed. It is important to note that the blood glucose
values must be measured venously and determined in a central laboratory. HbA1c is
not suitable for the
diagnosis of gestational diabetes. 15–17%
of all pregnant women have gestational
diabetes or pre-existing diabetes
mellitus [16].
If, during the first prenatal visit, the HbA1c value is ≥6.5%, fasting glucose is
≥7.0
mmol/l or the 2-hour value is ≥11.1
mmol/l, pre-existing diabetes
mellitus is diagnosed. Gestational
diabetes can only be diagnosed before the 24th week of pregnancy with a
fasting blood glucose ≥5.1 mmol/l
[15].
During the first 16 weeks of pregnancy,
insulin sensitivity is increased and potentially more hypoglycaemia occurs with
pre-existing type 1 or insulin-dependent diabetes [17], if the daily insulin dose
is not reduced. From the 20th week of pregnancy, insulin sensitivity decreases and
the total insulin requirement increases accordingly.
From the 20th week of pregnancy, the foetal
pancreas begins to react to maternal blood sugar spikes [18–20]. The
consequence of maternal hyperglycaemia is hyperinsulinaemia (in mother and
child) and macrosomia (in the child). For this reason, the blood glucose target
values in Switzerland from the 20th week of pregnancy have been set at <5.3
mmol/l while fasting and <8.0 mmol/l at 1 hour postprandially
(internationally 7.8 mmol/l or 140 mg/dl) [12]. As approximately 25% of women
with gestational diabetes need to be treated with insulin to achieve these
target levels, driving was difficult to manage with the 2017 recommendations
(blood glucose should never be <5.0 mmol/l before driving). As pregnant
women need to measure blood glucose before every meal and 1 hour after eating
and before sleeping, continuous glucose monitoring is now recommended in this
situation, along with the use of an ultra-long-acting insulin and, if needed, a
short-acting insulin. For women with pre-existing type 1 diabetes mellitus,
therapy with an hybrid closed-loop insulin pump and continuous blood glucose monitoring
is
recommended. This increases the time within the pregnancy target range, 3.5–7.8
mmol/l, and reduces the number of hypoglycaemic episodes <3.5 mmol/l during
all trimesters and, thus, also the rate of macrosomia of the child. The lower
limit for driving ability, 4.0 mmol/l, is the same as outside of pregnancy.
Contribution of continuous glucose monitoring and hybrid
closed-loop insulin pumps as well as ultra-long-acting basal insulins to road
safety
The information density of interstitial continuous
glucose monitoring is several times higher than that of capillary self-monitoring
of blood glucose values. With continuous glucose monitoring, interstitial glucose
concentration is determined every five minutes and a 30-minute prediction is
made. Today, all continuous glucose monitoring systems issue a warning if the
glucose is predicted to fall below a certain value, which can be set
individually. As already mentioned, 2–4 hours after a glucose measurement ≥5.0
mmol/l before driving, the blood glucose drops to a value <3.9 mmol/l in
13.8% of patients with type 1 and in 4.4% of patients with type 2 diabetes
mellitus treated with insulin. After 4 hours it is even 22% and 8.4%,
respectively [7]. This means that with the help of continuous glucose
monitoring, the driver can be warned of hypoglycaemia and can correct the blood
sugar with carbohydrates before hypoglycaemia occurs. It is possible,
therefore, to set the minimum blood glucose levels before driving lower for a continuous
glucose monitoring user than for those using capillary self-monitoring of blood
glucose alone. The latest hybrid closed-loop insulin pumps also help to prevent
hypoglycaemia. In the earliest models, when the hypoglycaemia
value (usually 3.9 mmol/l) was reached, the basal insulin application of the
pump was stopped. A further development step led to the predictive switch-off
of the insulin pump before the occurrence of hypoglycaemia; today these pumps
can automatically correct excessively high blood glucose levels and insulin
delivery is automatically interrupted when the blood glucose level drops. The
only step still missing to achieve a fully automated pump is automatic insulin
delivery before a meal without manual input. Today, the patient still has to inform
the pump of how much carbohydrate he/she is eating and the necessary amount of
insulin is calculated and delivered based on the current blood glucose value
(possibly corrective insulin is added) and the stored carbohydrate factor [21].
In the past, only the HbA1c value and the number of severe hypoglycaemia episodes (level 3; external help required or unconsciousness) were used to assess blood
glucose control. With the latest technologies, there are many factors that need
to be considered (recommended values in brackets): HbA1c value (<7.0%), hypoglycaemia
<3.9 or level 1 (<4%) and hypoglycaemia <3.0 mmol/l or level 2 (<1%),
the coefficient of variation (<36%) and the time spent in the target range
of 3.9–10 mmol/l (>70%). It is even more efficient to assign a score of 1
(worst) to 4 (best) for each of these four factors and then sum the scores to
obtain a single score [22] (table 1).
Table 1Evaluation of continuous glucose
monitoring system (CGMS) blood glucose values [22]. Very good glycaemic control: 14–16
points; good glycaemic control: 11–13 points; sufficient glycaemic control: 9–10 points;
insufficient glycaemic control: <9 points.
| HbA1c (%) |
Coefficient
of variation* (%) |
Hypoglycaemia
<3.0 mmol/l (%) |
Time in
range 3.9–10 mmol/l (%) |
Points |
| <6.5% |
≤25% |
<1% |
≥80% |
4 |
| 6.5–6.9% |
26–35% |
1–4% |
70–79% |
3 |
| 7.0–8.0% |
36–49% |
5–10% |
51–69% |
2 |
| >8.0% |
≥50% |
>10% |
≤50% |
1 |
The most modern continuous glucose
monitoring systems coupled with insulin pumps significantly reduce the number
of hypoglycaemic episodes and the coefficient of variation and, if the HbA1c is
too high, also the HbA1c. This is the reason why certain restrictions on higher
vehicle categories can now be removed as exceptions when using these
technologies. As an example of such an exception: a cab or truck driver with
type 2 diabetes mellitus treated with metformin, a GLP-1 receptor agonist and an
SGTL-2 inhibitor with an HbA1c of 9.0%; he/she needs a basal insulin with the
lowest risk of hypoglycaemia (recommended: degludec or glargine 300) and must
be willing to wear a continuous glucose monitoring device. In this case, the
diabetologist and the department of traffic medicine still have to decide whether
to approve this category,
as a high HbA1c increases the risk of long-term consequences and road traffic
incidents due to the higher risk of cardiovascular events. The same applies to tram,
bus and train drivers.
The new Swiss Society for Endocrinology and
Diabetes (SSED) recommendations for the treatment of type 2 diabetes mellitus changed
as well. The use of sulfonylureas and glinides is no longer recommended. The
recommended antidiabetic agents (metformin, SGLT-2 inhibitors, GLP-1 or
GLP-1/GIP receptor agonists) given alone or in combination do not cause hypoglycaemia.
If insulin has to be used, the ultra-long-acting insulins degludec and glargine
300 are now recommended as they have a significantly lower hypoglycaemic
frequency than glargine 100 or insulin detemir; NPH insulin, which carries the
highest risk of hypoglycaemia among the long-acting insulins, is no longer
recommended.
It has also been shown that with the co-formulated insulin Ryzodeg®
(30% NovoRapid® and 70% Tresiba®), which is given once or
twice daily with the main meals, the same HbA1c can be achieved as with a basal-bolus
regimen but with a much lower rate of hypoglycaemia [8].
Basic guidelines for all driver’s licence holders
with diabetes mellitus
If diabetes mellitus is present, there must
be stable blood sugar control without hypo- or hyperglycaemia relevant to
driving. There must be no other metabolic disorders with a significant impact
on the ability to drive a motor vehicle safely. In particular, there must be no
traffic-relevant secondary complications, which are specified in detail in the first
and second medical group below, and no hyperglycaemia.
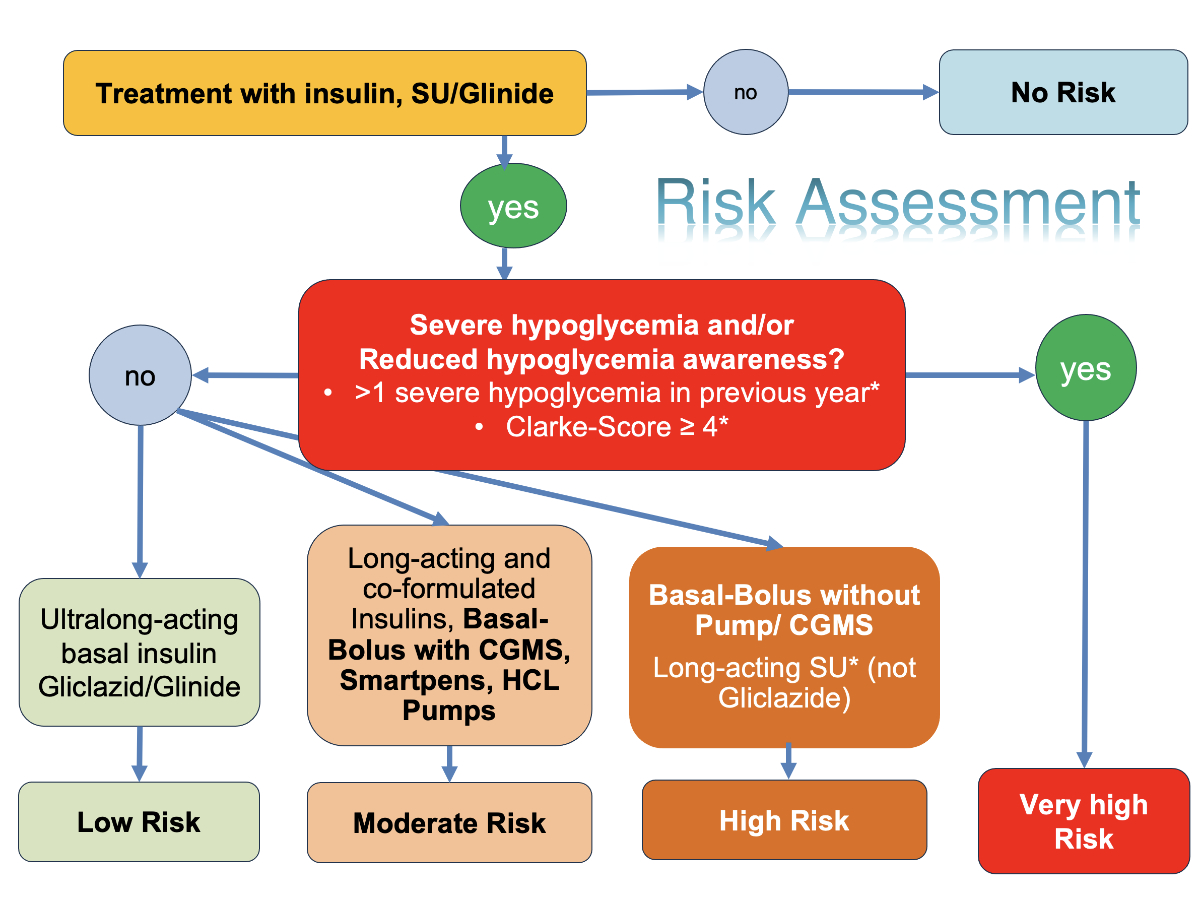
In addition, the individual risk of hypoglycaemia
must be determined for all motor vehicle drivers depending on the type of treatment
with particular emphasis on hypoglycaemia unawareness (figure 1 and table 2). This
results in different recommendations for action depending on the driver’s licence
category, which are listed in the following sections. Special consideration
must be given to whether a continuous glucose monitoring system is worn.
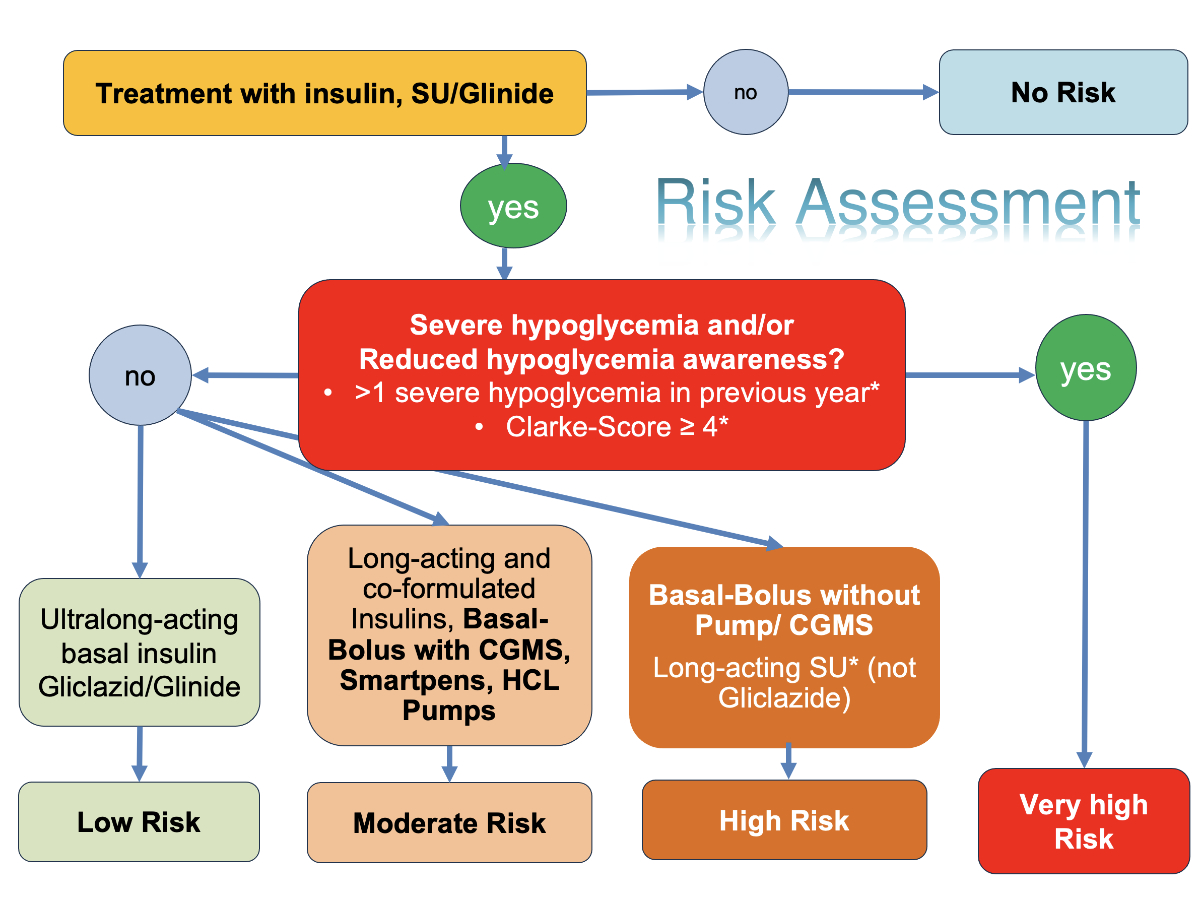
Figure 1Flowchart for assessing the risk of
hypoglycaemia during therapy with insulin or gliclazide/glinides. *
particularly if >70 years of age and with impaired renal function
(estimated glomerular filtration rate [eGFR] <30 ml/min) or with a diabetes
duration >20 years and impaired renal function.
Table 2Overview of risk categories for motor vehicle
drivers with diabetes mellitus.
| Category |
Therapy |
| No risk |
Metformin, GLP-1 receptor agonists,
GLP-1/GIP-receptor agonists, DPP-4 inhibitors, SGLT-2 inhibitors or their
combination |
| and |
| No therapy with insulin, sulfonylureas or
glinides |
| Low risk |
Ultralong-acting basal insulins (degludec/glargine
300) |
| or |
| Gliclazide or glinides |
| Intermediate risk |
Long-acting insulins (glargine U100, detemir)
|
| Co-formulated insulin Ryzodeg® 1–2× daily |
| or |
| Basal-bolus insulin therapy (incl. smart
pens) with continuous glucose monitoring systems (CGMS) |
| or |
| Hybrid closed-loop insulin pump systems
(HCL) |
| High risk |
Basal-bolus insulin therapy without CGMS |
| or |
| Non-hybrid closed-loop insulin pump systems |
| or |
| Long-acting sulfonylureas (not gliclazide/glinides) |
| Very high risk |
≥1 severe hypoglycaemia/year and/or
hypoglycaemia unawareness (Clarke Score 4 or higher) |
For the treating physician, it is crucial
to ask about severe hypoglycaemia, since a very high percentage of patients do
not mention hypoglycaemia spontaneously. The Clarke score (in the appendix) can
also be used to assess hypoglycaemia awareness. It is the joint responsibility
of the treating physician and the patient to avoid severe hypoglycaemia, as
this can also lead to serious consequences apart from those affecting driving: higher
risk of dementia, more cardiovascular events (including sudden cardiac death),
increased risk of thrombosis and more systemic inflammatory reactions [23].
Guidelines for driver’s licence holders of the first
medical group (A, B, A1, B1, F, G, M and C1 for private use)
The following conditions must be met for
initial registration or continued registration as a motor vehicle driver in the
first medical group:
- No traffic-relevant diabetes complications
(diabetic eye disease impairing vision, nephropathy, neuropathy, no
traffic-relevant macrovascular complications)
- No traffic-relevant
restrictions in the cardiovascular system
- No significant long-term hyperglycaemia (no approval or further approval with HbA1c >10%)
Behaviour before and during driving
In case of treatment with low risk of hypoglycaemia
(i.e. ultra-long-acting basal insulin, gliclazide or glinides), blood glucose measurements
before driving and during longer trips are not required. However, a blood
glucose meter and carbohydrates as hypoglycaemia prophylaxis have to be in the
vehicle.
In case of treatment with intermediate risk
of hypoglycaemia, we differentiate between the following situations:
- In the case of treatment with
long-acting insulins (glargine U100 / detemir), co-formulated insulin (70% degludec
and 30% insulin aspart [Ryzodeg®]) or if no continuous glucose
monitoring system (CGMS) is used, blood glucose has to be measured before driving
and regularly during longer trips (at least every 2 hours) [7]. If the blood
sugar is <4.0 mmol/l, it must be corrected by taking carbohydrates before
starting or continuing driving. A 45-minute break must be taken. If the blood
sugar is 4–5 mmol/l, 10–20 g of carbohydrates have to be consumed.
- In the case of a basal-bolus
insulin regimen with a continuous glucose monitoring system (CGMS) or hybrid
closed-loop insulin pump system, blood glucose measurements before or
during the journey are not necessary, as these systems have an alarm function.
If the CGMS shows a downward trend in blood glucose with a risk of hypoglycaemia,
this must be corrected early by taking carbohydrates. If the blood glucose is <4.0
mmol/l, carbohydrates must be immediately consumed. Afterwards, a waiting
period of at least 45 minutes is required before driving can be resumed (in
case of doubt, a capillary blood glucose measurement is recommended).
In case of treatments with high risk of hypoglycaemia
(basal-bolus insulin therapy without CGMS, non-hybrid closed-loop insulin pump systems,
long-acting sulfonylureas), the blood glucose must be measured before driving
and regularly (at least every 2 hours) [7] during longer car trips. If the
blood glucose is <5.0 mmol/l, it must be corrected by taking carbohydrates
before starting or continuing the journey. Furthermore, for the initial or
continued approval as a motor vehicle driver in the first medical group, in
addition to the conditions mentioned in the chapter
“Hypoglycaemia and driving ability” (no
traffic-relevant late complications, HbA1c <10%), the following conditions
must be met:
- Stable blood glucose control over the past year without severe hypoglycaemia (Grade III) and
without hypoglycaemia unawareness.
- Stable ability to reliably
avoid hypoglycaemia while driving (i.e. the ability
to measure blood glucose before driving and regularly on longer journeys).
- Adherence to behavioural
guidelines, particularly: The blood glucose must be
≥5.0 mmol/l before driving and during longer trips (if no CGMS is used) or ≥4.0
mmol/l (if a CGMS is used). If the blood glucose is <5.0 mmol/l (without
CGMS) or <4.0 mmol/l (with CGMS), carbohydrates must be consumed immediately.
If blood glucose is <4.0 mmol/l, a waiting period of at least 45 minutes is
required before resuming driving (in case of doubt, a capillary blood glucose
test is recommended).
At the
beginning of a treatment with a higher risk of hypoglycaemia, fitness to drive is
only considered valid once the aforementioned
conditions are met and, in particular, it is ensured that hypoglycaemia can be
reliably avoided while driving a motor vehicle.
In case of very high risk of hypoglycaemia (≥1
severe hypoglycaemia grade III per year
and/or hypoglycaemia unawareness), a special assessment by a specialist
in endocrinology/diabetology is required.
After an episode of severe hypoglycaemia (grade
III) for
holders of a driver’s licence in the first medical group, ability to drive is
only granted under the condition of wearing a continuous glucose monitoring
system (CGMS) or performing 6–8 capillary blood glucose measurements daily for at least one year.
The measures required for each hypoglycaemia
risk level when driving motor vehicles for drivers in the first medical group
are summarised in table 3.
Table 3Risk of hypoglycaemia
and required measures, first medical group (A, B, A1, B1, F and C1 for private
use).
| Category |
Therapy |
Action |
| No risk |
Metformin, GLP-1 receptor agonists,
GLP-1/GIP-receptor agonists, DPP-4 inhibitors, SGLT-2 inhibitors or their
combination and no therapy with insulin, sulfonylureas or glinides |
No blood glucose measurement necessary
before or during the journey |
| Low risk |
Ultralong-acting basal insulins (degludec/glargine
U300) or gliclazide or glinides |
No blood glucose measurement necessary
before or during each trip |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| Intermediate risk |
Long-acting insulins (glargine 100, detemir)
or Ryzodegâ once or twice daily or basal-bolus insulin
therapy (including smart pens) with continuous glucose monitoring systems
(CGMS) or hybrid closed-loop insulin pump systems (HCL) |
Capillary blood glucose measurement before
each trip |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| CGMS: No capillary blood sugar
measurements, due to provision of predictive low glucose alerts |
| If blood glucose <4.0
mmol/L, correct with rapid-acting carbohydrates and wait for 45 minutes |
| High risk |
Basal-bolus insulin therapy without CGMS or
non-hybrid closed-loop insulin pump systems or long-acting sulfonylureas (not
gliclazide/glinide) |
Capillary blood glucose measurement before
driving and during longer trips |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| _Hlk168493418If capillary
blood glucose 4–5 mmol/L, correct with 10–20 g carbohydrates |
| No driving if capillary blood glucose <4.0
mmol/L |
| If capillary blood
glucose <4.0 mmol/L, correct with rapid-acting carbohydrates and wait for
45 minutes |
| Very high risk |
≥1 severe hypoglycaemia/year and/ or
hypoglycaemia unawareness (Clarke Score 4 or higher) |
Assessment by a
specialist in endocrinology/diabetology |
| Ability
to drive only with continuous blood glucose monitoring (CGMS) or 6–8 capillary blood
glucose measurements
daily |
| Hypoglycaemia
prophylaxis and blood glucose meter in the vehicle |
| If blood glucose <5.0
mmol/L, correct with carbohydrates |
| No driving if blood
glucose <5.0 mmol/L |
| If blood glucose <4.0
mmol/L, correct with rapid-acting carbohydrates and wait for 45 minutes |
Guidelines for driver’s licence holders of the second
medical group (D, D1, C, C1, professional passenger transport permit [BPT],
traffic experts)
For the initial registration or renewal of
a driver’s licence in the second group, the following conditions must be met
for individuals with diabetes mellitus:
- No
traffic-relevant diabetes complications (diabetic eye
disease impairing vision, nephropathy, neuropathy, no traffic-relevant
macrovascular complications).
- No
traffic-relevant restrictions in the cardiovascular system and no traffic-relevant
impairment of kidney function with a significant impact on general health.
- No
significant hyperglycaemic derangement
(no issuance or renewal of the driving licence, if HbA1c >8.5%)
Therapy with risk of hypoglycaemia
Fitness to drive may be granted under
particularly favourable circumstances under the same conditions as in the first
medical group. Specifically, the following applies:
Categories D and D1
According to minimum medical requirements, fitness
to drive for categories D and D1 is excluded.
Suitability to drive for categories D and
D1 can be assessed by a permission level 4 physician as an exception permit
according to Article 7, Paragraph 3 of the Road Traffic Ordinance (VZV),
provided the following conditions are met:
- Treatment and monitoring by a
specialist in endocrinology and diabetology.
- Type 1
diabetes with hybrid closed-loop insulin pump therapy and continuous
glucose monitoring, or
- Type 2
diabetes with ultra-long-acting basal insulin and the use of a continuous
glucose monitoring system.
- No
severe hypoglycaemia in the last twelve months.
- Hybrid
closed-loop insulin pump therapy and continuous glucose monitoring (type
1 diabetes), or continuous glucose monitoring (type 2 diabetes) for at least
three months.
- Preserved
hypoglycaemia awareness (Clarke Score <4).
- Confirmation
from the treating specialist in endocrinology and diabetology that the affected
person has been trained and is proficient in the use of hybrid closed-loop
insulin pump therapy and continuous glucose monitoring (for type 1
diabetes) or continuous glucose monitoring (for type 2 diabetes).
Categories C and
C1, Permit for Professional Passenger Transport (BPT),
Traffic Experts
For categories C and C1, for the permit for
professional passenger transport, as well as for traffic experts, fitness to
drive is granted under the following conditions:
- Stable glucose control with a
therapy that does not result in hypoglycaemia (i.e. a therapy other than insulin,
sulfonylureas/glinides).
- Stable ability to prevent hypoglycaemia
and regular glucose monitoring at low, medium, high and very high hypoglycaemia
risk (table 4).
- There must always be an
assessment by a specialist in endocrinology/diabetology and an evaluation by a
traffic specialist (physician with at least permission level 3).
Table 4Hypoglycaemia risk and required measures, 2nd
medical group (D, D1, C, C1, permit for professional passenger transport,
traffic experts).
| Category |
Therapy |
Action |
| No risk |
Metformin, GLP-1 receptor agonists,
GLP-1/GIP-receptor agonists, DPP-4 inhibitors, SGLT-2 inhibitors or their
combination |
No blood glucose measurement
necessary before or during the trip |
| Low risk |
Ultralong-acting basal insulins (degludec/glargine
300) or gliclazide or glinides |
No suitability to drive for driving license
categories D and D1; exception permit as mentioned above, traffic medical
assessment by level 4 is mandatory |
| Capillary
self-monitoring of blood glucose levels 3–4 times daily (or CGMS) |
| No blood glucose measurement necessary
before or during each trip |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| Assessment by a specialist in
endocrinology/diabetology and evaluation by a traffic specialist (physician
with at least permission level 3) |
| Intermediate risk |
Long-acting insulins (glargine 100, detemir)
or Ryzodeg® once or twice daily or basal-bolus insulin
therapy (including smart pens) with continuous glucose monitoring systems
(CGMS) or hybrid closed-loop insulin pump systems (HCL) |
No suitability to drive for driving license
categories D and D1; exception permit as mentioned above, traffic medical
assessment by permission level 4 physician is mandatory |
| Blood glucose measurement before each trip |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| CGMS: No capillary blood sugar
measurements, since alarm function |
| If capillary blood
glucose <4.0 mmol/L, correct with rapid-acting carbohydrates and wait for
45 minutes |
| Assessment by a specialist in endocrinology/diabetology
and evaluation by a traffic specialist (physician at least permission level
3) |
| High risk |
Basal-bolus insulin therapy without CGMS or
non-hybrid closed-loop insulin pump systems or long-acting sulfonylurea (not
gliclazide/glinide) |
No suitability to drive for driving license
categories D and D1 |
| Normally 3 months’ waiting time |
| Capillary blood glucose measurement before
driving and during longer trips |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| If capillary blood glucose 4–5 mmol/L,
correct with 10–20 g carbohydrates |
| No driving if capillary blood glucose <4
mmol/L |
| Assessment by a specialist in
endocrinology/diabetology and evaluation by a traffic specialist (physician
at least permission level 3) |
| Very high risk |
≥1 severe hypoglycaemia/year and/or hypoglycaemia
unawareness (Clarke Score 4 or higher) |
No ability to drive for driving license
categories D and D1 |
| Waiting time of normally 3 months without
severe hypoglycaemia |
| Use of a continuous glucose monitoring
system (CGMS) |
| Capillary blood glucose measurement before
driving and during longer trips |
| Hypoglycaemia prophylaxis and blood glucose
meter in the vehicle |
| No driving if capillary blood glucose <5
mmol/L |
| Close monitoring and assessment by a
specialist in endocrinology/diabetology and evaluation by a traffic
specialist (permission level 4 physician) |
Required intervals for issuing
a certificate for road traffic authorities
The control interval for diabetes
management is determined by the treating physician. The better the glycaemic
control, the longer the control interval can be. The following general
guidelines apply:
- Newly diagnosed type 2 diabetes
without insulin or sulfonylurea treatment: Check-ups with the doctor to
determine HbA1c, assess self-monitoring of blood glucose or continuous glucose
monitoring system every 3–4 months, annual measurement of eGFR and albuminuria,
and peripheral neuropathy using a reflex hammer, vibration test at the base
joint of the big toe (first metatarsal joint) and with a monofilament. Annual
to every two year report from the ophthalmologist, including visual acuity,
visual field and retinopathy grade. A certificate for the road traffic authority
every 3 years is sufficient. With optimal conditions, this interval can be
extended to 5 years.
- Newly diagnosed type 1 diabetes
mellitus: Motivation for the use of CGMS (continuous glucose monitoring system)
and also the use of a hybrid closed-loop insulin pump. Check-ups as for newly diagnosed
T2DM but with a diabetologist. First
ophthalmologist’s report to be requested after 5 years then, depending on the
ophthalmologist’s assessment, at least once every 1–2 years. The interval for
the certificate to the road traffic authority is initially 1 year; with optimal
conditions and no severe hypoglycaemia, every 3 years, and in the best case,
every 5 years.
- For longstanding type 1 or type
2 diabetes: Check-ups with the diabetologist (for type 1 diabetes) or with the general
practitioner (for type 2 diabetes) every 3 to 4 months, along with monitoring of
the parameters mentioned above. At least once a year, a report from the
ophthalmologist is required. The interval for the certificate to the road
traffic authority depends on the existing complications of diabetes, blood
sugar control and severe hypoglycaemia: ideally every 5 years, otherwise every
3 years or annually if blood sugar control is insufficient.
- Higher categories (second
medical group, which excludes C1 for private use): Certificate interval is annually.
Conclusions
In recent years, several pharmacological
and technological innovations have revolutionised diabetes care. Continuous glucose
monitoring system
(CGMS) technology was developed in 1999, but it has only recently become
increasingly integrated into diabetes therapy. Today, except for insulin, none
of the treatments recommended for type 2 diabetes mellitus causes hypoglycaemia,
and the risk of hypoglycaemia with ultra-long-acting insulins is lower. As a
result, recommendations for driving motor vehicles have had to be adjusted [8].
Since hypoglycaemia is the greatest risk factor for impaired driving ability,
the latest technology (CGMS coupled with hybrid closed-loop insulin
pumps) is able to reduce the number of hypoglycaemic events and blood glucose
fluctuations. In addition, HbA1c and time in target range can be improved. Patients
with type 1 diabetes mellitus are now, in exceptional cases, allowed to hold a
licence in higher vehicle categories.
With the analysis of CGMS data, an
objective assessment of the frequency of hypoglycaemia grade 1 and 2 is now
possible (table 1), which was previously only partially possible with blood
glucose logs (not all hypoglycaemia episodes were recorded, particularly nocturnal
hypoglycaemia or were not entered in the glucose control logs).
The Federal Office of Public Health has
thus far set the indications for reimbursement of continuous glucose monitoring
systems rather high. However, as the prices of these systems have fallen or are
expected to fall further, this working group believes that every patient with
type 1 diabetes mellitus who accepts technology should have access to an hybrid closed-loop
pump coupled with CGMS. Likewise, patients who are treated with insulin should
also have the opportunity to use a CGMS. This also applies to gestational diabetes
and diabetes during pregnancy. Since these systems warn of impending hypoglycaemia,
they will also improve road safety, and the safety margin for blood glucose,
which was previously set at 5 mmol/l, can be lowered to 4 mmol/l. With these
new recommendations, all driver’s licence holders are able to achieve the blood
glucose control recommendations of the SSED, including pregnancy; for CGMS
users, blood glucose measurements every 2 hours while driving are no longer
necessary.
If hypoglycaemia occurs during driving, the
vehicle must immediately be pulled over to the side of the road, the hazard
lights turned on, the car key removed and the driver must move to the passenger
seat. The hypoglycaemia should be corrected with rapid-acting carbohydrates
(emergency supply in the car). Since the brain takes longer to fully regain its
responsiveness after prolonged hypoglycaemia, a waiting period of 45 minutes is
required before continuing driving. With the use of technology, such situations
should become significantly rarer (especially when CGMS is coupled with hybrid closed-loop
insulin pumps).
Prof. Roger Lehmann
Department of Endocrinology, Diabetes and Clinical Nutrition
University
Hospital Zurich
CH-8091
Zurich
roger.lehmann[at]usz.ch
References
1. Graveling AJ, Warren RE, Frier BM. Hypoglycaemia and driving in people with insulin-treated
diabetes: adherence to recommendations for avoidance. Diabet Med. 2004 Sep;21(9):1014–9.
doi: https://doi.org/10.1111/j.1464-5491.2004.01288.x
2. Inkster B, Frier BM. Diabetes and driving. Diabetes Obes Metab. 2013 Sep;15(9):775–83.
doi: https://doi.org/10.1111/dom.12071
3. Kagan AH, Hashemi G, Korner-Bitensky N. Diabetes Fitness to Drive: A Systematic Review
of the Evidence with a Focus on Older Drivers. Can J Diabetes. 2010;34(3):233–42.
doi: https://doi.org/10.1016/S1499-2671(10)43012-9
4. Hostiuc S, Negoi I, Hostiuc M. Diabetes and collision risk. A meta-analysis and meta-regression.
Int J Clin Pract. 2016 Jul;70(7):554–68. doi: https://doi.org/10.1111/ijcp.12832
5. Cox DJ, Penberthy JK, Zrebiec J, Weinger K, Aikens JE, Frier B, et al. Diabetes and
driving mishaps: frequency and correlations from a multinational survey. Diabetes
Care. 2003 Aug;26(8):2329–34. doi: https://doi.org/10.2337/diacare.26.8.2329
6. Stork AD, van Haeften TW, Veneman TF. Diabetes and driving: desired data, research
methods and their pitfalls, current knowledge, and future research. Diabetes Care.
2006 Aug;29(8):1942–9. doi: https://doi.org/10.2337/dc05-2232
7. Rayman G, Kröger J, Bolinder J. Could FreeStyle Libre™ sensor glucose data support
decisions for safe driving? Diabet Med. 2018 Apr;35(4):491–4. doi: https://doi.org/10.1111/dme.13515
8. Gastaldi G, Lucchini B, Thalmann S, Alder S, Laimer M, Brändle M, et al.; Working
group of the SGED/SSED. Swiss recommendations of the Society for Endocrinology and
Diabetes (SGED/SSED) for the treatment of type 2 diabetes mellitus (2023). Swiss Med
Wkly. 2023 Apr;153(4):40060. doi: https://doi.org/10.57187/smw.2023.40060
9. Lehmann V, Zueger T, Maritsch M, Kraus M, Albrecht C, Bérubé C, et al. Machine learning
for non-invasive sensing of hypoglycaemia while driving in people with diabetes. Diabetes
Obes Metab. 2023 Jun;25(6):1668–76. doi: https://doi.org/10.1111/dom.15021
10. Lehmann V, Zueger T, Maritsch M, Notter M, Schallmoser S, Bérubé C, et al. Machine
learning to infer a health state using biomedical signals – detection of hypoglycemia
in people with diabetes while driving real cars. NEJM AI. 2024 Jan;1(3): 10.1056/AIoa2300013
11. Diabetes UK. Know Diabetes. Fight Diabetes. Driving and diabetes – What healthcare
professionals should know. Available from: https://www.diabetes.org.uk/for-professionals/get-involved/news-and-updates/driving-and-diabetes--what-healthcare-professionals-should-know
12. Orchard TJ, Dorman JS, Maser RE, Becker DJ, Drash AL, Ellis D, et al. Prevalence of
complications in IDDM by sex and duration. Pittsburgh Epidemiology of Diabetes Complications
Study II. Diabetes. 1990 Sep;39(9):1116–24. doi: https://doi.org/10.2337/diab.39.9.1116
13. Hatz K, Minder AE, Lehmann R, Drescher T, Gerendas B, Schmidt-Erfurth U, et al. The
prevalence of retinopathy in patients with type 1 diabetes treated with education-based
intensified insulin therapy and its association with parameters of glucose control.
Diabetes Res Clin Pract. 2019 Feb;148:234–9. doi: https://doi.org/10.1016/j.diabres.2019.01.016
14. Lehmann R, Troendle A, Brändle M; Schweizerischen Gesellschaft für Endokrinologie
und Diabetologie. [New insights into diagnosis and management of gestational diabetes
mellitus: recommendations of the Swiss Society for Endocrinology and Diabetes]. Ther
Umsch. 2009 Oct;66(10):695–706. doi: https://doi.org/10.1024/0040-5930.66.10.695
15. Sweeting A, Wong J, Murphy HR, Ross GP. A Clinical Update on Gestational Diabetes
Mellitus. Endocr Rev. 2022 Sep;43(5):763–93. doi: https://doi.org/10.1210/endrev/bnac003
16. Group HS; HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy
Outcome (HAPO) Study: associations with neonatal anthropometrics. Diabetes. 2009 Feb;58(2):453–9.
doi: https://doi.org/10.2337/db08-1112
17. Nielsen LR, Pedersen-Bjergaard U, Thorsteinsson B, Johansen M, Damm P, Mathiesen ER.
Hypoglycemia in pregnant women with type 1 diabetes: predictors and role of metabolic
control. Diabetes Care. 2008 Jan;31(1):9–14. doi: https://doi.org/10.2337/dc07-1066
18. Grasso S, Palumbo G, Rugolo S, Cianci A, Tumino G, Reitano G. Human fetal insulin
secretion in response to maternal glucose and leucine administration. Pediatr Res.
1980 May;14(5):782–3. doi: https://doi.org/10.1203/00006450-198005000-00016
19. Obenshain SS, Adam PA, King KC, Teramo K, Raivio KO, Räihä N, et al. Human fetal insulin
response to sustained maternal hyperglycemia. N Engl J Med. 1970 Sep;283(11):566–70.
doi: https://doi.org/10.1056/NEJM197009102831104
20. Jovanovic L. Medical nutritional therapy in pregnant women with pregestational diabetes
mellitus. J Matern Fetal Med. 2000;9(1):21–8. doi: https://doi.org/10.1002/(SICI)1520-6661(200001/02)9:1<21::AID-MFM6>3.0.CO;2-P
21. Kowalski A. Pathway to artificial pancreas systems revisited: moving downstream. Diabetes
Care. 2015 Jun;38(6):1036–43. doi: https://doi.org/10.2337/dc15-0364
22. Lehmann R. Technologie bei der Behandlung des Diabetes mellitus Typ 1: ersetzt das
künstliche Pankreas das traditionelle Basis-Bolus-System? Diabetes Stoffwechs Herz.
2019;28(2):98–101.
23. Snell-Bergeon JK, Wadwa RP. Hypoglycemia, diabetes, and cardiovascular disease. Diabetes
Technol Ther. 2012;14 Suppl 1(Suppl 1):S51-8. doi: https://doi.org/10.1089/dia.2012.0031
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4665.