Association between a mismatch of maternal/neonatal body size and obstetrical interventions
in Switzerland in the 1920s: a cross-sectional study
DOI: https://doi.org/https://doi.org/10.57187/s.4546
Nora Haaga,
Mathilde Le Vuab,
Adrian V. Jaeggia,
David Baudcd,
David Desseauvece,
Martin
Haeuslera,
Kaspar Stauba,
Katarina L. Matthesa
a Institute of Evolutionary Medicine, University of Zurich, Zurich, Switzerland
b Research Institute for Environmental and Occupational Health (Irset), UMR_S 1085,
National Institute of Health and Medical Research (INSERM), University of Rennes and
EHESP School of Public Health, Rennes, France
c Materno-Foetal and
Obstetric Research Unit, Woman-Mother-Child Department, University Hospital of
Lausanne (CHUV), Lausanne, Switzerland
d University of Lausanne (UNIL), Lausanne, Switzerland
e Obstetric
Units, Child Couple University Hospital, University of
Grenoble, Grenoble, France
Summary
INTRODUCTION: Human
childbirth remains a complex and risky process for both mothers and infants,
even with modern advancements in medical care. This study investigated the
prevalence of obstetric interventions, namely caesarean sections, episiotomies,
and forceps deliveries, along with the role of maternal-foetal body size mismatch
in influencing delivery outcomes.
METHODS: Utilising
two datasets from similar archival sources in two Swiss cities (Basel and
Lausanne) from the 1920s, we explored the relevance of a mismatch between the body
size of the mother
and the foetus as a risk factor for obstetrical interventions and the duration
of the expulsion phase during delivery.
RESULTS: Over 91%
of births (1290/1407 in Basel and 1062/1145 in Lausanne) featured the foetal
head in a normal position (either the right or left occiput anterior position).
Episiotomies were performed in 8–17% of cases (233/1407 in Basel and 98/1145 in
Lausanne) and forceps deliveries in 1–5% (17/1407 in Basel and 54/1145 in
Lausanne). Caesarean sections were rare (<1%, 19/1407 in Basel and 6/1145 in
Lausanne). Key findings indicated that larger foetal head diameters and
narrower pelvic measurements were linked to prolonged expulsion phases and an
increased likelihood of intervention. Abnormal head positions and first-time
births were also associated with obstetrical interventions. Additionally,
rickets was documented in 2% of mothers (23/1145) in Lausanne, correlating with
increased forceps use and caesarean section rates.
CONCLUSION: This
research provides insights into obstetric practices and maternal health
conditions over a century ago, emphasising the significant impact of maternal-foetal
body size mismatches on childbirth complications in a historical context.
Introduction
Human
childbirth is a complex process, and despite improved medical care, it is still
associated with risks for both the mother and child. In the worst cases, it can
be fatal for both. The global burden of maternal morbidity and mortality
remains high despite progress in recent decades
[1]. An estimated 295,000 maternal deaths occurred
worldwide in 2017. The global maternal mortality ratio (MMR) was estimated at
211 per 100,000 live births in 2017, a 38% reduction from 2000, when it was 342
per 100,000 [2]. However, there are important geographical
disparities, which have been even more pronounced since the 1990s, as the
burden of maternal mortality is very high in developing countries [1]. The UN has
therefore explicitly included reducing
maternal mortality worldwide in the Sustainable Development Goals (SDG Goal
3.1) [3]. Approximately 73% of maternal deaths
between 2003 and 2009 were due to direct obstetric causes (e.g. abortion,
embolism, intrapartum haemorrhage, hypertension, and pregnancy-related sepsis)
and indirect causes (e.g. pre-existing medical conditions and HIV-related
maternal deaths) [4]. Neonatal health (e.g.,
stillbirths and neonatal morbidities or deaths) is closely related to maternal
health and remains a major health problem, particularly in developing countries
[5].
The
traditional explanation for the uniquely precarious birth process of modern
humans compared with that of other mammals is the obstetrical dilemma
hypothesis [6]. It describes an evolutionary compromise
between the selection pressures for giving birth to a large-brained foetus and
our pelvic adaptations for walking upright, which led to a shortened hipbone
compared with that of our common ancestor with chimpanzees and bonobos.
However, many other explanations have been suggested, and the obstetrical
dilemma hypothesis remains debated [7–11]. In general, many factors determine whether
a
birth is complicated. On the infant’s side, factors that can affect delivery include
neonatal weight, length, head circumference, position, and gestational age [9, 12].
For example, it is well documented that an infant’s birth weight is
associated with gestational age and the mother’s height and body shape: taller women
and those with obesity generally give birth to larger, heavier infants [13–17]. Pelvic
dimensions are also major maternal factors that influence the
birth process [13, 15–17]. However, the relationship between
maternal height and pelvic size is complex. Short women can have large pelvises
[18, 19]. In particular, a potential mismatch between the foetus’s
and the mother’s body dimensions in the form of cephalopelvic disproportion is
relevant to the course of birth [20]. Depending on geographical region and its exact
definition, cephalopelvic disproportion is estimated to affect between 1% and
8% of women giving birth each year [20].
It is more common in heavier
neonates (>4000 g) and even more so in infants with larger head sizes [21, 22].
These factors, among others, cause
obstructed labour and other birth complications such as shoulder dystocia, and they
prompt hospital obstetricians to perform medical interventions such as episiotomy
(i.e., a surgical incision of the perineum and the posterior vaginal wall) or caesarean
sections to minimise maternal and neonatal risks [23].
According to the Swiss Federal Statistical Office, in 2017, 32.3% of all births
in Switzerland were caesarean sections (51.1% planned and 49.9% emergency caesarean
sections). Vaginal operative deliveries (mainly using a vacuum cup) were
performed in 11.1% of all births. Episiotomies were performed in 17% of all
vaginal births, mainly in cases of instrumental births [24].
In caesarean sections, obstructed labour due to maternal pelvic abnormalities
was one of the most important reasons (this diagnosis was 72.6 times more
common in caesarean sections than in vaginal deliveries) [25].
However, obstetric practice has
changed significantly over the past 100 years [26, 27].
At the beginning of the 20th century, fewer than 1% of all births at
the Maternity Hospital in Lausanne were caesarean sections, but other
interventions were much more common. An important determinant for these
interventions was a tight and small pelvis (at the Maternity Hospital in Basel,
9.3% of births between 1895 and 1907 were assessed by contemporary physicians
as involving a narrow pelvis) [28]. As late as
the mid-20th century, external dimensions of the pelvis were used as
indicators of internal dimensions and size of the birth canal, with relatively
good agreement [29–31]. A century ago, mean
maternal skeletal dimensions, such as stature, were different from today’s
standards. In Switzerland at the beginning of the 20th century,
people were 10–15 cm shorter on average than today. Apart from the lower
standard of living, this was due to widespread iodine deficiency and rickets [32–36].
In addition, undernutrition was more common
than overnutrition. Whether the body dimensions of infants were also smaller
during the late 19th and the first half of the 20th century is unclear
in the literature [36–39].
Before the rise in living standards in
the 20th century, conditions of scarcity were relatively common in countries
that are now considered developed [40]. For
some newly developing countries and regions, malnutrition and conditions such
as rickets and iodine deficiency remain a problem. In addition, optimal
obstetric care is not always available within a reasonable timeframe,
especially in remote areas. For settings where caesarean sections are performed
only in exceptional emergencies, the knowledge of risk factors related to
maternal and infant size disparities is helpful. Historical data from developed
countries can provide valuable information. However, few contemporary studies
have used this information, despite rich data in European maternity hospital
archives from the early 20th century. In this study, we digitised
and analysed extensive, nearly complete information on 2500 births collected in
the early 1920s in the maternity hospitals of Lausanne and Basel. These two
sites were chosen for their wealth of data.
We
addressed the following research questions: How common were obstetric
interventions such as caesarean sections, episiotomies, and forceps deliveries?
Was the mismatch between the mother’s body size and the foetus’s body size a
relevant risk factor for such interventions and for the duration of the
expulsion phase during delivery (as a proxy for a complicated birth)? We
approached these questions through the lens of historical epidemiology and
evolutionary medicine using quantitative methods rather than classical approaches
in medical history. Therefore, a comprehensive qualitative text analysis of
obstetric textbooks is outside the scope of this paper.
Data and methods
Historical context of the data
The early 1920s marked a transitional
phase after the crisis years at the end of the First World War and the 1918–19
influenza pandemic (“Spanish flu”). Switzerland was not directly
involved in WWI but was affected by major economic disruptions. Although the
socioeconomic conditions during the final years of the war (1917 and 1918) were
not severe enough to cause famine (as in Russia), adverse effects on
nutritional status in general and neonatal health were evident. The 1918–19
influenza pandemic likely exacerbated these effects [14,
38, 41]. In a longer-term context, Switzerland was already one of the
wealthiest countries in Europe in terms of gross domestic product (GDP) at the
beginning of the 20th century [42].
This article focuses on two medium-to-large cities in southwest and northwest
Switzerland: French-speaking Lausanne (70,000 inhabitants in 1925) and
German-speaking Basel (145,000 inhabitants in 1925). Other indicators of the
standard of living also showed an upward trend during this period: overall mortality
rates, particularly infant and child mortality, declined. Life expectancy
increased, and the health burden due to infectious diseases declined [42–45]. Using
average height as an indicator of the
standard of living, Switzerland approximately corresponded to the central
European average at the beginning of the 20th century. Comparable
sources for this paper present data from women born between 1890 and 1899 with
an average height of 158–162 cm [33].
The maternity hospitals in Lausanne and Basel
This study takes advantage of the fact
that all births in large Swiss maternity hospitals were carefully documented
and preserved in the early 20th century. At that time, Switzerland
had only a handful of maternity hospitals. The hospitals in Lausanne and Basel,
the two with the most data, were included. In both cities, the cantonal
maternity hospitals were the only maternity hospitals in the city. Both
hospitals’ birth registers include births to women from the upper and lower
socioeconomic classes and both complicated and uncomplicated births.
The cantonal hospital of Lausanne
became a university hospital with the opening of the medical faculty of the
University of Lausanne in 1890 [46–50]. Since
the 1890s, there have been no specific restrictions on admissions [51]. Over the years,
an increasing proportion of
all births in the city took place in this hospital. Most of these births were
to parents from the city and its immediate surroundings. A comparison of the
number of births in the registers with the official birth statistics shows that
in 1910, 37% of all births in the city of Lausanne took place in this hospital,
and in 1920, the proportion increased to 66% [52].
In Basel, the Chair of Gynaecology and Obstetrics was established at the
university in 1887. Most patients (>85%) were residents of the city of
Basel. Around 1920, 60% of all births in Basel took place at the university
hospital [14].
This study combines two similar
datasets from identical archival sources to address the research questions. For
the Lausanne dataset, individual data were transcribed from the birth records
of the Canton of Vaud Maternity Hospital (Archives cantonales vaudoises, K VIII
e 256–262, 1922). This series of archives covers full calendar years. In the
books, each birth record extends over four pages and contains much precise
information about the mother, the infant, and the birth itself. A total of 1145
cases were used from the archive books in 1922 (excluding non-birth-related
cases, miscarriages, and multiple births). Individual data from Basel were
extracted from the birth records of the Canton of Basel City University
Maternity Hospital (kept at the State Archives Basel City, Sanität X29), where
births have been recorded in detail since 1896. The Basel archive series covers
about one-third of each calendar year (3–4 months). An individual birth record
extends over five pages and contains detailed information on the mother, the
birth, and the infant. Incomplete records are scarce [38].
Data from three years for Basel were combined to approximate the size of the
dataset from Lausanne: 1921 (covering August to December, n = 510), 1922
(January to March, n = 423), and 1923 (May to July, n = 474). In total, the
Basel dataset contained 1407 births.
The demographic data included the
mother’s date of birth, place of residence, occupation, marital status, age, height
(cm), general and skeletal condition (signs of rickets or not), waist
circumference just before delivery (cm), and age at menarche. Obstetric
measurements (all in cm) included the interspinous distance (the distance
between the two anterior superior iliac spines), the intercristal distance (the
widest distance between the two iliac cristae), and the conjugata externa (the distance
from the upper edge of the symphysis to the processus spinosus of the fifth
lumbar vertebra) (appendix figure S1). Solid evidence indicates that external
pelvic measurements correlate well with internal measurements [53, 54]. Parity and
date of last menstruation were
also recorded. Maternal mortality was recorded, as well as the number of
obstetric interventions performed (caesarean section, episiotomy, forceps
delivery, and extraction). Because forceps deliveries and caesarean sections were
relatively uncommon, these two interventions were classified together as the
next stage of intervention after episiotomy. During birth, the dilation,
expulsion, and postpartum phases were recorded for each birth. The two most
common vertex presentations that are generally associated with the least risk
were categorised as normal. These are the left occipito-anterior (LOA) and right
occipito-anterior (ROA) positions, which were recorded in Lausanne with the
French terms OIGA (Occipito-lliaque Gauche Antérieure) and OIDA
(Occipito-lliaque Droite Antérieure), respectively, and in Basel with the
German terms “erste vordere Hinterhauptslage” (HHL I) and “zweite vordere
Hinterhauptslage” (HHL II), respectively. All other head positions and foetal
presentations were classified as abnormal. For the infant, the vital status at
birth and in the first days after birth (early neonatal mortality), date of
birth, gestational age in
weeks, and sex were recorded. Anthropometric data included birthweight, head
circumference, length, placental weight and size, and postnatal weight after several
days during the hospital stay (infant weight loss).
Ethics statement
This study was approved by the
Cantonal Ethics Committee of the Canton of Zurich (BASEC number 2021-00628). Approval
meant that informed consent was not required, as the study was based on
historical data from the 1920s. Data collection was performed between
01.07.2021 and 31.07.2024. In the archives, the study team had access to non-anonymised
personal information in the historical medical records, but in agreement with
the ethics committee, the data were fully anonymised in the course of the study.
Statistical methods
Logistic regression models were used
to estimate the risk of episiotomy (yes or no) or caesarean section/forceps
delivery (yes or no) in the presence of several explanatory variables. For
episiotomy, the following explanatory variables were included: sex, parity,
head position, maternal height, birthweight, the ratio of the conjugata externa
to head circumference (3 groups: normal; large vs small [3rd tercile
conjugata externa vs 1st tercile head circumference], and small vs
large [1st tercile conjugata externa vs 3rd tercile head
circumference]), and the duration of the expulsion phase (3 groups: terciles). Because
of the low number of females who underwent caesarean section or forceps
delivery (Lausanne: n = 60, Basel: n = 35), the model only included sex,
parity, head position, head circumference (continuous in cm), and conjugata
externa (continuous in cm) as explanatory variables. To make the expulsion
phase comparable in both data sets, the duration of the phase was z-transformed
and modelled using a linear regression model, including sex, parity, head
position, maternal height, birth weight, and the ratio of the conjugata externa
to head circumference as explanatory variables. Because maternal height and
pelvic breadth measurements (crests) are strongly correlated, we only used
maternal height as an explanatory variable in the model for the episiotomy and
expulsion phases. However, a sensitivity analysis with crests is shown in the
supplementary material. In addition, a sensitivity analysis was performed for
these two models (the number of births for caesarean section/forceps was too
low), including only primiparous women. Because of the multicollinearity
between gestational age and head circumference, gestational age was only
controlled for in sensitivity analyses (a univariable analysis including
gestational age is shown in the supplementary material). For the Lausanne
dataset, additional information was available on the maternal body morphology
(normal, thin, or obese) and whether the mother had rickets; for Basel, additional
information included socioeconomic position (SEP) based on the partner’s
occupation. Univariable analyses were performed for these additional variables.
Model assumptions regarding multicollinearity, homoscedasticity, and
independence were fulfilled for all models. The assumption of normally
distributed residuals was not completely fulfilled for the dependent variable “expulsion
time”, but evidence shows that Gaussian models are robust even when this
assumption is violated [55]. The sample size is
relatively large; in addition, the predictors are relatively normally
distributed or only slightly skewed, so the results are assumed to be robust (appendix
figure S2).
All statistical analyses were
performed using R version 4.3.2.
Results
Data from 1407 births in Basel and 1145
births in Lausanne between 1921 and 1923 were included in the analysis. Episiotomy
was performed in 16.6% of births in Basel and 8.6% of births in Lausanne (8.0%
difference, 95% confidence interval (CI) 5.4 to 10.6, p <0.001) (table 1).
In Basel, however, forceps delivery was performed in 1.2% of the births,
compared with 4.7% in Lausanne (3.5% difference, 95% CI 2.1 to 4.9, p <0.001).
In Basel, 19 caesarean sections were performed, and in Lausanne, 6 were
performed (1.4% vs 0.5% of all births, difference not significant). The foetal
head position was normal in over 90% of births (the difference between Basel
and Lausanne was not significant). In Basel, the mothers were slightly older on
average than in Lausanne (28.7 years vs 28.0 years, p = 0.003). They were marginally
taller (158.0 cm vs 156.5 cm, p <0.001) and had a slightly larger conjugata
externa (19.9 cm vs 19.6 cm, p <0.001). Their infants were slightly heavier
(3282.0 g vs 3205.9 g, p <0.001) with a larger head circumference (34.7 cm vs
34.5 cm, p = 0.001). The mean expulsion phase was longer in Basel than in
Lausanne (52.2 min vs 33.1 min, p <0.001), and there were more first births
in Basel than in Lausanne (51.7% vs 36.9%, p <0.001). By contrast, no
significant difference was observed in the rate of premature births (<37
weeks), number of stillbirths, the proportion of female neonates, or the mean
intercristal distance. The distribution plots in figure S2 show that most
continuous body dimensions tended towards symmetry.
Table 1Summary
of the two samples from Lausanne and Basel for outcomes/interventions and all
co-factors, continuous variables (including individual body measurements and
ratios), and categorical variables. SD: Standard deviation;
CI: Confidence interval.
|
Basel |
Lausanne |
Difference (Basel vs
Lausanne) |
| n/value |
% |
n/value |
% |
Difference |
95% CI |
p |
| Year |
1921 |
510 |
|
|
|
|
|
|
| 1922 |
423 |
|
1145 |
|
|
|
|
| 1923 |
474 |
|
|
|
|
|
|
| Total |
1407 |
|
1145 |
|
|
|
|
| Episiotomy |
No |
1174 |
83.4 |
1047 |
91.4 |
|
|
|
| Yes |
233 |
16.6 |
98 |
8.6 |
8.0 |
5.4 to 10.6 |
p <0.001 |
| Missing |
0 |
0.0 |
0 |
0.0 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Forceps |
No |
1390 |
98.8 |
1091 |
95.3 |
|
|
|
| Yes |
17 |
1.2 |
54 |
4.7 |
−3.5 |
2.1 to 4.9 |
p <0.001 |
| Missing |
0 |
0.0 |
0 |
0.0 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Caesarean section |
No |
1388 |
98.6 |
1139 |
99.5 |
|
|
|
| Yes |
19 |
1.4 |
6 |
0.5 |
0.8 |
0.0 to 1.6 |
p = 0.056 |
| Missing |
0 |
0.0 |
0 |
0.0 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Foetal position |
Abnormal |
117 |
8.3 |
83 |
7.2 |
1.1 |
−1.1 to 3.2 |
p = 0.356 |
| Normal |
1290 |
91.7 |
1062 |
92.8 |
|
|
|
| Missing |
0 |
0.0 |
0 |
0.0 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Maternal height (cm) |
n |
949 |
|
1102 |
|
|
|
|
| Mean |
158.0 |
|
156.5 |
|
1.5 |
0.9 to 2.1 |
p <0.001 |
| SD |
6.3 |
|
6.5 |
|
|
|
|
| Missing |
458 |
32.6 |
43 |
3.8 |
|
|
|
| Sex of neonate |
Female |
690 |
49.0 |
580 |
50.7 |
−1.6 |
−5.6 to 2.3 |
p = 0.440 |
| Male |
712 |
50.6 |
555 |
48.5 |
|
|
|
| Missing |
5 |
0.4 |
10 |
0.9 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Stillbirth |
No |
1343 |
95.5 |
1107 |
96.7 |
|
|
|
| Yes |
61 |
4.3 |
35 |
3.1 |
1.3 |
−0.3 to 2.8 |
p = 0.113 |
| Missing |
3 |
0.2 |
3 |
0.3 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Birthweight (g) |
n |
1399 |
|
1139 |
|
|
|
|
| Mean |
3282.0 |
|
3205.9 |
|
76.2 |
33.2 to 119.0 |
p <0.001 |
| SD |
551.4 |
|
544.3 |
|
|
|
|
| Missing |
8 |
0.6 |
6 |
0.5 |
|
|
|
| Head circumference (cm) |
n |
1365 |
|
1114 |
|
|
|
|
| Mean |
34.7 |
|
34.5 |
|
0.2 |
0.1 to 0.3 |
p = 0.001 |
| SD |
1.6 |
|
1.5 |
|
|
|
|
| Missing |
42 |
3 |
31 |
2.7 |
|
|
|
| Maternal age (years) |
n |
1407 |
|
1133 |
|
|
|
|
| Mean |
28.7 |
|
28.0 |
|
0.7 |
0.2 to 1.6 |
p = 0.003 |
| SD |
5.8 |
|
5.9 |
|
|
|
|
| Missing |
0 |
0 |
12 |
1 |
|
|
|
| Intercristal distance (cm) |
n |
1237 |
|
1120 |
|
|
|
|
| Mean |
28.5 |
|
28.6 |
|
−0.1 |
−0.2 to 0.1 |
p = 0.118 |
| SD |
1.5 |
|
1.6 |
|
|
|
|
| Missing |
170 |
12.1 |
25 |
2.2 |
|
|
|
| Conjugata externa (cm) |
n |
1231 |
|
1056 |
|
|
|
|
| Mean |
19.9 |
|
19.6 |
|
0.3 |
0.2 to 0.4 |
p <0.001 |
| SD |
1.3 |
|
1.6 |
|
|
|
|
| Missing |
176 |
12.5 |
89 |
7.8 |
|
|
|
| Duration of expulsion phase
(min) |
n |
1348 |
|
1073 |
|
|
|
|
| Mean |
52.2 |
|
33.1 |
|
19.0 |
14.2 to 24.0 |
p <0.001 |
| SD |
71.8 |
|
44.1 |
|
|
|
|
| Missing |
59 |
4.2 |
72 |
6.3 |
|
|
|
| Gestational age (weeks) |
n |
1194 |
|
1141 |
|
|
|
|
| Mean |
39.8 |
|
40.1 |
|
−0.2 |
−0.5 to −0.1 |
p <0.001 |
| SD |
2.5 |
|
2.7 |
|
|
|
|
| Missing |
213 |
15.1 |
4 |
0.3 |
|
|
|
| Gestational age categories
(weeks) |
<37 |
83 |
5.9 |
74 |
6.5 |
−0.6 |
−2.5 to 1.4 |
p = 0.612 |
| 37 to 41 |
795 |
56.5 |
709 |
61.9 |
|
|
|
| ≥41 |
315 |
22.4 |
358 |
31.3 |
|
|
|
| Missing |
214 |
15.2 |
4 |
0.3 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Parity |
1 |
727 |
51.7 |
423 |
36.9 |
14.7 |
10.8 to 18.6 |
p <0.001 |
| 2 |
358 |
25.4 |
279 |
24.4 |
|
|
|
| ≥3 |
322 |
22.9 |
421 |
36.8 |
|
|
|
| Missing |
0 |
0.0 |
22 |
1.9 |
|
|
|
| Total |
1407 |
100.0 |
1145 |
100.0 |
|
|
|
| Maternal socioeconomic position background |
Low |
331 |
23.5 |
|
|
|
|
|
| Medium |
728 |
51.7 |
|
|
|
|
|
| High |
318 |
22.6 |
|
|
|
|
|
| Housewives |
21 |
1.5 |
|
|
|
|
|
| Missing |
9 |
0.6 |
|
|
|
|
|
| Total |
1407 |
100.0 |
|
|
|
|
|
| Maternal obesity |
Yes |
|
|
41 |
3.6 |
|
|
|
| No |
|
|
1081 |
94.4 |
|
|
|
| Missing |
|
|
23 |
2.0 |
|
|
|
| Total |
|
|
1145 |
100.0 |
|
|
|
| Maternal undernutrition |
Yes |
|
|
23 |
2.0 |
|
|
|
| No |
|
|
1099 |
96.0 |
|
|
|
| Missing |
|
|
23 |
2.0 |
|
|
|
| Total |
|
|
1145 |
100.0 |
|
|
|
| Maternal goitre |
Yes |
|
|
47 |
4.1 |
|
|
|
| No |
|
|
1075 |
93.9 |
|
|
|
| Missing |
|
|
23 |
2.0 |
|
|
|
| Total |
|
|
1145 |
100.0 |
|
|
|
| Maternal rickets |
Yes |
|
|
23 |
2.0 |
|
|
|
| No |
|
|
1122 |
98.0 |
|
|
|
| Missing |
|
|
23 |
2.0 |
|
|
|
| Total |
|
|
1145 |
100.0 |
|
|
|
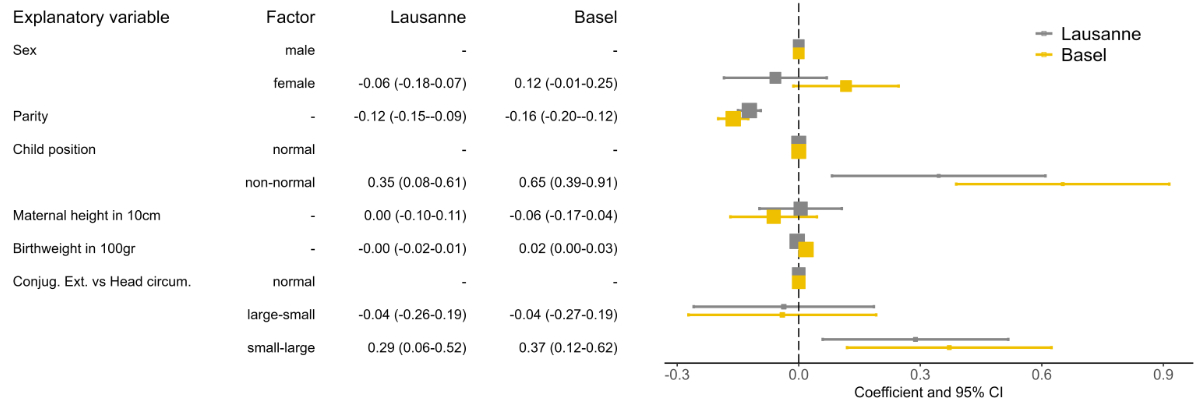
Regarding the duration of the
expulsion phase (figure 1), a very large infant head circumference in
combination with a small maternal conjugata externa led to a significantly
prolonged expulsion phase (z = 0.37 [95% CI 0.12–0.62] for Basel and z = 0.29
[95% CI 0.06–0.52] for Lausanne, expressed in z-values). Of the other
co-factors, a higher parity led to a significantly shorter expulsion phase, and
an abnormal foetal position led to a considerably longer expulsion phase in
Basel and Lausanne. These factors were significant in both the univariable and
multivariable models. The significant association between the ratio of the
conjugata externa to head circumference remained when the model was reduced to
first births, when the maternal intercristal distance was included in the model
instead of maternal height, and when the model was additionally adjusted for
SEP in Basel and for the health or rickets status of the mother in Lausanne (appendix
figures S3A, S4A, S5A, S6A, and S7A).
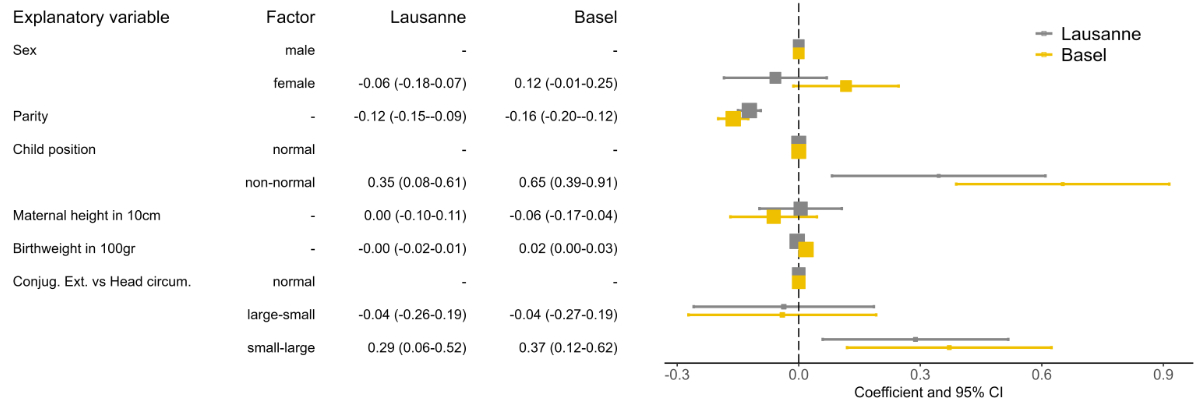
Figure 1Expulsion
time coefficients and 95% confidence intervals (CIs) from the linear regression
model. All explanatory variables were mutually adjusted. The models were
performed separately for Lausanne and Basel. To make the expulsion phase
comparable between Basel and Lausanne, the expulsion time was z-transformed.
“Conjug. Ext vs Head circum” shows the ratio of the conjugata externa to head
circumference (3 groups: normal; large vs small [3rd tercile
conjugata externa vs 1st tercile head circumference]; and small vs
large [1st tercile conjugata externa vs 3rd tercile head
circumference]).
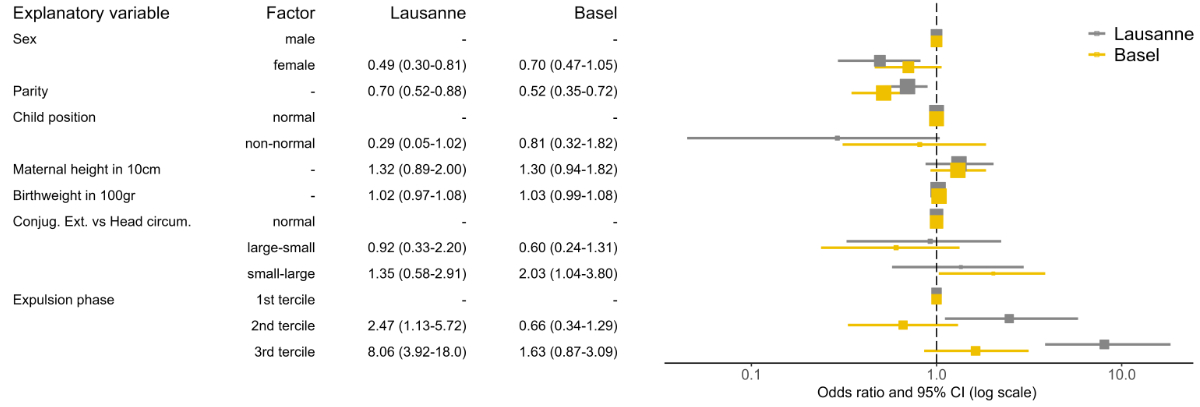
The risk of performing an episiotomy
was lower for female infants (significant in Lausanne) and with increased parity
(figure 2). A large head circumference combined with a small conjugata externa
significantly increased the risk of episiotomy in Basel (odds ratio (OR) 2.03,
95% CI 1.04–3.80), and the trend was the same but not significant in Lausanne
(OR 1.35, 95% CI 0.58–2.91). When the expulsion phase was particularly long (3rd
tercile), the risk of an episiotomy was also higher. The effect of the
pelvis-to-head circumference ratio became somewhat less pronounced when the
model was reduced to first births, when the intercristal distance was used in
the model instead of maternal height, and when the model was additionally
adjusted for SEP in Basel and for the health status of the mother in Lausanne
in the sensitivity analyses (appendix figures S3B, S4B, S5B, S6B, and S7B).
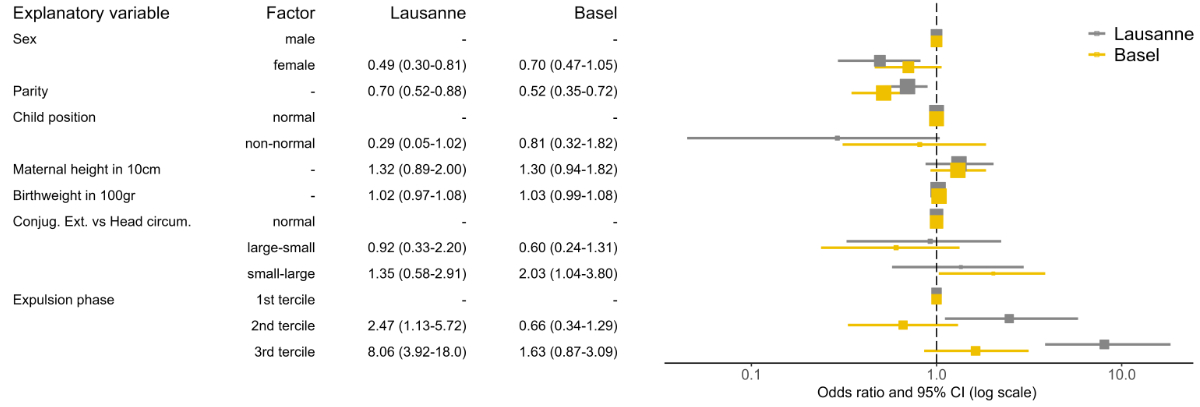
Figure 2Episiotomy
odds ratios (ORs) and 95% confidence intervals (CIs) from the logistic
regression model. All explanatory variables were mutually adjusted. The models
were performed separately for Lausanne and Basel. “Conjug. Ext vs Head circum”
shows the ratio of the conjugata externa to head circumference (3 groups:
normal; large vs small [3rd tercile conjugata externa vs 1st
tercile head circumference]; and small vs large [1st tercile conjugata
externa vs 3rd tercile head circumference]).
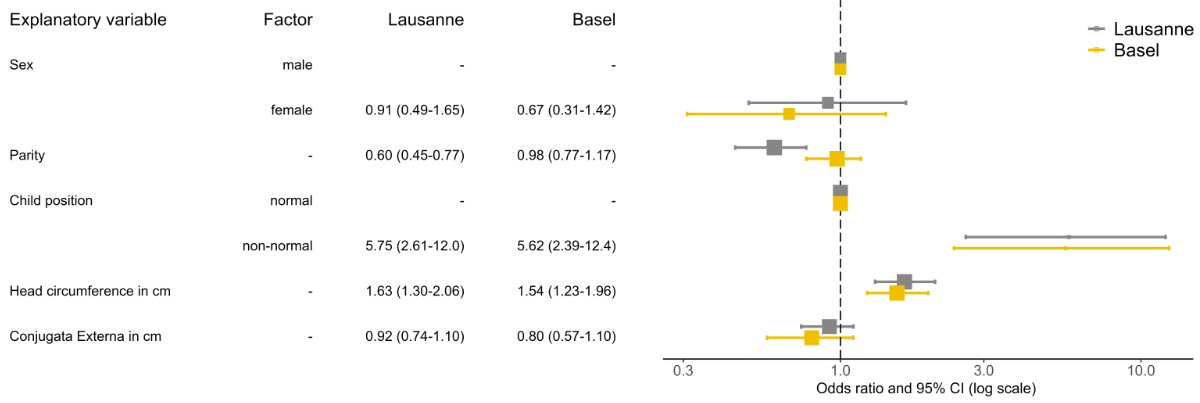
An abnormal foetal position and a
higher head circumference were associated with forceps use or caesarean section
in the simplified models (not fully adjusted for all cofactors) (figure 3). By contrast,
the risk was lower with a longer conjugata externa and a higher parity. In
general, physician-recorded maternal rickets was not associated with the
duration of the expulsion phase or with episiotomy, but it was associated with
a higher risk of forceps use or caesarean section (OR 6.98, 95% CI 2.44–17.5).
However, overall maternal health status and maternal body shape (thin or
obese), as assessed by a physician, did not have a significant effect in any
model in Lausanne (appendix figures S5C, S6C, and S7C).
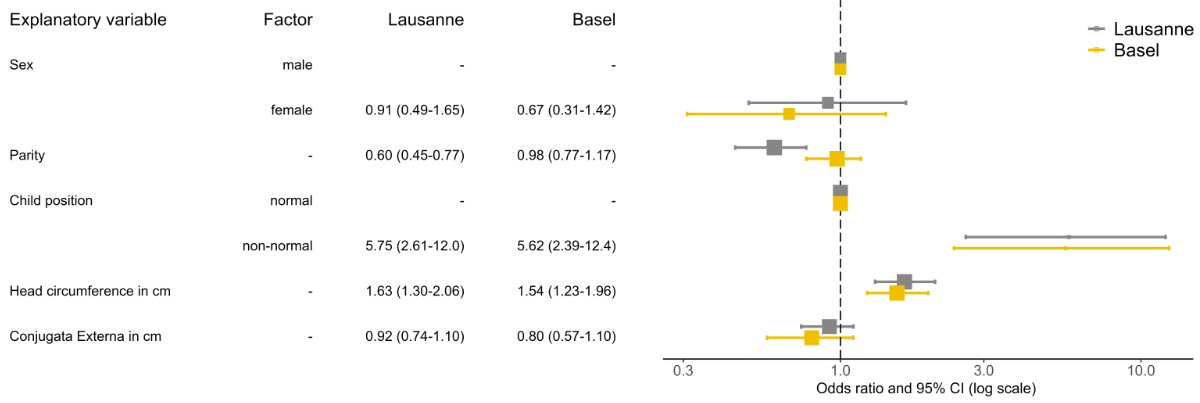
Figure 3Forceps
and caesarean section odds ratios (OR) and 95% confidence intervals (CIs) from
the logistic regression model. All explanatory variables were mutually
adjusted. The models were performed separately for Lausanne and Basel.
Discussion
Using
historical data sets from the 1920s from Basel and Lausanne, which each had
only one maternity hospital, we showed that in over 90% of births, the position
of the foetal head was either right occiput anterior or left occiput anterior
(i.e., considered normal); episiotomy was performed in 8–17% of births and forceps
delivery was performed in 1–5%, while caesarean sections were rarely performed
(<1% of all births). Regarding the primary exposure variable, a large foetal
head diameter and a short conjugata externa (as an indicator of an
anteroposteriorly narrow pelvis), either alone or in combination with each
other, tended to prolong the expulsion phase and increase the risk of
intervention. Abnormal head position and first births were also associated with
prolonged expulsion phase and increased intervention risk. Rickets (noted by physicians
in 2% of Lausanne mothers) increased the risk of forceps delivery or caesarean
section.
We
are unaware of similar modern studies that have analysed comparable historical
datasets from maternity hospitals, so we cannot compare our results with other
studies of historical data. While traditional external pelvic
measurements such as interspinous, intercristal, and conjugata externa provide
valuable insights into pelvic dimensions, their routine use has declined with
the advent of advanced imaging technologies. These modern methods, particularly
MRI pelvimetry, offer more accurate and detailed assessments, improving the
prediction of labour outcomes and management of childbirth. However, despite
their superior precision, advanced imaging techniques are mainly reserved for
specific circumstances due to their availability and cost, such as in cases of
breech or twin pregnancies. Moreover, most pelvimetric studies have concluded
that the sensitivity of such simple linear dimensions to predict the risk of dystocia
in births with cephalic presentations was too low to be clinically relevant [56, 57].
However, traditional clinical
pelvimetry remains vital in settings where advanced imaging is inaccessible [54].
At the population level, studies have suggested that clinical pelvimetry can
offer valuable predictive information, especially when combined with other
maternal and foetal factors. Moreover, the transition from clinical to
imaging-based pelvimetry reflects broader trends in obstetric practice, where
technological advancements continually reshape clinical decision-making. These
developments underscore the importance of integrating both traditional and
modern approaches to optimise maternal and foetal outcomes [53].
Our
study has several limitations. First, sample selection bias may have affected the
two datasets. Although around two-thirds of all births in the two cities
occurred at these hospitals at the beginning of the 1920s, it is unclear
whether our results are generalisable to the remaining home births. Interventions
and abnormal births may have been more common among hospital births than among all
births. Second, medical interventions during labour are often stepwise when
complications arise. Although the birth registers analysed may allow a precise
reconstruction of all birth sequences and the reasons behind interventions,
this detailed analysis was not possible for our dataset of around 2500 births due
to time and effort constraints. More in-depth medical-historical analyses
should be conducted. Third, the elasticity of the soft tissue plays a major
role in the processes under consideration, in addition to the bony shape of the
maternal pelvis. Unfortunately, we were unable to include these soft tissue
factors in our analysis. In addition, maternal body mass index and weight gain
during pregnancy, which might affect the weight of the infant, as well as any
pathological process, were not available. Fourth, it is immediately apparent
from examining the birth registers that both hospitals worked according to
precise internal and obstetric guidelines. Unfortunately, despite intensive
archive research, these guidelines could not be reconstructed. The two
hospitals may have measured and documented the variables of interest
differently, which could explain specific differences observed in our data. Obstetric
textbooks and literature from this period should be consulted in a more
in-depth medical-historical analysis to gain a better understanding of the use
of these interventions. Finally, the observed differences may also reflect
differences in patient populations between French-speaking southern Switzerland
and German-speaking northern Switzerland, with potentially varying socioeconomic
and cultural differences.
Conclusion
Our
study provides insights into the health situation and obstetric practice over
100 years ago, when obstetric processes were precisely documented in the
maternity hospitals. At that time, maternal body shape and health differed
considerably due to living conditions, and modern obstetric methods were not
yet widely used. Under these conditions, the mismatch between maternal body
shape and the foetus was an important factor in complicated births.
Data sharing statement
The data are available in a public, open-access
repository at https://doi.org/10.5281/zenodo.15576871, and
the statistical codes can be found at https://github.com/KaMatthes/Obstetrical_interventions_1922.
Acknowledgments
The authors would like to thank Lukas Helm, Joël
Floris, Kaspar Pohl, Laura Grogg, Nikola Koepke, and Ulrich Woitek for their
help in collecting and preparing the data and for previous collaborations. They
also express gratitude to the staff of the Basel-Stadt and Vaud State Archives
for their help and support.
Prof. Dr phil. Kaspar Staub
Institute of Evolutionary Medicine (IEM)
University of Zurich
Winterthurerstrasse 190
CH-8057 Zurich
kaspar.staub[at]iem.uzh.ch
References
1. Ward JL, Azzopardi PS, Francis KL, Santelli JS, Skirbekk V, Sawyer SM, et al.; GBD
2019 Adolescent Mortality Collaborators. Global, regional, and national mortality
among young people aged 10-24 years, 1950-2019: a systematic analysis for the Global
Burden of Disease Study 2019. Lancet. 2021 Oct;398(10311):1593–618. 10.1016/S0140-6736(21)01546-4
2. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World
Bank Group and UNDESA/Population Division. Available from: https://www.who.int/publications/i/item/9789240068759 (accessed 15 July 2025)
3. THE 17 GOALS | Sustainable Development. Available from: https://sdgs.un.org/goals (accessed 15 July 2025)
4. Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal
death: a systematic review. Lancet. 2006 Apr;367(9516):1066–74. 10.1016/S0140-6736(06)68397-9
5. Lawn JE, Cousens S, Zupan J; Lancet Neonatal Survival Steering Team. 4 million neonatal
deaths: when? Where? Why? Lancet. 2005 Mar;365(9462):891–900. 10.1016/S0140-6736(05)71048-5
6. Washburn SL. Tools and human evolution. Sci Am. 1960 Sep;203(3):63–75. doi: https://doi.org/10.1038/scientificamerican0960-62
7. Dunsworth HM, Warrener AG, Deacon T, Ellison PT, Pontzer H. Metabolic hypothesis for
human altriciality. Proc Natl Acad Sci USA. 2012 Sep;109(38):15212–6. 10.1073/pnas.1205282109
8. Grunstra ND, Betti L, Fischer B, Haeusler M, Pavlicev M, Stansfield E, et al. There
is an obstetrical dilemma: misconceptions about the evolution of human childbirth
and pelvic form. Am J Biol Anthropol. 2023 Aug;181(4):535–44. doi: https://doi.org/10.1002/ajpa.24802
9. Haeusler M, Grunstra ND, Martin RD, Krenn VA, Fornai C, Webb NM. The obstetrical dilemma
hypothesis: there’s life in the old dog yet. Biol Rev Camb Philos Soc. 2021 Oct;96(5):2031–57.
doi: https://doi.org/10.1111/brv.12744
10. Frémondière P, Thollon L, Marchal F, Fornai C, Webb NM, Haeusler M. Dynamic finite-element
simulations reveal early origin of complex human birth pattern. Commun Biol. 2022 Apr;5(1):377.
doi: https://doi.org/10.1038/s42003-022-03321-z
11. Cordey C, Webb NM, Haeusler M. Take it to the limit: the limitations of energetic
explanations for birth timing in humans. Evol Med Public Health. 2023 Oct;11(1):415–28.
doi: https://doi.org/10.1093/emph/eoad035
12. Wells JC, DeSilva JM, Stock JT. The obstetric dilemma: an ancient game of Russian
roulette, or a variable dilemma sensitive to ecology? Am J Phys Anthropol. 2012;149(S55 Suppl
55):40–71. doi: https://doi.org/10.1002/ajpa.22160
13. Addo OY, Stein AD, Fall CH, Gigante DP, Guntupalli AM, Horta BL, et al.; Consortium
on Health Orientated Research in Transitional Societies (COHORTS) Group. Maternal
height and child growth patterns. J Pediatr. 2013 Aug;163(2):549–54. 10.1016/j.jpeds.2013.02.002
14. Floris J, Staub K, Woitek U. The Benefits of Intervention: Birth Weights in Basle
1912-1920. SSRN Electronic Journal. Published Online First: 24 October 2016. doi:
10.2139/SSRN.2858945
15. Franz M, Kainer F, Husslein P. Physiologie des mütterlichen Organismus und Erkrankungen
in der Schwangerschaft. Die Geburtshilfe; 2016. pp. 395–448. 10.1007/978-3-662-45064-2_21
16. Günther V, Alkatout I, Vollmer C, Maass N, Strauss A, Voigt M. Impact of nicotine
and maternal BMI on fetal birth weight. BMC Pregnancy Childbirth. 2021 Feb;21(1):127.
doi: https://doi.org/10.1186/s12884-021-03593-z
17. Warrington NM, Beaumont RN, Horikoshi M, Day FR, Helgeland Ø, Laurin C, et al.; EGG
Consortium. Maternal and fetal genetic effects on birth weight and their relevance
to cardio-metabolic risk factors. Nat Genet. 2019 May;51(5):804–14. doi: https://doi.org/10.1038/s41588-019-0403-1
18. Wanner CL. Was hat die Körpergrösse der Frau für eine Auswirkung auf die Beckengrösse
und damit auf Geburtsproblematiken? Vorgelegt von Caroline Laura Wanner. Zürich: Deutsche
Nationalbibliothek; 2023.
19. Kurki HK. Protection of obstetric dimensions in a small-bodied human sample. Am J
Phys Anthropol. 2007 Aug;133(4):1152–65. doi: https://doi.org/10.1002/ajpa.20636
20. Pavličev M, Romero R, Mitteroecker P. Evolution of the human pelvis and obstructed
labor: new explanations of an old obstetrical dilemma. Am J Obstet Gynecol. 2020 Jan;222(1):3–16.
doi: https://doi.org/10.1016/j.ajog.2019.06.043
21. Elvander C, Högberg U, Ekéus C. The influence of fetal head circumference on labor
outcome: a population-based register study. Acta Obstet Gynecol Scand. 2012 Apr;91(4):470–5.
doi: https://doi.org/10.1111/j.1600-0412.2012.01358.x
22. Lipschuetz M, Cohen SM, Ein-Mor E, Sapir H, Hochner-Celnikier D, Porat S, et al. A
large head circumference is more strongly associated with unplanned cesarean or instrumental
delivery and neonatal complications than high birthweight. Am J Obstet Gynecol. 2015 Dec;213(6):833.e1–12.
doi: https://doi.org/10.1016/j.ajog.2015.07.045
23. Sexual and reproductive health and rights. Available from: https://www.who.int/health-topics/sexual-and-reproductive-health-and-rights#tab=tab_1 (accessed 15 July 2025)
24. Entbindungen und Gesundheit der Mütter im Jahr 2017 - | Publikation. Available from:
https://www.bfs.admin.ch/asset/de/8369420 (accessed 15 July 2025)
25. 08.3935 | Zunahme von Kaiserschnittgeburten | Geschäft | Das Schweizer Parlament.
Available from: https://www.parlament.ch/de/ratsbetrieb/suche-curia-vista/geschaeft?AffairId=20083935 (accessed 15 July 2025)
26. Drife J. The start of life: a history of obstetrics. Postgrad Med J. 2002 May;78(919):311–5.
doi: https://doi.org/10.1136/pmj.78.919.311
27. Loudon I. General practitioners and obstetrics: a brief history. J R Soc Med. 2008 Nov;101(11):531–5.
doi: https://doi.org/10.1258/jrsm.2008.080264
28. Liebermann E. Die Geburt bei engem Becken. 1908.
29. Hess H. Die Bedeutung der äusseren Beckenmasse für die Diagnose des engen Beckens. 1932.
30. Westermann H. Die Bedeutung der äusseren Beckenmasse für die Diagnose des engen Beckens. 1937.
31. Lang E. Die Bedeutung der äusseren Beckenmasse, insbesondere der Dist. crist. il.
für die Erkenntniss der Becken-form. 1922.
32. Staub K, Bender N, Floris J, Pfister C, Rühli FJ. From Undernutrition to Overnutrition:
The Evolution of Overweight and Obesity among Young Men in Switzerland since the 19th
Century. Obes Facts. 2016;9(4):259–72. 10.1159/000446966
33. Koepke N, Floris J, Pfister C, Rühli FJ, Staub K. Ladies first: female and male adult
height in Switzerland, 1770-1930. Econ Hum Biol. 2018 May;29:76–87. 10.1016/j.ehb.2018.02.002
34. Vinci L, Floris J, Koepke N, Matthes KL, Bochud M, Bender N, et al. Have Swiss adult
males and females stopped growing taller? Evidence from the population-based nutrition
survey menuCH, 2014/2015. Econ Hum Biol. 2019 May;33:201–10. doi: https://doi.org/10.1016/j.ehb.2019.03.009
35. Staub K, Rühli FJ. “From growth in height to growth in breadth”: the changing body
shape of Swiss conscripts since the late 19th century and possible endocrine explanations.
Gen Comp Endocrinol. 2013 Jul;188:9–15. doi: https://doi.org/10.1016/j.ygcen.2013.03.028
36. Cole TJ. Secular trends in growth. Proc Nutr Soc. 2000;59:317–24. doi: S0029665100000355
doi: https://doi.org/10.1017/S0029665100000355
37. Solth K, Abt K. [Changes in neonatal weight during the past five years; a comparison
of statistics of German clinics and the Basel Gynecologic and Obstetric Hospital].
Schweiz Med Wochenschr. 1951 Jan;81(3):58–61.
38. Butie C, Matthes KL, Hösli I, Floris J, Staub K. Impact of World War 1 on placenta
weight, birth weight and other anthropometric parameters of neonatal health. Placenta.
2020 Oct;100:150–8. doi: https://doi.org/10.1016/j.placenta.2020.07.003
39. Schneider EB. Fetal health stagnation: have health conditions in utero improved in
the United States and Western and Northern Europe over the past 150 years? Soc Sci
Med. 2017 Apr;179:18–26. 10.1016/j.socscimed.2017.02.018
40. Oecd. How Was Life? Global Well-being Since 1820.
41. Floris J, Kaiser L, Mayr H, Staub K, Woitek U. Investigating survivorship bias: the
case of the 1918 flu pandemic. Appl Econ Lett. 2022;29(21):2047–52. 10.1080/13504851.2021.1971614
42. Floris J, Höpflinger F, Stohr C, Studer R, Staub K. Wealthier – older – taller: measuring
the standard of living in Switzerland since the 19th century. Schweiz Z Gesch. 2019;69(2):207–32.
doi: https://doi.org/10.24894/2296-6013.00037
43. Floris J, Staub K. Water, sanitation and mortality in Swiss towns in the context of
urban renewal in the late nineteenth century. Hist Fam. 2019;24(2):249–76. 10.1080/1081602X.2019.1598460
44. The World Economy | OECD. Available from: https://www.oecd.org/en/publications/the-world-economy_9789264189980-en.html (accessed 15 July 2025)
45. Statistik | Kanton Basel-Stadt. Available from: https://statistik.bs.ch/unterthema/einwohner (accessed 15 July 2025)
46. La Maternité de Lausanne. Un patrimoine pour la vie - Institut des humanités en médecine
- CHUV. Available from: https://www.chuv.ch/fr/ihm/ihm-home/editions-bhms/catalogue/catalogue/la-maternite-de-lausanne-un-patrimoine-pour-la-vie (accessed 16 July 2025)
47. Schaub C. La Maternité et la Clinique infantile - Lausanne : l’Hôpital Neslé - Lausanne :
étude historique et morpho-logique des fenêtres. 2016.
48. Rossier G. Clinique obstétricale (Maternité de Lausanne) : Communication avec présentations
faite à la Séance cli-nique du 5 mars 1908 de la Société vaudoise de médecine. 1908.
49. Gerber S. Inversion Utérine. Rev Med Suisse Romande. 1996 Apr;116(4):277–83.
50. La Maternité de Lausanne. Vues historiques | BHMS Editions | Boutique Médicale Suisse.
Available from: https://boutique.revmed.ch/la-maternite-de-lausanne-vues-historiques (accessed 16 July 2025)
51. Hôpital cantonal Lausanne. Règlement pour les admissions à l’Hôpital cantonal et à
la Maternité, pour les consultations et la délivrance gratuite de médicaments. 1882.
52. Browse - Historische Statistik der Schweiz. Available from: https://hsso.ch/ (accessed 16 July 2025)
53. Frémondière P, Servat E. Interval Versus External Pelvimetry: A Validation Study With
Clinical Implications. Int J Childbirth. Published Online First; 2023. 10.1891/IJC2023-0023
54. Hynčík L, Jansová M, Němec M, et al. Correlation between internal and external bony
pelvis dimensions in nulliparous women. Published Online First: 12 April 2023. doi: https://doi.org/10.21203/rs.3.rs-2723568/v1
55. Knief U, Forstmeier W. Violating the normality assumption may be the lesser of two
evils. Behav Res Methods. 2021 Dec;53(6):2576–90. doi: https://doi.org/10.3758/s13428-021-01587-5
56. Korhonen U, Taipale P, Heinonen S. Fetal pelvic index to predict cephalopelvic disproportion
- a retrospective clinical cohort study. Acta Obstet Gynecol Scand. 2015 Jun;94(6):615–21.
doi: https://doi.org/10.1111/aogs.12608
57. Pattinson RC, Cuthbert A, Vannevel V. Pelvimetry for fetal cephalic presentations
at or near term for deciding on mode of delivery. Cochrane Database Syst Rev. 2017 Mar;3(3):CD000161.
10.1002/14651858.CD000161.pub2
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4546.