Characteristics of severely injured trauma patients transported by helicopter emergency
medical services in Switzerland: a retrospective cohort study
DOI: https://doi.org/https://doi.org/10.57187/s.4502
Martin Müllera*,
Patrick
Micallefbc*,
Sebastian
Judd,
Aristomenis
Exadaktylosa,
Dominik A. Jakobae**,
Urs Pietschacf**, and the
Swiss Trauma Registryg
a Department of Emergency Medicine, Inselspital
Bern, University Hospital Bern, Bern, Switzerland
b Department of Anesthaesiology, Emergency and
Pain Medicine, Cantonal Hospital St. Gallen, St. Gallen, Switzerland
c Rega (Rettungsflugwacht/Guarde Aérienne), Swiss
Air-Ambulance, Zurich, Switzerland
d Department of General Internal Medicine,
Cantonal Hospital St. Gallen, St. Gallen, Switzerland
e Department of Visceral Surgery, Lindenhofspital,
Private Hospital Bern, Bern, Switzerland
f Department of Perioperative and Intensive Care
Medicine, Cantonal Hospital St. Gallen, St. Gallen, Switzerland
g Swiss Trauma Board
* Contributed equally to first authorship
** Contributed
equally to senior authorship
Summary
BACKGROUND: Information on
severely injured patients transported by helicopter emergency medical services
(HEMS) in Switzerland is scarce. This study, with a special focus on sex differences,
aimed to gain insights into the demographics, injury characteristics and
outcomes of these patients and to provide data that could help improve
prehospital trauma care.
METHODS: This is a retrospective multicentre cohort study analysing
data collected by the Swiss Trauma Registry. Patients aged 16 or older, who
were admitted by helicopter emergency medical services to a level 1 trauma centre
in Switzerland between 2018 and 2022, with an Injury Severity Score (ISS) of ≥16,
were included.
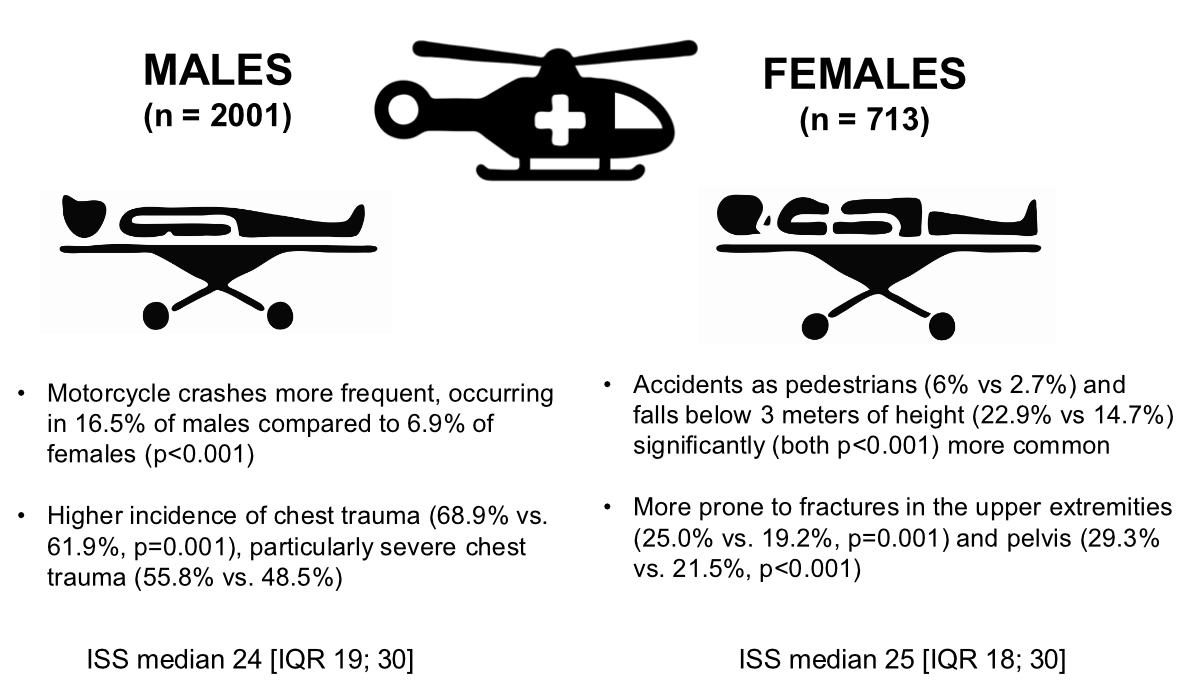
RESULTS: Overall, 2714 trauma patients were analysed
in the present study. The majority of these patients were male (73.7%). Blunt
trauma was the main cause of injury (93.6%), with
traffic accidents (43.5%) and falls (43.3%) being the most common accident
mechanisms. A greater percentage
of male patients than female patients were involved in motorcycle crashes
(16.5% vs 6.9%, p <0.001). Female patients were more frequently involved in
accidents as pedestrians (6% vs 2.7%, p <0.001) and experienced more falls below
3 metres of height (22.9% vs 14.7%, p <0.001). The median ISS of our cohort was 24
(interquartile range
[IQR]: 19–30). The most common injuries were thoracic trauma (67%), head
trauma (66.7%) and spine trauma (50.3%). Men suffered more thoracic injuries
(68.9% vs 61.9%, p = 0.001) and their median Abbreviated Injury Score (AIS) Thorax
was significantly higher (3.0 [IQR: 0–3] vs 2.0 [IQR: 0–3], p <0.001). Women
had a higher prevalence of pelvic fractures (29.3% vs 21.5%, p <0.001) and suffered
more fractures of long bones in their upper extremities (22.2% vs 15.7%, p <0.001).
There was no significant difference in in-hospital mortality between women and
men (15.7% vs 14.6%, p = 0.493), nor in other outcome parameters.
CONCLUSION: To our knowledge, this is the first analysis of data on severely
injured trauma patients transported by helicopter emergency medical services in
Switzerland. While there were notable differences between women and men in
terms of accident mechanisms and injury characteristics, no significant
differences in outcome parameters were observed.
Introduction
Background
Helicopter emergency medical services
(HEMS) are a cornerstone of trauma care in most Western countries and have been
shown to reduce mortality after trauma and shorten rescue time, particularly in
rural or geographically challenging areas like the alpine regions of
Switzerland, which cover over 50 percent of the country [1–8]. Due to these challenging
geographical conditions, fast and
efficient rescue is often only possible by helicopter. As a result, helicopter
emergency medical services are more established in Switzerland than in many
other European countries and respond to around 6% to 10% of all emergency calls
[9, 10]. This is also reflected in the
finding that a smaller proportion of patients were transported by helicopter
emergency medical services in Europe. In Switzerland, around 35% of seriously
injured people are transported to a hospital by helicopter [11]. Differences in trauma
outcomes according
to sex have already been identified, with most studies showing that women
appear to be relatively advantaged compared to men when looking at overall
mortality [12]. Researchers are
increasingly exploring new sex-specific perspectives in acute care medicine,
particularly in the fields of trauma and resuscitation. However, systematic
reviews and meta-analyses of sex-based disparities in trauma sample only a
small proportion of the published literature, which biases conclusions. Few
studies on trauma outcomes present data by sex, and the bias against publishing
negative studies persists. It is therefore important to address sex-specific
issues in trauma and resuscitation.
Recent papers from the Netherlands and
Denmark have reported data on patients transported by helicopter emergency
medical services, looking into the characteristics of trauma- and non-trauma
patients, and comparing the characteristics of trauma patients by mode of
transportation (helicopter emergency medical services vs ambulance) [13, 14]. To our
knowledge, there exists no
similar information on trauma patients transported by helicopter emergency
medical services in Switzerland.
Objective
The aim of this study was to provide an
overview of severely injured trauma patients transported by helicopter
emergency medical services in Switzerland, with a particular focus on
differences between men and women. This information can help to better
understand trauma patients transported by helicopter emergency medical services
and to further improve prehospital trauma care.
Methods
Study design and setting
In Switzerland, deployment of helicopter
emergency medical services is organised either by regional medical emergency
call centres or directly by the national operation centre of the Rega (Rettungsflugwacht/Guarde
Aérienne). The entire Swiss helicopter emergency medical
services operation area is accessible within 15 minutes of flying time day and
night by a helicopter at one of the four main Swiss helicopter emergency
medical services providers: Rega, Air-Glaciers, Air Zermatt and Alpine Air
Ambulance. A helicopter emergency medical services team comprises at least a
pilot, a paramedic and an emergency physician, usually an anaesthetist or
intensive care doctor with a specialisation in prehospital emergency medicine.
All helicopter emergency medical services providers conduct primary missions to
aid patients in need of emergency medical treatment, search and rescue missions
and in addition offer rapid transfer of critically ill patients between
hospitals.
In this retrospective multicentre cohort
study, we analysed data from the Swiss Trauma Registry (STR) on severely
injured trauma patients transported by helicopter emergency medical services.
The Swiss Trauma Registry plays a crucial role in the advancement of trauma
care by collecting, providing and reviewing data on critically injured trauma
patients. All twelve level 1 trauma centres in Switzerland are obliged to
document trauma patients aged ≥16 years with an Injury Severity Score (ISS) ≥16
and/or Abbreviated Injury Score (AIS) Head ≥3 in the Swiss Trauma Registry [15, 16].
The Swiss Trauma Registry excludes
patients with isolated burns or in whom the burn is the clear primary injury,
as well as patients who have experienced suffocation, hanging or drowning
without any accompanying injuries. Patients who reached the emergency
department without signs of life are also excluded if either no or only very
limited diagnostic or treatment measures have been performed. Patients who meet
the criteria mentioned above are then registered by the trauma centres in the Swiss
Trauma Registry, which forms the basis for coordinated clinical care and
research in Switzerland by, in return, providing participating clinics with data
on severely injured trauma patients for further research [17].
The Swiss Trauma Registry has been
systematically collecting a wide range of trauma data in a pseudoanonymous
manner since 2015 [15]. The registry
includes detailed demographics, injury characteristics, prehospital and
admission parameters, medical interventions and various outcome measures. Data
entry follows standardised protocols, ensuring consistency across all
participating level 1 trauma centres in Switzerland. Clinicians and trained
registry personnel collect patient data from health records, prehospital
emergency reports and hospital documentation. To ensure data integrity and
accuracy, the Swiss Trauma Registry performs regular internal validation checks
[15].
The present review is published in
accordance with Swiss Trauma Registry publication guidelines under STR-ID 19
and uses STROBE reporting guidelines [18, 19].
Eligibility criteria
For our study, we identified all patients
in the Swiss Trauma Registry admitted by helicopter emergency medical services
between January 2018 and December 2022. This starting point was selected
because we believe that from this time onward, data quality in the Swiss Trauma
Registry is sufficiently high to ensure reliable analysis. The endpoint was
determined by the latest fully available year of data at the time of study
initiation.
We excluded all open cases, all non-primary
admissions, all cases with an unknown accident date or where the accident date
was more than one day prior to admission, and all cases without a documented
ISS. We also excluded all patients with an ISS <16 to ensure that only
severely injured patients were analysed.
Statistical methods
All statistical analyses were conducted
using STATA 18.1 (StataCorp, College Station, TX, USA). Descriptive statistics
for categorical variables are presented as frequencies and corresponding
percentages. For continuous variables, either medians with interquartile ranges
(IQR) or means with standard deviations (SD) are reported, depending on the
results of normality testing (Shapiro-Wilk test). P-values were calculated
using the Wilcoxon rank-sum test for non-normally distributed data and the
unpaired t-test for normally distributed data. For categorical variables,
p-values were obtained using the chi-squared test. A p-value of <0.05 was
considered statistically significant.
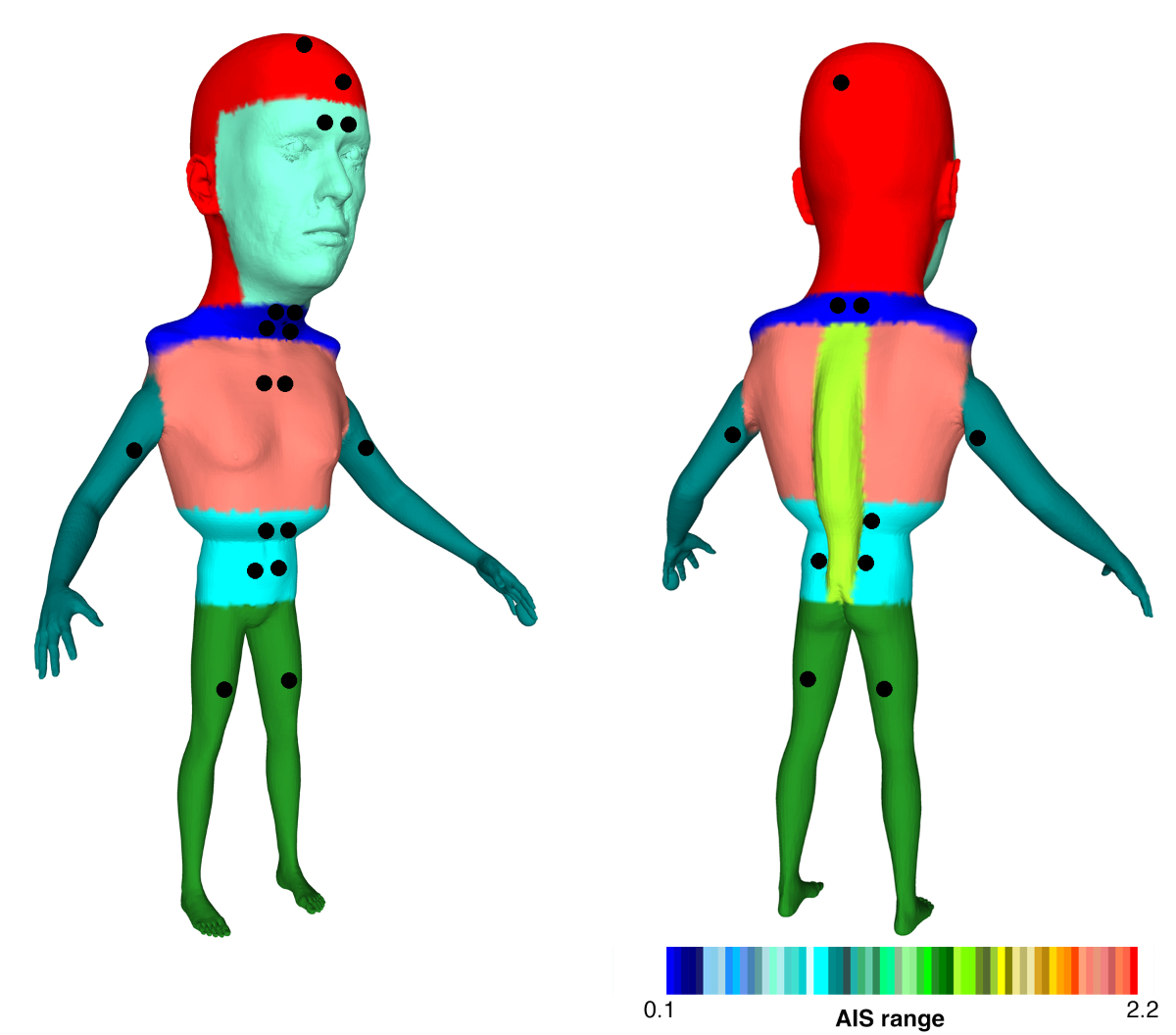
Creation of graphical cohort description
To visually represent the Swiss helicopter
emergency medical services severe trauma cohort, a 3D deformed human figure –
referred to as the Swiss helicopter emergency medical services severe trauma “traumunculus”
(a portmanteau word formed from trauma and homunculus) – was constructed,
inspired by the well-known 3D sensory/motor male and female homunculus [20, 21]. The
traumunculus integrates various
cohort trauma characteristics, including the proportion of males, mean age,
trauma severity, relative frequency of injuries to each body region and trauma
type (e.g. penetrating trauma). Its construction is detailed in the appendix.
Ethics approval and consent to participate
The cantonal ethics committee of St. Gallen
(EKOS) reviewed the study design, classified it as a quality evaluation analysis and
granted
permission for using patient data without individual consent (BASEC Nr. Req-2022-01540
EKOS 22/198).
Results
Study population
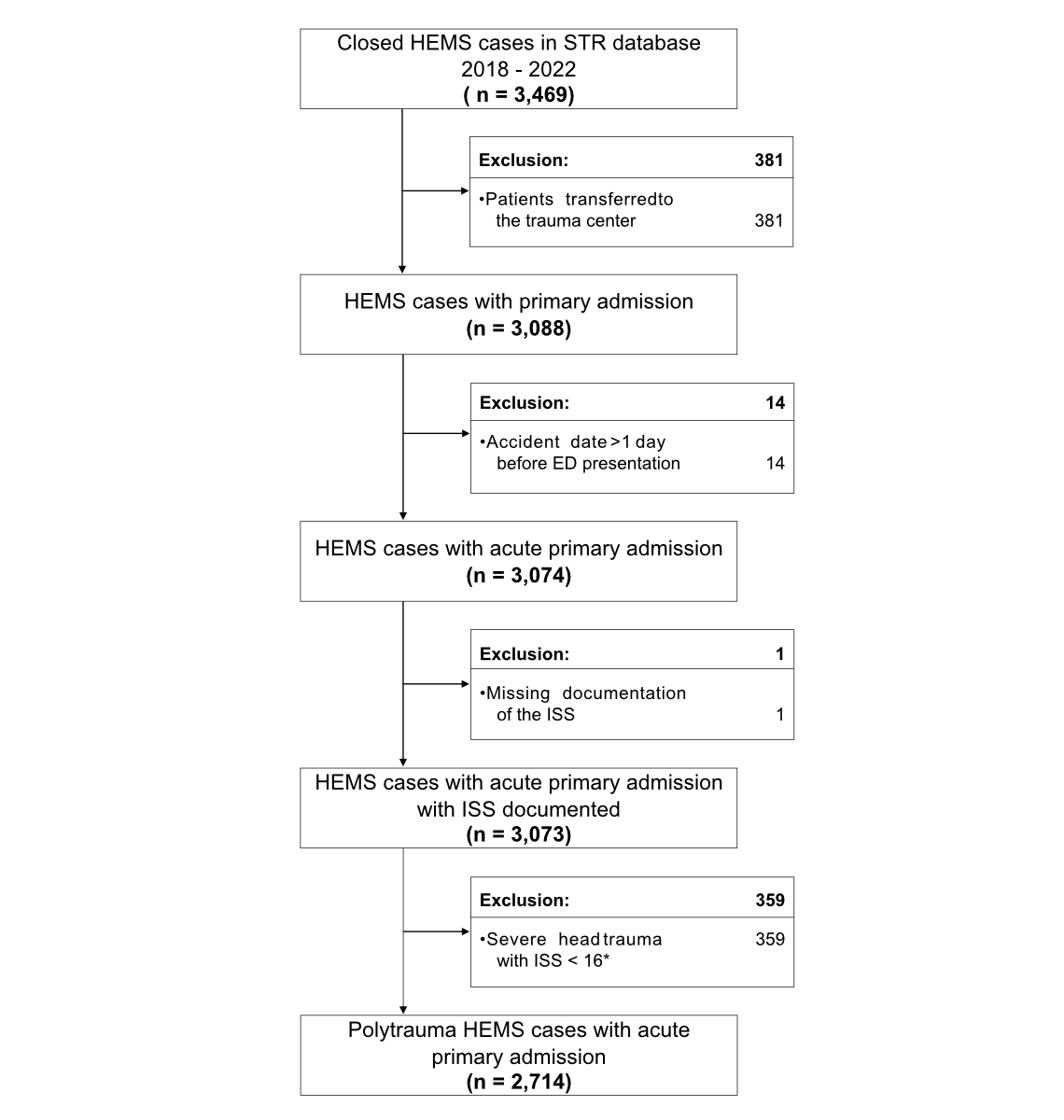
In total, 3652 primary helicopter emergency
medical services cases were identified in Swiss Trauma Registry database
between January 2018 and December 2022, of which 3469 were closed cases. After applying
the previously stated exclusion criteria, 2714 cases were analysed in the
present study (figure 1).
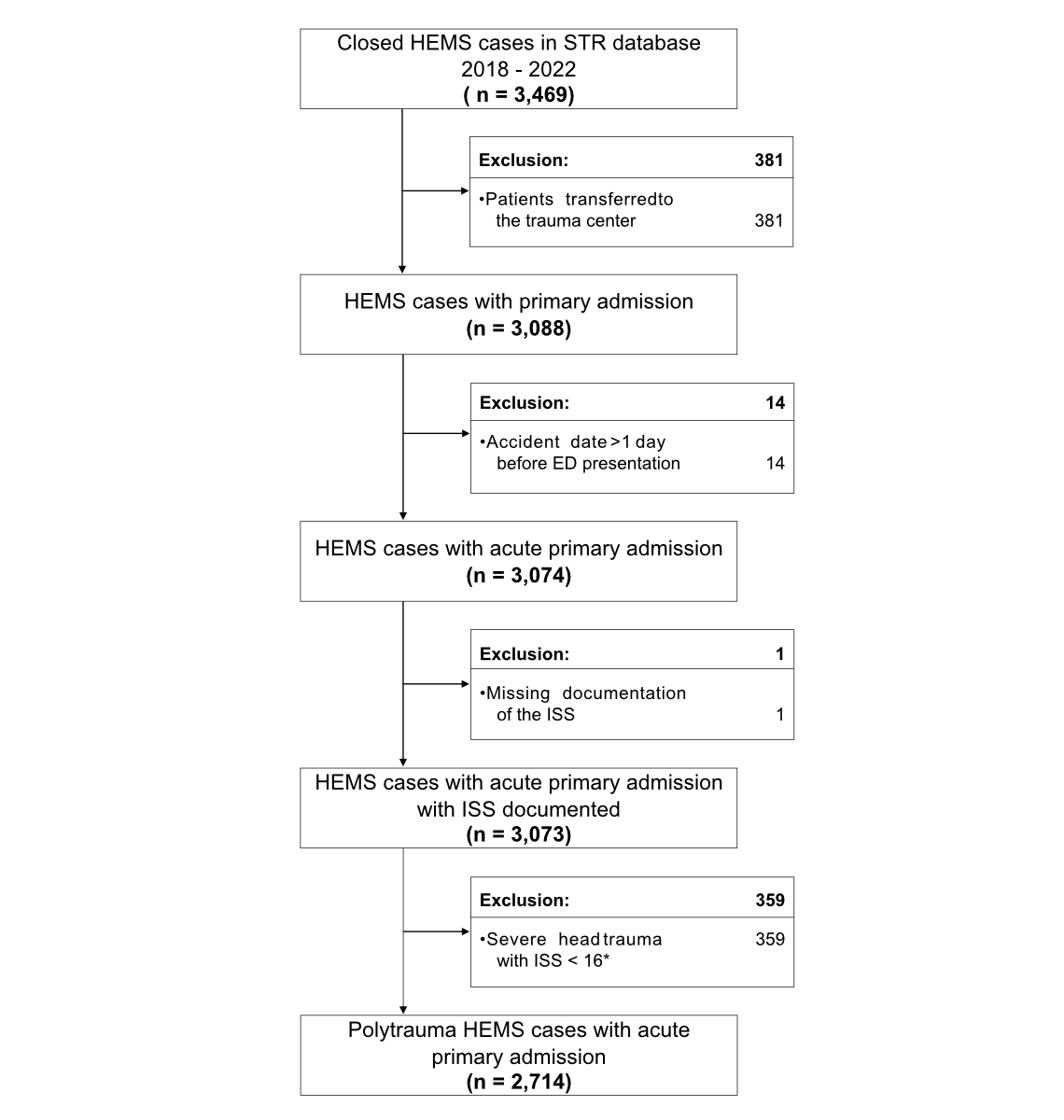
Figure 1Study flowchart. * Excluding
patients with an Injury Severity Score (ISS) of less than 16 results in the omission
of individuals with severe head trauma (Abbreviated
Injury Score [AIS] Head ≥3) who have an overall ISS below 16. ED: Emergency Department;
HEMS:
Helicopter Emergency Medical Service; STR: Swiss Trauma Registry.
Baseline characteristics and admission data
Table 1 shows patient demographics, trauma
characteristics and vital signs at hospital admission for men, women and the entire
cohort. The median age of all patients was 54 years (IQR: 35–67). Patient
numbers declined with increasing age, from 1022 in the youngest age group to
363 aged 75 years or over. Women accounted for approximately one-quarter of
patients across all age groups except those aged >75 years, where the
percentage of female patients rose to 36.6%. Overall, male patients were slightly
younger than female patients (median age 53 years [IQR: 35–66] vs median age 55
years [IQR: 36–70], p = 0.007).
Table 1Demographics, accident
characteristics and vital signs at hospital admission according to sex. The
p-values are across all age categories and accident characteristics. Vitals
were obtained at hospital admission.
|
Total (n = 2714) |
Female (n = 713) |
Male (n = 2001) |
p-value |
| Demographics |
|
[%] |
|
[%] |
|
[%] |
|
| Age
groups |
16–45
years, n (%) |
1022 |
[37.7%] |
259 |
[36.3%] |
763 |
[38.1%] |
|
| >45–65
years, n (%) |
950 |
[35.0%] |
227 |
[31.8%] |
723 |
[36.1%] |
|
| >65–75
years, n (%) |
379 |
[14.0%] |
94 |
[13.2%] |
285 |
[14.2%] |
|
| >75
years, n (%) |
363 |
[13.4%] |
133 |
[18.7%] |
230 |
[11.5%] |
<0.001 |
| Age in years |
54.0 |
[35.0–67.0] |
55.0 |
[36.0–70.0] |
53.0 |
[35.0–66.0] |
0.007 |
| Accident characteristics |
|
|
|
|
|
|
|
| Type of
injury* |
Blunt
trauma |
2540 |
[93.6%] |
672 |
[94.2%] |
1868 |
[93.4%] |
|
| Penetrating
injury |
95 |
[3.5%] |
22 |
[3.1%] |
73 |
[3.6%] |
|
| Blunt
& penetrating injury |
77 |
[2.8%] |
18 |
[2.5%] |
59 |
[2.9%] |
|
| Type of
injury, detail |
Traffic –
car, truck |
319 |
[11.8%] |
94 |
[13.2%] |
225 |
[11.2%] |
|
| Traffic –
motorcycle crash |
379 |
[14.0%] |
49 |
[6.9%] |
330 |
[16.5%] |
|
| E-bike/E-scooter |
34 |
[1.3%] |
10 |
[1.4%] |
24 |
[1.2%] |
|
| Bicycle |
281 |
[10.4%] |
64 |
[9.0%] |
217 |
[10.8%] |
|
| Pedestrian |
98 |
[3.6%] |
43 |
[6.0%] |
55 |
[2.7%] |
|
| Traffic,
other |
66 |
[2.4%] |
21 |
[2.9%] |
45 |
[2.2%] |
|
| Fall over
3 metres |
596 |
[22.0%] |
145 |
[20.3%] |
451 |
[22.5%] |
|
| Fall
below 3 metres |
457 |
[16.8%] |
163 |
[22.9%] |
294 |
[14.7%] |
|
| Fall at
ground level |
54 |
[2.0%] |
18 |
[2.5%] |
36 |
[1.8%] |
|
| Fall of
unknown height |
68 |
[2.5%] |
22 |
[3.1%] |
46 |
[2.3%] |
|
| Other – blow |
111 |
[4.1%] |
29 |
[4.1%] |
82 |
[4.1%] |
|
| Gunshot
wound |
27 |
[1.0%] |
4 |
[0.6%] |
23 |
[1.1%] |
|
| Stab
wound |
13 |
[0.5%] |
3 |
[0.4%] |
10 |
[0.5%] |
|
| Explosion |
2 |
[0.1%] |
0 |
[0.0%] |
2 |
[0.1%] |
|
| Avalanche,
landslide, spillage |
25 |
[0.9%] |
5 |
[0.7%] |
20 |
[1.0%] |
|
| Other |
175 |
[6.4%] |
42 |
[5.9%] |
133 |
[6.6%] |
|
| Unknown |
9 |
[0.3%] |
1 |
[0.1%] |
8 |
[0.4%] |
<0.001 |
| Vitals |
|
[IQR or
%] |
|
[IQR or
%] |
|
[IQR or
%] |
|
| Systolic
blood pressure [mm Hg] |
130 |
[110–147] |
123 |
[106–140] |
130 |
[111–149] |
<0.001 |
| Systolic
blood pressure <90 mm Hg |
267 |
[9.8%] |
72 |
[10.1%] |
195 |
[9.7%] |
0.786 |
| Pulse
clinical [/min] |
86 |
[72–101] |
85 |
[71–100] |
87 |
[72–102] |
0.057 |
| Pulse
<60/min |
193 |
[7.1%] |
50 |
[7.0%] |
143 |
[7.1%] |
0.905 |
| Pulse
>100/min |
701 |
[25.8%] |
165 |
[23.1%] |
536 |
[26.8%] |
0.056 |
| Glasgow
Coma Scale (GCS)** |
14.0 |
[3–15] |
14.0 |
[3–15] |
14.0 |
[3–15] |
0.833 |
| Glasgow
Coma Scale (GCS) <9** |
876 |
[33.3%] |
229 |
[33.3%] |
647 |
[33.3%] |
0.993 |
| Respiratory
rate [/min]*** |
16.0 |
[14–20] |
16.0 |
[14–20] |
16.0 |
[14–21] |
0.010 |
| Bradypnoea
<10/min*** |
54 |
[3.2%] |
15 |
[3.6%] |
39 |
[3.0%] |
0.557 |
| Tachypnoea
>30/min*** |
60 |
[3.5%] |
10 |
[2.4%] |
50 |
[3.9%] |
0.156 |
| Temperature
[° C]# |
36.3 |
[35.6–36.8] |
36.2 |
[35.5–36.7] |
36.3 |
[35.7–36.9] |
0.001 |
| Oxygen
saturation [%]## |
98.0 |
[95–100] |
99.0 |
[96–100] |
98.0 |
[95–100] |
0.001 |
Most injuries originated from blunt trauma
(93.6%) with traffic accidents (43.5%) or falls of any height (43.3%) being the
predominant causes of injury. Further analysis of traffic accidents revealed
that 14% of all patients had been involved in a motorcycle crash, 11.8% in a
car or truck accident, 10.4% in a bicycle accident, 3.6% had been a pedestrian
at the time of the accident and 1.3% were involved in an e-bike or e-scooter
accident. Falls were further divided into three groups according to height: 22%
of all patients fell from a height greater than 3 metres, 16.8% from a height less
than 3 metres and 2% fell at ground level. In 68 patients, a fall was reported
but no specific height documented.
Men were more frequently involved in
motorcycle accidents (16.5% vs 6.9%, p <0.001), whereas women were
relatively more often involved in accidents as pedestrians (6% vs 2.7%, p <0.001)
and were more likely to experience a fall from a height below 3 metres (22.9% vs
14.7%, p <0.001).
When comparing vital signs at hospital
admission between the two sex groups, statistically significant differences in
systolic blood pressure, respiratory rate, temperature and oxygen saturation
were noted.
Injury characteristics
The most common and severe injury among all
patients was trauma to the thorax (67%, median AIS: 3.0 [IQR: 0–3]), followed closely
by head trauma (66.7%, median AIS: 2.0 [IQR: 0–4]) and spine trauma (50.3%,
median AIS: 1.0 [IQR: 0–2]). The median ISS in our cohort was 24.0 (IQR: 19–30).
Men suffered relatively more thoracic
injuries than women (68.9% vs 61.9%, p = 0.001) and the median AIS Thorax for
male patients was significantly higher than for female patients (3.0 [IQR: 0–3]
vs 2.0 [IQR: 0–3], p <0.001). A considerably higher proportion of men than
women had concomitant lung injuries (30.1% vs 23.6%, p = 0.001), haemo- or
pneumothorax (38.8% vs 34.5%, p = 0.041) and rib fractures (55.5% vs 51.2%, p =
0.046).
Women suffered more pelvic fractures than
male patients (29.3% vs 21.5%, p <0.001), as well as more fractures of long
bones of the upper extremities (22.2% vs 15.7%, p <0.001), with more
fractures of the humerus (9% vs 5.3%, p <0.001) and fractures of forearm
bones (16% vs 11.9%, p = 0.005). There was no significant difference in the
median ISS between men and women (24.0 [IQR: 19–30] vs 25.0 [IQR: 18–30], p = 0.780)
(table 2).
Table 2Injury characteristics according
to sex.
|
Total (n = 2714) |
Female (n = 713) |
Male (n = 2001) |
p-value |
| Injury characteristics |
|
[%] |
|
[%] |
|
[%] |
|
| …Any head trauma |
1810 |
[66.7%] |
479 |
[67.2%] |
1331 |
[66.5%] |
0.747 |
| …Any face trauma |
940 |
[34.6%] |
233 |
[32.7%] |
707 |
[35.3%] |
0.201 |
| …Any neck trauma |
134 |
[4.9%] |
38 |
[5.3%] |
96 |
[4.8%] |
0.573 |
| …Any thorax trauma |
1819 |
[67.0%] |
441 |
[61.9%] |
1378 |
[68.9%] |
0.001 |
| …Any abdomen trauma |
733 |
[27.0%] |
199 |
[27.9%] |
534 |
[26.7%] |
0.527 |
| …Any spine trauma |
1365 |
[50.3%] |
359 |
[50.4%] |
1006 |
[50.3%] |
0.972 |
| …Any upper extremity trauma |
1262 |
[46.5%] |
330 |
[46.3%] |
932 |
[46.6%] |
0.893 |
| …Any lower extremity (incl. pelvis) trauma |
1228 |
[45.2%] |
340 |
[47.7%] |
888 |
[44.4%] |
0.128 |
| …Any external trauma |
112 |
[4.1%] |
24 |
[3.4%] |
88 |
[4.4%] |
0.234 |
| Abbreviated Injury Scale (AIS) |
|
|
|
|
|
|
|
| …AIS Head |
2.0 |
[0.0–4.0] |
3.0 |
[0.0–4.0] |
2.0 |
[0.0–4.0] |
0.192 |
| …AIS Face |
0.0 |
[0.0–1.0] |
0.0 |
[0.0–1.0] |
0.0 |
[0.0–1.0] |
0.182 |
| …AIS Neck |
0.0 |
[0.0–0.0] |
0.0 |
[0.0–0.0] |
0.0 |
[0.0–0.0] |
0.568 |
| …AIS Thorax |
3.0 |
[0.0–3.0] |
2.0 |
[0.0–3.0] |
3.0 |
[0.0–3.0] |
<0.001 |
| …AIS Abdomen |
0.0 |
[0.0–1.0] |
0.0 |
[0.0–2.0] |
0.0 |
[0.0–1.0] |
0.472 |
| …AIS Spine |
1.0 |
[0.0–2.0] |
1.0 |
[0.0–2.0] |
2.0 |
[0.0–2.0] |
0.700 |
| …AIS Upper Extremity |
0.0 |
[0.0–2.0] |
0.0 |
[0.0–2.0] |
0.0 |
[0.0–2.0] |
0.708 |
| …AIS Lower Extremity (incl. pelvis) |
0.0 |
[0.0–3.0] |
0.0 |
[0.0–3.0] |
0.0 |
[0.0–3.0] |
0.036 |
| …AIS External |
0.0 |
[0.0–0.0] |
0.0 |
[0.0–0.0] |
0.0 |
[0.0–0.0] |
0.234 |
| Severe body region trauma* |
|
|
|
|
|
|
|
| …Head |
1325 |
[48.8%] |
358 |
[50.2%] |
967 |
[48.3%] |
0.387 |
| …Face |
139 |
[5.1%] |
31 |
[4.3%] |
108 |
[5.4%] |
0.275 |
| …Neck |
63 |
[2.3%] |
19 |
[2.7%] |
44 |
[2.2%] |
0.478 |
| …Thorax |
1463 |
[53.9%] |
346 |
[48.5%] |
1117 |
[55.8%] |
0.001 |
| …Abdomen |
420 |
[15.5%] |
121 |
[17.0%] |
299 |
[14.9%] |
0.199 |
| …Spine |
531 |
[19.6%] |
134 |
[18.8%] |
397 |
[19.8%] |
0.545 |
| …Upper extremity |
62 |
[2.3%] |
21 |
[2.9%] |
41 |
[2.0%] |
0.169 |
| …Lower extremity |
750 |
[27.6%] |
212 |
[29.7%] |
538 |
[26.9%] |
0.144 |
| …External |
3 |
[0.1%] |
1 |
[0.1%] |
2 |
[0.1%] |
0.781 |
| Injury severity |
|
[IQR] |
|
[IQR] |
|
[IQR] |
|
| …Injury Severity Score (ISS) |
24.0 |
[19.0–30.0] |
25.0 |
[18.0–30.0] |
24.0 |
[19.0–30.0] |
0.780 |
Traumunculus
Figure 2 visualises the Swiss helicopter
emergency medical services severe trauma traumunculus as described in the “Methods”
section based on a 52-year-old (mean of cohort) with a 72% male appearance (proportion
of males) base mesh. The size of its body parts reflects the prevalence
of injury, the colour reflecting mean AIS and black holes denoting penetrating
injury per body
region (one percent per hole).
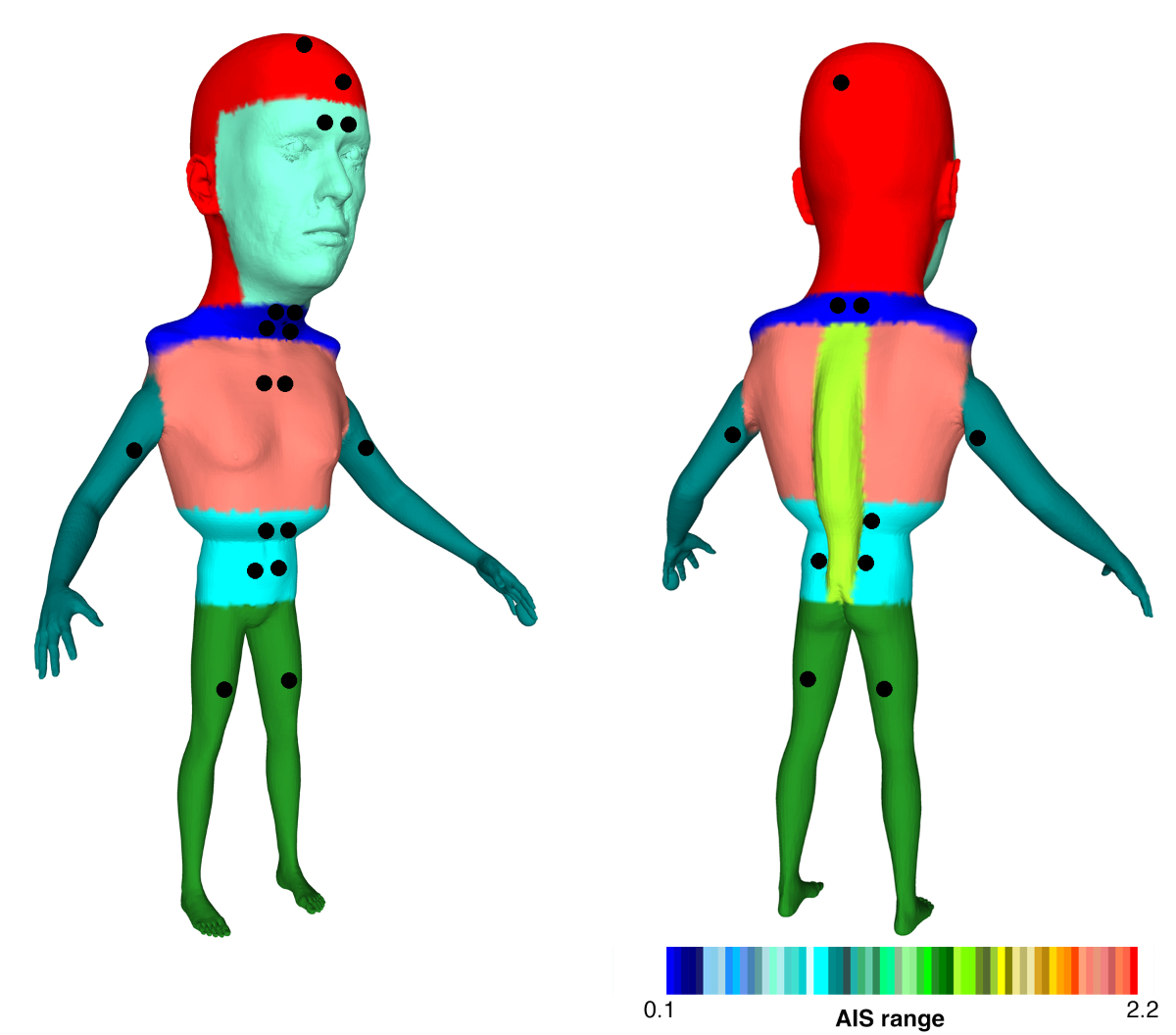
Figure 2Swiss
helicopter emergency medical services (HEMS) severe trauma traumunculus.
Outcome
Overall, 405 of 2714 patients (14.9%) died
during their hospital stay, and 14 patients died after discharge but within 28
days after trauma. The lowest mortality rate was observed in the population
aged 16–45 years (8.7%). The rate of mortality increased with age, reaching 38%
in the group of individuals aged over 75 years (appendix table S1).
There was no statistically significant
difference between male and female patients in hospitalisation length, intensive
care unit (ICU) stay, duration of mechanical ventilation, 28-day mortality or
in-hospital mortality (table 3, appendix table S2).
Table 3Outcome according to sex.
|
Total (n = 2714) |
Female (n = 713) |
Male (n = 2001) |
p-value |
| Outcome |
|
[IQR or %] |
|
[IQR or %] |
|
[IQR or %] |
|
| Length
of hospital stay [days] |
11.0 |
[6–18] |
11 |
[6–17] |
11 |
[6–18] |
0.295 |
| Length
of ICU stay [hours] |
48 |
[19–149] |
46 |
[20–133] |
48.0 |
[19–155] |
0.435 |
| Mechanical
ventilation* |
1176 |
[47.0%] |
300 |
[46.0%] |
876 |
[47.4%] |
0.541 |
| Duration
of mechanical ventilation [hours]** |
8 |
[0.0–69] |
6 |
[0.0–53] |
9.0 |
[0–72] |
0.155 |
| 28-day
mortality (from accident)*** |
419 |
[18.0%] |
115 |
[18.8%] |
304 |
[17.7%] |
0.545 |
| In-hospital
mortality |
405 |
[14.9%] |
112 |
[15.7%] |
293 |
[14.6%] |
0.493 |
Discussion
To our knowledge, this is the first analysis
of severely injured trauma patients transported by helicopter emergency medical
services in Switzerland. In our cohort, these patients are predominantly male,
and although some trauma mechanisms and injury characteristics vary between
male and female patients, outcome parameters are similar between the two groups.
Sex distribution of accidents
We can only hypothesise why men make up
almost three quarters of the patients in this cohort. Past and ongoing research
assumes that men tend to engage in riskier activities and behaviours than women,
especially in younger years [22]. This has
led to the term “young male syndrome”, although it has been questioned by more
recent studies [23, 24]. They also suffer
more injuries with potentially grave consequences during work in hazardous jobs
such as construction work or when handling heavy machinery [25]. According to one
paper, men’s higher
prevalence of risk-taking behaviour results in an overall non-fatal injury
incidence of 10.1/100 for men in the United States, compared with 8.5/100 for
women. Age-adjusted mortality rate from trauma was three times higher for men
than for women [26]. According to a
publication in 2024 by the Momentum Institute, relying on data from the
Austrian national statistical system, male drivers caused two-thirds of all
traffic accidents in 2023, of which almost a quarter occurred under the
influence of alcohol or drugs, compared with 9% of accidents with female
drivers [27]. We agree that riskier
behaviour and greater activity in potentially hazardous jobs, along with other
factors, may contribute to higher numbers of male patients in our study. We
found that men were more involved in motorcycle crashes, which could underline more
involvement in hazardous activities. The Swiss Council for Accident Prevention
(Beratungsstelle für Unfallverhütung [BFU]) highlighted in its 2021–2025 action
programme that motorcycles are particularly popular among young men and that,
despite accounting for only 2% of all vehicles on the road, motorcyclists (both
male and female) represent 30% of all severely injured road users – a figure
that closely aligns with our own findings. The BFU also addresses the role of
peer pressure among young men as a contributing factor to risk-taking behaviour.
With numerous action plans and programmes, the BFU aims to prevent
non-work-related severe injuries in Switzerland and to mitigate the impact of
this major public health concern. Non-work-related accidents account for
approximately one million incidents annually, leading to 36,000 severely
injured patients, 2400 fatalities and 12 billion Swiss Francs in material
damage [28].
Our study’s results further emphasise the
need for targeted prevention campaigns to reduce the burden of severe injuries,
particularly among young men. Potential preventive strategies might include (a)
traffic safety campaigns, (b) mandatory advanced rider training, (c)
peer-driven interventions, (d) further enforcement of traffic laws, (e)
infrastructure improvements (road safety modifications) and (f) early public
health education starting as early as primary school.
Injury characteristics
Regarding the consequences of trauma, men
seemed to experience thoracic trauma more frequently and with a significantly
higher Abbreviated Injury Score (AIS) Thorax, including greater incidence of lung
injuries, rib fractures and haemo- or pneumothoraxes. Severe thoracic injuries can
originate from high-energy trauma, possibly reflecting men’s higher prevalence
in motorcycle accidents. Women in our cohort suffered pelvic and upper extremity
fractures, including humerus and forearm fractures, more frequently. While
pelvic fractures are also associated with high-energy trauma, another factor
increasing the fracture rate in women may be underlying osteoporosis, which is most
prevalent in older female patients [29, 30].
After the age of 50, women are five times more likely to develop osteoporosis
than the general population. This, coupled with the effects of ageing, frailty
and more frequent falls, can significantly increase the likelihood of hip
fractures in women over 70 years of age. The incidence of forearm fractures
also rises, but not as sharply [31, 32].
Sex-based differences in quality of care
Published data suggests that the quality of
prehospital care varies between men and women due to sex-related factors. A
2012 retrospective cohort analysis of severely injured patients in Canada
looked at sex-based differences in direct transport by emergency medical
services to trauma centres, as well as secondary transfer from non-trauma centres
to trauma centres. The study revealed that female patients were less likely to
be directly admitted or transferred to a trauma centre than male patients [33]. A
2016 retrospective observational study
from Stockholm underlines these results. The study showed that severely injured
female trauma patients were given less priority in prehospital care and more
often did not receive direct transport to a trauma centre compared to their
male counterparts [34]. In accordance
with our study, they also reported that women suffered more injuries from falls
than men and that mortality between the male and female groups did not differ
significantly.
A possible explanation for this sex gap in
triage and admission might be that elderly female patients more frequently
suffer from “less spectacular” mechanisms of trauma, such as falls, and despite
being severely injured, may be more likely undertriaged due to the apparent “low-energy”
mechanism of trauma. Men, who more often suffer serious injuries from eye-catching
high-energy trauma mechanisms such as motorcycle crashes might be more likely
to be directly transported to a trauma centre because of the obvious accident
mechanism. However, it is important to point out that diagnosis in the
prehospital setting, particularly during helicopter emergency medical services
missions, can be very challenging. Evidence without regard to sex groups shows
that even trained professionals can miss severe chest and pelvic injuries in
these situations [35, 36].
There is conflicting data on patient
outcomes when focusing on sex in emergency medicine. The evidence so far does
not indicate a difference in mortality when male and female trauma patients are
compared [34, 37–39]. On the other hand,
research has shown that sex can influence medical treatment and outcome in
various conditions such as myocardial infarction, stroke care and triage to the
ICU [40–50]. A recent nationwide registry
study from Switzerland with 41,733 cardiac arrest patients, 34.9% of whom were
women, concluded that female patients were less frequently admitted to an ICU
after cardiac arrest. In addition, fewer advanced treatment measures were taken,
and their risk of ICU mortality was higher compared to their male counterparts,
especially after out-of-hospital cardiac arrest [50].
In our study, there were no significant
differences between the two sex groups in terms of outcome parameters;
mortality was similar between men and women, as was their duration of hospital stay
and other outcome data. Nevertheless, more and more data with a special focus
on sex differences is emerging and future research will play an important role
in unearthing or denying inequality in medical care between male and female trauma
patients. It is important for helicopter emergency medical services crew members
to acknowledge this potential sex bias and to keep it in mind on missions, ensuring
that all patients receive equal high-quality care regardless of their sex.
Limitations
Our cohort does not represent all patients
admitted to Swiss level 1 trauma centres with comparable injury severity as helicopter
emergency medical services tend to operate in more remote regions than ground
emergency medical services (GEMS). In Switzerland, ground emergency medical
services provide emergency medical aid in more densely populated areas. Here helicopter
emergency medical services are mostly dispatched for additional support of ground
emergency medical services, for example if a physician is needed on-site, to
provide rapid transport to a medical centre further away or if no ground
emergency medical service is available. Further research comparing Swiss trauma
patients transported by helicopter emergency medical services and ground
emergency medical services, such as that published by Blok et al. with data
from a Danish helicopter emergency medical services provider, would be needed
to gain insight into potential differences [31].
Furthermore, this study only analysed
severely injured trauma patients, excluding those with a lower Injury Severity Score
(ISS), which limits its significance for all trauma patients. We also excluded
patients who were transferred to a trauma centre after primary admission to a
non-trauma centre, thus not enabling us to provide data on the correct triage
of male and female trauma patients by the crews on the scene as has been
described in other studies and mentioned in our discussion. Another limitation
of this study is of course its retrospective design and analysis of data. Due
to the summarised nature of the dataset, we were not able to compare the
baseline characteristics of the two sexes with their injuries, mechanisms of
accidents and outcomes, preventing us from drawing conclusions about relationships between these variables
such as injuries or injury mechanisms suffered predominantly in certain age
groups of the two sexes.
Conclusion
The data provided by the Swiss Trauma
Registry enabled us to present an overview of the patients encountered by
medical professionals on their helicopter emergency medical services missions
in Switzerland. Although differences between women and men were observed in
terms of trauma mechanisms and injuries, no significant differences in outcome
parameters were noted.
An
illustrative and short summary of the results can be found in figure 3.
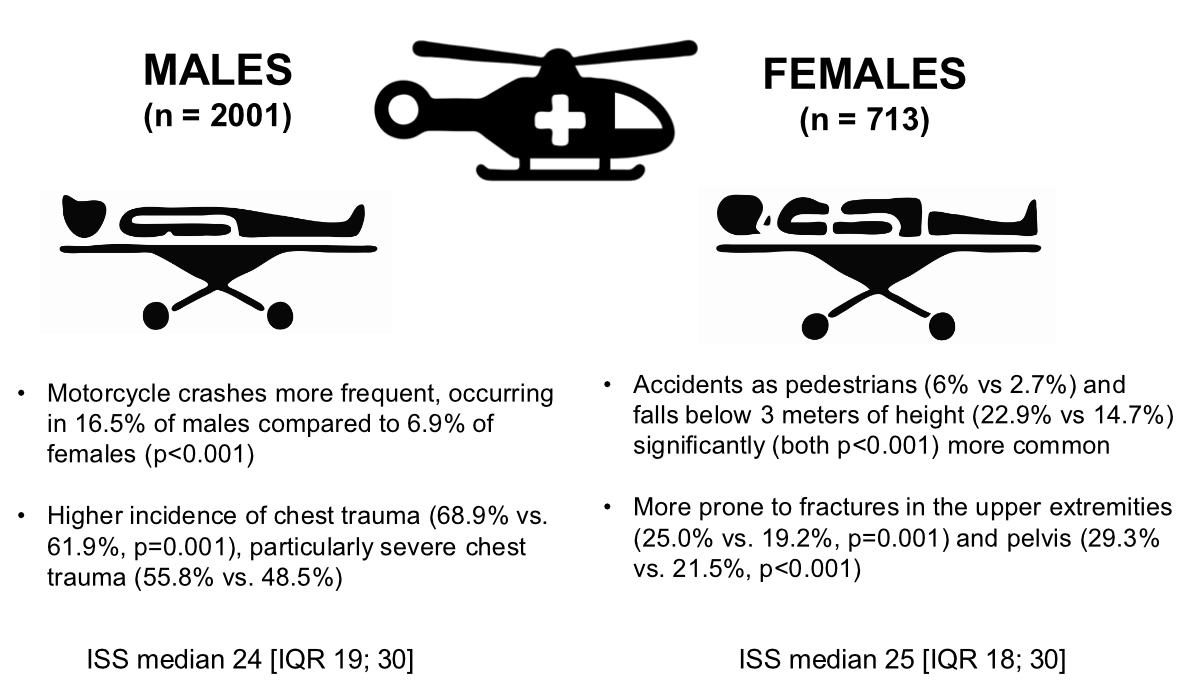
Figure 3Summary of the results.
ISS: Injury Severity Score.
Data sharing statement
The complete and deidentified dataset used
to create any tables and figures in the current study is available from the
corresponding author upon reasonable request.
Acknowledgments
Author contributions: UP designed the study. MM built the database. PM, MM and SJ
analyzed the data. All authors performed the literature search. MM and DAJ wrote the
structure of the manuscript. PM, SJ and DAJ wrote the first draft of the manuscript.
All
authors contributed to the interpretation of the data and writing of the final manuscript
and
approved the final version of the manuscript.
Special thanks go to the Swiss Trauma Registry, which provided the data. The
publication of this review has taken place in accordance with the Swiss Trauma Registry
publication guidelines
under the STR-ID 19.
Martin Müller
Department of Emergency Medicine
Inselspital
University Hospital Bern
CH-3010 Bern
martin.mueller[at]insel.ch
References
1. Pietsch U, Knapp J, Mann M, Meuli L, Lischke V, Tissi M, et al. Incidence and challenges
of helicopter emergency medical service (HEMS) rescue missions with helicopter hoist
operations: analysis of 11,228 daytime and nighttime missions in Switzerland. Scand
J Trauma Resusc Emerg Med. 2021 Jul;29(1):92. doi: https://doi.org/10.1186/s13049-021-00898-y
2. Loyd JW, Larsen T, Kuhl EA, et al. Aeromedical Transport. StatPearls. Treasure Island
(FL): StatPearls Publishing; 2024 May., Available from https://www.ncbi.nlm.nih.gov/books/NBK518986/
3. Guinzburg A, Gelikas S, Tsur AM, Nadler R, Sorkin A, Avital G, et al. The association
between helicopter emergency medical services and early casualty survival: a nationwide
study. Eur J Emerg Med. 2022 Dec;29(6):397–403. doi: https://doi.org/10.1097/MEJ.0000000000000940
4. Smith RM, Conn AK. Prehospital care - scoop and run or stay and play? Injury. 2009 Nov;40 Suppl
4:S23–6. doi: https://doi.org/10.1016/j.injury.2009.10.033
5. Galvagno SM Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ Jr, et al. Association
between helicopter vs ground emergency medical services and survival for adults with
major trauma. JAMA. 2012 Apr;307(15):1602–10. doi: https://doi.org/10.1001/jama.2012.467
6. Moors XR, Van Lieshout EM, Verhofstad MH, Stolker RJ, Den Hartog D. A Physician-Based
Helicopter Emergency Medical Services Was Associated With an Additional 2.5 Lives
Saved per 100 Dispatches of Severely Injured Pediatric Patients. Air Med J. 2019;38(4):289–93.
doi: https://doi.org/10.1016/j.amj.2019.04.003
7. Den Hartog D, Romeo J, Ringburg AN, Verhofstad MH, Van Lieshout EM. Survival benefit
of physician-staffed Helicopter Emergency Medical Services (HEMS) assistance for severely
injured patients. Injury. 2015 Jul;46(7):1281–6. doi: https://doi.org/10.1016/j.injury.2015.04.013
8. Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, et al. Helicopter
transport improves survival following injury in the absence of a time-saving advantage.
Surgery. 2016 Mar;159(3):947–59. doi: https://doi.org/10.1016/j.surg.2015.09.015
9. Helge Regener AW. Das Schweizer Rettungswesen 2023 in Zahlen. 2024. Available from:
https://www.144.ch/wp-content/uploads/2024/05/SPA_SOL_2-24_web_Das-Schweizer-Rettungswesen-in-Zahlen.pdf
10. Rega. 37 Patientinnen und Patienten pro Tag: Hilfe der Rega auch 2023 häufig gefragt.
2024. Available from: https://www.rega.ch/aktuell/neues-aus-der-rega-welt/detailseite/37-patientinnen-und-patienten-pro-tag-hilfe-der-rega-auch-im-2023-haeufig-gefragt
11. Schweigkofler U, Reimertz C, Lefering R, Hoffmann R; TraumaRegister DGU®. Bedeutung
der Luftrettung für die Schwerverletztenversorgung [Importance of air ambulances for
the care of the severely injured]. Unfallchirurg. 2015 Mar;118(3):240-4. German. doi:
10.1007/s00113-014-2566-7
12. Sethuraman KN, Marcolini EG, McCunn M, Hansoti B, Vaca FE, Napolitano LM. Gender-specific
issues in traumatic injury and resuscitation: consensus-based recommendations for
future research. Acad Emerg Med. 2014 Dec;21(12):1386–94. doi: https://doi.org/10.1111/acem.12536
13. Blok B, Slagt C, van Geffen GJ, Koch R. Characteristics of trauma patients treated
by Helicopter Emergency Medical Service and transported to the hospital by helicopter
or ambulance. BMC Emerg Med. 2024 Sep;24(1):173. doi: https://doi.org/10.1186/s12873-024-01088-6
14. Sørensen LM, Rognås L, Alstrup K. Trauma Versus Nontrauma Patients Treated by the
Danish Helicopter Emergency Medical Service: A Register-Based Study of Patient Characteristics,
Hospitalization, and Mortality. Air Med J. 2021;40(5):325–30. doi: https://doi.org/10.1016/j.amj.2021.05.005
15. Swiss Trauma Board. Swiss Trauma Registry (STR). 2025, last change: 02.01.2020. Available
from: http://www.swisstraumaboard.ch/
16. Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for
describing patients with multiple injuries and evaluating emergency care. J Trauma.
1974 Mar;14(3):187–96. doi: https://doi.org/10.1097/00005373-197403000-00001
17. Swiss Trauma Board. HSM Behandlung von Schwerverletzen. 2025. Available from: https://www.swisstraumaboard.ch/hsm-schweiz/hsm-behandlung-von-schwerverletzen/index.php
18. Swiss Trauma Board. Publikations- und Auswertungsrichtlinie Schweizer Traumaregister
(STR). 2025. Available from: https://www.swisstraumaboard.ch/downloads/str---publikationsrichtlinie-final-1.1-2016-11.pdf
19. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)
statement: guidelines for reporting observational studies. Lancet. 2007 Oct;370(9596):1453–7.
doi: https://doi.org/10.1016/S0140-6736(07)61602-X
20. Penfield W, Boldrey E. Somatic Motor and Sensory Representation in the Cerebral Cortex
of Man as Studied by Electrical Stimulation. Brain. 1937;60(4):389–443. doi: https://doi.org/10.1093/brain/60.4.389
21. Wright H, Foerder P. The Missing Female Homunculus. Leonardo. 2021;54(6):653–6. doi: https://doi.org/10.1162/leon_a_02012
22. Ashton LM, Hutchesson MJ, Rollo ME, Morgan PJ, Collins CE. A scoping review of risk
behaviour interventions in young men. BMC Public Health. 2014 Sep;14(1):957. doi: https://doi.org/10.1186/1471-2458-14-957
23. Wilson M, Daly M. Competitiveness, risk taking, and violence: the young male syndrome.
Ethol Sociobiol. 1985;6(1):59–73. doi: https://doi.org/10.1016/0162-3095(85)90041-X
24. Tamás V, Kocsor F, Gyuris P, Kovács N, Czeiter E, Büki A. The Young Male Syndrome-An
Analysis of Sex, Age, Risk Taking and Mortality in Patients With Severe Traumatic
Brain Injuries. Front Neurol. 2019 Apr;10:366. doi: https://doi.org/10.3389/fneur.2019.00366
25. Bundesamt für Statistik. Arbeitsunfälle und andere arbeitsbedingte Gesundheitsprobleme. 2024.
Available from: https://www.bfs.admin.ch/bfs/de/home.assetdetail.19204488.html
26. Marcolini EG, Albrecht JS, Sethuraman KN, Napolitano LM. Gender Disparities in Trauma
Care: How Sex Determines Treatment, Behavior, and Outcome. Anesthesiol Clin. 2019 Mar;37(1):107–17.
doi: https://doi.org/10.1016/j.anclin.2018.09.007
27. Brigitte Allex. Straßenverkehrsunfälle 2023. Bundesanstalt Statistik Österreich. 2024.
Available from: https://www.statistik.at/fileadmin/user_upload/Strassenverkehrsunfaelle2023.pdf
28. Beratungsstelle für Unfallverhütung. Mehrjahresprogramm 2021–2025. 2020. Available
from: https://www.bfu.ch/de/die-bfu/ueber-die-bfu/ziele
29. Davis DD, Tiwari V, Kane SM, et al. Pelvic Fracture. StatPearls [Internet]Treasure
Island (FL): StatPearls Publishing; 2025 Jan., Available from https://www.ncbi.nlm.nih.gov/books/NBK430734/
30. Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology
of osteoporosis. Br Med Bull. 2020 May;133(1):105–17.
31. Salari N, Darvishi N, Bartina Y, Larti M, Kiaei A, Hemmati M, et al. Global prevalence
of osteoporosis among the world older adults: a comprehensive systematic review and
meta-analysis. J Orthop Surg Res. 2021 Nov;16(1):669. doi: https://doi.org/10.1186/s13018-021-02821-8
32. Lorentzon M, Johansson H, Harvey NC, Liu E, Vandenput L, McCloskey EV, et al. Osteoporosis
and fractures in women: the burden of disease. Climacteric. 2022 Feb;25(1):4–10. doi: https://doi.org/10.1080/13697137.2021.1951206
33. Gomez D, Haas B, de Mestral C, Sharma S, Hsiao M, Zagorski B, et al. Gender-associated
differences in access to trauma center care: A population-based analysis. Surgery.
2012 Aug;152(2):179–85. doi: https://doi.org/10.1016/j.surg.2012.04.006
34. Rubenson Wahlin R, Ponzer S, Lövbrand H, Skrivfars M, Lossius HM, Castrén M. Do male
and female trauma patients receive the same prehospital care?: an observational follow-up
study. BMC Emerg Med. 2016 Jan;16(1):6. doi: https://doi.org/10.1186/s12873-016-0070-9
35. Müller M, Hautz W, Louma Y, Knapp J, Schnüriger B, Simmen HP, et al.; Swiss Trauma
Board. Accuracy between prehospital and hospital diagnosis in helicopter emergency
medical services and its consequences for trauma care. Eur J Trauma Emerg Surg. 2024 Aug;50(4):1681–90.
doi: https://doi.org/10.1007/s00068-024-02505-y
36. Hasler RM, Kehl C, Exadaktylos AK, Albrecht R, Dubler S, Greif R, et al. Accuracy
of prehospital diagnosis and triage of a Swiss helicopter emergency medical service.
J Trauma Acute Care Surg. 2012 Sep;73(3):709–15. doi: https://doi.org/10.1097/TA.0b013e31825c14b7
37. Napolitano LM, Greco ME, Rodriguez A, Kufera JA, West RS, Scalea TM. Gender differences
in adverse outcomes after blunt trauma. J Trauma. 2001 Feb;50(2):274–80. doi: https://doi.org/10.1097/00005373-200102000-00013
38. Sperry JL, Nathens AB, Frankel HL, Vanek SL, Moore EE, Maier RV, et al.; Inflammation
and the Host Response to Injury Investigators. Characterization of the gender dimorphism
after injury and hemorrhagic shock: are hormonal differences responsible? Crit Care
Med. 2008 Jun;36(6):1838–45. doi: https://doi.org/10.1097/CCM.0b013e3181760c14
39. Gannon CJ, Napolitano LM, Pasquale M, Tracy JK, McCarter RJ. A statewide population-based
study of gender differences in trauma: validation of a prior single-institution study.
J Am Coll Surg. 2002 Jul;195(1):11–8. doi: https://doi.org/10.1016/S1072-7515(02)01187-0
40. Kapral MK, Fang J, Hill MD, Silver F, Richards J, Jaigobin C, et al.; Investigators
of the Registry of the Canadian Stroke Network. Sex differences in stroke care and
outcomes: results from the Registry of the Canadian Stroke Network. Stroke. 2005 Apr;36(4):809–14.
doi: https://doi.org/10.1161/01.STR.0000157662.09551.e5
41. Glader EL, Stegmayr B, Norrving B, Terént A, Hulter-Asberg K, Wester PO, et al.; Riks-Stroke
Collaboration. Sex differences in management and outcome after stroke: a Swedish national
perspective. Stroke. 2003 Aug;34(8):1970–5. doi: https://doi.org/10.1161/01.STR.0000083534.81284.C5
42. Niewada M, Kobayashi A, Sandercock PA, Kamiński B, Członkowska A; International Stroke
Trial Collaborative Group. Influence of gender on baseline features and clinical outcomes
among 17,370 patients with confirmed ischaemic stroke in the international stroke
trial. Neuroepidemiology. 2005;24(3):123–8. doi: https://doi.org/10.1159/000082999
43. Gargano JW, Reeves MJ; Paul Coverdell National Acute Stroke Registry Michigan Prototype
Investigators. Sex differences in stroke recovery and stroke-specific quality of life:
results from a statewide stroke registry. Stroke. 2007 Sep;38(9):2541–8. doi: https://doi.org/10.1161/STROKEAHA.107.485482
44. Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CD, et al.; European
BIOMED Study of Stroke Care Group. Sex differences in the clinical presentation, resource
use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational
hospital-based registry. Stroke. 2003 May;34(5):1114–9. doi: https://doi.org/10.1161/01.STR.0000068410.07397.D7
45. Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG. Gender-related differences in
intensive care: a multiple-center cohort study of therapeutic interventions and outcome
in critically ill patients. Crit Care Med. 2003 Jul;31(7):1901–7. doi: https://doi.org/10.1097/01.CCM.0000069347.78151.50
46. Romo H, Amaral AC, Vincent JL. Effect of patient sex on intensive care unit survival.
Arch Intern Med. 2004 Jan;164(1):61–5. doi: https://doi.org/10.1001/archinte.164.1.61
47. Kudenchuk PJ, Maynard C, Martin JS, Wirkus M, Weaver WD; The MITI Project Investigators.
Comparison of presentation, treatment, and outcome of acute myocardial infarction
in men versus women (the Myocardial Infarction Triage and Intervention Registry).
Am J Cardiol. 1996 Jul;78(1):9–14. doi: https://doi.org/10.1016/S0002-9149(96)00218-4
48. Steingart RM, Packer M, Hamm P, Coglianese ME, Gersh B, Geltman EM, et al.; Survival
and Ventricular Enlargement Investigators. Sex differences in the management of coronary
artery disease. N Engl J Med. 1991 Jul;325(4):226–30. doi: https://doi.org/10.1056/NEJM199107253250402
49. Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men
hospitalized for coronary heart disease. N Engl J Med. 1991 Jul;325(4):221–5. doi: https://doi.org/10.1056/NEJM199107253250401
50. Amacher SA, Zimmermann T, Gebert P, Grzonka P, Berger S, Lohri M, et al.; Swiss ICU
Trial Group. Sex disparities in ICU care and outcomes after cardiac arrest: a Swiss
nationwide analysis. Crit Care. 2025 Jan;29(1):42. doi: https://doi.org/10.1186/s13054-025-05262-5
51. Wallace AB. The exposure treatment of burns. Lancet. 1951 Mar;1(6653):501–4. doi: https://doi.org/10.1016/S0140-6736(51)91975-7
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4502.