Figure 1Participation flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.4344
Tobacco smoking is the leading preventable cause of early mortality and morbidity in developed countries. Approximately 9500 deaths per year are attributable to tobacco smoking in Switzerland [1].
By delivering effective interventions to support smoking cessation, community pharmacies play an important role in reducing the tobacco burden in the population [2]. Since pharmacists are easily accessible to the community, they can counsel a broad clientele [2]. Although brief opportunistic counselling on smoking cessation has proven helpful, more sustainable success can be achieved with dedicated counselling [2, 3].
Community pharmacies also serve as smokers’ preferred source of evidence-based smoking cessation medication therapies, such as nicotine replacement therapies [4, 5]. However, costs for nicotine replacement therapies vary between 5 and 11 Swiss francs per day (according to the Swiss market, April 2024), and these therapies are typically not reimbursed by health insurance in Switzerland. Therefore, many smokers seek alternative nicotine delivery systems. These systems involve methods of delivering nicotine that differ from traditional cigarettes. As shown in table 1, alternative nicotine delivery systems include e-cigarettes, tobacco heating systems, nicotine pouches, and snus, which are up to five times cheaper than nicotine replacement therapies, with the exception of tobacco heating systems in Switzerland [6]. Liakoni and colleagues recently described the characteristics of nicotine delivery products to determine their potential in cigarette smoking cessation [7]. The popularity of e-cigarettes has increased to the point that they are among the most common smoking cessation aids in Switzerland [8]. Given the inherent price competition around alternative nicotine delivery systems compared to tobacco cigarettes, the role of pharmacies in smoking cessation interventions must be explored in this context.
Table 1Brief explanations of alternative nicotine delivery systems.
| Alternative nicotine delivery system | Explanation |
| E-cigarettes | A battery-powered device that vaporises a liquid containing nicotine, flavourings, and other chemicals. |
| Tobacco heating systems (THSs) | A device that heats tobacco to a temperature below combustion, releasing a nicotine-containing aerosol without burning the tobacco. |
| Nicotine pouches | A product that contains a nicotine-based formulation, which is placed under the lip. |
| Snus | A product that contains moist tobacco, which is placed under the lip. |
Despite pharmacies’ potential as providers of smoking cessation interventions [9, 10], several previous international and national studies have shown that the prevalence of these services is limited [11–18]. The most recent of these studies was conducted nearly a decade ago, when only nicotine replacement therapies were available as nicotine alternatives to tobacco cigarettes. Therefore, we explored Swiss community pharmacists’ interest in offering and improving smoking cessation counselling and their openness to integrating alternative nicotine delivery systems into their smoking cessation interventions. These findings provide a foundation for planning, testing, and disseminating future interventions to strengthen and expand smoking cessation services in Swiss community pharmacies to reduce the harm caused by tobacco smoking.
This cross-sectional study was conducted in Switzerland, where community pharmacies play a key role in patient care by providing both medication dispensation and various patient-services. The counselling provided during medication dispensation (e.g. prescribed medication such as bupropion) is reimbursed by mandatory health insurance under a remuneration system established in 2001. Other services that community pharmacies offer (e.g. cardiovascular risk factors such as blood pressure measurement or smoking cessation counselling) are not covered by mandatory health insurance; customers or complementary health insurance must pay for them.
The study was reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cross-sectional studies.
The online survey was sent to all pharmacies affiliated with the Swiss Pharmacists’ Association (pharmaSuisse) in the German- and French-speaking regions of Switzerland. Pharmacies in the Italian-speaking region were excluded to avoid language barriers, as the survey was only available in French or German. To increase the response rate, a printed version was sent to all pharmaSuisse member pharmacies in the cantons of Bern and Lucerne, with a reminder email sent 2 weeks later, and the cantonal pharmacy associations of Lucerne, Zug, Fribourg, Geneva, Thurgau, Aargau, Jura, and Vaud were asked to inform their members about the survey via newsletter or email through their communication channels. Additionally, the Swiss Pharmacists’ Association was asked to publish the link to the online survey in a monthly newsletter. One pharmacist per pharmacy was asked to fill out the survey, even though several pharmacists often work in one pharmacy. The questions focused on the processes and attitudes of an individual pharmacist, which could be influenced by the environment of the pharmacy in which they work.In line with ethical considerations, the surveys were collected anonymously. Because no sensitive or personal health data were collected, the study was not subject to the Federal Act on Research Involving Human Beings and did not require ethical approval.
For this study, an online survey was developed through interprofessional collaboration with an epidemiologist and several physicians and pharmacists. To capture the current clinical practice of smoking cessation counselling, the development process began with semi-structured interviews with four community pharmacists (three women and one man)who were experienced in offering these services to their patients. The four pharmacists were selected based on convenience. They contributed to adapting the vignettes and questions by improving clarity and assessing feasibility. The interview questions were based on several previous surveys [11–18, 20]. The interviews and the inclusion of specific literature [11–16, 18, 20] enabled the development of the survey.
The survey was piloted for content, format, relevance, clarity, and time for completion within the research group and with two of the four pharmacists who participated in the initial interview. The survey was finalised after refinement based on their suggestions. The final version consisted of three sections with 39 questions in total. Responses were recorded using ordinal or 6-point Likert-type scales. Section 1 collected sociodemographic data on the participants and the pharmacies where they worked. Section 2 explored the clinical practice of smoking cessation interventions and pharmacists’ perceptions of and future needs for the interventions. Smoking cessation counselling was classified into three categories based on the level of involvement of pharmacists in supporting the smoking cessation process:
A clinical vignette corresponding to a typical situation in community pharmacy practice was used to assess pharmacists’ behaviour in clinical practice [21]. The vignette presented the case of a 35-year-old long-term smoker who visited a pharmacy to inquire about nicotine replacement therapy as she considered quitting. Section 3 collected data on pharmacists’ perceptions of the efficacy and safety of alternative nicotine delivery systems as smoking cessation aids. The questionnaire was developed in German and translated into French with the help of two native French speakers. The questionnaire was coded on FindMind® [22].
Completed surveys received between 1 April and 9 May 2022 were included in the descriptive statistical analyses. Primary outcome measures focused on the frequency and duration of smoking cessation interventions provided by pharmacists. Secondary outcome measures provided additional insights into pharmacists’ perceptions of nicotine products, their counselling practices, and external factors such as training and compensation. The frequencies and proportions of the answers to the categorical questions are reported. To evaluate the 6-point Likert-type scale, the mean, standard deviation, and 95% confidence interval were calculated, and the results are displayed in figures. Statistical analyses were performed using R version 4.2.0 and the packages tidyverse (v.1.3.2), bfsMaps (v.1.199.3), and ggplot2 (v.3.4.1).
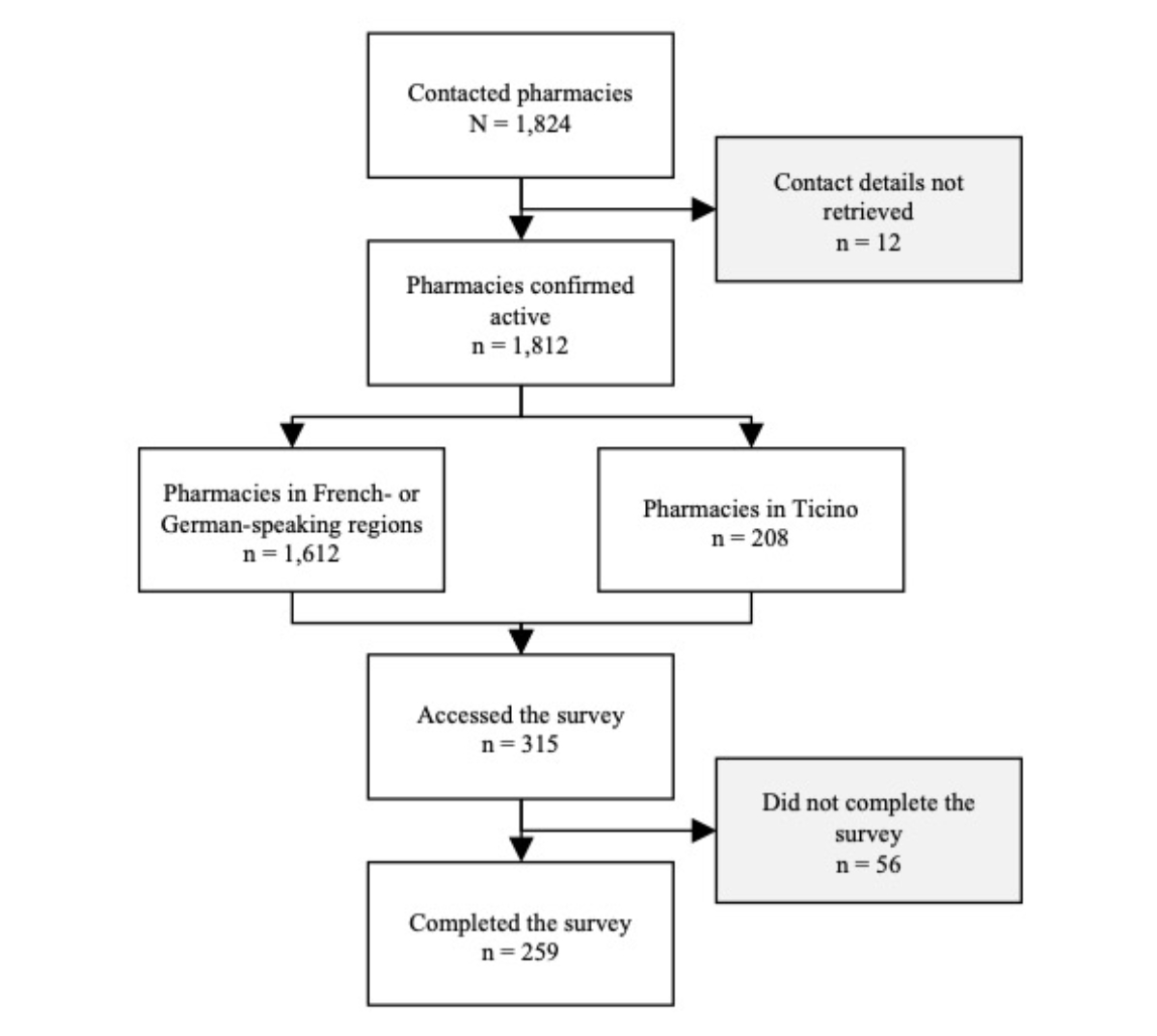
Based on Swiss Federal Statistics [23], there were 1839 community pharmacies in Switzerland in 2022 (appendix figure S1). In April 2022, 1824 pharmacies were invited to participate in the survey (1812 were confirmed active based on a follow-up in 2025). Of these, 208 pharmacies (11.4%) were in the Italian-speaking region of Switzerland (Ticino) and were therefore not expected to complete the survey in another language, reducing the number of eligible pharmacies to 1612. Overall, 250 of 1612 pharmacists (15.5%) completed the survey, along with 9 pharmacists located in Ticino, who were thus included in the statistical analysis. As depicted in figure 1, the total sample size was 259, accounting for 14.1% of the pharmacies in Switzerland in 2022.
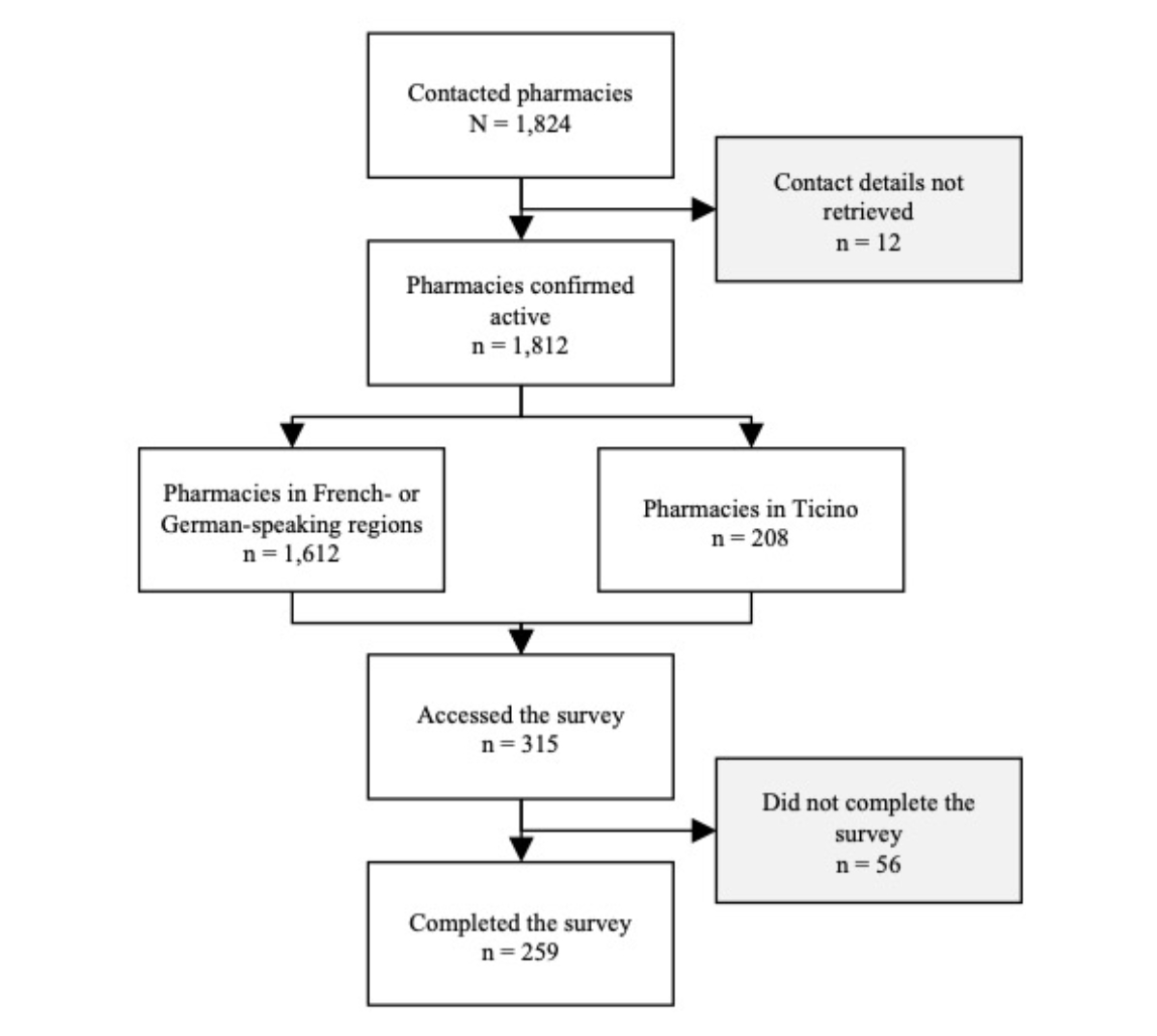
Figure 1Participation flowchart.
Most participants were women (n = 189, 73.0%), German-speaking (n = 194, 74.9%), under 51 years old (n = 230, 88.8%), and working in a leading position (n = 179, 69.1%). Ninety (34.7%) worked in the countryside, 72 (27.8%) in suburbs, and 97 (37.5%) in cities (table 2). In total, 44 (17%) participants had never received any training on smoking cessation counselling during their career. Figure 2 presents the distribution of participants and their characteristics across cantons. The Mittelland region (Bern, Lucerne, and Aargau) and the cantons of Obwalden, Nidwalden, and Thurgau had the highest participation rates (up to 50%), while French- and Italian-speaking cantons showed a limited response rate (less than 10%). Only a few responses were collected from pharmacies in Ticino (where the spoken language differed from the survey languages). Finally, no responses were collected from pharmacies in Appenzell, Glarus, Schwyz, or Uri, although most of these cantons have fewer than 10 pharmacies.

Figure 2Recruitment by canton (n = 259). The map plotted in this figure is provided by the Swiss Federal Statistical Office©. The total number of pharmacies per canton is proxied by the number of pharmacies registered in February 2025. A total of 59 pharmacists did not indicate their canton and are not represented in the plot.
Table 2Descriptive statistics of the sample.
| Characteristic | n | % | |
| Gender | Women | 189 | 73.0 |
| Men | 66 | 25.5 | |
| Other (trans or non-binary) | 2 | 0.8 | |
| Information missing | 2 | 0.8 | |
| Language | French | 65 | 25.1 |
| German | 194 | 74.9 | |
| Age in years | Less than 30 | 41 | 15.8 |
| 30 to 40 | 82 | 31.7 | |
| 41 to 50 | 54 | 20.8 | |
| 51 to 60 | 53 | 20.5 | |
| 61 or more | 25 | 9.7 | |
| Information missing | 4 | 1.5 | |
| Years of experience | Less than 5 | 54 | 20.8 |
| 5 to 15 | 87 | 33.6 | |
| 16 to 25 | 50 | 19.3 | |
| 26 to 35 | 52 | 20.1 | |
| 36 or more | 15 | 5.8 | |
| Information missing | 1 | 0.4 | |
| Role at the pharmacy | Head/adjunct pharmacist | 179 | 69.1 |
| Employee | 77 | 29.7 | |
| Information missing | 3 | 1.2 | |
| Working time at the pharmacy | Less than 60% | 30 | 11.6 |
| 61% to 80% | 55 | 21.2 | |
| 81% to 100% | 170 | 65.6 | |
| Information missing | 4 | 1.5 | |
| Location of the pharmacy | Countryside | 90 | 34.7 |
| Suburb | 72 | 27.8 | |
| City | 97 | 37.5 | |
| Post-graduate qualifications | Anamnesis in primary care | 122 | 47.1 |
| Clinical pharmacy | 17 | 6.6 | |
| Community pharmacy | 125 | 48.3 | |
| Hospital pharmacy | 1 | 0.4 | |
| Doctorate | 28 | 10.8 | |
| None | 4 | 1.5 | |
| Information missing | 39 | 15.1 | |
| Counselling room in the pharmacy | Yes | 238 | 91.9 |
| No | 20 | 7.7 | |
| Information missing | 1 | 0.4 | |
| Trained in smoking cessation | Yes | 215 | 83.0 |
| No | 44 | 17.0 | |
Brief counselling during sales of nicotine replacement therapies was offered at least once a month by 180 (71.1%) pharmacists (figure 3). Brief opportunistic smoking cessation counselling was offered by 128 pharmacists (51.2%) at least once a month. Dedicated smoking cessation counselling was offered by 49 (20.7%) pharmacists; 115 reported never offering dedicated counselling. Regarding the duration of the different interventions, 174 respondents (67.2%) spent 5 to 15 minutes on brief counselling during the sale of nicotine replacement therapies, while 133 (51.4%) spent the same amount of time on brief opportunistic smoking cessation counselling. For dedicated smoking cessation counselling, 57 (22.0%) pharmacists reported spending 16 to 30 minutes on the intervention, and 15 (5.8%) reported spending more than 30 minutes, accounting for 46.2% of the pharmacists offering such counselling.
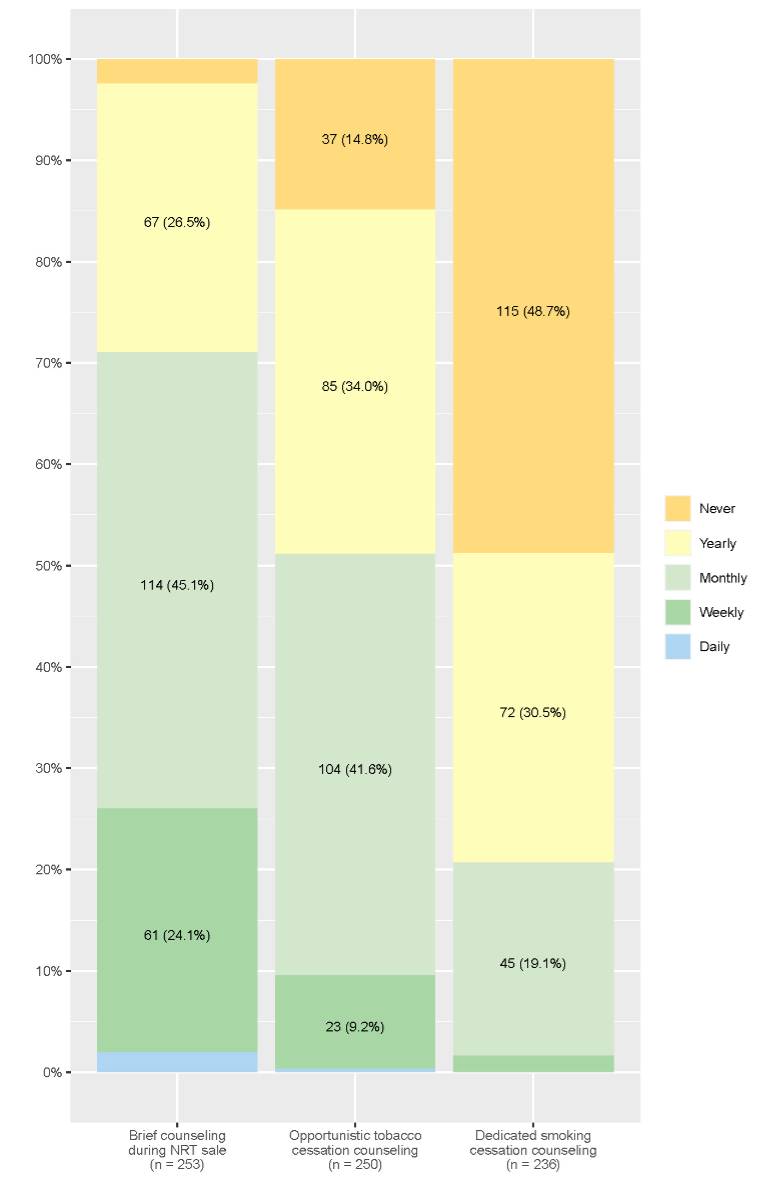
Figure 3Frequency of smoking cessation interventions offered in community pharmacies [n, (%)], as reported by pharmacists. Frequencies with percentages below 2.5% are not displayed. There are 6 missing values for “Brief counselling during nicotine replacement therapy sale”, 9 for “Opportunistic tobacco cessation counselling”, and 23 for “Dedicated smoking cessation counselling”.
Figure 4 presents mean scores and 95% confidence intervals of the perceived risks of addictiveness, health hazards, and carcinogenicity for each nicotine-based product, based on a 6-point Likert scale. Overall, conventional cigarettes were perceived as the most addictive (mean = 5.91, standard deviation [SD] = 0.33), hazardous to health (mean = 5.92, SD = 0.33), and carcinogenic (mean = 5.91, SD = 0.31) nicotine-containing products. Nicotine replacement therapies were considered the least hazardous to health (mean = 2.87, SD = 1.13), the least carcinogenic (mean = 1.96, SD =1.16), and the least addictive (mean = 4.11, SD = 1.15) products. Regarding alternative nicotine delivery systems, all were considered similarly strongly addictive (mean ≥5.25). The products considered most hazardous by pharmacists were tobacco heating systems (mean = 4.81, SD = 0.89) and snus (mean = 4.88, SD = 0.91). Regarding carcinogenicity, tobacco heating systems had the highest perceived risk (mean = 4.63, SD = 1.09), followed by snus (mean = 4.48, SD = 1.30). By contrast, lower perceived risks were reported for e-cigarettes (mean = 4.13, SD = 1.32) and nicotine pouches (mean = 3.61, SD = 1.63).

Figure 4Perceived addictiveness, health hazard, and carcinogenicity of the different nicotine-based products and nicotine replacement therapies (NRT) (n = 259). 6-point Likert scale: 1: Not at all; 6: Totally. The mean value is displayed with 95% confidence intervals. Missing values for each question are as follows: addictiveness: 14 for cigarettes, 61 for tobacco heating systems, 28 for e-cigarettes, 57 for snus, 118 for nicotine pouches, and 0 for pharmaceutical nicotine replacement therapies; health hazard: 6 for cigarettes, 53 for tobacco heating systems, 21 for e-cigarettes, 49 for snus, 83 for nicotine pouches, and 11 for pharmaceutical nicotine replacement therapies; carcinogenicity: 12 for cigarettes, 83 for tobacco heating systems, 69 for e-cigarettes, 83 for snus, 106 for nicotine pouches, and 34 for pharmaceutical nicotine replacement therapies.
Figure 5 presents how often pharmacists recommended nicotine products. Nicotine replacement therapies were the most frequently recommended, with 67 (27.0%) pharmacists always recommending them and 105 (42.3%) recommending them to more than half of the patients who were interested in quitting smoking.
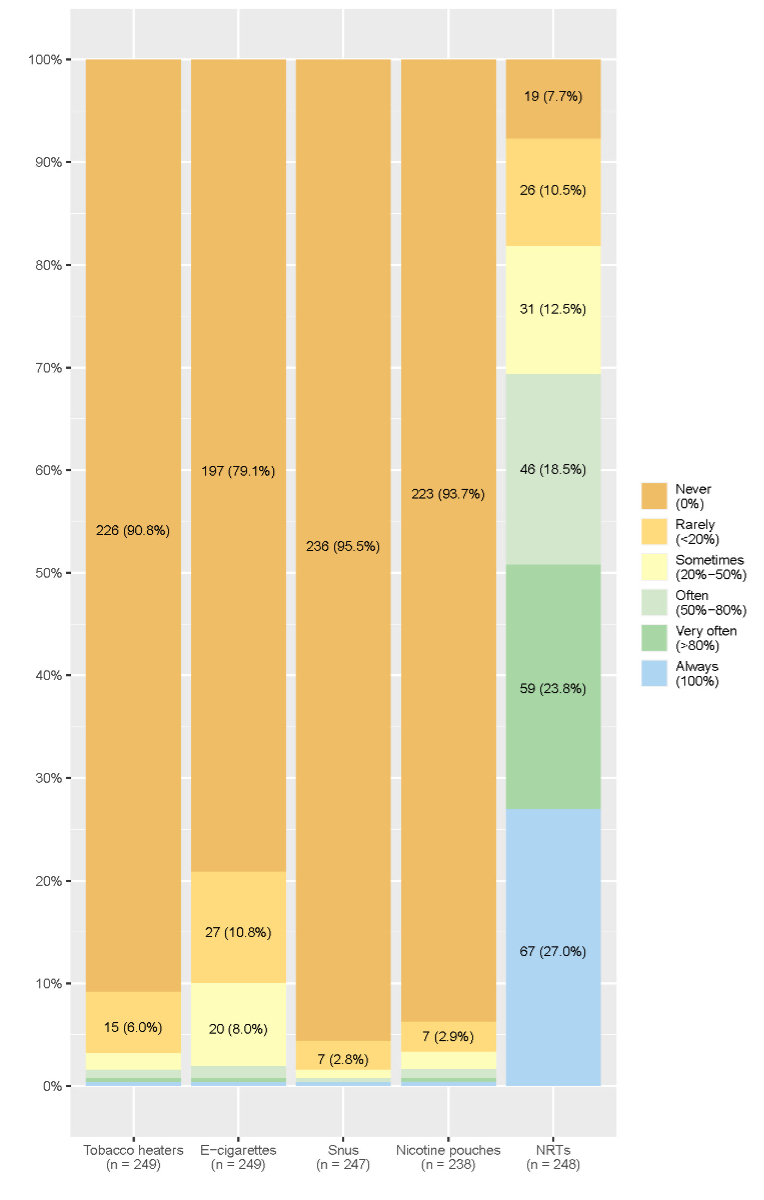
Figure 5Pharmacists’ self-reported frequency of recommendation of alternative nicotine delivery systems and nicotine replacement therapies as smoking cessation aids [n, (%)]. Frequencies with percentages below 2.5% are not displayed. There are 11 missing values for nicotine replacement therapies, 10 for tobacco heating systems, 10 for e-cigarettes, 21 for nicotine pouches, and 12 for snus.
Regarding other nicotine products, at least 90% of pharmacists reported never recommending tobacco heating systems, snus, or nicotine pouches; 52 (20.9%) reported recommending e-cigarettes in some situations; and 5 reported recommending e-cigarettes most frequently. When asked under what circumstances they would recommend e-cigarettes, three pharmacists always recommended them as smoking cessation aids, six considered them for patients who did not want to use medications, nine considered them for patients who had used medications to stop smoking in the past, and six stated that they typically did not recommend e-cigarettes or discouraged their patients from using them. In total, 99 (32.2%) pharmacists provided reasons for refraining from recommending e-cigarettes: 30 (30.3%) pointed out the lack of data on safety or efficacy as a smoking cessation aid, 30 (30.3%) favoured other smoking cessation aids, 33 (33.3%) highlighted the addictive potential of e-cigarettes, and 6 (6.1%) provided various other reasons.
Regarding the perceptions of smoking cessation counselling, pharmacists moderately agreed that such counselling was part of their profession (mean = 4.27, SD = 1.48), and their motivation to conduct such counselling was moderate (mean = 4.43, SD = 1.29). Their sense of being well-trained corresponded to the midpoint of the Likert-type scale (mean = 3.60, SD = 1.39).
More than half (154, 59.5%) of the pharmacists did not answer the question about how much they were paid by their clients for smoking cessation interventions; among the 105 who answered, 68 (64.8%) reported not being remunerated, 44 (32.4%) reported remuneration lower than 60 Swiss francs, and 3 (2.9%) reported remuneration of more than 60 Swiss francs.
To improve smoking cessation counselling as a regular activity for pharmacists, the most frequently identified need was higher demand (mean = 4.78, SD = 1.42), followed by the availability of decision aids (mean = 4.58, SD = 1.51), more training (mean = 4.39, SD = 1.43), financial compensation, preferably by health insurance (mean = 4.35, SD = 1.63), and better collaboration with other health professionals (mean = 4.25, SD = 2.13).
Most pharmacists considered supplemental training on alternative nicotine delivery systems useful (n = 211, 86.5%), and 168 (68.9%) stated that alternative nicotine delivery systems should be integrated into general training on smoking cessation.
Smoking cessation interventions are offered sporadically in Swiss community pharmacies.
Of the three types of smoking cessation interventions, brief counselling during the sale of nicotine replacement therapies was pharmacists’ most frequently performed intervention. Nicotine replacement therapy must be dispensed in community pharmacies, as its use can increase quit rates by up to twofold [5]. In Switzerland, nicotine replacement therapies can be purchased only in pharmacies, drugstores, and online [24]. Most clients prefer to purchase medication at pharmacies rather than online [25], which could increase the frequency of counselling during sales and provide an opportunity to transition to a more intensive smoking cessation intervention. Brief opportunistic smoking cessation counselling was less frequently reported, with almost half of the participants offering it less than once a month. According to NHS guidance on brief interventions for smoking cessation [26], a short intervention takes between 5 and 10 minutes. The duration reported by Swiss pharmacists (5 to 15 minutes) for the short interventions is slightly longer than what the guidance suggests, but it remains broadly consistent with the intent of brief intervention guidelines. In a meta-analysis by Stead et al., brief advice as part of a minimal intervention demonstrated a statistically significant increase in quit rates by 1 to 3% compared to no advice [3]. Since short interventions provided by healthcare professionals have proven effective, a higher frequency of such interventions would be desirable and is recommended by the WHO [27]. Dedicated smoking cessation counselling is especially rare in Swiss community pharmacies. Only 20.7% of participating pharmacists offered dedicated counselling in their pharmacies, with most offering it as rarely as once a year. In 2012, a survey by Müller et al. showed similar results, with 46% of Swiss pharmacists offering dedicated smoking cessation counselling [15]. The decrease since then, as well as the only moderate motivation of pharmacists to offer the intervention, indicates the need for a transition to strengthen future dedicated smoking cessation counselling. The frequency of dedicated smoking cessation counselling offered in other countries [11, 14] reveals that there is room for growth in Switzerland. Increasing the availability and frequency of the service is important, as intensive counselling has proven to be not only effective [2, 3] but also cost-effective [28].
Considering the recommended smoking cessation aids, roughly 20% of pharmacists would actively recommend e-cigarettes as smoking cessation aids. In 2021, the Sentinella study found that 31% of Swiss general practitioners recommended e-cigarettes as smoking cessation aids to their patients [20], indicating that Swiss pharmacists responding to our study were more reluctant to recommend them than Swiss general practitioners in the Sentinella network. Several factors may contribute to this difference. First, while physician guidelines consider e-cigarettes a valid second-line smoking cessation method when other methods fail [29, 30], a position shared by various health professional organisations [29], pharmacy guidelines for smoking cessation typically do not mention them. Additionally, while nicotine replacement therapies are primarily available through pharmacies and drugstores, with online platforms serving as the only alternative source, e-cigarettes are not available in any Swiss community pharmacies but can be obtained through both online platforms and physical retail outlets. Unlike nicotine replacement therapies, which are widely approved and supported by national guidelines, e-cigarettes face regulatory uncertainty. Nicotine replacement therapies are generally not reimbursed, and e-cigarettes are never covered. Thus, regulatory differences between nicotine replacement therapies and e-cigarettes, along with legal restrictions that hinder the reimbursement of preventive services by health insurance, may influence pharmacists’ willingness to recommend and sell these products, particularly in the context of smoking cessation counselling, which is product-centred. By contrast, general practitioners can provide smoking cessation counselling as a service reimbursed by health insurance. However, they typically do not dispense nicotine replacement therapies or e-cigarettes directly. This structural difference may partly explain their greater willingness to recommend e-cigarettes, particularly as part of a harm reduction strategy.
Pharmacists were particularly concerned about the efficacy of e-cigarettes as smoking cessation aids. However, the newest Cochrane living systematic review (2024) found high-certainty evidence that nicotine-containing e-cigarettes increase quit rates compared with nicotine replacement therapies [31]. Another primary concern for pharmacists regarding e-cigarettes was safety. Surveys of smoking cessation practitioners (Hiscock et al.) and pharmacists in the UK (Gomes et al.) also identified safety as a key concern [32, 33] and suggested that more research on safety may reduce this concern. Although studies have demonstrated that e-cigarettes are safer than combustible cigarettes [34], the most recent NICE guidelines on treating tobacco dependency recommend research on the health effects, especially long-term effects, of e-cigarettes [35]. Health practitioners’ concern that e-cigarette addiction will replace cigarette addiction contributes to their reluctance to recommend e-cigarettes. The results of the Swiss ESTxENDS RCT, published in 2024, confirmed an increase in the abstinence rate from tobacco smoking when e-cigarettes were added to standard-of-care counselling and a decrease in the rate of nicotine abstinence [6]. Professional organisations are expected to adapt official guidelines and position statements on the use of alternative nicotine delivery systems in light of the ESTxENDS RCT results.
Overall, we found that pharmacists perceived alternative nicotine delivery systems as safer than conventional cigarettes. This finding aligns with studies showing alternative nicotine delivery systems’ potential for harm reduction [34]. According to a report by the Swiss Federal Commission for Questions on Addiction and Prevention of Noncommunicable Diseases, participating pharmacists rated tobacco heating systems as more hazardous to health than e-cigarettes [36]. On the other hand, participants did not distinguish much between the addictive potential of the different alternative nicotine delivery systems. According to the report, however, e-cigarettes and tobacco heating systems are expected to increase the proportion of consumers who develop addictive behaviour compared with other alternative nicotine delivery systems [36]. The discrepancy between our survey and the abovementioned report emphasises the importance of proper training on alternative nicotine delivery systems. This aligns with the participants’ interest in attending training about alternative nicotine delivery systems. Because most alternative nicotine delivery systems are tied to the tobacco industry, whose primary goal is expanding its consumer base, training in smoking cessation counselling should be led by independent organisations to ensure that the focus is on helping smokers quit while limiting exposure to alternative nicotine delivery systems among non-smokers and youth.
Despite the large amount of time invested in the interventions, most pharmacists requested no financial compensation. Accordingly, most participants supported the idea of receiving remuneration for the service, preferably through healthcare funding, as a need for future smoking cessation counselling. In a study by Roski et al., the impact of providing financial incentives was tested on adherence to smoking cessation clinical practice guidelines and patients’ cessation behaviours [37]. They found that clinics of a large multispecialty medical group that received a financial incentive for their services were significantly more likely to identify their patients’ tobacco use status. Although this result is based solely on the increased identification of smoking status, it may indicate potential for enhancing smoking cessation counselling by pharmacists through reimbursement. In a report for the Tobacco Prevention Fund (TPF), one proposal for reimbursement through healthcare funding was to create a list of supplementary insurance contracts that cover non-medical smoking cessation counselling. This list would include pharmacists as eligible service providers [38]. Reimbursement for such a service appears feasible, as the Swiss healthcare system is increasingly recognising the value of pharmacy-based services beyond dispensing medication. In 2027, a revision of the Swiss health insurance law will enable pharmacists to charge for various preventive and pharmaceutical services, such as optimising drug therapy and improving treatment adherence, directly via compulsory health insurance, provided that these preventive services are part of a national or cantonal programme [39].
Another possibility to strengthen future smoking cessation counselling is higher demand, which most pharmacists reported. To increase demand, awareness of pharmacy-based services must be raised. As shown in previous studies, this can be achieved by conducting campaigns promoting the availability of smoking cessation counselling in pharmacies. In an evaluation of the campaign “Tabak Adieu” (“Goodbye Tobacco”) in 1996 in Basel, Gschwend et al. reported a 41% increase in encounters with clients interested in smoking cessation during the campaign [18]. They also showed that intensive counselling increased from 32% to 58%. Therefore, a campaign could be modelled on “Tabak Adieu”, which relied on training events for the pharmacists before the campaign and public promotion with placards, newspaper articles, and window advertisements during the campaign. The training included in such campaigns would address the perceived lack of training identified in this survey, another need reported by most participants. Similar findings have been reported in neighbouring countries. For example, a study by Gautier et al. [40] found that primary healthcare professionals in France viewed additional education and training as essential to improving smoking cessation efforts among older adults. Likewise, research by Twardella and Brenner [41] involving general practitioners in Germany identified insufficient training as a key barrier to effectively promoting smoking cessation services. This theme is echoed outside Europe. For instance, the study by Aquilino et al. in Iowa, USA, investigated the effect of previous training in smoking cessation on the provision of the service [11]. They found pharmacists who had recently attended a smoking cessation programme or obtained a certificate in smoking cessation counselling to be more likely to provide cessation counselling to patients.
Finally, most pharmacists indicated that improvement in interprofessional collaboration is necessary to enhance future smoking cessation counselling. Professionals involved in smoking cessation support, such as general practitioners, are often overwhelmed by their workload. As a result, certain responsibilities may need to be transferred to other healthcare providers. Our study indicates that pharmacists recognise the potential for this shift, suggesting that increased collaboration between pharmacists and other healthcare professionals is a viable solution.
According to the Tobacco Control Scale, Switzerland ranks poorly compared with other countries, indicating that the country is behind in the implementation and effectiveness of tobacco control programs on the international stage. This underscores the need to enhance smoking cessation interventions in community pharmacies as a way to bridge the gap.
This study took steps to maximise the response rate, and our survey’s response rate was the highest to date for such a topic in Switzerland; however, the response rate remained low at around 16%, similar to another survey of pharmacies using comparable methods [42]. Therefore, the results apply only to the pharmacies that responded to this survey, and extrapolation to the general population of pharmacists is limited. A strength of our work is the differentiation between three types of smoking cessation interventions and the clarification of each with a short description. This increased the accuracy of the data collected on the interventions offered in community pharmacies in Switzerland. Additionally, by including alternative nicotine delivery systems, our survey captured a broader context of nicotine delivery systems. Another strength was the availability of the survey in French and German, allowing a large proportion of Swiss pharmacists to answer the questions in their mother tongue. Our results were based on self-reported data, which is the most appropriate way to assess attitudes and perceptions. However, participants were prone to not replying to some questions, and a few inconsistent answers were also identified in the data (e.g. two pharmacists reported that they never conducted brief opportunistic smoking cessation interventions but also that they spent more than 15 minutes on such interventions). Additionally, because the surveys were collected anonymously, we were unable to verify whether participants filled out the questionnaire multiple times or whether more than one pharmacist per pharmacy completed it. Another limitation is the absence of data on the proportion of nicotine replacement therapy sales accompanied by counselling, as pharmacists were not asked about the frequency of nicotine replacement therapy dispensing, and the occurrence of counselling does not necessarily indicate that nicotine replacement therapies were sold. Additionally, we lacked external data sources to verify self-reported attitudes.
This cross-sectional study shows that while many pharmacists engage in basic interventions such as brief counselling during nicotine replacement therapy sales, there remains significant scope to expand more intensive, dedicated counselling services. The reluctance to incorporate alternative nicotine delivery systems, particularly e-cigarettes, into smoking cessation strategies reflects concerns about their safety and efficacy. Moving forward, greater financial incentives for counselling, targeted campaigns, improved training, including training on alternative nicotine delivery systems, and collaboration with other healthcare professionals could empower pharmacists to offer more comprehensive support to smokers, ultimately reducing tobacco-related harm in the population.
Both the data and the code used for the analyses are included in the supplementary files available for download at https://doi.org/10.57187/s.4344.
We would like to thank all the pharmacists who participated in our survey, contributing immensely to this work. Furthermore, we thank all the other individuals involved in the development and distribution of the survey.
This study was funded by internal funds at BIHAM. RA’s work on the efficacy, safety, and toxicology of e-cigarettes was supported by grants (173552 and 213614) from the Swiss National Science Foundation, a grant (19.017477) from the Swiss Tobacco Prevention Fund, a grant (KFS4744-02-2019) from Swiss Cancer Research, and by LungeZürich.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. – Isabelle Jacot-Sadowski: payment to her institution for travel to the Congress of the “Société francophone de tabacologie”, and for leadership or fiduciary role in Swiss Expert Group on Smoking and Nicotine Cessation (co-chair), EviPrev Swiss recommendations for prevention in medical practice (member of committee) and PEPra -Evidence-based prevention in the medical practice (task force member), unrelated to this article. – Reto Auer: funding from Swiss National Science Foundation (SNSF) (grant number IICT_33IC30_173552 and PLS 32003B_214832), Swiss Tobacco Prevention Fund (TPF) (grant number 19.017477 and 326.5-2/60), Swiss Cancer Research (SCR) (grant number KFS4744-02-2019) and “Lunge Zürich”. Institutional fees for participation in “Eidgenössische Kommission für Fragen zu Sucht und Prävention nichtübertragbarer Krankheiten (EKSN)” and “Fachgremium für die Tabak- und Nikotinentwöhnung”, all unrelated to this article. – No other potential conflict of interest related to the content of this manuscript was disclosed.
1. Swiss Health Observatory. Swiss Monitoring System of Addiction and Noncommicable Diseases (MonAM) – Tobacco consumption (age: 15+) 2024. Available from: https://ind.obsan.admin.ch/en/indicator/monam/tobacco-consumption-age-15
2. Carson-Chahhoud KV, Livingstone-Banks J, Sharrad KJ, Kopsaftis Z, Brinn MP, To-A-Nan R, et al. Community pharmacy personnel interventions for smoking cessation. Cochrane Database Syst Rev. 2019 Oct;2019(10):CD003698. doi: https://doi.org/10.1002/14651858.CD003698.pub3
3. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013 May;2013(5):CD000165. doi: https://doi.org/10.1002/14651858.CD000165.pub4
4. McBane SE, Corelli RL, Albano CB, Conry JM, Della Paolera MA, Kennedy AK, et al. The role of academic pharmacy in tobacco cessation and control. Am J Pharm Educ. 2013 Jun;77(5):93. doi: https://doi.org/10.5688/ajpe77593
5. Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2004;(3):CD000146.
6. Auer R, Schoeni A, Humair JP, Jacot-Sadowski I, Berlin I, Stuber MJ, et al. Electronic Nicotine-Delivery Systems for Smoking Cessation. N Engl J Med. 2024 Feb;390(7):601–10. doi: https://doi.org/10.1056/NEJMoa2308815
7. Liakoni E, Christen SE, Benowitz NL. E-cigarettes, synthetic nicotine, heated-tobacco and smokeless nicotine delivery products: the nicotine landscape beyond combustible cigarettes. Swiss Med Wkly. 2024 Nov;154(11):3583. doi: https://doi.org/10.57187/s.3583
8. Kuendig H, Notari L, Gmel G. Désaccoutumance tabagique en Suisse en 2015 - Analyse des données du Monitorage suisse des addictions. Lausanne, Suisse: Addiction Suisse; 2016.
9. Saba M, Diep J, Saini B, Dhippayom T. Meta-analysis of the effectiveness of smoking cessation interventions in community pharmacy. J Clin Pharm Ther. 2014 Jun;39(3):240–7. doi: https://doi.org/10.1111/jcpt.12131
10. Dent LA, Harris KJ, Noonan CW. Tobacco interventions delivered by pharmacists: a summary and systematic review. Pharmacotherapy. 2007 Jul;27(7):1040–51. doi: https://doi.org/10.1592/phco.27.7.1040
11. Aquilino ML, Farris KB, Zillich AJ, Lowe JB. Smoking-cessation services in Iowa community pharmacies. Pharmacotherapy. 2003 May;23(5):666–73. doi: https://doi.org/10.1592/phco.23.5.666.32192
12. Margolis JA, Meshack AF, McAlister AL, Boye-Doe H, Simpson L, Hu S. Smoking cessation activities by pharmacists in East Texas. J Am Pharm Assoc. 2002;42(3):508–9. doi: https://doi.org/10.1331/108658002763316941
13. El Hajj MS, Al Nakeeb RR, Al-Qudah RA. Smoking cessation counseling in Qatar: community pharmacists’ attitudes, role perceptions and practices. Int J Clin Pharm. 2012 Aug;34(4):667–76. doi: https://doi.org/10.1007/s11096-012-9663-x
14. Hudmon KS, Prokhorov AV, Corelli RL. Tobacco cessation counseling: pharmacists’ opinions and practices. Patient Educ Couns. 2006 Apr;61(1):152–60. doi: https://doi.org/10.1016/j.pec.2005.03.009
15. Müller R, Krebs H. Rauchstoppberatung in schweizerischen Apotheken 2012 - Schriftliche Befragung bei Apothekerinnen und Apothekern sowie bei Pharmaassistenten und -Assistentinnen. Freiburg, Zürich: Nationales Rauchstopp-Programm; 2013.
16. Dey M, Haug S. Rauchstoppberatung durch Gesundheitsfachpersonen in der Schweiz 2016. ISGF Zürich; 2016.
17. Wick M, Ackermann-Liebrich U, Bugnon O, Cerise C. Evaluation der Kampagne “Künftige Nichtraucher” des Schweizerischen Apothekerverbands [Evaluation of the “future non-smokers” campaign of the Swiss Society of Pharmacists]. Soz Praventivmed. 2000;45(2):73–84. doi: https://doi.org/10.1007/BF01624615
18. Gschwend P, Steffen T, Hersberger K, Ackermann-Liebrich U. Raucherentwöhnung in Apotheken — Evaluation der Raucherentwöhnungskampagne “Tabak adieu” der Apotheker/-innen beider Basel [Smoking cessation in pharmacies — evaluation of the smoking cessation campaign “Tobacco adieu!” among pharmacists in Basel]. Soz Praventivmed. 1999;44(1):14–21. doi: https://doi.org/10.1007/BF01624806
19. MedizinalTarif-Kommission. Apotheker-Tarif 2025. Available from: https://www.mtk-ctm.ch/de/tarife/apotheker-tarif/
20. Habfast-Robertson I, Hempel-Bruder C, Guttinger E, Schöni A, Jakob J, Auer R, et al. Sentinella - General practitioner opinions and practices regarding vaping for smoking cessation. Manuscript in preparation. 2021.
21. Veloski J, Tai S, Evans AS, Nash DB. Clinical vignette-based surveys: a tool for assessing physician practice variation. Am J Med Qual. 2005;20(3):151–7. doi: https://doi.org/10.1177/1062860605274520
22. Keller F. Findmind. Available from: https://findmind.ch/
23. Federal Statistical Office of Switzerland. Médecins, cabinets dentaires et pharmacies, évolution de l’effectif 2024. Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/sante/systeme-sante/autres-prestataires.assetdetail.32946331.html
24. PharmaSuisse Schweizerischer Apothekenverband. Heutige Abgabekategorien von Arzneimitteln. 2021.
25. PharmaSuisse Schweizerischer Apothekenverband. Fakten und Zahlen Schweizer Apotheken 2021. 2021.
26. National Institute for Health and Clinical Excellence. Brief interventions and referral for smoking cessation in primary care and other settings. London: National Health Service; 2006.
27. World Health Organisation. WHO clinical treatment guideline for tobacco cessation in adults. Geneva: WHO; 2024.
28. Bauld L, Boyd KA, Briggs AH, Chesterman J, Ferguson J, Judge K, et al. One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services. Nicotine Tob Res. 2011 Feb;13(2):135–45. doi: https://doi.org/10.1093/ntr/ntq222
29. Informationsplattform für Prävention im Praxisalltag (PEPra). Tabak 2025. Available from: https://www.pepra.ch/de/tabak#elektronische-zigaretten
30. Swiss Association for Tobacco Control. Electronic Nicotine Delivery Systems (ENDS) 2022. Available from: https://www.at-schweiz.ch/en/knowledge/products/ends/
31. Lindson N, Butler AR, McRobbie H, Bullen C, Hajek P, Begh R, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2024 Jan;1(1):CD010216.
32. Hiscock R, Goniewicz ML, McEwen A, Murray S, Arnott D, Dockrell M, et al. E-cigarettes: online survey of UK smoking cessation practitioners. Tob Induc Dis. 2014 Aug;12(1):13. doi: https://doi.org/10.1186/1617-9625-12-13
33. Marques Gomes AC, Nabhani-Gebara S, Kayyali R, Buonocore F, Calabrese G. Survey of community pharmacists’ perception of electronic cigarettes in London. BMJ Open. 2016 Nov;6(11):e013214. doi: https://doi.org/10.1136/bmjopen-2016-013214
34. Abrams DB, Glasser AM, Villanti AC, Pearson JL, Rose S, Niaura RS. Managing nicotine without smoke to save lives now: evidence for harm minimization. Prev Med. 2018 Dec;117:88–97. doi: https://doi.org/10.1016/j.ypmed.2018.06.010
35. NICE. Tobacco: preventing uptake, promoting quitting and treating dependence. 2021.
36. Eidgenössische Kommission für Fragen zu Sucht und Prävention nichtübertragbarer Krankheiten (EKSN). Stellungnahme der EKSN im Rahmen der Vernehmlassung zur Änderung des Tabaksteuergesetzes (Besteuerung von elektronischen Zigaretten) - Zusammenfassung. Bern: Schweizerische Eidgenossenschaft; 2022.
37. Roski J, Jeddeloh R, An L, Lando H, Hannan P, Hall C, et al. The impact of financial incentives and a patient registry on preventive care quality: increasing provider adherence to evidence-based smoking cessation practice guidelines. Prev Med. 2003 Mar;36(3):291–9. doi: https://doi.org/10.1016/S0091-7435(02)00052-X
38. Bischof T, Ziegler S, Föhn Z, Di Maio G, Laubereau B. Auslegeordnung Abrechnung von Rauchstoppberatungen in verschiedenen medizinischen und angrenzenden Berufsgruppen. Bericht zuhanden des Tabakpräventionsfonds (TPF). Luzern: Interface Politikstudien Forschung Beratung; 2023.
39. Schweizerischer Apothekerverband (pharmaSuisse). Apotheken stärken: Parlament verabschiedet wegweisende KVG-Revision 2025. Available from: https://pharmasuisse.org/de/medienmitteilung/apotheken-staerken-parlament-verabschiedet-wegweisende-kvg-revision
40. Gautier S, Cloppet A, Mir S, Duville C, Morvillers JM, Simzac AB, et al. Knowledge, attitudes and practices of primary healthcare professionals regarding smoking and smoking cessation among the elderly in France. Tob Prev Cessat. 2023 Oct;9(October):32. doi: https://doi.org/10.18332/tpc/173401
41. Twardella D, Brenner H. Lack of training as a central barrier to the promotion of smoking cessation: a survey among general practitioners in Germany. Eur J Public Health. 2005 Apr;15(2):140–5. doi: https://doi.org/10.1093/eurpub/cki123
42. Mulder F, Löwinger D, Jenkinson SP, Kaiser E, Scharf T, Maire M, et al. Counselling for Chronic Insomnia in Swiss Pharmacies: A Survey Study Based on Case Vignettes. Pharmacy (Basel). 2023 Jun;11(3):105. doi: https://doi.org/10.3390/pharmacy11030105
The supplementary files are available for download https://doi.org/10.57187/s.4344.
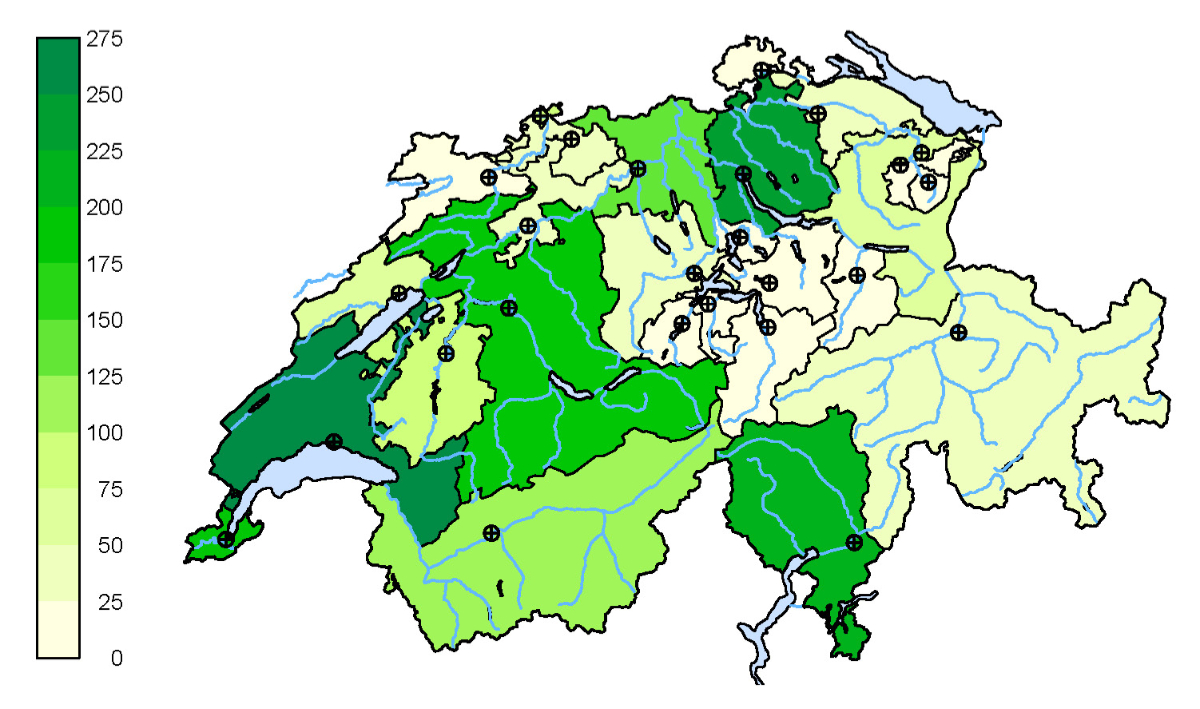
Figure S1Frequencies of community pharmacies in Switzerland (n = 1839). The map plotted in this figure belongs to the Swiss Federal Statistical Office ©. The figure is based on the list of community pharmacies registered on pharmaSuisse website (data extracted on March 1st 2025), excluding pharmacies located in Liechtenstein.