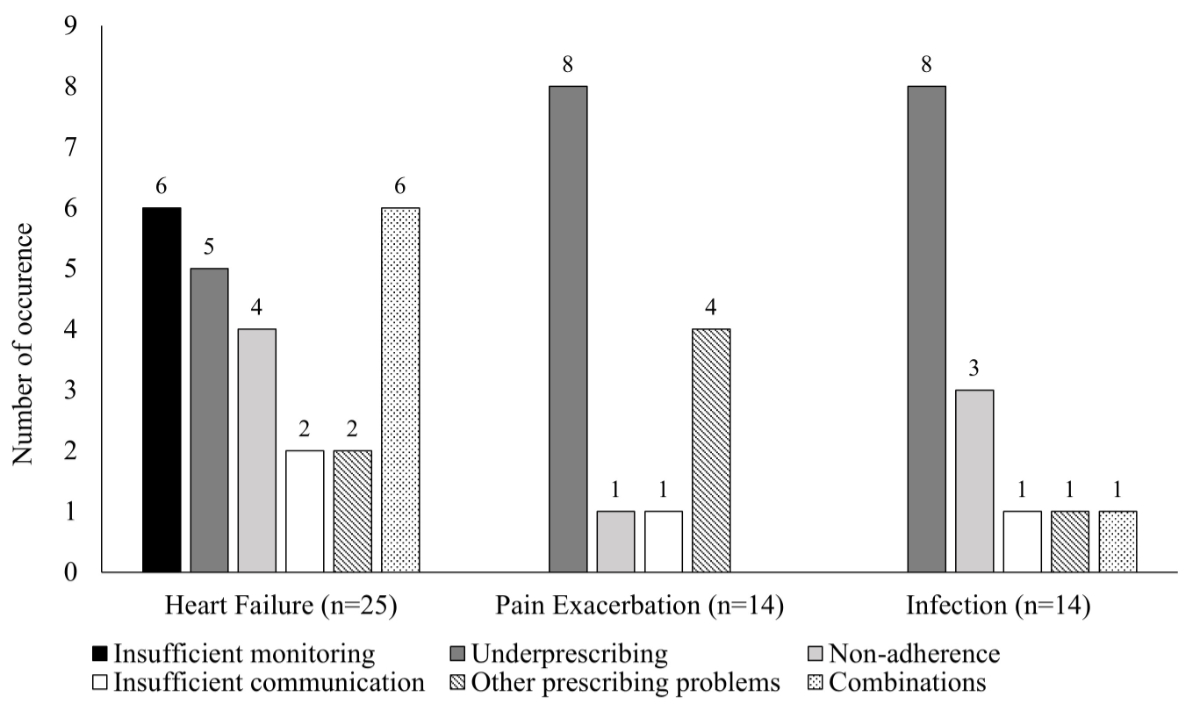
Figure 1Adverse drug events associated with potentially preventable medication-related readmissions involving patients readmitted due to heart failure, worsening pain or infection.
DOI: https://doi.org/https://doi.org/10.57187/s.4259
Medication errors, defined as any mistake occurring in the medication use process, are prevalent in all healthcare contexts, especially at transitions of care [1, 2]. While not all medication errors result in harm, those that do are classified as preventable adverse drug events (ADEs) [3]. In contrast, adverse drug reactions (ADRs), defined as “a response that is noxious and unintended, and which occurs at doses normally used in humans”, are non-preventable adverse drug events [4]. The Institute of Medicine estimates that at least 1.5 million preventable adverse drug events occur each year in the United States. Similarly, studies conducted in Europe also found a high prevalence of preventable adverse drug events [5, 6].
If adverse drug events are severe enough, they can lead to hospitalisations and, if there has been a previous hospitalisation, to medication-related readmissions (MRRs). The prevalence of medication-related readmissions varies by country, the type of patient population, the timeframe for readmissions and, most importantly, the method used to detect medication-related readmissions. Whereas some studies only classify readmissions due to adverse drug reactions as medication-related readmissions [7], others use a more comprehensive method categorising all readmissions as medication-related readmissions if any type of adverse drug event cannot be ruled out as having played a substantial role [8, 9]. In one systematic review, the median prevalence of medication-related readmissions across the 12 studies included was 21%, with a range of 3–64%, and the median rate of preventability was 69% [10]. A more recent meta-analysis of four studies found a pooled prevalence for medication-related readmissions of 9%, with a range of 3–22% [11].
Any type of readmission implies a burden on a patient’s health and the healthcare system’s finances [12, 13]. As a substantial proportion of readmissions involves potentially preventable medication-related readmissions (ppMRRs), their risk factors have been investigated to better understand and mitigate their occurrence. In this study, potentially preventable medication-related readmissions include both adverse drug events (e.g. underprescribing, overprescribing, non-adherence) and systemic issues such as insufficient communication or monitoring. These factors were assessed using predefined criteria. Older adults’ age puts them at a higher risk of medication-related readmissions because they are a population associated with other risk factors for medication-related readmissions, including polypharmacy and the prescription of certain medication groups [14]. Medication classes that have been shown to increase the risk of medication-related readmissions include antidiabetic agents, particularly insulin, antithrombotics and opioids [15–18]. The underlying causes of medication-related readmissions include non-preventable adverse drug reactions and preventable adverse drug events. Adverse drug events predominantly include non-adherence by patients, prescribing problems and transition-of-care errors, such as insufficient communication between different healthcare professionals or institutions [17–19]. Prescribing problems include underprescribing, in which a medication is omitted despite being indicated, and overprescribing, where a medication is prescribed without a valid indication. Other prescribing problems include the prescription of a medication for which the patient does have a valid indication but where the duration, dose or choice of medication is inappropriate. The inappropriateness may be due to drug interactions, contraindications, a suboptimal route of administration or high cost.
In Switzerland, where the healthcare system is decentralised and older adults are often affected by polypharmacy [20], addressing potentially preventable medication-related readmissions poses particular challenges. Moreover, communication across sectors and institutions can be fragmented, increasing the risk of medication-related issues during transitions of care.
In order to introduce targeted measures to prevent medication-related readmissions, the causes of potentially preventable medication-related readmissions need to be better understood. In many countries, including Switzerland, where the present study was conducted, the causes of potentially preventable medication-related readmissions have never been specifically investigated. The present study’s objectives, therefore, were to quantify the prevalence of 30-day potentially preventable medication-related readmissions in older adults discharged from a general internal medicine department of a university hospital in Switzerland and readmitted to the same hospital, and to analyse their underlying causes.
We analysed 30-day readmissions for their medication-relatedness and preventability in a retrospective observational cohort study comprising the data of 500 randomly selected patients hospitalised in the general internal medicine department of the University Hospital of Bern. All had been discharged between 1 January 2022 and 18 October 2023 and readmitted to a department in the same hospital within 30 days. The random selection was performed by assigning a random number to each patient in an Excel (2016 version, Microsoft, Redmond, WA, USA) spreadsheet using its RAND() function. Patients were then sorted into ascending order, and the 500 patients with the lowest random numbers were included in the analysis. No patients were excluded due to incomplete records, and the random selection was applied to all eligible cases. Study eligibility required patients to be at least 65 years old and to have given general consent to the further use of their data. No other inclusion or exclusion criteria were used.
The present study was reviewed by the Cantonal Ethics Committee of Bern, and its need for approval was waived as it was classified as a quality improvement project (submission number 2023-01025).
The primary study outcome were 30-day potentially preventable medication-related readmissions. The patient and case identifiers (unique numbers assigned to every patient at hospital admission) of our 500 readmissions were extracted to enable full access to the electronic health records of their index hospitalisation and readmission. Data were also automatically extracted on each patient’s medications prescribed at discharge, age, sex, number of hospitalisations in the year before their index hospitalisation, index hospitalisation length of stay, number of days before readmission, number of diagnoses and primary language documented in the electronic health record. Descriptive summaries of patient and case characteristics are given in tables 1 and 2, respectively.
In step one, two clinical pharmacists (CMM and NS) independently screened readmissions for medication relatedness. This was done using the validated AT-HARM10 instrument for classifying older adult admissions as potentially medication-related or unlikely to be medication-related [21]. The tool comprises ten closed-ended questions, three of which are used to identify admissions that are unlikely medication-related and seven of which are used to identify admissions that are possibly medication-related. It is designed so that once the answer to a question is “yes”, the assessment can be terminated and the admission categorised. The complete tool, with all its questions, is provided in appendix 1. In the original validation study, the AT-HARM10 tool showed a sensitivity of 70–86%, a specificity of 70–74% and an interrater agreement (Cohen’s κ) of 0.45–0.75 [21]. The average time required per case was 5.7 minutes [21]. The AT-HARM10 tool was chosen because it is validated for identifying medication-related hospital admissions in older adults. Compared to other tools, it shows similar performance while requiring less time to complete, making it particularly suitable for this study [21]. In step two, preventability was assessed for each readmission categorised as medication-related. We assessed preventability using judgements similar to the Schumock statements (i.e. inappropriate prescribing due to medication choice or dosage, inappropriate monitoring, interactions, poor adherence, contraindication, etc) [22]. While the tool has not been formally validated in the same way as AT-HARM10, its reliability has been assessed in several studies. For example, a multicentre observational study reported a Cronbach’s alpha of 0.76, indicating good internal consistency [23]. In step three, the two pharmacists discussed every readmission, comparing their findings. In cases of disagreement, an experienced physician (TB) screened the readmission concerned using the same approach. All three investigators then discussed that readmission until a consensus was reached. The physician assessed 57 (11%) readmissions; the others were reviewed by the pharmacists alone. All three investigators jointly assessed a pilot sample of 20 (4%) readmissions to harmonise their approach and confirm the feasibility of the assessment process. Preventability and medication-relatedness were assessed solely based on information explicitly documented in the electronic health records. Missing information, for example regarding medication intake or adherence, was acknowledged as a limitation of the retrospective study design.
After completing the chart reviews, we extracted the reasons for readmission, the underlying adverse drug event (i.e. underprescribing, overprescribing, Other prescribing problems, non-adherence, insufficient communication) and the medications involved; we then analysed the automatically extracted data. Medications involved in each potentially preventable medication-related readmission were identified during chart reviews based on clinical judgement. Medication classes were not pre-defined but were grouped into broader categories during analysis to detect common patterns.
We identified 116 (23.2%) potentially preventable medication-related readmissions among the 500 30-day readmissions screened. The baseline characteristics of the patients with a potentially preventable medication-related readmission are shown in table 1.
Table 1Baseline characteristics of patients with a 30-day potentially preventable medication-related readmission.
| Characteristics | 30-day potentially preventable medication-related readmissions (n = 116) | |
| Age, median (IQR) [years] | 78.0 (70.0–84.0) | |
| Sex, n (%) | Male | 66 (56.9%) |
| Female | 50 (43.1%) | |
| Primary language, n (%) | German | 102 (87.9%) |
| French | 3 (2.6%) | |
| Italian | 3 (2.6%) | |
| Other | 8 (6.9%) | |
| Time to readmission, median (IQR) [days] | 10.0 (4.0–18.3) | |
| Number of hospitalisations (same hospital) in the 12 months before the index admission, median (IQR) | 2.0 (1.0–3.0) | |
| Length of stay of the index hospital admission, median (IQR) [days] | 5.0 (3.0–8.0) | |
| Number of medications at discharge from the index admission, median (IQR) | 12.0 (8.0–15.0) | |
| Number of ICD-10 codes at discharge from the index admission, median (IQR) | 17.0 (13.0–21.0) | |
The most common diagnoses among readmitted patients and the underlying reason for their adverse drug events are summarised in table 2. The most common readmission diagnoses were heart failure, worsening pain and infection. Figure 1 illustrates the underlying reasons associated with these three prevalent diagnoses.
Table 2Readmission diagnoses of patients who experienced a potentially preventable medication-related readmission and the reasons for their adverse drug events.
| Diagnoses of potentially preventable readmissions | Underlying reason for the adverse drug event |
| Heart failure (n = 25, 21.6%) | Insufficient monitoring (n = 6, 24.0%) |
| Underprescribing (n = 5, 20.0%) | |
| Non-adherence (n = 4, 16.0%) | |
| Insufficient communication (n = 2, 8.0%) | |
| Other prescribing problems (n = 2, 8.0%): 1 underdose, 1 interaction | |
| A combination of the above (n = 6, 24.0%) | |
| Worsening pain (n = 14, 12.1%) | Underprescribing (n = 8, 57.1%) |
| Other prescribing problems (n = 4, 28.6%): 4 underdoses | |
| Non-adherence (n = 1, 7.1%) | |
| Insufficient communication (n = 1, 7.1%) | |
| Infection (n = 14, 12.1%) | Underprescribing (n = 8, 57.1%) |
| Non-adherence (n = 3, 21.4%) | |
| Insufficient communication (n = 1, 7.1%) | |
| Other prescribing problems (n = 1, 7.1%): 1 wrong duration | |
| A combination of the above (n = 1, 7.1%) | |
| Worsening COPD (n = 6, 5.2%) | Underprescribing (n = 5, 83.3%) |
| Other prescribing problems (n = 1, 16.7%): 1 suboptimal medication selection | |
| Obstipation (n = 6, 5.2%) | Non-adherence (n = 3, 50.0%) |
| Other prescribing problems (n = 2, 33.3%): 1 underdose, 1 suboptimal medication selection | |
| Underprescribing (n = 1, 16.7%) | |
| Fall (n = 6, 5.2%) | Other prescribing problems (n = 3, 50.0%): 1 overdose, 1 contraindication, 1 suboptimal medication selection |
| Overprescribing (n = 2, 33.3%) | |
| Insufficient communication (n = 1, 16.7%) | |
| Acute kidney injury (n = 4, 3.4%) | Other prescribing problems (n = 3, 75.0%): 1 overdose, 1 interaction, 1 contraindication |
| Insufficient monitoring (n = 1, 25.0%) | |
| Delirium (n = 3, 2.6%) | Other prescribing problems (n = 2, 66.7%): 2 suboptimal medication selections |
| Overprescribing (n = 1, 33.3%) | |
| Hypotension (n = 3, 2.6%) | Other prescribing problems (n = 3, 100.0%): 1 overdose, 1 suboptimal medication selection, 1 contraindication |
| Ischaemic stroke (n = 3, 2.6%) | Underprescribing (n = 2, 66.7%) |
| Other prescribing problems (n = 1, 33.3%): 1 underdose | |
| Others (n = 32, 27.6%) | Other prescribing problems (n = 12, 37.5%): 3 suboptimal medication selections, 3 overdoses, 2 contraindications, 2 underdoses, 1 suboptimal dosage form, 1 suboptimal dosing regimen |
| Underprescribing (n = 6, 18.8%) | |
| Non-adherence (n = 4, 12.5%) | |
| Insufficient communication (n = 2, 6.3%) | |
| Insufficient monitoring (n = 2, 6.3%) | |
| Overprescribing (n = 1, 3.1%) | |
| A combination of the above (n = 5, 15.6%) |
COPD: chronic obstructive pulmonary disease.
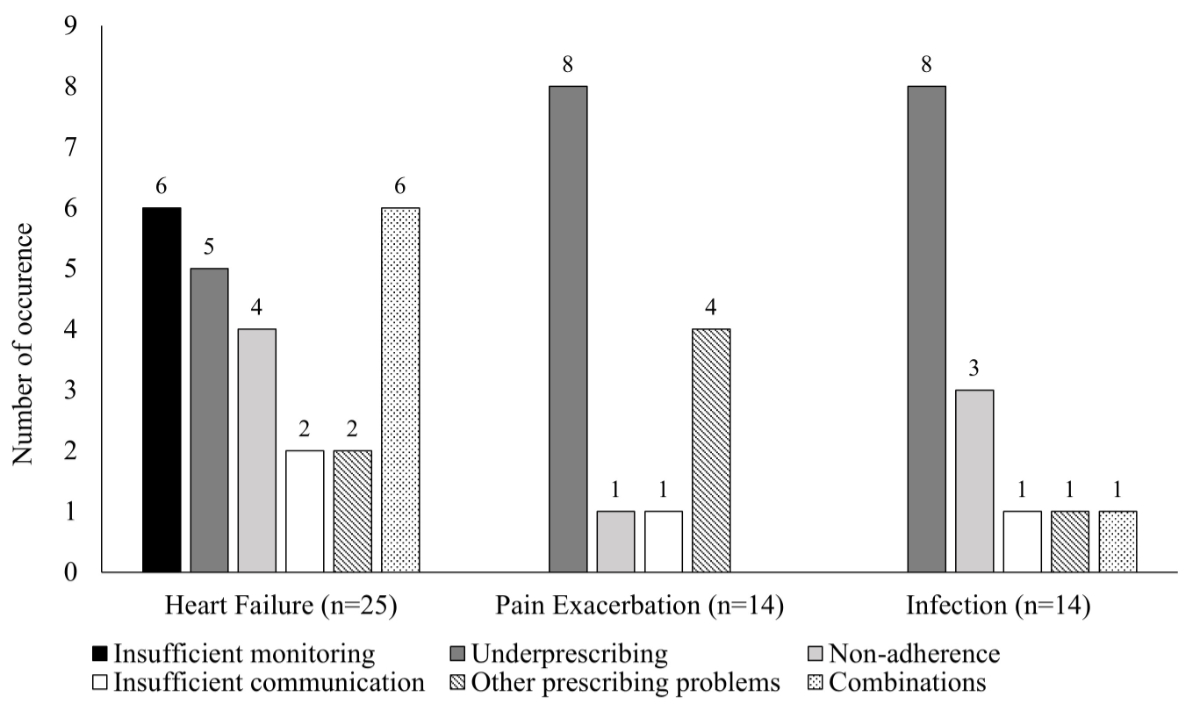
Figure 1Adverse drug events associated with potentially preventable medication-related readmissions involving patients readmitted due to heart failure, worsening pain or infection.
Across all the diagnoses, the most commonly encountered reasons for adverse drug events were underprescribing (n = 34, 29.3%), Other prescribing problems (n = 33, 28.4%), non-adherence (n = 15, 12.9%), insufficient monitoring (n = 9, 7.8%), insufficient communication (n = 7, 6.0%) and overprescribing (n = 5, 4.3%). Combinations of different adverse drug events were found in 13 (11.2%) potentially preventable medication-related readmissions.
When looking at potentially preventable medication-related readmissions where a single medication was involved, diuretics (n = 17, 17.0%), analgesics (n = 16, 16.0%), antibiotics (n = 11, 11.0%), anticoagulants (n = 7, 7.0%), inhalants (n = 6, 6.0%) and laxatives (n = 6, 6.0%) were the most frequently encountered. The most frequently observed combination of medication class and reason for readmission included insufficient monitoring for diuretics, underprescribing for analgesics, antibiotics, anticoagulants and inhalants, and non-adherence for laxatives. More than one drug was involved in 16 cases (13.8%).
This retrospective cohort study provided valuable insights into 30-day potentially preventable medication-related readmissions. Our findings suggested that a substantial proportion (23.2%) of general internal medicine patients readmitted within 30 days had experienced a potentially preventable medication-related readmission. The most common readmission diagnoses were heart failure, worsening pain and infection, with underprescribing, Other prescribing problems (excluding overprescribing) and non-adherence being the most common reasons for adverse drug events. These findings suggested that improved medication management for older adult patients is critical. This need was further emphasised by a systematic literature review conducted by the World Health Organization, which found that 17% of older adult patients experience preventable medication-related harm [24]. Furthermore, that review found that 53% of all preventable medication-related harm occurs during the ordering or prescribing stage, which also aligned with our findings [24].
Our results aligned with prior research showing that medication-related issues were important drivers of readmissions [8, 18, 19, 25–28]. However, the exact rates of potentially preventable medication-related readmissions found vary greatly, depending especially on the patient populations and methods used to detect medication-relatedness and preventability. A similar study by Dalleur et al. found that 13.1% of 30-day potentially preventable readmissions were medication-related [19]. It remains unclear why there were significantly fewer potentially preventable medication-related readmissions in their study, but it could be because of the high proportion of cancer patients in their population. Although chemotherapies carry an inherently high risk of adverse drug reactions and cancer patients are often readmitted, preventability is often not recorded. This can be seen in our results, where cancer was never the primary reason for readmission. Another study found similar results to ours, with potentially preventable medication-related readmissions being involved in 26% of readmissions [26]. Glans et al. also used the AT-HARM10 tool with older adult patients and found that 40% of all readmissions were medication-related, although their preventability was not assessed [25]. Given the median preventability rate found in the systematic review by El Morabet et al., however, they probably would have found similar results to our study [10]. Other studies have found lower rates of potentially preventable medication-related readmissions. For example, Uitvlugt et al. found that 16% of readmissions were medication-related readmissions and 40% of them were preventable [18]. This lower percentage could be because medication-related readmissions were only considered in this analysis if an adverse drug reaction was present. As the most prevalent issue identified in our study was underprescribing, it is unsurprising that a higher prevalence of potentially preventable medication-related readmissions was found too. Two large randomised controlled trials have found the overall prevalence of medication-related readmissions within one year of discharge to be approximately 22% [8, 28]. Direct comparison with these two studies is difficult, however, as their readmission timeframe was different and they did not give rates of medication-related readmissions for all readmissions. They nevertheless also illustrated that medication-related readmissions are a pertinent topic.
The prescribing problems that we identified, such as underprescribing, Other prescribing problems and overprescribing, are not unique to Switzerland’s healthcare system but reflect global concerns, especially for older adults. Underprescribing, for instance, has been well-documented as a significant issue in older populations due to concerns about polypharmacy and adverse drug reactions [29, 30]. However, this can often lead to suboptimal management of their chronic conditions, including heart failure, hypertension and pain, as our study revealed. Similarly, Other prescribing problems, where medication selection or dosing is inappropriate, are important issues and common problems for older adults [31, 32]. Notably, the inappropriate prescribing of analgesics and diuretics identified in our study aligns with findings from similar ones where these medication classes were frequently involved in adverse drug events that lead to readmissions [19, 27]. Opioids were also included in the PAR-Risk Score, a prediction model developed in Switzerland to flag patients at high risk of potentially preventable all-cause readmissions [33]. Medication non-adherence was another common reason for potentially preventable medication-related readmissions in our study and aligns well with previous research identifying non-adherence as a major risk factor for medication-related readmissions [18, 19, 27]. Non-adherence is frequently encountered in clinical practice and may be either intentional or unintentional [34, 35]. Studies have shown that patients with heart failure exhibit particularly high rates of non-adherence [36], which overlaps with our findings.
Our findings suggested that improving prescription practices and patient adherence, especially during transitions of care, may help mitigate the risk of potentially preventable medication-related readmissions. Previous studies have demonstrated that interventions to optimise prescription practices, such as medication reconciliation and comprehensive medication reviews, can effectively reduce readmission rates [37, 38] and medication-related readmissions [39]. Similarly, enhanced patient education programmes focusing on adherence have shown promise in minimising readmissions [40, 41]. Improvements in transitions of care, including better communication between healthcare professionals, particularly regarding medication changes and the need for follow-up assessments or intensified monitoring, have also been associated with reductions in readmissions [42]. Given that the median time to readmission was only 10 days in our study, it seems plausible that transitional care and additional interventions shortly after discharge could be particularly relevant. Evidence of the effectiveness of these interventions remains inconsistent. The reasons for this inconsistency are not fully understood, though we hypothesise that interventions may not have been implemented using multimodal approaches that combined different interventions. More holistic approaches could be beneficial. A meta-analysis of randomised controlled trials by Dutzenberg et al. demonstrated that while medication reviews alone did not reduce readmissions, combining them with other interventions, such as medication reconciliation or patient education, significantly reduced readmission rates [43]. In contexts involving limited healthcare resources, however, providing comprehensive approaches for every patient may not always be feasible. In Switzerland, the availability of clinical pharmacists or coordinated follow-up care after discharge is often limited [44], which may further reduce the feasibility of implementing comprehensive interventions for all patients. Therefore, further research is needed to determine which interventions are most effective at reducing the risk of potentially preventable medication-related readmissions and to identify the patients most likely to benefit. This targeted approach could help optimise resource allocation while maximising patient outcomes. In addition, factors such as patients’ socioeconomic situation, cognitive function or the availability of social support may also influence the occurrence of potentially preventable medication-related readmissions. These aspects were not captured in our dataset but should be considered when designing future interventions.
The present study had several strengths. First, it is one of the few studies to have focused specifically on potentially preventable medication-related readmissions in an older adult population, and it was the first conducted in a hospital in Switzerland. By using a robust, validated tool (AT-HARM10) for identifying medication-related readmissions, we ensured a structured and reliable classification process. Using independent reviews by pharmacists and involving a physician in cases of disagreement strengthened the validity of our findings. Additionally, including a large, randomly selected cohort of 500 patients enhanced the generalisability of our results to similar clinical populations.
The study had some limitations, nevertheless. Using a retrospective cohort made the study dependent on the accuracy and completeness of electronic health records, which may not fully capture critical aspects such as medication adherence or nuances of patient behaviour. Non-adherence was assessed based on explicit documentation in the medical record, but such information was not consistently available. As a result, some cases of non-adherence may have gone undocumented and thus unrecognised, potentially leading to an underestimation of its contribution to potentially preventable medication-related readmissions. Additionally, the reasoning behind certain ambulatory care decisions or interventions could not always be extracted from the records, potentially limiting our understanding of medication-relatedness or preventability. For example, while we relied on the medication history documented upon readmission, changes made by general practitioners after discharge may have occurred without being systematically recorded. Although random sampling was applied to all eligible patients, we cannot fully exclude the possibility of subtle selection bias, for example due to variations in documentation quality. The study was conducted at a single institution, which may restrict the generalisability of the findings to other healthcare settings. Another limitation was that we could only track readmissions to the same hospital institution, potentially underestimating the true rate of readmissions. Finally, although the AT-HARM10 tool provided a structured approach to identifying medication-related readmissions, it may not fully capture more complex or nuanced cases. Both the identification of medication-related readmissions and the assessment of their preventability retain an element of subjectivity despite the rigorous review process employed.
In this retrospective cohort study, we found that 23.2% of 30-day readmissions among older adults were medication-related and potentially preventable, with underprescribing, Other prescribing problems (like suboptimal medication selection or dosing issues) and non-adherence being the most common causes. The medications most commonly involved were diuretics, analgesics and antibiotics, whereas the most common readmission diagnoses were heart failure, worsening pain and infection. Due to the multifactorial nature of potentially preventable medication-related readmissions, multimodal and interdisciplinary strategies are likely required to effectively reduce these events. Given that the median time to readmission was only 10 days, timely post-discharge interventions may be particularly relevant to prevent such events. Although interventions such as medication reviews, medication reconciliation at discharge and improved care transitions might have prevented these readmissions, their effectiveness remains inconsistent across the scientific literature. Targeted efforts to reduce potentially preventable medication-related readmissions are urgently needed. Further research should focus on identifying the most effective strategies and determining which patient subgroups are most at risk of preventable medication-related readmissions. This will enable the more targeted and efficient use of healthcare resources.
Due to ethics regulations, the non-anonymised data cannot be made publicly available. Access to more detailed aggregated data may be granted by the authors upon reasonable request.
Authors’ contributions: NS, CMM, TB and BH developed the research plan. NS, CMM and TB conducted the readmission reviews. LW performed the statistical analyses. NS drafted the manuscript, and all authors reviewed and approved the final version. NS and CMM submitted the grant proposal to Smarter Medicine – Choosing Wisely Switzerland.
This project was supported by a research grant from Smarter Medicine – Choosing Wisely Switzerland. The funding body had no role in designing the study, collecting data, analysing and interpreting results, or preparing the manuscript.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Institute of Medicine. Preventing Medication Errors. Washington (DC): The National Academies Press; 2007.
2. Foulon V, Wuyts J, Desplenter F, Spinewine A, Lacour V, Paulus D, et al. Problems in continuity of medication management upon transition between primary and secondary care: patients’ and professionals’ experiences. Acta Clin Belg. 2019 Aug;74(4):263–71.
3. Gandhi TK, Seger DL, Bates DW. Identifying drug safety issues: from research to practice. Int J Qual Health Care. 2000 Feb;12(1):69–76.
4. World Health Organization. International drug monitoring: the role of national centres. Report of a WHO meeting. Geneva; 1972.
5. Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2021 Feb;30(2):96–105.
6. Sell R, Schaefer M. Prevalence and risk factors of drug-related problems identified in pharmacy-based medication reviews. Int J Clin Pharm. 2020 Apr;42(2):588–97.
7. Banholzer S, Dunkelmann L, Haschke M, Derungs A, Exadaktylos A, Krähenbühl S, et al. Retrospective analysis of adverse drug reactions leading to short-term emergency hospital readmission. Swiss Med Wkly. 2021 Jan;151(304):w20400.
8. Blum MR, Sallevelt BT, Spinewine A, O’Mahony D, Moutzouri E, Feller M, et al. Optimizing Therapy to Prevent Avoidable Hospital Admissions in Multimorbid Older Adults (OPERAM): cluster randomised controlled trial. BMJ. 2021 Jul;374(1585):n1585.
9. Kempen TGH, Bertilsson M, Hadziosmanovic N, Lindner K-J, Melhus H, Nielsen EI, et al. Effects of Hospital-Based Comprehensive Medication Reviews Including Postdischarge Follow-up on Older Patients’ Use of Health Care: A Cluster Randomized Clinical Trial. JAMA Netw Open. 2021;4(4):e216303-e. doi: .
10. El Morabet N, Uitvlugt EB, van den Bemt BJ, van den Bemt PM, Janssen MJ, Karapinar-Çarkit F. Prevalence and Preventability of Drug-Related Hospital Readmissions: A Systematic Review. J Am Geriatr Soc. 2018 Mar;66(3):602–8.
11. Prasad N, Lau EC, Wojt I, Penm J, Dai Z, Tan EC. Prevalence of and Risk Factors for Drug-Related Readmissions in Older Adults: A Systematic Review and Meta-Analysis. Drugs Aging. 2024 Jan;41(1):1–11.
12. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr;360(14):1418–28.
13. Kum Ghabowen I, Epane JP, Shen JJ, Goodman X, Ramamonjiarivelo Z, Zengul FD. Systematic Review and Meta-Analysis of the Financial Impact of 30-Day Readmissions for Selected Medical Conditions: A Focus on Hospital Quality Performance. Healthcare (Basel). 2024 Mar;12(7):750.
14. Schönenberger N, Meyer-Massetti C. Risk factors for medication-related short-term readmissions in adults - a scoping review. BMC Health Serv Res. 2023 Sep;23(1):1037.
15. Cooper JB, Jeter E, Sessoms CJ. Rates and Types of Medication-Related Problems in Patients Rehospitalized Within 30 Days of Discharge From a Community Hospital. J Pharm Technol. 2020 Apr;36(2):47–53.
16. Ekerstad N, Bylin K, Karlson BW. Early rehospitalizations of frail elderly patients - the role of medications: a clinical, prospective, observational trial. Drug Healthc Patient Saf. 2017 Aug;9:77–88. doi: https://doi.org/10.2147/DHPS.S139237
17. Rothwell M, Jukka C, Lum E, Mitchell C, Kyriakides P. Retrospective Analysis of Emergency Readmissions to Rural and Regional Hospitals. J Pharm Pract Res. 2011;41(4):290–4.
18. Uitvlugt EB, Janssen MJ, Siegert CE, Kneepkens EL, van den Bemt BJ, van den Bemt PM, et al. Medication-Related Hospital Readmissions Within 30 Days of Discharge: Prevalence, Preventability, Type of Medication Errors and Risk Factors. Front Pharmacol. 2021 Apr;12:567424.
19. Dalleur O, Beeler PE, Schnipper JL, Donzé J. 30-Day Potentially Avoidable Readmissions Due to Adverse Drug Events. J Patient Saf. 2021 Aug;17(5):e379–86. doi: https://doi.org/10.1097/PTS.0000000000000346
20. Twerenbold S, Schur N, Wittwer N, Schneider C, Marxer C, Spöndlin J, et al. Helsana-Arzneimittelreport für die Schweiz 2022. Auswertungsergebnisse der Helsana Arzneimitteldaten aus den Jahren 2018 bis 2021. Zürich: Helsana-Gruppe; 2022.
21. Kempen TG, Hedström M, Olsson H, Johansson A, Ottosson S, Al-Sammak Y, et al. Assessment tool for hospital admissions related to medications: development and validation in older patients. Int J Clin Pharm. 2019 Feb;41(1):198–206.
22. Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hosp Pharm. 1992 Jun;27(6):538.
23. Iftikhar S, Sarwar MR, Saqib A, Sarfraz M. Causality and preventability assessment of adverse drug reactions and adverse drug events of antibiotics among hospitalized patients: A multicenter, cross-sectional study in Lahore, Pakistan. PLoS One. 2018 Jun;13(6):e0199456.
24. World Health Organization. Global burden of preventable medication-related harm in health care: a systematic review. Geneva; 2023.
25. Glans M, Kragh Ekstam A, Jakobsson U, Bondesson Å, Midlöv P. Medication-related hospital readmissions within 30 days of discharge-A retrospective study of risk factors in older adults. PLoS One. 2021 Jun;16(6):e0253024.
26. Pellegrin KL, Lee E, Uyeno R, Ayson C, Goo R. Potentially preventable medication-related hospitalizations: A clinical pharmacist approach to assessment, categorization, and quality improvement. J Am Pharm Assoc (Wash DC). 2017;57(6):711–6.
27. Whitaker AS, Cottrell WN. What proportion of unplanned re-presentations to an emergency department are medication related and preventable? J Pharm Pract Res. 2019;49(6):546–56.
28. Kempen TG, Hedman AN, Hadziosmanovic N, Lindner KJ, Melhus H, Nielsen EI, et al. Risk factors for and preventability of drug-related hospital revisits in older patients: A post-hoc analysis of a randomized clinical trial. Br J Clin Pharmacol. 2023 May;89(5):1575–87.
29. Lombardi F, Paoletti L, Carrieri B, Dell’Aquila G, Fedecostante M, Di Muzio M, et al. Underprescription of medications in older adults: causes, consequences and solutions-a narrative review. Eur Geriatr Med. 2021 Jun;12(3):453–62.
30. Cherubini A, Corsonello A, Lattanzio F. Underprescription of beneficial medicines in older people: causes, consequences and prevention. Drugs Aging. 2012 Jun;29(6):463–75.
31. Schietzel S, Zechmann S, Rachamin Y, Neuner-Jehle S, Senn O, Grischott T. Potentially Inappropriate Medication Use in Primary Care in Switzerland. JAMA Network Open. 2024;7(6):e2417988-e. doi: .
32. Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007 Apr;32(2):113–21.
33. Blanc AL, Fumeaux T, Stirnemann J, Dupuis Lozeron E, Ourhamoune A, Desmeules J, et al. Development of a predictive score for potentially avoidable hospital readmissions for general internal medicine patients. PLoS One. 2019 Jul;14(7):e0219348.
34. Hugtenburg JG, Timmers L, Elders PJ, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: a challenge for tailored interventions. Patient Prefer Adherence. 2013 Jul;7:675–82. doi: https://doi.org/10.2147/PPA.S29549
35. Frankl SE, Breeling JL, Goldman L. Preventability of emergent hospital readmission. Am J Med. 1991 Jun;90(6):667–74. doi: https://doi.org/10.1016/S0002-9343(05)80053-1
36. Ruppar TM, Delgado JM, Temple J. Medication adherence interventions for heart failure patients: A meta-analysis. Eur J Cardiovasc Nurs. 2015 Oct;14(5):395–404.
37. Wood D, Moy SF, Zhang S, Lightfoot N. Impact of a prescriber and patient educational intervention on discharge analgesia prescribing and hospital readmission rates following elective unilateral total hip and knee arthroplasty. BMJ Open Qual. 2022 Aug;11(3):e001672.
38. Mekonnen AB, McLachlan AJ, Brien JA. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016 Feb;6(2):e010003.
39. Renaudin P, Boyer L, Esteve MA, Bertault-Peres P, Auquier P, Honore S. Do pharmacist-led medication reviews in hospitals help reduce hospital readmissions? A systematic review and meta-analysis. Br J Clin Pharmacol. 2016 Dec;82(6):1660–73.
40. Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar-Jacob JM. Medication Adherence Interventions Improve Heart Failure Mortality and Readmission Rates: Systematic Review and Meta-Analysis of Controlled Trials. J Am Heart Assoc. 2016 Jun;5(6):e002606.
41. Zemaitis CT, Morris G, Cabie M, Abdelghany O, Lee L. Reducing Readmission at an Academic Medical Center: Results of a Pharmacy-Facilitated Discharge Counseling and Medication Reconciliation Program. Hosp Pharm. 2016 Jun;51(6):468–73.
42. March KL, Peters MJ, Finch CK, Roberts LA, McLean KM, Covert AM, et al. Pharmacist Transition-of-Care Services Improve Patient Satisfaction and Decrease Hospital Readmissions. J Pharm Pract. 2022 Feb;35(1):86–93.
43. Dautzenberg L, Bretagne L, Koek HL, Tsokani S, Zevgiti S, Rodondi N, et al. Medication review interventions to reduce hospital readmissions in older people. J Am Geriatr Soc. 2021 Jun;69(6):1646–58.
44. Studer H, Boeni F, Messerli M, Hersberger KE, Lampert ML. Clinical Pharmacy Activities in Swiss Hospitals: How Have They Evolved from 2013 to 2017? Pharmacy (Basel). 2020 Feb;8(1):19.
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4259.