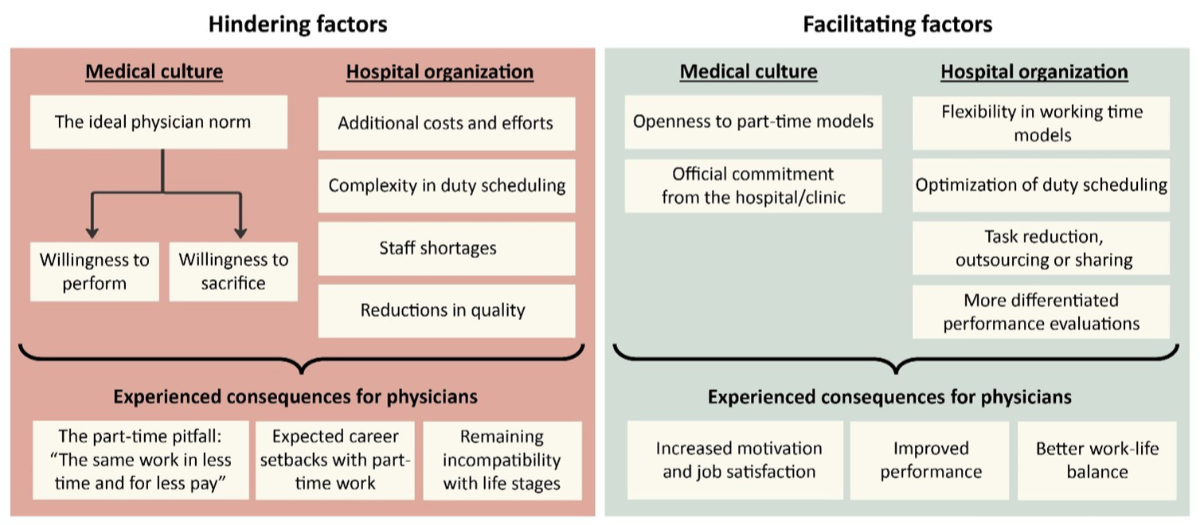
Figure 1Hindering and facilitating factors for the implementation of part-time working for physicians.
DOI: https://doi.org/https://doi.org/10.57187/s.4205
The current demographic shift has resulted in a significant increase in the demand for qualified physicians [1, 2]. This has rendered Switzerland reliant on international practitioners, posing a serious threat to the longevity and sustainability of its healthcare infrastructure [1, 2]. Consequently, there is an urgent need for more individuals to pursue careers in medicine and for strategies to retain professionals within this field.
The most frequent factors associated with the intention to leave the medical profession include work-life conflicts and a high workload [3, 4]. According to Hämmig [5], almost 70% of physicians in Switzerland experience a high work-life imbalance. The difficulties that Swiss physicians encounter in balancing their work and personal lives have been linked to several adverse outcomes, including reduced wellbeing and health problems, particularly burnout symptoms, and decreased job satisfaction [4–8]. Especially in hospital settings, where round-the-clock operations require physicians to work various shifts and overtime, their work-life balance is challenged [4, 9].
To address these work-life conflicts, there are ongoing discussions in Switzerland about reducing the full-time working hours, for example by implementing a 42-hour work week with an additional four hours dedicated to structured further education [10]. However, these systemic changes have yet to be widely implemented, leaving individual-level adjustments as the primary recourse: Part-time employment, defined as a workload below 90%, emerges as a key strategy to address work-life conflicts [11, 12]. Although part-time work has long been discussed as a solution to mitigate work-life conflicts [13], the average workload of hospital physicians has decreased only marginally since 2014, from 94.2% to 93.9% in 2023, whereas a 100% workload equates to 50 hours per week, not including potential overtime [14]. Currently, 25% of Swiss hospital physicians work part-time [14].
Due to round-the-clock operations, various shifts and unforeseeable circumstances (e.g. treatment complications, new patients), organising part-time work in a hospital setting is perceived as particularly challenging [15–17]. Moreover, cultural factors, such as lack of acceptance of part-time work models, also present challenges to the implementation of part-time work [15, 18, 19]. At the individual level, limited career advancement opportunities and high time constraints [16, 20–22], as well as negative attitudes from colleagues [16, 18, 20] are discussed as consequences experienced by physicians.
To date, the specific factors that hinder or facilitate part-time work among hospital physicians at different organisational levels and in different clinical settings remain understudied. Additionally, it is unclear to what extent Swiss hospital physicians desire part-time work, perceive it as feasible, or what their general attitudes towards such options are. This study aims to explore the attitudes of hospital physicians towards part-time work and the barriers and facilitators to its implementation through an exploratory mixed-methods approach. The objective is to propose solutions that can effectively meet the needs of both hospitals and physicians without significant adverse consequences.
To address the research objective, a convergent mixed-methods approach was used, integrating both qualitative and quantitative methods. This combination enables a comprehensive evaluation of the research question from multiple perspectives. The qualitative approach provides in-depth insights into physicians’ attitudes and experiences with part-time employment, while the quantitative approach facilitates generalisation of the findings to a broader population and identification of group differences.
Both the qualitative and quantitative studies were approved after ethical review by the FHNW School of Applied Psychology Ethics Committee (reference number: EAaFE230623).
The data collection was conducted in seven hospital organisations in the German-speaking part of Switzerland, including one bilingual (French and German) hospital, as part of an applied research project by the FHNW School of Applied Psychology. The project’s objective is to establish preventive measures to improve work organisation in Swiss hospitals, with the goal of aligning medical careers to life stage-specific requirements of employees. Participants were informed that the study was part of this project. The study was conducted by academic staff of the FHNW. The research team received training in both qualitative and quantitative methods as part of their academic education (all authors have an MSc in Psychology, one a PhD) and have participated in several research projects.
Participants were recruited by HR specialists of the participating hospitals, with the project leads instructing them to select two to three physicians from different functional levels. HR specialists were also asked to include individuals with diverse perspectives (maximum variation sampling), such as critical views or specific experiences (e.g. job-sharing). Participation was voluntary, and written consent for participation and data use was obtained. One participant did not return the signed consent form and was therefore excluded. The second author (JF) contacted participants via e-mail and conducted the interviews online via MS Teams. A total of 11 female physicians (58%) and 8 male physicians (42%) were interviewed between 17 August and 8 November 2023. The sample included resident physicians (n = 5), attending physicians (n = 6), senior attending physicians (n = 5) and chief physicians (n = 3).
Interviews were guided by a semi-structured question guide covering, among other things, physicians’ attitudes towards part-time work as well as challenges and facilitating factors associated with it. The question guide was developed collaboratively by the research team (JF, AS, JK) and pre-tested with a physician. The interviews, which lasted an average of 51 minutes, were recorded via MS Teams and transcribed with the assistance of Töggl.
The data were analysed using an inductive reflexive thematic analysis, following the six-phase process outlined by Braun and Clarke [23]. Inductive reflexive thematic analysis was chosen as an evaluation method that enables an in-depth exploration of participants’ experiences without predefined theoretical constraints, while also ensuring a clear and systematic analytical process [23]. Initially, three authors (JK, BG, JF) familiarised themselves with the data. JK led the generation of codes and construction of themes, using the software MAXQDA. The other researchers (BG, JF) carefully reviewed and refined these preliminary themes. This iterative process continued with all researchers making further adjustments after collaborative discussions, leading to the final analysis. The final study report was reviewed by all authors.
An e-mail containing a link to an online questionnaire was sent to participants via the Human Resources department, with a voluntary request to complete it. The survey period varied depending on the hospital, spanning from 4 September to 12 November, with individual survey durations ranging from 26 to 48 days. In six of the seven hospitals, reminders to complete the survey were sent 8 to 23 days after the initial distribution. In five hospitals, the survey was distributed to all physicians, while one hospital participated in the project with a pilot clinic. In one hospital, a stratified random sample of 390 individuals (out of a total of approximately 2500 staff) was selected to ensure representativeness based on role, hierarchical level and sex. Eligibility was limited to hospital staff, excluding affiliated physicians.
The sample of this study comprised 553 physicians (301 females, 54.4%; 252 males, 45.6%), with a response rate of 28.1%. The mean age of the participants was 40.0 years (SD 9.8 years, range 25–68 years). A total of 283 participants (51.2%) had children. On average, respondents had been working as physicians for 13.5 years (SD 9.6 years, range <1–39 years) and in their current hospital for 5.4 years (SD 5.9 years, range <1–25 years). Of the respondents, 177 were resident physicians (32.0%), 206 were attending physicians (37.3%), 108 were senior attending physicians (19.5%) and 62 were chief physicians (11.2%). A total of 394 respondents (71.2%) have acquired a qualification as a medical specialist.
The survey covered various elements of career planning tailored for different life stages. Among others, the study gathered variables to assess attitudes towards part-time employment: Participants were queried about their current and ideal workload. To gauge perceptions of the feasibility of working part-time, participants were asked, “If you would like to reduce your working hours in the near future: Do you think this would be granted?” with response options of “Yes, definitely”, “Yes, probably”, “Probably not”, “No, definitely not” and “I cannot judge”. To examine potential barriers to part-time work, respondents answered three questions: (a) “Do you believe that part-time work compromises medical quality?” with responses “Yes”, “No” or “I don’t know”; (b) “When colleagues opt for work-life balance benefits such as reduced working hours, this typically results in…” with options “A lot of extra work”, “Some extra work”, “No extra work” or “I cannot judge”; (c) “Employees who temporarily reduce their working hours due to personal reasons are less likely to advance in the organisation” using a scale from 1 (“Strongly disagree”) to 5 (“Strongly agree”) along with the option “I cannot judge”. This assessment item was adapted from a scale developed by Dikkers et al. [24].
Data cleaning was conducted with R version 4.3.3 (packages haven, dplyr and base) and data analysis was carried out using SPSS™ version 28. Descriptive statistics were used to illustrate the findings. An analysis of variance (ANOVA) and a t-test were used to assess group differences, followed by Tukey’s Honestly Significant Difference (HSD) test for post-hoc ANOVA comparisons.
The interview data were thematically categorised into hindering and facilitating factors for part-time work among physicians. These factors encompass two key areas: first, the medical culture within the hospital, which includes the attitudes, norms and expectations surrounding physicians’ roles; and second, organisational aspects, which refer to the hospital’s structure, policies and logistical frameworks that influence the feasibility of part-time work. Additionally, the perceived consequences for physicians were examined within both categories (see figure 1).
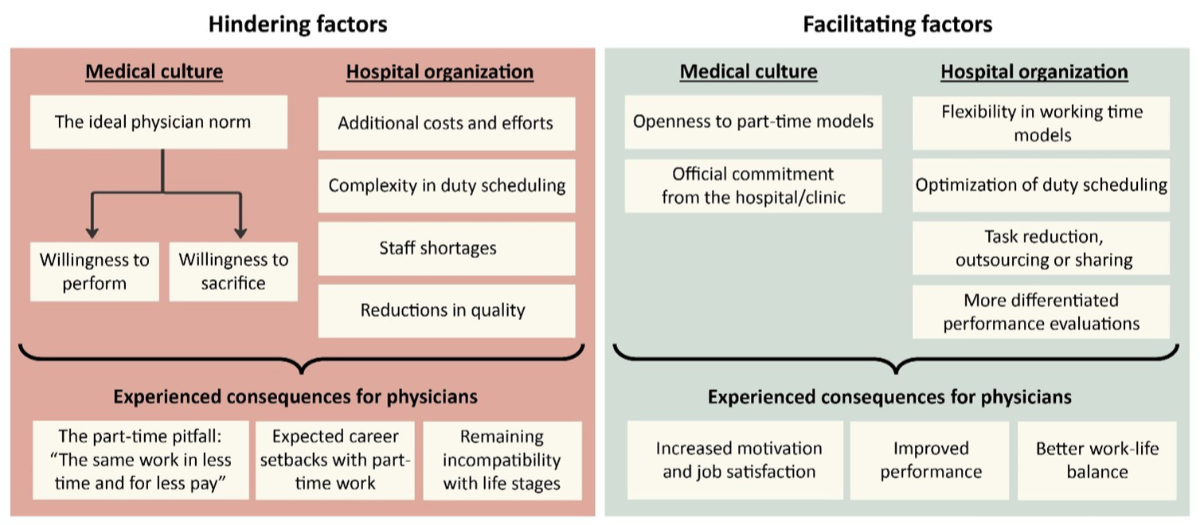
Figure 1Hindering and facilitating factors for the implementation of part-time working for physicians.
The qualitative data indicate that the prevailing medical culture in hospitals is characterised by an “ideal physician norm” that places a high value on performance and personal sacrifice. According to the interviewees, the willingness to perform is primarily linked to a physician’s physical presence in daily clinical life. The reduction in working hours and the associated limited availability in the hospital and for patients is thus perceived as an obstacle by some interviewees:
Ultimately, it’s so individual how much time you’re willing and able to invest. If someone says they want to create a 40% position in a leadership role, it becomes difficult to remain clinically active. At some point, especially in surgical disciplines, you’re just not there enough (…). I don’t know if that’s true, but it’s an opinion that most colleagues would probably share. [Interview Q]
It is notable that the examples provided by the interviewees in this sample frequently refer to very low workloads (<50%), as illustrated by the just-mentioned example.
Another aspect of the “ideal physician norm” is grounded in the assumption that a “successful” medical career often requires personal sacrifices:
I have not yet seen a positive example of someone with children who reduced their workload while still managing to specialise. Instead, I have only encountered individuals in leadership positions who work full-time and have made significant personal sacrifices. [Interview B]
In particular, the “younger generation” (the exact age cohort is not specified by the interviewees) is noted for prioritising personal life over career, potentially conflicting with the willingness to sacrifice:
The generation gap is becoming apparent. (…) The senior physicians (…) had to endure everything, but they are not entirely happy that they had to. (…) And to be honest, you can also see that (…) the younger the residents are, the less willing they are to accept things, or they are much more likely to say, “I’m going home now; I don’t care what happens here”. [Interview P]
At the organisational level, interviewees noted that physicians’ part-time work can result in an additional workload for colleagues and increased costs due to higher coordination and communication efforts. Duty scheduling was also perceived as more complex when accommodating part-time arrangements. Furthermore, interviewees expressed concerns about worsening staff shortages due to reduced workloads as well as potential declines in patient care quality, primarily due to a feared loss of continuity. Interviewees further indicated that the challenges in accommodating part-time work are particularly pronounced in certain medical specialties, especially surgical fields.
As a consequence of working part-time, interviewees described what we call the “part-time pitfall”. This refers to the expectation placed upon part-time physicians to maintain the same amount of work despite the reduction in hours and remuneration. Therefore, part-time physicians seeking career advancement frequently strive to fulfil unadjusted performance expectations:
I currently manage a ward on my own with a 50% workload, yet my manager expects me to work 100% within that 50%. She claims this is reasonable for me. Even after I explained that this is neither possible nor feasible in practice, her answer was simply, “Then that’s your problem. You don’t have good time management”. [Interview B]
Furthermore, there are concerns about potential career setbacks associated with part-time employment:
If you reduce your workload to 80%, or even 60%, as is completely normal in certain professions, that’s not the case in this profession. Instead, you’re sidelined – not everywhere – but the chances of that happening are very very high. [Interview P]
For residents, this means that reduced workloads may extend training duration, limit necessary rotations or flatten the learning curve due to fewer cases.
Moreover, interviewees highlighted that although part-time models are often assumed to improve work-life balance, existing part-time solutions may still be incompatible with the needs and requirements of different life stages. Physicians described arrangements such as the “4 weeks on, 1 week off” model or long block shifts, which hinder external childcare use due to incompatible opening hours and/or require flexibility from partners. This is particularly noteworthy because the most frequently reported negative effects of career expansion are mainly related to the timing of starting a family:
I have to say quite clearly that it was the birth of my first daughter that really had a profound impact on my career. [Interview T]
This not only affects career opportunities for women in medicine but also contributes to female physicians leaving hospital employment:
I lose far too many women in their careers who end up quitting or going into a niche or only working 20%. Ultimately, this is also an economic problem. I’ve invested a lot of time and, this may not be politically correct, but you invest a lot of time and money in women who suddenly stop working. [Interview M]
In the context of medical culture, a supportive culture is deemed conducive if it exhibits “openness to part-time work not only on paper, but also in reality” [Interview B] and if it exemplifies tangible, functioning work-life balance models with the hospital’s official to support such arrangements. At the organisational level, interviewees indicated that concrete support includes increased flexibility in working time models, particularly the ability to adapt workloads promptly to various life situations:
And that you give people the opportunity to temporarily step back (…), work reduced hours, and not have to deal with a hundred other tasks. (…) We just had a colleague, a great physician, whose husband was seriously ill. And then she stopped working altogether. So, if we could have offered her a lower workload (…), we might have been able to keep her. [Interview T]
This is in line with the ability to address adjustment requests promptly and confidentially, as well as to receive support in finding solutions. Furthermore, interviewees highlighted the importance of early and high-quality duty scheduling, as well as the preservation of time and monetary resources for training and further education. Additionally, they discussed the potential benefits of reducing or outsourcing administrative and service tasks for physicians, implementing job-sharing arrangements, establishing dedicated on-call or late shift teams and automating certain processes. Building upon the previously described theme that for physicians, strong performance is closely associated with physical presence, a more comprehensive approach to performance evaluation is required. This approach should consider a physician’s potential and motivation independently of their workload:
(...) I had very open people among those who mentored me, who never measured performance by presence, but precisely by performance. I would say, that’s what made the difference for me. [Interview R]
As a consequence of part-time work, the interviewees reported that they have observed increased motivation, job satisfaction and better work-life balance among part-time physicians:
I find that my part-time employees are much more motivated, they enjoy coming to work (…). I had a really great manager who, back in 2006, said that he preferred part-time employees because they brought enthusiasm and commitment while still balancing family and personal life (…) He almost only had part-time staff, even residents. He was way ahead of his time. [Interview A]
Furthermore, improved performance was also identified as an outcome of physicians engaging in part-time work:
I believe someone working at 80% performs better than 80% of someone working full-time. (…) If you have 10 full-time positions but hire people at 80%, you get 13 or 14 employees. You have a better team performance than with people who all work full-time. [Interview L]
To contextualise the results presented here within a broader dataset, the results of the questionnaire survey are presented below.
The results of the qualitative interviews suggested that the feasibility of part-time work might vary depending on position and specialisation. Therefore, in addition to general results including all participants, descriptive statistics were presented separately for these two categories, recognising potential differences in responses within each group. Furthermore, insights from the interviews indicated that a desire to work part-time is mostly expressed by younger generations and women. These hypotheses were subsequently tested. Percentages were rounded to one decimal place, which may result in totals that do not sum to exactly 100%.
The analysis revealed significant insights into the participants’ workload distribution and their perceptions regarding part-time employment. Of the 553 survey respondents, most (63.7%) stated that their current workload falls between 90% and 100%. However, a majority (61.5%) expressed a preference for a part-time workload of 60% to 89% (see table 1). While 55.5% of respondents wished to maintain their current workload, 40.7% favoured reducing it. Among those desiring a reduction, 89.8% indicated that they preferred a modest decrease ranging from 10% to 20%.
Table 1Workload distribution and average workload among all respondents (n = 553).
| Measure | Workload categories, n (%) | Average (current/ideal) % workload, mean (SD) | ||
| 10–59 | 60–89 | 90–100 | ||
| Current workload | 27 (4.9%) | 174 (31.5%) | 352 (63.7%) | 88.3% (SD 17.1) |
| Ideal workload | 33 (6.0%) | 340 (61.5%) | 180 (32.5%) | 81.0% (SD 15.6) |
SD: standard deviation.
When participants were asked if they thought reduced working hours would be granted, 50 (9.0%) responded “Yes, definitely”, while 282 (51.0%) chose “Yes, probably”. In contrast, 154 (27.8%) thought it would probably not be possible and 25 (4.5%) answered “No, definitely not”. The remaining 42 physicians (7.6%) said they could not judge.
Additionally, the survey investigated participants’ attitudes towards potential obstacles to part-time work. When asked whether part-time work compromises medical quality, 97 respondents (17.5%) thought it did. However, the majority of 406 respondents (73.4%) disagreed, while another 50 respondents (9.0%) were uncertain. Respondents were also asked how they were typically affected by their colleagues’ use of work-life balance benefits, such as part-time work. Most (298, 53.9%) said it resulted in some extra work, while 125 (22.6%) thought it resulted in a lot of extra work. Sixty respondents (10.8%) felt it did not add any extra work, and 70 (12.7%) were unsure if it did.
Furthermore, participants were asked if they agreed with the statement that employees who temporarily reduce their working hours for personal reasons are less likely to advance in the organisation. While 15 respondents (2.7%) strongly disagreed, 97 respondents (17.5%) somewhat disagreed and 107 respondents (19.3%) partially agreed. Most respondents either agreed (151 respondents, 27.3%) or strongly agreed (68 respondents, 12.3%) with the statement. An additional 115 respondents (20.8%) said they could not judge.
The analysis proceeded to examine position-specific perceptions and attitudes towards part-time employment, as detailed in table 2. Residents showed the largest discrepancy between current and desired workloads and were also the only group where a majority (53.1%) expressed doubt about the possibility of workload reduction. The potential negative impact of part-time work on medical quality was a significant concern among senior physicians, particularly chief physicians, with a third sharing this view. Senior attending and chief physicians were also more concerned than resident and attending physicians about the increased workload caused by part-time work of colleagues. Furthermore, the perception that physicians working part-time have fewer career advancement opportunities was most prevalent among attending physicians.
Table 2Average current/ideal workload, perceived feasibility of part-time work and perceived barriers, by respondents’ position.
| Position | n | Current % workload, mean ± SD | Ideal % workload, mean ± SD | Responses, n (%) | |||
| Workload reduction feasible * | Part-time reduces quality ** | Part-time results in extra work for others *** | Part-time reduces career chances **** | ||||
| Resident physicians | 177 | 96.8% ± 8.8% | 86.0% ± 11.8% | 83 (46.9%) | 19 (10.7%) | 121 (68.4%) | 100 (56.5%) |
| Attending physicians | 206 | 80.6% ± 19.8% | 75.5% ± 17.7% | 141 (68.4%) | 35 (17.0%) | 159 (77.2%) | 139 (67.5%) |
| Senior attending physicians | 108 | 84.5% ± 17.2% | 78.6% ± 14.5% | 72 (66.7%) | 22 (20.4%) | 89 (82.4%) | 58 (53.7%) |
| Chief physicians | 62 | 96.0% ± 8.6% | 89.2% ± 11.9% | 36 (58.1%) | 21 (33.9%) | 54 (87.1%) | 29 (46.8%) |
SD: standard deviation.
* Number of respondents, by position, who believe they would be granted a workload reduction.
** Number of respondents, by position, who believe that part-time work negatively impacts medical quality.
*** Number of respondents, by position, who believe that a colleague’s part-time work results in extra work.
**** Number of respondents, by position, who partially agreed, agreed or strongly agreed that part-time work hinders career advancement opportunities.
Analysis of data by specialty revealed some notable trends, as shown in table 3. Across specialties, the average workload ranged from 73.3% to 91.7%, with paediatrics/adolescent physicians reporting the lowest current workload and (orthopaedic) surgeons reporting the highest. There is a desire to reduce workload across all specialties. At least 50% of respondents in each specialty believed they would be granted a workload reduction. The proportion of respondents who expressed concern about the potential impact of part-time working on the quality of care was generally below 20%, except for surgeons and cardiologists. Responses to the perceived impact of colleagues working part-time varied, with 69.4% to 88.9% of physicians expressing concern. Gynaecologists and cardiologists were most concerned about the negative impact of part-time work on career progression, while those in intensive care were least concerned. These findings should be interpreted with caution due to potential sample size limitations.
Table 3Average current/ideal workload, perceived feasibility of part-time work and perceived barriers, by specialty.
| Specialty | n | Current % workload, mean ± SD | Ideal % workload, mean ± SD | Responses, n (%) | |||
| Workload reduction feasible * | Part-time reduces quality ** | Part-time results in extra work for others *** | Part-time reduces career chances **** | ||||
| All physicians with specialist title# | 394 | 85.2% ± 18.1% | 79.5% ± 16.1% | 258 (65.5%) | 76 (19.3%) | 311 (78.9%) | 242 (61.4%) |
| Internal medicine## | 62 | 83.0% ± 19.4% | 78.1% ± 15.6% | 41 (66.1%) | 11 (17.7%) | 45 (72.6%) | 38 (61.3%) |
| (Ortho)surgery | 53 | 91.7% ± 16.0% | 82.1% ± 15.1% | 34 (64.2%) | 15 (28.3%) | 44 (83.0%) | 34 (64.1%) |
| Anaesthesiology | 49 | 85.5% ± 15.5% | 78.8% ± 15.5% | 35 (71.4%) | 6 (12.2%) | 34 (69.4%) | 29 (59.2%) |
| Paediatrics / adolescent medicine | 42 | 73.3% ± 25.3% | 72.5% ± 22.9% | 32 (76.2%) | 6 (14.3%) | 32 (76.2%) | 26 (61.9%) |
| Intensive care medicine | 28 | 88.9% ± 12.6% | 84.8% ± 13.4% | 20 (71.4%) | 5 (17.9%) | 21 (75.0%) | 14 (50.0%) |
| Gynaecology | 27 | 88.5% ± 16.6% | 82.2% ± 16.0% | 21 (77.8%) | 3 (11.1%) | 22 (81.5%) | 22 (81.5%) |
| Radiology | 18 | 85.8% ± 17.5% | 80.3% ± 16.5% | 10 (55.6%) | 1 (5.6%) | 16 (88.9%) | 10 (55.6%) |
| Cardiology | 15 | 89.3% ± 12.8% | 80.7% ± 15.3% | 8 (53.3%) | 7 (46.7%) | 11 (73.3%) | 11 (73.3%) |
SD: standard deviation.
* Number of respondents, by position, who believe they would be granted a workload reduction.
** Number of respondents, by position, who believe that part-time work negatively impacts medical quality.
*** Number of respondents, by position, who believe that a colleague’s part-time work results in extra work.
**** Number of respondents, by position, who partially agreed, agreed or strongly agreed that part-time work hinders career advancement opportunities.
# This category includes all respondents who indicated that they had a specialist title. Only those specialties with at least 15 respondents were considered separately.
## Only internal medicine specialists without additional titles were included in this category.
Analysis of the data revealed significant differences in the ideal workload across age groups, F(3, 553) = 11.625, p <0.001 and sex, p <0.001, as shown in tables 4 and 5. In particular, the youngest cohort of physicians reported the highest ideal workload, which differed significantly to that of the 31–40 and 41–50 age groups. The lowest ideal workload was reported by the 41–50 age group, which differed significantly from that of the other age groups. Female physicians reported a significantly lower ideal workload than male physicians. However, the difference between current and ideal workload was slightly more pronounced for male than for female physicians.
Table 4Differences in average ideal workload between age groups. Tukey’s Honestly Significant Differences (HSD) was applied to test for post-hoc ANOVA comparisons. Only differences reaching a 95% level of significance are shown.
| Age group | n | Current % workload, mean ± SD | Ideal % workload, mean ± SD | Significant difference in ideal % workload vs age group(s): |
| 20–30 years | 96 | 99.1% ± 5.0% | 87.9% ± 11.6% | 31–40 years (p <0.001) |
| 41–50 years (p <0.001) | ||||
| 31–40 years | 216 | 87.5% ± 16.4% | 80.5% ± 14.5% | 20–30 years (p <0.001) |
| 41–50 years (p = 0.047) | ||||
| 41–50 years | 143 | 82.0% ± 19.2% | 76.2% ± 17.1% | 20–30 years (p <0.001) |
| 31–40 years (p = 0.047) | ||||
| 51+ years (p = 0.009) | ||||
| 51+ years | 98 | 88.6% ± 17.9% | 82.5% ± 16.8% | 41–50 years (p = 0.009) |
SD: standard deviation.
Table 5Current/ideal workload by sex.
| Sex | n | Current % workload, mean ± SD | Ideal % workload, mean ± SD |
| Female | 301 | 85.0% ± 18.6% | 77.8% ± 16.7% |
| Male | 252 | 92.2% ± 14.0% | 84.8% ± 13.3% |
SD: standard deviation.
This exploratory mixed-methods study investigated hospital physicians’ attitudes towards part-time employment and factors that hinder or facilitate part-time work among hospital physicians.
The quantitative data revealed a widespread desire for workload reduction across all roles, specialties, age groups and sex, with an average ideal workload of 81%. Contrary to some beliefs expressed in the qualitative interviews, which suggested that young physicians predominantly prefer part-time work, the youngest age group reported the highest desired workloads in the quantitative survey. This could be due to the demanding nature of the residency period, which necessitates the completion of a certain number of rotations [25, 26]. Consequently, residents may opt to maintain a higher workload to shorten their training. It is also noteworthy that when interviewees discussed part-time scenarios, they frequently provided fictitious examples with very low workloads. However, the quantitative data indicated that only a minority of respondents expressed interest in such low workloads. The majority of those who would like to reduce their workload preferred a decrease in the range 10–20%. Interestingly, most respondents (60%), particularly non-resident physicians, believed that they would be granted a workload reduction. This raises the question of why such reductions are not more widely sought. One reason provided in the interviews is the perceived diminished likelihood of career progression. In the survey, almost 60% of respondents partially agreed, agreed or strongly agreed that part-time workers are less likely to have advancement opportunities within the organisation, with this perception being more prevalent among residents and in certain specialties. These concerns are consistent with findings from previous studies in which physicians reported perceived limited career opportunities as part-time workers [16, 20–22]. Additionally, some physicians reported managing the same amount of work despite working part-time, either by compressing their tasks into fewer hours or facing heightened expectations, a phenomenon we refer to as the “part-time pitfall”. The increased time pressure associated with working part-time was also reported in an earlier study by Kiechl-Kohlendorfer and Hackl [21]. Additionally, in a study by de Jong et al. [27], part-time physicians worked similar or more hours per full-time equivalent as full-time physicians.
One potential explanation for the difficulties encountered by part-time working physicians in hospitals is that hospital structures, such as performance appraisals, shift schedules and training programmes, are predominantly designed around full-time work models [15, 22]. Consequently, part-time working arrangements cannot be readily incorporated into existing structures, and their integration may necessitate particular consideration. Regarding this situation, interviewees in this study describe several barriers, including increased coordination and communication requirements, as well as heightened complexity in staff scheduling. As a result, interviewees report that part-time working among colleagues generally results in additional work for other employees. This view is shared by more than three-quarters of the respondents in the survey.
Given the challenges associated with implementing part-time work, interviewees expressed concerns that introducing part-time work arrangements could potentially compromise medical quality and undermine the educational development of resident physicians. However, the survey data showed that most respondents (82.5%) did not share the concern about a decline in medical quality due to part-time work. Notably, the concern was more prevalent in senior positions and varied across different medical specialties, with cardiologists and surgeons expressing the highest levels of concern. To date, research on the impact of part-time work among hospital-based physicians on patient outcomes has yielded mixed results. Some studies suggest positive outcomes, such as higher patient satisfaction, consistent quality of work, and continuity of care [28–30]. Conversely, other research findings suggest potential negative effects, such as higher mortality rates associated with part-time work [31]. Prior research on part-time physicians indicates that organisational factors of healthcare institutions influence the quality of care delivered under reduced working hour arrangements [30, 32, 33]. Optimising these organisational factors may be crucial for mitigating any potential negative consequences associated with reduced working hours [34].
The interviewees made several recommendations for improving part-time working arrangements, such as reducing or outsourcing administrative and service tasks for physicians, implementing job-sharing arrangements, establishing dedicated on-call or late-shift teams and automating certain processes. Some of these solutions have also been discussed by other researchers [15, 16, 20, 35, 36]. However, the findings of this study indicate that the organisation of part-time work varies significantly across medical specialties.
Given the variation in patient care continuity, treatment characteristics and complexity across specialties, we argue that customised solutions are necessary for each clinic. Effective solutions require insight into operational logistics and a comprehensive understanding of system design [17]. It is thus recommended that a collaborative approach is applied when developing part-time solutions, involving all relevant stakeholders, including physicians, managers and HR specialists. The involvement of employees is essential to ensure that solutions are identified that effectively address the personal needs of individual employees and offer them compatibility with various life stages.
Ultimately, a cultural change within the medical profession is required to successfully implement part-time working arrangements [20, 22, 37]. A key finding of this study is that the prevailing “ideal physician norm” which prioritises physical presence and professional obligations over personal life, remains widely held and is fundamentally incompatible with part-time work. Many interviewees reported an omnipresent (mis)conception that a good physician has to work full-time. Overcoming this norm and adopting a new model of medical practice that embraces part-time work as a viable and prominent option for all physicians across different specialties might be essential for the sustainable integration of part-time arrangements. The more receptive and adaptable hospital systems are to part-time work, the more profitable the integration of such arrangements into the workforce will be [15]. Importantly, the potential benefits of part-time work highlighted in the interviews and supported by the literature, such as increased motivation and satisfaction [38], improved performance [16] and better work-life balance [39], should not be overlooked. Additionally, it is important to address the misconception that physicians seek very low part-time positions, as this study finds that physicians generally aspire to substantial workloads, suggesting that modest reductions may be sufficient for meaningful change. Furthermore, this study highlights that, despite persistent stereotypes about younger generations preferring reduced workloads, physicians across all age groups show a clear interest in workload reduction. This aligns with broader workforce trends, where work-life balance has increasingly become a priority for individuals across various age groups [40, 41].
There are potential limitations to this exploratory study. First, due to the limited sample size, especially in the professional subgroups, and the fact that the study was conducted in the German-speaking part of Switzerland, the results cannot be generalised and must be interpreted with caution. Future research should investigate part-time work and its implementation, as well as its effects in different subfields and regions of Switzerland. Secondly, the study relies on self-reported data from physicians, who assess the impact of part-time work on various factors, such as their career or the quality of care. These perceptions may not reflect actual outcomes. Further research, particularly longitudinal research, is needed to examine the impact of part-time work on various outcomes for workers, patients and colleagues. Thirdly, although the qualitative sample was selected by HR specialists in accordance with the instructions provided, the research team lacked direct insight into the process, thereby limiting transparency. Furthermore, while physician online surveys frequently experience low and declining response rates [42, 43], the 28.1% response rate may introduce self-selection bias, affecting the generalisability of the findings. These sampling limitations should be considered when interpreting the results.
To our knowledge, this is the first study to examine the attitudes of Swiss hospital physicians towards part-time work across various positions and specialisations, and the factors that hinder or facilitate its adoption. This study highlights the desire for a reduction in workload across different roles, specialties, ages and sexes, as well as specific challenges for physicians and hospitals in implementing part-time work. Given the varying circumstances of each subspecialty and position, we suggest that context-specific solutions for clinics or teams be found through participatory processes. This process should begin by addressing misconceptions and dismantling the ideal physician norm, which is based solely on time availability. Furthermore, to achieve a reasonable balance between the demands of a medical career and a personal life, it is important to consider that part-time work is not the only – and may not always be the most suitable – solution. Additional structural and cultural interventions should be considered to meet the individual needs of today’s medical profession [37, 44].
Given the small number of eligible hospitals and the familiarity within the medical community, participating physicians voiced concerns about confidentiality, as institutional identities could be inferred from data patterns (e.g. specialty, role, career path). To address this, the survey guaranteed secure FHNW oversight of all data, balancing transparency, confidentiality and trust.
This research was funded by the Federal Office for Gender Equality (FOGE) and the FHNW School of Applied Psychology.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Burla L, Widmer M, Zeltner C. Zukünftiger Bestand und Bedarf an Fachärztinnen und -ärzten in der Schweiz. Teil 1: Total der Fachgebiete, Hausarztmedizin, Pädiatrie, Psychiatrie und Psychotherapie sowie Orthopädie [Future supply and demand for medical specialists in Switzerland. Part 1: Total of specialities, family medicine, paediatrics, psychiatry and psychotherapy and orthopaedics]. Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2022 Apr. Available from: https://www.obsan.admin.ch/de/publikationen/2022-zukuenftiger-bestand-und-bedarf-fachaerztinnen-und-aerzten-der-schweiz
2. Burla L, Widmer M, Zeltner C. Zukünftiger Bestand und Bedarf an Fachärztinnen und -ärzten in der Schweiz. Teil 2: Total der Fachgebiete, Gynäkologie und Geburtshilfe, Kinder- und Jugendpsychiatrie und -psychotherapie, Ophthalmologie sowie Kardiologie [Future supply and demand for medical specialists in Switzerland. Part 2: Total of specialities, gynaecology and obstetrics, child and adolescent psychiatry and psychotherapy, ophthalmology and cardiology]. Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2023 May. Available from: https://www.obsan.admin.ch/de/publikationen/2023-zukuenftiger-bestand-und-bedarf-fachaerztinnen-und-fachaerzten-der-schweiz
3. Bolliger C, Golder L, Jans C. (Büro Vatter AG, gfs.bern, Bern). Der Ausstieg aus der kurativen ärztlichen Tätigkeit [The exit from curative medical practice]. Schlussbericht. Bern: Verband der Schweizerischen Assistenz- und Oberärztinnen und -ärzte (VSAO) & Verbindung der Schweizer Ärztinnen und Ärzte (FMH); 2016 May. Available from: https://vsao.ch/wp-content/uploads/2019/11/Schlussbericht-Studie-Berufsausstieg-2016_DE.pdf
4. Peter KA, Hahn S, Schols JM, Halfens RJ. Work-related stress among health professionals in Swiss acute care and rehabilitation hospitals-A cross-sectional study. J Clin Nurs. 2020 Aug;29(15-16):3064–81. doi: https://doi.org/10.1111/jocn.15340
5. Hämmig O. Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC Health Serv Res. 2018 Oct;18(1):785. doi: https://doi.org/10.1186/s12913-018-3556-1
6. Goehring C, Bouvier Gallacchi M, Künzi B, Bovier P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med Wkly. 2005 Feb;135(7-8):101–8.
7. Knecht M, Bauer GF, Klaghofer R, Buddeberg-Fischer B, Stamm M, Hämmig O. Work-life conflicts and health among Swiss physicians—in comparison with other university graduates and with the general Swiss working population. Swiss Med Wkly. 2010 Jul;140(2728):w13063. doi: https://doi.org/10.4414/smw.2010.13063
8. Villiger S, Hämmig O. Work Related Demands and Resources as Predictors of Well-being at Work Among Healthcare Workers in Switzerland. J Occup Environ Med. 2023 Aug;65(8):689–93. doi: https://doi.org/10.1097/JOM.0000000000002885
9. Jung FU, Luppa M, Riedel-Heller SG. Arbeitszeit bei Ärzt:innen und Auswirkungen auf Gesundheit, Zufriedenheit und Gesundheitsversorgung [Physician working hours and effects on health, satisfaction, and healthcare]. Zentralbl Arbeitsmed Arbeitsschutz Ergon. 2023 Apr;73(4):1–7.
10. Verband Schweizerischer Assistenz- und Oberärztinnen und -ärzte (VSAO). Die 42+4-Stunden Woche [The 42+4-hour week]. 2023. Available from: https://vsao.ch/arbeitsbedingungen/42plus4/
11. Bodendieck E, Jung FU, Luppa M, Riedel-Heller SG. Burnout and work-privacy conflict - are there differences between full-time and part-time physicians? BMC Health Serv Res. 2022 Aug;22(1):1082. doi: https://doi.org/10.1186/s12913-022-08471-8
12. Flury Bodenmann B, Zeller A. Arztberuf und Familiengründung: Karrierevorstellungen von Medizinstudierenden der Universität Basel [Medical profession and starting a family: career ideas of medical students at the University of Basel]. Praxis (Bern). 2016 Jul;105(15):877–83.
13. Buddeberg-Fischer B, Stamm M, Buddeberg C, Bauer G, Häemmig O, Knecht M, et al. The impact of gender and parenthood on physicians’ careers—professional and personal situation seven years after graduation. BMC Health Serv Res. 2010 Feb;10(1):40. doi: https://doi.org/10.1186/1472-6963-10-40
14. FMH Swiss Medical Association. FMH-Ärztestatistik 2023 [FMH Medical Statistics 2023]. Available from: https://www.fmh.ch/themen/aerztestatistik/fmh-aerztestatistik.cfm
15. Aebi C, Kühni R, Suri P, Schellinger J. Teilzeitarbeit auf mittlerer Kaderstufe – eine spezielle Herausforderung im Krankenhaus[Part-time work at middle management level - a special challenge in hospitals]. In: Tokarski K, Schellinger J, Berchtold P, editors. Strategische Organisation. Wiesbaden: Springer Gabler; 2018. pp. 225–58. doi: https://doi.org/10.1007/978-3-658-18246-5_11
16. Hendrickson SA, Ibrahim I, Eccles S, Fitzgerald A. Less than full time training in plastic surgery: A qualitative survey-based study and practical suggestions for improvement. J Plast Reconstr Aesthet Surg. 2022 Sep;75(9):2875–81. doi: https://doi.org/10.1016/j.bjps.2022.06.042
17. Molema JJ, Groothuis S, Baars IJ, Kleinschiphorst M, Leers EG, Hasman A, et al. Healthcare system design and parttime working doctors. Health Care Manag Sci. 2007 Dec;10(4):365–71. doi: https://doi.org/10.1007/s10729-007-9032-9
18. Harries RL, Gokani VJ, Smitham P, Fitzgerald JE; councils of Association of Surgeons in Training and British Orthopaedic Trainees Association. Less than full-time training in surgery: a cross-sectional study evaluating the accessibility and experiences of flexible training in the surgical trainee workforce. BMJ Open. 2016 Apr;6(4):e010136. doi: https://doi.org/10.1136/bmjopen-2015-010136
19. Kellogg KC. Challenging Operations. Medical Reform and Resistance in Surgery. Chicago: University of Chicago Press; 2003.
20. Cathcart J, Mayne KJ, Hull R, Jones M, Miller A. Less than full-time training (LTFT), is this the new norm? A cross-sectional study using a UK-wide online survey to evaluate trainees’ views and intentions for LTFT. BMJ Open. 2022 Nov;12(11):e064518. doi: https://doi.org/10.1136/bmjopen-2022-064518
21. Kiechl-Kohlendorfer U, Hackl JM. Arztliche Teilzeitarbeit [Physicians working part-time]. Wien Med Wochenschr. 2004 Apr;154(7-8):170–4. doi: https://doi.org/10.1007/s10354-004-0049-0
22. Pudasaini S, Schenk L, Möckel M, Schneider A. Work-life balance in physicians working in two emergency departments of a university hospital: results of a qualitative focus group study. PLoS One. 2022 Nov;17(11):e0277523. doi: https://doi.org/10.1371/journal.pone.0277523
23. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: https://doi.org/10.1191/1478088706qp063oa
24. Dikkers JS, Geurts SA, den Dulk L, Peper B, Taris TW, Kompier MA. Dimensions of work-home culture and their relations with the use of work-home arrangements and work-home interaction. Work Stress. 2007;21(2):155–72. doi: https://doi.org/10.1080/02678370701442190
25. Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One. 2018 Nov;13(11):e0206840. doi: https://doi.org/10.1371/journal.pone.0206840
26. Zumbrunn B, Stalder O, Limacher A, Ballmer PE, Bassetti S, Battegay E, et al. The well-being of Swiss general internal medicine residents. Swiss Med Wkly. 2020 Jun;150(2324):w20255. doi: https://doi.org/10.4414/smw.2020.20255
27. de Jong JD, Heiligers P, Groenewegen PP, Hingstman L. Part-time and full-time medical specialists, are there differences in allocation of time? BMC Health Serv Res. 2006 Mar;6(1):26. doi: https://doi.org/10.1186/1472-6963-6-26
28. Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000 Feb;15(2):122–8. doi: https://doi.org/10.1046/j.1525-1497.2000.02219.x
29. Fairchild DG, McLoughlin KS, Gharib S, Horsky J, Portnow M, Richter J, et al. Productivity, quality, and patient satisfaction: comparison of part-time and full-time primary care physicians. J Gen Intern Med. 2001 Oct;16(10):663–7. doi: https://doi.org/10.1111/j.1525-1497.2001.01111.x
30. Rosland AM, Krein SL, Kim HM, Greenstone CL, Tremblay A, Ratz D, et al. Measuring patient-centered medical home access and continuity in clinics with part-time clinicians. Am J Manag Care. 2015 May;21(5):e320–8.
31. Kato H, Jena AB, Figueroa JF, Tsugawa Y. Association Between Physician Part-time Clinical Work and Patient Outcomes. JAMA Intern Med. 2021 Nov;181(11):1461–9. doi: https://doi.org/10.1001/jamainternmed.2021.5247
32. Heje HN, Vedsted P, Sokolowski I, Olesen F. Doctor and practice characteristics associated with differences in patient evaluations of general practice. BMC Health Serv Res. 2007 Apr;7(1):46. doi: https://doi.org/10.1186/1472-6963-7-46
33. Murray A, Safran DG, Rogers WH, Inui T, Chang H, Montgomery JE. Part-time physicians. Physician workload and patient-based assessments of primary care performance. Arch Fam Med. 2000 Apr;9(4):327–32. doi: https://doi.org/10.1001/archfami.9.4.327
34. Kegreiss S, Studer C, Beeler PE, Essig S, Tomaschek R. Impact of primary care physicians working part-time on patient care: A scoping review. Eur J Gen Pract. 2023 Dec;29(1):2271167. doi: https://doi.org/10.1080/13814788.2023.2271167
35. Antony P, Kalkum E, Muller MK, Hager L, Probst P. The introduction of a 42 + 4 h work week for surgical residents in Switzerland - a stakeholder analysis. Langenbecks Arch Surg. 2024 Jun;409(1):197. doi: https://doi.org/10.1007/s00423-024-03385-x
36. Höltje M, Osthaus WA, Koppert W. Teilzeitmodelle in der Anästhesie - Beispiel einer Anästhesieabteilung eines deutschen Universitätsklinikums [Part-time concepts in anaesthesia -example of a department of anaesthesiology at a university hospital in Germany]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2015 May;50(5):358–63. doi: https://doi.org/10.1055/s-0040-100507
37. Frey J, Kwakye D, Liebig B. Vereinbarkeit von Beruf und Privatleben von Spitalärztinnen und -ärzten: Eine Wegleitung [Work-life balance for hospital physicians: A guide]. Olten: Hochschule für Angewandte Psychologie FHNW, Institut für Kooperationsforschung und -entwicklung; 2023 Mar. Available from: https://doi.org/
38. Mechaber HF, Levine RB, Manwell LB, Mundt MP, Linzer M, Schwartz M, et al.; MEMO Investigators. Part-time physicians...prevalent, connected, and satisfied. J Gen Intern Med. 2008 Mar;23(3):300–3. doi: https://doi.org/10.1007/s11606-008-0514-3
39. Peter KA, Halfens RJ, Hahn S, Schols JM. Factors associated with work-private life conflict and leadership qualities among line managers of health professionals in Swiss acute and rehabilitation hospitals - a cross-sectional study. BMC Health Serv Res. 2021 Jan;21(1):81. doi: https://doi.org/10.1186/s12913-021-06092-1
40. Wielers R, Münderlein M, Koster F. Part-time work and work hour preferences: an international comparison. Eur Sociol Rev. 2014 Feb;30(1):76–89. doi: https://doi.org/10.1093/esr/jct023
41. Waworuntu EC, Kainde SJ, Mandagi DW. Work-life balance, job satisfaction, and performance among Millennial and Gen Z employees: a systematic review [Work-Life Balance, Kepuasan Kerja, dan Kinerja Di Antara Karyawan Milenial dan Gen Z: Tinjauan Sistematis]. Society. 2022 Dec;10(2):384–98. doi: https://doi.org/10.33019/society.v10i2.464
42. Barnhart BJ, Reddy SG, Arnold GK. Remind Me Again: Physician Response to Web Surveys: The Effect of Email Reminders Across 11 Opinion Survey Efforts at the American Board of Internal Medicine from 2017 to 2019. Eval Health Prof. 2021 Sep;44(3):245–59. doi: https://doi.org/10.1177/01632787211019445
43. Cho YI, Johnson TP, Vangeest JB. Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response. Eval Health Prof. 2013 Sep;36(3):382–407. doi: https://doi.org/10.1177/0163278713496425
44. Karakash S, Solone M, Chavez J, Shanafelt T. Physician Work-Life Integration: Challenges and Strategies for Improvement. Clin Obstet Gynecol. 2019 Sep;62(3):455–65. doi: https://doi.org/10.1097/GRF.0000000000000442