Does health insurance status influence surgical complications? An analysis of abdominal,
thoracic and vascular interventions in a Swiss tertiary referral centre
DOI: https://doi.org/https://doi.org/10.57187/s.4179
Maximilian Bleyab*,
Stefan Gutknechta*,
Laurin Burlaa,
Christoph Zindelacd,
Markus Webera,
Simon Wranna
a Department
for Abdominal, Thoracic, and Vascular Surgery, Triemli Hospital Zurich, Zurich,
Switzerland
b Chair
for Gender Medicine, University of Zurich, Zurich, Switzerland
c Department
of Orthopaedics, Balgrist University Hospital, University of Zurich, Zurich,
Switzerland
d Division
of Orthopaedics and Trauma Surgery, Department of Surgery, Cantonal Hospital Graubuenden,
Chur, Switzerland
* Equal
contribution as first authors
Summary
STUDY AIMS: In Switzerland, basic health insurance
is compulsory. Supplementary or private health insurance may be arranged, providing
advantages such as hospital comfort and a free choice of doctors. Since there is
limited data on whether insurance status influences the outcome of surgery, this
study aimed to investigate the influence of supplementary insurance status on the
overall complication occurrence in a group of abdominal, thoracic and vascular surgeries.
METHODS: This study is based on surgical
patient data prospectively collected between September 2016 and March 2018 from
one participating Swiss tertiary referral hospital of the StOP?-trial (NCT02428179),
which investigated the effect of structured intraoperative briefings on patient
outcomes. First, additional data, including insurance status, demographic and surgical
parameters within 30 days was collected. Second, due to endogeneity concerns in
the sample driven by selective access to a supplementary insurance, propensity-score
matching (PSM) was used to balance samples for the treatment variable (insurance
status) by demographic parameters and surgical complexity. The primary outcome was
the estimated treatment effect of a supplementary insurance on the occurrence of
surgical complications, categorised by the Clavien-Dindo classification (CDC). Finally,
multiple logistic regression was used to detect further conditional associations
of demographic and surgical variables with the occurrence of complications.
RESULTS: Of all 3173 procedures, 64.3% were
elective, 48.2% had a higher surgical complexity (excluding appendectomies, cholecystectomies,
hernia surgery and lymph node excision) and 18.6% of all patients had supplementary
insurance. The occurrence of complications, including surgical site infection and
postoperative complications, was 30.4%. After matching 591 patients with basic insurance
to 591 patients with a supplementary insurance, no significant association between
insurance status and complications could be found (crude odds ratio [OR] [95%
CI]: 0.97 [0.77–1.23]). In contrast to insurance status, multiple logistic regression
identified
that variables such as surgical complexity (adjusted OR [95% CI]: 1.80 [1.27–2.56]),
contamination (adjusted OR [95% CI]: 1.90 [1.41–2.56]) and duration of surgery (adjusted
OR [95% CI]: 1.008 [1.006–1.009]) were associated with the occurrence of complications.
CONCLUSION: Despite the different cost-liable
insurance levels, there were no significant differences and, therefore, no disadvantages
for basic insured patients regarding the complication rate in this Swiss cohort
undergoing abdominal, thoracic or vascular surgery.
Introduction
In Switzerland, basic health insurance is compulsory
by law. The goal of this compulsory insurance system is that everyone receives the
same quality of medicine [1], meeting the highest standards. This means that market-orientated
healthcare insurance companies cover all standard treatment costs. Many different
providers also offer various supplementary insurance models, which include, e.g.
benefits in advanced hospitality and Swiss-wide choice of attending doctors [2].
Ethically, medical treatment and the implicated
outcome should be independent of financial concerns. Still, studies of the US healthcare
system found disadvantages for surgical outcomes, as measured by mortality and complication
rates of different surgical procedures, between patients with no insurance or public
insurance such as Medicare or Medicaid [3–5]. Similar findings were reported for
surgical site infections [6]. These studies implicate a strong influence of insurance
status on medical treatment outcomes. There is less knowledge about disparities
in European healthcare systems. A Swiss retrospective study of 30,175 trauma patients
suggests a positive effect of supplementary health insurance on surgical complications
[7]. On the contrary, smaller studies in general and abdominal surgery reflect no
benefit on surgical complication [8] or surgical site infections [9]. Despite showing
less importance of the insurance status in the Swiss health system, many factors
are still indistinct. One main uncharted factor in the medical outcome is the
experience of the lead surgeon. This consideration is of major importance, as many
patients raise concerns about not having the option to choose the most experienced
surgeon. The supplementary insurance often allows the treatment by a more experienced
doctor in the clinic [10]. Abdominal, thoracic and vascular surgery may offer highly
complex anatomical relations. Therefore, repetitive intraoperative decision-making
to adjust the surgical procedure may occur. Intraoperative decision-making may be
highly demanding and rely mainly on the lead surgeon’s experience. Surgical experience
could therefore have a strong impact on intra- and postoperative complications.
Given the lack of studies of comprehensive size
in the field of abdominal, thoracic and vascular surgery, the present study aimed
to investigate the estimated treatment effect of supplementary insurance on surgical
complications for patients for this specialty in Switzerland. Furthermore, we wanted
to evaluate the role of potential confounders on this relationship, including demographic
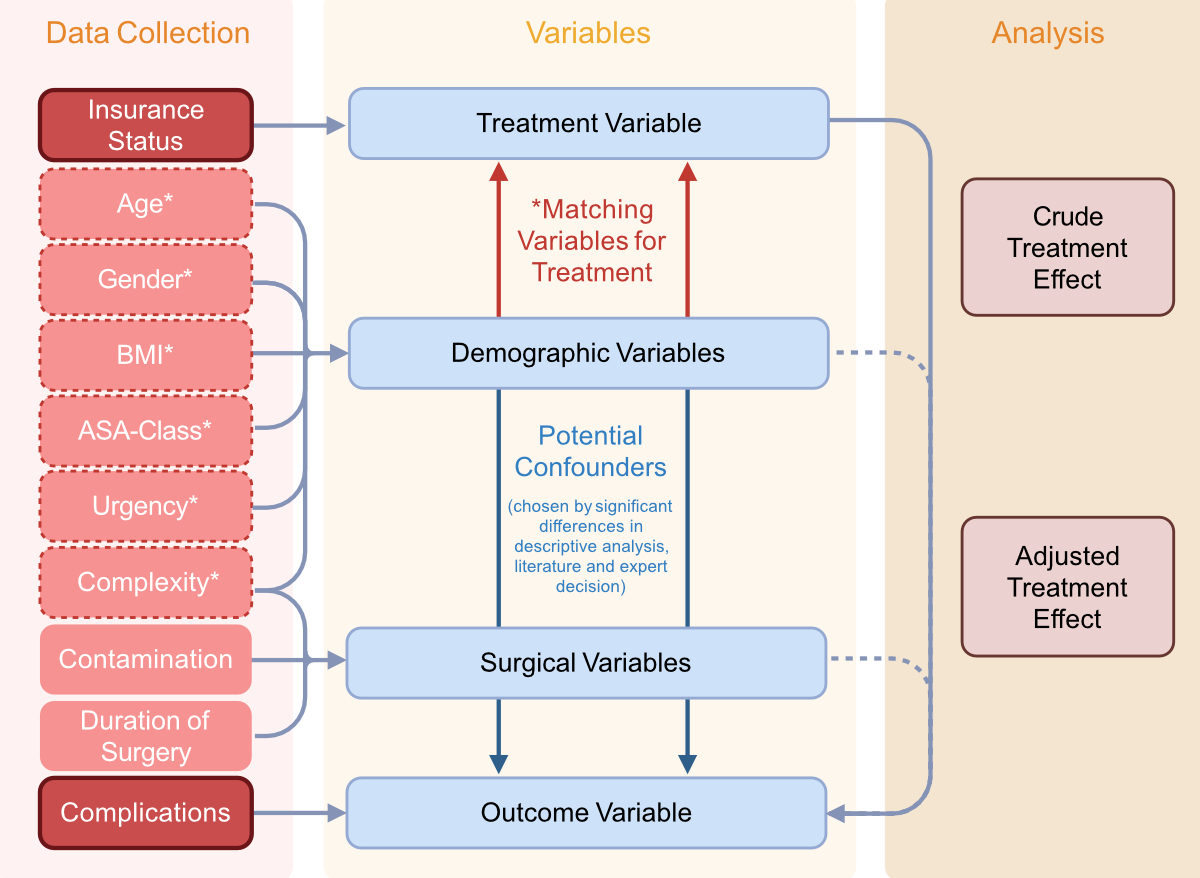
and surgical variables (figure 1).
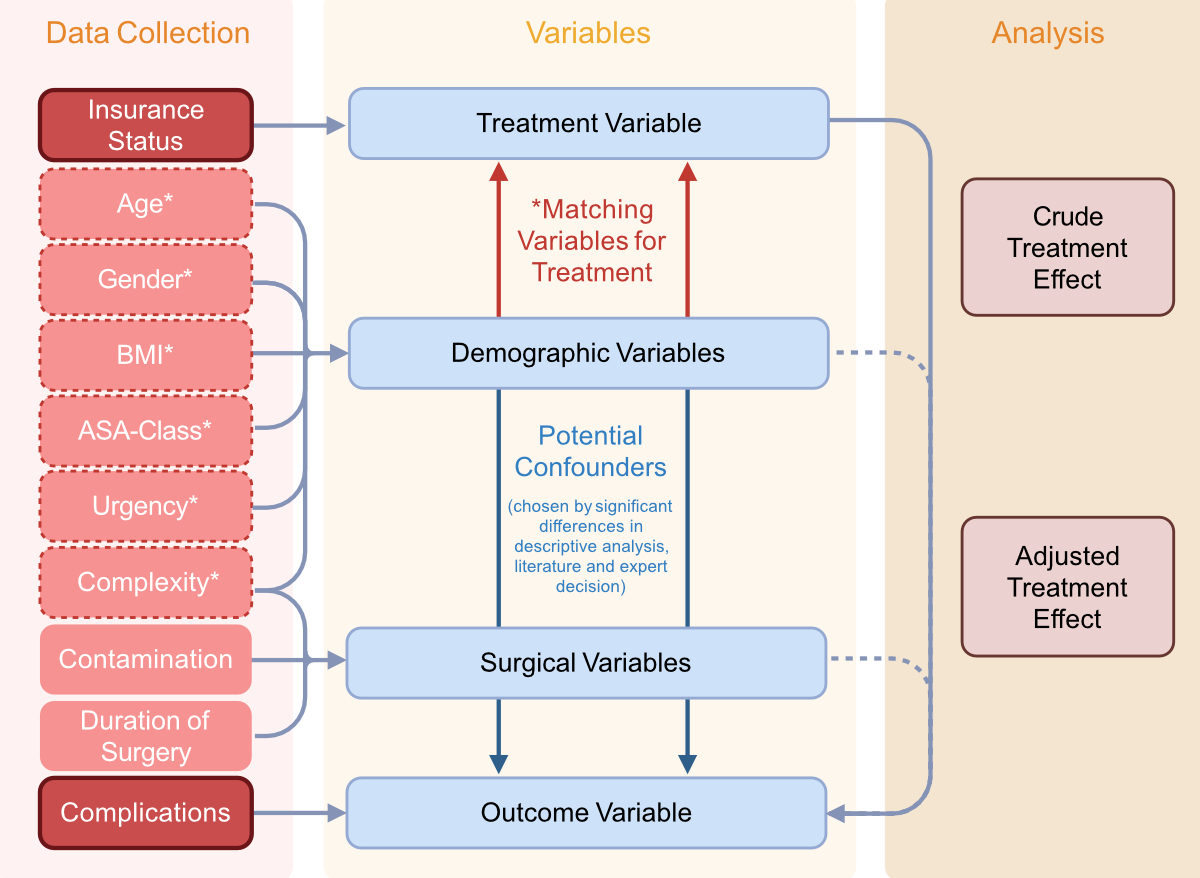
Figure 1Summary of assessed variables, included
confounders and matching variables. Assessed variables from the StOP-trial and internal
medical records. Matching treatment (insurance) by simulation of a selection process
for insurance along with categories of demographics (age, sex), patient status (body
mass index [BMI], American Society of Anesthesiologists (ASA) score ≥III) and surgical
relevance (urgency, surgical complexity),
which could be potentially influenced by the insurance status. Inclusion of variables
was determined by expected influence for insurance status and occurrence of complications
through the literature, significant differences in first descriptive analysis and
expert decision (SW, SG, MB). Created with BioRender.com.
Methods
Patients
Data from consecutive patients undergoing surgical
procedures at a tertiary referral hospital in Switzerland was collected prospectively
between September 2016 and March 2018 as part of the StOP?-trial (NCT02428179) [11].
In the original multicentre trial, a protocol
for structured pre-surgical communication was tested for influences on surgical
parameters, however, without significant effect for surgical site infection. For
the present study, data of one participating centre (Triemli Hospital, Switzerland)
was used with a focus on patients’ insurance status. Further information about included
patients (demographic and surgical parameters) was obtained from the clinic-internal
digital patient file system. The study was approved by the local ethics committee
before initiation (ID 2020-00265), and general consent was required for the analysis.
The study size depended on the collective of the StOP?-trial of one centre (Triemli
hospital).
Inclusion and exclusion criteria
Patients aged over 16 years undergoing surgery
(elective or emergency) in the abdominal, thoracic or vascular surgical department
were included in this study from the StOP?-trial (appendix table S1). This included
patients
with a highly unfavourable prognosis at the time of admission (multiorgan failure
in septic conditions, life-threatening abdominal complications after complex cardiac
surgery, aortic aneurysm rupture, mesenteric ischaemia or other life-threatening
thromboembolic conditions) despite their imminent risk of death within 72 hours,
however without procedures of deliberate termination. Excluded were low-complexity
surgeries, like the opening of a subcutaneous abscess as well as endovascular interventions
and thyroid surgeries, due to their very low degree of surgical site infection.
Additional reasons for exclusion were (b) withdrawal of general consent, (c) repeated
procedures, (d) errors in clinical documentation as well as (e) missing essential
data, such as age, body mass index (BMI) or duration.
Data collection
A summary of included variables is shown in
figure 1. Even though the StOP?-trial concentrated on surgical site infection as
the primary outcome [11], all complications were documented according to the
Clavien-Dindo classification (CDC) as well as other available parameters (e.g.
contamination of the surgical field) used in this analysis. Following the protocol
of the StOP?-trial, all included parameters were collected within 30 days post-surgery
by study nurses and validated independently. Collection of missing values and additional
demographic parameters (insurance status, age, BMI, American Society of Anesthesiologists
[ASA] classification, urgency and duration of surgery) was completed at time of
admission from internal electronic medical records.
Classification of surgical and demographic variables
All patients were separated by their insurance
status into basic insurance (mandatory, public) and additional supplementary insurance
(private) based on their system records. We categorised the surgical procedures
into six groups by their anatomical region
or similar surgical protocol: (a) upper gastrointestinal, (b) hepatic/biliary/pancreatic/splenic,
(c) colorectal, (d) hernia, (e) thoracic and vascular and (f) Other, which
included non-defined exploratory laparotomies or laparoscopies, nephrectomies or
endocrine surgery and lymph node excisions. Furthermore, surgeries were classified
as either “intermediate” or of “major complexity” according to the classification scheme
used by the National Institute for Health and Care Excellence (NICE) [12]. The group
of “intermediate complexity” surgeries was represented by
appendectomies, cholecystectomies, hernia surgeries and lymph node excisions. All
other surgeries were classified as surgeries of “major complexity”. Complications
were assessed by study nurses within
30 days post-surgery using the Clavien-Dindo classification [13]. All procedures were
classified into six categories:
free of complications (0), complications without required treatment (I), complications
with required pharmacological treatment (II), complications with requirement of
an intensified intervention (radiological, endoscopic or surgical) (III), life-threatening
complications (IV) and death (V). Additional assessed parameters of the intervention
were patient age in years, sex, BMI
in kg/m2, urgency (elective vs emergency) and duration of surgery in
minutes. The ASA classification was
used as a surrogate parameter to assess the patient’s morbidity, categorising all
patients with a few pre-existing diseases as low morbidity (ASA I–II) and those
with major pre-existing diseases as high morbidity (ASA III–V). The grade of surgical
wound contamination was classified
according to swissnoso (I to IV, clean to dirty-infected), corresponding to the
CDC’s surgical wound classification grades [14].
Outcomes
The primary outcome of this analysis was the
estimated treatment effect of supplementary insurance on the occurrence of complications
(outcome variable) in a comparable population. Furthermore, the association of potential
confounders on the occurrence of complications including surgical parameters such
as complexity, contamination and duration of surgery was assessed (figure 1).
Statistical analysis
Standard descriptive statistics were performed
for analysis of characteristics such as absolute and relative frequencies for categorical
variables and median with a 95% confidence interval (95% CI) for continuous variables.
For comparisons between basic and supplementary insured patients, Fisher’s exact
tests were used for nominal data and Mann-Whitney tests for continuous data. Two-sided
p-values <0.05 were considered statistically significant.
Since the limited access to a supplementary
insurance as well as many different demographic and surgical variables can have
a profound influence on the occurrence of complications, two different approaches
were used to obtain the estimated treatment effect as well as the adjusted association
of several variables (figure 1).
First, given that the endogenous diversity in
our sample of basic and supplementary insured can be attributed, in part, to the
selected access to a supplementary insurance, we used propensity score matching
to balance the probability of being in either insurance group [15]. The matching
variables were chosen according to their potential use in a randomisation protocol
of a clinical trial and as criteria relevant for the insurance selection process
from the perspective of an applicant from an insurance company [16]. Demographic
variables (age, sex, BMI, comorbidities in the form of the ASA classification, and
urgency) were therefore included for matching. Besides these variables, surgical
complexity was used in addition to demographic variables as it could be shown to
be a helpful variable to balance patient characteristics of different included surgeries
(table S2) and therefore allowing a reduction of their heterogeneity for the estimated
treatment effect after matching (appendix figure S1). Furthermore, the complexity
also influences
the choice of insurance status, e.g. through the aim of freely choosing a certain
doctor, making it even more important as a matching variable. With these matching
variables, a propensity score was calculated by logistic regression, estimating
the probability of each patient being in either the treatment or the control group
based on the observed covariates.
We used the R package matchit [15] with
the implemented “1:1 matching” and “nearest” approach for the necessary calculations.
Using 1:1 matching, our model aimed for a straightforward interpretation and increased
comparability. Standardised mean differences (SMD) were used as a balance measure
indicating the success of balancing in matched with a value of <0.1 (table 1)
[17]. However, 1:1 matching led to a substantial reduction in number of patients
with basic insurance, creating potential concerns about reduced generalisability
and robustness. The chosen matching approach was therefore compared to a weighted
“full matching” approach as well as a propensity score-based sensitivity analysis
in a regression model with the treatment variable and propensity score as an independent
variable. For the “full matching”, all procedures were matched with the implemented
function in the matchit package by creating different weights from the observed
matching covariates. Without dropping procedures through 1:1 or k:1 matching, full
matching allows compensation of disadvantages and can achieve balance without dropping
procedures [18]. We used standardised mean differences as well as estimations of
the treatment effect on outcome and surgical variables for comparing the described
matching approaches (table S3 and figure S2). The reduction of standardised
mean difference <0.1 was assumed as a sufficient balancing of either approach
[17]. Comparable estimations of the treatment effect for outcome and surgical variables
between propensity score-based sensitivity analysis, 1:1 and full matching approaches
suggest a robustness of the results despite a loss of numbers in the 1:1 matching
(table S3). Based on these results, 1:1 matching was chosen for the implantation
in our main analysis owing to its advantages in interpretation.
Second, multiple logistic regression was performed
to assess associations of the insurance status, demographic and surgical variables
with the occurrence of complications as shown in figure 1. The pre-defined inclusion
as potential confounders was based on their significant differences in descriptive
analysis, literature research of previous studies [7, 9, 11] or expert decision
(SW, SG, MB). Crude and adjusted odds ratios (OR) as well as their 95% CI were reported
for both, unmatched and 1:1 matched samples (figure
3). The multiple regression model
of the matched samples included matching variables in order to account for differences
remaining after matching [19].
The statistical environment R (version 4.1.2)
/ R Studio (version 2024.12.1+563) (session information in supplementary
information) and PRISM (version 10.4.1)
were used for statistical and graphical analyses.
Ethics
All procedures performed in studies involving
human participants complied with ethical standards of the institutional and/or national
research committee and with the 1964 Helsinki Declaration and its later amendments
or comparable ethical standards. This study was approved before its initiation by
the local ethics committee (ID 2020-00265).
Informed consent was obtained from all individual participants included in
the study, where appropriate.
Results
Analyses of demographic and surgical parameters before
and after matching
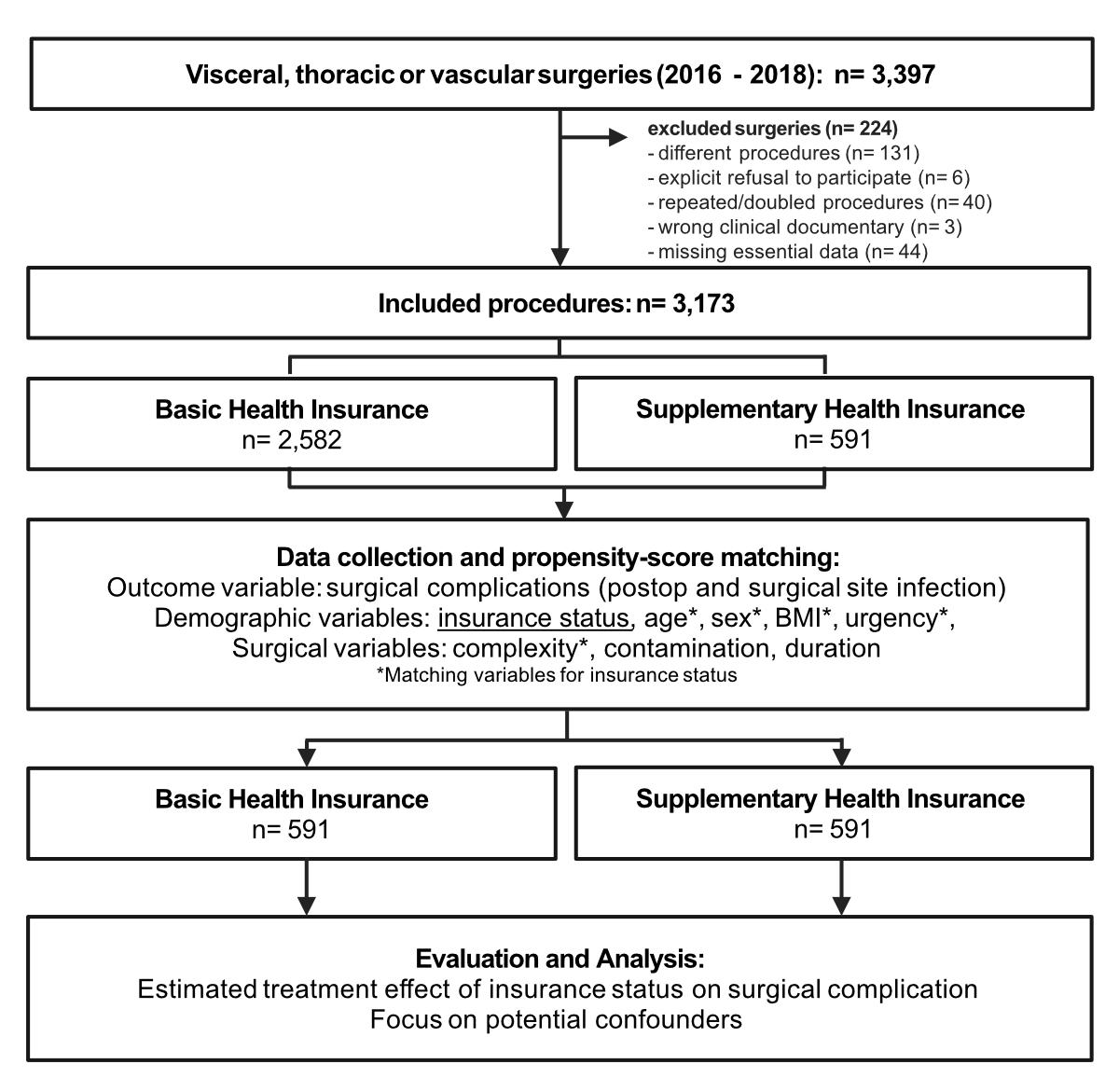
A total of 3397 surgeries meeting the inclusion
criteria were identified (figure 2). Of these 3397 surgeries, 224 were excluded,
giving a final number of 3173 interventions included in the study. Of these, 2645
(83.3%) were abdominal (8.5% upper gastrointestinal, 19.9% hepatic/biliary/pancreatic/
splenic, 20.9% colorectal, 25.3% hernia surgeries) and 528 (16.6%) were thoracic
or vascular surgeries (table S1).
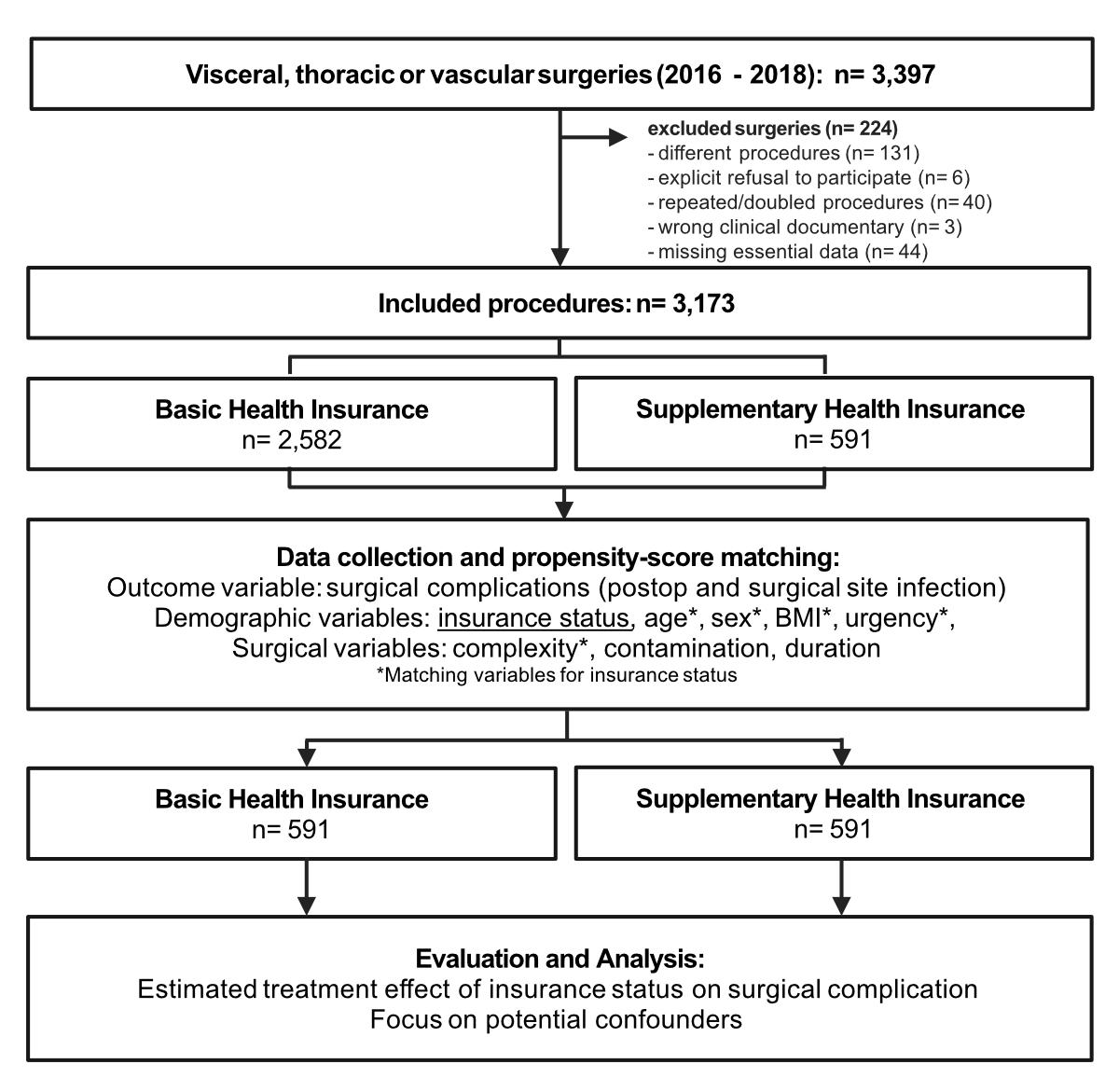
Figure 2Flowchart of study design. Shown
is a summary of included and excluded procedures. After exclusion, 3173 procedures
were analysed, including 2582 with basic health insurance and 591 with supplementary
health insurance. Created with BioRender.com.
In the unmatched population, 2582 (81.4%) had
basic insurance and 591 (18.6%) had supplementary insurance (table 1). Overall,
the median age was 61 years (IQR: 44–73); 1830 were male (57.7%) and 1343 were female
(42.3%). The median BMI for all patients was 25 (IQR: 22–29). The surgeries
were approximately evenly divided between those of “major complexity” (48.2%; n
= 1530) and “intermediate complexity” (51.8%; n = 1643). Two-thirds of surgeries (64.3%;
n = 2039) were electively
planned and 1134 (35.7%) were emergency procedures. One-third (34.0%; n = 1080)
of all patients had major pre-existing diseases with high morbidity (ASA score ≥3).
Interestingly, a significantly higher number of patients with supplementary insurance
had a pre-existing high morbidity (40.0% vs 32.6%). Patients with supplementary
insurance were older: 69 years (IQR: 56–76) vs 59 years (IQR: 42–72). The median
BMI was lower in patients with supplementary insurance: 25.0 (IQR: 23–29) vs 24
(IQR: 22–28). There was an increased rate of “major complexity” surgeries in patients
with supplementary insurance (45.8% vs 58.7%). There were no sex differences between
the basic and supplementary groups. The differences in standardised mean difference
were shown before and after matching by the matching variables. After 1:1 matching,
591 procedures of each insurance status were compared with improved balance, suggested
by the standardised mean difference <0.1 (table 1).
Table 1Demographic and surgical parameters
before and after propensity-score matching. Age and BMI are shown as median with IQR
(interquartile
range); all other categories are shown as counts and %.
| |
Unmatched sample |
Matched sample * |
| Basic |
Supplementary |
Standardised mean
difference (SMD) |
Basic |
Supplementary |
Standardised mean
difference (SMD) |
| Independent variable |
Health insurance |
2582 (81.4) |
591 (18.6) |
|
591 (50.0) |
591 (50.0) |
|
| Matching variables |
*Age in years |
59 (42–72) |
69 (56–76) |
0.477 |
67 (55–78) |
69 (56–76) |
0.004 |
| *Sex: male |
1498 (58.0) |
332 (56.2) |
0.037 |
341 (57.7) |
332 (56.2) |
0.031 |
| *BMI in kg/m2 |
25 (23–29) |
24 (22–28) |
0.219 |
25 (22–28) |
24 (22–27) |
0.026 |
| *Elective cases |
1637 (63.4) |
402 (68.0) |
0.099 |
399 (67.5) |
402 (68.0) |
0.011 |
| *ASA-score ≥III |
|
843 (32.6) |
237 (32.6) |
0.152 |
237 (40.1) |
237 (40.1) |
0.000 |
| ASA I+II |
1739 (67.4) |
354 (59.9) |
|
354 (59.9) |
354 (59.9) |
|
| ASA III |
784 (30.4) |
226 (8.2) |
|
220 (37.2) |
226 (38.2) |
|
| ASA IV |
55 (2.1) |
9 (1.5) |
|
14 (2.4) |
9 (1.5) |
|
| ASA V |
4 (0.1) |
2 (0.3) |
|
3 (0.5) |
2 (0.3) |
|
| *Surgical complexity: major |
1183 (45.8) |
347 (58.7) |
0.262 |
355 (60.1) |
347 (58.7) |
0.028 |
Surgery complication rate, duration and contamination
by insurance status
In total, postsurgical complications occurred
in 964 (30.4%) of all interventions without PS-matching (table 2). Patients with
supplementary insurance had an increased rate of overall postsurgical complications
compared to patients with basic insurance (29.2% vs 35.5%, p = 0.003). The most
relevant difference between basic and supplementary insurance was detectable in
the CDC II group (5.3% vs 8.3%) with a minor difference in mortality (1.8%
vs 2.9%).
In the matched sample, there was no significant
difference in occurrence of complications (35.5% vs 36.2%, p = 0.86). We did not
detect a relevant difference in mortality in the matched sample neither (3.2% vs
2.9%). As shown in table 2, surgeries of patients with supplementary insurance were
shorter compared to their matched procedures (95 min [IQR: 62–172] vs 90 min [IQR:
50–165]; p = 0.005). The number of surgeries with increased contamination was not
significantly different between basic and supplementary insured patients.
Table 2Analysis of surgical complications,
contamination and duration separated by complexity. Complications, assessed by the
Clavien-Dindo classification (CDC), and contamination, assessed by degree (I–IV),
are shown as counts and %, while duration is shown as medians with IQR (interquartile
range).
| |
Unmatched sample |
Matched sample* |
| Basic |
Supplementary
insurance |
p-value** |
Basic |
Supplementary
insurance |
p-value** |
| All
complexities*** |
No
complications |
1828 (70.8) |
381 (64.5) |
0.003 |
377 (63.8) |
381 (64.5) |
0.86 |
| All complications |
|
754 (29.2) |
210 (35.5) |
214 (36.2) |
210 (35.5) |
| CDC I |
341 (13.2) |
85 (14.4) |
|
92 (15.6) |
85 (14.6) |
|
| CDC II |
138 (5.3) |
49 (8.3) |
|
39 (6.6) |
49 (8.3) |
|
| CDC III |
184 (7.1) |
52 (8.8) |
|
47 (8.0) |
52 (8.8) |
|
| CDC IV |
45 (1.7) |
7 (1.2) |
|
17 (2.9) |
7 (1.2) |
|
| CDC V (death) |
46 (1.8) |
17 (2.9) |
|
19 (3.2) |
17 (2.9) |
|
| CDC low (I–II) |
479 (63.5) |
134 (63.8) |
0.99 |
131 (61.2) |
134 (63.8) |
0.62 |
| CDC high (III–V) |
275 (36.5) |
76 (36.2) |
83 (38.8) |
76 (36.2) |
| Duration in min |
85 (55–144) |
90 (50–165) |
0.78 |
95 (62–172) |
90 (50–165) |
0.005 |
| Contamination (II–IV) |
1509
(58.5) |
341
(57.7) |
0.75 |
341 (57.7) |
341 (57.7) |
0.99 |
| Intermediate complexity*** |
No complications |
1190
(85.1) |
208
(85.2) |
0.99 |
191 (80.9) |
208 (85.2) |
0.22 |
| All complications |
|
209
(14.9) |
36
(14.8) |
45 (19.1) |
36 (14.8) |
| CDC I |
118
(8.4) |
19 (7.8) |
|
21 (8.9) |
19 (7.8) |
|
| CDC II |
24 (1.7) |
6 (2.5) |
|
4 (1.7) |
6 (2.5) |
|
| CDC III |
53 (3.8) |
9 (3.7) |
|
13 (5.5) |
9 (3.7) |
|
| CDC IV |
8 (0.6) |
0 (0.0) |
|
5 (2.1) |
0 (0.0) |
|
| CDC V (death) |
6 (0.4) |
2 (0.8) |
|
2 (0.8) |
2 (0.8) |
|
| CDC low (I–II) |
142
(67.9) |
25
(69.4) |
0.99 |
25 (55.6) |
25 (69.4) |
0.25 |
| CDC high (III–V) |
67
(32.1) |
11
(30.6) |
20 (44.4) |
11 (30.6) |
| Duration in minutes |
65 (50–95) |
55 (40–75) |
<0.001 |
65 (50–94) |
55 (40–75) |
<0.001 |
| Contamination (II–IV) |
736
(52.6) |
118
(48.4) |
0.24 |
112 (47.5) |
118 (48.4) |
0.86 |
| Major complexity*** |
No complication |
638
(55.3) |
173
(50.9) |
0.15 |
186 (52.4) |
173 (49.9) |
0.54 |
| All complications |
|
515
(44.7) |
167
(49.1) |
169 (47.6) |
174 (50.1) |
| CDC I |
223
(19.3) |
66
(19.4) |
|
71 (19.4) |
66 (19.0) |
|
| CDC II |
114
(9.9) |
43
(12.7) |
|
35 (10.3) |
43 (12.4) |
|
| CDC III |
131
(11.4) |
43
(12.7) |
|
34 (12.6) |
43 (12.4) |
|
| CDC IV |
7 (0.6) |
0 (0.0) |
|
12 (4.4) |
7 (2.0) |
|
| CDC V (death) |
40 (3.5) |
15 (4.4) |
|
17 (3.8) |
15 (4.3) |
|
| CDC low (I–II) |
337
(61.8) |
65
(62.6) |
0.86 |
106 (62.7) |
109 (62.6) |
0.99 |
| CDC high (III–V) |
208
(38.2) |
66
(37.4) |
63 (37.3) |
65 (37.4) |
| Duration in minutes |
136 (80–225) |
140 (80–222) |
0.88 |
146 (90–235) |
140 (80–222) |
0.33 |
| Contamination (II–IV) |
773
(65.4) |
223
(64.3) |
0.75 |
229 (64.5) |
223 (64.3) |
0.99 |
Surgical complications, contamination and duration
separated by insurance status and surgical complexity
In the matched population, the surgical complexity
was evenly distributed in both insurance groups. In total, 480 (40.6%) interventions
were of intermediate complexity,
while 702 (59.4%) were of major complexity.
Based on the higher frequency of major complexity surgeries, we analysed both groups
of surgical complexity separately
(table 2). Of all 424 complications, 81 (19.1%) appeared in surgeries of intermediate
complexity and 343 (80.9%) in
those of major complexity. Separated
by their surgical complexity and
insurance status, there was a substantial but non-significant trend of reduced occurrence
of complications for patients with supplementary insurance with surgeries of intermediate
complexity (intermediate basic: 45
[19.1%] vs supplementary: 36 [14.8%], p = 0.22). There was no significant difference
in occurrence of complications in the group with major complexity (major basic: 169
[47.6%] vs supplementary 174 [50.1%],
p = 0.54). There were no relevant differences within the grades of complications
or between low- and high-risk complications (CDC I–II vs CDC III–V). The observed
difference in duration of surgery in combined complexity was even more pronounced
in the matched intermediate complexity group (basic: 65 min [IQR: 50–94] vs supplementary:
55 min [IQR: 40–75], p <0.001) without statistical significance in procedures
of major complexity. There was no difference in surgical contamination, either if
separated by the surgical complexity nor
in the overall group.
Estimated treatment effect of insurance status on complication
rate and other variables
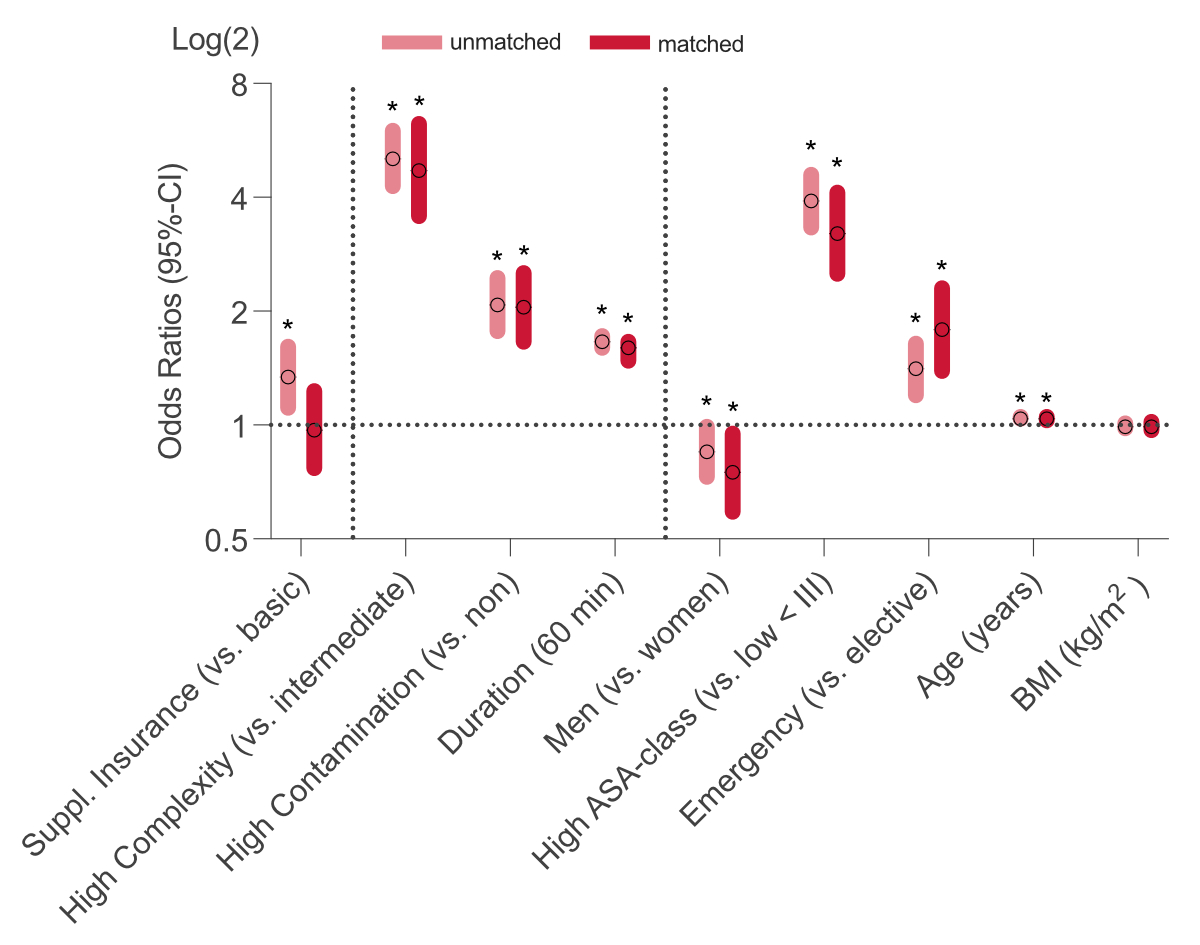
To determine the estimated treatment effect
of insurance status, we compared odds ratios between unmatched and matched samples
of the occurrence of complications (outcome variable) including treatment, surgical
and demographic variables
(figure 3). It was possible to show a change from a significant estimated treatment
effect of insurance status (crude OR [95% CI]: 1.34 [1.11–1.61], p = 0.003) to no
significance by matching (crude OR [95% CI]: 0.97 [0.77–1.23], p = 0.81). There
was no relevant influence of matching on the odds ratios of other variables. The
most pronounced associations with the occurrence of complications were major surgical
complexity (crude OR [95% CI]: 5.06 [4.28–6.00], p <0.001), an increased ASA
classification (crude OR [95% CI]: 3.91 [3.33–4.59], p <0.001) and increased
contamination (crude OR [95% CI]: 2.08 [1.77–2.45], p <0.001).
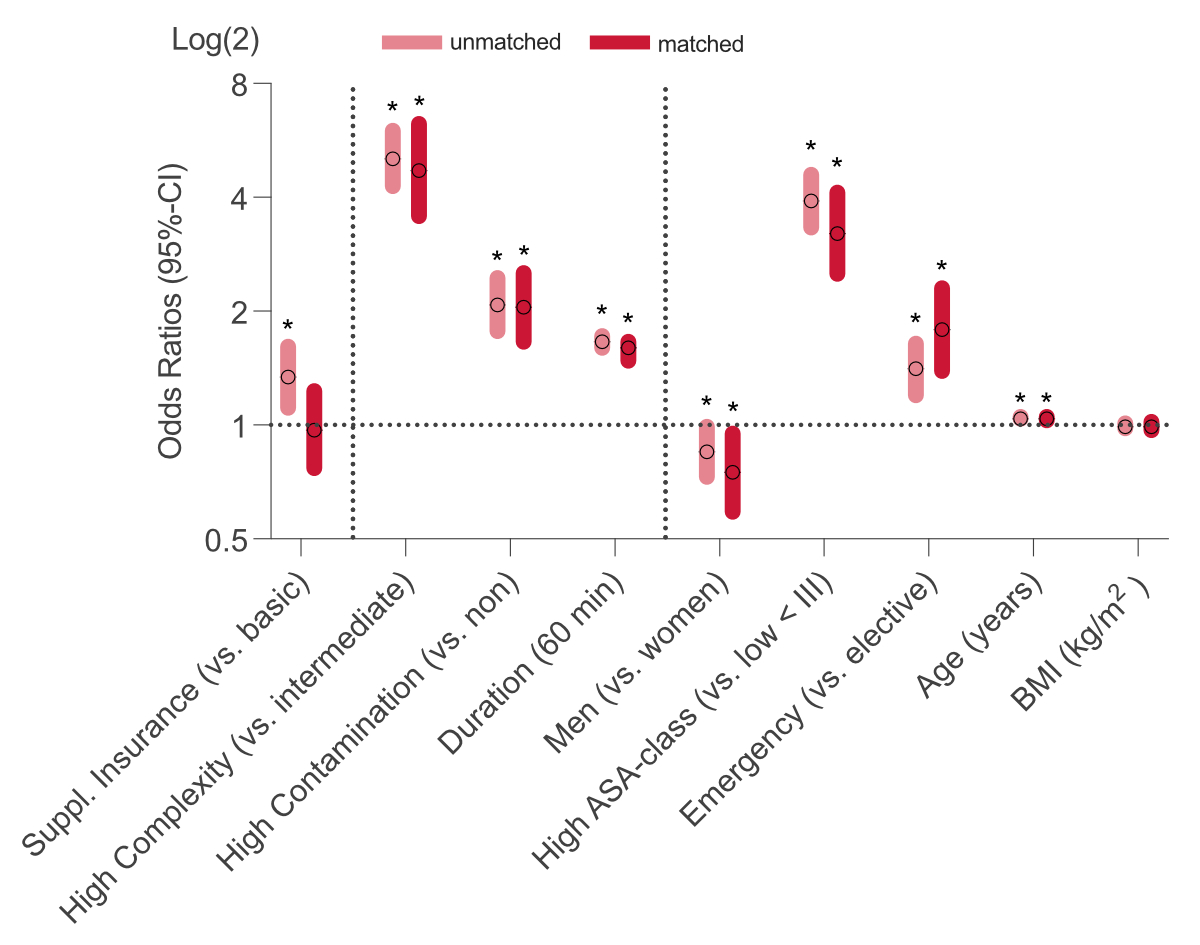
Figure 3Influence of the treatment (supplementary
insurance) and other variables on the occurrence of complications in unmatched and
matched samples. Shown are associations in odds ratios and 95% confidence interval
(CI) of treatment (insurance status), surgical variables (complexity, contamination,
duration) and demographic variables (sex, American Society of Anaesthesiology [ASA]
classification, urgency, age and body mass index [BMI])
on the occurrence of complications in unmatched (pink) and matched (red) samples.
Statistical significance was set at p <0.05 and is indicated with an
asterisk (*). Analysed variables were included by their expected significance in
first descriptive analysis and expert decision. Binary variables were compared to
a reference level as indicated beside the group.
Association of insurance status, demographic and surgical
variables with occurrence of complications
Based on
the potential confounding of included variables on the occurrence of complications,
multiple logistic regression analyses were performed on
unmatched and matched samples, adjusting for treatment, surgical and demographic
variables (table 3). Similar to the
matching, adjustment for confounding showed no remaining association of insurance
status in the unmatched and matched samples. The following descriptions focus on
associations from the matched sample as both the unmatched and matched samples showed
similar trends after adjustment.
Table 3Logistic regression analyses
of complications of unmatched and propensity-matched surgeries for potential confounding.
| |
Unmatched sample* |
1:1 Matched sample* |
| Unadjusted** |
Adjusted*** |
Unadjusted** |
Adjusted*** |
| Odds ratio (95% CI) |
p-value |
Odds ratio (95% CI) |
p-value |
Odds ratio (95% CI) |
p-value |
Odds ratio (95% CI) |
p-value |
| Treatment variable |
Supplementary insurance (vs basic) |
1.34 (1.11–1.61) |
0.003 |
1.02 (0.81–1.27) |
0.88 |
0.97 (0.77–1.23) |
0.81 |
1.04 (0.79–1.38) |
0.77 |
| Surgical variables |
Major surgical complexity (vs intermediate) |
5.06 (4.28–6.00) |
<0.001 |
2.05 (1.66–2.52) |
<0.001 |
4.71 (3.57–6.26) |
<0.001 |
1.80 (1.27–2.56) |
0.001 |
| Increased contamination (vs non) |
2.08 (1.77–2.45) |
<0.001 |
1.56 (1.28–1.90) |
<0.001 |
2.50 (1.95–3.24) |
<0.001 |
1.90 (1.41–2.56) |
<0.001 |
| Duration in minutes |
1.011 (1.01–1.012) |
<0.001 |
1.008 (1.007–1.009) |
<0.001 |
1.01 (1.008–1.011) |
<0.001 |
1.008 (1.006–1.009) |
<0.001 |
| Matching variables |
Men (vs women) |
0.85 (0.73–0.99) |
0.04 |
0.89 (0.75–1.07) |
0.22 |
0.75 (0.59–0.95) |
0.02 |
0.82 (0.62–1.08) |
0.16 |
| High ASA score (vs low <III) |
3.91 (3.33–4.59) |
<0.001 |
1.56 (1.27–1.91) |
<0.001 |
3.21 (2.51–4.12) |
<0.001 |
1.57 (1.15–2.13) |
0.004 |
| Emergency (vs elective procedure) |
1.41 (1.20–1.64) |
<0.001 |
1.87 (1.54–2.28) |
<0.001 |
1.79 (1.39–2.30) |
<0.001 |
2.14 (1.59–2.91) |
<0.001 |
| Age in years |
1.04 (1.04–1.05) |
<0.001 |
1.03 (1.02–1.03) |
<0.001 |
1.04 (1.03–1.05) |
<0.001 |
1.03 (1.02–1.04) |
<0.001 |
| BMI in kg/m2 |
0.99 (0.98–1.01) |
0.66 |
0.99 (0.97–1.01) |
0.30 |
0.99 (0.97–1.02) |
0.56 |
0.99 (0.96–1.02) |
0.48 |
After adjustment, surgical variables such as
major surgical complexity (adjusted
OR [95% CI]: 1.80 [1.27–2.56], p <0.001), high surgical contamination (adjusted
OR [95% CI]: 1.90 [1.41–2.56], p <0.001) and surgical duration (adjusted OR [95%
CI]: 1.008 [1.006–1.009], p <0.001) remained significantly associated with the
occurrence of surgical complication. Adjustment for demographic variables showed
that a high (≥III) ASA classification (OR [95% CI]: 1.57 [1.15–2.13], p = 0.004),
an
emergency (OR [95% CI]: 2.14 [1.59–2.19], p <0.001) and higher age (OR [95%
CI]: 1.03 [1.02–1.04], p <0.001) were positively associated with the occurrence
of complications. Urgency is the only variable whose association increased after
adjustment (crude OR: 1.79 vs adjusted OR: 2.14). Male sex had a significant association
with a reduced occurrence of complications in the univariate analysis (OR [95%
CI]: 0.75 [0.59–0.95], p = 0.02) without significant association after adjustment
(OR [95% CI]: 0.82 [0.62–1.08], p = 0.16). There was no association between the
BMI and occurrence of complication throughout the analyses.
Discussion
This study provides data
concerning overall complications of surgical
patients undergoing abdominal, thoracic
and vascular surgical interventions in relation to the patient’s insurance
status. We were able to investigate a large cohort of patients acquired prospectively
for 18 months. The cohort represents an average patient population and interventions
of a large Swiss hospital.
We found no evidence for an association between
supplementary insurance and reduced surgical complications. In the analysis of the
unmatched sample, patients with basic insurance had even fewer overall complications
than those with supplementary insurance. To investigate this initial finding, we
used propensity-score matching (PSM) to balance an endogenous diversity of demographic
parameters as we expected a selective access to supplementary imbalances and searched
for other possible confounders of the found association. We showed no significant
estimated treatment effect of a supplementary insurance in a balanced sample with
a comparable patient population. However, demographic parameters, as well as contamination
of the surgical wound according to the standards of swissnoso [14], complexity of
the performed surgeries adapted to the National Institute for Health and Care
Excellence (NICE) classification [12] and duration of surgery were found to be significantly
associated with the occurrence of surgical complications. We conclude therefore
that the statement of comparable standards in healthcare quality in general surgical
patients, regardless of the insurance status, remains valid.
Contextualisation of the study results within the Swiss
healthcare system
Intuitively, benefits regarding complication
rates from a supplementary insurance status in the Swiss healthcare system were
expected, while no such benefits were statistically measurable in this study. A
potential explanation could be that the Swiss healthcare system meets high quality
standards for all general surgical patients. Furthermore, intensive supervision
of surgical residents is standard to provide this quality, and if treatment exceeds
the resident’s experience, the threshold for attending doctors to intervene is low.
Therefore, the expected benefit of supplementary insurance is mainly the direct
care by an experienced attending doctor, which is eliminated by the described intensive
supervision.
In this study, it was impossible to measure
the impact of surgical experience in a statistically reliable manner, and reasoning
would remain hypothetical. However, adjusted to the surgical complexity and influences
such as the emergency status, our results showed no association between surgical
complications and insurance status. Therefore, we can agree with the conclusions
made by Schneider et al. and Duggan et al., which focused on the correlation between
surgical site infection or medical outcomes of oncological surgical procedures and
insurance status in the Swiss healthcare system [8–9]. In their studies, no negative
impact of basic insurance could be found either. In comparison to their studies, our analyses showed
results for a larger spectrum of complications and surgeries, better representing
the real-world situation. Funke et al. showed a significant increase in surgical
complications among trauma patients with basic insurance [7]. However, a direct
comparison of trauma and abdominal surgery remains speculative and can differ in
terms of complexity and variety of surgical procedures. Furthermore, as major surgeries
in the abdominal, thoracic or vascular field require a high level of interdisciplinary
cooperation, for example with intensive care medicine and complex post-operative
management, the number of complications could be less reliant on the experience of
the surgeon alone. Similar to our study,
Funke et al. did not find a difference in mortality associated with health insurance
status [7].
Association of included variables interfering with
the insurance status
Our results emphasise the importance of recognising
external influences when investigating insurance status. Matching our sample by
the probability to have access to a supplementary insurance through balanced co-variables
influenced the estimated treatment effect substantially. We found that age especially
was a relevant factor for the probability of being supplementary insured – which
has also been shown by Altwicker-Hamori [16]. Age is of special importance, as older
patients can be for example more likely to have a supplementary insurance and have
higher rate of ASA-associated physical status, associated with an increased occurrence
of complications. Those results are similar to Funke et al [7]. Another example
could be that supplementarily insured patients also had more surgeries with major
complexity, which was then associated
with a higher occurrence of complications. However, it is also likely that patients
with planned major surgery rely on supplementary insurance for the free choice of
doctors or hospital. In our perspective, it is therefore necessary to acknowledge
both influences, the selected access to health insurances as well as the potential
confounding of different demographic and surgical variables. For future studies,
we support considering other relevant demographic parameters such as education or
income. Another important association that should be considered for future studies
was the significant time reduction of surgeries for patients with supplementary
insurance similar to Schneider et al. and Duggan et al. [8–9]. This time reduction
was especially present within surgeries of intermediate complexity. Whether this result
was a simple expression of a more subtle
difference of complexity in surgery with an intermediate profile or that the surgery
performed by
a senior surgeon just took less time was not evident in our analysis. Our analyses
support that a prolonged duration of surgery, as a surrogate of a more challenging
surgery, was associated with an increased occurrence of complications. However,
we could not detect a significant reduction of complications along with the time
reduction of patients with supplementary insurance.
Generalisability of the study results
The patients themselves might expect a more
beneficial outcome for the additional cost of supplementary insurance. Several studies
in the US healthcare system show an evident difference with private/supplementary
healthcare plans [3–4]. The American system risks creating different classes in
medical treatment. But in contrast to the Swiss healthcare system and our study,
most US studies focus on patients with private health insurance and those without
insurance at all [20]. Especially in Switzerland, fundamental treatment is covered
by compulsory basic healthcare, and the increment to the therapy within a supplementary
healthcare plan is marginal regarding the medical quality [2]. Therefore, a significant
difference in medical treatment and outcome may be expected in the American healthcare
system but not in the universal coverage system of Switzerland. However, political
debates regarding the Swiss health insurance system are omnipresent in Swiss politics.
The fear of a two-tier medical system is a recurring argument in such debates. At
this point, our study indicates no evidence for a two-tier medical system in Switzerland
regarding surgical treatment.
There is also the probability that benefits
offered by supplementary insurances in Switzerland might influence the intended
medical outcome without being reflected by the complication rate. Complications
of surgical patients can only be a surrogate marker for treatment quality but are
not the same as the intended medical outcome, for example the overall survival in
cancer patients. There might be many connections between complications and medical
outcomes without absolute certainty that overcoming complications may affect the
medical outcome. Furthermore, the quality of the management of surgical complications
may outweigh the original impact of the complication.
Limitations
This study is limited in its conclusion as there
is no general definition of medical outcome, and investigations require the assessment
of different surrogate parameters, such as surgical site infection or postsurgical
complications. Thus, making final statements about causality can be challenging
after all and requires comprehensive future guidance to improve robust definitions
which can be summarised in research, such as meta-analyses.
There are different possibilities of selection
biases inherent through the study design. First, this study is limited to the data
of the initial StOP?-trial, which was not randomised, and accumulates a further
selection bias through the focus on one centre and higher complexity surgery. However,
similar to the StOP?-trial, our study tried to increase the generalisability by
a broad inclusion and restricted exclusion. While the inclusion of many different
surgery types can lead to heterogeneity, we tried to minimise it through categorisation
into intermediate and high complexity, matching and statistical adjustment, with
the purpose of reducing the influences of heterogeneity on the outcome variable
(figure S1). Including surgeries typical for a department of abdominal, thoracic
and vascular surgery, we hope to allow increased generalisability and comparison
to a typical Swiss tertiary referral centre. However, it is important to encourage
further studies to focus on a comparison within separate surgery types. Second,
we experienced a high endogenic heterogeneity of patients with basic and supplementary
insurance. We tried to reduce this imbalance and increase plausibility through the
use of propensity-score matching. As already stated in the methods, 1:1 matching
can lead to a selection bias by dropping important residues during the matching
process. In our study, the experienced bias was limited as we could show robustness
of our matching through sensitivity analysis (figure S2 and table S3). However,
there will always be a risk for residual and unmeasured confounding, as the matching
uses a retrospective approach based on observed variables. Third, patients were
excluded when data was missing to simplify the analysis, creating a potential for
selection bias and unknown confounding. It is therefore important to point out that
our results aim not for causality but to reflect associations of treatment on the
outcome translatable to a comparable cohort. Propensity-score matching cannot substitute
for prospective randomisation and a multicentric view to allow casual conclusions
and increased generalisability.
As our study data was limited by the framework
of the StOP?-trial, we want also to address the need for further investigations
of important parameters such as Comprehensive Complication Index (CCI) or surgical
experience, which could not be assessed in this study.
Conclusion
We demonstrated evidence that insurance status
is not associated with surgical complications of abdominal, thoracic and vascular
surgeries within the Swiss healthcare
system. The duration of surgery of intermediate complexity did differ significantly
in favour of patients with supplementary insurance. Nevertheless, basic insurance
status did not increase significantly the occurrence of surgical complications in
a comparable cohort.
Data sharing statement
Upon reasonable request, individual data or codes that support results can be shared
with necessary adjustments for deidentification, ending after 48 months following
publication.
Requests must be approved by the corresponding author as well as an independent
committee for measures of ethical approval.
Acknowledgments
We want to thank for all involved support, especially
Prof. Ulrike Held and Dr Leo Schmallenbach for their help and critical comments.
Author contributions: Study conception and design: SW, LB, SG.
– Acquisition of data: MB, SW, SG, LB, CZ. – Analysis and interpretation of data:
MB, SW, SG. – Drafting of manuscript: MB. – Critical revision of manuscript: All
mentioned authors.
Dr med. Maximilian Bley, MSc
Chair
for Gender Medicine
University
of Zurich
Wagistrasse
12
CH-8952
Schlieren
maximilian.bley[at]uzh.ch
References
1. Swiss Federal Council, Botschaft über die Revision der Krankenversicherung. 1991.
2. Paccagnella O, Rebba V, Weber G. Voluntary private health insurance among the over
50s in Europe. Health Econ. 2013 Mar;22(3):289–315. doi: https://doi.org/10.1002/hec.2800
3. Veltre DR, Sing DC, Yi PH, Endo A, Curry EJ, Smith EL, et al. Insurance Status Affects
Complication Rates After Total Hip Arthroplasty. J Am Acad Orthop Surg. 2019 Jul;27(13):e606–11.
doi: https://doi.org/10.5435/JAAOS-D-17-00635
4. Williams DM, Thirukumaran CP, Oses JT, Mesfin A. Complications and Mortality Rates
Following Surgical Management of Extradural Spine Tumors in New York State. Spine.
2020 Apr;45(7):474–82. doi: https://doi.org/10.1097/BRS.0000000000003294
5. Goodair B, Reeves A. The effect of health-care privatisation on the quality of care.
Lancet Public Health. 2024 Mar;9(3):e199–206. doi: https://doi.org/10.1016/S2468-2667(24)00003-3
6. Manoso MW, Cizik AM, Bransford RJ, Bellabarba C, Chapman J, Lee MJ. Medicaid status
is associated with higher surgical site infection rates after spine surgery. Spine.
2014 Sep;39(20):1707–13. doi: https://doi.org/10.1097/BRS.0000000000000496
7. Funke L, Canal C, Ziegenhain F, Pape HC, Neuhaus V. Does the insurance status influence
in-hospital outcome? A retrospective assessment in 30,175 surgical trauma patients
in Switzerland. Eur J Trauma Emerg Surg. 2022 Apr;48(2):1121–8. doi: https://doi.org/10.1007/s00068-021-01689-x
8. Schneider MA, Rickenbacher A, Frick L, Cabalzar-Wondberg D, Käser S, Clavien PA, et
al. Insurance status does not affect short-term outcomes after oncological colorectal
surgery in Europe, but influences the use of minimally invasive techniques: a propensity
score-matched analysis. Langenbecks Arch Surg. 2018 Nov;403(7):863–72. doi: https://doi.org/10.1007/s00423-018-1716-8
9. Duggan BT, Roth JA, Dangel M, Battegay M, Widmer AF. Impact of health insurance status
on surgical site infection incidence: A prospective cohort study. Infect Control Hosp
Epidemiol. 2019 Sep;40(9):1063–5. doi: https://doi.org/10.1017/ice.2019.195
10. Sagan A, Thomson S, editors. Voluntary health insurance in Europe: Country experience.
Copenhagen, Denmark; 2016.
11. Tschan F, Keller S, Semmer NK, Timm-Holzer E, Zimmermann J, Huber SA, et al. Effects
of structured intraoperative briefings on patient outcomes: multicentre before-and-after
study. Br J Surg. 2021 Dec;109(1):136–44. doi: https://doi.org/10.1093/bjs/znab384
12. NICE. Routine preoperative tests for elective surgery, Guideline [NG45]National Institute
for Health and Care Excellence; 2016.
13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new
proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann
Surg. 2004 Aug;240(2):205–13. doi: https://doi.org/10.1097/01.sla.0000133083.54934.ae
14. Ruef, C., M.C. Eisenring, and N. Troillet, Erfassung postoperativer Wundinfektionen.
Nationales Programm durchgeführt von Swissnoso im Auftrag des ANQ, 2013.
15. Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential
outcomes: concepts and analytical approaches. Annu Rev Public Health. 2000;21(1):121–45.
doi: https://doi.org/10.1146/annurev.publhealth.21.1.121
16. Altwicker-Hámori S, Stucki M. Factors associated with the choice of supplementary
hospital insurance in Switzerland - an analysis of the Swiss Health Survey. BMC Health
Serv Res. 2023 Mar;23(1):264. doi: https://doi.org/10.1186/s12913-023-09221-0
17. Kuss O. The z-difference can be used to measure covariate balance in matched propensity
score analyses. J Clin Epidemiol. 2013 Nov;66(11):1302–7. doi: https://doi.org/10.1016/j.jclinepi.2013.06.001
18. Heinz P, Wendel-Garcia PD, Held U. Impact of the matching algorithm on the treatment
effect estimate: A neutral comparison study. Biom J. 2024 Jan;66(1):e2100292. doi: https://doi.org/10.1002/bimj.202100292
19. Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing
model dependence in parametric causal inference. Polit Anal. 2007;15(3):199–236. doi: https://doi.org/10.1093/pan/mpl013
20. Congress of the United States Congressional Budget Office, Federal Subsidies for Health
Insurance Coverage for People Under Age 65: 2019 to 2029. 2019.
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4179.