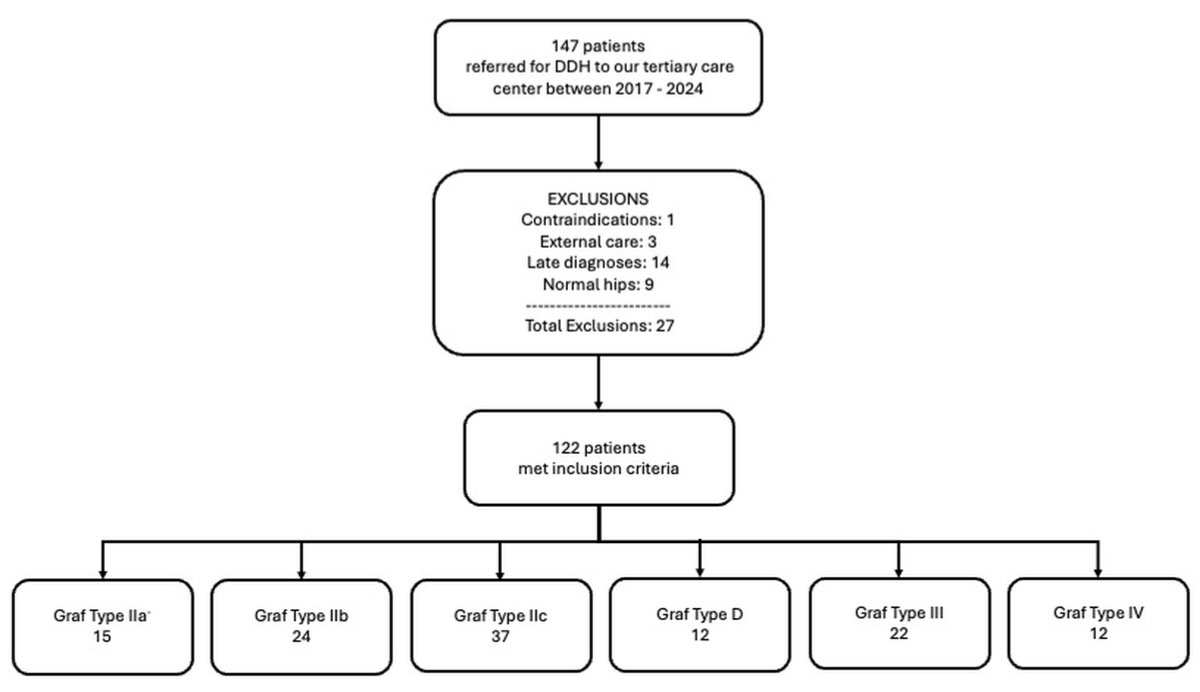
Figure 1Study data flow. DDH: developmental dysplasia of the hip.
DOI: https://doi.org/https://doi.org/10.57187/s.4077
Developmental dysplasia of the hip is one of the most frequent congenital skeletal diseases, with an incidence ranging between 1 and 20 per 1000 infants depending on the population and region. This variation reflects differences in diagnostic criteria, screening methods and population characteristics [1].
Developmental dysplasia of the hip encompasses a wide range of conditions, from a stable hip with mild acetabular dysplasia to complete hip dislocation. If developmental dysplasia of the hip is not treated promptly, it can deteriorate and have a detrimental impact on the child’s normal development and healthy growth [2].
Before the introduction of ultrasound technology for neonatal hip assessments in the early 1980s, physical examination was the primary method used for screening. With time, ultrasound gradually gained prominence as the predominant method of screening for developmental dysplasia of the hip [2, 3]. Screening for developmental dysplasia of the hip has been debated for many years. In Europe, screening programmes are unregulated and vary widely. There is no agreement on whether hip ultrasound should be performed on all newborns (universal screening) or only in those with risk factors or clinical instability of the hip during clinical examination (selective screening) [4, 5]. Risk factors such as a positive family history, breech position and multiple gestation are considered in selective screening. However, most infants diagnosed with symptomatic developmental dysplasia of the hip do not exhibit any identifiable risk factors [6].
Furthermore, the optimal timing of when to perform ultrasound in the first weeks of life is not yet clear due to the high frequency of hip immaturities observed in the first 6–8 weeks of life which tend towards spontaneous resolution before the 12th week of life in almost 90% of cases. This leads to significant differences in the different screening programmes in Europe, making comparison studies difficult [7]. Table 1 summarises the different practices in Europe.
Table 1Screening programmes in Europe.
| Country | Screening type | Timing of ultrasound (weeks) |
| Austria | Universal | 6–8 |
| Belgium | Selective | <12 |
| England | Selective | 6 |
| France | Selective | <4 |
| Germany | Universal | 6–8 |
| Italy | Universal | 4–12 |
| Netherlands | Selective | 12 |
| Norway | Selective | 1 |
| Portugal | Selective | 6–8 |
| Slovakia | Universal | 1–12 |
| Sweden | Selective | 1–12 |
| German-speaking Switzerland | Universal | 4–6 |
| French-speaking Switzerland | Selective | 4–6 |
Despite the lack of benefit in terms of reducing the rates of late-detected cases in randomised clinical trials, universal ultrasound screening for developmental dysplasia of the hip has gained increasing popularity [4, 8]. The International Interdisciplinary Consensus Meeting on the evaluation of developmental dysplasia of the hip strongly supports that ultrasound screening is essential [9]. This is also supported by several studies, which highlight a discrepancy between clinical findings and ultrasound examination. Indeed, the literature confirms that ultrasound examination has a sensitivity of more than 90%, while clinical examination presents a sensitivity of less than 30% in some studies [10]. Clinical examination can detect instability but not dysplasia with a stable hip [9]. On the other hand, a Cochrane review published in 2013 did not show any long-term advantages of a universal screening programme [5].
Our study aimed to estimate the sensitivity of clinical screening for developmental dysplasia of the hip performed at a Swiss tertiary care centre.
This was a retrospective cohort study conducted at a tertiary paediatric orthopaedic care centre in Switzerland. The study included newborns aged between 0 and 120 days diagnosed with developmental dysplasia of the hip between May 2017 and June 2023.
Patient records were retrieved from the hospital’s electronic archived medical records.
Inclusion criteria were infants aged 0–120 days with a confirmed developmental dysplasia of the hip diagnosis (Graf type IIa to IV) based on hip ultrasound.
Patients with normal ultrasound findings (Graf type I), with neuromuscular diseases, referred from other hospitals or with a diagnosis made after 120 days of age were excluded.
Clinical examination results (Barlow, Ortolani, Galeazzi and limited abduction tests) were extracted from paediatric orthopaedic consultation records.
All clinical examinations had been carried out by the same senior consultant.
Hip ultrasound findings (Graf classification) were retrieved from radiology reports.
All ultrasound examinations were performed either by a paediatric radiologist or by the senior orthopaedic surgeon specialising in paediatric hip disorders, minimising variability in assessment.
Demographic variables and risk factors (breech position, family history, birth order) were recorded. The timing of developmental dysplasia of the hip diagnosis and treatment initiation were also documented.
A second reviewer (a paediatric orthopaedic specialist) verified data extraction for a subset of cases. Any missing or inconsistent data were flagged and addressed before statistical analysis.
The study period was chosen as the senior orthopaedic specialist has been present at this tertiary care centre since 2017, ensuring consistency in clinical assessments and diagnostic approaches. The sample included all patients treated at the centre since 2017, providing a comprehensive dataset reflecting real-world clinical practice.
The primary outcome of this study was the sensitivity of clinical screening for developmental dysplasia of the hip. Sensitivity was calculated as the proportion of patients with developmental dysplasia of the hip who had at least one positive clinical finding (Barlow, Ortolani, Galeazzi, limited abduction) compared to the reference standard of ultrasound diagnosis using the Graf method [11]. Sensitivity was analysed separately for stable hips (Graf IIa, IIb, IIc) and unstable hips (Graf D, III, IV).
For the statistical analysis, Pearson’s chi-square test was used to determine whether sensitivity significantly differed between stable and unstable hips. The t-test was used to determine whether the mean and median age at diagnosis differed for the diagnosis of stable vs unstable hips.
The study protocol was approved by the Ethics Review Committee (ID 2023-00787). The data and analysis code are available on request.
Of 149 infants referred for suspected developmental dysplasia of the hip, 27 were excluded for the following reasons: 9 had normal hips (Graf type I) confirmed on ultrasound, 1 had contraindications for clinical examination and 3 had initially been treated at other centres. Fourteen patients were excluded because they had surpassed 120 days of age at the time of their initial diagnosis. A total of 122 patients met the inclusion criteria and were analysed. Figure 1 shows their distribution across Graf categories. Most (84%) were female. Median age at diagnosis was 52 days (0–120). Among the included patients, 40% (49/122) had a breech presentation, 37% (45/122) had a positive family history of developmental dysplasia of the hip and 29% (35/122) were first-born children.
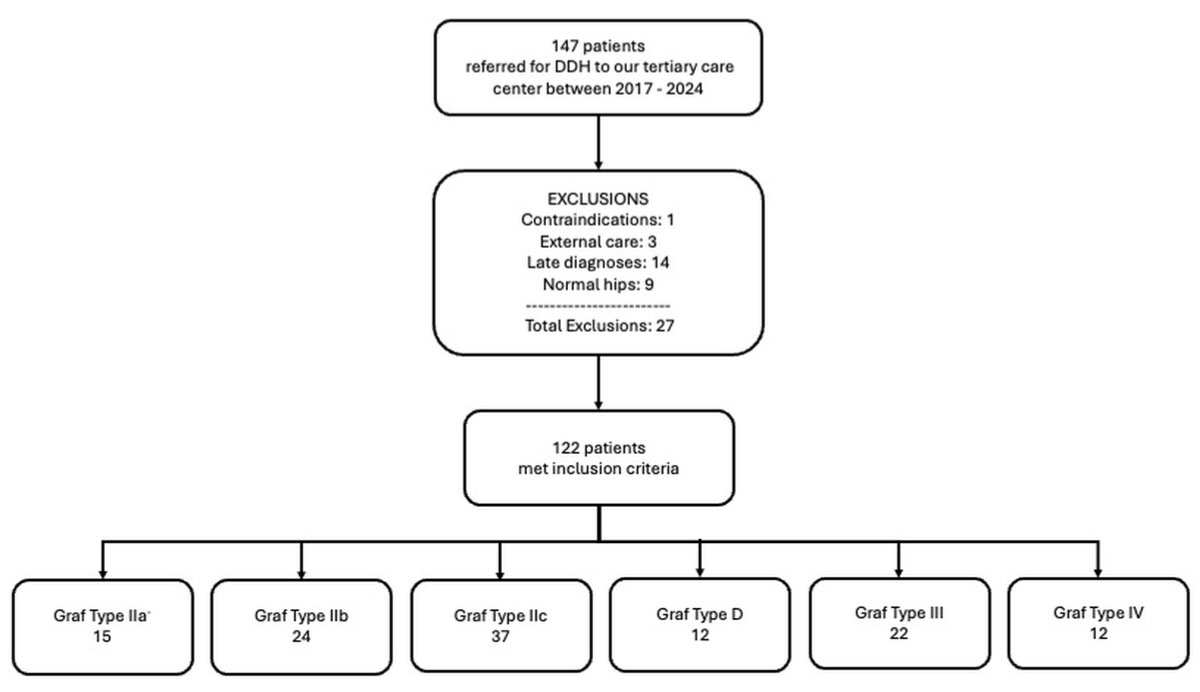
Figure 1Study data flow. DDH: developmental dysplasia of the hip.
Table 2 summarises the demographics of our study group according to the severity of developmental dysplasia of the hip. Clinical screening demonstrated an overall sensitivity of 66% (95% confidence interval [CI]: 58–74%). Sensitivity was higher for unstable hips (Graf types D, III, IV) than for stable hips (Graf types IIa, IIb, IIc): respectively, 91% (95% CI: 82–99%) and 50% (95% CI: 38–62%). The Pearson chi-square test confirmed a significant difference in sensitivity between stable and unstable hips (χ2 = 5.7114, p = 0.017). Among individual tests, limited abduction had the highest sensitivity (48%, 95% CI: 39–57%). Table 3 provides detailed test performance. Diagnosis was significantly delayed for stable hips compared to unstable hips. The mean age at diagnosis for stable hips was 59 days (range: 3–119 days), significantly different from the 41 days (range: 1–115 days) for unstable hips (t = 3.09, p = 0.001); the median age at diagnosis was 59.5 days and 44 days, respectively. Only 24% of stable hips were diagnosed and treated before 6 weeks of age, compared to 48% of unstable hips.
Table 2Demographic variables by Graf classification.
| Variable | Total (n = 122) | Graf IIa | Graf IIb | Graf IIc | Graf D | Graf III | Graf IV |
| n = 15 | n = 24 | n = 37 | n = 12 | n = 22 | n = 12 | ||
| Female (%) | 84% | 87% | 75% | 89% | 83% | 91% | 75% |
| Mean age at diagnosis, in days (min–max; standard deviation) | 52.6 (2–120; 32) | 56 (7–119; 24) | 80 (6–120; 25) | 47 (6–113; 30) | 38 (5–115; 38) | 42 (5–112; 29) | 43 (2–111; 30) |
| Median age at diagnosis, in days | 52.5 | 57 | 87 | 52 | 21 | 45.5 | 44 |
| Breech (%) | 40% | 47% | 33% | 43% | 25% | 32% | 67% |
| Twins (%) | 2.4% | 0 | 8% | 3% | 0 | 0 | 0 |
| Family history (%) | 37% | 60% | 37% | 32% | 25% | 36% | 33% |
| First-born (%) | 29% | 0 | 21% | 38% | 42% | 32% | 33% |
Table 3Sensitivity (%) of the clinical examination for developmental dysplasia of the hip.
| Test | Overall (95% CI) | Graf IIa (95% CI) | Graf IIb (95% CI) | Graf IIc (95% CI) | Graf D (95% CI) | Graf III (95% CI) | Graf IV (95% CI) | Stable (95% CI) | Unstable (95% CI) |
| Barlow | 34% (26–42%) | 20% (10–30%) | 4% (0–12%) | 35% (24–46%) | 50% (35–65%) | 55% (40–70%) | 58% (42–74%) | 22% (13–31%) | 54% (43–65%) |
| Ortolani | 23% (16–30%) | 7% (1–13%) | 0% (0–0%) | 11% (4–18%) | 25% (12–38%) | 68% (53–83%) | 42% (26–58%) | 7% (2–12%) | 50% (39–61%) |
| Galeazzi | 16% (10–22%) | 0% (0–0%) | 8% (1–15%) | 3% (0–7%) | 0% (0–0%) | 36% (21–51%) | 75% (59–91%) | 4% (0–8%) | 37% (26–48%) |
| Abduction limitation | 48% (39–57%) | 33% (21–45%) | 38% (26–50%) | 43% (31–55%) | 42% (28–56%) | 64% (49–79%) | 83% (68–98%) | 39% (28–50%) | 63% (52–74%) |
| At least one positive finding | 66% (58–74%) | 40% (28–52%) | 38% (26–50%) | 62% (50–74%) | 75% (61–89%) | 95% (88–100%) | 100% (100–100%) | 50% (39–61%) | 91% (84–98%) |
CI: confidence interval.
Looking at the demographics in our study population, 84% of patients were female. Epidemiological data have reported that developmental dysplasia of the hip is two to three times more common in females than in male infants [12]. When examining risk factors, 40% of patients had breech presentation, 37% had a positive family history and 29% were first-born. These factors are well-documented as risk factors for developmental dysplasia of the hip, with a relative risk of 1.39 for positive family history (95% CI: 1.23–1.57), 3.8 for breech presentation (95% CI: 2.3–6.2) and 1.44 for first-born status (95% CI: 1.12–1.86) [13, 14].
However, a systematic literature review indicates that, apart from sex, only 10–27% of infants diagnosed with developmental dysplasia of the hip in population-based studies show discernible risk factors [6]. This raises concerns about selective screening, which recommends ultrasound examination only for infants presenting at least one risk factor or a pathological clinical examination.
This challenge is compounded by the fact that the sensitivity for identifying at least one positive clinical finding was only 66% in our study group for all hips (table 3). When considering only stable developmental dysplasia of the hip cases, the sensitivity drops to 50%. Conversely, sensitivity increases to 91% in the unstable group, a significantly better result. Despite experienced paediatric orthopaedic surgeons performing the clinical examinations, this suggests that selective screening based on clinical examination could miss approximately 50% of stable developmental dysplasia of the hip cases. Our results correlate with previous literature, where clinical screening sensitivity for developmental dysplasia of the hip varies between 28.1% and 57% [10, 15]. This variability has also been shown in a Danish study, which found a low predictive positive value for clinical screening of developmental dysplasia of the hip [15]. Furthermore, a study by Kyung et al. demonstrated that approximately 7% of clinically normal hips were found to be abnormal upon ultrasound examination in a sample of 156 ultrasounds [16].
The limited abduction was the most sensitive and prevalent clinical sign in our study group for both stable and unstable hips. This finding confirms previously reported data [4, 17]. The Ortolani and Barlow tests have a specificity above 90%, but their sensitivity drops to 35% and are therefore only useful in detecting unstable hips [15]. This has also been confirmed in our cohort, with sensitivities of 7% and 4%, respectively, in the stable developmental dysplasia of the hip group.
Timing at diagnosis was later in stable cases than in unstable ones with a mean age at diagnosis of 59 days in stable hips which corresponds to 8.5 weeks of life, while unstable hips were diagnosed at a mean age of 41 days. This is, compared to other authors, quite belated [18, 19].
Only 24% of stable hips were treated before the age of 6 weeks. The delayed diagnosis of stable developmental dysplasia of the hip may be attributed to the lack of clinical instability, which often leads to delayed screening ultrasound. It is one of the reasons why the international interdisciplinary consensus meeting on the evaluation of developmental dysplasia of the hip supports a universal screening programme for developmental dysplasia of the hip [9].
Considering the literature, different authors have reported a substantial reduction in surgical interventions, hospitalisations and delayed diagnoses resulting from a universal US screening programme [6, 20]. The outcomes of Austria’s universal screening initiative demonstrated a significant reduction in the frequency of open reduction, pelvic surgery and hospital admissions for developmental dysplasia of the hip. Furthermore, the expenses incurred by a US screening programme were outweighed by the costs saved through the avoidance of surgical and non-surgical treatments, confirming the programme’s cost-effectiveness [21, 22]. On the other hand, numerous recent studies and meta-analyses have failed to demonstrate the utility of universal screening in reducing late dysplasia [5, 23]. Selective screening is also supported by the American Academy of Pediatrics. They recommend clinical screening of all newborns with subsequent clinical exam of the hips at every regular health visit until the child is walking normally [24].
These variations in screening practices worldwide, coupled with the lack of a national register for dysplasia and long-term follow-up, complicate international comparisons [7].
Our study has limitations. The variability in ultrasound examiners – even if all ultrasound examinations were performed either by a paediatric radiologist or by the senior orthopaedic surgeon, thereby minimising variability in assessment – and the exclusion of patients with normal ultrasound scans limit the generalisability of our findings. Additionally, the small sample size and lack of interobserver reliability in clinical examination reduce the strength of our conclusions. Notably, all clinical assessments were performed by a single examiner, preventing an evaluation of consistency across different practitioners. Furthermore, the absence of a control group of patients without developmental dysplasia of the hip is a significant limitation, as all included patients were referred to our paediatric orthopaedic department based on an initial pathological ultrasound. Future studies should aim to incorporate a broader cohort, including patients without developmental dysplasia of the hip, to allow for the calculation of specificity and predictive values and to enhance the overall applicability of the findings.
In conclusion, our study highlights the limited sensitivity of clinical screening for developmental dysplasia of the hip, especially for stable cases. Even when performed by experienced clinicians, clinical examinations may miss nearly half of stable developmental dysplasia of the hip cases, which supports previous studies showing a wide range of clinical sensitivity (28–57%). Universal ultrasound screening offers a more comprehensive approach, reducing the risk of delayed diagnoses and the complications associated with missed cases. Although Austrian data support the cost-effectiveness of universal screening, international comparisons are complicated by inconsistent screening practices and the lack of long-term follow-up data.
Data are available by the authors on request.
Author contributions: Dr Enrica Pittaluga designed the data collection instruments, collected data, drafted the initial manuscript and critically reviewed the manuscript. Dr Alexis Arnoux collected data, and critically reviewed and revised the manuscript. Dr Sophie Rosa Merckaert conceptualised and designed the study, coordinated and supervised data collection, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
The present study received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Pollet V, Percy V, Prior HJ. Relative Risk and Incidence for Developmental Dysplasia of the Hip. J Pediatr. 2017 Feb;181:202–7. doi: https://doi.org/10.1016/j.jpeds.2016.10.017
2. Han J, Li Y. Progress in screening strategies for neonatal developmental dysplasia of the hip. Front Surg. 2022 Oct;9:995949. doi: https://doi.org/10.3389/fsurg.2022.995949
3. Graf R. [Hip ultrasonography. Basic principles and current aspects]. Orthopade. 1997 Jan;26(1):14–24.
4. Wilf-Miron R, Kuint J, Peled R, Cohen A, Porath A. Utilization of ultrasonography to detect developmental dysplasia of the hip: when reality turns selective screening into universal use. BMC Pediatr. 2017 Jun;17(1):136. doi: https://doi.org/10.1186/s12887-017-0882-0
5. Shorter D, Hong T, Osborn DA. Cochrane Review: screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013 Jan;8(1):11–54. doi: https://doi.org/10.1002/ebch.1891
6. Shipman SA, Helfand M, Moyer VA, Yawn BP. Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics. 2006 Mar;117(3):e557–76. doi: https://doi.org/10.1542/peds.2005-1597
7. Kilsdonk I, Witbreuk M, Van Der Woude HJ. Ultrasound of the neonatal hip as a screening tool for DDH: how to screen and differences in screening programs between European countries. J Ultrason. 2021 Jun;21(85):e147–53. doi: https://doi.org/10.15557/JoU.2021.0024
8. Degnan AJ, Hemingway J, Otero HJ, Hughes DR. Developmental hip dysplasia and hip ultrasound frequency in a large American payer database. Clin Imaging. 2021 Aug;76:213–6. doi: https://doi.org/10.1016/j.clinimag.2021.04.023
9. O’Beirne JG, Chlapoutakis K, Alshryda S, Aydingoz U, Baumann T, Casini C, et al. Internationales interdisziplinares Konsensustreffen zur Evaluation der Diagnostik und Therapie der angeborenen Hüftdysplasie [International Interdisciplinary Consensus Meeting on the Evaluation of Developmental Dysplasia of the Hip]. Ultraschall Med. 2019 Aug;40(4):454–64. doi: https://doi.org/10.1055/a-0924-5491
10. Arti H, Mehdinasab SA, Arti S. Comparing results of clinical versus ultrasonographic examination in developmental dysplasia of hip. J Res Med Sci. 2013 Dec;18(12):1051–5.
11. Graf R. Hip sonography: background; technique and common mistakes; results; debate and politics; challenges. Hip Int. 2017 May;27(3):215–9. doi: https://doi.org/10.5301/hipint.5000514
12. Vafaee AR, Baghdadi T, Baghdadi A, Jamnani RK. DDH Epidemiology Revisited: Do We Need New Strategies? Arch Bone Jt Surg. 2017 Nov;5(6):440–2.
13. Ran L, Chen H, Pan Y, Lin Q, Canavese F, Chen S. Comparison between the Pavlik harness and the Tübingen hip flexion splint for the early treatment of developmental dysplasia of the hip. J Pediatr Orthop B. 2020 Sep;29(5):424–30. doi: https://doi.org/10.1097/BPB.0000000000000667
14. Ortiz-Neira CL, Paolucci EO, Donnon T. A meta-analysis of common risk factors associated with the diagnosis of developmental dysplasia of the hip in newborns. Eur J Radiol. 2012 Mar;81(3):e344–51. doi: https://doi.org/10.1016/j.ejrad.2011.11.003
15. Chavoshi M, Soltani G, Shafiei Zargar S, Wyles CC, Kremers HM, Rouzrokh P. Diagnostic Performance of Clinical Examination Versus Ultrasonography in the Detection of Developmental Dysplasia of Hip: A Systematic Review and Meta-Analysis. Arch Bone Jt Surg. 2022 May;10(5):403–12.
16. Kyung BS, Lee SH, Jeong WK, Park SY. Disparity between Clinical and Ultrasound Examinations in Neonatal Hip Screening. Clin Orthop Surg. 2016 Jun;8(2):203–9. doi: https://doi.org/10.4055/cios.2016.8.2.203
17. Čustović S, Šadić S, Vujadinović A, Hrustić A, Jašarević M, Čustović A, et al. The predictive value of the clinical sign of limited hip abduction for developmental dysplasia of the hip (DDH). Med Glas. 2018 Aug;15(2):174–8. doi: https://doi.org/10.17392/954-18
18. Seidl T, Lohmaier J, Hölker T, Funk J, Placzek R, Trouillier HH. [Reduction of unstable and dislocated hips applying the Tübingen hip flexion splint?]. Orthopade. 2012 Mar;41(3):195–9. doi: https://doi.org/10.1007/s00132-011-1873-8
19. Pavone V, Testa G, Riccioli M, Evola FR, Avondo S, Sessa G. Treatment of Developmental Dysplasia of Hip With Tubingen Hip Flexion Splint. J Pediatr Orthop. 2015;35(5):485–9. doi: https://doi.org/10.1097/BPO.0000000000000313
20. von Kries R, Ihme N, Oberle D, Lorani A, Stark R, Altenhofen L, et al. Effect of ultrasound screening on the rate of first operative procedures for developmental hip dysplasia in Germany. Lancet. 2003 Dec;362(9399):1883–7. doi: https://doi.org/10.1016/S0140-6736(03)14957-4
21. Thallinger C, Pospischill R, Ganger R, Radler C, Krall C, Grill F. Long-term results of a nationwide general ultrasound screening system for developmental disorders of the hip: the Austrian hip screening program. J Child Orthop. 2014 Feb;8(1):3–10. doi: https://doi.org/10.1007/s11832-014-0555-6
22. Thaler M, Biedermann R, Lair J, Krismer M, Landauer F. Cost-effectiveness of universal ultrasound screening compared with clinical examination alone in the diagnosis and treatment of neonatal hip dysplasia in Austria. J Bone Joint Surg Br. 2011 Aug;93(8):1126–30. doi: https://doi.org/10.1302/0301-620X.93B8.25935
23. Mulpuri K, Song KM, Goldberg MJ, Sevarino K. Detection and Nonoperative Management of Pediatric Developmental Dysplasia of the Hip in Infants up to Six Months of Age. J Am Acad Orthop Surg. 2015 Mar;23(3):202–5. doi: https://doi.org/10.5435/JAAOS-D-15-00006
24. American Academy of Pediatrics. Clinical practice guideline: early detection of developmental dysplasia of the hip. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. Pediatrics. 2000 Apr;105(4 Pt 1):896–905.