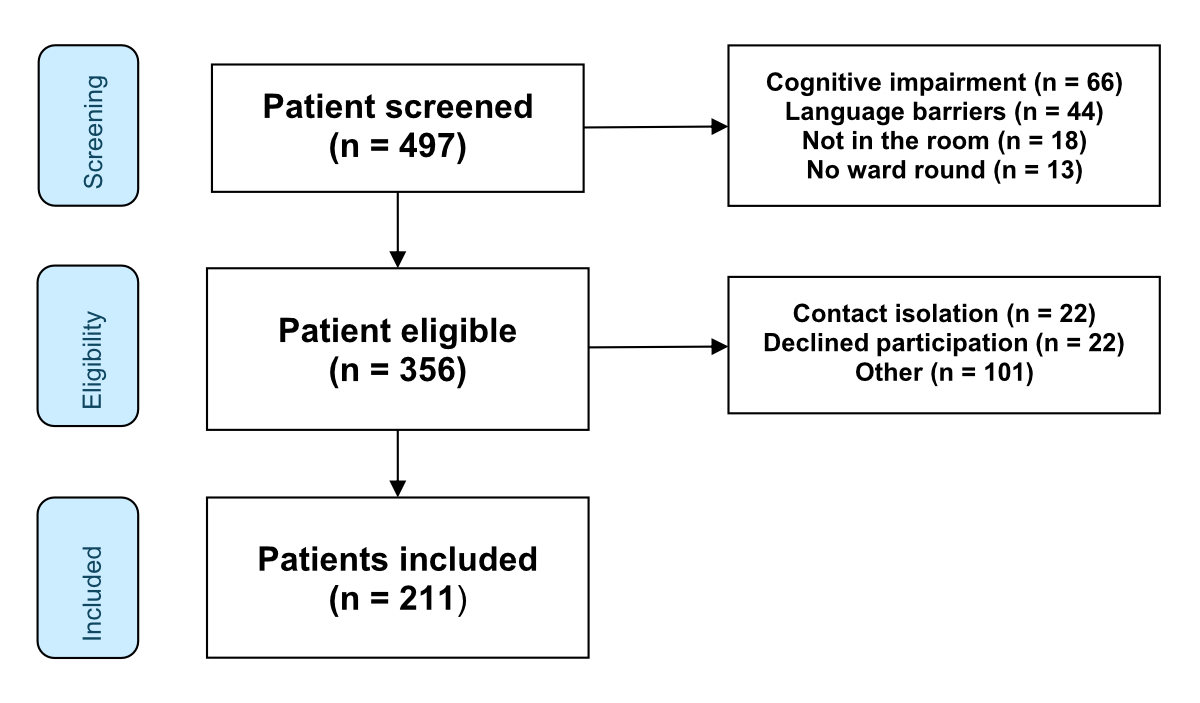
Figure 1Flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.4070
In the field of internal medicine, ward rounds are an integral element of patient-centred care. Ward rounds are crucial for two aspects: for information exchange, discussion and coordination between nurses and physicians; and for communicating and interacting with the patient. Ward rounds have previously been described as a “central marketplace for information” [1]. The UK’s Royal College of Physicians (RCP) and Royal College of Nursing (RCN) emphasise that healthcare professionals should not underestimate the importance of ward round interactions from the patient’s perspective [2]. Despite their importance, ward rounds remain complex and challenging [1, 3–5]. As patient-physician contact during ward rounds only lasts between 6 and 11 minutes, it is important for physicians to optimise the time available [6]. Despite the constraints, patient-centred care should consider both the informational and emotional needs of patients [7, 8].
Unfortunately, literature on ward rounds focusing on patient-related outcomes such as satisfaction is scarce. One 2019 meta-analysis was only able to identify five randomised trials that analysed patient satisfaction with ward rounds. These studies mainly used dichotomous outcome formats (satisfied vs not satisfied) [9] and did not include well-defined factors which could be used to improve clinical practices. Other studies examining benefits and barriers of interprofessional work during ward rounds focused primarily on the perspective of nurses and physicians. Findings highlighted the benefits of interprofessional collaboration, particularly in terms of communication and coordination [10, 11].
Few studies have focused on patient expectations of interprofessional rounds. This study aimed to investigate the patient perspective of ward rounds, which in turn could potentially help clinicians improve interaction during ward rounds.
The study uses a mixed-methods design, combining both quantitative and qualitative research techniques. Standards for reporting qualitative research (SRQR) were used [12].
Participation in the survey was voluntary. Participants were made aware of this and were interviewed verbally. The Ethics Committee of Northern and Central Switzerland waived the need for ethical approval.
We applied Practices for Survey Research and Strengthening the Reporting of Observational Studies in Epidemiology [13] guidelines and consulted current literature concerning ward round procedures for the development and implementation of the survey, as well as reporting of the data.
The survey was designed according to the following three-step process: (1) The authors developed a questionnaire based on current literature and their clinical expertise; (2) The survey was evaluated by two senior physicians working in internal medicine wards. After incorporating their feedback, we presented the revised version to five randomly selected healthcare professionals who regularly took part in medical ward rounds; and (3) We asked patients for their input on the clarity and relevance of the questions, incorporated their feedback into the refinement process according to the principles of Patient and Public Involvement (PPI), and refined the survey accordingly [14]. The final version comprised a total of 13 questions (open-ended, visual analogue scale [VAS] and multiple-choice questions) and took approximately 10 minutes to complete (table 1). Patients were interviewed in person and answers were documented in writing.
Table 1Survey summary.
| Question | Question type | Outcomes |
| Expectations and current state of ward round | ||
| How long did this morning's round take? | minutes | |
| What is the ideal length of time for a ward round? | minutes | |
| How satisfied are you with this morning's round? | close-ended | VAS 0-10 |
| Reasons/remarks/comments | open-ended | |
| Were you able to bring your questions, concerns and needs into the last round? | close-ended | VAS 0-10 |
| Did you feel that you had enough time to speak or that you were listened to? | close-ended | |
| How clear were the doctors' explanations? | close-ended | VAS 0-10 |
| What do you think the round should include? | open-ended | |
| What do you expect from your doctor during the round? | open-ended | |
| What do you expect from the nursing staff during the round? | open-ended | |
| Were there any sensitive topics discussed during the round? | open-ended | |
| Do you prefer a joint round or a round by physicians only? | close-ended | |
| Why do you prefer a joint round with the medical/nursing team? | open-ended | |
Data collection took place between 25 August and 8 September 2023. Hospitalised patients from 4 teaching hospitals (University Hospital Basel, University Hospital Bern, Cantonal Hospital Aarau, Cantonal Hospital Baselland Liestal) were interviewed by members of the study team. A total of 211 participants were recruited using a convenience sampling strategy, with approximately 50 patients per centre to ensure proportional representation and logistical feasibility. Switzerland’s healthcare system ensures universal health insurance coverage and is known for its high standards of care. Internal medicine wards in Swiss hospitals provide multidisciplinary care for adults with diverse acute and chronic medical conditions, including cardiovascular, respiratory, gastrointestinal and metabolic diseases. Inclusion criteria were at least one completed ward round (either with a resident, attending or consultant physician), sufficient knowledge of the local language, availability for interview and no present cognitive impairment. Ward rounds were conducted by the resident physician either alone or with an attending physician or consultant physician.
The primary outcome was patient-perceived satisfaction with ward rounds, measured on a VAS of 0–10; with 0 indicating the lowest possible satisfaction and 10 the highest possible satisfaction. Presumed factors included estimated and ideal duration of ward rounds, perceived comprehensibility and participation, and preference for interprofessional or separate ward rounds.
Baseline characteristics (age, sex, medical centre, principal diagnosis upon admission) were based on patient report. We included six open-ended questions and provided patients the opportunity to provide qualitative free-text feedback on perceived quality and expectations of ward rounds.
Study team members systematically approached all patients on the medical ward to identify eligible patients and to minimise selection bias. Patients unlikely to complete the interview were excluded from the study (e.g. due to dementia or delirium). Demographic information, including age, sex and principal diagnosis, were based on patient report. Interviews were conducted by trained personnel to ensure a consistent approach in data collection. Participants were asked questions regarding their satisfaction with the ward rounds (table 1). Rather than recording responses, the study team transcribed them manually. Data collection was conducted on a tablet using “Umfrageonline.ch”, a web-based survey tool that facilitates the completion of questionnaires in a secure and accessible manner. All data were anonymised, electronically documented and subsequently analysed.
The assumptions of all hypothesis tests were assessed and confirmed to be met prior to analysis. Baseline characteristics were stratified by the primary outcome. Dichotomisation of the primary outcome into higher and lower satisfaction was performed according to a median split, with lower satisfaction including values at and below the median. The median cutoff point was chosen a priori to emphasise the importance of addressing even moderate levels of lower satisfaction. This approach acknowledges that hospitalised patients may hesitate to express strong negative feedback. By utilising the median, the analysis ensures that even subtle levels of lower satisfaction are captured and highlighted, preventing it from being overlooked. Baseline characteristics were stratified by primary outcome and groups compared using Pearson’s chi-squared test, ANOVA and the two-tailed Student’s t-test or Wilcoxon rank-sum test, as appropriate, following an assessment of data distribution. We also performed the following analyses: (a) univariable logistic regression to evaluate associations between baseline variables and perceived lower satisfaction; (b) multivariable models adjusted for age and sex. A p-value of <0.05 (two-tailed) was considered statistically significant. STATA 15.0 statistical software (Stata Corp., College Station, TX, USA) was used for all quantitative analyses.
We asked patients to provide qualitative feedback regarding their experience with ward rounds and their views regarding interprofessional collaboration. The interviewers were instructed to strictly adhere to the survey wording and avoid providing any additional explanations. Responses were documented verbatim and categorised thematically. Categorisation was performed by two investigators who discussed differences until consensus was reached. As each answer was also broken down into thematic items, one answer could be assigned to multiple categories.
A total of 497 patients were screened, of whom 356 met the eligibility criteria. Of these, 123 were excluded and 22 declined participation, resulting in the inclusion of data from 211 patients in the final analysis (figure 1). Reasons for exclusion were contact isolation (n = 22) and other (n = 101). We used a convenience sampling approach [15] and subsequently collected data from 211 participants (59.3% participation rate). The mean age of patients was 67.6 years (range: 50.1–85.2) and 42.7% were female. Approximately one quarter had an infection and 18% had cardiovascular disease as a principal diagnosis at time of admission. Further demographic characteristics of the study population are shown in table 1.
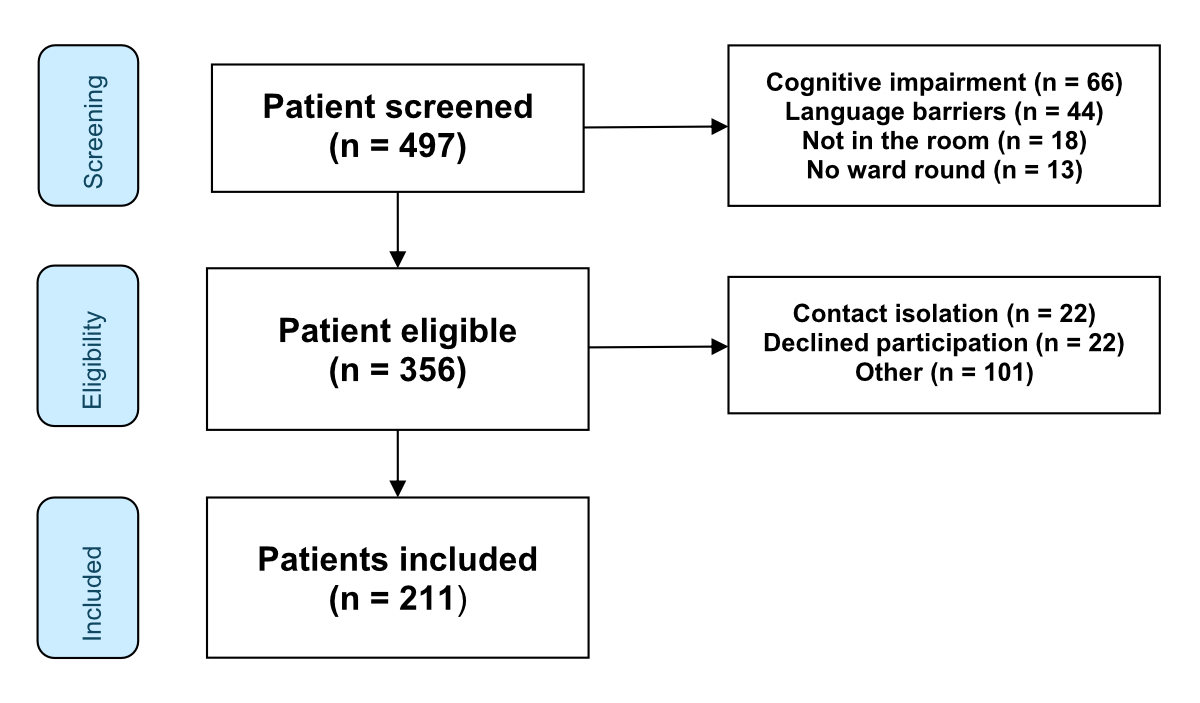
Figure 1Flowchart.
Overall, the median reported satisfaction score was 8 points (interquartile range [IQR] 7–10). Patients who reported lower satisfaction were compared with patients reporting higher satisfaction. Patients who reported lower satisfaction had a mean (±SD) age of 68.2 (± 15.9) years. Patients with lower and higher satisfaction did not differ in terms of age, sex, medical centre or principal diagnosis on admission (table 2).
Table 2Factors affecting satisfaction (n = 211).
| Sociodemographic factors | All | Higher satisfaction | Lower satisfaction | p-value | Univariable odds ratio (95% confidence interval) | p-value | Adjusted odds ratio (95% confidence interval) | p-value | |
| n | 211 | 104 | 107 | ||||||
| Age (years), mean (SD) | Per 1-year increase | 67.6 (17.6) | 67.0 (19.2) | 68.2 (15.9) | 0.62 | 1.00 (0.99–1.02) | 0.62 | 1.00 (0.99–1.02) | 0.61 |
| Sex, n (%) | Female | 90 (42.7%) | 46 | 44 | 0.65 | 0.88 (0.51–1.52) | 0.65 | 0.88 (0.51–1.51) | 0.63 |
| Medical centre, n (%) | University Hospital Basel | 53 (25.1%) | 23 | 30 | 0.16 | (ref) | n.a. | (ref) | n.a. |
| University Hospital Bern | 52 (24.6%) | 21 | 31 | 1.13 (0.52–2.46) | 0.76 | 1.15 (0.53–2.50) | 0.73 | ||
| Cantonal Hospital Aarau | 55 (26.1%) | 33 | 22 | 0.51 (0.24–1.10) | 0.09 | 0.49 (0.23–1.07) | 0.07 | ||
| Cantonal Hospital Liestal | 51 (24.2%) | 27 | 24 | 0.68 (0.31–1.48) | 0.33 | 0.71 (0.32–1.54) | 0.38 | ||
| Principal diagnosis on admission | Cardiovascular disease | 37 (17.5%) | 18 | 19 | 0.61 | (ref) | n.a. | (ref) | n.a. |
| Tumour | 33 (15.6%) | 13 | 20 | 1.46 (0.56–3.77) | 0.44 | 1.60 (0.59–4.30) | 0.36 | ||
| Infectious disease | 49 (23.2%) | 27 | 22 | 0.77 (0.33–1.82) | 0.55 | 0.82 (0.34–1.96) | 0.65 | ||
| Gastrointestinal disease | 15 (7.1%) | 6 | 9 | 1.42 (0.42–4.80) | 0.57 | 1.55 (0.45–5.35) | 0.49 | ||
| Other | 77 (36.5%) | 40 | 37 | 0.88 (0.40–1.92) | 0.74 | 0.94 (0.42–2.10) | 0.88 | ||
| Patient-reported ward round-related factors | |||||||||
| Estimated duration of ward round (minutes), mean (SD) | 12.1 (7.5) | 12.7 (8.1) | 11.6 (6.8) | 0.29 | 0.98 (0.94–1.02) | 0.29 | 0.98 (0.94–1.01) | 0.23 | |
| Ideal duration of ward round (minutes), mean (SD) | 12.2 (6.7) | 12.4 (6.8) | 12.0 (6.6) | 0.71 | 0.99 (0.95–1.03) | 0.70 | 0.99 (0.95–1.03) | 0.64 | |
| Perceived comprehensibility (0–10 on VAS), mean (SD) | 8.3 (1.7) | 9.1 (1.2) | 7.7 (1.9) | <0.001 | 0.55 (0.45–0.69) | <0.001 | 0.55 (0.45–0.69) | <0.001 | |
| Perceived participation (0–10 on VAS), mean (SD) | 8.2 (2.0) | 9.2 (1.0) | 7.1 (2.2) | <0.001 | 0.39 (0.30–0.52) | <0.001 | 0.39 (0.30–0.52) | <0.001 | |
| Ward round team | Not interprofessional | 68 (32.2%) | |||||||
| Interprofessional | 143 (67.8%) | 74 | 69 | 0.30 | 0.74 (0.41–1.32) | 0.30 | 0.73 (0.41–1.30) | 0.28 | |
| Team preference | Physician only / Indifferent | 91 (43.1%) | |||||||
| Prefer interprofessional | 120 (56.9%) | 57 | 63 | 0.55 | 1.18 (0.68–2.04) | 0.55 | 1.17 (0.68–2.02) | 0.57 | |
VAS: Visual Analogue Scale.
Most patients (86.3%) reported satisfaction with the time they had to speak and express themselves during the ward round. Ten percent of all patients were moderately satisfied and 4.3% were not satisfied with their allotted speaking time. A minority of patients (13.7%) reported that they felt that sensitive topics were discussed during the round. They were asked whether they encountered any topics during the ward round they considered sensitive, and if so, asked for details on those topics [16].
Lower satisfaction was less frequent among patients who reported a high comprehensibility (clarity and understanding) of their current medical situation (mean VAS 7.7 vs 9.1 points, adjusted OR for lower satisfaction 0.55, 95% CI 0.45–0.69; p <0.001). Similarly, patients who felt more involved with their medical care were less likely to report lower levels of satisfaction (mean VAS 7.1 vs 9.2 points, adjusted OR for lower satisfaction 0.39, 95% CI 0.3–0.52; p <0.001).
The mean ward round duration estimated by patients (12.1 minutes) was not associated with levels of satisfaction. Slightly over half (56.9%) reported a preference for interprofessional ward rounds. According to patient reports, ward rounds were performed in interprofessional teams for approximately two thirds of patients (67.8%).
Three themes emerged when patients were asked about reasons for level of satisfaction with ward rounds (table 3). One third (31.1%) indicated that receiving information and explanations (including test results, diagnosis and treatment) regarding the current medical situation was the most important factor. They were also grateful for any answered questions and clarification of gaps in knowledge. A similarly high proportion (31.1%) of patients cited the ability to participate actively, as well as interpersonal contact with the treatment team as the most important factors. Fourteen percent of patients reported their level of satisfaction was influenced by organisational issues such as information flow within the medical team, physicians’ knowledge of the case and efficient use of time.
Table 3Reasons affecting satisfaction (n = 211).
| Expectations regarding ward rounds | Category | # answers in category (% of 211) | Examples of positive answers | Examples of negative answers |
| Why were you satisfied with the ward round? | Information and explanation about current medical situation, clarification of uncertainties. | 66 (31.3%) | “Information was clear and understandable, anything unclear was addressed, and no unnecessary information was given” | “It was all good, but there was just too much information to process right away” |
| “I'm the last to know. The flow of information between the disciplines is difficult.” | ||||
| “It was fast and informative. I was able to decide if I wanted to ask about something.” | ||||
| Taking time, interpersonal relationships, patient participation. | 66 (31.3%) | “Did not get the impression that they were stressed. I felt comfortable. People took me seriously and fear was taken away.” | “It wasn't really a dialogue. I would have liked to discuss more and be more involved.” | |
| “Having a single person to talk to would be important. A doctor can also sit on the bed and talk to me as a person, eye level is important.” | ||||
| “The chemistry was right for a trusting relationship” | ||||
| “I had to call the doctor back twice because he finished so fast” | ||||
| “You are informed and make your own decisions. And you make your own decisions.” | ||||
| “One person was talking and everyone else is staring at you. I felt not comfortable.” | ||||
| “You can talk to him. He listens. I was able to express all my concerns.” | ||||
| Organisation, prior knowledge of the case, time management and efficacy. | 29 (13.7%) | “The doctors were proactive, efficient and well prepared” | “Sometimes there are misunderstandings between the disciplines. Unfortunately, there are often team changes, which makes the flow of information difficult.” | |
| “Today’s visit was more detailed and without phone interruptions / distractions” | ||||
| “I was often asked the same question.” | ||||
| “I found the ward round very professional. They discuss things in the hallway first.” | ||||
| Discussion of further procedures, treatment plan. | 18 (8.5%) | “Clear information about what will happen next, options were explained” | “The therapy and the explanations are always changing; everybody says something different.” | |
| “The communication flow regarding discharge was not always ideal, there is no plan” | ||||
| “The senior physician was quite dominant, but that wasn’t a bad thing as he defined a clear procedure” | ||||
| “No decisions were made. It was always said that this would have to be discussed with the attending physician” | ||||
| Non-influenceable patient-related factors (e.g. bad news, private burdens). | 15 (7.1%) | “Good news received” | “The doctor wanted to suggest a nursing home” | |
| “I did not get any positive news otherwise it was good” |
Over two thirds of patients (71.1%) stated that receiving information and explanations was their highest priority during ward rounds, whereas 39.3% reported discussions about next steps to be the most important. When asked about their expectations of the physicians, responses were heterogeneous – with qualities such as honesty, transparency and reliability mentioned most frequently (42 patients, 19.9%).
Patients preferred interprofessional ward rounds for two main reasons: Firstly, they felt that nurses and physicians should possess the same level of information to reduce potential misunderstandings (37.4%). This would also enable nurses to contribute observations and viewpoints as they have closer contact and see patients performing daily activities. Secondly, nurses were cited as an important source of support during ward rounds as they facilitate patients’ active participation (18.0%) (table 4). ((Table mention was missing in the text. Was it placed correctly?))
Table 4Patients’ perception of current state of interprofessional ward rounds (n = 211).
| Question | Category | # answers in category | Examples of patient answers |
| What should a ward round include according to you? | Information and explanation about current medical situation, clarification of uncertainties. | 150 (71.1%) | “Clarification that I know where I stand and answers to any questions patients may have” |
| “Explanations about the overall situation and the disease” | |||
| “The findings and test results need to be discussed and explained in an understandable manner” | |||
| Discussion of further procedures, treatment plan. | 83 (39.3%) | “A clear plan of how you want to proceed and explain why” | |
| “Explanations about the plan is for the next 24 hours. Information about further diagnostics and tests.” | |||
| “Outlook and options” | |||
| “Information about discharge and about what I need to consider at home” | |||
| What do you expect from a doctor during ward rounds? | Honesty, transparency, reliability. | 42 (19.9%) | “He should tell me openly and honestly what’s going on and not hide the truth from me” |
| “Full transparency means communicating directly, not in bits and pieces” | |||
| Why do you prefer a ward round together with the nursing staff? | Interprofessional collaboration and information flow. | 79 (37.4%) | “They should talk together. It’s not the same if they just read, it has to be person to person.” |
| “It allows that information is exchanged properly and not everything has to be said twice. And it gives nurses a better overview of the treatment.” | |||
| “The professions can complement each other, then everyone is on the same level” | |||
| “Different perspectives are united. Otherwise, there are detours.” | |||
| “It gives me a sense of security that when the doctors are gone, the nurses know what has been done” | |||
| Perspective of nursing care, encouragement of patient participation. | 38 (18.0%) | “Nurses can bring their views in. They are closer to the patient.” | |
| “Nurses remind me of aspects that I may have forgotten” | |||
| “Because they know the most about me and see me the most” | |||
| What do you expect from the nursing staff during the ward round? | To be informed, no expectations. | 104 (49.3%) | “That they then implement what is said” |
| “They just need to know what is being discussed and how to proceed” | |||
| “That they are present and hears exactly what is being said” | |||
| Inform the doctors about the condition / provide additional information. | 34 (16.1%) | “That they address what has not yet been said” | |
| “Support for the doctors. They are like the right hand of the doctor and deliver information that they don’t notice.” | |||
| Support the patient during and after the ward round. | 34 (16.1%) | “Nurses help me to participate actively and support me” | |
| “Nurses report to the doctor things I have discussed with her” | |||
| “Concerns I have previously raised with the nursing staff are addressed during the round” |
Twenty-seven percent of patients expected nurses to play a more active role during ward rounds. They reported that nurses should communicate or supplement missing information, and support patients during and after ward rounds.
Our data identified two key parameters of lower satisfaction with ward rounds: lower perceived comprehensibility, and lower perceived patient participation. Among those reporting lower ward round satisfaction, the quality of information about the current medical situation, a desire to participate and organisational factors were cited as the most important reasons. Although overall satisfaction with ward rounds was generally high (which is consistent with previous studies), our data identified potential areas of improvement and revealed insights into the patient perspective [6, 17].
Our results indicate that clear and understandable information is a key factor of satisfaction with ward rounds and the most important expectation from the patient’s perspective. The important role of comprehensible information has been shown in previous studies in emergency medicine, where clear and understandable communication at time of discharge positively impacted patient satisfaction and even readmission rates [18]. Although less data are available for the inpatient setting, one previous cohort study with 5440 participants found that a lower understanding of health information was associated with 11.1% longer length of stay [19]. The complexity of medical information and confusion produced by medical jargon may lead to misunderstandings and patient distress [6]. Patients often prioritised understanding their current medical situation over discussions about discharge.
Many patients in our sample reported that physicians’ empathy and their own involvement were the most important factors affecting the level of satisfaction with ward rounds. Individuals valued physicians who took time to listen and address patients’ needs, fears and concerns – and expect their physician to be honest, transparent and reliable. The effect of patient involvement on satisfaction outcomes should be an important consideration for clinicians. Another study found that approximately 3 out of 4 patients prefer to actively participate in the decision-making process during ward rounds [20]. However, the same study also found that patients with a higher preference for participation were significantly more critical and distrustful of the healthcare team, and less satisfied with their overall hospital stay.
A substantial proportion of patients favoured interprofessional ward rounds. Better flow of information was the most reported reason, and well-informed nurses was the most reported expectation. In previous studies, nurse participation in rounds was measured by the number of utterances, with the assumption that fewer utterances meant less participation. One of these studies found that only 13.5% of all utterances were made by nurses, compared to 51.6% by physicians and 34.8% by patients [1]. This suggests that active participation of nurses in rounds may be improved.
This study has several strengths. Firstly, patients were interviewed during their hospital stay shortly after a ward round, which minimises the potential for recall bias [21]. Secondly, the qualitative approach provides a deeper insight into patients’ perceptions. Thirdly, the multicentre design and mix of two university hospitals and two larger cantonal hospitals enables a representative assessment of Swiss hospitals with comparable ward round organisation. However, the study also has several limitations: The observational convenience sampling design inherently introduces selection bias, as the sample may not fully represent all patient populations, such as those who declined participation or were unavailable during the data collection period. Information bias could also affect the findings, as patients’ responses might be influenced by the timing of interviews shortly after their interactions with medical staff. Finally, the generalisability of the findings might be constrained by the focus on Swiss hospitals, as ward round practices and organisational structures may differ significantly in other countries or healthcare settings.
This Swiss multicentre survey provides important insights from the patient perspective regarding various elements of patient-centred care during medical ward rounds. Interviewees were more interested in information about their current state of health than information about possible next steps. The study also underscores the essential role of nurses in ward rounds, emphasising the need for their active participation and collaboration with physicians to ensure comprehensive patient care and support. These findings have implications for clinical practice, suggesting that clear communication, prioritisation of patient-centred communication and active involvement of nursing staff during ward rounds may be key drivers to optimise patient satisfaction and enhance the overall patient experience. Comprehensible information and active involvement of patients may further improve the patient experience and satisfaction with care.
We plan to make the data collected during this study available to others. This includes de-identified individual participant data and a data dictionary explaining each field in the dataset. Additionally, related materials such as the trial protocol, written code, and the statistical analysis plan will be provided. The data will be accessible following the publication of our primary manuscript and any secondary projects, upon receipt of a detailed letter of intent outlining the study hypothesis and statistical analysis plan. Each request will be reviewed by the authors, who will collectively decide on the appropriateness of data sharing. Applicants will be required to sign a data access agreement. For inquiries, please contact the principal investigator of this trial at sabina.hunziker[at]usb.ch.
Armon Arpagaus has received grants from the Gottfried and Julia Bangerter-Rhyner Foundation, Switzerland. Grant Reference YTCR 06/23. Sabina Hunziker was supported by the Gottfried and Julia Bangerter-Rhyner Foundation, the Swiss National Science Foundation (SNSF) and the Swiss Society of General Internal Medicine (SSGIM) during the conduct of the study. Grant References 10001C_192850/1 and 10531C_182422.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Weber H, Stöckli M, Nübling M, Langewitz WA. Communication during ward rounds in internal medicine. An analysis of patient-nurse-physician interactions using RIAS. Patient Educ Couns. 2007 Aug;67(3):343–8. doi: https://doi.org/10.1016/j.pec.2007.04.011
2. RCoN. R.C.o.P., Ward Rounds in Medicine: Principles for best practice. RCP. 2012. Available from https://www.rcp.ac.uk/media/yvaozxqf/ward_rounds_in_medicine.pdf
3. Lancet. Ward rounds: what goes around comes around. Lancet. 2012 Oct;380(9850):1281. doi: https://doi.org/10.1016/S0140-6736(12)61740-1
4. Weber, H. and W. Langewitz, Basler Visitenstandard–Chance für eine gelingende Interaktionstriade Patient-Arzt-Pflegefachperson. PPmP-Psychotherapie· Psychosomatik· Medizinische Psychologie, 2011. 61(03/04): p. 193-195.
5. Weber E, Vgele S, Hopbach K, Huber LC. Ein alter Zopf oder moderne interprofessionelle Teamarbeit? - Die Visite als Instrument der spitalinternistischen Tätigkeit. Prim Hosp Care. 2020;20(6):205–7.
6. Becker C, Gamp M, Schuetz P, Beck K, Vincent A, Hochstrasser S, et al.; BEDSIDE-OUTSIDE Study Group. Effect of Bedside Compared With Outside the Room Patient Case Presentation on Patients’ Knowledge About Their Medical Care : A Randomized, Controlled, Multicenter Trial. Ann Intern Med. 2021 Sep;174(9):1282–92. doi: https://doi.org/10.7326/M21-0909
7. Stewart M. Towards a global definition of patient centred care. BMJ. 2001 Feb;322(7284):444–5. doi: https://doi.org/10.1136/bmj.322.7284.444
8. Bardes CL. Defining" patient-centered medicine. Health Aff (Millwood). 2009;28(4):w555–65.
9. Gamp M, Becker C, Tondorf T, Hochstrasser S, Metzger K, Meinlschmidt G, et al. Effect of bedside vs. non-bedside patient case presentation during ward rounds: a systematic review and meta-analysis. J Gen Intern Med. 2019 Mar;34(3):447–57. doi: https://doi.org/10.1007/s11606-018-4714-1
10. Gonzalo JD, Kuperman E, Lehman E, Haidet P. Bedside interprofessional rounds: perceptions of benefits and barriers by internal medicine nursing staff, attending physicians, and housestaff physicians. J Hosp Med. 2014 Oct;9(10):646–51. doi: https://doi.org/10.1002/jhm.2245
11. Sharma U, Klocke D. Attitudes of nursing staff toward interprofessional in-patient-centered rounding. J Interprof Care. 2014 Sep;28(5):475–7. doi: https://doi.org/10.3109/13561820.2014.907558
12. O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014 Sep;89(9):1245–51. doi: https://doi.org/10.1097/ACM.0000000000000388
13. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007 Oct;147(8):573–7. doi: https://doi.org/10.7326/0003-4819-147-8-200710160-00010
14. Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016 Aug;25(8):626–32. doi: https://doi.org/10.1136/bmjqs-2015-004839
15. Shorten A, Moorley C. Selecting the sample. Evid Based Nurs. 2014 Apr;17(2):32–3. doi: https://doi.org/10.1136/eb-2014-101747
16. Gross S, Becker C, Beck K, Memma V, Gaab J, Schütz P, et al. Occurrence of sensitive topics during ward round: an ancillary analysis of the BEDSIDE-OUTSIDE trial. BMJ Open. 2023 Sep;13(9):e073584. doi: https://doi.org/10.1136/bmjopen-2023-073584
17. Lehmann LS, Brancati FL, Chen MC, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997 Apr;336(16):1150–5. doi: https://doi.org/10.1056/NEJM199704173361606
18. Becker C, Zumbrunn S, Beck K, Vincent A, Loretz N, Müller J, et al. Interventions to improve communication at hospital discharge and rates of readmission: a systematic review and meta-analysis. JAMA Netw Open. 2021 Aug;4(8):e2119346–2119346. doi: https://doi.org/10.1001/jamanetworkopen.2021.19346
19. Jaffee EG, Arora VM, Matthiesen MI, Meltzer DO, Press VG. Health literacy and hospital length of stay: an inpatient cohort study. J Hosp Med. 2017 Dec;12(12):969–73. doi: https://doi.org/10.12788/jhm.2848
20. Becker C, Gross S, Gamp M, Beck K, Amacher SA, Mueller J, et al. Patients’ Preference for Participation in Medical Decision-Making: Secondary Analysis of the BEDSIDE-OUTSIDE Trial. J Gen Intern Med. 2023 Apr;38(5):1180–9. doi: https://doi.org/10.1007/s11606-022-07775-z
21. Pacheco Barzallo D, Köhn S, Tobler S, Délitroz M, Gemperli A. Measuring patient satisfaction in acute care hospitals: nationwide monitoring in Switzerland. Z Evid Fortbild Qual Gesundhwes. 2021 Oct;165:27–34. doi: https://doi.org/10.1016/j.zefq.2021.07.001