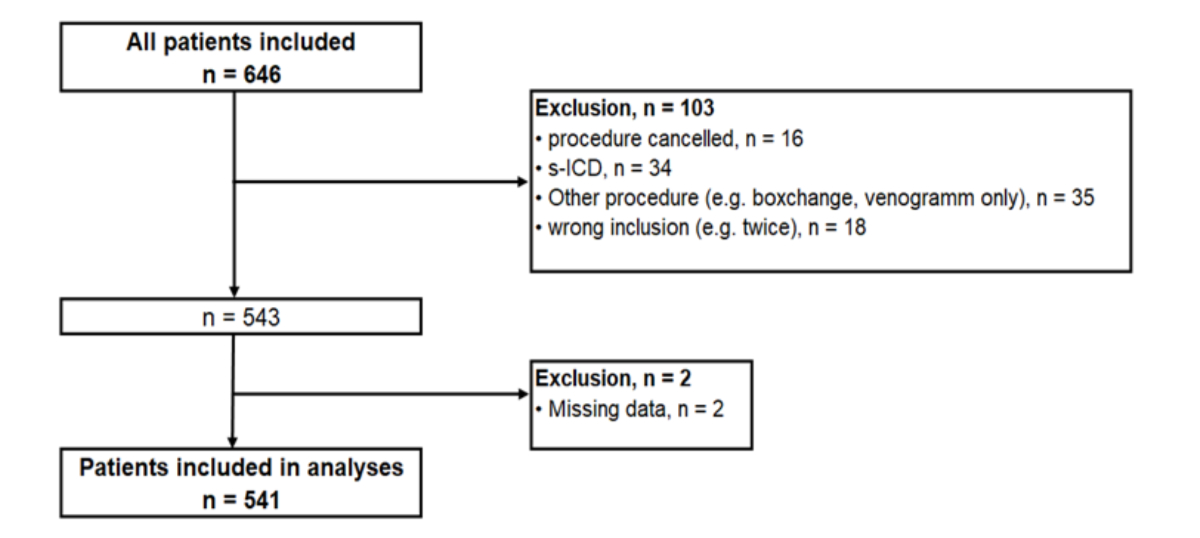
Figure 1Patient flowchart shown for the 646 patients included. The reasons for exclusion and the absolute numbers of patients excluded are shown in the boxes on the right. 541 patients were included in the final analysis.
DOI: https://doi.org/https://doi.org/10.57187/s.4053
Over the past few decades, interventional electrophysiology has experienced substantial growth, particularly in the realms of ablation procedures and device implantations [1]. The rising adoption and intricacy of imaging and interventional techniques have resulted in higher radiation exposure levels, with cardiologists increasingly contributing to the total cumulative effective radiation dose received by the US population [2]. Fluoroscopy continues to be the primary imaging technique used in the majority of interventional procedures in cardiology [3–5].
Considering these developments, there is growing apprehension about potential health hazards associated with exposure to ionising radiation including stochastic effects (for example radiation carcinogenesis) and tissue reactions (such as skin injuries) [3–7]. In order to mitigate health risks, it is imperative to implement measures aimed at optimising patient radiation exposure and clinical practice as mandated by relevant legislation [3, 8]. One of these measures is clinical radiation audits, which aim to ensure ideal use of ionising radiation in clinical practice [9]. The first clinical radiation audit in a cardiology department in Switzerland took place at our department in 2019. The team of external auditors consisted of a cardiac electrophysiologist, an interventional cardiologist, a medical physicist and an allied professional working in the catheterisation laboratory. By reducing the usage of cine acquisitions, there was a significant reduction in patient radiation exposure for conventional pacemaker implantation [9].
Additionally, national diagnostic reference levels are used to help guide good clinical practice. If patient dose values consistently surpass the established diagnostic reference levels, it is recommended to take corrective actions by assessing and potentially amending practice or the configuration of X-ray systems [3, 7, 10]. Local diagnostic reference levels can also be used to further monitor and optimise local practice, as irradiating protocols of radiological devices and training of operators may improve over time.
The aim of this study was to establish local diagnostic reference levels for cardiac implantable electronic device procedures at a tertiary care centre and to compare the local values to the currently available national Swiss diagnostic reference levels.
We conducted a single-centre retrospective cohort study including all consecutive patients who underwent a cardiac implantable electronic device procedure between October 2018 and October 2020 at University Hospital Zurich. The approval of the ethics committee (BASEC-Nr. 2022-01326) was obtained and the study was conducted in accordance with the ethical standards laid down in the Declaration of Helsinki.
Cardiac implantable electronic device procedures included pacemaker (including leadless), implantable cardioverter defibrillator (ICD) and cardiac resynchronisation therapy (CRT) implantation, as well as lead extractions / device explantation. We excluded patients who were incorrectly included (for example twice), had their procedure cancelled, underwent a procedure other than those mentioned above (such as subcutaneous ICD implantation or box changes)or where data was missing (figure 1).
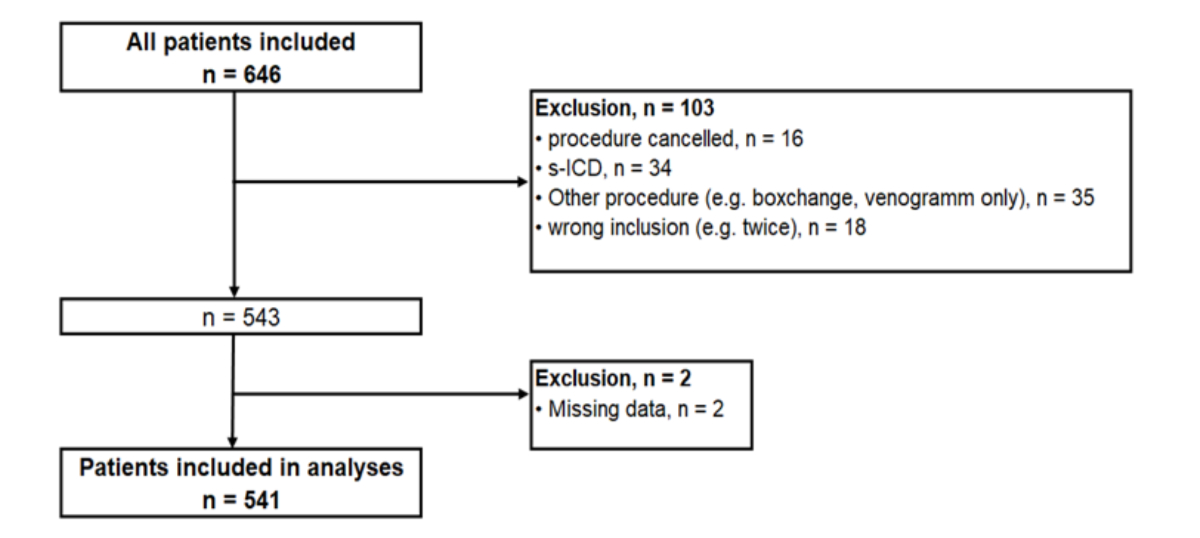
Figure 1Patient flowchart shown for the 646 patients included. The reasons for exclusion and the absolute numbers of patients excluded are shown in the boxes on the right. 541 patients were included in the final analysis.
In order to establish local diagnostic reference levels, the kerma area product (KAP in Gray [Gy] cm2), the incident air kerma at the patient entrance reference point (Ka,r), the fluoroscopy time (t) and the number of cine acquisitions were assessed. Ka,r, also known as the cumulative dose at the reference point and expressed in milligray (mGy), is the air kerma measured at 15 cm from the isocentre towards the X-ray tube. The isocentre is the midpoint between the X-ray tube and the detector. The reference point corresponds to the point where the X-ray beam enters a medium-sized patient – practically in interventional cardiology, the skin of the patient’s back – and is used to estimate patient tissue reactions. t corresponds to the time that the X-ray tube was on and includes the time for fluoroscopy and cine acquisitions. Cine acquisitions are pulsed images produced during the cine runs. All procedures were performed with a biplane cardiology system Artis Q.zen biplane (Siemens Healthcare AG) equipped with two flat-panel detectors 20 cm × 20 cm.
Data was collected from a dose management system (DMS, DOSE, Qaelum NV, Belgium) and was cross-checked for accuracy with the patient information system. The primary outcome was patient radiation exposure and was pre-specified. The median values of the overall kerma area product, cumulative dose and fluoroscopy time were set as typical / medical values for different procedures, more specifically pacemakers, leadless pacemakers, ICD, CRT and lead extraction / device explantation, and were used for comparison with national diagnostic reference levels [11]. R studio version 4.2.3 was used to perform all statistical analyses.
We analysed in total 541 cardiac implantable electronic device procedures. The results of our first analysis were recently published [9] so we hereby present the results focusing on diagnostic reference levels.
The baseline characteristics of the patients included in the study are presented in table 1. The median age was 73 years and 69% were male. 50% of patients underwent pacemaker implantation (including leadless pacemakers), most commonly due to a higher-degree AV block (24.2%). 21.1% of patients received an ICD, 17.2% a CRT and 11.5% underwent lead extraction / device explantation (table 2). The acute procedural success rate and 30-day complications are also shown in table 1. The overall acute procedural success rate was 98.7%. In total, 33 complications (6.1%) were reported within 30 days of the procedure.
Table 1Baseline characteristics, acute procedural success and 30-day complications shown for all patients. Continuous variables are presented as medians (interquartile range); categorical variables are presented as counts (percentage).
| n = 541 | |||
| Age (years) | 73.0 (61.0–80.3) | ||
| Sex: male | 372 (68.8%) | ||
| BMI (kg/m2) | 26.7 (23.3–29.4) | ||
| Medical history | Arterial hypertension | 336 (62.1%) | |
| Dyslipidaemia | 349 (64.5%) | ||
| Diabetes mellitus | 124 (22.9%) | ||
| Smoking | 276 (51.0%) | ||
| Coronary artery disease | 240 (44.4%) | ||
| Atrial fibrillation / flutter | 236 (43.6%) | ||
| Left ventricular ejection fraction | ≥50% | 293 (54.2%) | |
| 41–49% | 72 (13.3%) | ||
| ≤40% | 176 (32.5%) | ||
| Preprocedural medication | Oral anticoagulation | 241 (44.5%) | |
| Platelet aggregation inhibition | 221 (40.9%) | ||
| Beta-blockers | 270 (49.9%) | ||
| Antiarrhythmic medication | 58 (10.7%) | ||
| Acute procedural success | 534 (98.7%) | ||
| Complications | Total | 33 (6.1%) | |
| Cardiovascular death | 3 (0.6%) | ||
| Pneumothorax with chest drain | 5 (0.9%) | ||
| Pneumothorax with conservative management | 1 (0.2%) | ||
| Haemodynamically relevant pericardial effusion | 5 (0.9%) | ||
| Acute heart failure with hospitalisation | 5 (0.9%) | ||
| Severe tricuspid regurgitation | 2 (0.4%) | ||
| Lead dislocation with revision | 10 (1.8%) | ||
| Pocket haematoma with evacuation | 1 (0.2%) | ||
| Deep vein thrombosis left arm | 1 (0.2%) | ||
| Device infections | 0 (0%) | ||
Table 2Indication and type of procedure for all patients (n = 541). Values presented as count (percentage).
| Indications and procedures | n | |
| Indication for pacing | Intermittent higher-degree AV block | 131 (24.2%) |
| Complete higher-degree AV block | 103 (19.0%) | |
| Sinus node dysfunction | 113 (20.9%) | |
| Bundle branch block and heart failure | 69 (12.8%) | |
| Indication for defibrillator | Primary prevention | 72 (13.3%) |
| Secondary prevention | 49 (9.1%) | |
| Pacemaker | Total | 153 (28.3%) |
| Single chamber | 5 (0.9%) | |
| Dual chamber | 148 (27.4%) | |
| Leadless pacemaker | Total | 119 (22%) |
| Implantable cardioverter defibrillator (ICD) | Total | 114 (21.1%) |
| Single chamber | 68 (12.6%) | |
| Dual chamber | 46 (8.5%) | |
| Cardiac resynchronisation therapy (CRT) | Total | 93 (17.2%) |
| CRT-P | 35 (6.5%) | |
| CRT-D | 58 (10.7%) | |
| Lead extraction/ device explantation | 62 (11.5%) | |
Local diagnostic reference levels for the kerma area product, the cumulative dose and the fluoroscopy time are presented for the different types of procedure – pacemakers, leadless pacemakers, ICDs, CRT, and lead extraction / device explantation – in table 3. The currently available national diagnostic reference levels according to the Swiss Federal Office of Public Health (FOPH) [12] are also presented in the same table to facilitate the comparison.
Table 3Local and national diagnostic reference levels for the different types of procedures. Median values (typical values) are used as local diagnostic reference levels (LDRLs). The data is presented as median (IQR); outliers beyond the three standard deviation intervals were removed.
| Type of procedure | Kerma area product (KAP in Gray∙cm2) | Cumulative dose (mGy) | Fluoroscopy time (s) | |||
| Local values: median (IQR) | National diagnostic reference levels | Local values: median (IQR) | National diagnostic reference levels | Local values: median (IQR) | National diagnostic reference levels | |
| Pacemaker | 0.4 (0.3–0.6) | 30 | 2.7 (1.6–4.2) | 450 | 265.0 (190.5–386.0) | 600 |
| Implantable cardioverter defibrillator (ICD) | 0.4 (0.2–0.8) | 20 | 2.5 (1.3–5.3) | 418 | 253.5 (172.2–372.0) | 420 |
| Cardiac resynchronisation therapy (CRT) | 10.2 (5.7–20.3) | 57 | 113.8 (57.5–258.6) | – | 1006.0 (689.0–1423) | 3360 |
| Lead extraction / device explantation | 3.5 (0.7–10.9) | – | 28.5 (4.0–94.3) | – | 390.0 (148.0–755.5) | – |
| Leadless pacemaker | 6.3 (3.7–13.2) | – | 52.3 (29.4–93.7) | – | 232.0 (161.5–388.0) | – |
Typical values were used as local diagnostic reference levels. The local diagnostic reference levels for the kerma area product were lower than national diagnostic reference levels (0.4 Gy∙cm2 vs 30 Gy∙cm2 for pacemakers, 0.4 Gy∙cm2 vs 20 Gy∙cm2 for ICDs, 10.2 Gy∙cm2 vs 57 Gy∙cm2 for CRTs, respectively). Similarly, the local diagnostic reference levels for the cumulative dose (in mGy) and the fluoroscopy time (in seconds) were lower than national diagnostic reference levels with 2.7 mGy vs 450 mGy and 265 s vs 600 s for pacemakers; 2.5 mGy vs 418 mGy and 254 s vs 420 s for ICDs; and 1006 s vs 3360 s for CRTs, respectively. National diagnostic reference levels for the implantation of leadless pacemakers and for lead extraction / device explantation are not available yet. No diagnostic reference level values are provided for cine acquisition, for none of the procedures or for the cumulative dose for CRT implantations. The local diagnostic reference levels for cine acquisitions were 10 images for pacemaker and 100 for leadless pacemakers, 6 images for ICD, 171 images for CRT and 121 images for lead extraction / device explantation.
This retrospective cohort study assessed patient radiation exposure during device procedures by establishing local diagnostic reference levels and comparing them with the national diagnostic reference levels.
The local diagnostic reference levels for kerma area product, cumulative dose and fluoroscopy time during pacemaker, implantable cardioverter defibrillator (ICD) and cardiac resynchronisation therapy (CRT) implantations were notably far below the currently available national diagnostic reference levels established by the Federal Office of Public Health in 2018 [12]. This suggests that national diagnostic reference levels need to be updated more regularly, e.g. every 3 to 5 years. In comparison to current literature, the local diagnostic reference levels set at our institution for kerma area product during pacemaker / ICD implantations were lower than those reported in recent studies, with the kerma area product ranging from 2.0 to 20.9 Gy∙cm2 in recent studies from other groups. Similarly, the kerma area product for CRT implantations varied from 7.7 to 40.9 Gy∙cm2 [13–15]. The local diagnostic reference levels for fluoroscopy time during pacemaker / ICD implantations and CRT implantations were similar to the fluoroscopy time presented in a large retrospective study on 2055 device implantations conducted in Italy over a 7-year period [13].
Regarding patient radiation exposure during lead extraction / explantation, information in the literature is scarce [16]. For leadless pacemakers, our results extend and corroborate the findings of an observational study from two tertiary electrophysiology referral centres in Switzerland. However, national diagnostic reference levels for leadless pacemaker implantations have not yet been established by the Federal Office of Public Health since this is a rather novel technology. It is important that pacemaker implantations are clearly distinguished by device type, as leadless pacemakers often need longer fluoroscopy time and radiation exposure than conventional pacemakers due to the different access (mostly femoral) and differences in implant procedure.
We observed low patient radiation exposure during cardiac implantable electronic device interventions. We attribute this to optimised operator practices and evolving technology since the publication of the national diagnostic reference levels. First, we try to minimise the number of cine acquisitions as the related radiation dose typically exceeds the fluoroscopy dose by 10 times [3]. Additionally, protocols are by default set at 3 frames per second and we only use higher frame rates if the interventionists need better temporal resolution. This aligns with the results of a retrospective study involving 495 patients, showing that the reduction of the frame rate by half led to a 62% decrease in radiation dose during device procedures [14]. Our results confirmed that our goal should remain to minimise cine usage as much as possible. Furthermore, continuous education of personnel on optimising patient exposure by using a low frame rate and acquiring the fewest possible cine images help keep the radiation doses at low levels. Thus, setting national diagnostic reference level values for cine acquisitions during cardiac implantable electronic device procedures is essential.
To mitigate information bias, data was checked thoroughly, with two patients having to be excluded due to missing data. Performed procedures were heterogeneous and varied in complexity, making the establishment of diagnostic reference levels more challenging, however more representative. We recognise that data obtained solely from a single centre may lack representativeness as a standard. A multicentre approach to assess patient radiation exposure is strongly desired to establish revised national diagnostic reference levels.
Local diagnostic reference levels helped to increase awareness and review local practices for improvements in patient and operator protection. Regarding diagnostic reference levels, local values were far below the national diagnostic reference levels, which suggests that national diagnostic reference levels need to be updated more regularly to take into account the optimised protocols as well as new types of procedures.
The data that support the findings of this study is available in anonymised form from the corresponding author, AS, upon reasonable request.
We wish to thank the patients who participated in this study as well as the clinical teams caring for them
This study received no funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Julia Hermes-Laufer received speaker fees for device presentation for Abbot 2022 and educational grants and travel support from Biotronic, not related to this article. – Matthias Guckenberger received consulting fees from Varian and AstraZeneca, not related to this article. – Daniel Hofer reports educational grants, consultant or speaker fees, and fellowship support from Abbott, Medtronic, Biotronik, Boston Scientific, Biosense Webster, Novartis, Bayer, Pfizer, and Spectranetics, not related to this article. – Alexander Breitenstein has received consultant and/or speaker fees from Abbott, Bayer Healthcare, Biosense Webster, Biotronik, Boston Scientific, Bristol-Myers Squibb, Cook Medical, Daiichi Sankyo, Medtronic, Pfizer, Zoll and Spectranetics/Philipps, not related to this article. – Ardan M. Saguner received educational grants through his institution from Abbott, Bayer Healthcare, Biosense Webster, Biotronik, Boston Scientific, Bristol-Myers Squibb/Pfizer and Medtronic; and speaker / advisory board / consulting fees from Bayer Healthcare, Biotronik, Medtronic, Novartis, Pfizer, Stride Bio Inc and Zoll, not related to this article. He has stock or stock options from Gilead Sciences.
1. Raatikainen MJ, Arnar DO, Zeppenfeld K, Merino JL, Levya F, Hindriks G, et al. Statistics on the use of cardiac electronic devices and electrophysiological procedures in the European Society of Cardiology countries: 2014 report from the European Heart Rhythm Association. Europace. 2015 Jan;17 Suppl 1:i1–75. doi: https://doi.org/10.1093/europace/euu300
2. Report N. 184 – Medical Radiation Exposure of Patients in the United States (2019). National Council on Radiation Protection and Measurements. 2019.
3. Heidbuchel H, Wittkampf FH, Vano E, Ernst S, Schilling R, Picano E, et al. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014 Jul;16(7):946–64. doi: https://doi.org/10.1093/europace/eut409
4. Picano E, Vañó E, Rehani MM, Cuocolo A, Mont L, Bodi V, et al. The appropriate and justified use of medical radiation in cardiovascular imaging: a position document of the ESC Associations of Cardiovascular Imaging, Percutaneous Cardiovascular Interventions and Electrophysiology. Eur Heart J. 2014 Mar;35(10):665–72. doi: https://doi.org/10.1093/eurheartj/eht394
5. Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009 Aug;361(9):849–57. doi: https://doi.org/10.1056/NEJMoa0901249
6. Gerber TC, Carr JJ, Arai AE, Dixon RL, Ferrari VA, Gomes AS, et al. Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 2009 Feb;119(7):1056–65. doi: https://doi.org/10.1161/CIRCULATIONAHA.108.191650
7. Vañó E, Miller DL, Martin CJ, Rehani MM, Kang K, Rosenstein M, et al.; Authors on behalf of ICRP. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann ICRP. 2017 Oct;46(1):1–144. doi: https://doi.org/10.1177/0146645317717209
8. Council of the European Union. Council Directive 2013/59/EURATOM. Official Journal of the European Union. 2013. Availabe from: https://eur-lex.europa.eu/eli/dir/2013/59/oj/eng
9. Sazgary L, Samara ET, Stüssi A, Saltybaeva N, Guckenberger M, Ruschitzka F, et al. Impact of clinical radiation audits on patient radiation exposure in cardiac implantable electronic device procedures. Heart Rhythm. 2024 Oct;21(10):2046–7. doi: https://doi.org/10.1016/j.hrthm.2024.04.060
10. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37(2-4):1–332.
11. Damilakis J, Frija G, Brkljacic B, Vano E, Loose R, Paulo G, et al.; European Society of Radiology. How to establish and use local diagnostic reference levels: an ESR EuroSafe Imaging expert statement. Insights Imaging. 2023 Feb;14(1):27. doi: https://doi.org/10.1186/s13244-023-01369-x
12. Swiss Federal Office of Public Health (FOPH). Diagnostische Referenzwerte (DRW) für interventionelle radiologische Anwendungen. BAG. 2018. Wegleitung R-06-05. p.1–5. Availabe from: https://www.bag.admin.ch/bag/de/home/gesetze-und-bewilligungen/gesuche-bewilligungen/bewilligungen-aufsicht-im-strahlenschutz/informationen-fuer-medizinische-betriebe/diagnostische-referenzwerte-im-strahlenschutz.html
13. Casella M, Dello Russo A, Russo E, Catto V, Pizzamiglio F, Zucchetti M, et al. X-Ray Exposure in Cardiac Electrophysiology: A Retrospective Analysis in 8150 Patients Over 7 Years of Activity in a Modern, Large-Volume Laboratory. J Am Heart Assoc. 2018 May;7(11):e008233. doi: https://doi.org/10.1161/JAHA.117.008233
14. Bork FT, Boehmer AA, Zezyk C, Kaess BM, Ehrlich JR. Frame-rate reduction to reduce radiation dose for cardiac device implantation is safe. Heart Rhythm O2. 2023 May;4(7):427–32. doi: https://doi.org/10.1016/j.hroo.2023.05.003
15. Thibault B, Andrade JG, Dubuc M, Talajic M, Guerra PG, Dyrda K, et al. Reducing radiation exposure during CRT implant procedures: early experience with a sensor-based navigation system. Pacing Clin Electrophysiol. 2015 Jan;38(1):63–70. doi: https://doi.org/10.1111/pace.12522
16. Haeberlin A, Kozhuharov N, Knecht S, Tanner H, Schaer B, Noti F, et al. Leadless pacemaker implantation quality: importance of the operator’s experience. Europace. 2020 Jun;22(6):939–46. doi: https://doi.org/10.1093/europace/euaa097