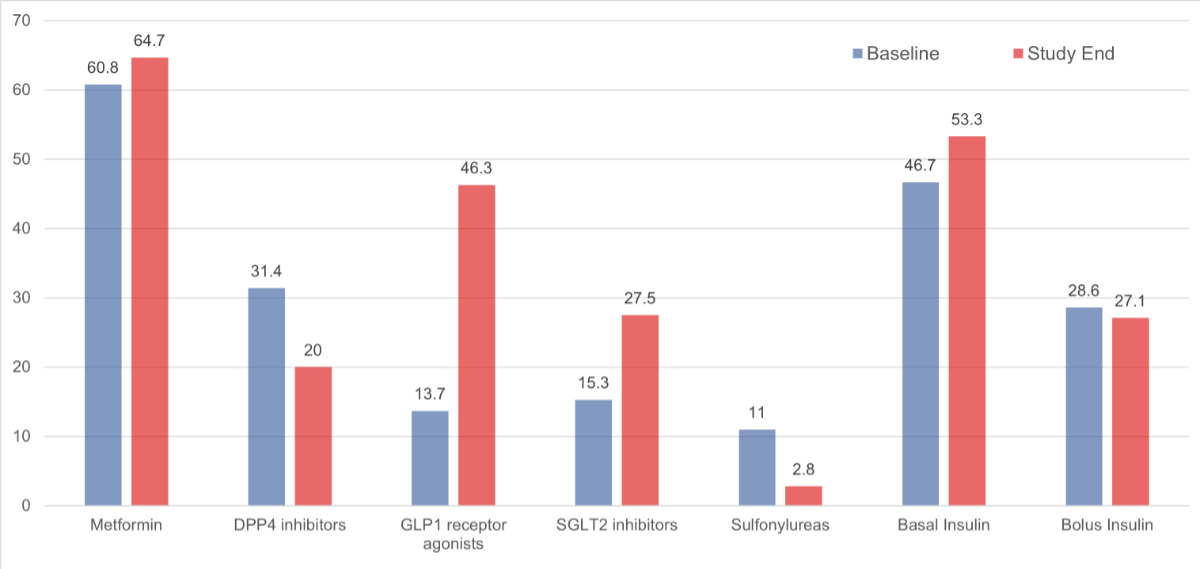
Figure 1Medication changes from baseline (blue) to study end (red). DPP4: Dipeptidyl peptidase-4; GLP1: glucagon-like peptide-1; SGLT2: sodium-glucose cotransporter 2.
DOI: https://doi.org/https://doi.org/10.57187/s.4031
Alanine aminotransferase
Aspartate aminotransferase
Body mass index
Dipeptidyl peptidase-4
Glucagon-like peptide-1
Glycated haemoglobin
Low-density lipoprotein
Sodium-glucose cotransporter 2
Type 2 diabetes mellitus is a major global health threat with a substantial social, economic and health burden [1–3]. Patients with type 2 diabetes mellitus are typically managed by general practitioners when management can be accomplished without sophisticated basal-bolus insulin therapy. However, when patients with long-standing type 2 diabetes mellitus show signs and symptoms of significant beta-cell dysfunction they are typically referred to a specialised outpatient diabetes centre.
The care of patients with type 2 diabetes mellitus is highly complex as it involves not only adequate glycaemic control, but also regular monitoring of body weight, control of cardiovascular risk factors (blood pressure, nicotine abuse, low-density lipoprotein [LDL] cholesterol), liver enzymes, and assessment of complications of type 2 diabetes mellitus in order to prevent macro- [4–6] and microvascular complications [5, 7, 8]. In addition, the management of patients with type 2 diabetes mellitus has become even more challenging for general practitioners due to the introduction of modern therapeutic options, such as glucagon-like peptide-1 (GLP1) receptor agonists and sodium-glucose cotransporter 2 (SGLT2) inhibitors [9]; both have established evidence for cardiovascular and renal benefits [10–12]. However, the number of therapeutic options within the same class of drugs is large and it can be difficult for general practitioners to maintain an overview.
It has not been established whether referral of patients with type 2 diabetes mellitus to an outpatient diabetes centre leads to significant improvements in clinical and metabolic parameters. Therefore, the aim of this study was to investigate the changes from baseline, in parameters of glycaemic and metabolic control, following adoption of a “pitstop” approach including a short-term assessment and intervention by a diabetologist (with an interprofessional approach, if needed) for patients with type 2 diabetes mellitus referred to an outpatient diabetes centre.
This study included all patients ≥18 years of age with type 2 diabetes mellitus who were referred by their general practitioner for evaluation/therapy at the outpatient diabetes centre of the regional hospital of the Gesundheitszentrum Fricktal in the Northern part of Switzerland, between 1 January 2019 and 31 December 2020. The Gesundheitszentrum Fricktal is a regional health centre with several locations, including Rheinfelden, where all the consultations relevant for this study took place. As a whole, the Gesundheitszentrum Fricktal treats around 9000 inpatients and around 50,000 outpatients per year. This includes internal medicine, surgery, orthopaedic surgery, gynaecology and obstetrics, as well as diagnostic procedures. For some years now, there has been a close collaboration with University Hospital Basel in endocrinology and diabetology. The study presented here was also conducted as part of this collaboration.
Patients were scheduled for a diabetologist assessment, which typically included two to three consultations. The duration of the diabetes specialist assessment was defined as the time between the first and last consultation at the diabetes centre. Patients with type 1 diabetes mellitus or gestational diabetes and patients who had been referred to another outpatient diabetologist or endocrinologist within the last year were excluded.
The primary outcome was the change in glycated haemoglobin (HbA1c) between the first and last consultation. Secondary endpoints included duration of intervention and changes in body weight, systolic and diastolic blood pressure, LDL cholesterol and usage of antidiabetic drug classes from baseline to the last visit. In addition, we aimed to describe the population under investigation as well as possible. To this end, we assessed their cardiovascular risk using all available parameters (age, sex, LDL cholesterol, smoking status, blood pressure and body mass index [BMI]).
We further assessed diabetic complications, encompassing macrovascular complications (i.e. coronary artery disease, cerebrovascular disease, peripheral artery disease), microvascular complications (i.e. diabetic retinopathy, diabetic nephropathy, diabetic neuropathy) and autonomic dysfunction (erectile dysfunction, orthostatic dysfunction, gastroparesis and diabetic foot syndrome).
These data were collected from electronic medical charts as well as during the consultation, including demographics, body weight, BMI, systolic and diastolic blood pressure, neuropathy assessment and smoking status.
Over 90% of the laboratory parameters used for this study were measured at the Gesundheitszentrum Fricktal during consultations using the on-site laboratory. The remaining laboratory parameters were collected from the patients’ referral documents. When evaluating the laboratory results (HbA1c, LDL cholesterol, ASAT, ALAT, microalbuminuria), we adhered to the limit values of the local laboratory and current guidelines.
Assessment of complications, cardiovascular risk factors as well as established cardiovascular diseases was based on the diagnosis by the diabetologist in charge; or referral letters/external reports from general practitioners, cardiologists or ophthalmologists.
Baseline data were defined as those obtained at the first consultation with the diabetologist, and follow-up data as those obtained at the last consultation before patients were referred back to the general practitioner.
In addition, all antidiabetic, antihypertensive, lipid-lowering and antithrombotic drugs were recorded at baseline and at the last visit. (All other concomitant prescribed drugs were reported as polypharmacy if a patient was prescribed more than four different additional drugs.)
Categorical variables are expressed as counts (percentages) and continuous variables as medians (interquartile ranges [IQR]), unless stated otherwise. Data were tested against a normal distribution using the Shapiro-Wilk test. We used a paired t-test to compare end-of-study variables with baseline variables. In case of non-normal distribution, the Wilcoxon matched-pair test was used. All p-values are two-sided and confidence intervals (CIs) are at the 95% level. Statistical analyses were performed using STATA 17.0 (Stata Corp, College Station, TX, USA).
The Ethics Committee Northwestern and Central Switzerland (EKNZ) approved this study (ID AO 2020-00032) on 11 November 2020. This research project falls outside the scope of Human Research Act article 51.
Baseline characteristics of all patients are summarised in table 1 and in some parts shown in table 2 and figure 1. Over the study period, 699 consecutive patients met the age criterion and so were eligible. Of them, 255 patients had been referred following a diagnosis of type 2 diabetes mellitus. Data from these 255 patients were extracted and analysed in the study. The median age was 66 years (IQR 58–75) and the majority (63.1%) were male. The majority of patients were obese (median BMI 31.0 kg/m2, IQR 28.0–34.8) with blood pressure measurements slightly elevated (systolic blood pressure 143 mm Hg, IQR 130–154). Mean HbA1c showed insufficient diabetes control (8.6% or 70.5 mmol/mol). The most common cardiovascular risk factor was hypertension with a prevalence of 73.3%, followed by dyslipidaemia diagnosed in 71.0% of patients. Obesity was documented in 55.3% of the patients. At baseline, coronary artery disease was diagnosed in 44 (17.3%) patients, peripheral arterial disease in 23 (9%) patients and cerebrovascular disease in 11 (4.3%) patients. Among microvascular complications, diabetic nephropathy was diagnosed in almost one-third of patients (31%), polyneuropathy in 36.1% and disorders of the autonomic nervous system in 9 (3.5%) patients. The most prescribed antidiabetic drug was metformin (155 patients or 60.8%), followed by basal insulin (119 patients or 46.7%) and dipeptidyl peptidase-4 (DPP4) inhibitors (80 patients or 31.4%). Modern antidiabetic drugs were less commonly prescribed: GLP1 receptor agonists in 13.7% and SGLT2 inhibitors in 15.3% of patients. For details, see figure 1. In addition to the above medications, each patient had an average of 3.2 other medications listed (range 0–17).
Table 1Baseline characteristics of included patients. Data are n (%) or median (interquartile range).
| Characteristic | Subgroup | Total (n = 255) |
| Age in years | 66 (58–75) | |
| Sex | Male | 161 (63.1%) |
| Female | 94 (36.9%) | |
| Family status | Unknown | 13 (5.1%) |
| Married | 148 (58.0%) | |
| Unmarried | 33 (12.9%) | |
| Divorced | 33 (12.9%) | |
| Widowed | 22 (8.6%) | |
| Separated | 6 (2.4%) | |
| Comorbidities | ||
| Cardiovascular risk factors | Dyslipidaemia | 181 (71.0%) |
| Hypertension | 187 (73.3%) | |
| Obesity | 141 (55.3%) | |
| Macrovascular complications | Coronary artery disease | 44 (17.3%) |
| Cerebrovascular disease | 11 (4.3%) | |
| Peripheral artery disease | 23 (9.0%) | |
| Obstructive sleep apnoea | 42 (16.5%) | |
| Microvascular complications | Retinopathy | 44 (17.3%) |
| Nephropathy | 79 (31.0%) | |
| Polyneuropathy | 92 (36.1%) | |
| Laboratory results | ||
| eGFR in ml/min/1.73 m2 | 84 (57–99) | |
| ALAT in U/l | 28 (19–38) | |
| ASAT in U/l | 24 (20–33) | |
| Albumin-creatinine ratio | 2.5 (0.5–15.2) | |
ALAT: alanine aminotransferase; ASAT: aspartate aminotransferase; eGFR: estimated glomerular filtration rate.
Table 2Primary and secondary outcomes. Changes in primary and secondary outcomes from baseline to the last consultation. Values at baseline and study end are presented as mean (standard deviation) or median (interquartile range). For statistical analyses, the Wilcoxon matched-pair test was used for body weight, body mass index and blood pressure. CI: confidence interval; HbA1c: haemoglobin A1c; LDL: low-density lipoprotein.
| Outcome | Baseline | Study end | Change from baseline (95% CI) | p-value | |
| Primary outcome | HbA1c (%) / (mmol/mol) | 8.6 / 70.5 (1.8) | 7.3 / 56.3 (1.2) | −1.28 / −14.2 (−1.50 to −1.05) | <0.001 |
| Secondary outcome | Body weight (kg) | 91.0 (81.0–100.0) | 88.0 (79.7–98.3) | −3.9 (−4.9 to −3.0) | <0.001 |
| Body mass index in (kg/m2) | 31.0 (28.0– 34.8) | 30.1 (27.1–33.8) | −1.5 (−1.9 to −1.0) | <0.001 | |
| Systolic blood pressure (mm Hg) | 143 (130– 154) | 141 (128–150) | −1.6 (−2.7 to −0.5) | 0.04 | |
| Diastolic blood pressure (mm Hg) | 85 (76–93) | 85 (75–92) | −0.5 (−1.0 to 0.0) | 0.47 | |
| LDL cholesterol (mmol/l) | 2.50 (1.25) | 2.64 (1.17) | −0.05 (−0.13 to 0.02) | 0.16 | |
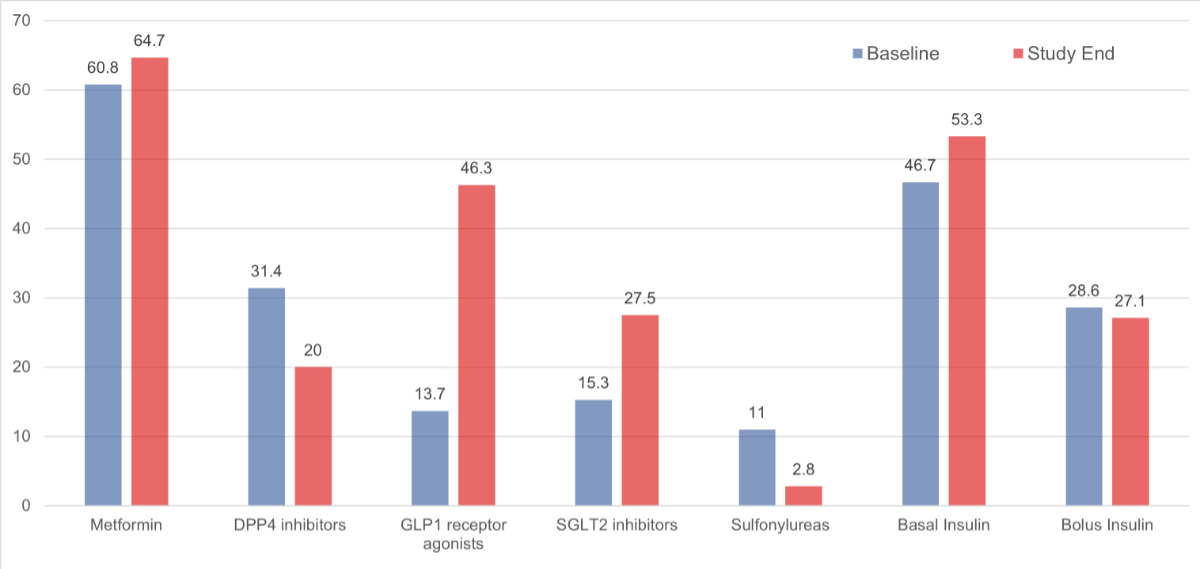
Figure 1Medication changes from baseline (blue) to study end (red). DPP4: Dipeptidyl peptidase-4; GLP1: glucagon-like peptide-1; SGLT2: sodium-glucose cotransporter 2.
The median follow-up time between the first and last visit to the outpatient diabetes centre was 5.1 months (IQR 3.0–9.1). During this time period, patients had a mean of 3.4 (standard deviation [SD] 3.0) consultations with the diabetologist, and 23 patients had a mean of 1.7 consultations with a specialised diabetes nurse that were prescribed as needed.
At the end of the intervention, there was a significant improvement in glycaemic control mirrored by a mean change in HbA1c of −1.28% or −14.2 mmol/mol (95% CI −1.50 to −1.05; median change −0.90%) (table 2). In total, 191 individuals (74.9%) experienced an improvement in their glycaemic control. The heterogeneity in the HbA1c change from baseline is depicted in figure 2; the best result was an 8.0% improvement while the worst was a 2.3% deterioration.
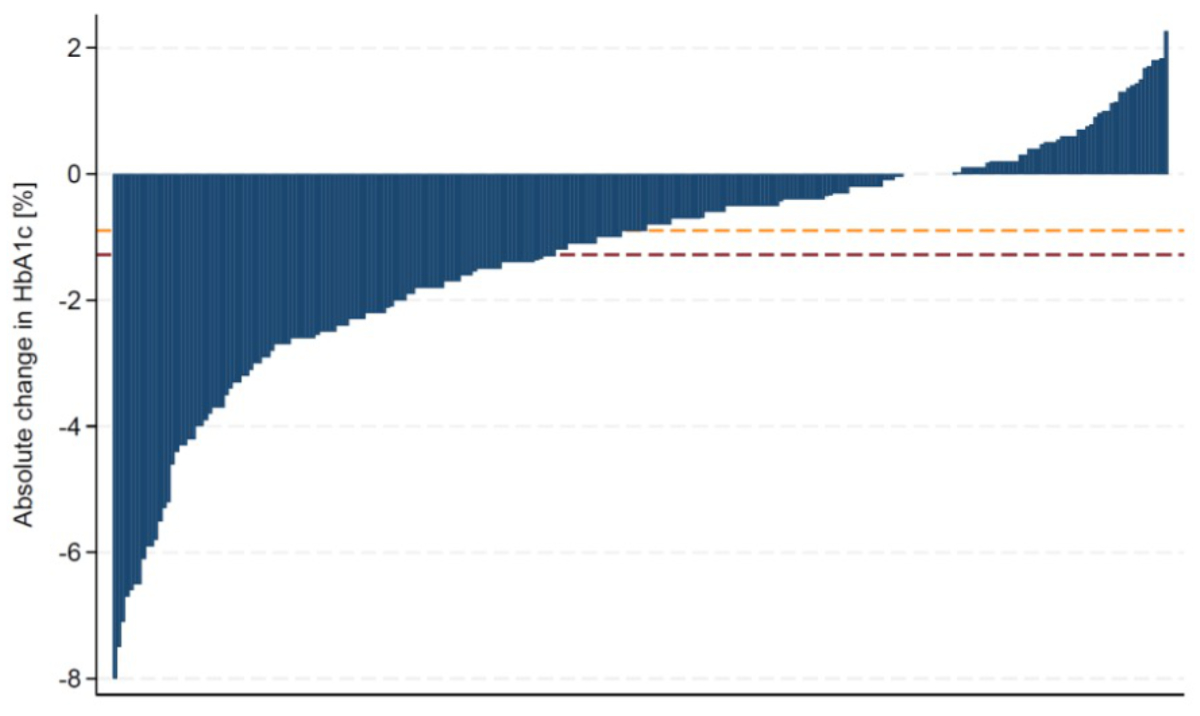
Figure 2Waterfall plot of HbA1c change from baseline. The majority of individuals (191/255; 74.9%) had an improvement. The orange dashed line represents the median change (−0.90%). The dark red dashed line represents the mean change (−1.28%). HbA1c: Glycated haemoglobin.
At the end of the intervention, individuals had a mean change in body weight of −3.9 (95% CI −4.9 to −3.0). Furthermore, slight improvements in systolic blood pressure were documented (table 2). However, there was no significant change in LDL cholesterol levels and urine albumin-to-creatinine ratio.
In total, 183 patients (71.8%) had a change in treatment, while 72 patients (28.2%) had no change in their antidiabetic medication or concomitant medications (lipid-lowering, antihypertensive and antithrombotic drugs). While the overall use of metformin remained almost unchanged (155 [60.8%] vs 165 [64.7%]), the pitstop approach resulted in decreased prescriptions for sulfonylureas (28 [11.0%] vs 7 [2.8%]) and DPP4 inhibitors (80 [31.4%] vs 51 [20.0%]), but an increased prescription for SGLT2 inhibitors (39 [15.3%] vs 70 [27.5%]) and GLP1 receptor agonists (35 [13.7%] vs 118 [46.3%]) (figure 1). The use of lipid-lowering, antihypertensive or antithrombotic drugs did not change significantly after the intervention.
The key findings of this study investigating the changes in HbA1c and other cardiometabolic parameters following a short-term diabetologist intervention (the “pitstop” approach) among 255 patients with type 2 diabetes mellitus are as follows: First, after a median intervention time of 5.1 months, patients achieved significant improvements in glycaemic control and body weight. Second, after the intervention, there was a significantly higher use of antidiabetic drugs with proven effect on micro- and macrovascular complications (GLP1 receptor agonists and/or SGLT2 inhibitors).
The baseline characteristics concerning age and HbA1c are comparable with those of type 2 diabetes mellitus patients in previous studies [13–15]. Studies conducted exclusively in a primary care setting have shown a lower mean HbA1c [16–18] probably due to the fact that our study population was mostly referred due to their insufficient glycaemic control [19]. Self-management and primary care programmes have lowered HbA1c by 0.6–1.4% in follow-up periods ranging from 6 months to a year [20, 21]. A meta-analysis summarising the effect of integrated diabetes care interventions showed a decrease of 0.77% among pre-post studies [14]. Furthermore, the proportions of microvascular and macrovascular complications are consistent with data in the literature [5]. Therefore, the results of this study are comparable and applicable to other primary care patients with type 2 diabetes mellitus in the industrialised world referred to a specialist.
The significant changes in HbA1c and weight can most likely be attributed to changes in drug treatment and possibly lifestyle interventions, but not exclusively [13, 22]. For example, real-world studies in comparable settings in Switzerland and Canada only showed an HbA1c reduction of 0.8% / 9 mmol/mol and 0.9% / 10 mmol/mol, respectively, just 7.5 months after starting a GLP-1 analogue in addition to a similar baseline medication. And at the end of these two studies, over 95% of the patients had received a GLP-1 analogue, whereas in our study only slightly less than one-third had received a new GLP-1 analogue and about one-eighth a new SGLT-2 inhibitor [23, 24]. The involvement of paramedical professionals like specialist diabetes nurses and/or dietitians as suggested by current guidelines may have contributed to the findings and are usually not available in general practitioner practices [25–27].
Thus, similar results concerning an HbA1c decrease were shown by Sousa et al. where the impact of a change of the treating physician within an endocrinological outpatient clinic was examined [28].
The final mean HbA1c of 7.3% seems to be quite high. While the majority of patients would be classified as uncontrolled on the basis of the classic threshold of 6.5% /48 mmol/mol a true proportion of controlled vs uncontrolled patients cannot be provided as the threshold is defined individually, based on age, established cardiovascular diseases and secondary diabetes-induced complications, besides others. Although evidence for the use of GLP1 receptor agonists and SGLT2 inhibitors for patients with a cardiorenal indication is overwhelming and clearly recommended [29, 30]. Although information on individual HbA1c goals was not available in the medical charts, taking into consideration the mean age of 65 years and the fact that more than a quarter had an established cardiovascular disease and more than half had diabetic complications, it can be assumed that the majority had achieved their individual goal.
This study provides additional evidence to support the view that concomitant cardiovascular risk factors (LDL cholesterol and blood pressure) are often not adequately controlled [16, 18, 31, 32]. The small improvements in blood pressure observed and the lack of changes in LDL cholesterol levels are related to the fact that the diabetologist usually recommended changes in cardiovascular risk factor therapy to the general practitioner but did not implement these changes immediately unlike the glucose-lowering drugs prescribed directly by the diabetologist. However, the current findings suggest that there is still room for improvement in the management of cardiovascular risk factors in patients with type 2 diabetes mellitus.
The decreasing trend in transaminases might reflect an improvement of metabolic dysfunction-associated steatotic liver disease [33].
Both interventions (modern treatment options and lifestyle counselling) can be challenging in the primary care setting, either due to time constraints or the overwhelming number of modern treatment options (GLP1 receptor agonists and SGLT2 inhibitors) in recent years [22, 34, 35]. This possibly explains the rather low rate of prescribed modern antidiabetic drugs by general practitioners in the current study at baseline, below 20%, which is consistent with the literature [36–38]. Regulatory issues are unlikely to explain these findings since the modern antidiabetic drugs are available and reimbursed in Switzerland by the health insurance, even in the primary care setting.
Although evidence for the use of GLP1 receptor agonists and SGLT2 inhibitors for patients with a cardiorenal indication is overwhelming and clearly recommended [10–12, 25–27, 29, 39], neither our study nor previous reports found a clear difference between patients with a cardiorenal risk and those without. This indicates that there is an evidence-performance gap concerning the indication of these modern drugs [35–37]. For instance in our study, only 40 of 58 patients (68.9%) with established macrovascular complications (coronary artery disease, cerebrovascular disease, peripheral artery disease) had a prescribed treatment with proven impact on macrovascular complications. Of the 44 patients with coronary artery disease, 11 (25%) received neither a GLP1 receptor agonist nor an SGLT2 inhibitor. Interestingly, a German study in the primary care setting found an association between GLP1 receptor agonist prescription and higher BMI, younger age, private health insurance and treatment by a diabetologist [40]. However these findings could not be confirmed by Perera et al., who deliberately chose a study population that was older and had more comorbidities yet still reported a rate of modern antidiabetic drugs below 20% [41]. Similarly, the number of sulfonylureas, which are no longer recommended due to their inherent risk of hypoglycaemias [29], was still quite high [41]. Only one study conducted in a US primary care medical centre – using a quality improvement intervention focusing on care of patients with type 2 diabetes mellitus based on a four-step knowledge translation model – showed a higher prescription rate of modern antidiabetic drugs [42]. Taken together, the findings of underuse of modern antidiabetic drugs in our study are consistent with previous reports. It is likely that there is a well-known latency period before evidence-based recommendations find their way into “real life” [43].
The intervention period of less than six months is relatively short in the context of a chronic disease. This indicates that the concept of a “pitstop” in an outpatient diabetes centre is a valid option to improve overall quality of care. It remains to be seen whether other options to support general practitioners in the management of patients with type 2 diabetes mellitus, such as telemedicine, should be explored [44].
This study has several strengths. First, the study evaluated the effect of a referral to a diabetologist on the quality of care in patients with type 2 diabetes mellitus in a real-world setting. Second, detailed laboratory parameters on several metabolic parameters were systematically evaluated and exact changes in drug prescription rates are reported. Third, during the conduct of the study, the diabetologist at the outpatient centre remained unchanged, reducing confounding.
However, due to the design of the study, some limitations need to be acknowledged. One inherent limitation is the lack of a control group. Thus, we cannot exclude the possibility that the patients would have improved without the specialist’s intervention [10–12, 29, 39]. However, as described in the preceding “Primary outcome” section, it can be assumed that there is a correlation, particularly with regard to the reduction in HbA1c [25–28]. Second, underlying reasons for referral were not identical for all patients and varied from insufficient glycaemic control to optimisation of cardiovascular risk factors. However, we included all patients referred to the diabetologist for treatment of diabetes type 2 only.
A short-term intervention by an outpatient diabetes clinic was associated with significant improvements in glycaemic control and body weight. These effects were largely explained by adapting the antidiabetic treatment towards modern medications with proven cardiorenal protective properties.
The findings of this study indicate that optimal management of cardiovascular risk factors is often not achieved in the primary care setting. Communication and fruitful collaboration with general practitioners with shared responsibilities are of utmost importance for improving the management of patients with type 2 diabetes mellitus. Future studies are needed to refine the target population that benefits most, to evaluate the cost-effectiveness as well as to confirm the effectiveness of the pitstop approach on hard clinical endpoints.
All data relevant to the comprehensibility of the study are available on request from the authors.
We would like to thank the team of the Spital Rheinfelden, especially the IT team, for their great support in making this paper possible.
Author contributions: All authors conceived and designed the study. FE, SH and SZ wrote the first draft of the paper. SZ supervised the project. FE performed the statistical analyses. All authors interpreted the data and contributed to the writing of the paper. All authors revised and approved the final version.
Swiss National Science Foundation P500PM_210866 (FE).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. FE has served on an advisory board for Boehringer Ingelheim. No other potential conflict of interest related to the content of this manuscript was disclosed.
1. Williams R, Karuranga S, Malanda B, et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2020;162:108072. https://doi.org/
2. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843. https://doi.org/
3. Khan MA, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020 Mar;10(1):107–11. doi: https://doi.org/10.2991/jegh.k.191028.001
4. Huang D, Refaat M, Mohammedi K, Jayyousi A, Al Suwaidi J, Abi Khalil C. Macrovascular Complications in Patients with Diabetes and Prediabetes. BioMed Res Int. 2017;2017:7839101.
5. Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019 Dec;26 2_suppl:25–32. doi: https://doi.org/10.1177/2047487319878371
6. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017 Jun;389(10085):2239–51. doi: https://doi.org/10.1016/S0140-6736(17)30058-2
7. Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K. Microvascular Complications of Type 2 Diabetes Mellitus. Curr Vasc Pharmacol. 2020;18(2):117–24. doi: https://doi.org/10.2174/1570161117666190502103733
8. Dietrich I, Braga GA, de Melo FG, da Costa Silva Silva AC. The Diabetic Foot as a Proxy for Cardiovascular Events and Mortality Review. Curr Atheroscler Rep. 2017 Oct;19(11):44. doi: https://doi.org/10.1007/s11883-017-0680-z
9. Call JT, Cortés P, Harris DM. A practical review of diabetes mellitus type 2 treatment in primary care. Rom J Intern Med. 2022 Mar;60(1):14–23. doi: https://doi.org/10.2478/rjim-2021-0031
10. Palmer SC, Tendal B, Mustafa RA, Vandvik PO, Li S, Hao Q, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2021 Jan;372:m4573. doi: https://doi.org/10.1136/bmj.m4573
11. Sharma A, Verma S. Mechanisms by Which Glucagon-Like-Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter-2 Inhibitors Reduce Cardiovascular Risk in Adults With Type 2 Diabetes Mellitus. Can J Diabetes. 2020 Feb;44(1):93–102. doi: https://doi.org/10.1016/j.jcjd.2019.09.003
12. Standl E, Schnell O. Treatment paradigm shifting implications of recent cardiovascular outcome trials: core insights on the brink of the 2020ies. Diabetes Res Clin Pract. 2020 Mar;161:108054. doi: https://doi.org/10.1016/j.diabres.2020.108054
13. Avnat E, Chodick G, Shalev V. Identifying Profiles of Patients With Uncontrolled Type 2 Diabetes Who Would Benefit From Referral to an Endocrinologist. Endocr Pract. 2023 Nov;29(11):855–61. doi: https://doi.org/10.1016/j.eprac.2023.08.002
14. Zarora R, Immanuel J, Chivese T, MacMillan F, Simmons D. Effectiveness of Integrated Diabetes Care Interventions Involving Diabetes Specialists Working in Primary and Community Care Settings: A Systematic Review and Meta-Analysis. Int J Integr Care. 2022 May;22(2):11.
15. Hoffman AF, Roberson CL, Cohen P, Jackson VL, Yeatts J, Gregory P, et al. Improving glycemic control in diabetes through virtual interdisciplinary rounds. Am J Manag Care. 2024 Mar;30(3):e78–84. doi: https://doi.org/10.37765/ajmc.2024.89518
16. Christ E, Czock A, Renström F, Ammeter T, Ebrahimi F, Zechmann S, et al. Evaluation of type 2 diabetes care management in nine primary care practices before and after implementation of the Criteria of Good Disease Management of Diabetes established by the Swiss Society of Endocrinology and Diabetology. Swiss Med Wkly. 2022 Jul;152(2930):w30197. doi: https://doi.org/10.4414/SMW.2022.w30197
17. Vlacho B, Simarro FL, Mata-Cases M, Miravet S, Escribano-Serrano J, Asensio D, et al. Adherence to antidiabetic treatment among patients managed in primary care centres in Spain: the INTENSE study. Prim Care Diabetes. 2022 Dec;16(6):760–7. doi: https://doi.org/10.1016/j.pcd.2022.10.004
18. Meier R, Valeri F, Senn O, Rosemann T, Chmiel C. Quality performance and associated factors in Swiss diabetes care - A cross-sectional study. PLoS One. 2020 May;15(5):e0232686. doi: https://doi.org/10.1371/journal.pone.0232686
19. McAlister FA, Majumdar SR, Eurich DT, Johnson JA. The effect of specialist care within the first year on subsequent outcomes in 24,232 adults with new-onset diabetes mellitus: population-based cohort study. Qual Saf Health Care. 2007 Feb;16(1):6–11. doi: https://doi.org/10.1136/qshc.2006.018648
20. Malik RA, Hwu CM, Jammah AA, Arteaga-Díaz JM, Djaballah K, Pilorget V, et al. Real-world effectiveness and safety of insulin glargine 100 U/mL plus lixisenatide in adults with type 2 diabetes: an international, multicentre, 12-month, prospective observational study. Diabetes Obes Metab. 2024 Jul;26(7):2811–9. doi: https://doi.org/10.1111/dom.15599
21. Khanna A, Bush AL, Swint JM, Peskin MF, Street RL Jr, Naik AD. Hemoglobin A1c improvements and better diabetes-specific quality of life among participants completing diabetes self-management programs: a nested cohort study. Health Qual Life Outcomes. 2012 May;10(1):48.
22. Setji TL, Page C, Pagidipati N, Goldstein BA. DIFFERENCES IN ACHIEVING HBA1C GOALS AMONG PATIENTS SEEN BY ENDOCRINOLOGISTS AND PRIMARY CARE PROVIDERS. Endocr Pract. 2019 May;25(5):461–9. doi: https://doi.org/10.4158/EP-2018-0405
23. Rudofsky G, Catarig AM, Favre L, Grau K, Häfliger S, Thomann R, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: results from the SURE Switzerland multicentre, prospective, observational study. Diabetes Res Clin Pract. 2021 Aug;178:108931. doi: https://doi.org/10.1016/j.diabres.2021.108931
24. Yale JF, Catarig AM, Grau K, Harris S, Klimek-Abercrombie A, Rabasa-Lhoret R, et al. Use of once-weekly semaglutide in patients with type 2 diabetes in routine clinical practice: results from the SURE Canada multicentre, prospective, observational study. Diabetes Obes Metab. 2021 Oct;23(10):2269–78. doi: https://doi.org/10.1111/dom.14468
25. Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022 Nov;45(11):2753–86. doi: https://doi.org/10.2337/dci22-0034
26. American Diabetes Association. Standards of Care in Diabetes-2023 Abridged for Primary Care Providers. Clin Diabetes. 2022;41(1):4–31.
27. Blonde L, Umpierrez GE, Reddy SS, McGill JB, Berga SL, Bush M, et al. American Association of Clinical Endocrinology Clinical Practice Guideline: Developing a Diabetes Mellitus Comprehensive Care Plan-2022 Update. Endocr Pract. 2022 Oct;28(10):923–1049. doi: https://doi.org/10.1016/j.eprac.2022.08.002
28. Sousa Santos F, Tavares Bello C, Roque C, Capitão R, Castro Fonseca R, Limbert C, et al. The Effect of Changing Regular Care Provider in Type 2 Diabetes Mellitus: A Retrospective Study. Acta Med Port. 2019 Sep;32(9):580–7. doi: https://doi.org/10.20344/amp.11304
29. Gastaldi G, Lucchini B, Thalmann S, Alder S, Laimer M, Brändle M, et al.; Working group of the SGED/SSED. Swiss recommendations of the Society for Endocrinology and Diabetes (SGED/SSED) for the treatment of type 2 diabetes mellitus (2023). Swiss Med Wkly. 2023 Apr;153(4):40060. doi: https://doi.org/10.57187/smw.2023.40060
30. ElSayed NA, Aleppo G, Bannuru RR, Beverly EA, Bruemmer D, Collins BS, et al.; American Diabetes Association Professional Practice Committee. Introduction and Methodology: Standards of Care in Diabetes-2024. Diabetes Care. 2024 Jan;47 Supplement_1:S1–4. doi: https://doi.org/10.2337/dc24-SINT
31. Schimke KE, Renström F, Meier S, Stettler C, Brändle M; SwissDiab Study Group. Compliance with guidelines for disease management in diabetes: results from the SwissDiab Registry. BMJ Open Diabetes Res Care. 2018 Feb;6(1):e000454. doi: https://doi.org/10.1136/bmjdrc-2017-000454
32. Corcillo A, Pivin E, Lalubin F, Pitteloud N, Burnier M, Zanchi A. Glycaemic, blood pressure and lipid goal attainment and chronic kidney disease stage of type 2 diabetic patients treated in primary care practices. Swiss Med Wkly. 2017 Jul;147(2728):w14459.
33. Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J Hepatol. 2018 Feb;68(2):305–15. doi: https://doi.org/10.1016/j.jhep.2017.11.013
34. Maitra NS, Mahtta D, Navaneethan S, Vaughan EM, Kochar A, Gulati M, et al. A Mistake Not to Be Repeated: What Can We Learn from the Underutilization of Statin Therapy for Efficient Dissemination of Cardioprotective Glucose Lowering Agents? Curr Cardiol Rep. 2022 Jun;24(6):689–98. doi: https://doi.org/10.1007/s11886-022-01694-5
35. Fernando K, Bain SC, Holmes P, Jones PN, Patel DC. Glucagon-Like Peptide 1 Receptor Agonist Usage in Type 2 Diabetes in Primary Care for the UK and Beyond: A Narrative Review. Diabetes Ther. 2021 Sep;12(9):2267–88. doi: https://doi.org/10.1007/s13300-021-01116-9
36. Hao R, Myroniuk T, McGuckin T, Manca D, Campbell-Scherer D, Lau D, et al. Underuse of cardiorenal protective agents in high-risk diabetes patients in primary care: a cross-sectional study. BMC Prim Care. 2022 May;23(1):124. doi: https://doi.org/10.1186/s12875-022-01731-w
37. Marasinghe DH, Butalia S, Garies S, Drummond N, Kim JW, Senior PA. Low Use of Guideline-recommended Cardiorenal Protective Antihyperglycemic Agents in Primary Care: A Cross-sectional Study of Adults With Type 2 Diabetes. Can J Diabetes. 2022 Jul;46(5):487–94. doi: https://doi.org/10.1016/j.jcjd.2022.02.002
38. Antonelli D, Rabkin Y, Turgeman Y, Jabaren M. Type 2 Diabetes Mellitus: GLP1 Receptor Agonists and SGLT2 Inhibitors in Patients Referred to Ambulatory Consultant Cardiology Clinics. Isr Med Assoc J. 2023 Feb;25(2):143–6.
39. Mingrone G, Castagneto-Gissey L, Bornstein SR. New Horizons: Emerging Antidiabetic Medications. J Clin Endocrinol Metab. 2022 Nov;107(12):e4333–40. doi: https://doi.org/10.1210/clinem/dgac499
40. Qiao Q, Grandy S, Hiller J, Kostev K. Clinical and Patient-Related Variables Associated with Initiating GLP-1 Receptor Agonist Therapy in Type 2 Diabetes Patients in Primary Care in Germany. PLoS One. 2016 Mar;11(3):e0152281. doi: https://doi.org/10.1371/journal.pone.0152281
41. Perera P, O’Donnabhain R, Fazio T, Johnson D, Lange P. ‘A Missed Therapeutic Opportunity? SGLT-2 Inhibitor Use in General Medicine Patients With Heart Failure: A Retrospective Audit of Admissions to a Tertiary Health Service’. Clin Med Insights Cardiol. 2022 Oct;16:11795468221133607.
42. Chawla K, Furlong R, Kamo N, Gerbino I, Smith D, Blackmore C. Clinical spotlight intervention to accelerate translation of evidence-based practices in primary care. BMJ Open Qual. 2022 Dec;11(4):e002032. doi: https://doi.org/10.1136/bmjoq-2022-002032
43. Blanchard M. Closing the gap between medical knowledge and patient outcomes through new training infrastructure. Trans Am Clin Climatol Assoc. 2023;133:119–35.
44. Winpenny EM, Miani C, Pitchforth E, King S, Roland M. Improving the effectiveness and efficiency of outpatient services: a scoping review of interventions at the primary-secondary care interface. J Health Serv Res Policy. 2017 Jan;22(1):53–64. doi: https://doi.org/10.1177/1355819616648982