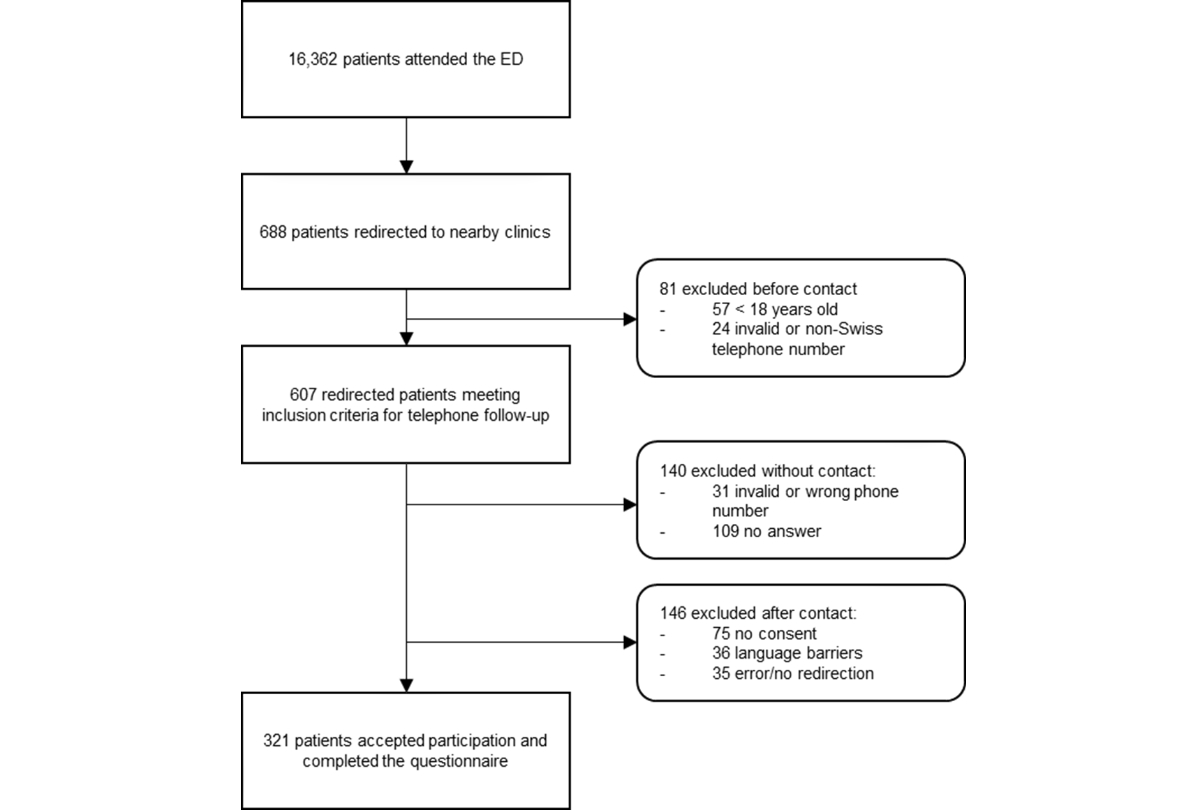
Figure 1Flow diagram of study patients.
DOI: https://doi.org/https://doi.org/10.57187/s.4030
Emergency department overcrowding compromises the quality and safety of care [1] and increases patient morbidity and mortality rates [2]. Furthermore, it negatively affects patient experiences [3] and contributes to health staff stress [1]. Numerous factors have been identified as contributing to overcrowding, such as insufficient staffing, a shortage of hospital beds, and non-urgent visits [4]. Several solutions have been suggested; these can be classified into three levels: input (on which this study is focused), throughput, and output.
The first level (input) includes all public health solutions that aim to decrease the number of non-urgent consultations in emergency departments. In Europe, various strategies have emerged to limit emergency service use. For example, Denmark has proposed a system in which general practitioners act as gatekeepers; patients only have access to emergency care after a general practitioner consultation (except for life-threatening emergencies) [5]. In France, emergency departments can be accessed by self-referral [4]. However, to limit overcrowding, most European countries are attempting to segment emergency department patient flow according to severity level by creating fast-track processes or structures adjacent to emergency departments to treat patients with non-life-threatening conditions and those not requiring complex hospital technical facilities. In Switzerland, in the absence of a unique health number to facilitate telephone medical advice and prevent excess emergency service use, redirecting low-severity patients to other partners is a potential complementary solution.
In 2022, a redirection process was implemented in our emergency department to limit overcrowding, based on the revised Swiss Emergency Triage Scale (SETS) [6] and triage nurse expertise. Identifying patients to redirect is the most crucial part of this process. Various methods have been described in the literature, such as medical triage by a senior doctor [4, 7], an electronic triage system [8], or a process based on a triage scale [9]. Safety in care is a key concept when introducing a new measure. It is generally defined as the prevention of adverse events or the reduction of morbidity and mortality. In the emergency department, in addition to the occurrence of adverse events, an unscheduled return within days of the first consultation is considered a crucial indicator of the quality of care provided [10]. Unscheduled returns may indicate diagnostic errors, poorly communicated discharge instructions, or inadequate pain management or disease progression handling. Therefore, this study assessed the safety of a newly implemented redirection process by examining the rate of unexpected returns to any healthcare facility (public or private healthcare establishment) within 2 and 7 days after redirection. This was based on a previous study [8].
This monocentric cohort study was performed at the adult emergency department of the Fribourg Cantonal Hospital in Western Switzerland, which receives 41,000 visits annually. The emergency department does not have a nearby partner general practice office. All adult patients who presented to the emergency department between 1 January and 31 May 2023 and accepted redirection were eligible for inclusion. They were identified using MedFolio, an electronic patient record system. The exclusion criteria were intrahospital redirection (gynaecology, ophthalmology, ear-nose-throat, and psychiatry), external redirection to dental clinics, and an invalid or non-Swiss telephone number. All patients who met the inclusion and exclusion criteria were selected for a telephone interview following redirection.
This redirection process occurs after triage and has been in place since July 2022. Triage nurses who carry out the triage process are qualified emergency care experts who have completed a diploma obtained after 2 years of further training, in addition to the 3-year basic diploma [11]. Patients are triaged according to the revised Swiss Emergency Triage Scale [6], which comprises four levels of emergency care categorised according to the main presenting complaint, vital signs, and medical history. The most critical cases that should be assessed immediately are categorised as level 1, whereas non-urgent conditions are grouped under level 4. Emergency grades are assigned according to the presenting complaint (e.g.,cardiac arrest = 1; shortness of breath = 1/2/3; confusion = 1/2; abdominal pain = 2/3; dysuria = 3/4). Nurses assign an emergency level based on vital signs, with a choice of two or more levels. Only grades 3 and 4 can be redirected if the nurse deems it possible. Patients selected for redirection are then asked to consult their general practitioner or nearby partner clinic within 24 hours without an appointment. However, patients can decline the offer and continue to receive medical care in the emergency department.
The partner clinics included three clinics in the same group as the hospital (located 13, 18, and 25 kilometres away by car) and a private clinic (3 kilometres away). In general, no additional follow-up was arranged. At the nurse’s request, a senior physician was available to assist with the triage process. Information about a senior doctor’s involvement in the process and transfer hospital (gynaecology, ophthalmology, ear-nose-throat, or psychiatry) was gathered in this step and included in MedFolio.
Demographic and triage characteristics and the presenting complaints of the included patients were collected from the emergency department electronic medical records. Telephone interviews were conducted within 6 months after emergency department consultation to collect outcome data. Patients who answered telephone calls were first informed about the study and asked for oral consent. Those who had a poor understanding of French, German, or English; could not give verbal consent or refused to participate; had no memory of redirection; or did not respond after three telephone call attempts on different days and at different times were excluded from the study. The questionnaire (see appendix) gathered information about the place and date of consultations within a week and hospitalisation for the same complaint within a week. To assess patient satisfaction, a 5-point Likert scale was used (1 = very dissatisfied; 2 = dissatisfied; 3 = neutral; 4 = satisfied; 5 = very satisfied) for three items (triage experience, care received at partner clinics, and the general redirection process). Patients were asked to rate each item separately.
The primary outcome was the rate of redirected patients seeking care at any healthcare facility for the same chief complaint in an unexpected visit within 2 days of the initial emergency department redirection. The secondary outcomes were the rate of unexpected returns to any healthcare facility within 7 days, the rate of hospitalisation within 7 days, and the patient satisfaction rate with the redirection process. All outcomes were also analysed by subgroup to facilitate comparison with other studies. Subgroups were separated into patients returning to any healthcare facility (hospitals, private clinics, and general practitioners) and patients returning specifically to hospitals.
Numeric data are presented as means (SD) or medians (range), depending on the data distribution. To assess patient satisfaction, questionnaires were analysed using descriptive statistics. For each item, the result was presented as the mean on a rating scale where 1 corresponded to “very dissatisfied” and 5 corresponded to “very satisfied”, as well as the proportion of satisfied patients (those who answered “satisfied” or “very satisfied”). All descriptive analyses were performed using IBM SPSS® Statistics V2 and Microsoft Excel.
This study project was approved by the cantonal ethics committee (CER-VD) as a quality assurance project, thus exempting it from the requirement to submit a full-length form for ethical approval. Additionally, the protocol was approved by Fribourg Hospital via the hospital’s internal quality department. The project was conducted in accordance with the Helsinki Declaration. Data were retrieved manually from electronic medical records and medical archives. Access to the data and material can be provided upon request to the corresponding author.
The patients’ baseline characteristics are summarised in table 1. Among 16,362 patients aged 16 years or over who presented to the emergency department, 688 (4%) were redirected to partner clinics for medical consultation. Of these, 81 were excluded before the follow-up telephone call (patients under 18 years and those with invalid/non-Swiss telephone numbers), and 607 were included for telephone calls. A further 286 were excluded after the telephone calls (no answer, no consent, or wrong/invalid telephone number), and a total of 321 patients were included in the final analysis (figure 1). Of these, 164 (51%) patients were female (median age 36 years [18–85]), and 304 (95%) lived in the same region (Canton of Fribourg). Forty-six patients (14%) reported having no specific general practitioner (table 1).
Table 1Baseline patient characteristics.
| Patients | Overall (n = 321) | |
| Age (years) | Mean (SD) | 39 (14) |
| Median (min, max) | 36 (18, 85) | |
| Gender | Female, n (%) | 164 (51%) |
| Male, n (%) | 157 (49%) | |
| Primary care physician | Yes, n (%) | 268 (84%) |
| No, n (%) | 46 (14%) | |
| Unsure, n (%) | 7 (2%) | |
| Canton of domicile | Fribourg, n (%) | 304 (95%) |
| Vaud, n (%) | 8 (2.5%) | |
| Jura, n (%) | 2 (0.5%) | |
| Valais, n (%) | 2 (0.5%) | |
| Other canton, n (%) | 5 (1.5%) | |
| Triage and redirection | ||
| Swiss Emergency Triage Scale level | U1, n (%) | 0 |
| U2, n (%) | 0 | |
| U3, n (%) | 168 (52) | |
| U4, n (%) | 153 (48) | |
| Medical triage | Yes, n (%) | 33 (10) |
| No, n (%) | 288 (90) | |
| Transfer | Personal, n (%) | 256/290 (88) |
| Public transport, n (%) | 32/290 (11) | |
| Taxi, n (%) | 2/290 (0.5) | |
SD: standard deviation; U1: most acute level of emergency; U4: least acute level of emergency.
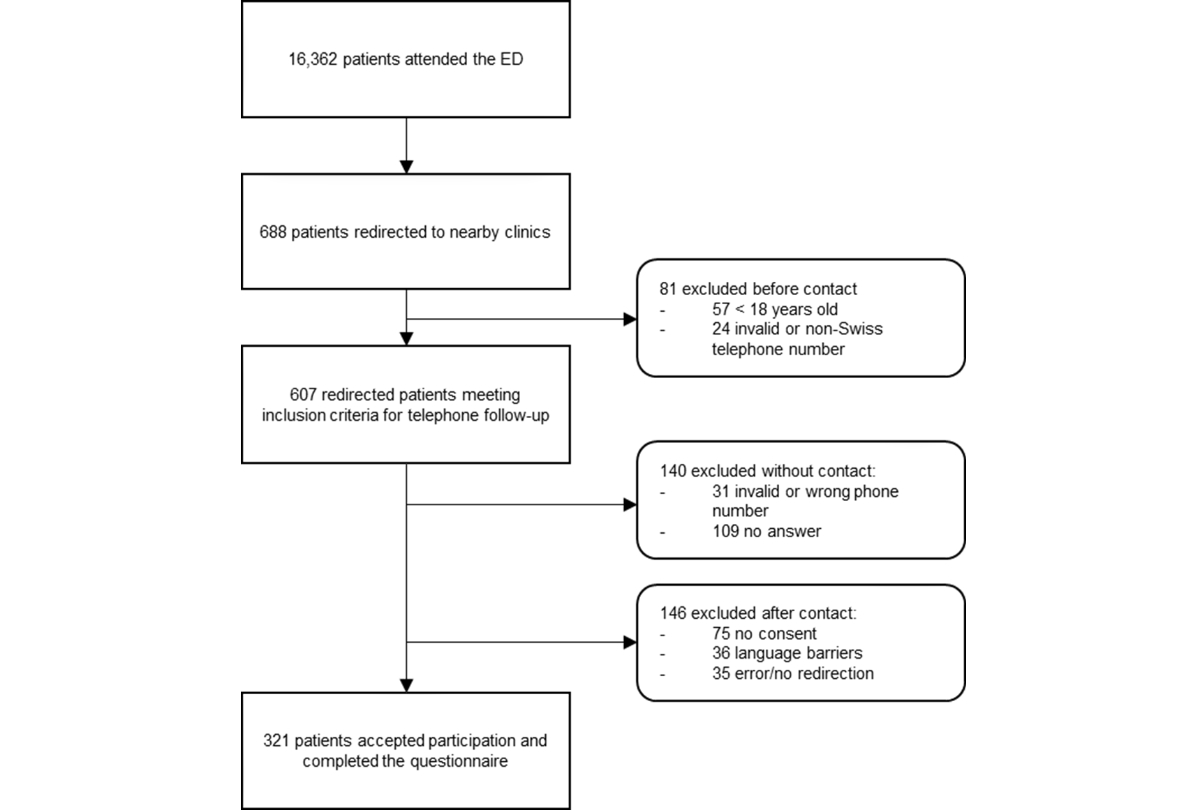
Figure 1Flow diagram of study patients.
The main presenting complaints are summarised in table 2. The most frequently reported complaints were influenza-like illnesses (23%) and neck, back, and lumbar pain (13%). The triage level and redirection characteristics are summarised in table 1.
Table 2Major presenting complaints of redirected patients.
| Major presenting complaint* | Number of patients |
| Influenza-like illness, n (%) | 75 (23.4) |
| Neck, back, and lumbar pain, n (%) | 42 (13.1) |
| Ear-nose-throat disease, n (%) | 40 (12.5) |
| Arthralgia, myalgia, neuralgia, lameness, n (%) | 36 (11.2) |
| Skin, soft tissue disorder/infection, n (%) | 18 (5.6) |
| Limb trauma, n (%) | 18 (5.6) |
| Limb pain and/or swelling, n (%) | 9 (2.8) |
| Abdominal pain, n (%) | 8 (2.5) |
| Cough, sputum, n (%) | 8 (2.5) |
| Dysuria, pollakiuria, n (%) | 5 (1.6) |
| Dyspnea, tachypnea, bradypnea, n (%) | 5 (1.6) |
| Allergic reactions, n (%) | 4 (1.2) |
| Fever, n (%) | 4 (1.2) |
| Nausea, vomiting, n (%) | 4 (1.2) |
| Other, n (%) | 41 (12.7) |
| No data available, n (%) | 4 (1.3) |
* Major complaints representing less than 1% of consultations have been grouped into the “other” category.
Following redirection, 290 (90%) patients consulted one of the partner clinics or their general practitioner after redirection on the same day. 31 patients (10%) did not follow the recommendation to consult within 24 hours. Of these, 45% (14) patients consulted unexpectedly during the following week. The main reasons given for not attending the consultation following redirection were improved symptomatology, accessibility problems, and anticipated waiting times at clinics.
The rate of unexpected returns to any healthcare facility for the same chief complaint was 4% within 2 days (14 patients). Of these, one patient (7.1%) returned to our emergency department, four (28.6%) consulted a partner hospital, and nine (64.3%) consulted their general practitioner. Within 7 days, the rate of unexpected returns increased to 16% (52 patients); four patients (1.2%) revisited our emergency department, eleven (21%) consulted a partner hospital, and thirty-seven (71%) consulted their general practitioner (table 3).
Table 3Unexpected returns within 2 and 7 days after redirection.
| Patients n (%) | ||
| Within 2 days | ||
| For all redirected patients (n = 321) | Unexpected returns to the same hospital | 1 (0.3) |
| Unexpected returns to any hospital | 4 (1.2) | |
| Unexpected returns to any healthcare facility | 14 (4.4) | |
| For patients who did consult after redirection (n = 290) | Unexpected returns to the same hospital | 1 (0.3) |
| Unexpected returns to any hospital | 3 (1) | |
| Unexpected returns to any healthcare facility | 6 (2.1) | |
| For patients who did not consult after redirection (n = 31) | Unexpected returns to the same hospital | 0 (0) |
| Unexpected returns to any hospital | 1 (3.2) | |
| Unexpected returns to any healthcare facility | 8 (25.8) | |
| Within 7 days | ||
| For all redirected patients (n = 321) | Unexpected returns to the same hospital | 4(1.2) |
| Unexpected returns to any hospital | 15(4.7) | |
| Unexpected returns to any healthcare facility | 52 (16.2) | |
| For patients who did consult after redirection (n = 290) | Unexpected returns to the same hospital | 3(1) |
| Unexpected returns to any hospital | 13(4.5) | |
| Unexpected returns to any healthcare facility | 38(13.1) | |
| For patients who did not consult after redirection (n = 31) | Unexpected returns to the same hospital | 1(3.2) |
| Unexpected returns to any hospital | 2(6.5) | |
| Unexpected returns to any healthcare facility | 14(45.2) | |
Hospital: clinic with a walk-in department for emergencies; Healthcare facility: any public or private healthcare establishment.
If we excluded patients who returned unexpectedly to their general practitioner after the initial consultation, the rate of return was 1.2% (4/321) within 2 days and 4.7% (15/321) within 7 days.
The rate of unexpected consultations at any healthcare facility within 2 and 7 days among patients who consulted a doctor after redirection within 24 hours was 2% (6/290) and 13% (38/290), respectively.
Six patients needed hospitalisation within 1 week following redirection (2%). No fatalities were reported in our hospital’s medical records. The reasons for hospital admission were ear-nose-throat infections (n = 1), pancolitis (n = 1), choledocholithiasis (n = 2), urolithiasis (n = 1) and neurological surveillance after head trauma (n = 1). Patients’ follow-up within 1 week of redirection is illustrated in figure 2.
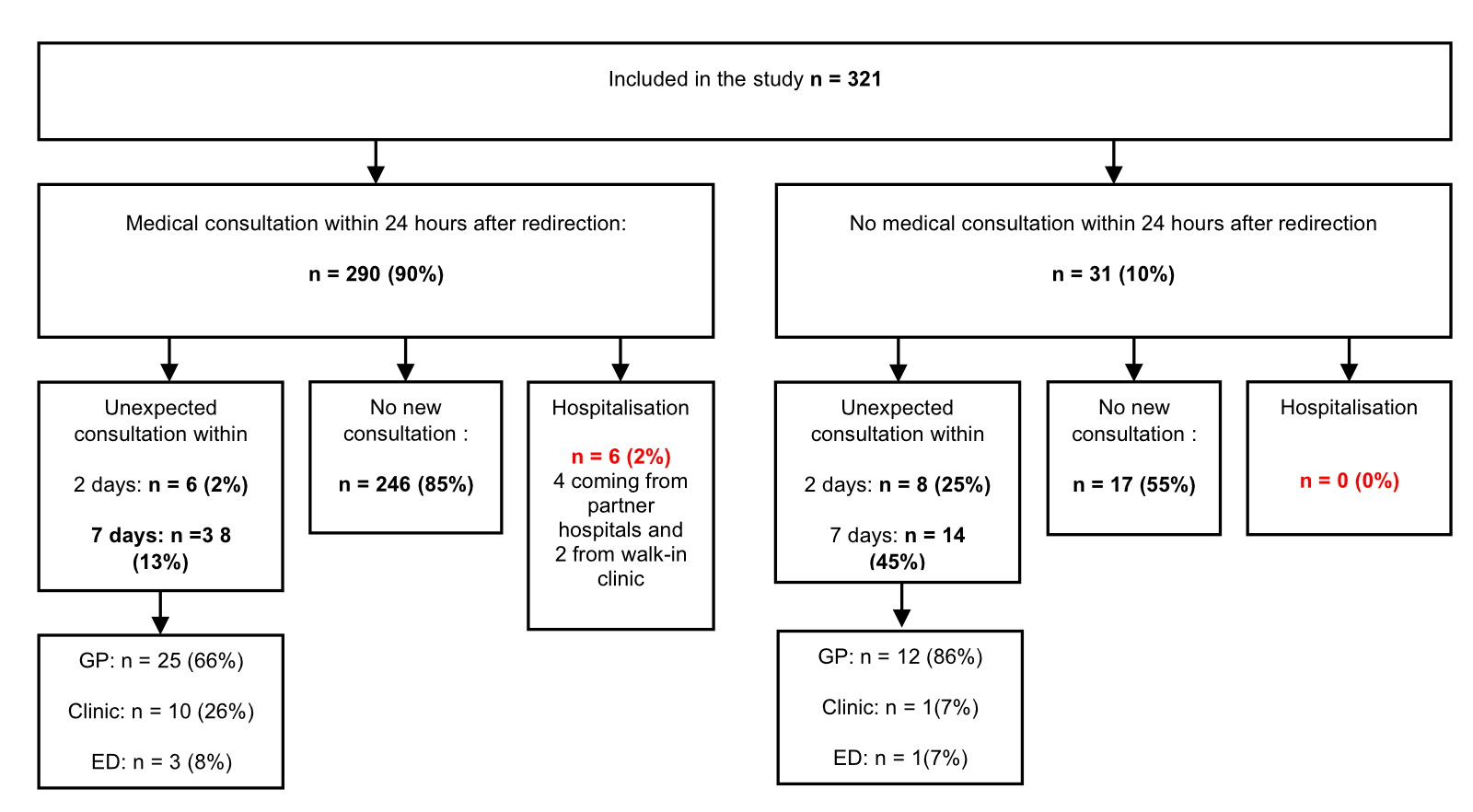
Figure 2Patient follow-up. GP: general practitioner; clinic: partner clinics; ED: emergency department.
Overall, the satisfaction rate with the triage experience was 66% (“very satisfied” or “satisfied”), with a mean score of 3.9 (SD = 1.1). For patients who did consult after redirection, 85% were ”satisfied” or “very satisfied” with the care they received, with a mean score of 4.4 (SD = 1). General satisfaction with the redirection process was 58%, with a mean score of 3.7 (SD = 1) in the entire cohort. The patient satisfaction data are detailed in figure 3.
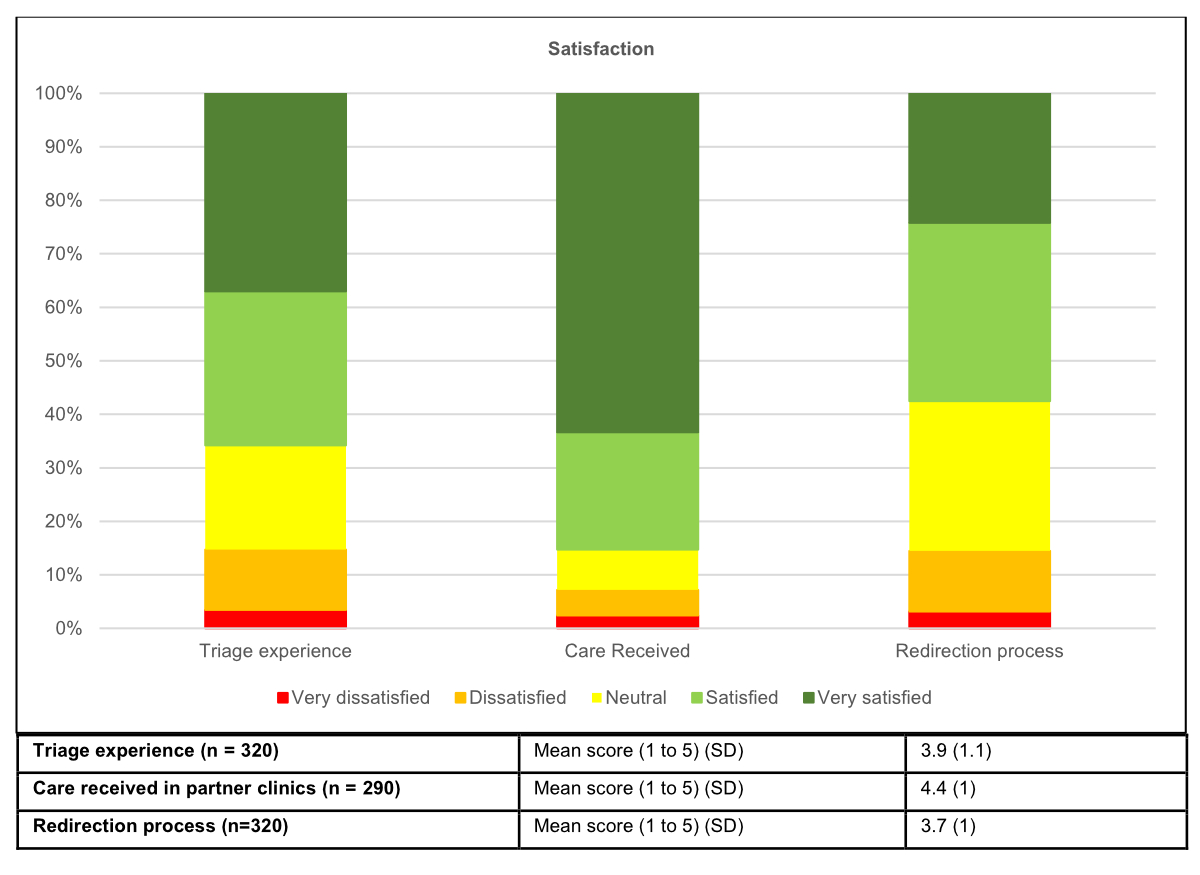
Figure 3Patient satisfaction. Triage experience (n = 320): mean score (1 to 5) (standard deviation [SD]): 3.9 (1.1); care received in partner clinics (n = 290): mean score (1 to 5) (SD): 4.4 (1); redirections process (n = 320): mean score (1 to 5) (SD): 3.7 (1).
This monocentric cohort study assessed the safety of a redirection process in which triage nurses redirected low-acuity patients after emergency triage by investigating the rate of unexpected returns to any healthcare facility within 2 days; the findings showed that this rate was low (4%), and the rate of unexpected returns to any hospital was even lower (1.2%). Previous studies analysing unexpected returns after redirection have shown similar rates of re-consultation at 2 days (2.8%) after triage using an electronic application [8] and 3 days after triage by a senior doctor (4.1%) [4]. This low 2-day return rate demonstrates the safety of this redirection process, which is based on the expertise of nurses after emergency department triage. Consequently, the study demonstrated that the redirection process can be safely managed by an experienced nurse.
Within 7 days, the overall unexpected return rate to any healthcare facility was 16% (n = 52), and the return rate to any hospital was 4.7% (n = 15). Most of these patients (71%) sought care from their general practitioner rather than returning to the emergency department. Furthermore, 31 patients (10%) did not follow the recommendation to consult a partner clinic or a general practitioner during the same day. Nearly half of them consulted during the following week. When we excluded these patients, the unexpected return rate to any healthcare facility within 7 days fell to 13%. A previous monocentric prospective cohort study reported a rate of unexpected returns of 4.8% to any hospital within 7 days (31 patients out of 642) of redirection using an electronic application for triage [8]. These results align with our study, where the rate of unexpected returns to any hospital was 4.7%. Another study found that 6% of redirected patients were admitted within 7 days of redirection [7], whereas others reported an unexpected return rate of 2% at 8 days [10] and 9.4% at 14 days [12] following initial emergency consultation. The re-consultation rate at 1 week seems to be a less powerful marker for assessing the safety of redirection process for patients presenting to emergency departments as returns may be linked to the progress of an acute illness or failure to comply with treatment [13, 14]. Comparison with the existing literature must be approached with caution, as studies vary in their definitions of the return rate. Some authors include only patients returning to emergency departments, whereas others include returns to any healthcare facility, including visits to general practitioners. Furthermore, redirection strategies and inclusion criteria vary across studies [15, 16].
The assessment of the safety of redirection must also account for the rate of fatality and hospitalisation following redirection. In this study, no fatalities were reported, and the hospitalisation rate following redirection was low (2%). This is at the low end of the existing literature, which reports hospitalisation rates ranging from 0 to 6% after redirection [4, 8, 17–20].
The proportion of patients redirected from the emergency department varies from 2 to 20%, depending on the methods used [4, 14, 15]. Using our process, it reached 4%. This low rate can be explained by several factors. Patients were mainly redirected during the day, depending on the opening hours of the partner centres, effectively excluding patients who consulted at night. Our study did not consider low-severity patients with gynaecological, dental, or ocular problems (internal redirection to specialist consultation); those uncomplicated urinary tract infections (medical treatment protocol delegated to nurses); or paediatric patients, who often visit emergency departments for low-severity issues. Finally, a physician was involved in 10% of redirection decisions. The tendency to over-triage seems more pronounced when triage is performed by a triage nurse [21], which could further explain our low redirection rate.
Several factors influence patient satisfaction in emergency departments, such as the quality of information received, waiting times, and staff empathy. We assessed patient satisfaction with three aspects (the triage experience, care received at partner clinics, and the general redirection process). Most patients were satisfied (“very satisfied” and “satisfied”) with the care they received at clinics. This encourages patients to be redirected to other healthcare facilities, even if they are far away. On the other hand, patients were less satisfied with the triage process. Dissatisfied patients cited the long waiting times before redirection and a lack of communication. This corresponds to the determinants found in the literature [22]. Satisfaction with the overall process was even lower, mainly because of waiting times at partner healthcare facilities. Improvements could be made by offering appointments at partner facilities, running public information campaigns on the role of emergency departments, and raising the possibility of redirection before the triage process. However, the literature on these points is not yet sufficient to allow comparisons.
This study has several limitations. First, the study lacks a control group, which would have enabled the verification of the link between redirection before medical consultation and the unexpected visit. Furthermore, only 53% of the approached patients were included in the final analysis; the remaining 47% who were not included potentially represent those with the worst outcomes or low satisfaction. The study period was 5 months and may not be representative of all patients who were seen in the emergency department. Second, this study is subject to selection bias, as the triage nurse alone decided after triage whether the patient could be redirected and may have refrained from redirecting because of excessive caution. Thus, some patients may have been admitted to the emergency department when they could have been redirected (overtriage). However, this study was not designed to measure this aspect. In addition, the number of patients who refused redirection was not assessed. Third, because this was an observational study, it was not designed to measure the impact of redirection on overcrowding, the average length of stay, or patient flows in the emergency department. Fourth, this is a single-centre study, and all nurses at this centre undergo specialised 2-year training in emergency care before performing triage. Consequently, these results cannot be directly generalised to other emergency departments in Switzerland or other countries. Finally, even if the telephone interview is standardised, it is subject to memory bias, and patients’ initial feelings may be influenced by the evolution of their pathology. Because answers had to be provided via telephone, information bias is also possible.
The rate of unexpected returns to any healthcare facility was 4% within 2 days and 16% within 7 days after redirection. The implementation of this protocol appeared to provide safe deferral to nearby clinics for redirected low-acuity patients. Patients’ satisfaction with the care they received at partner clinics was high, although it was lower for the redirection process and triage experience.
We sincerely thank Rosemary Sudan for editorial assistance.
TS, YG designed the study with the help of ALFP based on an existing protocol of ALFP. AD designed and monitored the data collection from which this paper was developed. AD, TS, CLT and YG analyzed the data. AD wrote the first draft. SR, TS, YG, CLT, ALFP and VR contributed to the writing and revision of the paper.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: A systematic review of causes, consequences and solutions. PLoS One. 2018 Aug;13(8):e0203316. doi: https://doi.org/10.1371/journal.pone.0203316
2. Badr S, Nyce A, Awan T, Cortes D, Mowdawalla C, Rachoin JS. Measures of Emergency Department Crowding, a Systematic Review. How to Make Sense of a Long List. Open Access Emerg Med. 2022 Jan;14:5–14. doi: https://doi.org/10.2147/OAEM.S338079
3. Sartini M, Carbone A, Demartini A, Giribone L, Oliva M, Spagnolo AM, et al. Overcrowding in Emergency Department: Causes, Consequences, and Solutions-A Narrative Review. Healthcare (Basel). 2022 Aug;10(9):1625. doi: https://doi.org/10.3390/healthcare10091625
4. Morin C, Choukroun J, Callahan JC. Safety and efficiency of a redirection procedure toward an out of hours general practice before admission to an emergency department, an observational study. BMC Emerg Med. 2018 Aug;18(1):26. doi: https://doi.org/10.1186/s12873-018-0173-6
5. Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012 Mar;25 Suppl 1:S34–8. doi: https://doi.org/10.3122/jabfm.2012.02.110216
6. Rutschmann OT, Hugli OW, Marti C, Grosgurin O, Geissbuhler A, Kossovsky M, et al. Reliability of the revised Swiss Emergency Triage Scale: a computer simulation study. Eur J Emerg Med. 2018 Aug;25(4):264–9. doi: https://doi.org/10.1097/MEJ.0000000000000449
7. Bentley JA, Thakore S, Morrison W, Wang W. Emergency Department redirection to primary care: a prospective evaluation of practice. Scott Med J. 2017 Feb;62(1):2–10. doi: https://doi.org/10.1177/0036933017691675
8. Feral-Pierssens AL, Morris J, Marquis M, Daoust R, Cournoyer A, Lessard J, et al. Safety assessment of a redirection program using an electronic application for low-acuity patients visiting an emergency department. BMC Emerg Med. 2022 Apr;22(1):71. doi: https://doi.org/10.1186/s12873-022-00626-4
9. Vertesi L. Does the Canadian Emergency Department Triage and Acuity Scale identify non-urgent patients who can be triaged away from the emergency department? CJEM. 2004 Sep;6(5):337–42. doi: https://doi.org/10.1017/S1481803500009611
10. Sauvin G, Freund Y, Saïdi K, Riou B, Hausfater P. Unscheduled return visits to the emergency department: consequences for triage. Acad Emerg Med. 2013 Jan;20(1):33–9. doi: https://doi.org/10.1111/acem.12052
11. Schmutz T, Ribordy V, Exadaktylos AK, Carron PN. Emergency medicine in Switzerland: a laboratory for professional experimentation. Eur J Emerg Med. 2021 Aug;28(4):264–5. doi: https://doi.org/10.1097/MEJ.0000000000000816
12. Berger D, King S, Caldwell C, Soto EF, Chambers A, Boehmer S, et al. Returns After Discharge From the Emergency Department Observation Unit: Who, What, When, and Why? West J Emerg Med. 2023 May;24(3):390–5. doi: https://doi.org/10.5811/WESTJEM.59023
13. Wu CL, Wang FT, Chiang YC, Chiu YF, Lin TG, Fu LF, et al. Unplanned emergency department revisits within 72 hours to a secondary teaching referral hospital in Taiwan. J Emerg Med. 2010 May;38(4):512–7. doi: https://doi.org/10.1016/j.jemermed.2008.03.039
14. Thijssen WA, Wijnen-van Houts M, Koetsenruijter J, Giesen P, Wensing M. The impact on emergency department utilization and patient flows after integrating with a general practitioner cooperative: an observational study. Emerg Med Int. 2013;2013:364659. doi: https://doi.org/10.1155/2013/364659
15. Gonçalves-Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev. 2018 Feb;2(2):CD002097. doi: https://doi.org/10.1002/14651858.CD002097.pub4
16. Kirkland SW, Soleimani A, Rowe BH, Newton AS. A systematic review examining the impact of redirecting low-acuity patients seeking emergency department care: is the juice worth the squeeze? Emerg Med J. 2019 Feb;36(2):97–106. doi: https://doi.org/10.1136/emermed-2017-207045
17. Dale J, Green J, Reid F, Glucksman E, Higgs R. Primary care in the accident and emergency department: II. Comparison of general practitioners and hospital doctors. BMJ. 1995 Aug;311(7002):427–30. doi: https://doi.org/10.1136/bmj.311.7002.427
18. Doran KM, Colucci AC, Hessler RA, Ngai CK, Williams ND, Wallach AB, et al. An intervention connecting low-acuity emergency department patients with primary care: effect on future primary care linkage. Ann Emerg Med. 2013 Mar;61(3):312–321.e7. doi: https://doi.org/10.1016/j.annemergmed.2012.10.021
19. Washington DL, Stevens CD, Shekelle PG, Baker DW, Fink A, Brook RH. Safely directing patients to appropriate levels of care: guideline-driven triage in the emergency service. Ann Emerg Med. 2000 Jul;36(1):15–22. doi: https://doi.org/10.1067/mem.2000.107003
20. van der Straten LM, van Stel HF, Spee FJ, Vreeburg ME, Schrijvers AJ, Sturms LM. Safety and efficiency of triaging low urgent self-referred patients to a general practitioner at an acute care post: an observational study. Emerg Med J. 2012 Nov;29(11):877–81. doi: https://doi.org/10.1136/emermed-2011-200539
21. Graversen DS, Christensen MB, Pedersen AF, Carlsen AH, Bro F, Christensen HC, et al. Safety, efficiency and health-related quality of telephone triage conducted by general practitioners, nurses, or physicians in out-of-hours primary care: a quasi-experimental study using the Assessment of Quality in Telephone Triage (AQTT) to assess audio-recorded telephone calls. BMC Fam Pract. 2020 May;21(1):84. doi: https://doi.org/10.1186/s12875-020-01122-z
22. Messina G, Vencia F, Mecheroni S, Dionisi S, Baragatti L, Nante N. Factors affecting patient satisfaction with emergency department care: an Italian rural hospital. Glob J Health Sci. 2014 Dec;7(4):30–9. doi: https://doi.org/10.5539/gjhs.v7n4p30
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.4030.