Figure 1Screening process.
DOI: https://doi.org/https://doi.org/10.57187/s.3894
Edinburgh Postpartum Depression Scale
Mother-Infant-Bonding scale
The COVID-19 pandemic spread to Switzerland in February 2020. Due to the rising number of infections, on 16 March 2020 the Federal Council declared an exceptional situation (highest level of danger) in accordance with the Epidemic Act. With the new regulation in effect, public life was markedly restricted. These drastic measures had a significant impact on the implementation of safety measures in Swiss hospitals to reduce local outbreaks and to protect patients, visitors and hospital staff. Consequently, local authorities restricted entrance exclusively to patients. Visitors were not permitted. Pregnant women were exceptionally allowed to be accompanied by their partners in the delivery ward while giving birth. The partners had to leave the hospital two to four hours after delivery. Further visits during the inpatient postpartum period were not allowed. After stabilisation of the surge in new SARS-CoV-2 infections in Switzerland, these restrictions were alleviated, allowing fathers to visit throughout their partners’ stay for two consecutive months, after which more extensive visits were allowed.
Risk factors for postnatal depression have been studied worldwide for decades and are multifactorial [1, 2]. The most important risk factors include existing or pre-existing mental illness, especially depression and anxiety disorders, lack of social support and traumatising experiences during pregnancy or in the early postpartum period [3]. These may influence mother-infant bonding as well [4].
The psychological and clinical impact of the COVID-19 restrictions on women postpartum is not yet well studied. The pandemic was associated with several risk factors for the development of postnatal depression – such as the lack of social support and a stressful life event in a physically and psychologically critical phase of a woman’s life [5, 6]. There is evidence demonstrating that women from COVID-19-affected populations showed significantly greater stress reactions at birth compared to a reference group [7]. This was associated with the occurrence of birth-related post-traumatic stress symptoms as well as challenges with bonding and breastfeeding [7]. The impact of social support in the early postpartum period and the putative consequences of prohibiting visits from the child’s father on mental health and mother-child bonding have not yet been investigated.
However, privacy in the early postpartum period may also create the opportunity for positive effects on mother-child interaction. Mothers were completely undisturbed by visitors, giving them space of room their recovery from childbirth and exclusive time for bonding and breastfeeding with the newborn. According to the feedback from nurses and physicians, many women reported that they could enjoy this undisturbed time in the puerperium without visitors.
Finally, even though women were not pressured to discharge early, hospital stay significantly decreased due to maternal fear of infection. This may have led to new mothers not being adequately observed and thus putatively placing them at risk of postpartum complications. To our knowledge, data on these questions are very limited.
The aim of our study was to analyse the impact of maternal isolation during early puerperium during the COVID-19 pandemic lockdown period on maternal depressive symptoms, and the mother-child interaction. Furthermore, we were interested to see the effects on breastfeeding, postpartum complications after discharge, and duration and satisfaction of the hospital stay.
The study was approved by the Northwest- and Central-Switzerland Ethics Committee (ID: 2020-02486) on 26 September 2020. All participants provided written informed consent.
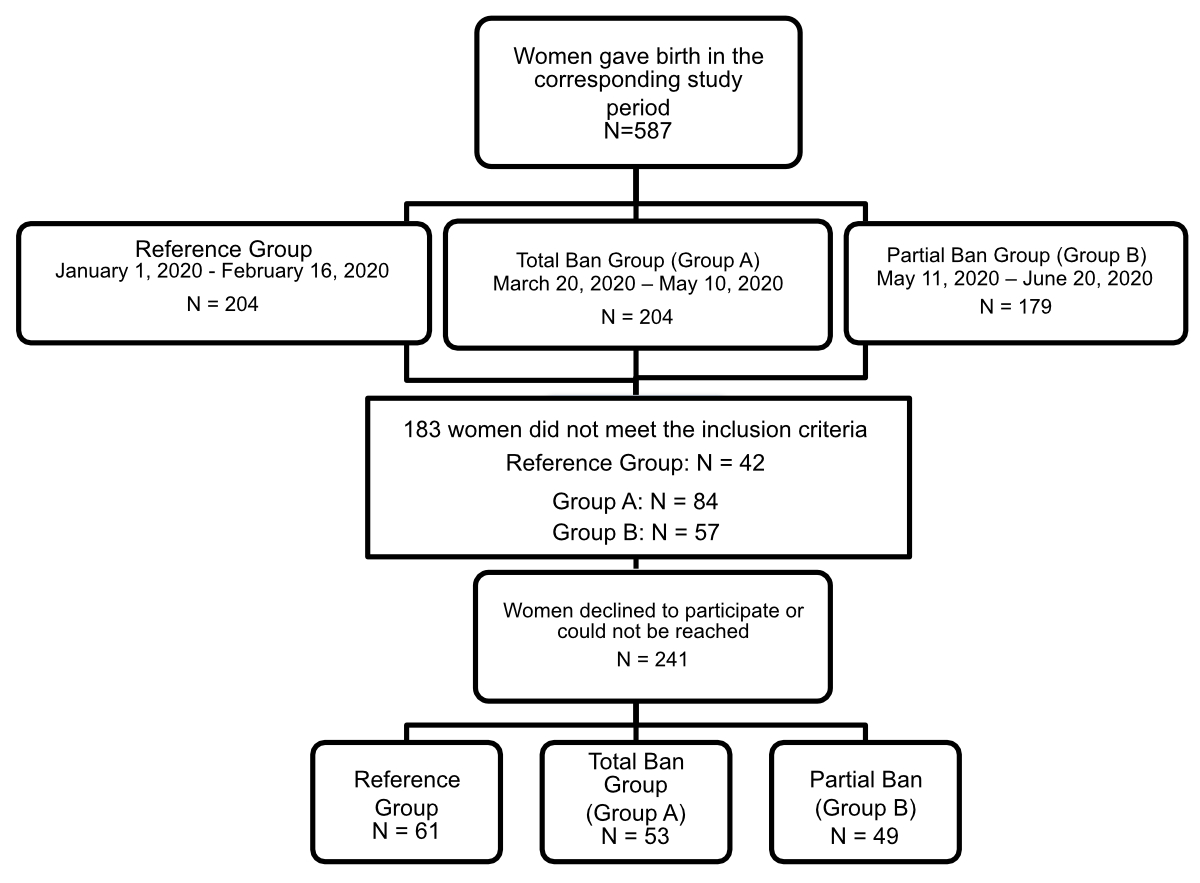
This was a single-centre observational retrospective cohort study conducted at a university-affiliated teaching hospital. A total of 587 women gave birth during the corresponding study periods (204 women each in the control group and the total ban group, and 179 women in the partial ban group). There were 183 women who did not meet the inclusion criteria; 42 of them were from the control group, 84 from the total ban group and 57 from the partial ban group. In total, 241 women declined to participate or could not be reached either in writing or by telephone.
Mothers who met any of the following criteria were excluded from the study: those with newborns requiring medical care or hospitalisation on the neonatal care unit; those with preterm infants; those aged below 18 years; those with previous mental illnesses or with physical illnesses resulting in limitations in caring for their infant independently. In addition, mothers who did not agree to participate in the trial or with language barriers were excluded.
The patients were interviewed one year after giving birth and were asked to evaluate their condition after giving birth (i.e. retrospectively) and their current wellbeing using the Edinburgh Postpartum Depression Scale (EPDS) and the Mother-Infant-Bonding Scale (MIBS).
The “total ban” group (n = 53) included women who delivered during the total ban on visitors (including the child’s father), i.e. from 20 March 2020 to 10 May 2020. The “partial ban” group (n = 49) included women who delivered during the partial ban on visitors (when only the child’s father was permitted), i.e. from 11 May 2020 to 20 June 2020. Women who delivered before the COVID-19 pandemic at the start of the same year (1 January 2020 to 16 February 2020) served as the reference group (n = 61).
The screening process is shown in figure 1.
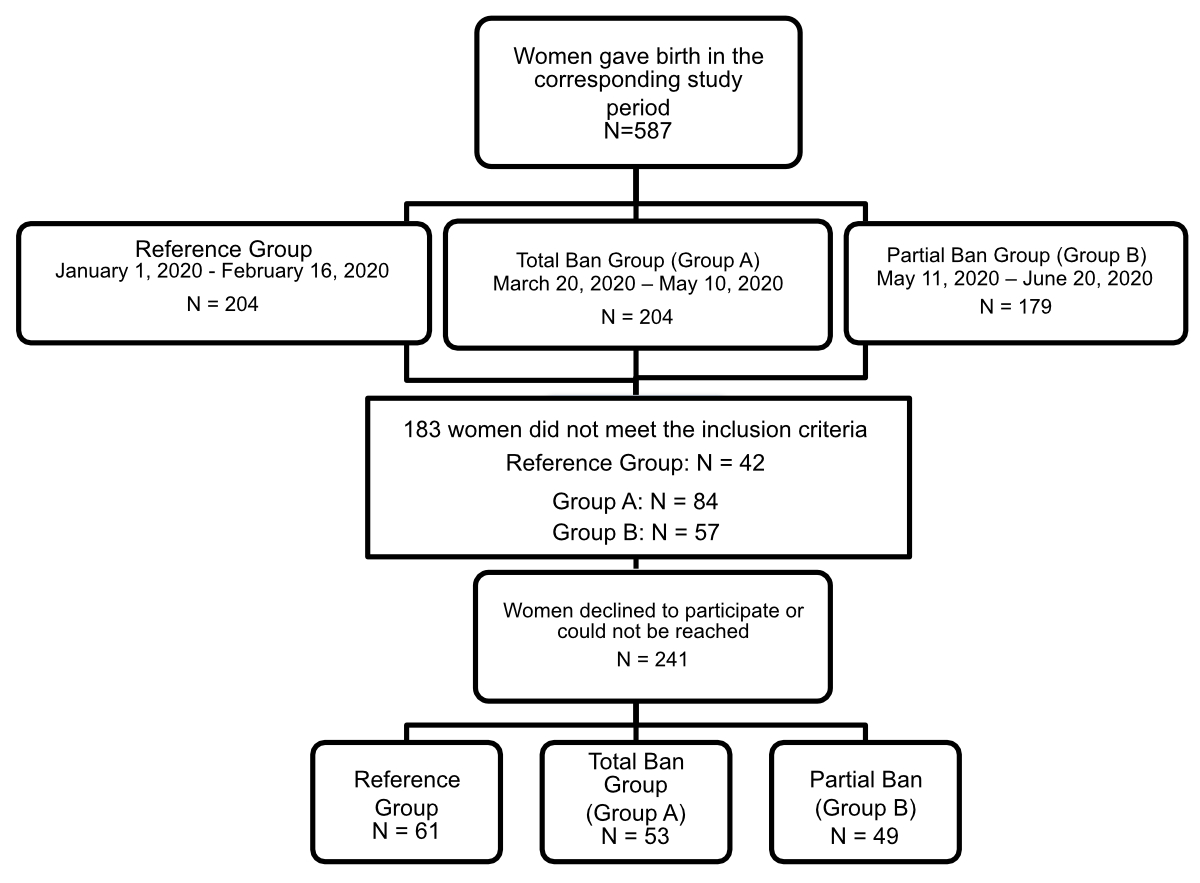
Figure 1Screening process.
Hospital records of all women who gave birth between 1 January 2020 and 20 June 2020 were screened. Women eligible for the study were invited by phone to participate in the trial. If they agreed, they received the patient study information and informed consent letter explaining the project. The study questionnaires were sent to participants after their signed informed consent had been received.
The questionnaire was composed of three blocks: general background data (education, medical history, breastfeeding duration and postpartum complications after discharge related to the breast, uterus, wound healing or others); the Edinburgh Postpartum Depression Scale (EPDS) questionnaire and the Mother-Infant-Bonding scale (MIBS) questionnaire. The reliability and validity of EPDS and MIBS have been previously reported [8, 9].
The EPDS is a 10-item questionnaire scored on a 4-point Likert scale that measures mood over the past seven days. Each item scored 0-3, the sum of all items is the score evaluated. A cut-off score ≥13 was used to identify major depressive symptoms, as suggested by Levis et al. [10]; however this does not mean that major depressive disorder could be diagnosed, as this would require a clinical diagnosis. Twelve months after they had given birth, we asked participants to evaluate their mood as it was during the first week after birth, i.e. retrospectively, and also their current mood.
The MIBS is an 8-item self-reported questionnaire, rated on a 4-point Likert scale from 0 to 3, that assesses maternal emotional involvement with the newborn. A high score indicates poorer mother-child bonding. A Japanese study has established that a score ≥2, ≥3 or ≥4 – depending on the period when it is done – is a risk factor for the development of impaired mother-child attachment [11]. The sum of all items is the score evaluated. There is no fixed cut-off and cut-off points may depend on period of evaluation; the later after birth, the lower the cut-off.
The primary outcome parameters were the influence of isolation in the early postpartum period on maternal depressive symptoms measured by the EPDS and on mother-child bonding measured by the MIBS. As secondary outcome parameters, we defined the influence of isolation due to the SARS-CoV-2 measures on breastfeeding, the length of hospital stay, patient satisfaction during the inpatient stay due to the reduced number of visitors and postpartum complications after discharge.
All data were stored in Redcap (Research Electronic Data Capture) version 9.9.1.
Sample characteristics and demographics were analysed by using descriptive statistics. Data from numerical scales, specifically the MIBS and the EPDS, were summarised using median/mean and range/standard deviation (SD). A higher score on the MIBS suggests problematic mother-to-infant bonding, while a score of 13 or higher on the EPDS was interpreted as a positive screen for major depression.
To assess central tendencies of bonding outcomes and mental health in relation to isolation, an analysis of variance (ANOVA) was conducted. For categorical variables with small cell counts, Fisher’s exact test was applied. In cases where significant deviations from the normal distribution were observed, a non-parametric rank-based approach, such as the Kruskal-Wallis test, was employed. As a follow-up step, we accounted for additional explanatory variables, including maternal age, employment, education, physical history, parity (primiparity/multiparity), delivery method, gestational age, breastfeeding status (Yes, Partial, No), breastfeeding after previous pregnancies and disturbances during the hospital stay. This was achieved using multiple linear regression.
The effects on breastfeeding were assessed using logistic regression, with partial breastfeeding and exclusive breastfeeding pooled into a single category. Dependencies between categorical or numerical and categorical covariates were analysed using contingency tables (chi-squared test) and student’s t-test. Statistical significance was defined as p <0.05.
All statistical analyses were conducted using R version 4.2.3 (R Core Team 2023) [12].
A total of 163 women were finally included in the study. For analytical purposes, participants were categorised into three groups: those who delivered under conditions of a total visitor ban, those who delivered under partial visitor restrictions (allowing the father’s presence) and those who delivered prior to the implementation of any pandemic-related measures (the reference cohort).
Baseline characteristics of the groups were similar (table 1).
Table 1Comparison of the demographic characteristics of the study participants, n= 163. Percentages rounded.
| Reference group (n = 61) | Total ban group (n = 53) | Partial ban group (n = 49) | p-value | |||
| Maternal age, in years, mean ± SD | 33.3 ± 4.6 | 33.2 ± 4.4 | 32.5 ± 4.6 | 0.558 | ||
| Gestational age of foetus at birth, in weeks, mean ± SD | 39.7 ± 1.3 | 39.5 ± 1 | 39.4 ± 1.1 | 0.585 | ||
| Parity, n (%) | 0.117 | |||||
| Primipara | 31 (51%) | 19 (36%) | 27 (55%) | |||
| Multipara | 30 (49%) | 34 (64%) | 22 (45%) | |||
| Birth mode, n (%) | – | |||||
| Spontaneous birth | 42 (69%) | 33 (62%) | 26 (53%) | |||
| Vacuum delivery | 5 (8%) | 3 (6%) | 8 (16%) | |||
| Planned Caesarean section | 8 (13%) | 13 (25%) | 11 (22%) | |||
| Unplanned Caesarean section | 6 (10%) | 48%) | 4 (8%) | |||
| Education, n (%) | 0.916 | |||||
| Low education or without a degree | 21 (34%) | 21 (40%) | 15 (31%) | |||
| High education | 39 (64%) | 31 (59%) | 33 (67%) | |||
| Others | 1 (2%) | 1 (2%) | 1 (2%) | |||
The sample primarily comprised women who delivered spontaneously (62%). The average gestational age at birth was 39.5 weeks. Almost two thirds of women (63%) had a higher education.
The mean scores from standardised measures (EPDS) are shown in table 2. There were no significant differences in mean EPDS scores between the three groups in the first seven days (p = 0.170) and after 12 months (p = 0.101).
Table 2Maternal mental health (measured by the Edinburgh Postpartum Depression Scale [EPDS]). Percentages rounded.
| Reference group (n = 61) | Total ban group (n = 53) | Partial ban group (n = 49) | p-value | ||
| EPDS ≥13, n (%) | First 7 days | 5 (9%) | 11 (23%) | 8 (20%) | 0.158 |
| After 12 months | 3 (5%) | 5 (11%) | 5 (11%) | 0.471 | |
| EPDS total, mean ± SD | First 7 days | 6.2 ± 5.4 | 7.6 ± 6.3 | 8.4 ± 5.1 | 0.170 |
| After 12 months | 4.9 ± 4.2 | 5.2 ± 4.8 | 6.7 ± 4.5 | 0.101 | |
However, when considering EPDS scores ≥13, which indicate an increased risk of postpartum depression, in both groups of isolation the rate was more than doubled at both time points (9% and 5% in the reference group vs 23% and 11% in the total ban group and 20% and 11% in the partial ban group). However, this did not reach statistical significance (p = 0.158 and p = 0.471, respectively) (figure 2).
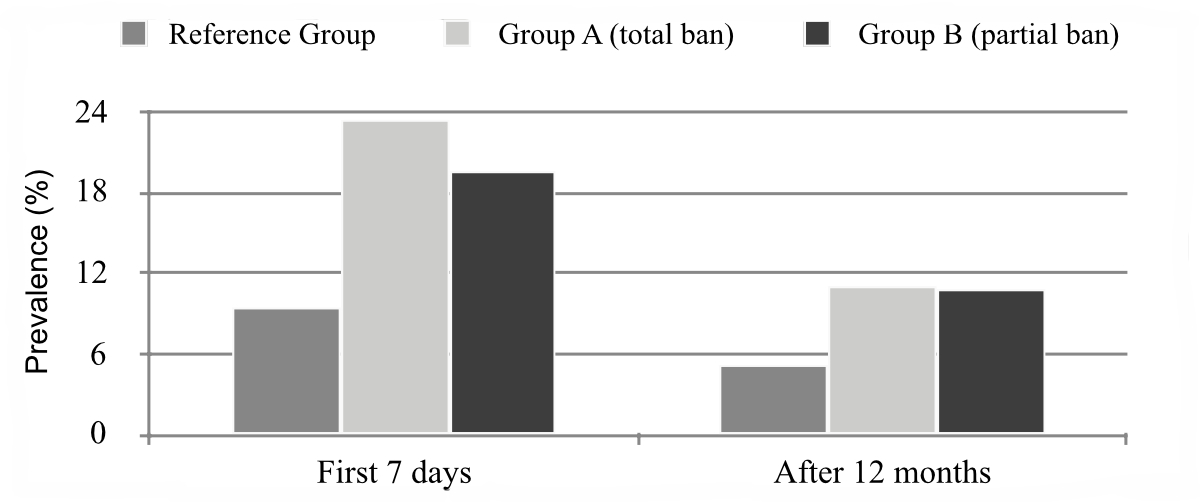
Figure 2Prevalence rates of maternal depression measured by a score ≥13 on the Edinburgh Postpartum Depression Scale (EPDS) at seven days postpartum and one year after delivery.
If we look at the correlation between EPDS and MIBS, it is positive, suggesting that mothers with higher EPDS had higher MIBS.
Analysis of the MIBS revealed very similar scores in the first week following delivery and after 12 months in all three groups (figure 3). There were no significant differences between the groups (p = 0.846 and p = 0.945) (table 3).
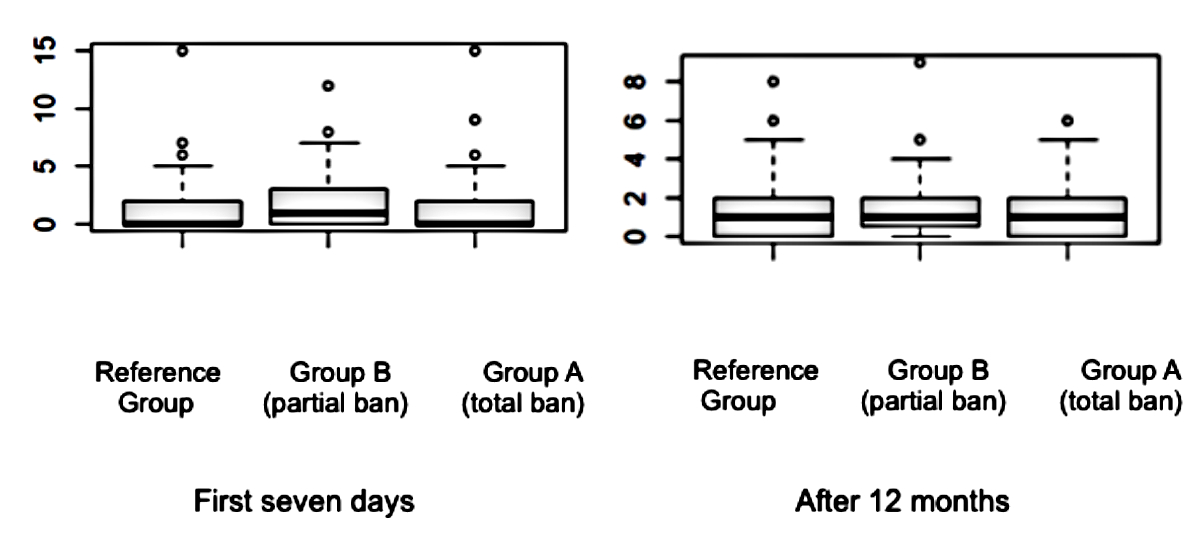
Figure 3Mother-to-Infant-Bonding scale at seven days postpartum and one year after delivery. * Explanation: The two hinges are versions of the first and third quartile. The whiskers extend to the most extreme data point which is no more than 1.5 times the interquartile range from the box. Observations outside the whisker range are plotted as points.
Table 3Mother-to-infant-bonding scale (MIBS).
| Reference group (n = 61) | Total ban group (n = 53) | Partial ban group (n = 49) | p-value | ||
| MIBS total, mean ± SD | First 7 days | 1.5 ± 2.6 | 1.5 ± 2.9 | 1.8 ± 2.6 | 0.846 |
| After 12 months | 1.3 ± 1.6 | 1.4 ± 1.6 | 1.4 ± 1.6 | 0.945 | |
Overall, 90% in the reference group breastfed (exclusively or partially) vs 92% in the total ban group and 96% in the partial ban group. There was no significant difference in breastfeeding rates between the three groups (p = 0.789).
Breastfeeding duration greater than six months was 69% in the reference group compared to 67% in the total ban group and 57% in the partial ban group, again without statistical significance (p = 0.402) (table 4).
Table 4Breastfeeding status. Percentages rounded.
| Reference group (n = 61) | Total ban group (n = 53) | Partial ban group (n = 49) | p-value | ||
| Incomplete data for breastfeeding duration, n | 7 | 7 | 3 | ||
| Breastfeeding, n (%) | 0.789 | ||||
| No | 6 (10%) | 4 (8%) | 2 (4%) | ||
| Partially | 6 (10%) | 7 (13%) | 5 (10%) | ||
| Yes | 49 (80%) | 42 (79%) | 42 (85%) | ||
| Breastfeeding duration, in months, n (%) | 0.402 | ||||
| <6 | 17 (32%) | 15 (33%) | 20 (44%) | ||
| >6 | 37 (69%) | 31 (67%) | 26 (57%) | ||
Hospital stays were clearly shorter during the partial and total visitor ban. While the reference group had a mean length of hospitalisation of 3.51 days after birth, groups with full as well as partial visiting restrictions had a significantly shorter hospitalisation (2.55 days and 3.06 days, respectively; p <0.001).
Finally, we looked at maternal satisfaction with the number and duration of visitors during the hospital stay. Interestingly, only 18% of the total ban group and 9% of the partial ban group were dissatisfied with the restriction. In contrast, 45% in the reference group would have been dissatisfied with a limitation in the number of visitors; this value was significantly different to that of the other groups (p <0.001).
However, only 24.6% in the reference group would have been dissatisfied with a shorter visiting time. There was no significant difference between the three groups (p = 0.159).
The postpartum complications after discharge are listed in table 5. Of these, problems with breastfeeding (mastitis, galactostasia, problems with the acromastium) were most frequently reported (55% of all complications in all three groups). These occurred more commonly in the total ban group (72%) than in the reference group (46%) and the partial ban group (43%), without reaching statistical significance though (p = 0.644).
Table 5Postpartum complications after discharge. Percentages rounded.
| Reference group (n = 61) | Total ban group (n = 53) | Partial ban group (n = 49) | P-value | ||
| Postpartum complications after discharge, n (%) | 0.693 | ||||
| No | 50 (82%) | 42 (79%) | 42 (86%) | ||
| Yes | 11 (18%) | 11 (21%) | 7 (14%) | ||
| Postpartum complications after discharge, n (%) | 0.644 | ||||
| Problems with the breast | 5 (46%) | 8 (73%) | 3 (43%) | ||
| Problems with the uterus | 2 (18%) | 2 (18%) | 1 (14%) | ||
| Wound healing disorder | 1 (9%) | 1 (9%) | 1 (14%) | ||
| Others | 3 (27%) | 0 (0%) | 2 (29%) | ||
Postnatal depression is the most common psychopathological illness occurring after childbirth [13]. The prevalence of postnatal depression outside of the COVID-19 pandemic is 16.4% antenatally and 13–19% postnatally [14, 15]. Studies in the context of the COVID-19 pandemic have shown wide ranges of postnatal depression prevalence, from 6.4% up to 56.9% [16].
Although the rate of women with an EPDS ≥13 during the COVID-19 pandemic almost doubled in our study, our numbers are still rather low compared to the studies mentioned above. The differences in prevalence of postnatal depression across various studies could be due to different social restrictions during the pandemic period and the sociodemographic structures of different countries in which the studies were conducted. In addition, different cut-off values (9–13) of the EPDS have been applied as well as varying methods for assessing mental wellbeing postpartum. Furthermore, different patient collectives were analysed, some including mothers with a history of depression.
The increase in EPDS score ≥13 during the first seven days after birth partly corresponds to trends in current COVID-19 studies [17]. Significantly lower scores only appear after one year. This could be a sign that individuals adapted to challenges posed by COVID-19. On the other hand, it is typical that the EPDS scores decrease over time, since the days immediately after birth represent the most psychologically vulnerable phase for women [18].
To our knowledge, this is the first study to compare the trends of EPDS scores in women during the COVID-19 pandemic immediately after birth and after one year.
It has been shown that the mere presence of a potential source of danger even without being directly affected – in this case the SARS-CoV-2 virus – can lead to an acute stress reaction in pregnant women [19]. Thus, one could interpret the doubling in EPDS score ≥13 as a result of the overall context of the COVID-19 pandemic and less provoked by visit restrictions in the early puerperium. This hypothesis is supported by the fact that numbers were quite similar for both total and partial bans, although it would be expected that the total ban without partners would be more psychologically distressing. Moreover, the pandemic may confound these results and the increase may be interpreted more in terms of the overall situation.
Nevertheless, the influence of social support should not be underestimated. It is interesting to compare this factor with other epidemics and pandemics that have taken place. For example, during the Severe Acute Respiratory Syndrome epidemic, it could be shown that the presence of social support seemed to alleviate symptoms of depression in pregnant women [20]. Overall, the data on psychological states during epidemics and pandemics for pregnant women and new mothers is limited. Studies in the general population have already shown a negative impact on psychological wellbeing [21].
Similarly, the first studies in the context of the COVID-19 pandemic also indicate a significant increase in psychological stress, anxiety and depression for pregnant women [19, 22]. These are accompanied by the fear of infection or transmission to the mother or newborn during the hospitalisation, a feeling of low social support also because of visitor restrictions during hospital stays, and COVID-19 related concerns [7, 23].
The risk of isolation during childbirth in the labour ward may be different. It had already been shown before the pandemic that support from a caregiver during birth, considered to be the most painful life event for a woman, is associated with a better emotional birth experience [24–26]. A traumatic birth experience increases the risk of developing a psychopathological disease after birth, both outside of and during the COVID-19 pandemic [27–30].
Two studies from the US have shown that SARS-CoV-2-positive women, who had visitor restrictions during childbirth, had much more pain during birth and a higher stress reaction to labour than SARS-CoV-2-positive women without isolation, which is considered a risk factor for developing a psychopathological disease after birth [29].
In the present study, a caregiver – usually the child’s father – was always present throughout the birth. This could explain the overall low rate of postnatal depression in our participants and indicates that the presence of a partner during delivery is likely much more relevant than during the first days postpartum.
Our study shows a correlation between increased Edinburgh Postpartum Depression Scale (EPDS) scores and higher Mother-Infant-Bonding Scale (MIBS) scores, but MIBS values remain low. Data on MIBS vary widely around the world. A Canadian study showed increased EPDS scores in women due to the COVID-19 epidemic, but a stable low MIBS [31]. In their study, postnatal depression and mother-infant relationships of two groups of mothers seeking treatment for psychological conditions were compared, one prior and one during the COVID-19 pandemic. Women enrolled during the COVID-19 pandemic were significantly more likely to develop depressive symptoms, without showing any effects on the mother-child bonding [31]. However, data on this topic are inconclusive. Studies from Europe and Asia have shown that the COVID-19 pandemic can lead to deterioration in maternal bonding [32, 33]. In contrast, a study from the US showed that mother-child bonding improved in mothers who were highly concerned about health impacts due to the COVID-19 pandemic, while depressive states worsened bonding [34]. In all of these studies, the exact extent of related restrictions is not described, and social settings and expectations during childbirth may have been quite different, making them difficult to compare.
Risks and resilience factors affecting mother-child bonding have been studied both before and during the pandemic, with existing depression playing a particularly important role [35, 36]. Since only women without pre-existing mental illness were included in our study, this could explain the consistently low MIBS scores in all groups.
Contrary to expectations, our study showed a breastfeeding rate of over 90% in all groups. Traumatic stress as a risk factor for maternal foetal attachment and breastfeeding problems had already been documented prior to the COVID-19 pandemic [37]. Furthermore, Mayopoulos et al. found that mothers in SARS-CoV-2-exposed communities experienced heightened acute stress responses during childbirth, which were associated with difficulties related to bonding and breastfeeding in the early postpartum phase [7]. In our study, the partner’s ability to always be present at birth – the event with the greatest stress factor – might be considered protective. On the other hand, more secluded phases postpartum did not seem to increase the already high breastfeeding rates in our study group. Likewise, Sakalidis et al. showed no negative impact on breastfeeding rates due to the lockdown with an exclusive breastfeeding rate of 82% and a partial breastfeeding rate of 18% [38]. This outcome was attributed to reduced pressure, enhanced bonding with the infant and increased time spent with family [38].
The hospital stays were significantly shorter during the partial and total visitor ban.
Interestingly, our study showed a significant difference between the study groups in the desire to reduce the number of visitors after childbirth. Likewise, two studies from Australia and New Zealand were able to show that in addition to the well-known negative effects of the pandemic after childbirth, women also experienced positive effects on motherhood, in particular less pressure, more time with their newborn, more rest and more time to breastfeed and for bonding with their newborn [38, 39].
Because of shortened hospital stay, we looked at postpartum complications after discharge. Overall, rates of complications were not significantly different except for an increased rate of postpartum problems related to the breasts in the total ban group (73% vs 46% in the reference group and 43% in the partial ban group). However, this was not statistically significant (p = 0.644). Several reviews before the COVID-19 pandemic had already shown that no statistical difference was found for relevant maternal and neonatal complications or readmission rates due to early discharge [40].
To our knowledge, this is the first study analysing hospital restrictions in a maternity unit in Switzerland. Limitations of the study include the retrospective design due to the rapid and unforeseeable changes in regulations, and the relatively small number of participants for statistical analysis that carries the risk of random error. Since the EPDS and MIBS scores for the first seven days after birth were collected retrospectively one year later, there is a risk of potential inaccuracy in the participants’ recollection. Overall, the small number of women in the sample with signs of depression and disturbed mother-child bonding makes it difficult to perform a meaningful statistical analysis so the findings should be interpreted with caution.
Likewise, the prevalence of postnatal depression in our study is rather low compared to other studies mentioned above. The difference in the prevalence of postnatal depression in some studies could be due to the choice of different cut-off points between 9 and 13 to assess for postnatal depression when the EPDS was used. This makes comparisons across different studies difficult. However, in a post-hoc analysis, even when using a cut-off value of 11, our results did not change (data not shown).
In addition, the occurrence of postpartum depression and a disturbed mother-child attachment is multifactorial and certainly cannot be explained solely by isolation. Indeed, it is not possible to differentiate the COVID-19-associated psychological effects on the women, namely health-related fears about herself and the newborn, but also potential financial burdens possibly due to loss of employment or reduced pay in the context of the pandemic. Therefore, we cannot say if the increase in women with EPDS scores ≥13 was due to the isolation/visitor ban or simply due to the general context of the pandemic. In this framework, we must emphasise that we have no information about the SARS-CoV-2 status of the participants during birth and in the early puerperium. A potential COVID illness is also likely to have a significant impact on mental health. Due to fear of infection, the illness could affect mother-child bonding and thus MIBS scores. We also did not record any data regarding complications during pregnancy or childbirth, which can also influence psychological wellbeing.
Additional limitations of this study include the voluntary nature of the participation, which led to a high demographic representation of well-educated women. As a result, financial stability and a relatively higher socioeconomic status among participants can be assumed.
All these factors may limit the generalisability of our findings. However, they appear to be comparable to similar settings, at least in Switzerland.
As we found a similar increase in the risk for postpartum depression in both groups of different postpartum isolation, it is unlikely that the increase was related to lack of partner support. Maternal bonding, breastfeeding rates and postpartum complications were not significantly affected by postpartal isolation.
Nevertheless, our study shows that many new mothers do not desire visitors in the period immediately after birth. Further clinical studies are needed in order to determine whether maternity hospitals should create environments with limited visitors and visiting hours to allow the mother more time to recover and bond with their newborn.
Our results show that the COVID-19-associated protective measures of isolation in many Swiss maternity units appear not to have had a clinically relevant negative impact on important aspects of maternal wellbeing. Additional studies are needed to further examine both risks and protective factors that impact maternal psychological wellbeing and the development of mother-child bonding during periods of isolation in our setting. Identifying these variables will enable physicians to promote tailored care for their patients.
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
The Project Leader acts as the sponsor.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. World Health Organization - WHO. Mental health aspects of women‘s reproductive health. A global review of the literature. World Health Organization, 2009 Jan. Available from: https://www.who.int/publications/i/item/9789241563567
2. Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017 Aug;6(1):60.
3. Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
4. Yarcheski A, Mahon NE, Yarcheski TJ, Hanks MM, Cannella BL. A meta-analytic study of predictors of maternal-fetal attachment. Int J Nurs Stud. 2009 May;46(5):708–15.
5. Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S. Depression and anxiety in pregnancy during COVID-19: A rapid review and meta-analysis. Psychiatry Res. 2021 Jun;300:113912.
6. Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JL, Roos LE. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord. 2020 Nov;276:765–74.
7. Mayopoulos GA, Ein-Dor T, Dishy GA, Nandru R, Chan SJ, Hanley LE, et al. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J Affect Disord. 2021 Mar;282:122–5.
8. Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. Deutschsprachige Fassung und Validierung der "Edinburgh postnatal depression scale" [German language version and validation of the Edinburgh postnatal depression scale]. Dtsch Med Wochenschr. 1998 Jan 16;123(3):35-40. German. doi: .
9. Ohara M, Okada T, Kubota C, Nakamura Y, Shiino T, Aleksic B, et al. Validation and factor analysis of mother-infant bonding questionnaire in pregnant and postpartum women in Japan. BMC Psychiatry. 2016 Jul;16(1):212.
10. Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) EPDS Group. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. 2020 Nov;371:m4022.
11. Hashijiri K, Watanabe Y, Fukui N, Motegi T, Ogawa M, Egawa J, et al. Identification of Bonding Difficulties in the Peripartum Period Using the Mother-to-Infant Bonding Scale-Japanese Version and Its Tentative Cutoff Points. Neuropsychiatr Dis Treat. 2021 Nov;17:3407–13.
12. R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/
13. Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Correction: mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021 Dec;11(1):640.
14. Okagbue HI, Adamu PI, Bishop SA, Oguntunde PE, Opanuga AA, Akhmetshin EM. Systematic Review of Prevalence of Antepartum Depression during the Trimesters of Pregnancy. Open Access Maced J Med Sci. 2019 May;7(9):1555–60.
15. O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9(1):379–407.
16. Low SR, Bono SA, Azmi Z. Prevalence and Factors of Postpartum Depression During the COVID-19 Pandemic: A Review. Curr Psychol. 2023 Jan:1–18.
17. Safi-Keykaleh M, Aliakbari F, Safarpour H, Safari M, Tahernejad A, Sheikhbardsiri H, et al. Prevalence of postpartum depression in women amid the COVID-19 pandemic: A systematic review and meta-analysis. Int J Gynaecol Obstet. 2022 May;157(2):240–7.
18. Monti F, Agostini F, Marano G, Lupi F. The course of maternal depressive symptomatology during the first 18 months postpartum in an Italian sample. Arch Womens Ment Health. 2008 Jul;11(3):231–8.
19. Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020 Dec;277:5–13.
20. Brooks SK, Weston D, Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020 Dec;189:26–36.
21. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 Mar;395(10227):912–20.
22. Allegri B, Brenna V, Confalonieri L, Puzzini A, Nichelatti M, Piccinini G, et al. The impact of the second COVID-19 lockdown on anxiety and depressive symptoms in pregnant women: A case study of pregnant women in northern Italy. Brain Behav Immun Health. 2023 Jul;30:100633.
23. Chen Q, Li W, Xiong J, Zheng X. Prevalence and Risk Factors Associated with Postpartum Depression during the COVID-19 Pandemic: A Literature Review and Meta-Analysis. Int J Environ Res Public Health. 2022 Feb;19(4):2219.
24. Thomson G, Feeley C, Moran VH, Downe S, Oladapo OT. Women’s experiences of pharmacological and non-pharmacological pain relief methods for labour and childbirth: a qualitative systematic review. Reprod Health. 2019 May;16(1):71.
25. Tan HS, Agarthesh T, Tan CW, Sultana R, Chen HY, Chua TE, et al. Perceived stress during labor and its association with depressive symptomatology, anxiety, and pain catastrophizing. Sci Rep. 2021 Aug;11(1):17005.
26. Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017 Jul;7(7):CD003766.
27. Shiva L, Desai G, Satyanarayana VA, Venkataram P, Chandra PS. Negative Childbirth Experience and Post-traumatic Stress Disorder - A Study Among Postpartum Women in South India. Front Psychiatry. 2021 Jul;12:640014.
28. Eitenmüller P, Köhler S, Hirsch O, Christiansen H. The Impact of Prepartum Depression and Birth Experience on Postpartum Mother-Infant Bonding: A Longitudinal Path Analysis. Front Psychiatry. 2022 May;13:815822.
29. Mayopoulos G, Ein-Dor T, Li K, Chan S, Dekel S. Giving birth under hospital visitor restrictions: Heightened acute stress in childbirth in COVID-19 positive women. Res Sq [Preprint]. 2020 Dec 9:rs.3.rs-112882. doi:
30. Mariño-Narvaez C, Puertas-Gonzalez JA, Romero-Gonzalez B, Peralta-Ramirez MI. Giving birth during the COVID-19 pandemic: the impact on birth satisfaction and postpartum depression. Int J Gynaecol Obstet. 2021 Apr;153(1):83–8.
31. Layton H, Owais S, Savoy CD, Van Lieshout RJ. Depression, Anxiety, and Mother-Infant Bonding in Women Seeking Treatment for Postpartum Depression Before and During the COVID-19 Pandemic. J Clin Psychiatry. 2021 Jul 6;82(4):21m13874. doi: .
32. Suzuki S. Psychological status of postpartum women under the COVID-19 pandemic in Japan. J Matern Fetal Neonatal Med. 2022 May;35(9):1798–800.
33. Fernandes DV, Canavarro MC, Moreira H. Postpartum during COVID-19 pandemic: portuguese mothers’ mental health, mindful parenting, and mother-infant bonding. J Clin Psychol. 2021 Sep;77(9):1997–2010.
34. Koire A, Mittal L, Erdei C, Liu CH. Maternal-fetal bonding during the COVID-19 pandemic. BMC Pregnancy Childbirth. 2021 Dec;21(1):846.
35. Tichelman E, Westerneng M, Witteveen AB, van Baar AL, van der Horst HE, de Jonge A, et al. Correlates of prenatal and postnatal mother-to-infant bonding quality: A systematic review. PLoS One. 2019 Sep;14(9):e0222998.
36. Kornfield SL, White LK, Waller R, Njoroge W, Barzilay R, Chaiyachati BH, et al. Risk And Resilience Factors Influencing Postpartum Depression And Mother-Infant Bonding During COVID-19. Health Aff (Millwood). 2021 Oct;40(10):1566–74.
37. Dekel S, Thiel F, Dishy G, Ashenfarb AL. Is childbirth-induced PTSD associated with low maternal attachment? Arch Womens Ment Health. 2019 Feb;22(1):119–22.
38. Sakalidis VS, Rea A, Perrella SL, McEachran J, Collis G, Miraudo J, et al. Wellbeing of Breastfeeding Women in Australia and New Zealand during the COVID-19 Pandemic: A Cross-Sectional Study. Nutrients. 2021 May;13(6):1831.
39. Wilson AN, Sweet L, Vasilevski V, Hauck Y, Wynter K, Kuliukas L, et al. Australian women’s experiences of receiving maternity care during the COVID-19 pandemic: A cross-sectional national survey. Birth. 2022 Mar;49(1):30–9.
40. Benahmed N, San Miguel L, Devos C, Fairon N, Christiaens W. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth. 2017 Sep;17(1):289.