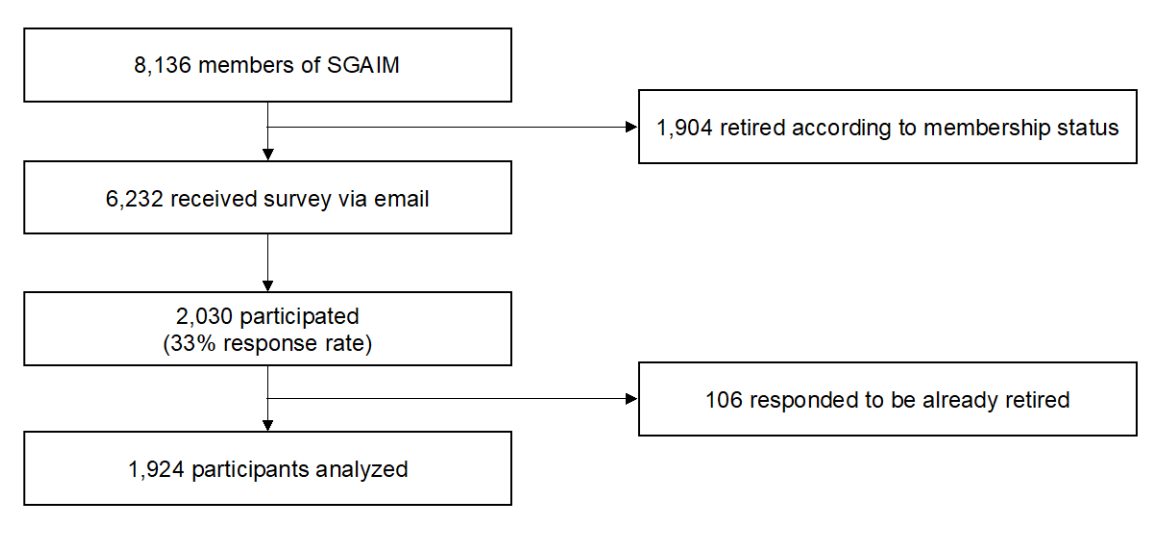
Figure 1Study flowchart
DOI: https://doi.org/https://doi.org/10.57187/s.3861
Generalists (general practitioners and internists in hospitals) play a crucial role in healthcare systems. They can be defined as “first level of professional care (…), where people present their health problems and where the majority of curative and preventive health needs are satisfied” [1–3]. Generalists can handle many health issues. Where necessary they match patient needs to health care resources as well as managing and triaging undifferentiated symptoms [4]. As complexity in medicine increases, more generalists are needed [5]. A balanced number of specialists and generalists is crucial. Generalists complement a healthcare system by dealing with a wide range of health problems, prioritising needs and providing person-centred care [6].
Similar to other countries, the Swiss healthcare system is highly dependent on the immigration of physicians trained outside of Switzerland, mainly from Germany. The latest available report of 2022 showed 1209 new doctors trained within Switzerland vs. 3053 doctors whose credentials were recognised to work as doctors in Switzerland. This proportion has remained about the same since 2011 and is about equal for general internal medicine [7]. Such official numbers are helpful in following trends and proportions of trained general internal medicine, but these registries tend to overestimate the current workforce of generalists [8] due to the trend to work part-time or to the fact that these registries are not necessarily designed to exclude doctors who no longer work.
Therefore, our study is needed to assess the current and future workforce of generalists in Switzerland and to allow a data-driven approach to maintaining the workforce of generalists in the Swiss healthcare system.
We conducted a cross-sectional study to analyse the current and future workforce of generalists in Switzerland. The online survey was open from 7 March 2023 to 5 April 2023.
The Swiss Society of General Internal Medicine, SSGIM (Schweizerische Gesellschaft für Allgemeine Innere Medizin, SGAIM / Société Suisse de Médecine Interne Générale, SSMIG / Società Svizzera di Medicina Interna Generale, SSMIG) is the representative body of general internal medicine. With more than 8,000 members, it is the largest medical society in Switzerland representing physicians specialising in general internal medicine in hospital and outpatient settings. SSGIM stands for reflective, critical and patient-centred medicine. It is committed to promoting young talent and ensuring the maintenance and development of professional expertise through congresses, further education and training. The society supports research and science by awarding various prizes and grants, among other endeavours [9].
The Swiss Society of General Internal Medicine's Young Talent Promotion Committee initiated this study (without a separate protocol paper), and the SSGIM sent an online survey to all newsletter subscribers, of whom >8,000 are members. The prerequisite for ordinary membership is the specialist title in general internal medicine. Resident physicians (still without the specialist title), interested master students and retired internists can become extraordinary members. Two reminders were sent. Retired members were excluded from this study.
The Swiss Society of General Internal Medicine's Young Talent Promotion Committee developed a questionnaire to assess the current and future workforce of generalists, using existing questions from similar workforce studies [8–10]. The questionnaire was an online, closed survey, sent to SSGIM members by e-mail and answered on a voluntary basis without incentives. The questionnaire was piloted for feasibility, length and clarity by peer generalists. The following data were collected: age (in 5-year clusters), gender, language, whether the person was still in residency, current place of work (multiple-choice question), current workload (total of clinical and administrative workload with no differentiation between the two) in percentage and workload, in percentage, 10 years in the future. The survey was anonymous and, therefore, ethical approval was not required.
We imported anonymised data from SurveyMonkey through Excel to Stata version 15.1 (STATA Corp., College Stata TX, USA). Data was prepared for the analysis using techniques such as summarising, analysing ranges and other consistency checks. Hard coding was done to reduce the future workload to 0% for participants who said they would retire by 2033. We reduced workload to 100% for 99 respondents who reported a workload of >100%. We showed data using descriptive methods of proportions, 95% confidence intervals (CI), means and standard deviations (SD). Since the SSGIM membership database used the same data (age bands and gender), we were able to compare participant characteristics with the full target population for generalisation. We reported full-time equivalents (FTEs) by multiplying the number of participants by their current or future workload. The decrease of FTEs over time (2023 to 2033) was calculated by year for easier understanding. To model for different factors and scenarios that will have an impact on the future workforce, the author group chose to focus on 1) interest in becoming a generalist at the end of medical school, 2) workload, 3) dropouts, 4) influx from abroad, 5) early retirement and 6) population growth.
The e-mail containing the survey was received by 6,232 active members, and 2,030 members participated (33% response rate). On average, it took participants 5 minutes to complete the survey. Excluded were 106 respondents because they reported that they had retired (figure 1).
Figure 1Study flowchart
Table 1 describes the baseline characteristics of participants: 46% women, 53% men and 1% non-binary. Participants’ age categories were: 18% younger than 35 years, 19% aged 35 to 45, 21% aged 46 to 55, 25% aged 56 to 65, 18% older than 65. Language preference for the survey was 82% German and 18% French. Of all participants, 19% indicated that they were still training to become generalists. Multiple answers were possible regarding place of work, with 953 participants working in a practice, 273 in a hospital, and 105 in another location. Similar results were found when comparing gender and age across participants and all SSGIM members (table S1 in the appendix).
Table 1Baseline characteristics of participating generalists (n = 1,924).
| Characteristics | n | |
| Gender | Female | 876 (46.0%) |
| Male | 1,016 (53.3%) | |
| Non-binary | 13 (0.7%) | |
| Missing | 19 (1.0%) | |
| Age group | Under 35 years | 344 (17.9%) |
| 35–45 years | 358 (18.6%) | |
| 46–55 years | 398 (20.7%) | |
| 56–65 years | 484 (25.2%) | |
| Over 65 years | 337 (17.5%) | |
| Missing | 3 (0.2%) | |
| Language | German | 1,584 (82.3%) |
| French | 340 (17.7%) | |
| Missing | 0 | |
| Postgraduate training | Ongoing | 370 (19.2%) |
| Completed | 1,554 (80.8%) | |
| Missing | 0 | |
| Years since board examination* | Mean years ± SD | 18.9 ± 10.9 |
| Missing | 360 (23%) | |
| Workplace** | Practice | 953 |
| Hospital | 273 | |
| Other*** | 105 | |
| Missing | 0 | |
* Only reported for generalists with completed postgraduate training
** Multiple-choice questions; hence no proportions in %
*** Other includes teaching or research
1,417 people (missing: 507, 26%) reported an average workload of 83%. Table 2 describes the workload in 2023 stratified by gender and other baseline characteristics. The average workload was 78% for female and 87% for male generalists. The average workload for residents was 89% for females and 94% for males. For generalists having passed board examination, the average workload for women was 76%, and for men 86%. The average workload for both female and male generalists decreases with increasing age, but for those still working at age >65 years (retirement), it is 66% (female) and 68% (male).
Table 2Current workload across age, language and board examination by gender.
| Characteristics | Female generalists | Male generalists | |||||
| n | Mean (95% CI) | p-value* | n | Mean (95% CI) | p-value* | ||
| Overall workload | 663 | 78.3 (76.8–79.8) | 754 | 87.0 (85.5–88.5) | |||
| Workload by age group | <35 years | 150 | 88.0 (85.2–90.8) | <0.001 | 88 | 94.0 (91.2–96.7) | <0.001 |
| 35–45 years | 180 | 72.7 (69.9–75.5) | 107 | 89.7 (87.4–92.0) | |||
| 46–55 years | 176 | 77.3 (74.5–80.1) | 148 | 92.8 (90.8–94.8) | |||
| 56–65 years | 135 | 78.5 (75.5–81.5) | 248 | 92.2 (90.3–94.1) | |||
| >65 years | 22 | 66.4 (53.3–79.5) | 162 | 68.2 (63.4–72.9) | |||
| Workload by language | German | 548 | 78.3 (76.6–80.0) | 0.90 | 625 | 87.1 (85.4–88.7) | 0.86 |
| French | 115 | 78.6 (75.1–82.1) | 129 | 86.7 (83.0–90.4) | |||
| Workload by board examination | Ongoing | 136 | 89.0 (85.9–92.0) | <0.001 | 71 | 93.5 (90.1–97.0) | 0.006 |
| Completed | 527 | 75.6 (74.0–77.2) | 683 | 86.3 (84.7–87.9) | |||
* All p-values derived from univariate regression for each gender separately. For age group, a p for trend is reported.
Information on planned workload in the next 10 years was provided by 1,411 physicians. A large proportion of respondents (38.4%) reported plans to retire by 2033, and another 30.5% planned to decrease their workload, while 21.5% intended to maintain their workload, and 9.6% to increase their workload. As shown in figure 2, our extrapolation of the number and workload per respondent to all SSGIM members (6,232 SSGIM members / 1,411 participants with data on workload 2023 and 2033 = factor 4.42), calculates a current (2023) workforce of 5,237 FTE, with significant changes in 2033: 1,935 FTEs (36%) lost due to retirement, 502 FTEs (10%) lost to workload reduction, 116 FTEs (2%) gained by workload increase and 2,800 FTEs (53%) remaining in the workforce with the same workload as in 2023. In order to maintain the same workforce as in 2023, 2,321 new FTEs (44%) will be needed by 2033.
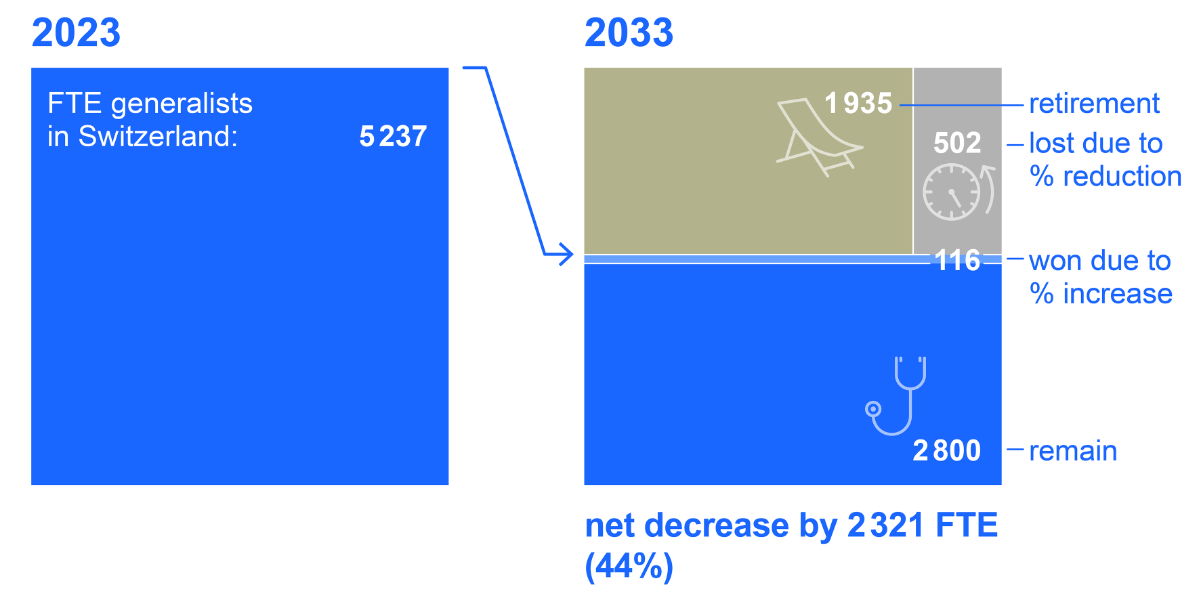
Figure 2Workforce 2023 and 2033. All data presented in full-time equivalent (FTE) by extrapolating data of participants (n = 1,411) on workforce 2023 and 2033 to all SSGIM members not yet retired (n = 6,323) with a respective factor of 4.42.
With the gap of 2,321 FTE by 2033, from figure 2, we modelled this gap for better interpretation on a yearly basis according to different scenarios stratified into the selected factors influencing the number of generalists needed by 2033 (tables 3 and 4).
Table 3Modelling enablers and barriers towards filling the gap in generalists by 2033. FTEs of new generalists per year needed according to interest o become generalists and workload scenarios. Illustrative interpretation of the table: In 2022, 1,200 medical students graduated [11]; if 30% of them became generalists (as in 2022), working at an employment level of 80%, this would generate 288 FTEs of new generalists per year.
| Interest to become generalists | ||||
| 20% | 30% | 50% | ||
| Workload scenarios | 60% | 144 | 216 | 360 |
| 70% | 168 | 252 | 420 | |
| 80% | 192 | 288 | 480 | |
Table 4Modelling enablers and barriers towards filling the gap in generalists by 2033. FTEs of new generalists per year available needed according to board examinations of residents from abroad and dropout scenarios. Illustrative interpretation of the table: In table 3, 252 new FTEs are expected to pass the Swiss board examination. If an additional 10% board-certified residents are expected to come to Switzerland from abroad, then, under the assumption of 15% dropouts, 236 additional new generalist FTEs would be available.
| Board examinations of residents from abroad | ||||
| 0% | 10% | 20% | ||
| Dropout scenarios | 10% | 227 | 249 | 272 |
| 15% | 214 | 236 | 257 | |
| 20% | 202 | 222 | 242 | |
In 2022, about 1,200 medical students graduated in Switzerland [11], and about 30% of all board certifications were in general internal medicine [12], but, according to a new survey among medical students in Switzerland, 47% are interested in becoming generalists [13]. As shown in table 3, we modelled the number of new FTE per year with interests of 20%, 30% and 50% in combination with different workloads such as 60%, 70% and 80%. This results in 252 new FTE per year (range 144 to 480).
We continue with the estimated 252 new FTE per year and model influx from abroad as well as dropouts. In 2022, 1,420 board certifications from outside Switzerland have been accepted of which 134 (9.4%) are in general internal medicine [12]. An earlier study indicates that about 14% of all students who graduate in Switzerland will not actually work in the field (dropouts) [10]. We therefore modelled an influx of generalists as 0%, 10% and 20% as well as dropouts of 10%, 15% and 20%. This results in 236 new FTE per year (range 202 to 272)
Early retirement: In our sample, 47 of 542 (9%) of all those who want to retire by 2033 are under age 55 at the time of this survey. This translates to 181 FTE lost by 2033 due to early retirement.
Change of population: By 2033, almost one million (+9.3%) more persons will live in Switzerland [14]. Therefore, our models could also be increased by +10% to account for this population growth.
The current workforce in general internal medicine will decrease by about 44% from 2023 to 2033 in Switzerland. The large number of almost 40% retirements is the main driver for the decrease while another 30% plan to decrease their workload; 20% plan to keep their workload and 10% intend to increase it. From now until 2033, the workforce of generalists in Switzerland will decrease by about 2,321 FTE. This gap needs to be filled by a new generation of generalists who will be trained mostly in Switzerland. Various factors influence the assumptions under which Switzerland will maintain its current workforce: interest, dropouts, influx from abroad and workload, in addition to early retirements and a growing and ageing population. Switzerland will struggle to close the gap; more efforts are needed to increase the workforce of generalists and to retain the workforce until their retirement.
Our findings agree with others that call for action for the future workforce of healthcare providers, specifically physicians [15–17]. Although we did not focus on the effects of the COVID-19 pandemic on the workforce, it should be noted that the pandemic’s long-term impact on health care is still largely unknown, but its toll on mental health, demoralisation and the wish to leave the profession should increase efforts to protect the workforce [18]. It should be noted that there are also domains and settings where a surplus rather than a lack is expected, such as emergency physicians in the US [19]. Workforce studies using surveys are subject to selection bias. However, official registries can significantly overestimate the healthcare workforce [8, 20] because the registries are not updated, the workload is not known or the future planned workforce is not reported. Many factors influence the development of the workforce, and we have tried to integrate some of them into our scenarios based on interest, workload, dropouts, influx from abroad, early retirement and population growth. We acknowledge that those factors are impacted not solely by decisions from the political decision-makers but also by how the professionals themselves position general internal medicine in the future. Sharpening the profile and acknowledging the broad field in which generalists work are key elements for general internal medicine to be considered and chosen as a career speciality [21].
We acknowledge several limitations in our study. 1) It is a cross-sectional study with a 33% participation rate from members of SSGIM including residents that chose membership, and possibly it does not capture the workforce of all current residents in general internal medicine. In addition, 26% of all respondents did not report their current or future workforce. However, since Switzerland lacks a trustworthy registry to assess the generalist (and residents) workforce, their FTE and their planned workforce, this design is the next best choice. Several reviews have concluded that such response rates in a survey of physicians do not introduce selection bias [22,23]. The characteristics of gender and age across study participants and non-participating SSGIM members are similar; thus generalisation can be assumed but not proven. 2) We asked generalists to predict their workload plans, which may differ from actual events. 3) When assessing future needs, several factors interact, and only the future will demonstrate which factors have the largest effect. Hence, expert opinions [24] form a basis for selecting those factors, as in this paper. Our choice to transparently mention all assumptions, their basis and their variance will help the reader to select the most realistic scenario and calculate the expected demand. To our knowledge, this is the first study to assess the workforce of generalists incorporating FTE instead of counting persons and focusing on generalists in contrast to all physicians or general practitioners (GP) specifically.
On the national level, the Swiss “numerus clausus”, currently applied due to capacity constraints at many universities, needs to be cautiously re-evaluated, with increased placements for bachelor and master students. In addition, we consider it necessary to evaluate an increase in capacity to train future generalists not only at universities but also later in hospitals and in general practice. Generalists themselves can help close the gap by promoting this interesting profession with a close connection to people and a very broad field of activity [25]. However, we acknowledge that shortage of healthcare professionals is a universal problem and that a solution needs not only an increase in FTE of generalists but also 1) better interprofessional collaboration with nurse practitioners, physician assistants, pharmacists and others, 2) a re-focus on patient care and resistance against the increase in unnecessary administrative work, 3) high-quality training opportunities for future generalists including mentoring and strengthening of resilience skills, 4) fostering digital transformation to allow generalists to work more efficiently with focus on patient care.
Switzerland’s workforce of generalists will dramatically decrease by 44% within 10 years. The main driver is retirement, followed by planned workload reductions. The need to fill this gap depends on various factors, including attracting more generalists, workload, dropouts, influx from abroad, retirement and population growth. Based on this study, policymakers, universities, healthcare institutions and professionals themselves should invest in attractive job options and career plans for generalists to fill the gap.
The data used and analysed in this study may be made available upon reasonable request.
We thank all members of SSGIM for their participation and the SSGIM secretariat for their support to distribute the survey and Dr. Kristie Weir and Renata Vidonscky Lüthold for her editorial assistance.
The study did not receive any funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Kringos D, Boerma W, Hutchinson A, Saltman RB. Building primary care in a changing Europe. Eur Obs Heal Syst Policies. 2015;(Observatory Studies Series 38):172.
2. Starfield B. Primary Care: Concept. Evaluation, and Policy; 1992.
3. Europe W. The european definition of primary care / family medicine. Europe. 2002.
4. Ferrer RL, Hambidge SJ, Maly RC. The essential role of generalists in health care systems. Ann Intern Med. 2005 Apr;142(8):691–9.
5. Misky AT, Shah RJ, Fung CY, Sam AH, Meeran K, Kingsbury M, et al. Understanding concepts of generalism and specialism amongst medical students at a research-intensive London medical school. BMC Med Educ. 2022 Apr;22(1):291.
6. Etz R, Miller WL, Stange KC. Simple rules that guide generalist and specialist care. Fam Med. 2021 Sep;53(8):697–700.
7. Büro für arbeits- und sozialpolitische Studien BASS. Bundesamt für Gesundheit BAG: Ärztinnen und Ärzte. 2022;2023:3.
8. Stierli R, Rozsnyai Z, Felber R, Jörg R, Kraft E, Exadaktylos AK, et al. Primary care physician workforce 2020 to 2025 - a cross-sectional study for the canton of bern. Swiss Med Wkly. 2021 Sep;151(35-36):w30024.
9. Schweizerische Gesellschaft für Allgemeine Innere Medizin (SGAIM). Website. https://www.sgaim.ch/de/ueber-uns/portraet. Accessed December 1, 2023.
10. Streit S, da Costa BR, Christensen S, Tal K, Tandjung R, Jüni P. One in seven Swiss physicians has left patient care - results from a national cohort study from 1980-2009. Swiss Med Wkly. 2019 Sep;149(September):w20116.
11. Bundesamt für Statistik. Statistiken aller Medizinalberufe; Website. https://www.bag.admin.ch/bag/de/home/zahlen-und-statistiken/statistiken-berufe-im-gesundheitswesen/statistiken-medizinalberufe1/statistiken-aller-medizinalberufe.html. Accessed March 22, 2024.
12. Bundesamt für Gesundheit. Statistiken Ärztinnen/Ärzte; Website. https://www.bag.admin.ch/bag/de/home/zahlen-und-statistiken/statistiken-berufe-im-gesundheitswesen/statistiken-medizinalberufe1/statistiken-aerztinnen-aerzte.html. Accessed March 22, 2024.
13. Neue Zürcher Zeitung, 55-Stunden-Woche: Damit muss den künftigen Ärztinnen niemand mehr kommen, Website. https://www.nzz.ch/schweiz/55-stunden-woche-damit-muss-den-kuenftigen-aerztinnen-und-aerzten-niemand-kommen-ld.1768569. Accessed March 22, 2024.
14. Bundesamt für Statistik. Szenarien zur Bevölkerungsentwicklung der Schweiz und der Kantone 2020 – 2050. BFS Aktuell. 2020:16. https://www.bfs.admin.ch/asset/de/14963221
15. Aluttis C, Bishaw T, Frank MW. The workforce for health in a globalized context—global shortages and international migration. Glob Health Action. 2014 Feb;7(1):23611.
16. Anderson M, O’Neill C, Macleod Clark J, Street A, Woods M, Johnston-Webber C, et al. Securing a sustainable and fit-for-purpose UK health and care workforce. Lancet. 2021 May;397(10288):1992–2011.
17. Vinci RJ. The Pediatric Workforce: Recent Data Trends, Questions, and Challenges for the Future. Pediatrics. 2021 Jun;147(6):e2020013292.
18. Hendrickson RC, Slevin RA, Hoerster KD, Chang BP, Sano E, McCall CA, et al. The Impact of the COVID-19 Pandemic on Mental Health, Occupational Functioning, and Professional Retention Among Health Care Workers and First Responders. J Gen Intern Med. 2022 Feb;37(2):397–408.
19. Marco CA, Courtney DM, Ling LJ, Salsberg E, Reisdorff EJ, Gallahue FE, et al. The Emergency Medicine Physician Workforce: projections for 2030. Ann Emerg Med. 2021 Dec;78(6):726–37.
20. O’Reilly-Jacob M, Chapman J, Subbiah SV, Perloff J. Estimating the Primary Care Workforce for Medicare Beneficiaries Using an Activity-Based Approach. J Gen Intern Med. 2023 Oct;38(13):2898–905.
21. Card SE, Clark HD, Elizov M, Kassam N. The Evolution of General Internal Medicine (GIM) in Canada: international Implications. J Gen Intern Med. 2017 May;32(5):576–81.
22. Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001 Jan;20(1):61–7.
23. Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997 Oct;50(10):1129–36.
24. Obsan Bericht 04/2022, Zukünftiger Bestand und Bedarf an Fachärztinnen und -ärzten in der Schweiz, Teil 1: Total der Fachgebiete, Hausarztmedizin, Pädiatrie, Psychiatrie und Psychotherapie sowie Orthopädie; Website. https://www.obsan.admin.ch/de/publikationen/2022-zukuenftiger-bestand-und-bedarf-fachaerztinnen-und-aerzten-der-schweiz. Accessed March 22, 2024.
25. Schweizerische Gesellschaft für Allgemeine Innere Medizin. Website. https://www.sgaim.ch/de/themen/nachwuchs/mehrvielfaltgibtsnirgends. Accessed March 22, 2024.
Table S1Comparison of participants and all SGAIM members.
| Characteristics | Participants | All SGAIM members | |
| Number | 1411 | 6232 | |
| Female gender | 46.6% | 46.9% | |
| Age category | Under 45 years | 36.5% | 35.1% |
| 46–55 years | 22.7% | 26.1% | |
| Over 55 years | 42.7% | 38.8% | |
1 All participants with full data on their workforce 2023 and 2023 (n = 513 excluded)
2 As described in the study flowchart, all retired SGAIM members (n = 1,904) were excluded