Figure 1Flowchart of participants (n = 1114).
DOI: https://doi.org/https://doi.org/10.57187/s.3851
Commonwealth Fund
Foederatio Medicorum Helveticorum
digital health
International Health Policy
mobile health
Digital health, or eHealth – a vast field encompassing mobile health (mHealth), health information technology, wearable devices, telehealth and telemedicine – is changing the practice of medicine [1]. Growing evidence suggests that digital health could help manage chronic conditions such as diabetes [2] and cardiovascular diseases [3] and enhance patient well-being [4]. It could also ease the delivery of health services through digital communication technologies [5] and improve medication adherence [6], which is crucial in addressing the challenges posed by increasing polypharmacy related to the rising burden of chronic diseases in the ageing population [7].
Care coordination is a critical component of a strong primary care system [8], and the digitalisation of medicine could help care coordination between healthcare professionals [5]. Patients increasingly can digitally monitor their health and share health data with healthcare professionals, strengthening their empowerment [9]. Access to digital tools, notably through primary healthcare providers, could be one element strengthening care coordination, notably to foster team-based and patient-centred care for the management of chronic diseases [10]. However, the acceptance of digital health by healthcare providers, including primary care physicians, is notably hindered by concerns that it may disrupt the therapeutic relationship with the patient and by the lack of evidence on its benefits and risks [11].
A survey carried out among Finnish physicians showed that 46% felt that digital health could promote an active role for patients in their care and 44% thought that it could improve their access to information [12]. In Germany, another survey showed that around 68% of doctors were positive about mHealth applications, but only 14% had ever prescribed them [13]. The American Medical Association reported that all forms of digital health tools have increased over recent years, from teleconsultations to clinical decision tools and workflow improvements. Furthermore, the doctors surveyed felt that digital health was improving clinical outcomes, diagnostic capabilities and care coordination [14]. In Switzerland, an “eHealth barometer” survey is regularly carried out among doctors and other healthcare professionals. In 2024, it revealed that the perceived potential for eHealth and the use of electronic systems to store and manage patient data were increasing. However, this survey does not examine the relationship between digital health and care coordination [15].
A better understanding of the use of digital health in patient care by primary care physicians and its relationship with care coordination is thus important. Using data from a large survey of primary care physicians, we aimed to (1) describe the digital health use of primary care physicians in Switzerland and its associations with sociodemographic characteristics and (2) assess the relationship between a digital health score (a score built on various items studying the physicians’ use of and involvement in digital health) and the degree of care coordination.
We conducted a secondary analysis of the 2022 International Health Policy (IHP) Survey of the Commonwealth Fund (CWF). The CWF is a non-profit foundation in the USA that has been conducting IHP surveys since 1998 to compare the health system performances of the USA and other high-income countries. The methodology of the IHP has been described elsewhere [16]. Since 2010, Switzerland has been one of the 11 participating high-income countries (with Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, the United Kingdom and the USA). Three target groups are surveyed every 3 years: the resident population aged 18 years and over, the resident population aged 65 years and over, and primary care physicians [17]. In 2022, the IHP survey of primary care physicians, on which our analysis was based, was conducted in 10 countries (Norway did not participate).
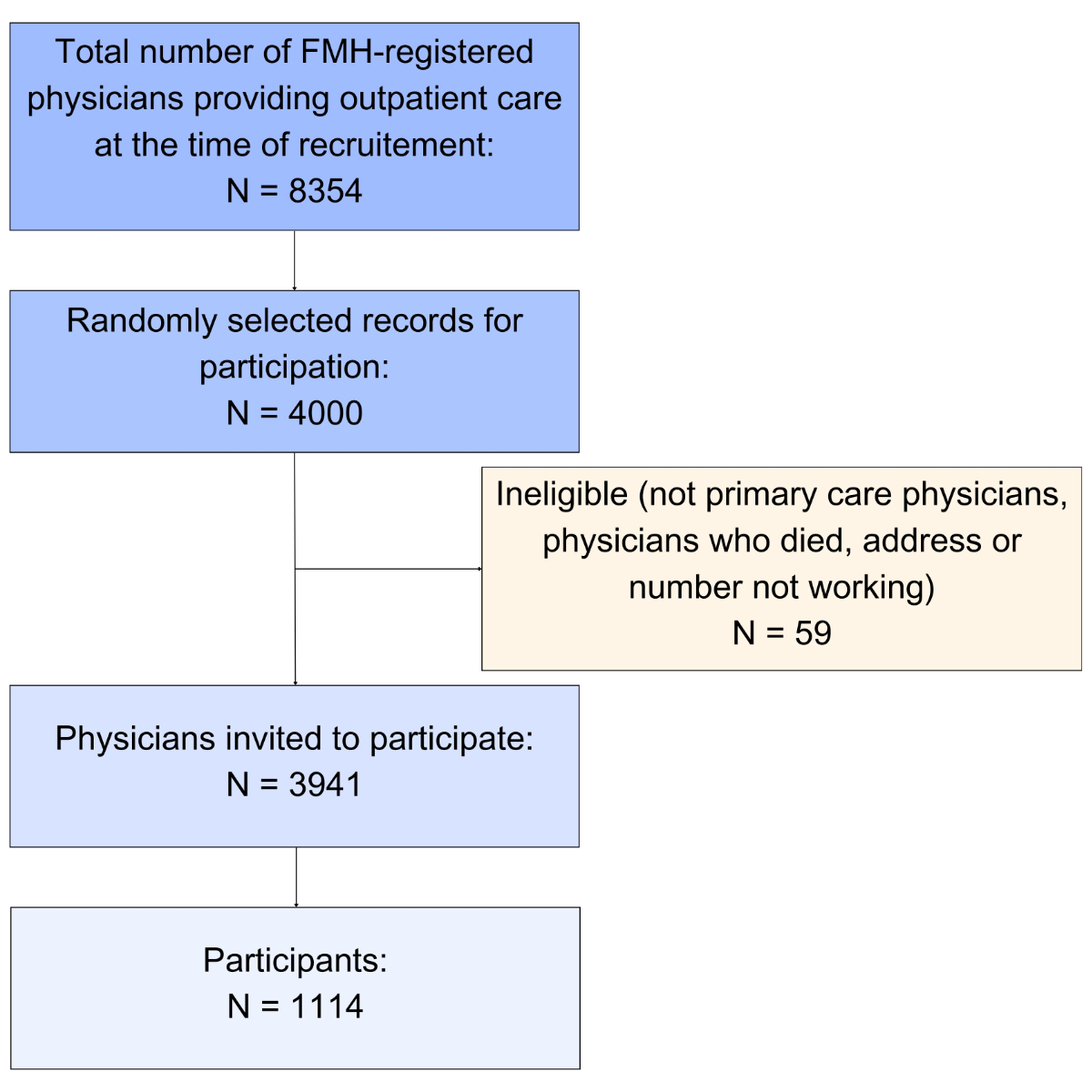
We used the data from the Swiss participants of the 2022 IHP survey. In Switzerland, the most common training to become a primary care physician is a specialisation in internal medicine or paediatrics, both lasting 5 years. Another possibility is to become a “practising physician”: a physician following shorter training, generally 3 years, after which they can set up practice in an outpatient setting [18]. In Switzerland, a large and growing share of physicians is trained abroad. The Swiss Medical Association (FMH [Foederatio Medicorum Helveticorum]) provided the CWF with a random sample of 4000 physicians, chosen from a pool of 8354 physicians registered in 2022, providing outpatient care and with a specialist title of internal medicine (n = 5891), practising physician (n = 1175) or paediatrician (n = 1288). Some 1114 participants completed the questionnaire and constituted our study population (participation rate: 28%). This sample did not include specialists working in a hospital. The flowchart of the participants included in the study is shown in figure 1.
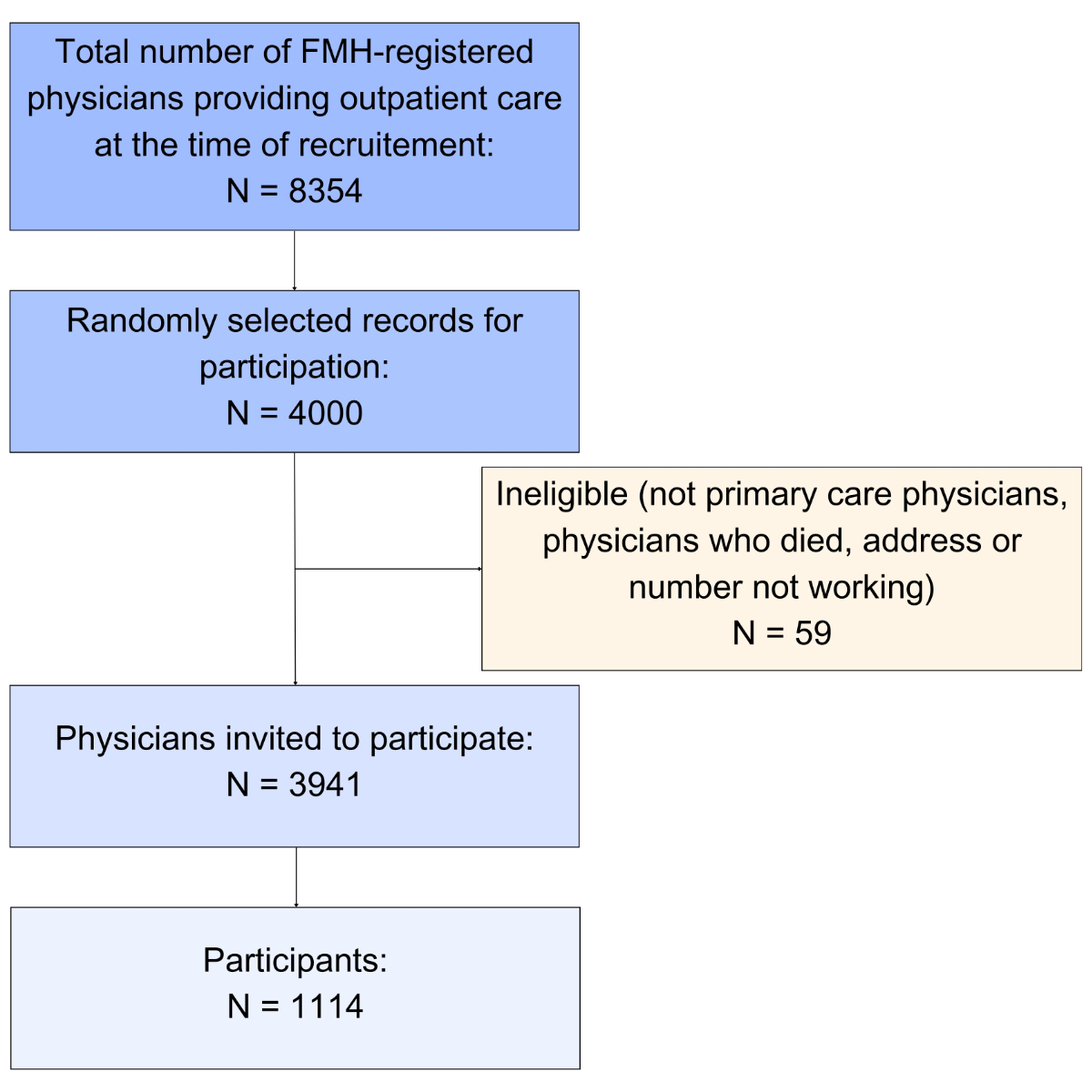
Figure 1Flowchart of participants (n = 1114).
Between March and May 2022, the physicians completed an online questionnaire about their personal and workplace characteristics, their use of digital health and their care coordination. The questionnaire was designed by the CWF, and the data collection in Switzerland was carried out by the company demoSCOPE. The questionnaire aimed to provide information on the physicians’ individual and workplace characteristics, care coordination, digital transformation, and evaluation of their work and the healthcare system in general [19].
For our analysis, we used the following physician and workplace characteristics: age, sex, degree of urbanisation of the practice location, speciality, weekly working hours, number of patients seen per week, type of practice setting (a group practice setting means a practice with at least two physicians) and number of full-time equivalents in the practice.
The assessment of physicians’ digital health use was based on their responses to 10 questions about teleconsultation, the use of connected health tools, electronic patient records and various online services for patients. We built the digital health score based on those items by assigning a value of 0 or 1 to each response and adding these values to obtain a score ranging from 0 to 10. The higher the digital health score, the higher the physicians’ use of and involvement in digital health.
A care coordination score was built based on the responses to five questions about the presence of nurses or case managers to help manage chronic conditions, communication with specialists, and collaboration with home care providers and social services. We built the care coordination score in the same way as the digital health score. Since only five questions on care coordination were available, the score ranged from 0 to 5. We assumed that the higher the care coordination score, the higher the physicians’ coordination with other healthcare professionals. The scores were created based on background knowledge and authors’ expertise because no score exists for physicians’ digital health use or care coordination based on the IHP data.
For the first aim of this study, we reported descriptive statistics on the characteristics, digital health use and care coordination of the primary care physicians. We presented the continuous variables as mean and standard deviation (SD) and categorical variables as number and percentage (%).
For the second aim, we assessed the association between the digital health score and the care coordination score. We first stratified the data by physician characteristics. We then modelled the association between the two scores through two linear regression analyses: one was unadjusted, and the other was adjusted for age, sex, medical speciality and type of practice setting.
Very few data were missing. For both scores, when the answer to a question was missing, we assigned a value of 0.
Ethical approval was obtained to conduct the IHP of the CWF, and no additional approvals were required for secondary analysis of IHP survey data.
The characteristics of the 1114 physicians are shown in table 1. The mean age was 52 years, and 46% were women. Most physicians were German-speaking (70%), had an internal medicine speciality (73%), worked in an urban setting (70%) and worked in a group practice (65%).
Table 1Characteristics of primary care physicians and practice care settings (n = 1114).
| Characteristic | n (%) | |
| Age [years], mean, SD | 52, 10.6 | |
| Sex | Female | 516 (46) |
| Male | 598 (54) | |
| Language | German | 780 (70) |
| French | 242 (22) | |
| Italian | 85 (8) | |
| Rhaeto-Romansch | 7 (1) | |
| Community type | Urban | 781 (70) |
| Intermediate | 201 (18) | |
| Rural | 132 (12) | |
| Medical specialty | Internal medicine | 812 (73) |
| Practising physician | 127 (11) | |
| Paediatrician | 175 (16) | |
| Weekly working hours | Less than 35 | 286 (26) |
| 35–44 | 258 (23) | |
| 45 or more | 568 (51) | |
| Number of patients seen per week | Less than 70 | 441 (40) |
| 70–119 | 418 (38) | |
| 120 or more | 251 (23) | |
| Type of practice setting | Solo practice | 338 (30) |
| Group practice* | 729 (65) | |
| Other | 47 (4) | |
| Number of full-time equivalents in office | Less than 2 | 550 (49) |
| 2 to 3 | 384 (34) | |
| 4 or more | 176 (16) |
SD: standard deviation
* At least two physicians.
Table 2 Digital health score items of primary care physicians (n = 1114).
| Digital health use | Score | n (%) | |
| Proportion of consultations by video | 5% or more | 1 | 36 (3) |
| Less than 5% | 0 | 1071 (96) | |
| Use of connected health tools to monitor the health of patients with chronic diseases | 25% or more | 1 | 185 (17) |
| Less than 25% | 0 | 229 (21) | |
| Never (0%) | 0 | 699 (63) | |
| Use of electronic patient medical records | Yes | 1 | 928 (83) |
| No | 0 | 186 (17) | |
| Possibility to electronically communicate patient clinical summaries | Yes | 1 | 586 (53) |
| No | 0 | 528 (47) | |
| Possibility to electronically communicate diagnostic and laboratory tests | Yes | 1 | 665 (60) |
| No | 0 | 447 (40) | |
| Possibility to electronically communicate lists of medications | Yes | 1 | 574 (52) |
| No | 0 | 539 (48) | |
| Practice allowing email or web communications with patients | Yes | 1 | 986 (89) |
| No | 0 | 128 (11) | |
| Practice allowing online appointment-taking with patients | Yes | 1 | 177 (16) |
| No | 0 | 936 (84) | |
| Practice allowing online medical prescription renewal | Yes | 1 | 226 (20) |
| No | 0 | 888 (80) | |
| Practice allowing online laboratory result acknowledgement by patients | Yes | 1 | 204 (18) |
| No | 0 | 907 (81) | |
| Use or plan to use the Swiss-wide “electronic patient record” | Already use it | 0 | 28 (3) |
| Plan to use it within the next 2 years | 0 | 268 (24) | |
| Plan to use it within 2 years or more | 0 | 379 (34) | |
| Not using it and not planning to | 0 | 433 (39) |
* Values used to build the score. We summed all variables to obtain a score ranging from 0 to 10.
Descriptive statistics of the care coordination of physicians are shown in table 3. Most physicians (79%) shared patient history with specialists during referral 75% of the time or more and shared (59%) or received (71%) patient information from homed-based nursing care 50% of the time or more. Some 56% were collaborating with nurses or case managers inside or outside the practice to help chronic disease management, and 94% had some collaboration with social services. The mean digital health score was 4.1 (SD: 2.0), and the median score was 4 (interquartile range [IQR]: 2 to 6). The care coordination score ranged from 0 to 5, with a mean of 3.6 (SD: 1.3) and a median of 4 (IQR: 3 to 5). Both scores increased as the number of weekly working hours increased (see stratified analyses in appendix table S1). Physicians’ speciality was associated with both scores, with paediatricians having the lowest means in both scores and practising physicians having the highest digital health scores. The digital health score was also associated with more full-time equivalent staff in the practice and being in a group practice setting compared to solo practice.
Table 3Care coordination score items of primary care physicians (n = 1114).
| Care coordination | Score* | n (%) | |
| Presence of a nurse or case manager to help chronic disease management inside or outside the practice | Yes | 1 | 624 (56) |
| No | 0 | 490 (44) | |
| When your patients have been referred to a specialist, how often do you send the patient history and the reason for the consultation to the specialist? | 75% or more | 1 | 876 (79) |
| 25–74% | 0 | 162 (15) | |
| Less than 25% | 0 | 75 (7) | |
| For your patients who receive home-based nursing care, how often do you communicate with home-based nursing care providers about your patients’ needs and the services to be provided? | 50% or more | 1 | 656 (59) |
| 25–49% | 0 | 229 (11) | |
| Less than 25% | 0 | 114 (10) | |
| Does not apply | 0 | 115 (10) | |
| For your patients who receive home-based nursing care, how often are you advised by the home-based nursing care providers of a relevant change in your patients’ condition or health status? | 50% or more | 1 | 788 (71) |
| 25–49% | 0 | 123 (11) | |
| Less than 25% | 0 | 86 (8) | |
| Does not apply | 0 | 111 (10) | |
| Collaboration with social services | Some collaboration | 1 | 1043 (94) |
| No collaboration | 0 | 71 (6) |
* Values used to build the score. We summed all variables to obtain a score ranging from 0 to 5.
Figure 2 shows the mean care coordination score stratified by physicians’ digital health score. The higher the care coordination score, the higher the digital health score. Table 4 shows the regression between the digital health score and the care coordination score, unadjusted and adjusted for age, sex, medical speciality and group practice setting. We found a positive association between both scores (regression coefficient 0.06, 95% confidence interval [CI] 0.03–0.10, p = 0.001).
Table 4Regression between digital health score and care coordination score (n = 1114), unadjusted and adjusted for age, sex, medical speciality and type of practice setting.
| Variable | Beta coefficient (95% CI) | R-squared | Prob >F | p-value |
| Unadjusted digital health score | 0.06* (0.02–0.10) | 0.01 | 0.001 | 0.001 |
| Adjusted digital health score | 0.06* (0.02–0.09) | 0.17 | <0.001 | 0.001 |
CI: confidence interval.
* For a difference of one unit in the digital health score, a difference existed in the care coordination score of an average of 0.06 units.
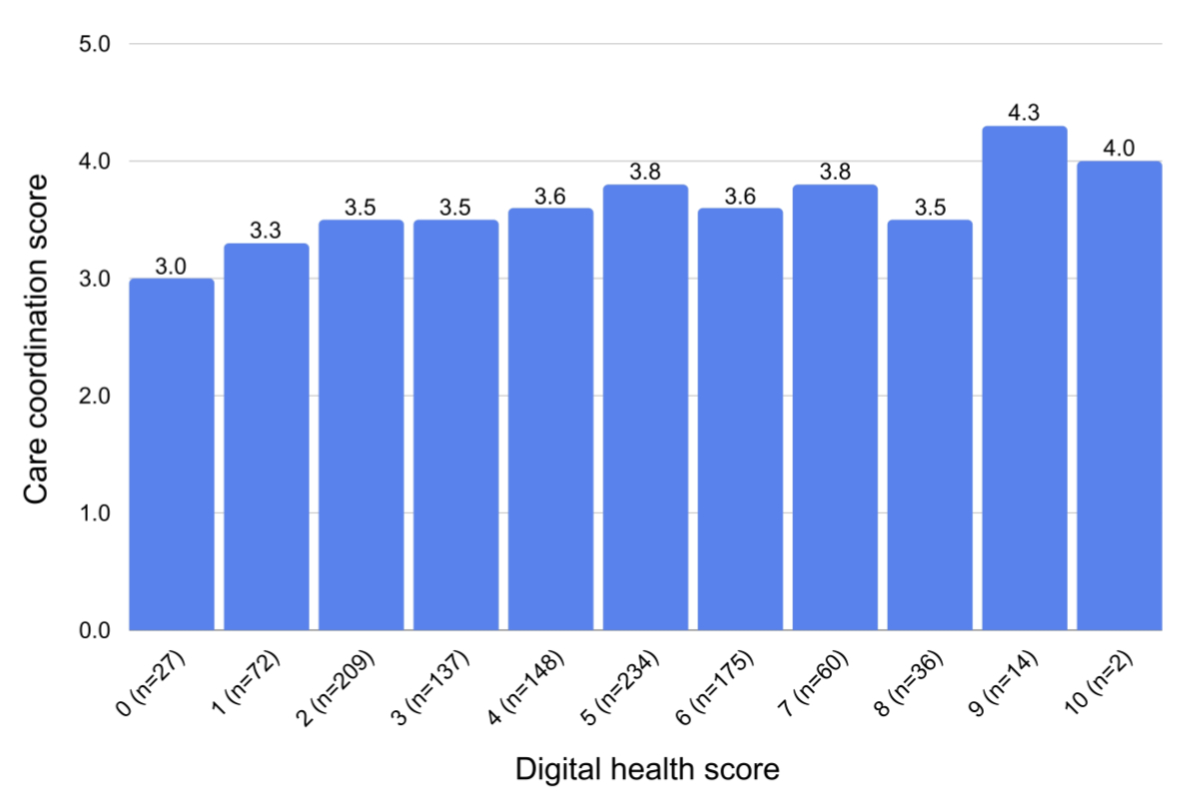
Figure 2Mean care coordination score by eHealth score (n = 1114).
This study aimed to explore the digital health use and care coordination practices of primary care physicians in Switzerland. Our results indicate a greater use of digital health tools in physicians who had more weekly working hours, worked in group practice settings and were practising physicians. This suggests that physicians who dedicated more time to their professional activities tended to have higher utilisation of digital health. Our results also indicate that physicians in solo practices were less likely to engage in digital health compared to their colleagues in group practice settings. This disparity could be attributed to the initial costs of electronic health records, along with the technical and time-related challenges associated with the adoption of digital health, which are frequently cited as barriers to its implementation and could be more easily addressed in collaborative environments [20].
We found a modest correlation between primary care physicians’ digital health score and care coordination score, suggesting that physicians who embraced digital health were overall more likely to engage in collaborative practices, such as sharing patient information with specialists and collaborating with home-based nursing care. Given other studies on the association of digital health with care coordination [21], considering that one could influence the other is becoming mainstream. However, due to the design of our study and the modest degree of association, this positive relationship could be confounded.
Many barriers exist to the adoption of digital health at both the patient and clinician levels. Our study shows a slight positive association between working hours and digital health use, where individuals with higher digital health use were also working more. A possible explanation is that physicians who work more tend to use more digital health tools to try to reduce their workload. However, the use of digital health could also add workload, which is often cited as a barrier to digital health adoption [22]. As suggested by a study published in 2021 in the Netherlands, this barrier can be addressed by adapting new technologies to the organisational structure and daily care processes and deploying the human resources required for daily care processes in line with the desired results [23]. This would reduce workload and increase adherence to digital health.
Internationally, the uptake of digital health varies by country, and Switzerland is often considered to lag behind many other countries. The International Health Policy Survey also revealed that, among the 10 OECD (Organisation for Economic Co-operation and Development) countries, Swiss physicians used the least electronic medical records and rarely transmitted patient-related documents electronically [19]. If the benefits of digital health are confirmed for patients and potentially for healthcare professionals, considering the central role of primary care physicians in patient care and engagement, policies seem necessary to enhance its implementation through better uptake among primary care physicians.
This study has some limitations. The survey was completed online and probably selected participants who were more likely to be involved in digital tools. The relatively low participation rate could have led to participation bias, and participants were probably keener to use eHealth tools. Nevertheless, the characteristics of primary care physicians are comparable between this survey and the 2022 FMH data. With a mean age of 52 versus 54 years for primary care physicians, and 46% versus 44% women, respectively [24], this similarity suggests that the survey may provide a representative portrayal of the situation in Switzerland. Additionally, self-reported information was reported in the questionnaire, suggesting a possible information bias.
A key limitation of the study is that we cannot claim that digital health use is the cause of greater care coordination. A causal relationship is possible, but it is also possible that both reflect another factor specific to the physician. Furthermore, although variables concerning medical and paramedical professionals were included, many aspects of care coordination were not fully reflected in the current score. Our study is a secondary data analysis and is strongly constrained by the data collected in this survey. Regarding the scores, we did not have another dataset to validate the score and did not perform any internal validation. We did not find a validated score that would fit our data.
The main strength of this study is its large number of participants from a random sampling of a significant share of physicians in the country. It also covers many variables characterising care coordination and the use of digital health and describes a wide range of possible uses for eHealth.
In conclusion, our findings might help better understand the use of digital health in primary care physicians in Switzerland and its association with care coordination. Recognising the factors associated with the adoption of digital health tools is essential for developing targeted strategies to overcome barriers and promote a more universally integrated and effective healthcare system.
The data and the code used to perform the analyses of this study can be shared upon request. Data are publicly available by contacting the CWF. A protocol or registration for this study was not prepared. Statistical analyses were performed using Stata 17 software (Stata Corp, TX, 2021) without using specific packages.
We thank the Swiss Federal Office of Public Health for granting access to the data.
Authors’ contributions: MJ, VS, ST and AC wrote the protocol for the study. MJ analysed the data under the guidance of ST and drafted the manuscript with contributions by VS, ST and AC. All authors revised and approved the final version of the manuscript before submission.
The Commonwealth Fund is primarily funded through an endowment consisting of financial assets and investments. Additionally, it may receive contributions and grants from philanthropic organisations, government agencies, and individual donors who support its mission to improve healthcare access and quality.
Funding for “The Commonwealth Fund’s 2022 International Health Policy Survey of Primary Care Physicians in 10 Countries”: Core funding: The Commonwealth Fund. Co-funding or technical assistance from the following organisations: The Australian Institute of Health and Welfare; The Canadian Institute for Health Information; Commissaire à la santé et au bien-être du Québec; Ministère de la Santé et des Services sociaux; French La Haute Autorité de Santé; the Caisse Nationale d'Assurance Maladie des Travailleurs Salariés; German Ministry of Health and IGES Institut GmbH; The Dutch Ministry of Health, Welfare and Sport; The Royal New Zealand College of General Practitioners; The Swedish Agency for Health and Care Services Analysis (Vård- och omsorgsanalys); The Swiss Federal Office of Public Health; The Health Foundation.
No specific funding existed for this study. The CWF data were obtained free from the Swiss Federal Office of Public Health.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. What is Digital Health? FDA. 2020. Available from: https://www.fda.gov/medical-devices/digital-health-center-excellence/what-digital-health
2. Wu X, Guo X, Zhang Z. The Efficacy of Mobile Phone Apps for Lifestyle Modification in Diabetes: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth. 2019 Jan;7(1):e12297. doi: https://doi.org/10.2196/12297
3. Bhardwaj V, Spaulding EM, Marvel FA, LaFave S, Yu J, Mota D, et al. Cost-effectiveness of a Digital Health Intervention for Acute Myocardial Infarction Recovery. Med Care. 2021 Nov;59(11):1023–30. doi: https://doi.org/10.1097/MLR.0000000000001636
4. Bassi G, Mancinelli E, Dell’Arciprete G, Rizzi S, Gabrielli S, Salcuni S. Efficacy of eHealth Interventions for Adults with Diabetes: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Aug;18(17):1–2. doi: https://doi.org/10.3390/ijerph18178982
5. Pais B, Buluschek DP, Nef T, Schütz N, Saner H, Gatica D, et al. De nouvelles technologies au service du maintien à domicile des personnes âgées. Rev Med Suisse. 2019;15(658):5. doi: https://doi.org/10.53738/REVMED.2019.15.658.1407
6. Pouls BP, Vriezekolk JE, Bekker CL, Linn AJ, van Onzenoort HA, Vervloet M, et al. Effect of Interactive eHealth Interventions on Improving Medication Adherence in Adults With Long-Term Medication: systematic Review. J Med Internet Res. 2021 Jan;23(1):e18901. doi: https://doi.org/10.2196/18901
7. Santschi V, Rodondi N, Bugnon O, Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: a cluster 12-month randomised controlled study. Eur J Intern Med. 2008 Oct;19(6):427–34. doi: https://doi.org/10.1016/j.ejim.2007.12.007
8. Sovran V, Ytsma A, Husak L, Johnson T. Coordination of Care Could Improve: Canadian Results from the Commonwealth Fund International Health Policy Survey of Primary Care Physicians. Healthc Q. 2020 Jul;23(2):6–8. doi: https://doi.org/10.12927/hcq.2020.26283
9. Ashrafzadeh S, Hamdy O. Patient-Driven Diabetes Care of the Future in the Technology Era. Cell Metab. 2019 Mar;29(3):564–75. doi: https://doi.org/10.1016/j.cmet.2018.09.005
10. Chiolero A, Rodondi N, Santschi V. High-value, data-informed, and team-based care for multimorbidity. Lancet Public Health. 2020 Feb;5(2):e84. doi: https://doi.org/10.1016/S2468-2667(20)30007-4
11. Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016 Oct;11(1):146. doi: https://doi.org/10.1186/s13012-016-0510-7
12. Saukkonen P, Elovainio M, Virtanen L, Kaihlanen AM, Nadav J, Lääveri T, et al. The Interplay of Work, Digital Health Usage, and the Perceived Effects of Digitalization on Physicians’ Work: Network Analysis Approach. J Med Internet Res. 2022 Aug;24(8):e38714. doi: https://doi.org/10.2196/38714
13. Wangler J, Jansky M. How can primary care benefit from digital health applications? – a quantitative, explorative survey on attitudes and experiences of general practitioners in Germany. BMC Digit Health. 2024 Mar;2(1):14. doi: https://doi.org/10.1186/s44247-024-00068-x
14. Henry TA. 5 insights into how physicians view, use digital health tools. American Medical Association. 2022. Available from: https://www.ama-assn.org/practice-management/digital/5-insights-how-physicians-view-use-digital-health-tools
15. Golder L, Keller T, Schena C, Rellstab S. Baromètre cybersanté suisse (eHealth Barometer) 2024: vers l’avenir avec l’IA. gfs.bern. 2024. Available from: https://cockpit.gfsbern.ch/fr/cockpit/ehealth-professionnels-de-sante-2024/
16. Rapoport R, Manley R, Kline C. Metholodogy report. International Health Policy Survey of Primary Care Doctors; 2022.
17. The Commonwealth Fund - International Surveys. The Commonwealth Fund. 2023. Available from: https://www.commonwealthfund.org/international-surveys
18. ISFM. Médecin praticien. 2023. Available from: https://www.siwf.ch/fr/formation-postgraduee/medecin-praticien.cfm
19. Pahud O, Dorn M. Ärztinnen und Ärzte in der Grundversorgung – Situation in der Schweiz und im internationalen Vergleich. Swiss Health Observatory. 2023. Available from: https://www.obsan.admin.ch/de/publikationen/2023-aerztinnen-und-aerzte-der-grundversorgung-situation-der-schweiz-und-im
20. Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to Electronic Health Record Adoption: a Systematic Literature Review. J Med Syst. 2016 Dec;40(12):252. doi: https://doi.org/10.1007/s10916-016-0628-9
21. Ibrahim MS, Mohamed Yusoff H, Abu Bakar YI, Thwe Aung MM, Abas MI, Ramli RA. Digital health for quality healthcare: A systematic mapping of review studies. Digit Health. 2022 Mar;8:20552076221085810. doi: https://doi.org/10.1177/20552076221085810
22. Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HG. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. 2021 Feb;2(1):62–74. doi: https://doi.org/10.1093/ehjdh/ztab005
23. Tossaint-Schoenmakers R, Versluis A, Chavannes N, Talboom-Kamp E, Kasteleyn M. The Challenge of Integrating eHealth Into Health Care: Systematic Literature Review of the Donabedian Model of Structure, Process, and Outcome. J Med Internet Res. 2021 May;23(5):e27180. doi: https://doi.org/10.2196/27180
24. Hostettler S, Kraft E. Statistique médicale 2022. Bull Médecins Suisses. 2023;104(12):24–9.
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3851.