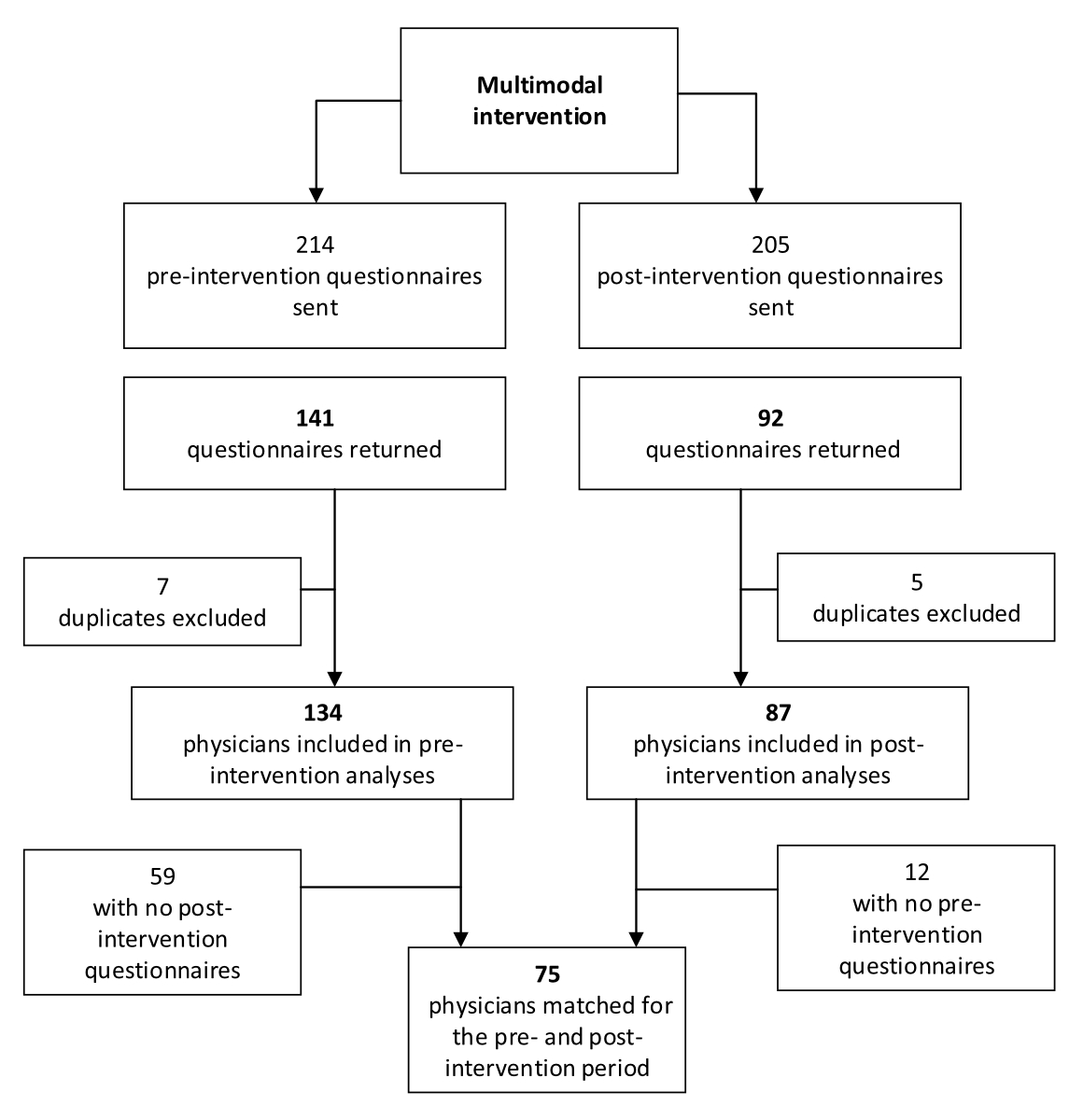
Figure 1Study flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.3801
Physician wellbeing is defined as the optimal interaction of efficient clinical practice, a culture of wellness and personal resilience, and it is related to job and career satisfaction [1]. The concept has come under increasing scrutiny recently due to growing levels of burnout and stress among all medical professionals [2]. Physicians are twice as likely as other professionals to be dissatisfied with their work-life balance, and to think that their schedules do not leave them enough time for personal or family life [3]. Indeed, cross-sectional epidemiological studies have shown that 10–20% of physicians are depressed and 30–45% have symptoms of burnout [3–5]. In cross-sectional prevalence studies in Switzerland, about one third of primary care physicians presented with moderate burnout [6]. This prevalence is even higher among residents in General Internal Medicine (GIM), with 60% complaining of burnout, 19% reporting reduced wellbeing and 21% having career-choice regrets [7]. Physician wellbeing is, therefore, an important issue.
Some medical specialties are at greater risk. In a large 2011 US study, General Internal Medicine ranked 2nd among 24 specialties (after emergency medicine) in terms of the prevalence of burnout symptoms and 18th in terms of satisfaction with work-life balance [3]. Measures were subsequently taken, but constraints also increased (e.g. computerisation, administrative workload). In 2022, a new longitudinal follow-up study of the same population showed a decline in the prevalence of burnout overall. However, GIM physicians’ satisfaction with their work-life balance had not improved over this 10-year period [8]. Internal Medicine remained one of the specialties (like rehabilitation) reporting significant rates of burnout and low proportions of job satisfaction [8].
Panagioti et al. also found that young physicians were at a higher risk of burnout than more experienced physicians [9]. For residents, a low proportion of working time spent on activities that were perceived as rewarding and a high number of total hours worked are the most significant modifiable predictors of reduced wellbeing [4, 7, 10].
Better wellbeing has a direct positive impact on physician productivity, quality of care [11] and patient safety [12]. Physician wellbeing correlates negatively with the prevalence of suicidal ideation and motor vehicle accidents [7]; thus, their wellbeing should be a cornerstone of physician and patient health. Interventions to reduce stress and burnout among physicians can be organisation-directed interventions, which adapt work environments and organisational structure (e.g. shorter shifts, modifications in clinical work processes), or individual-focused interventions (e.g. stress management, self-care training). Meta-analyses of randomised and cohort studies have shown promising results, with mean absolute reductions in burnout proportions from 54% to 44% (p <0.001) [13]. However, additional research is needed to clarify which categories of beneficial interventions best reduce physician burnout, and which interventions or combinations of interventions might be most effective [13]. New research should also focus on prevention among physicians at a higher risk of burnout, like less experienced physicians working in General Internal Medicine, emergency departments (ED) or rehabilitation [9].
We hypothesised that a hospital programme for improving physician wellbeing (e.g. promoting breaks) could mitigate certain modifiable factors and have a measurable impact on work-related quality of life. Thus, we aimed to quantify the change in self-reported wellbeing and job satisfaction among residents and senior physicians after a multimodal intervention to promote an institutional culture of wellbeing.
We conducted a single-centre, cross-sectional, pre- and post-intervention study using a self-reporting questionnaire completed before (September–October 2022) and two months after (March–April 2023) a multimodal programme on wellbeing. All physicians received written and oral information about the study and gave their informed consent to participate. The Human Research Ethics Committee of the Canton of Vaud approved the study (reference number: CER-VD 2022-01078). This article follows the STROBE Checklist for reporting observational studies [14]. The study was co-funded by the Swiss Society of General Internal Medicine Foundation and the local institution where the study took place.
Neuchâtel Hospital Network (NHN) is a mid-sized public teaching hospital spread over multiple sites, and it is the main regional hospital for a population of nearly 180,000 inhabitants. All the residents, chief residents and senior physicians working in one of the NHN’s two General Internal Medicine wards, its ED or the Rehabilitation Department, were eligible.
Eligible participants were identified using the lists of staff working in the participating departments during the study period. They received oral and written information on the study and then had to sign a consent form if they were willing to participate. We used a commercial survey distributor (SurveyMonkey©, SurveyMonkey Inc., Mateo, CA, USA) that enabled us to invite participants to complete our questionnaire using email. A maximum of three emails were sent out to remind participants to complete the survey. Participants received a unique participation code and were invited to complete the same questionnaire twice (before and after the intervention); therefore they did not provide any identifying personal data (first name, surname or age) on the questionnaire. At the end of the study, each participant’s two questionnaires were matched. Only the first author had access to the coded data. Before the statistical analyses, the study participants’ codes were erased from the final databases so that no links could be made between the results and the participants. Since NHN is a teaching hospital, many physicians doing their residency come and go each year. Thus, the unmatched study population included residents and chief residents present at either the pre- or post-intervention period.
The multimodal intervention resulted from a decision to quantify a change in the NHN’s institutional culture regarding its employees’ wellbeing that will remain after the study’s completion. The intervention combined individual-directed and organisation-directed measures involving hospital administrators, shift schedulers (in the hierarchy) and physicians (supplementary figures 1–7).
Four interviews were held with hospital administrators over nine months to promote senior and junior physicians’ wellbeing and to describe their needs. This led to the institution’s official and financial support for the study and a one-day institutional campaign named “Wellbeing inspires doing well” (supplementary figure 1).
Shift schedulers in every department on every NHN site were involved so as to produce optimal local shift schedules to ensure systematic undisturbed (pager- and/or phone-free) lunch breaks (supplementary figure 2), to encourage 15-minute morning and afternoon breaks (supplementary figure 3) and to share ideas on how to decrease physicians’ administrative workloads (supplementary figure 2). Two quiet rooms with multisensory relaxation pods were also made available (supplementary figures 4 and 5).
Occupational health and wellbeing were promoted using information posters (supplementary figure 6), advertisements on the hospital’s website, lecture sessions (30 minutes on sleep hygiene and one hour on creating a break-taking culture) and flyers (supplementary figure 7). Finally, study champions were identified in each department to promote study adherence (e.g. break planning) and to collect feedback.
Data were collected through online questionnaires. Monthly overtime hours worked and sick days were collected anonymously from the human resources management system over the 2-month periods before (September–October 2022) and after (March–April 2023) the intervention.
The study questionnaire collected self-reported data on sociodemographics, sports habits, time spent on recreational activities, the number and duration of lunch breaks (last 5 days), the number of short breaks taken during the day (not including lunch break), mean hours of sleep (last 3 days), numbers of evenings (17:00–22:00) and night shifts (22:00–07:00) in the last 30 days, awareness of existing resources available to support health, working conditions, employee benefits (supplementary figure 7), past episodes of sick leave for work overload or burnout (in the last 3 years) and a work-related quality-of-life measurement. We chose the University of Portsmouth’s Work-Related Quality of Life (WRQoL) scale [15] as it is a commonly used measure of job satisfaction, has been used in hospital environments and has a validated French translation. All questions in the 23-item psychometric scale are scored on a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree) and are grouped into six psychosocial subscales: General Well-Being (GWB), Home-Work Interface (HWI), Job and Career Satisfaction (JCS), Control at Work (CAW), Working Conditions (WCS) and Stress at Work (SAW). The mean scores for each subscale are averaged into a single mean WRQoL score (1–5, with higher scores meaning higher WRQoL) [15]. The overall WRQoL score is the mean of all 23 items.
The primary outcome was the proportion of physicians who scored >3 on the overall WRQoL score. This arbitrary cut-off was chosen to identify the physicians whose average quality of life was better than neutral (scored 3 on the Likert scale). Secondary outcomes were the overall WRQoL score, WRQoL subscale scores, the number of short breaks during the working day, the number of lunch breaks, physicians’ likeliness to recommend their job to peers (0–10, with higher scores meaning more likely), monthly overtime hours worked and monthly sick days.
The sample size was determined by the number of physicians working in participating departments. We expected a 70% participation rate among junior residents and senior physicians working in the NHN’s departments of internal, emergency and rehabilitation medicine. A sample of 105 participants (pre- and post-intervention) yielded a power of 0.7 to demonstrate a 5% improvement in physician job satisfaction (from 50% to 55%) with a two-sided alpha error of 5% (McNemar test) and a power of 0.9 to demonstrate a 10% improvement (from 50% to 60%) [3].
The primary analysis used a McNemar test to examine the difference in the number of physicians satisfied with their job pre- and post-intervention (matched analysis). The secondary analysis used a chi-squared test to examine the difference in the proportions of physicians satisfied with their job in the unmatched population. Participants with data missing on the main outcome (WRQoL) were not included in the primary matched analysis. However, they were analysed in the unmatched analysis. No imputed analysis for missing data was planned.
Pre- and post-intervention overall WRQoL scores and subscales were compared using the paired Wilcoxon signed-rank test. This was repeated for three subgroups: women vs men, residents vs chief residents/senior physicians and participants with vs without children. Differences in intervention effects between subgroups were tested by comparing changes in WRQoL scores (i.e. post-intervention scores minus pre-intervention scores) using Wilcoxon rank-sum tests.
Factors that might have influenced the overall WRQoL scores in the pre-intervention population (sex, job position, having children, living alone, sleep, number of evening or night shifts, time spent doing sports activities or hobbies, and number and length of breaks) were divided into categories. The differences in each category’s WRQoL scores were tested using a Kruskal-Wallis test. These factors were chosen based on previous reports or on plausible association [3, 7, 11].
Monthly pre- and post-intervention overtime hours were compared using an (unpaired) Wilcoxon rank-sum test. As few sick days were reported, this secondary outcome was not analysed.
A two-tailed p-value of <0.05 was considered statistically significant. Since we did not account for multiplicity, p-values for the secondary outcomes should only be considered hypothesis-generating. We present descriptive continuous data using medians and interquartile ranges (IQRs), since they are non-normally distributed. We present categorical data as counts and percentages. We used chi-squared, Fisher’s exact and Kruskal-Wallis tests to compare different groups appropriately. All analyses were performed using STATA software, version 18.0 (StataCorp LP, College Station, TX, USA).
Between 25 August 2022 and 10 January 2023, 214 pre-intervention questionnaires were sent out and 134 physicians responded (63% response rate) (figure 1). Between 10 March and 5 May 2023, 205 post-intervention questionnaires were sent out and 87 physicians responded (42% response rate).
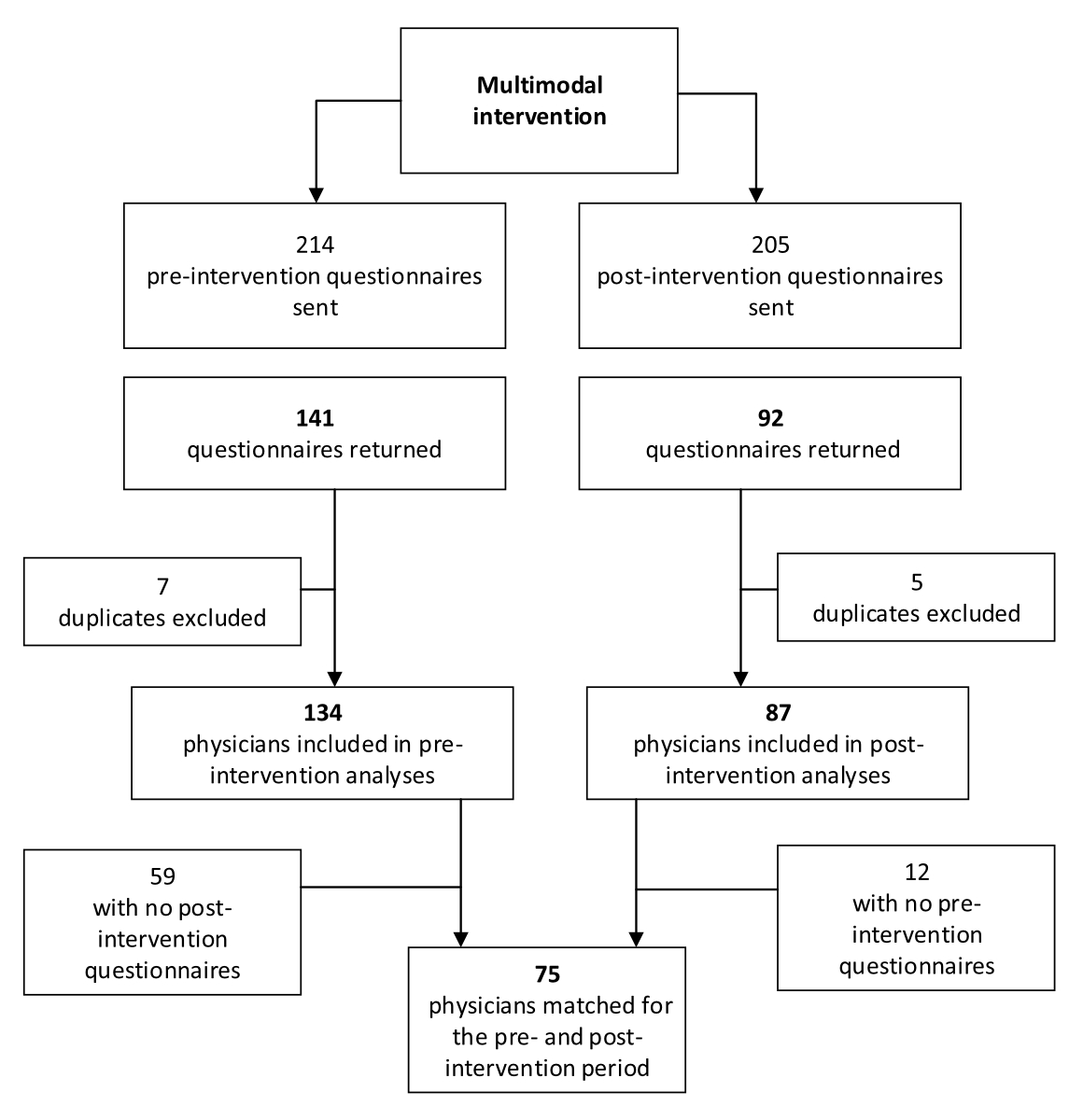
Figure 1Study flowchart.
Seventy-five physicians had matched pre- and post-intervention questionnaires. The characteristics of the matched and unmatched pre- and post-intervention population participants were similar (table 1).
Table 1Pre-intervention, post-intervention and matched population characteristics.
| Unmatched population | Matched population* (n = 75); n (%) | ||||
| Pre-intervention (n = 134); n (%) | Post-intervention (n = 87); n (%) | p-value | |||
| General sociodemographics | |||||
| Women | 74/133 (56%) | 42 (48%) | 0.28 | 34 (45%) | |
| Work position | Residents | 84 (63%) | 45 (52%) | 0.23 | 38 (51%) |
| Chief residents | 17 (13%) | 12 (14%) | 11 (15%) | ||
| Seniors | 33 (25%) | 30 (34%) | 26 (35%) | ||
| Lives | Lives alone | 44 (33%) | 20 (23%) | 0.18** | 17 (23%) |
| Lives as a couple | 74 (55%) | 59 (68%) | 50 (67%) | ||
| Lives with flatmates | 16 (12%) | 8 (9%) | 8 (11%) | ||
| Has children | 42 (31%) | 38 (44%) | 0.07 | 33 (44%) | |
| Age of children | Children in pre-school | 18 (43%) | 16 (41%) | 0.90** | 12/31 (39%) |
| Children in school | 14 (33%) | 15 (38%) | 13/31 (42%) | ||
| Children older than school age | 10 (24%) | 8 (21%) | 6/31 (19%) | ||
| Health, sports and sleep | |||||
| Past history of sick leave due to work-related overload | 13 (10%) | 4 (5%) | 0.20** | 6 (8%) | |
| Mean sleep duration (last 3 days) | <7 h | 69 (51%) | 47 (54%) | 0.59** | 41 (55%) |
| 7–8 h | 64 (48%) | 38 (44%) | 33 (44%) | ||
| >8 h | 1 (1%) | 2 (2%) | 1 (1%) | ||
| Time spent on sports activities during the week (min) | <30 min | 63 (47%) | 39/86 (45%) | 0.61** | 38 (51%) |
| 31–60 min | 33 (25%) | 19/86 (22%) | 16 (21%) | ||
| 61–120 min | 26 (19%) | 19/86 (22%) | 13 (17%) | ||
| 121–240 min | 9 (7%) | 4/86 (5%) | 3 (4%) | ||
| >240 min | 3 (2%) | 5/86 (6%) | 5 (7%) | ||
| Time spent on sports activities at weekends (min) | <30 min | 49 (37%) | 37/86 (43%) | 0.59** | 30 (40%) |
| 31–60 min | 42 (31%) | 26/86 (30%) | 24 (32%) | ||
| 61–120 min | 27 (20%) | 17/86 (20%) | 13 (17%) | ||
| 121–240 min | 9 (7%) | 5/86 (6%) | 6 (8%) | ||
| >240 min | 7 (5%) | 1 (1%) | 2 (3%) | ||
| Time spent on recreational activities during the week (min) | <30 min | 37 (28%) | 26 (30%) | 0.89** | 23 (31%) |
| 31–60 min | 39 (29%) | 28 (32%) | 24 (32%) | ||
| 61–120 min | 32 (24%) | 18 (21%) | 15 (20%) | ||
| 121–240 min | 20 (15%) | 10 (11%) | 8 (11%) | ||
| >240 min | 6 (4%) | 5 (6%) | 5 (7%) | ||
| Time spent on recreational activities at weekends (min) | <30 min | 13 (10%) | 17 (20%) | 0.29 | 7 (9%) |
| 31–60 min | 33 (25%) | 21 (24%) | 24 (32%) | ||
| 61–120 min | 43 (32%) | 21 (24%) | 20 (27%) | ||
| 121–240 min | 21 (16%) | 13 (15%) | 10 (13%) | ||
| >240 min | 24 (18%) | 15 (17%) | 14 (19%) | ||
| Home-hospital travel time (min) | <15 min | 54 (40%) | 34 (39%) | 0.46** | 31 (41%) |
| 16–30 min | 46 (34%) | 27 (31%) | 27 (36%) | ||
| 31–60 min | 25 (19%) | 23 (26%) | 13 (17%) | ||
| >60 min | 9 (7%) | 3 (3%) | 4 (5%) | ||
| Number of evening shifts (16:00–22:00) in last 30 days | 0 | 34/133 (26%) | 23 (26%) | 0.94 | 20 (27%) |
| 1–3 | 27/133 (20%) | 20 (23%) | 14 (19%) | ||
| 4–7 | 29/133 (22%) | 19 (22%) | 19 (25%) | ||
| >7 | 43/133 (32%) | 25 (29%) | 22 (29%) | ||
| Number of night shifts (22:00–07:00) in last 30 days | 0 | 58 (43%) | 35 (40%) | 0.90 | 36 (48%) |
| 1–3 | 23 (17%) | 18 (21%) | 14 (19%) | ||
| 4–7 | 25 (19%) | 17 (20%) | 13 (17%) | ||
| >7 | 28 (21%) | 17 (20%) | 12 (16%) | ||
| Which value most strongly associated with a sense of work satisfaction | Fairness | 12/133 (9%) | 8/86 (9%) | 0.12** | 11 (15%) |
| Training | 48/133 (35%) | 25/86 (29%) | 22 (29%) | ||
| Shift schedules | 15/133 (11%) | 15/86 (17%) | 9 (12%) | ||
| Institutional values | 13/133 (10%) | 4/86 (5%) | 7 (9%) | ||
| Breaks | 3/133 (2%) | – | 1 (1%) | ||
| Recognition by the institution | 39/133 (29%) | 27/86 (31%) | 22 (29%) | ||
| Salary | 3/133 (2%) | 7/86 (8%) | 3 (4%) | ||
* Numbers and values reported for matched participants are derived from the pre-intervention questionnaire.
** Fisher’s exact test.
The primary analysis done among the matched population showed that the proportion of participants satisfied with their job was greater after the intervention than before it (table 2). The same difference was found in the unmatched population but did not reach statistical significance (93/134 [69%] before and 67/87 [77%] after the intervention, p = 0.21) (supplementary table 1).
Participants had statistically significant higher overall WRQoL scores and GWB and HWI subscale scores after the intervention (table 2).
Table 2Main results (matched). Numbers are medians (interquartile ranges) unless stated otherwise. Associations were tested using a matched Wilcoxon rank test or a McNemar test.
| Pre-intervention (n = 75) | Post-intervention (n = 75) | p-value | |
| Primary outcomea | |||
| Physician satisfied with his/her jobb | 49 (65%) | 58 (77%) | 0.02c |
| Secondary WRQoL questionnaire outcomesa | |||
| Overall Work-Related Quality of Life, median (IQR)d | 3.3 (2.8–3.8) | 3.5 (3.1–3.8) | <0.01 |
| Job and Career Satisfaction subscale, median (IQR) | 3.8 (3.2–4.2) | 3.8 (3.5–4.2) | 0.14 |
| Control at Work subscale, median (IQR) | 3.3 (3.0–4.0) | 3.3 (2.7–3.7) | 0.12 |
| General Well-Being subscale, median (IQR) | 3.4 (2.6–4.0) | 3.6 (3.0–4.0) | <0.01 |
| Home-Work Interface subscale, median (IQR) | 2.7 (2.0–3.3) | 3.0 (2.3–3.7) | 0.01 |
| Stress at Work subscale, median (IQR) | 2.5 (2.0–3.5) | 2.5 (2.0–4.0) | 0.19 |
| Working Conditions subscale, median (IQR) | 3.7 (2.7–4.0) | 3.7 (3.0–4.0) | 0.68 |
| Other secondary outcomesa | |||
| Number of lunch breaks last week | 4.0 (2.0–5.0) | 4.0 (3.0–5.0) | 0.36 |
| Time spent at lunch 30–60 min (vs <30 min) | 14 (19%) | 25 (29%) | 0.07 |
| Number of breaks per day (not including lunch) | 0 (0–2) | 1 (0–2) | 0.39 |
| Number of individuals aware of available resources [appendix 7] | 41 (55%) | 43 (57%) | 0.67 |
| How strongly would you recommend your job to others? (0–10), higher number = stronger recommendatione | 8.0 (5.0–8.0) | 8.0 (6.0–9.0) | 0.03 |
a Since we did not account for multiplicity, p-values for the secondary outcomes are only hypothesis-generating
b Participants who scored greater than 3 on the overall Work-Related Quality of Life (WRqoL) score
c McNemar test
d The overall WRQoL score is determined by the average of all items and comprises six subscales
e For this outcome, results are only available for 67 participants. There were no missing values for the primary and other secondary outcomes.
No differences in intervention effects were observed between women and men or between participants with and without children. Residents reported greater benefits from the intervention than chief residents or senior physicians (table 3).
Table 3Pre- and post-intervention Work-Related Quality of Life (WRQoL) changes by subgroups.
| Scalea | Subgroup A | Subgroup B | p-value for group differencesc | ||||
| Pre-intervention: median (IQR) | Post- intervention: median (IQR) | p-valueb | Pre-intervention: median (IQR) | Post-intervention: median (IQR) | p-valueb | ||
| Women (n = 34) | Men (n = 41) | ||||||
| Overall Work-Related Quality of Life | 3.2 (2.6–3.4) | 3.3 (3.0–3.7) | 0.01 | 3.4 (2.9–3.9) | 3.5 (3.3–3.8) | 0.02 | 0.55 |
| Job and Career Satisfaction | 3.7 (3.2–4.0) | 3.7 (3.2–4.2) | 0.31 | 3.8 (3.2–4.2) | 4.0 (3.5–4.3) | 0.29 | 0.84 |
| Control at Work | 3.3 (2.3–3.7) | 3.3 (3.0–3.7) | 0.33 | 3.3 (2.7–4.0) | 3.7 (3.3–4.0) | 0.24 | 0.87 |
| General Well-Being | 3.2 (2.4–4) | 3.4 (2.8–4) | 0.01 | 3.6 (2.8–4.0) | 3.6 (3.0–4.0) | 0.01 | 0.32 |
| Home-Work Interface | 2.7 (2–3) | 2.7 (2.3–3.3) | 0.12 | 3.0 (2.3–3.7) | 3.3 (2.3–3.7) | 0.05 | 0.12 |
| Stress at Work | 2.5 (2–4) | 2.5 (2–3.5) | 0.57 | 3.0 (2.0–3.0) | 3.0 (2.0–4.0) | 0.20 | 0.58 |
| Working Conditions | 3.3 (2.7–4) | 3.7 (3–4) | 0.16 | 3.7 (3.0–4.0) | 3.7 (2.7–4.0) | 0.52 | 0.16 |
| Resident (n = 38) | Chief resident or senior (n = 37) | ||||||
| Overall Work-Related Quality of Life | 3.2 (2.7–3.6) | 3.5 (3.3–3.8) | <0.01 | 3.3 (2.9–3.9) | 3.4 (3.0–3.8) | 0.19 | <0.01 |
| Job and Career Satisfaction | 3.7 (3.3–4.2) | 3.9 (3.7–4.2) | 0.02 | 3.8 (3.2–4.2) | 3.7 (3.2–4.2) | 0.81 | 0.07 |
| Control at Work | 3.0 (2.3–3.7) | 3.3 (3.0–3.7) | 0.05 | 3.7 (3.0–4.0) | 3.7 (3.0–4.0) | 0.91 | 0.14 |
| General Well-Being | 3.5 (2.6–4.0) | 3.7 (3.2–4.0) | <0.01 | 3.4 (2.6–3.6) | 3.4 (2.8–3.8) | 0.06 | 0.38 |
| Home–Work Interface | 2.3 (2.0–3.0) | 2.7 (2.3–3.3) | 0.08 | 3.3 (2.3–4.0) | 3.3 (2.3–3.7) | 0.09 | 0.95 |
| Stress at Work | 2.5 (2.0–3.5) | 3.0 (2.0–4.0) | 0.05 | 3.0 (2.0–3.5) | 2.5 (2.0–3.5) | 0.78 | 0.06 |
| Working Conditions | 3.7 (2.7–4.0) | 3.7 (3.3–4.0) | 0.03 | 3.3 (3.0–4.0) | 3.3 (2.3–4.0) | 0.09 | 0.01 |
| No children (n = 42) | One or more children (n = 33) | ||||||
| Overall Work-Related Quality of Life | 3.3 (2.8–3.7) | 3.5 (3.3–3.8) | <0.01 | 3.2 (2.9–3.8) | 3.3 (3.0–3.7) | 0.07 | 0.13 |
| Job and Career Satisfaction | 3.8 (3.3–4.2) | 3.9 (3.7–4.2) | 0.07 | 3.8 (3.2–4.2) | 3.7 (3.2–4.0) | 0.91 | 0.25 |
| Control at Work | 3.2 (2.7–3.7) | 3.3 (3.0–3.7) | 0.09 | 3.7 (3.0–4.0) | 3.7 (3.0–3.7) | 0.75 | 0.34 |
| General Well-Being | 3.5 (2.6–4.0) | 3.8 (3.2–4.0) | <0.01 | 3.2 (2.6–3.6) | 3.4 (2.8–3.8) | 0.04 | 0.67 |
| Home–Work Interface | 2.5 (2.0–3.3) | 2.7 (2.3–3.3) | 0.19 | 3.0 (2.3–3.3) | 3.3 (2.3–4.0) | 0.03 | 0.43 |
| Stress at Work | 2.5 (2.0–4.0) | 3.0 (2.0–4.0) | 0.16 | 3.0 (2.0–3.0) | 2.5 (2.0–3.5) | 0.68 | 0.42 |
| Working Conditions | 3.7 (2.7–4.0) | 3.7 (3.3–4.0) | 0.12 | 3.3 (3.0–4.0) | 3.3 (2.3–4.0) | 0.30 | 0.07 |
a The overall WRQoL score is determined by the average of all items and comprises six subscales
b Paired Wilcoxon sign-rank test
c The difference in intervention effect between subgroups was tested by comparing changes in WRQoL score (i.e. post-intervention scores minus pre-intervention scores) using Wilcoxon rank-sum tests.
The differences in pre- and post-intervention numbers of lunch breaks and short breaks taken during shifts, and the number of participants who took long breaks, were not statistically significant (table 2).
In the unmatched pre-intervention population, self-reported time spent doing sports activities on weekdays was associated with higher scores on the WRQoL scale and all its subscales (table 4, supplementary table 2). Self-reported time spent doing sports activities on weekends was only associated with GWB subscale scores. Compared to sleeping fewer hours, sleeping 7 hours or more was associated with a higher overall WRQoL score and higher GWB, HWI and SAW subscale scores. Taking a daily lunch break was associated with a higher overall WRQoL score and higher GWB, HWI, SAW and WCS subscale scores.
Table 4Overall Work-Related Quality of Life (WRQoL) scores by category of factors of interest. The analyses were performed in the pre-intervention (n = 134), unmatched population.
| Factors | Overall WRQoL score: Median (IQR) | p-value | |
| Sex | Women (n = 74)* | 3.2 (3.0–3.5) | 0.30 |
| Men (n = 59)* | 3.3 (2.9–3.8) | ||
| Work position | Resident (n = 84) | 3.2 (2.9–3.6) | 0.30 |
| Other (n = 50) | 3.3 (3.0–3.8) | ||
| Has children? | Yes (n = 92)No (n = 42) | 3.3 (3.0–3.7) 3.2 (2.9–3.8) | 0.82 |
| Lives | Alone (n = 44) | 3.3 (3.0–3.9) | 0.69 |
| With flatmates (n = 16) | 3.2 (2.9–3.6) | ||
| As a couple (n = 74) | 3.3 (2.9–3.6) | ||
| Sleep | <7 h (n = 69) | 3.2 (2.8–3.5) | 0.04 |
| ≥7 h (n = 65) | 3.4 (3.0–3.8) | ||
| Number of evening shifts in last 30 days | <4 (n = 61)* | 3.3 (3.0–3.7) | 0.73 |
| ≥4 (n = 72)* | 3.3 (2.9–3.7) | ||
| Number of night shifts in last 30 days | <4 (n = 81) | 3.2 (2.9–3.6) | 0.73 |
| ≥4 (n = 53) | 3.3 (2.9–3.8) | ||
| Sports on weekdays | <30 min (n = 63) | 3.0 (2.7–3.4) | <0.01 |
| 31–60 min (n = 33) | 3.2 (3.0–3.8) | ||
| >60 min (n = 38) | 3.6 (3.3–3.9) | ||
| Sports on weekends | <30 min (n = 49) | 3.2 (2.9–3.4) | 0.06 |
| 31–60 min (n = 42) | 3.2 (2.8–3.8) | ||
| >60 min (n = 43) | 3.4 (3.1–3.8) | ||
| Hobbies on weekdays | <30 min (n = 37) | 3.2 (2.6–3.6) | 0.77 |
| 31–60 min (n = 39) | 3.3 (2.9–3.7) | ||
| >60 min (n = 58) | 3.2 (2.9–3.8) | ||
| Home-work travel time | <15 min (n = 54) | 3.3 (3.0–3.7) | 0.66 |
| 16–30 min (n = 46) | 3.3 (2.9–3.7) | ||
| >31–60 min (n = 34) | 3.2 (2.9–3.6) | ||
| Number of short breaks taken in last 5 days | 0 (n = 71) | 3.3 (3.0–3.8) | 0.36 |
| 1–2 (n = 39) | 3.2 (2.9–3.8) | ||
| 3–10 (n = 24) | 3.2 (2.8–3.7) | ||
| Number of lunch breaks taken in last 5 days | 0–2 (n = 32) | 3.3 (3.0–3.9) | 0.04 |
| 3–4 (n = 46) | 3.1 (2.8–3.5) | ||
| 5 (n = 56) | 3.4 (3.0–3.8) | ||
| Mean lunch break duration (last 5 days) | 0–15 min (n = 25) | 3.3 (2.7–3.8) | 0.57 |
| 15–30 min (n = 84) | 3.2 (2.9–3.7) | ||
| 30–60 min (n = 25) | 3.4 (3.0–3.7) | ||
WRQoL: Work-Related Quality of Life
* One participant with missing value (n = 133)
The difference in the median number of monthly overtime hours per physician pre- (14.0; IQR: 9.0–22.8) and post-intervention (16.4; IQR: 10.6–25.2) was not statistically significant (p = 0.52).
The present study showed that after a multimodal intervention, there was an increase in the proportion of physicians who were satisfied with their job and perceived QoL as employees. They also self-reported higher General Well-Being and Home-Work Interface subscale scores. The intervention’s effects were statistically significant and encouraging. However, the difference in QoL was small and its relevance uncertain.
The overall intervention effect was not uniform, however, with residents reporting feeling greater benefits than did chief residents or senior physicians. This observation contrasts with previous reports. In a meta-analysis including randomised trials and observational studies, no differences were found between residents and experienced physicians with regard to burnout reduction [13]. In contrast, experienced physicians had greater benefit in high emotional exhaustion reduction than residents did [13]. In another meta-analysis focusing on randomised trials, experienced physicians benefited from a greater reduction in burnout scores than their less experienced colleagues [9]. Our intervention’s greater impact on residents may have a number of explanations. Firstly, the intervention was developed around residents’ work schedules. Young physicians must learn many administrative and social skills on top of their clinical skills. With so much to learn, it is easy to overlook the importance of rest. The intervention aimed to structure their work days, including breaks. Senior physicians probably already had personal strategies for coping with their tasks. Secondly, our intervention was (mainly) institutionally led. For reducing burnout, meta-analyses have shown such structural or organisational interventions (e.g. shift reorganisation) to be more effective than those focusing on individuals (e.g. stress management, self-care training) [13, 16]. Thirdly, we included participants at a high risk of lower wellbeing (e.g. General Internal Medicine residents) [3, 9]. This population would be more likely to benefit from an intervention. Finally, we used the WRQoL scales, whereas most other studies have focused on burnout scales.
We hypothesise that the benefits observed after our intervention were mostly due to the positive impacts of introducing a scheduled break during shifts and banning interruptions during meals. This real ‘disconnection’ from clinical work may have favoured calmer, more-enjoyable meal breaks, increased social interactions with colleagues, and a sense of belonging and community at work. Indeed, the importance of regular breaks is recognised [17]. A meta-analysis of studies performed among workers (not healthcare professionals) confirmed the benefit of short breaks on wellbeing, and the effect was proportional to the length of the breaks [18]. Breaks longer than 10 minutes may be necessary to impact performance or to recover properly from highly strenuous tasks [18]. Another systematic review found that breaks improved physician wellbeing, but most of the studies included had a high risk of bias [19].
We also identified factors/behaviours leading to a statistically higher QoL at work: time spent on sports activities, hours of sleep and the number of lunch breaks taken in the last week. Interestingly, sports activities on weekdays had a greater impact than sports activities on the weekend. These results were concordant with previous reports. In one qualitative study, junior physicians identified exercise, sleep quality, a healthy diet and a well-organised workplace as factors supporting their wellbeing [20]. One Chinese study showed that physicians’ emotional exhaustion could be relieved using physical or behavioural interventions (i.e. doing sports) [21]. A review published by Gates et al., associated fatigue and insufficient sleep with lower physician health and wellbeing outcomes [22]. Hakro et al. found that a one-hour lunch break had a positive impact on employees’ physical and psychological health and performance, and reduced their stress at work [23]. All these factors should be targeted in future studies aiming to increase physician wellbeing. In contrast to other studies, we did not find a lower workplace QoL among women [7, 8] or participants without children [7].
The study had some limitations, including a lower-than-expected sample size and a poor response rate (mainly in post-intervention) that affected the study’s power. Although responses were anonymised, the low rate may nevertheless reflect the survey’s sensitive nature. Also, as an observational study, it was impossible to infer the causative nature of the intervention on the differences in wellbeing observed in the pre- and post-intervention periods. Young physicians face a steep learning curve during the first year of work that certainly affects their wellbeing. Because the study did not include a control group, the authors cannot account for this time-related phenomenon without reference to the intervention. Similarly, we cannot evaluate the effects of other, unmeasured confounding factors, such as improvements in ward organisation, which are unrelated to the study but can still affect physicians’ wellbeing. There is no known or validated minimal clinically important difference for the overall WRQoL score, and our primary outcome was based on an arbitrary dichotomisation of the scale that had not previously been used in other studies. Thus, while statistically significant, the true impact of the difference in participants’ quality of life reported after the intervention is unknown and might not be perceptible. Despite its limitations, the present study highlighted some important considerations for hospitals wishing to successfully implement staff health and wellbeing initiatives. A strength of this study lies in its matching questionnaire design that reduced confounding factors in the pre- and post-intervention populations.
Recent reports highlight the “human energy crisis” facing many employees today [18]. In an “always-on” culture, finding a balance between being effective at work and ensuring one’s optimal wellbeing is essential. This intervention on physicians’ wellbeing increased mean overall WRQoL scores; however, the difference was small and its relevance remains uncertain.
The authors would like to thank Mylène Cordary-Basin, Occupational Health Coordinator at the Neuchâtel Hospital Network, and Gérald Brandt, Director of Human Resources at NHN, for their valuable contribution to shaping a culture of wellbeing for our institution’s physicians, for playing a leading role in advising the first author on raising awareness of the issue among hospital administrators and for many other interventions, such as the purchase of multisensory relaxation pods, improvements to quiet rooms, the “Wellbeing inspires doing well” campaign, and the promotion of occupational health. The authors also thank all the participants, especially the participating departments, as well as their local project managers, including Yolanda Espolio, MD, Head of the Geriatrics, Rehabilitation and Palliative Care Department, and Vincent Della Santa, MD, Head of the Emergency Department, for their energy and assistance in increasing study adherence among the physicians working in their departments.
This project was co-funded by the Neuchâtel Hospital Network and the Swiss Society of General Internal Medicine Foundation. Funders had no role in the study’s design, conduct or reporting.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Bohman BD, Sinsky CA, Linzer M, Olson K, Babbott S, Murphy ML, et al. Physician Well-Being: The Reciprocity of Practice Efficiency, Culture of Wellness, and Personal Resilience. NEJM Catal. 2017.
2. Fadel M, Roquelaure Y, Descatha A. Interventions on Well-being, Occupational Health, and Aging of Healthcare Workers: A Scoping Review of Systematic Reviews. Saf Health Work. 2023 Mar;14(1):135–40. doi: https://doi.org/10.1016/j.shaw.2022.12.003
3. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct;172(18):1377–85. doi: https://doi.org/10.1001/archinternmed.2012.3199
4. Luk AL, Yau AF. Experiences of Public Doctors on Managing Work Difficulties and Maintaining Professional Enthusiasm in Acute General Hospitals: A Qualitative Study. Front Public Health. 2018 Mar;6:19. doi: https://doi.org/10.3389/fpubh.2018.00019
5. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009 Nov;374(9702):1714–21. doi: https://doi.org/10.1016/S0140-6736(09)61424-0
6. Goehring C, Bouvier Gallacchi M, Künzi B, Bovier P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med Wkly. 2005 Feb;135(7-8):101–8.
7. Zumbrunn B, Stalder O, Limacher A, Ballmer PE, Bassetti S, Battegay E, et al. The well-being of Swiss general internal medicine residents. Swiss Med Wkly. 2020 Jun;150(2324):w20255. doi: https://doi.org/10.4414/smw.2020.20255
8. Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Wang H, et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2020. Mayo Clin Proc. 2022 Mar;97(3):491–506. doi: https://doi.org/10.1016/j.mayocp.2021.11.021
9. Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017 Feb;177(2):195–205. doi: https://doi.org/10.1001/jamainternmed.2016.7674
10. Montgomery A, Panagopoulou E, Esmail A, Richards T, Maslach C. Burnout in healthcare: the case for organisational change. BMJ. 2019 Jul;366:l4774. doi: https://doi.org/10.1136/bmj.l4774
11. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002 Mar;136(5):358–67. doi: https://doi.org/10.7326/0003-4819-136-5-200203050-00008
12. Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017 Jun;7(6):e015141. doi: https://doi.org/10.1136/bmjopen-2016-015141
13. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016 Nov;388(10057):2272–81. doi: https://doi.org/10.1016/S0140-6736(16)31279-X
14. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007 Oct;370(9596):1453–7. doi: https://doi.org/10.1016/S0140-6736(07)61602-X
15. Van Laar D, Edwards JA, Easton S. The Work-Related Quality of Life scale for healthcare workers. J Adv Nurs. 2007 Nov;60(3):325–33. doi: https://doi.org/10.1111/j.1365-2648.2007.04409.x
16. De Simone S, Vargas M, Servillo G. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res. 2021 Apr;33(4):883–94. doi: https://doi.org/10.1007/s40520-019-01368-3
17. Coburn M, Henzler D, Baumert JH, Fimm B, Drüke B, Rossaint R. Influence of a 30-min break on divided attention and working memory in resident anaesthetists on daily routine. Br J Anaesth. 2006 Sep;97(3):315–9. doi: https://doi.org/10.1093/bja/ael151
18. Albulescu P, Macsinga I, Rusu A, Sulea C, Bodnaru A, Tulbure BT. “Give me a break!” A systematic review and meta-analysis on the efficacy of micro-breaks for increasing well-being and performance. PLoS One. 2022 Aug;17(8):e0272460. doi: https://doi.org/10.1371/journal.pone.0272460
19. O’Neill A, Baldwin D, Cortese S, Sinclair J. Impact of intrawork rest breaks on doctors’ performance and well-being: systematic review. BMJ Open. 2022 Dec;12(12):e062469. doi: https://doi.org/10.1136/bmjopen-2022-062469
20. Hobi M, Yegorova-Lee S, Chan CC, Zhao H, Jiang S, Tran D, et al. Strategies Australian junior doctors use to maintain their mental, physical and social well-being: a qualitative study. BMJ Open. 2022 Sep;12(9):e062631. doi: https://doi.org/10.1136/bmjopen-2022-062631
21. Wang H, Zheng X, Liu Y, Xu Z, Yang J. Alleviating Doctors’ Emotional Exhaustion through Sports Involvement during the COVID-19 Pandemic: The Mediating Roles of Regulatory Emotional Self-Efficacy and Perceived Stress. Int J Environ Res Public Health. 2022 Sep;19(18):11776. doi: https://doi.org/10.3390/ijerph191811776
22. Gates M, Wingert A, Featherstone R, Samuels C, Simon C, Dyson MP. Impact of fatigue and insufficient sleep on physician and patient outcomes: a systematic review. BMJ Open. 2018 Sep;8(9):e021967. doi: https://doi.org/10.1136/bmjopen-2018-021967
23. Hakro SJ, Hussain A, Aslam MS, Khan WA, Sadiq S, Asma N. A lunch break time and its impact on employees health, performance and stress on work. J Pharm Res Int. 2021;33:84–97. doi: https://doi.org/10.9734/jpri/2021/v33i38B32102
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3801.