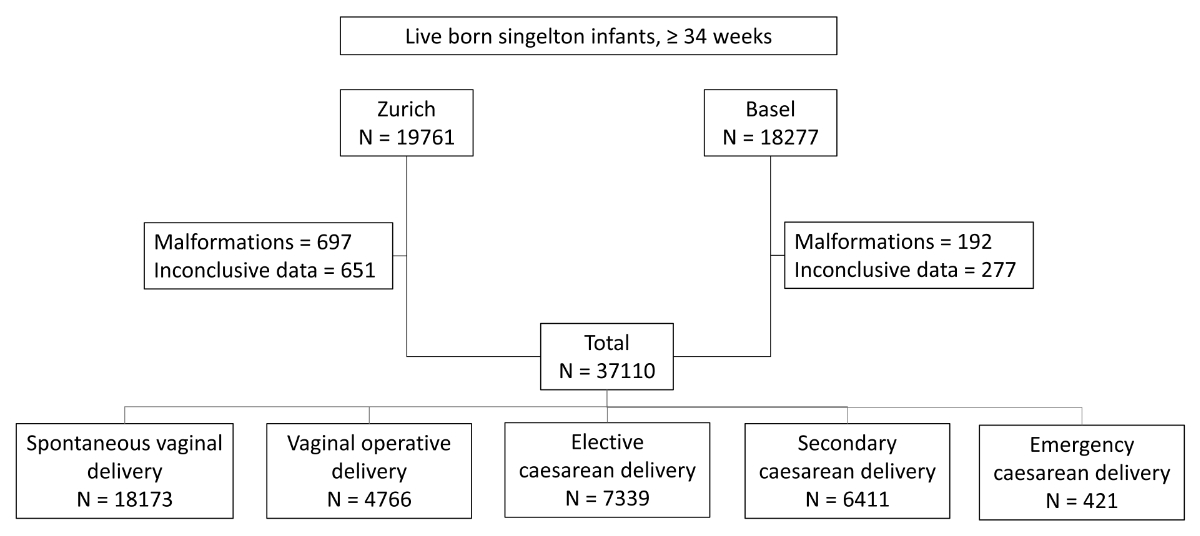
Figure 1Study selection chart.
DOI: https://doi.org/https://doi.org/10.57187/s.3798
Respiratory morbidity is a leading cause of admission to a neonatal intensive care unit in late preterm (34–36 weeks gestational age) and early term neonates (37–38 weeks gestational age), with dysfunctional resorption of lung fluid as the primary reason for admission [1, 2]. Elective caesarean delivery, without preceding labour or rupture of the membranes, is associated with an increased risk for respiratory morbidity and mortality compared to vaginal delivery [3, 4].
Recent studies have compared the incidence of respiratory distress syndrome (RDS) between caesarean deliveries before 39 weeks and caesarean deliveries after 39 weeks [5]. Previous studies have shown a detectable decrease in the incidence of respiratory morbidity in the early term period between 37 and 39 weeks using week-by-week grouped data [3, 4]. Antenatal corticosteroids administered to women experiencing preterm and early-term deliveries have been shown to lower the risk for respiratory distress syndrome [6, 7]. In addition to their effect on foetal surfactant production, antenatal corticosteroids also trigger an increase in the number and modification of lung epithelial sodium channels, which promote alveolar fluid clearance [8–10]. These positive effects are, however, in contrast to an increased risk for adverse effects, such as postnatal hypoglycaemia, alterations of the hypothalamus-pituitary-adrenal axis, arterial hypertension and neurodevelopmental impairment. Hence, antenatal corticosteroids are not recommended for women at risk for preterm delivery after 34 completed weeks of gestation [11].
The purpose of this retrospective cohort study was to evaluate the incidence of neonatal intensive care unit admissions due to respiratory morbidity – dependent on delivery mode and gestational age – and identify the point in gestation when the difference in the risk of respiratory morbidity is minimal, or absent, between infants delivered vaginally and by elective caesarean.
This retrospective cohort study was conducted at the University Hospitals of Zurich and Basel in Switzerland. Both hospitals are tertiary perinatal centres that oversee 2500 to 3000 births annually. Data from all in-house live births with at least 34 weeks of gestation between 2009 and 2016 were included in the study. Data were obtained from the clinical databases of the departments of obstetrics and neonatology from each hospital if there was no written refusal to use the data for scientific purposes. Maternal and neonatal data from infants admitted to the neonatal intensive care units were electronically matched using date of birth, sex, birth weight and surname. The consistency of all variables was checked electronically and, in part, manually. The study’s consent protocol was reviewed, and the need for written, informed consent was waived by the ethics committees of the cantons of Zurich and Northwest and Central Switzerland (BASEC-Nr.2017-00078).
Study inclusion criteria were pregnancy with delivery at or after 34 + 0 weeks of gestation as determined by sonography, foetal crown-rump length, and biparietal diameter in the first trimester. Exclusion criteria were the presence of chromosomal aberrations, major birth defects or a priori palliative care. Characteristics of the mothers and infants were collected from the medical charts. The following variables were collected from the mothers: gestational diabetes mellitus, age at delivery and gestational age at delivery. Data from the infants included umbilical artery pH, birth weight, and APGAR scores at 5 and 10 minutes of life. Gestational diabetes mellitus was diagnosed using a 75-gram oral glucose tolerance test in the second trimester. Respiratory distress syndrome was defined as persistent respiratory morbidity (intercostal retractions, grunting, nasal flaring, cyanosis, and tachypnea) requiring admission to the neonatal intensive care unit following the guidelines of the Swiss Society of Neonatology [12].
Delivery modes were grouped and defined as follows: spontaneous vaginal delivery, operative vaginal delivery, elective caesarean delivery, secondary caesarean delivery and emergency caesarean delivery. Children born vaginally in the breech position were included in the operative vaginal delivery group. Elective caesarean delivery was defined as occurring before the onset of labour or rupture of membranes. In contrast, secondary caesarean delivery was defined as occurring after the onset of labour or the rupture of membranes. Emergency caesarean delivery was defined as occurring under general anaesthesia in cases of imminent, life-threatening foetal or maternal conditions, such as foetal bradycardia or placental abruption.
Demographic data were analysed using descriptive statistics, with the median (minimum-maximum) for non-parametric variables and the mean ± standard deviation for parametric variables. The incidence of respiratory distress syndrome according to gestational age (with weekly intervals) was calculated for each delivery mode. Odds ratios (ORs) for respiratory distress syndrome incidence were calculated and adjusted for gestational age with weekly intervals. Multiple logistic regression was used to test for known influencing factors (other than gestational age) on respiratory distress syndrome incidence, such as birth acidosis (defined as umbilical artery pH <7.15), 5-minute APGAR <7, gestational diabetes mellitus, and small for gestational age (birth weight <5th percentile). These risk factors were part of the clinical record and available for all included pregnancies. A separate analysis was conducted for respiratory distress syndrome incidence in spontaneous vaginal and elective caesarean deliveries according to gestational age with daily intervals. Pregnancies associated with gestational diabetes mellitus, birth acidosis, small for gestational age or 5-minute APGAR <7 were excluded from this analysis. Based on the daily respiratory distress syndrome incidences, a polynomial regression model was used to describe the relationship between incidence and gestational age at daily intervals.
Statistical analyses were performed using Stata 15.1 software (StataCorp, College Station, Texas, USA).
The study was approved by the ethics committees of the Zurich Canton and Northwest and Central Switzerland (BASEC-Nr.2017–00078). The study was considered to reuse biological material and/or health-related personal data. Hence, further use without prior consent is allowed if there is no documented refusal (Federal Act on Research involving Human Beings Art. 34, Art. 37–40, The Federal Assembly of the Swiss Confederation).
During the study period from 2009 to 2016, 38,382 infants with a gestational age of at least 34 weeks at birth were identified. After excluding records with incomplete data (n = 383) and infants with major birth defects (n = 889), a total of 37,110 infants were included for analysis (figure 1). Of these, 1,980 (5.34%) were admitted to a neonatal intensive care unit due to respiratory distress syndrome. Over the entire study period, the incidence of respiratory distress syndrome decreased from 7.3% (296/4162) in 2009 to 4.4% (230/5107) in 2016 (figure 2).
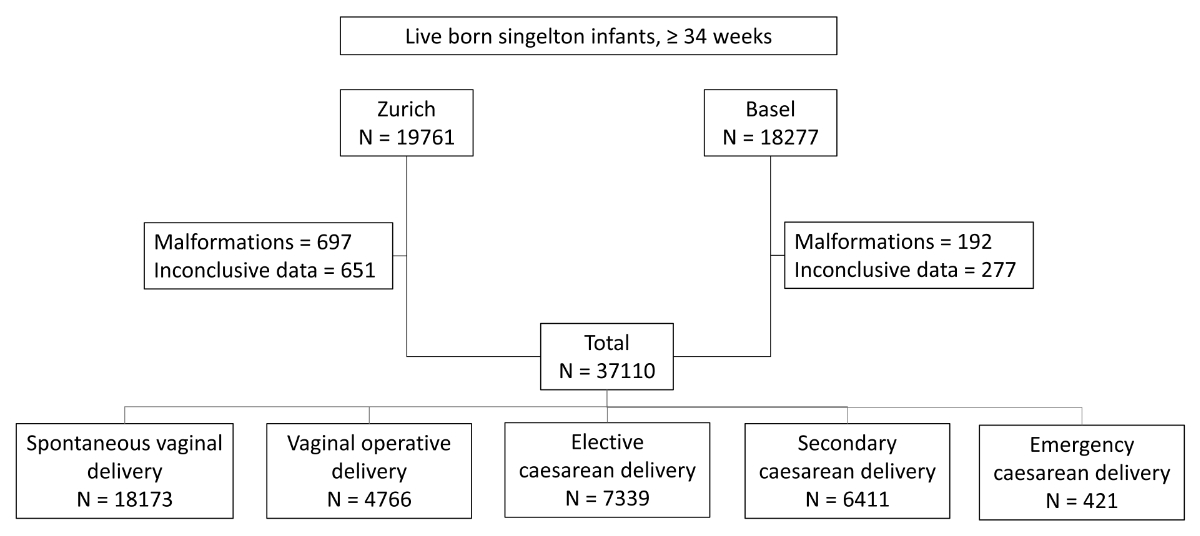
Figure 1Study selection chart.
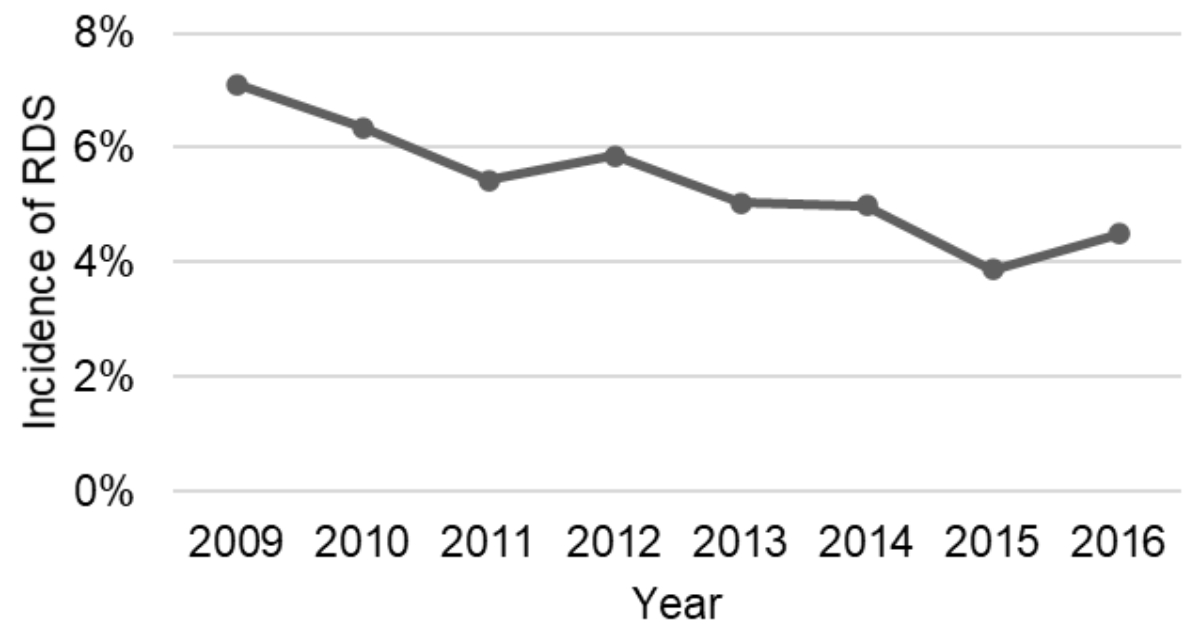
Figure 2Annual incidence of respiratory distress syndrome (RDS) among all deliveries.
Maternal demographics and neonatal characteristics are presented in table 1.
Table 1Maternal and neonatal characteristics. APGAR values are shown as medians (minimum-maximum). All other variables are mean values and standard deviations (SDs).
| Maternal characteristics | Parity | 1.7 ± 0.89 |
| Maternal age (years) | 32.1 ± 5.3 | |
| Neonatal characteristics | Gestational age (days at birth) | 274 ± 11.6 |
| Birth weight (g) | 3288.8 ± 544.9 | |
| Birth weight percentile | 50 ± 32.6 | |
| 5-minute APGAR | 9 (1–10) |
The distribution of all five delivery modes in the total study population was as follows: spontaneous vaginal delivery 49% (n = 18173), operative vaginal delivery 12.8% (n = 4766), elective caesarean 19.8% (n = 7339), secondary caesarean 17.3% (n = 6411) and emergency caesarean 1.1% (n = 421).
The incidence of respiratory distress syndrome was highest in infants born at 34 weeks gestational age and steadily decreased up to 39 weeks, with a slight increase in later weeks of gestational age (figure 3). Infants born via spontaneous vaginal delivery had the lowest incidence of respiratory distress syndrome (2.92%) versus 13.3% for emergency caesarean and 8.98% for elective caesarean. A breakdown of respiratory distress syndrome incidence per week of gestational age according to the five different modes of delivery, found that incidence was lowest at 39 completed weeks of gestational age regardless of delivery mode (figure 3). Gestational age at the time of elective caesarean delivery remained unchanged (38.3 ± 1.38 weeks) throughout the entire study period.
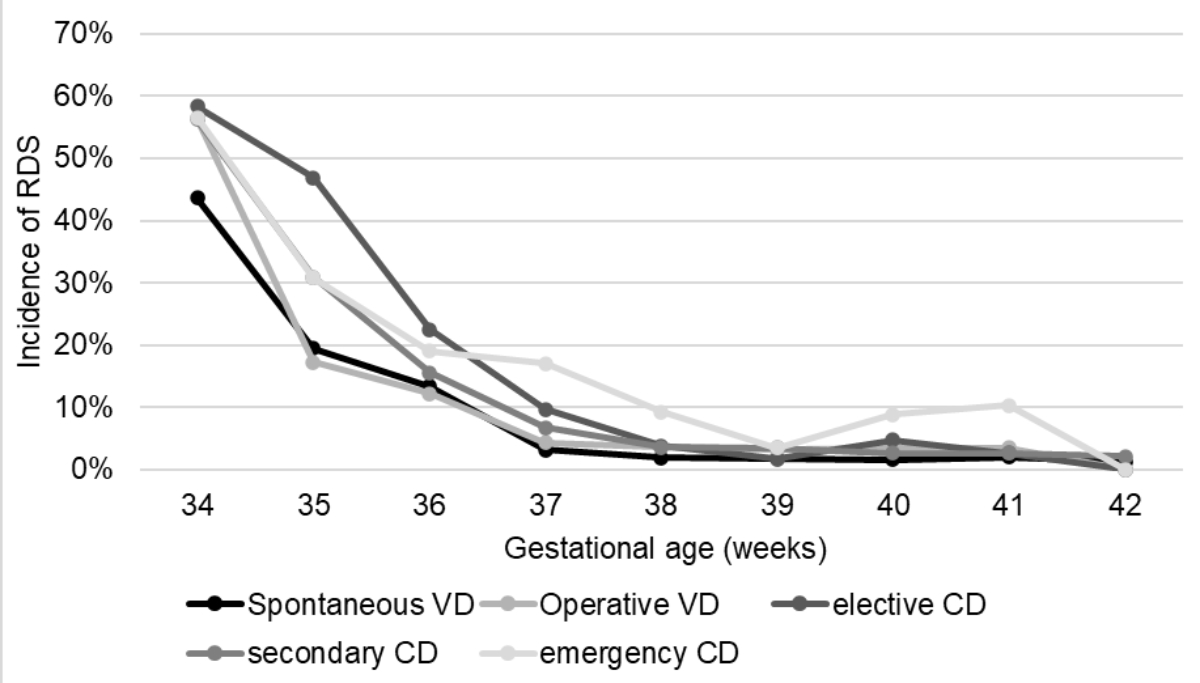
Figure 3Incidence of respiratory distress syndrome (RDS) in relation to all delivery modes per week of gestation. VD: vaginal delivery; CD: caesarean delivery.
Multivariate analysis showed that the OR of respiratory distress syndrome was highest for elective and emergency caesarean deliveries and significantly increased for all delivery modes when compared to spontaneous vaginal delivery (table 2). However, emergency caesarean deliveries were omitted from this calculation due to low numbers. An analysis of possible confounding factors showed a higher risk for all tested variables (table 3).
Table 2Unadjusted odds ratio and (95% confidence intervals) for respiratory distress syndrome depending on delivery mode and gestational age (in completed weeks), excluding deliveries with gestational diabetes, birth acidosis, 5-minute APGAR below 7 and small for gestational age.
| Gestational age (weeks) | |||||||
| 34 | 35 | 36 | 37 | 38 | 39 | 40 | |
| Spontaneous vaginal delivery* | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Operative vaginal delivery | 1.7 (0.71–4.07) | 1.22 (0.43–3.45) | 0.9 (0.42–1.93) | 1.94 (0.84–4.5) | 1.56 (0.71–3.43) | 1.05 (0.32–1.93) | 1.56 (1.05–2.31) |
| Elective caesarean delivery | 2.31 (1.49–3.56) | 5.61 (3.39–9.3) | 1.5 (0.95–2.38) | 3.28 (1.95–5.54) | 2.51 (1.65–3.81) | 0.51 (0.24–1.07) | 2.84 (1.68–4.82) |
| Secondary caesarean delivery | 1.61 (1.1–2.35) | 2.45 (1.52–3.94) | 0.96 (0.6–1.54) | 2 (1.05–3.81) | 1.84 (0.99–3.4) | 1.75 (1.06–2.9) | 1.83 (1.29–2.61) |
*Spontaneous vaginal delivery is the baseline category.
Table 3Effects of gestational age, delivery mode, 5-minute APGAR, gestational diabetes, umbilical artery pH and small for gestational age on the incidence of respiratory distress syndrome in a multivariate logistic regression model (odds ratios [ORs] with 95% confidence intervals [CIs]).
| OR (95% CI) | ||
| Gestational age [weeks] | ≥40* | 1 |
| 39 | 0.93 (0.77–1.12) | |
| 38 | 1.13 (0.95–1.36) | |
| 37 | 2.42 (2.00–2.92) | |
| 36 | 6.97 (5.76–8.42) | |
| 35 | 15.59 (12.95–18.77) | |
| 34 | 42.07 (35.03–50.53) | |
| Delivery mode | Spontaneous vaginal delivery* | 1 |
| Operative vaginal delivery | 1.30 (1.08–1.56) | |
| Elective caesarean delivery | 2.20 (1.91–2.53) | |
| Secondary caesarean delivery | 1.61 (1.40–1.86) | |
| Emergency caesarean delivery | 1.82 (1.28–2.61) | |
| 5-minute APGAR | ≥7* | 1 |
| <7 | 5.25 (4.32–6.39) | |
| Gestational diabetes | No* | 1 |
| Yes | 1.40 (1.17–1.69) | |
| Umbilical artery pH | ≥7.15* | 1 |
| <7.15 | 3.24 (2.68–3.93) | |
| Small for gestational age | No* | 1 |
| Yes | 1.38 (1.19–1.60) | |
* baseline category
In a sub-group analysis that excluded potential risk factors for respiratory distress syndrome (gestational diabetes, birth acidosis, 5-minute APGAR below 7, and small for gestational age), gestational age was stratified into days, and spontaneous vaginal delivery versus elective caesarean delivery was compared. As shown in figure 4, the frequency of respiratory distress syndrome was consistently higher in infants delivered by elective caesarean up until 270 days (38 weeks + 4 days). After 270 days, no significant difference between the two delivery modes was found.
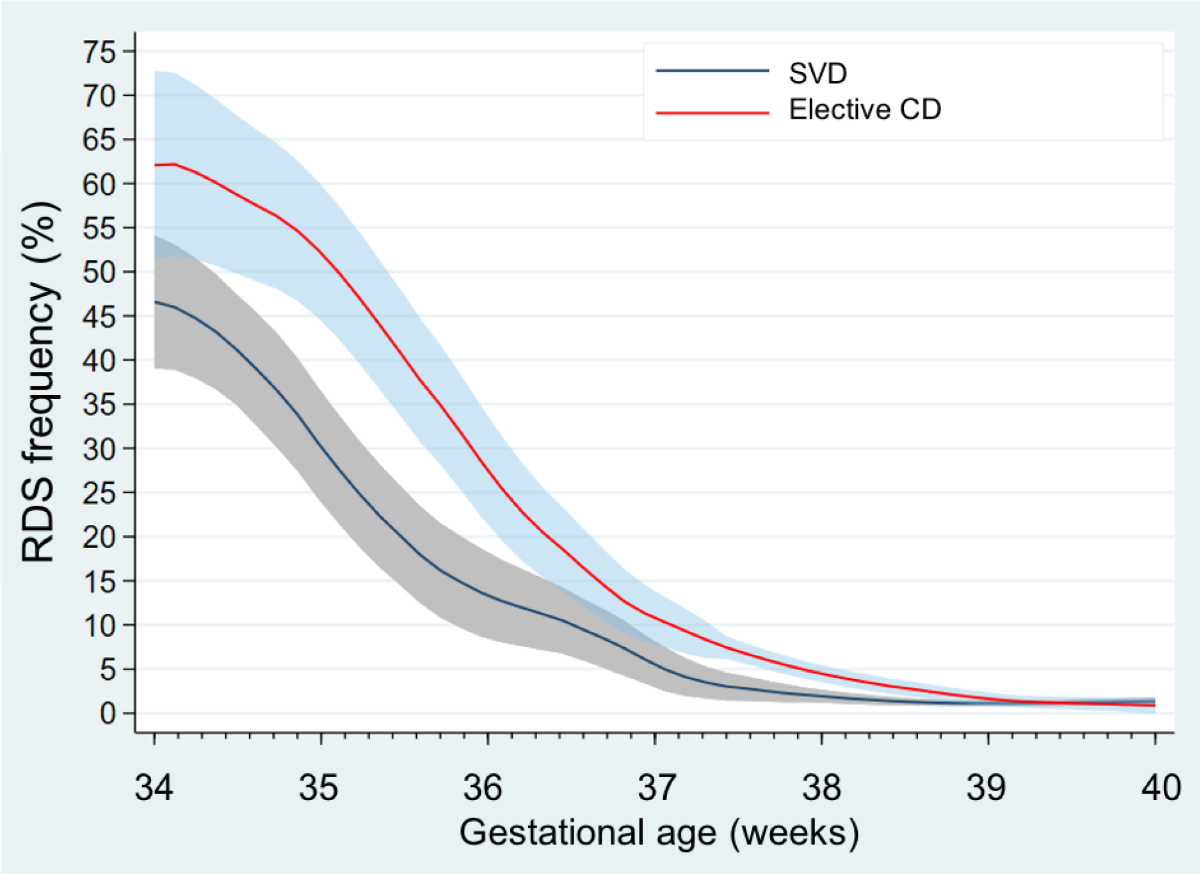
Figure 4Frequency of respiratory distress syndrome (RDS) according to spontaneous vaginal delivery and elective caesarean delivery by week of gestation. A polynomial regression model with a 95% confidence interval based on the RDS frequency was calculated for each day of gestational age. Only pregnancies respective infants without gestational diabetes, small for gestational age, birth acidosis or 5-minute APGAR <7 were considered. SVD: spontaneous vaginal delivery; CD: caesarean delivery. Line: smoothed polynomial of RDS frequency; area: 95% confidence interval.
Respiratory morbidity is a leading cause of neonatal intensive care unit admissions for infants born at 34 or more weeks of gestation [2]. Caesarean sections are a risk factor for respiratory distress syndrome in late preterm and term infants, which has been confirmed in numerous studies [3, 4, 13, 14]. Antenatal corticosteroids are effective in reducing this risk, but they are not recommended for use in most guidelines world-wide due to concerns about potential side effects [11]. To determine the rate of respiratory distress syndrome in late preterm and term-born infants according to the delivery mode in Switzerland, we conducted a retrospective cohort study investigating the incidence of respiratory distress syndrome requiring admission to a neonatal intensive care unit in all live-born infants with at least 34 weeks of gestation delivered at two academic hospitals in Switzerland between 2009 and 2016.
Our study had several key findings. Firstly, the incidence of respiratory distress syndrome was significantly higher in infants delivered by elective caesarean compared to spontaneous vaginal delivery up to 38 + 4 weeks of gestational age. Secondly, the absolute incidence of respiratory distress syndrome decreased over the study period from 7.3% in 2009 to 4.4% in 2016, whereas the time point of elective caesarean delivery remained stable at 39.3 ± 1.65 weeks of gestation. Thirdly, perinatal risk factors, including a 5-minute APGAR score below 7, birth acidosis, gestational diabetes mellitus and small for gestational age, were independent risk factors for respiratory distress syndrome in this population.
The data presented here provide evidence that elective caesarean delivery should be performed after 38 + 4 weeks of gestation whenever clinically possible to minimise the risk of respiratory distress syndrome and subsequent admission to a neonatal intensive care unit. Our study provides data for a day-specific calculation of the risk of respiratory distress syndrome, while previous studies have only reported data for completed weeks [3, 4]. Our results are in line with a previous report from Switzerland investigating the incidence of respiratory distress syndrome from 1982 to 2004 [3], and we confirm the findings of at least a 2-fold higher risk for respiratory distress syndrome following an elective caesarean versus spontaneous vaginal delivery under 39 weeks of gestation (and no significant difference in week 39). Thus, despite a reduction in the incidence of respiratory distress syndrome in general, which might be due to improved resuscitation management [10], the increased risk ratio for infants delivered by elective caesarean compared to vaginal delivery has remained stable over the past 20 years. It can be speculated that improved neonatal care has contributed to a general reduction in the incidence of respiratory distress syndrome. However, other clinical care parameters require adjustment to narrow the risk ratio between elective caesareans and vaginal delivery; for example, the introduction of antenatal corticosteroids in women at high risk for preterm delivery before 37 weeks of gestation.
Our study has several limitations. First, there may be missing and/or unreliable data due to the retrospective design. Second, taking into consideration known confounder variables does not exclude the possibility that other unavailable or unknown factors may have significantly influenced the incidence of respiratory distress syndrome. Third, despite the clear definition of respiratory distress syndrome by the Swiss Society of Neonatology, a diagnosis is never independent of the neonatologist’s subjective assessment. Finally, both study centres are tertiary-care facilities in an urban area with a high proportion of risky pregnancies. Thus, it is not possible to draw conclusions from the study population to the country as a whole. Our study also has several strengths. Specifically, we had a large sample size, both study centres were equipped with electronic databases and both used the same national guidelines to diagnose neonatal respiratory morbidity. Finally, we tested the association of neonatal respiratory morbidity with potential known confounders in a multivariate logistic regression model.
In conclusion, the results of this study can be used to plan the most advantageous moment to perform an elective caesarean delivery and could contribute to reducing respiratory morbidity in neonates. In everyday clinical life the prolongation of pregnancy behind 38 weeks is not always possible for various reasons. Furthermore, we have generated a basis for studies in Switzerland and beyond that address respiratory outcomes after elective caesarean deliveries and promote discussions concerning administering antenatal corticosteroids in the late preterm and early term gestation period.
The data supporting this study’s findings are not publicly available due to institutional data protection regulations but are available from the corresponding author [TB].
Author contributions: Idea and Concept: Tilo Burkhardt, Sven Wellmann. Acquisition of data: Mark Adams, Gwendolin Manegold-Brauer. Analysis of data: Julia Gromann, Isabella Mancino. Manuscript writing: Julia Gromann, Isabella Mancino. Final corrections and improvements: Tilo Burkhardt, Sven Wellmann.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Sven Wellmann is the co-founder and chief medical officer of the academic spinoff NeoPrediX from the University of Basel, Switzerland. Tilo Burkhardt and Sven Wellman hold a research grant from the Family Larsson-Rosenquist Foundation (Rheinstrasse 1, 8500 Frauenfeld, Switzerland) to conduct a clinical intervention study. No other potential conflict of interest related to the content of this manuscript was disclosed.
1. Jain L. Stress at Birth and Its Inextricable Link to the Neonatal Transition. Obstet Gynecol. 2016 Oct;128(4):685–7. 10.1097/AOG.0000000000001657
2. Yang X, Meng T. Admission of full-term infants to the neonatal intensive care unit: a 9.5-year review in a tertiary teaching hospital. J Matern Fetal Neonatal Med. 2020 Sep;33(17):3003–9. 10.1080/14767058.2019.1566901
3. De Luca R, Boulvain M, Irion O, Berner M, Pfister RE. Incidence of early neonatal mortality and morbidity after late-preterm and term cesarean delivery. Pediatrics. 2009 Jun;123(6):e1064–71. 10.1542/peds.2008-2407
4. Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ. 2008 Jan;336(7635):85–7. 10.1136/bmj.39405.539282.BE
5. Pirjani R, Afrakhteh M, Sepidarkish M, Nariman S, Shirazi M, Moini A, et al. 'Elective caesarean section at 38-39 weeks gestation compared to > 39 weeks on neonatal outcomes: a prospective cohort study. BMC Pregnancy Childbirth. 2018 May;18(1):140. 10.1186/s12884-018-1785-2
6. Saccone G, Berghella V. Antenatal corticosteroids for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ. 2016 Oct;355:i5044. 10.1136/bmj.i5044
7. Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita AT, Reddy UM, Saade GR, et al.; NICHD Maternal–Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016 Apr;374(14):1311–20. 10.1056/NEJMoa1516783
8. Jain L, Eaton DC. Physiology of fetal lung fluid clearance and the effect of labor. Semin Perinatol. 2006 Feb;30(1):34–43. 10.1053/j.semperi.2006.01.006
9. Riley CA, Boozer K, King TL. Antenatal corticosteroids at the beginning of the 21st century. J Midwifery Womens Health. 2011;56(6):591–7. 10.1111/j.1542-2011.2011.00119.x
10. Wellmann S, Manegold-Brauer G, Fischer T, Schäffer L, Gaertner VD, Malfertheiner SF, et al. Improving Neonatal and Maternal Outcome by Inducing Mild Labor before Elective Cesarean Section: The Lacarus Randomized Controlled Trial. Neonatology. 2021;118(1):116–21. 10.1159/000512752
11. Dagklis T, Şen C, Tsakiridis I, Villalaín C, Allegaert K, Wellmann S, et al. The use of antenatal corticosteroids for fetal maturation: clinical practice guideline by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine foundation. J Perinat Med. 2022 Mar;50(4):375–85. 10.1515/jpm-2022-0066
12. Pfister R. Die Unterstützung der Adaptation und Reanimation des Neugeborenen. Paediatrica. 2017;28(5):9–22.
13. Sengupta S, Carrion V, Shelton J, Wynn RJ, Ryan RM, Singhal K, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr. 2013 Nov;167(11):1053–9. 10.1001/jamapediatrics.2013.2581
14. Jones MD Jr, Burd LI, Bowes WA Jr, Battaglia FC, Lubchenco LO. Failure of association of premature rupture of membranes with respiratory-distress syndrome. N Engl J Med. 1975 Jun;292(24):1253–7. 10.1056/NEJM197506122922401