Figure 1The clinical practice guideline that was implemented at University Children’s Hospital Zurich in February 2021 [31].
DOI: https://doi.org/https://doi.org/10.57187/s.3781
Fractures are a common reason for paediatric emergency department visits, with annual incidence rates of paediatric fractures ranging from 12 to 36 per 1000 children [1, 2]. In infants, the annual incidence of fractures is notably lower, ranging from 0.7 to 3.6 per 1000 children [3–5], yet distinguishing between accidental and non-accidental injuries in this vulnerable population remains a crucial concern. Conversely, the proportion of fractures attributed to abuse is higher in younger children, with estimates ranging from 25% to 56% in hospitalised children younger than 12 months [5, 6], and 1% to 36% in a general emergency department population of infants [4, 7–9]. Estimations of abuse-related fractures in younger children, particularly infants, have been challenging due to the difficulty in substantiating cases conclusively, compounded by variations in study inclusion criteria and abuse definitions.
To differentiate between accidental and non-accidental injuries, physicians must consider various factors, including the injury’s history, the child’s age and developmental stage, fracture localisation, the fracture’s age and understanding the mechanism responsible for the specific localisation of the fracture [10]. Indicators suggestive of potential child abuse include multiple fractures, fractures at different healing stages, delays in seeking medical treatment and co-existing injuries such as skin injuries, internal organ damage or central nervous system trauma [10]. An injury’s history must also be compatible with a fracture in terms of biomechanics [11]. Previous research has demonstrated that individuals trained in child protection possess a higher accuracy in assessing suspected cases of child abuse [12, 13].
The American Academy of Pediatrics (AAP) recommends a standardised assessment protocol for infants with fractures, which includes a mandatory skeletal survey for all infants with a fracture, with a few exceptions such as distal radial/ulna buckle fractures, toddler fractures of the tibia or fibula in a cruising child with a history of a fall, linear unilateral skull fractures in children over six months old with a history of a significant fall and clavicle fractures attributable to birth [14]. However, in Switzerland, no guidelines exist for evaluating child abuse in infants with fractures. A recent Swiss study investigated obstacles and enablers for detecting and reporting child abuse among nursing and medical staff in paediatric emergency and surgery departments. Implementation of a clearly defined clinical practice guideline was one of the most frequently reported enablers (23%), along with mandatory child protection courses, encouragement of low thresholds to express and report suspicions and improvement of child protection service resources [15].
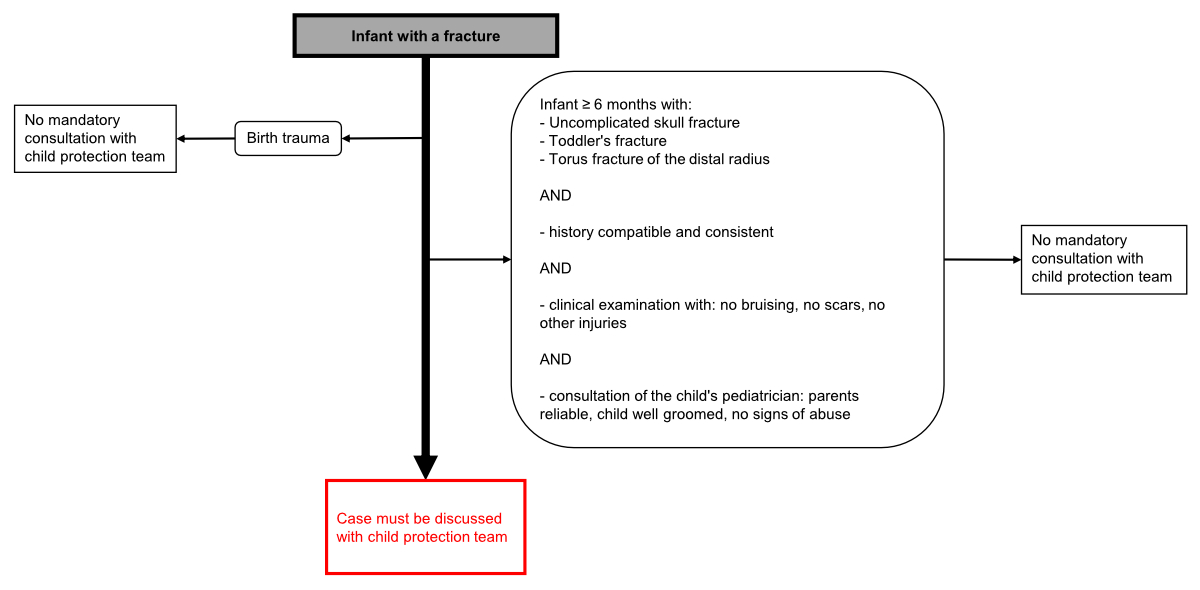
In 2021, University Children’s Hospital Zurich instituted a clinical practice guideline aimed at standardising the management of infants with fractures (figure 1). The guideline requires that a detailed medical history and clinical examination must be conducted for infants with a fracture. The attending physician in the emergency department or inpatient ward must also contact the paediatrician or family doctor to record any abnormalities in the child’s previous medical history. Depending on the age and location of the fracture, the hospital’s internal child protection team must also be involved.
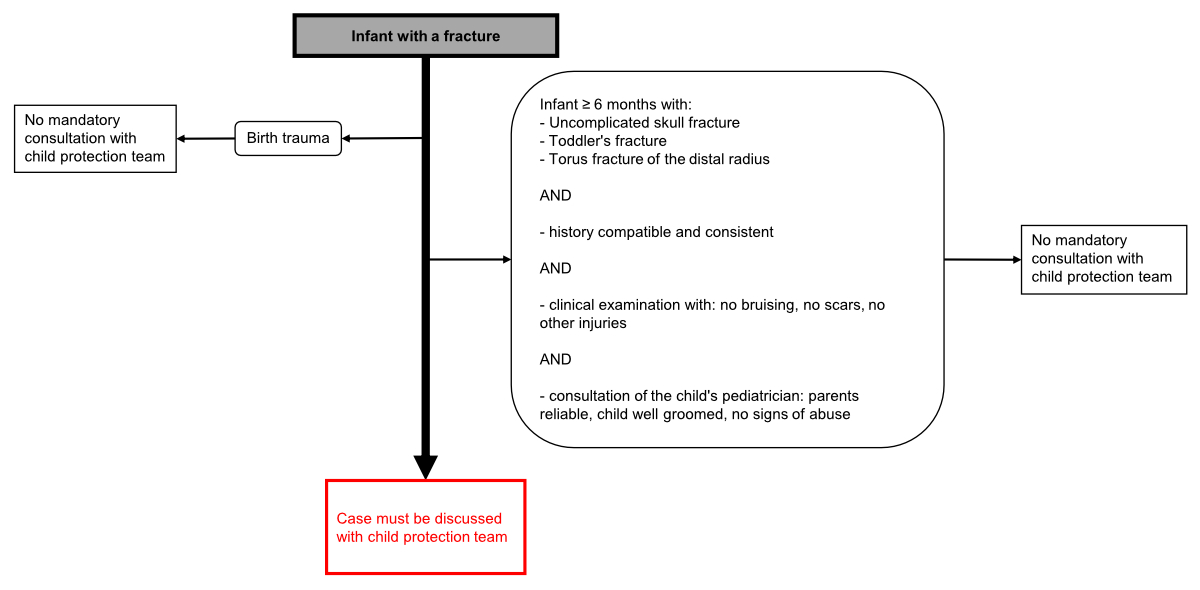
Figure 1The clinical practice guideline that was implemented at University Children’s Hospital Zurich in February 2021 [31].
This guideline is based on the AAP guideline, with the exception that a skeletal survey is not mandatory. Instead, the decision regarding a skeletal survey is made in conjunction with the child protection team, providing an opportunity to increase abuse detection rates while minimising radiation exposure. It is important to emphasise that a skeletal survey is only one component of evaluating a child with fractures, and a normal skeletal survey does not definitively rule out child abuse. Abused children may have only a single fracture [10] and occult fractures may be missed even if the skeletal survey is performed correctly [16].
This study aims to evaluate adherence to the implemented guideline and compare the frequency of child protection team involvement, skeletal survey rate and child abuse detection rate with the period before the guideline was implemented. These findings substantially support our long-term goal to establish a national guideline for the evaluation of child abuse in infants with fractures.
This retrospective single-centre quality control study included infants diagnosed with fractures at the emergency department of University Children’s Hospital Zurich between 1 February 2021 and 31 August 2022. This timeframe was chosen to ensure an adequate duration for physicians at our hospital to become familiar with this guideline and integrate it into daily practice at the emergency department and on the ward. Exclusions comprised infants with prior diagnoses of bone diseases, such as osteogenesis imperfecta or those whose parents declined the use of their children’s data for research. Data collection relied on the hospital’s clinical information system (CGM clinical). All X-ray images from the emergency department are stored in a picture archiving and communication system (PACS) for evaluation by paediatric radiologists. All infants with fractures in the PACS were eligible for this control study. Additionally, all infant visits to the emergency department due to trauma were screened daily by two authors (LR, MS) to ensure no cases were missed.
Collected patient characteristics included age, sex, fracture localisation, and whether patients received inpatient or outpatient care. In accordance with our hospital’s guidelines, fracture diagnosis predominantly involved radiographs, except for toddler’s fractures and skull fractures. A clinical diagnosis was permissible for these specific cases based on a clear history of trauma and corresponding clinical findings, such as swelling and refusal to walk (in cases of leg injuries) or swelling combined with a palpable fracture or bony step-off (for skull fractures). It was left at the discretion of the attending physician to determine whether additional imaging, such as sonography or computed tomography (CT), was necessary. While the specificity and sensitivity of a clinical diagnosis of skull fractures are lower compared to those of a CT diagnosis [17–19], the clinical focus is not solely on identifying every skull fracture but rather on performing CT scans or MRI only on children suspected of relevant intracranial bleeding. This approach aligns with current standard practice at University Children’s Hospital Zurich, which we did not change for the purpose of this study. In cases of toddler’s fractures, initial radiographs often yield negative results, so the primary diagnosis is typically based on history and physical examination [20]. A fracture was classified as birth-associated if the child presented in the first month of life, the caregiver’s history aligned with the birth reports, and if there were no other suspicious findings in the child’s personal history and clinical examination.
The primary outcome was to assess adherence rates to the guideline. This was accomplished by reviewing individual medical reports from the emergency department and, if applicable, the inpatient ward. The reports were reviewed regarding personal history, clinical examination details, fracture localisation, documentation of consultation with the paediatrician or family doctor, and involvement of the child protection team. If these actions were not documented, they were classified as not having occurred. Based on this information, we compared the management with the guideline’s flowchart to determine whether the patient’s medical team had adhered to the guideline or not. We also identified specific steps within the guideline that were omitted by clinicians. The adherence rates were compared between infants under and over six months and between inpatient and outpatient care, as our guideline requests different steps based on age and fracture localisation.
Secondary outcomes were the frequency of child protection team involvement, the rate of skeletal surveys and the rate of detection of potential child abuse. These three values were then compared with the corresponding values before implementation of the guideline.
Data were initially recorded in Microsoft Excel (Microsoft Corp, Redmond, Wash) and subsequently imported into R statistical software (R Studio Version 2022.07.1+554) for analysis. The statistical analyses were conducted at visit level, as each visit by a child to the emergency department should be assessed separately, especially if they present more than once. The statistical findings were described using frequencies and percentages for categorical data, whereas continuous variables were presented as medians and ranges.
This study was performed in accordance with the principles of the Declaration of Helsinki. The Ethics Committee of Zurich (2020-02762) granted a waiver of consent as this project was classified as quality control.
Over a 19-month period, 87 infants presented with fractures out of 9523 infant visits (0.9%) to our emergency department. Ten visits (of 2 different children) were excluded because of a prior diagnosis of osteogenesis imperfecta, and 16 visits (of 16 different children) were excluded because of parental non-consent to use their children’s data for research. Thus, 61 visits were included in this study (figure 2). Each included visit refers to a single child; none of the included children presented multiple times to the emergency department, and none of them had multiple fractures.
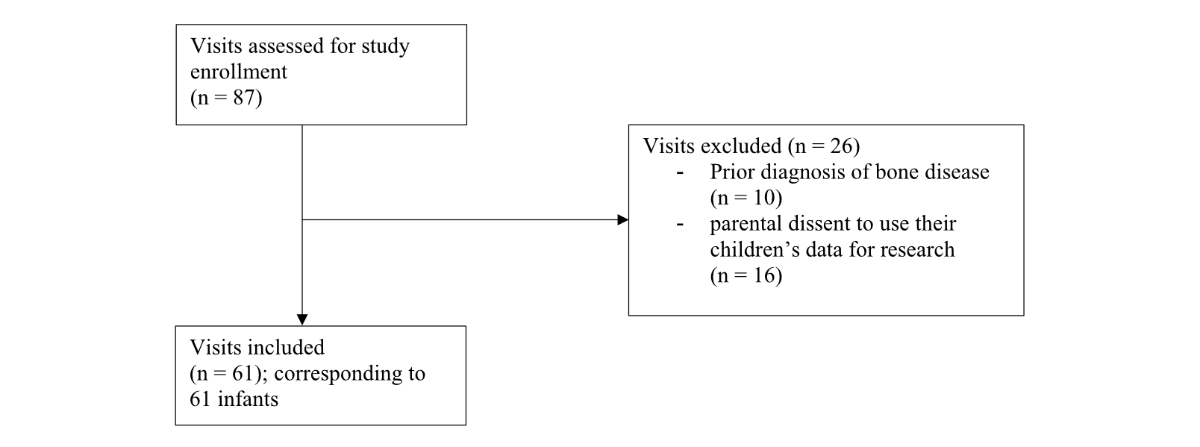
Figure 2Patient selection chart.
The patient cohort consisted of 46% females (n = 28) and 54% males (n = 33) with a median age of seven months. The age distribution revealed a predominant age group between 6 and 12 months, with a peak at 11 months (figure 3). Nineteen children were younger than six months (31%) and 42 patients were older than six months (69%). Patient characteristics, including age distribution, fracture localisation and patient care (inpatient versus outpatient) are presented in table 1. Thirty-one patients (51%) received outpatient care and 30 patients were treated as inpatients (49%). Notably, 84% (n = 26) of the outpatients were older than six months, vs 53% (n = 16) of the inpatients. Younger children, those under six months of age, were primarily treated as inpatients (74%, n = 14), whereas among those older than six months, only a minority were admitted to the ward (38%, n = 16). Among inpatients, 87% (n = 26) of all fractures were skull fractures, followed by femur fractures (7%, n = 2). The most common fractures in outpatients were lower leg fractures (32%, n = 10), skull fractures (23%, n = 7) and forearm and clavicle fractures (13%, n = 4). Three fractures (5%), including two skull fractures and one upper-arm fracture, were classified as birth traumas.
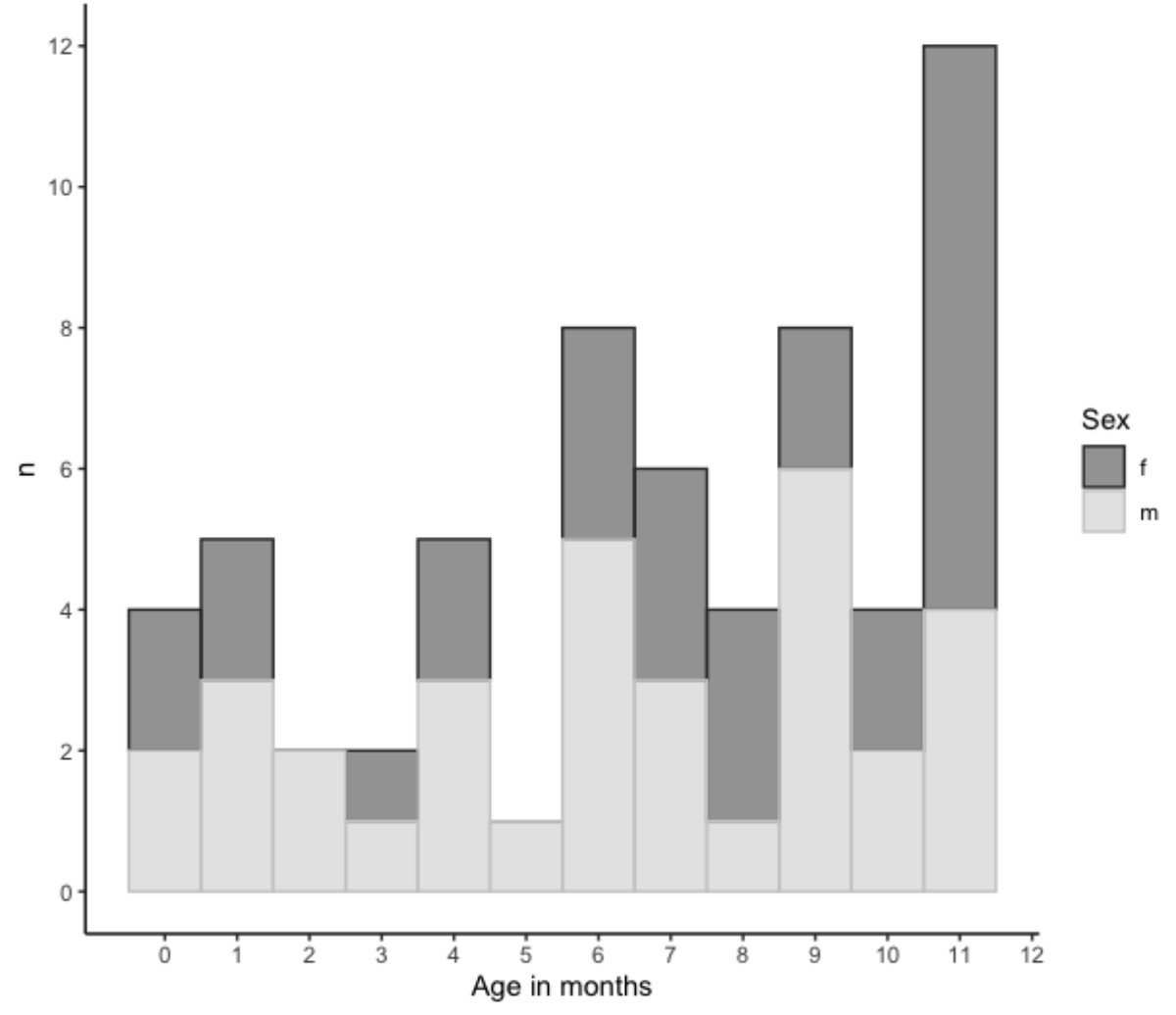
Figure 3The distribution of age and sex of the patients included.
Table 1Patient characteristics. Fracture localisation and range of age of the 61 infants included in the study.
| n (%) (n = 61) | Age, median (range) in months | Inpatient care | ||
| Skull | 33 (54%) | 6 | (0–11) | 26/33 (79%) |
| Lower leg | 10 (16%) | 9 | (7–11) | 0/10 |
| Femur | 5 (8%) | 7 | (0–8) | 2/5 (40%) |
| Clavicle | 4 (7%) | 6 | (4–9) | 0/4 |
| Forearm | 4 (7%) | 10.5 | (9–11) | 0/4 |
| Humerus | 4 (7%) | 4.5 | (0–9) | 1/4 (25%) |
Guideline adherence was observed in 39% (n = 24) of cases, with non-adherence occurring in 61% (n = 37). The reasons for non-adherence varied: in 68% (n = 25) of cases, the paediatrician or family doctor was not consulted, while in 32% (n = 12), the child protection team was not consulted despite being requested. Adherence rates were similar in children aged under vs over six months, with adherence rates of 42% (n = 8) and 38% (n = 16), respectively. Among infants younger than six months, the primary reason for non-adherence was missing child protection team involvement in 64% (n = 7) of cases, whereas in children older than six months, non-adherence was primarily due to the absence of consultation with the paediatrician or family doctor in 81% (n = 21).
Figure 4 illustrates adherence to the guideline, highlighting that outpatient care was associated with a lower rate of adherence (26%, n = 8) compared to inpatient care (53%, n = 16). Among outpatient cases, 83% (n = 19) of non-adherent cases were attributed to the absence of a consultation with the paediatrician or family doctor, while 17% (n = 4) were due to missing child protection team involvement. In contrast, in inpatient care, 43% (n = 6) of non-adherent cases were linked to a missing consultation with the paediatrician or family doctor, while 57% (n = 8) were attributed to missing child protection team involvement.
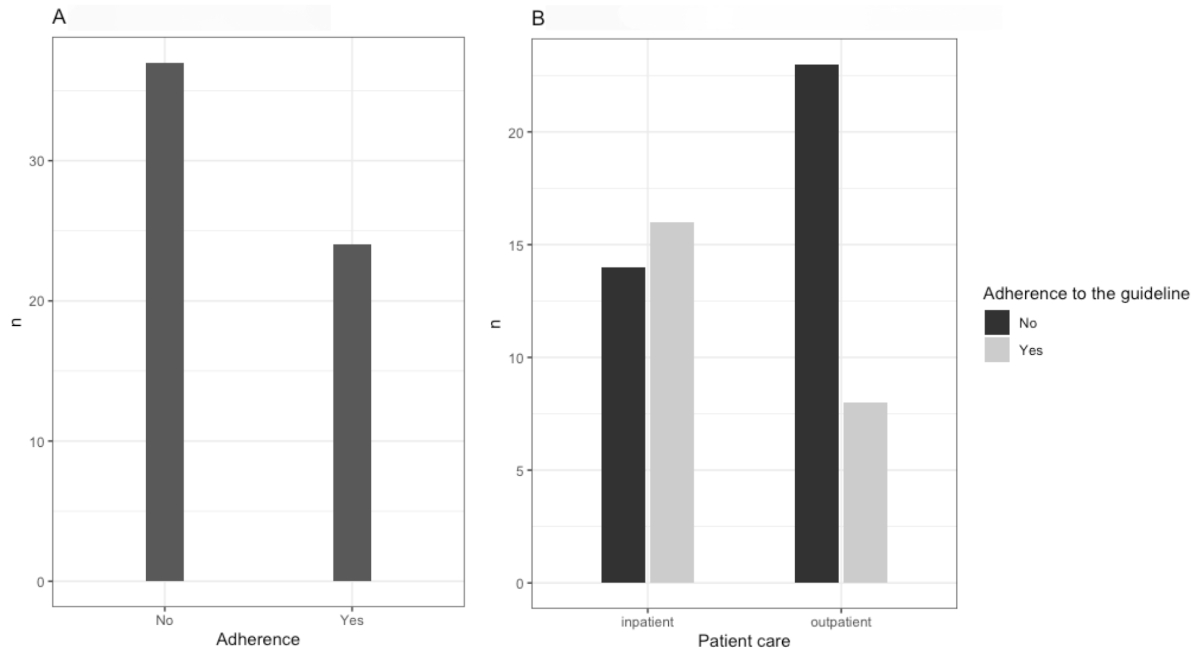
Figure 4(A) Overall adherence and non-adherence. (B) Number of cases of adherence and non-adherence, illustrated per group of patient care (inpatient vs outpatient).
Child protection team involvement occurred in 54% cases (n = 33), resulting in further diagnostics in 15% (n = 5) of those cases. Characteristics of patients for whom the child protection team ordered further diagnostics are detailed in table 2. Overall, the skeletal survey rate was 8% (n = 5). While one skeletal survey was ordered by the attending physician on the ward due to suspicion of bone disease, the remaining four were ordered by the child protection team. One case (1/61, 1.6%) aroused high suspicions of child abuse due to the identification of an old rib fracture, leading to a report to the child and adult protection authority. In the skeletal survey ordered by the attending physician on the ward, a clavicle fracture was found and later the diagnosis of osteogenesis imperfecta was established.
Table 2Patients with further diagnostics ordered by the child protection team.
| Case No | Age (months) | Fracture localisation | Adequate history for trauma | Further diagnostics ordered by child protection team | New findings through further diagnostics |
| 1 | 6 | Skull | no | Skeletal survey | no |
| 2 | 9 | Humerus | no | Skeletal survey; urine (bone metabolism), fundoscopy | no |
| 3 | 7 | Skull | no | Skeletal survey; basic coagulation tests | no |
| 4 | 2 | Femur | no | Skeletal survey; urine (bone metabolism); fundoscopy | Old rib fracture |
| 5 | 11 | Skull | no | Fundoscopy | no |
Our study evaluated adherence to the 2021 guideline for infants with fractures, revealing an overall low adherence rate. However, the child protection team involvement rate doubled post-implementation, indicating an improvement in child abuse assessment. Our findings indicate a low overall adherence rate of only 39%, with non-adherence primarily attributed to the absence of paediatrician or family doctor consultation (68%), followed by child protection team omission (32%). Additionally, outpatient care had a lower adherence rate compared to inpatient care.
Differences in guideline adherence were observed between children aged under and over six months. While the overall guideline adherence did not differ between these age groups, the underlying reasons for non-adherence were distinct. Among infants under six months, the primary factor contributing to non-adherence was the absence of child protection team involvement. Conversely, in children older than six months, non-adherence predominantly stemmed from missing consultations with the paediatrician or family doctor.
We also found differences in guideline adherence between inpatient and outpatient management, notably with insufficient adherence in outpatient care, where 74% of children were not managed according to the guideline. Most outpatient cases involved children older than six months (84%), with prevalent fractures including lower leg, skull and forearm fractures. In the outpatient group, guideline non-adherence primarily stemmed from a lack of consultation with the paediatrician or family doctor. Previous studies have shown that there are differences in child abuse guideline adherence depending on the race, socioeconomic status and type of insurance of the child [21–23]. To our knowledge, this is the first study investigating differences in child abuse guideline adherence in infants with fractures depending on their age and inpatient vs outpatient care.
Our findings indicate a potential oversight among physicians, particularly in older infants treated as outpatients for common childhood fractures such as tibial and radial fractures. The poor guideline adherence in older infants treated as outpatients raises the question of whether we should revise our guideline to mandate child protection team involvement for all infants with fractures, regardless of age and fracture localisation. This question will be further discussed in the following sections, along with potential opportunities to improve the implementation of the guideline.
Our guideline specifically mandates child protection team involvement solely for infants under six months with fractures, making it optional for older children with certain common fractures under clearly defined circumstances (figure 1). The rationale for our different approach towards older children with specific fractures stems from evidence that most infants begin rolling over by six months, subsequently increasing the risk of falls from beds or changing tables. Falling incidents emerged as the leading cause of fractures in infants [7, 24]. Therefore, we advocate that in cases where parents provide a plausible history of falling in a child older than six months, emphasis should be placed on implementing primary and secondary prevention campaigns rather than enforcing general child protection measures.
Certain fractures such as skull, radial and tibial fractures frequently occur from a fall from a sitting or standing height, whereas femoral and humeral fractures usually result from higher falls [24]. Skull fractures are the most frequent fractures in children younger than 12 months of age [5, 8, 24]. Linear skull fractures are generally not associated with abuse [25]. In cases of isolated skull fractures, occult fractures in skeletal surveys (which raise suspicions of child abuse) are most commonly found in children younger than six months of age [26, 27]. Tibial and radial fractures, more frequent in ambulatory children, are rarely found in children younger than six months of age [8], and most frequently are non-inflicted [10]. Nevertheless, a recent study encompassing children under 36 months of age reports a small proportion of long bone fractures attributed to abuse, 8% of tibial/fibular fractures and 3% of radial fractures, regardless of fracture type (i.e. metaphyseal or diaphyseal) [9]. In our view, these data suggest that in mobile infants older than six months presenting with skull, tibial or radial fractures, while abuse remains rare, a comprehensive assessment, considering previous medical history and additional information, is essential. This emphasises the crucial role of paediatricians or family doctors in understanding a family’s circumstances and identifying any previous sentinel injuries that might have been mistakenly attributed to non-inflicted trauma [28]. While mandatory child protection team involvement may not be needed in low-probability abuse cases, prompt consultations with the paediatrician or family doctor by the treating attending physician are essential.
Evidence suggests that the mere implementation of guidelines may be insufficient to change patient management. Therefore, strategies such as continuous physician training and embedding guidelines into electronic patient record systems have demonstrated effectiveness [29, 30]. Thus, our findings of low guideline adherence highlight the need for ongoing clinical training, particularly in outpatient care, to increase awareness and improve the differential diagnosis of child abuse.
We did not collect data on the reasons behind the lack of consultations with paediatricians or family doctors or the child protection team. However, we hypothesise that the absence of suspicion regarding potential child abuse was a common reason for guideline non-adherence. Furthermore, we presume that in older children with certain common fractures, adherence to the guideline’s recommendation to consult paediatricians or family doctors was lacking, particularly in cases where consultations occurred during evenings or weekends when outpatient clinics were closed. This limitation underscores the need to explore the feasibility of adapting the guideline to address these challenges. Potential adaptations might include implementing systems to facilitate communication with paediatricians or family doctors, especially in outpatient-treated children, possibly involving other professional groups such as social workers.
As secondary outcomes, we assessed the frequency of child protection team involvement, the skeletal survey rate and the child abuse detection rate, comparing them with data collected by Bataenjer et al. prior to the guideline’s introduction [31]. Post-implementation, the child protection team involvement rate doubled, from 25% to 54%; however, the skeletal survey rate decreased and the child abuse detection rate remained unchanged. This indicates that the guideline’s implantation promoted discussions on differentiating child abuse, thereby enhancing the quality of assessment for infants with fractures.
Conversely, the rate of skeletal surveys decreased from 17% to 8% following guideline implementation. In both instances before and after the implementation of the guideline, skeletal surveys were generally ordered by the child protection team. We are unable to provide a clear explanation for the decrease in the rate of skeletal surveys following the implementation of the guideline. However, given our study’s small sample size, certainty regarding this decrease as a definite trend remains uncertain. Nonetheless, our skeletal survey yield of 40% (with two out of five skeletal surveys revealing an occult fracture) exceeded the 16.7% reported by Bataenjer, aligning with approaches in hospitals that refrain from mandating routine skeletal surveys in infants with fractures [29, 32].
Regarding child abuse detection, our study identified a consistent rate of 1.6% after the guideline implementation compared to the prior rate of 2.8%. These findings agree with reports from other research groups that also observed no significant change in abuse detection rates after implementing guidelines for infants with fractures [23]. This suggests that non-standardised management by physicians before the guideline may not have significantly hindered abuse detection. However, it is important to acknowledge that our study’s lack of change in the abuse detection rate could be influenced by a type II error due to our relatively small sample size. Our observed abuse detection rate is lower than earlier studies by Leventhal et al. and Worlock et al. [5, 6] but consistent with more recent findings [4, 7, 9]. The complex nature of changes in abuse detection rates over time are influenced by various factors, as suggested by Sharkey et al., who observed a decrease in abuse proportion over the decades attributed to an increase in total recorded fractures with stable absolute abuse case numbers [9].
This study underscores its strength in demonstrating the practical implementation and effectiveness of a guideline designed for assessing infants with fractures. This research provides valuable insights into the guideline’s feasibility within clinical settings, thereby having direct implications for daily clinical practice in paediatric emergency departments. To the best of our knowledge, this is the first study to evaluate and compare the management of infants with fractures across both outpatient and inpatient care settings. Consequently, it offers unique insights into potential differences that were previously unexplored.
The limitations of this study predominantly arise from its small sample size, potentially limiting the generalisability of the findings. It is important to exercise caution when comparing data collected before and after the guideline’s implementation because a considerable proportion of patients were not managed in accordance with the guideline, potentially introducing bias to the results. Data collection relied on written reports, and actions not documented in writing were considered missing. This reliance on documentation may have led to discrepancies between the recorded data and actual practices, potentially affecting the accuracy of the findings. Additionally, the high number of children excluded due to the absence of parental consent may have resulted in underrepresentation of cases of non-accidental trauma, thus contributing to selection bias. Furthermore, the relatively low prevalence of child abuse cases within the study population may have limited the study’s ability to detect substantial changes in abuse detection rates.
No funding was received for conducting this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Moon RJ, Harvey NC, Curtis EM, de Vries F, van Staa T, Cooper C. Ethnic and geographic variations in the epidemiology of childhood fractures in the United Kingdom. Bone. 2016 Apr;85:9–14.
2. Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007 Aug;38(8):913–22.
3. Rosendahl K, Myklebust R, Ulriksen KF, Nøttveit A, Eide P, Djuve Å, et al. Incidence, pattern and mechanisms of injuries and fractures in children under two years of age. BMC Musculoskelet Disord. 2021 Jun;22(1):555.
4. Wolfe JA, Wolfe H, Banaag A, Tintle S, Perez Koehlmoos T. Early Pediatric Fractures in a Universally Insured Population within the United States. BMC Pediatr. 2019 Oct;19(1):343.
5. Leventhal JM, Martin KD, Asnes AG. Incidence of fractures attributable to abuse in young hospitalized children: results from analysis of a United States database. Pediatrics. 2008 Sep;122(3):599–604.
6. Kemp AM, Dunstan F, Harrison S, Morris S, Mann M, Rolfe K, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008 Oct;337 oct02 1:a1518.
7. Rodà D, Trenchs V, Curcoy AI, Martínez AD, Pou J, Luaces C. Epidemiology of Fractures in Children Younger Than 12 Months. Pediatr Emerg Care. 2019 Apr;35(4):256–60. doi: https://doi.org/10.1097/PEC.0000000000001157
8. Clarke NM, Shelton FR, Taylor CC, Khan T, Needhirajan S. The incidence of fractures in children under the age of 24 months—in relation to non-accidental injury. Injury. 2012 Jun;43(6):762–5.
9. Sharkey MS, Buesser KE, Gaither JR, Tate V, Cooperman DR, Moles RL, et al. Abusive fracture incidence over three decades at a level 1 pediatric trauma center. Child Abuse Negl. 2018 Feb;76:364–71.
10. Flaherty EG, Perez-Rossello JM, Levine MA, Hennrikus WL, Christian CW, Crawford-Jakubiak JE, et al.; American Academy of Pediatrics Committee on Child Abuse and Neglect; Section on Radiology, American Academy of Pediatrics; Section on Endocrinology, American Academy of Pediatrics; Section on Orthopaedics, American Academy of Pediatrics; Society for Pediatric Radiology. Evaluating children with fractures for child physical abuse. Pediatrics. 2014 Feb;133(2):e477–89.
11. Pierce MC, Bertocci G. Injury biomechanics and child abuse. Annu Rev Biomed Eng. 2008;10(1):85–106. doi: https://doi.org/10.1146/annurev.bioeng.9.060906.151907
12. Banaszkiewicz PA, Scotland TR, Myerscough EJ. Fractures in children younger than age 1 year: importance of collaboration with child protection services. J Pediatr Orthop. 2002;22(6):740–4. doi: https://doi.org/10.1097/01241398-200211000-00009
13. Shum M, Asnes A, Leventhal JM, Bechtel K, Gaither JR, Tiyyagura G. The Use of Experts to Evaluate a Child Abuse Guideline in Community Emergency Departments. Acad Pediatr. 2021 Apr;21(3):521–8.
14. Wood JN, Fakeye O, Feudtner C, Mondestin V, Localio R, Rubin DM. Development of guidelines for skeletal survey in young children with fractures. Pediatrics. 2014 Jul;134(1):45–53.
15. Berchtold MB, Wüthrich C, Garcia D, Berger S, Löllgen RM. Nurses’ and physicians’ reported difficulties and enablers to recognising and reporting child abuse in Swiss paediatric emergency and paediatric surgery departments - an observational study. Swiss Med Wkly. 2023 Jun;153(6):40017.
16. Harper NS, Eddleman S, Lindberg DM. The utility of follow-up skeletal surveys in child abuse. Pediatrics. 2013;131(3):e672-8. Epub 20130211. doi: . PubMed PMID: 23400607.
17. Metz JB, Otjen JP, Perez FA, Done SL, Brown EC, Wiester RT, et al. Fracture-Associated Bruising and Soft Tissue Swelling in Young Children With Skull Fractures: How Sensitive Are They to Fracture Presence? Pediatr Emerg Care. 2021 Dec;37(12):e1392–6. doi: https://doi.org/10.1097/PEC.0000000000002058
18. Zaman S, Logan PH, Landes C, Harave S. Soft-tissue evidence of head injury in infants and young children: is CT head examination justified? Clin Radiol. 2017;72(4):316-22. Epub 20170121. doi: . PubMed PMID: 28118993.
19. Greenes DS, Schutzman SA. Clinical indicators of intracranial injury in head-injured infants. Pediatrics. 1999 Oct;104(4 Pt 1):861–7.
20. Wang Y, Doyle M, Smit K, Varshney T, Carsen S. The Toddler’s Fracture. Pediatr Emerg Care. 2022 Jan;38(1):36–9. doi: https://doi.org/10.1097/PEC.0000000000002600
21. Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408-14. Epub 20100816. doi: . PubMed PMID: 20713477.
22. Stavas N, Paine C, Song L, Shults J, Wood J. Impact of Child Abuse Clinical Pathways on Skeletal Survey Performance in High-Risk Infants. Acad Pediatr. 2020;20(1):39-45. Epub 20190314. doi: . PubMed PMID: 30880065; PubMed Central PMCID: PMC7898241.
23. Higginbotham N, Lawson KA, Gettig K, Roth J, Hopper E, Higginbotham E, et al. Utility of a child abuse screening guideline in an urban pediatric emergency department. J Trauma Acute Care Surg. 2014 Mar;76(3):871–7. doi: https://doi.org/10.1097/TA.0000000000000135
24. Wegmann H, Orendi I, Singer G, Eberl R, Castellani C, Schalamon J, et al. The epidemiology of fractures in infants—which accidents are preventable? Injury. 2016 Jan;47(1):188–91.
25. Piteau SJ, Ward MG, Barrowman NJ, Plint AC. Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics. 2012 Aug;130(2):315–23.
26. Laskey AL, Stump TE, Hicks RA, Smith JL. Yield of skeletal surveys in children ≤ 18 months of age presenting with isolated skull fractures. J Pediatr. 2013 Jan;162(1):86–9.
27. Wood JN, Henry MK, Berger RP, Lindberg DM, Anderst JD, Song L, et al. Use and Utility of Skeletal Surveys to Evaluate for Occult Fractures in Young Injured Children. Acad Pediatr. 2019;19(4):428–37.
28. Christian CW; Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse. Pediatrics. 2015 May;135(5):e1337–54.
29. Deutsch SA, Henry MK, Lin W, Valentine KJ, Valente C, Callahan JM, et al. Quality Improvement Initiative to Improve Abuse Screening Among Infants With Extremity Fractures. Pediatr Emerg Care. 2019 Sep;35(9):643–50. doi: https://doi.org/10.1097/PEC.0000000000001671
30. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999 Oct;282(15):1458–65.
31. Bataenjer R, Grotzer M, Seiler M. For Infants With Fractures: Involvement of a Child Protection Team Is Mandatory With Few Exceptions. Pediatr Emerg Care. 2022 Feb;38(2):e724–30. doi: https://doi.org/10.1097/PEC.0000000000002325
32. Loos MH, Ahmed T, Bakx R, van Rijn RR. Prevalence and distribution of occult fractures on skeletal surveys in children with suspected non-accidental trauma imaged or reviewed in a tertiary Dutch hospital. Pediatr Surg Int. 2020 Sep;36(9):1009–17.