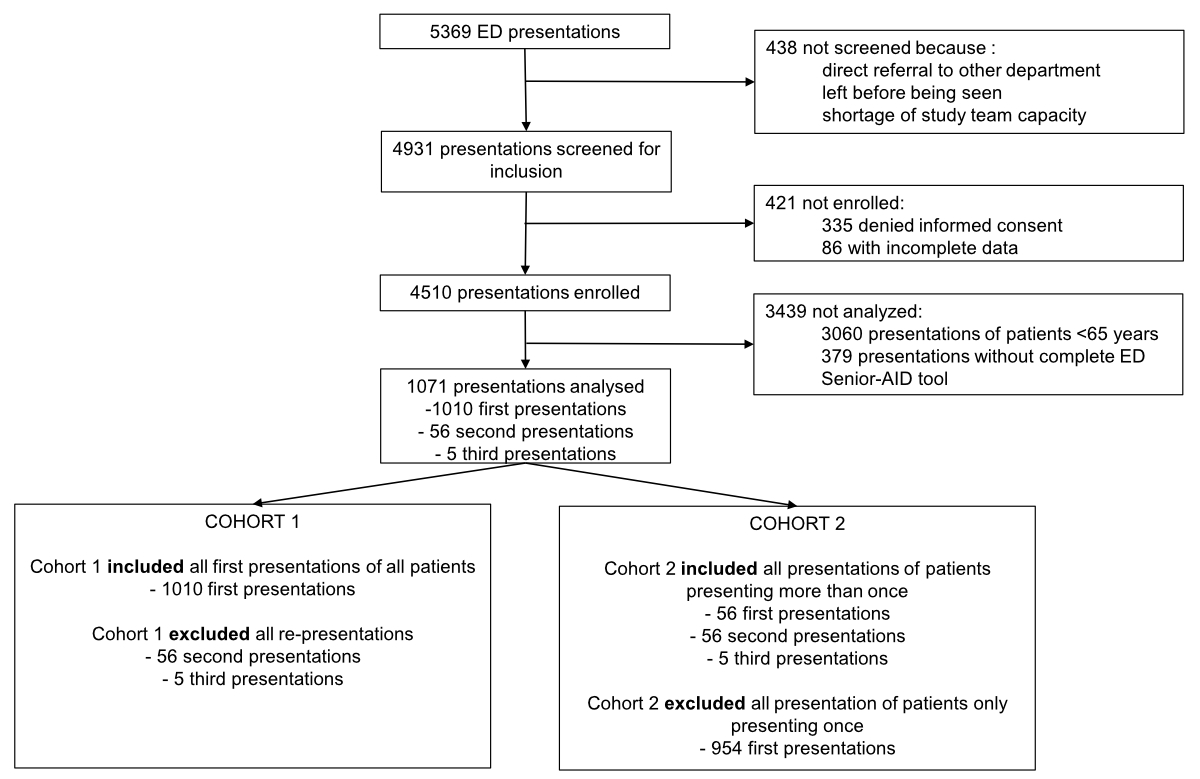
Figure 1Flow chart of the study population. The chart shows the recruitment procedure of emergency department presentations for which the Emergency Department Senior Abuse Identification (ED Senior AID) tool was used.
DOI: https://doi.org/https://doi.org/10.57187/s.3775
Mistreatment of older adults is a global social and health problem [1]. Its prevalence in community-dwelling older adults was estimated at up to 15% [2]. While physical mistreatment, involving intentional actions to inflict pain or injury, might be more apparent and overt, neglect is the more common form of mistreatment in older adults [3–6]. Neglect, which refers to the failure of the assigned caregiver to fulfil the needs of an older dependent adult, can present, for example, as poor hygiene, pressure sores, and dehydration [5, 7–9]. Other forms of mistreatment can be emotional or psychological, which involves intentional actions aimed at causing emotional pain or injury, and financial, which involves the improper use or misappropriation of an older adult’s money or property [4, 5, 9]. Sexual mistreatment, defined as non-consensual sexual contact of any kind, was reported less frequently [2, 5].
Previous studies have shown all forms of mistreatment to be associated with mortality [5, 6, 10, 11], depression [5, 12], emergency department visits [13–15], and hospitalisations [16]. Nevertheless, the reported numbers are low [17, 18] since emergency department screening is barely established [3, 5]. Therefore, data on the prevalence of elder mistreatment in the emergency department are scarce and primarily based on retrospective data and surveys from the USA and Singapore. Most studies did not use a dedicated screening tool and showed a prevalence ranging from 0.01% to 0.03% in older adults presenting to the emergency department [17, 18]. Such low numbers make unreported cases likely and indicate a potential failure to identify mistreatment cases [19, 20]. Studies using screening tools for elder mistreatment demonstrated a positive screening rate of 4%–7% among older adults presenting to the emergency department in the US [7, 21]. No studies have examined the prevalence of elder mistreatment in European emergency departments, with or without the use of a dedicated screening tool.
Since older adults who have experienced mistreatment are probably more likely to visit the emergency department, emergency department staff might be uniquely positioned to recognise elder mistreatment [13, 20]. The Emergency Department Senior Abuse Identification (ED Senior AID) tool [7] was developed and validated in North America to screen for elder mistreatment in the emergency department and showed high sensitivity and specificity [21]. The Emergency Department Senior Abuse Identification tool uses questions to gather information about physical, emotional, and financial aspects and also involves a physical examination [7, 22]. Professionals can use this tool to identify potential mistreatment cases in the emergency department and take appropriate actions involving social services or law enforcement early on if needed.
As the validated tool is in English, our aims included translating and culturally adapting the Emergency Department Senior Abuse Identification tool for use in German-speaking regions, screening for elder mistreatment with the German version, and comparing the characteristics of patients who screened positive and negative.
This study was conducted at the University Hospital Basel in Switzerland. This tertiary academic urban hospital has >55,000 emergency department visits per year, of which approximately one-third are aged ≥65 years. Western Europeans (Caucasian) comprise two-thirds of the regional population, with the remainder mainly from Mediterranean countries and Eastern Europe [23]. This prospective observational cohort study was designed for quality control using routine data at emergency department presentation. It included all consecutive patients presenting to the emergency department from 25 April to 30 May 2022. Inclusions were conducted 24 hours a day, seven days a week. Elder mistreatment was defined as the intentional or negligent action by a caregiver or trusted person causing harm or risk to an older adult in the past six months [24].
This study received ethical approval from the Local Ethics Committee (Project-ID: 236/13; http://eknz.ch) and was conducted according to the principles of the Declaration of Helsinki. It was registered with the National Institute of Health on ClinicalTrials.gov and assigned the registration number NCT05400707. It was reported according to the STROBE guidelines [25].
All consecutive patients who presented to the emergency department during the study period were eligible. Patients who refused to consent or could not communicate (e.g. immediate transfers to the operating room or treatment in the resuscitation bay) were excluded. Per previous recommendations, patients presenting with mild cognitive impairment [26] who could give verbal consent were not excluded to minimise bias. This analysis excluded all patients aged <65 years.
A dedicated study team screened and interviewed every patient during the study period. The study team consisted of trained medical students.
The Emergency Department Senior Mistreatment Identification (ED Senior AID) tool was translated into German following the ISPOR guidelines [7, 27]. Two independent forward translations into German were made. These were then aligned by having the translators compare their versions. The resulting common version was independently translated back into English by two native English speakers. These back-translations were then compared to the original. All translations were harmonised to ensure conceptual equality between the original and the translation. No cross-cultural adaptations were needed. The resulting German translation of the Emergency Department Senior Abuse Identification tool was then used and can be found in the appendix of this article (Figure S1). The study team performed the first two steps, and the attending physician in charge performed the subsequent steps.
The study team conducted the first step, which uses a cognitive test, the Abbreviated Mental Test-4 (AMT-4), to evaluate the patient’s cognitive ability. In this test, the patient is asked four questions about their age, birthday, place, and year [28]. The second step consists of a series of questions designed to cover all areas of elder mistreatment. It was performed after the cognitive test by a study team member.
The attending emergency department physicians performed the third and fourth steps. In the third step, the attending physician decided if the patient could reliably report mistreatment or if they should receive a physical assessment for mistreatment. In the last step, the attending physician decided if mistreatment was suspected. If the attending physician was confident about the patient’s ability to report mistreatment but was still unsure if they should suspect elder mistreatment, they could return to step three and conduct a physical assessment for elder mistreatment. After this additional physical assessment, the attending physician had to make a final decision on the suspicion of elder mistreatment [7].
Machine-readable case report forms were used to record all data. These were then scanned and cleaned in a two-step process. In the first step, the emergency department administrators corrected handwriting issues. In the second step, an external company, digx GmbH, transferred the data to a database.
Baseline demographics, the National Early Warning Score (NEWS) and the Clinical Frailty Scale (CFS) assigned at triage were extracted from the electronic health records.
Some patients re-presented during the study period. Due to re-presentations, we formed two separate cohorts. Cohort 1 included only index presentations of all unique patients aged ≥65 years for whom the Emergency Department Senior Abuse Identification tool was completed.
Cohort 2 included the presentations of patients re-presenting during the study period, as this could be a subtle hint of elder mistreatment. Some presented twice during the study period, while others presented three times. Cohort 2 included all presentations of patients who re-presented during the study period, including their index presentations and subsequent visits.
The primary outcome of this study was the positive screening rate of elder mistreatment using the Emergency Department Senior Abuse Identification tool in a tertiary academic urban emergency department.
The secondary outcomes of this study were the characteristics of patients that screened positive and their hospitalisation rate, as well as the tool’s usability, defined as the percentage of fully completed assessments.
In the descriptive analysis, metric variables are presented as means with standard deviations, and categorical variables are presented as counts and frequencies. We compared the characteristics and results of the Emergency Department Senior Abuse identification tool of patients who screened positive and negative. We also aimed to distinguish the features of patients who underwent screening and those who did not. Moreover, we explored differences between patients who presented once and those who presented multiple times. Missing data were tested for bias using the Kruskal–Wallis test, Chi-square test, or Fisher’s exact test, as appropriate. This analysis aimed to compare the characteristics of missing data with the overall study population. All analyses were performed using R studio software (version 4.2.2) [29].
From 25 April to 30 May 2022, 5,369 consecutive presentations were recorded, 1,450 of which were by patients aged ≥65 years. Of these, 379 presentations were not or incompletely screened for elder mistreatment and subsequently excluded from further analysis. Therefore, the analysis included 1,071 presentations by 1,010 patients aged ≥65 years.
For further analysis, we formed two separate cohorts. Cohort 1 included only index presentations of all 1,010 unique patients aged ≥65 years for which the Emergency Department Senior Abuse Identification tool was used.
Cohort 2 comprised 56 patients, of whom 51 presented twice and five presented thrice during the study period. This cohort comprised 56 index presentations (included in Cohort 1), 56 second presentations (excluded from Cohort 1), and five third presentations (excluded from Cohort 1; figure 1).
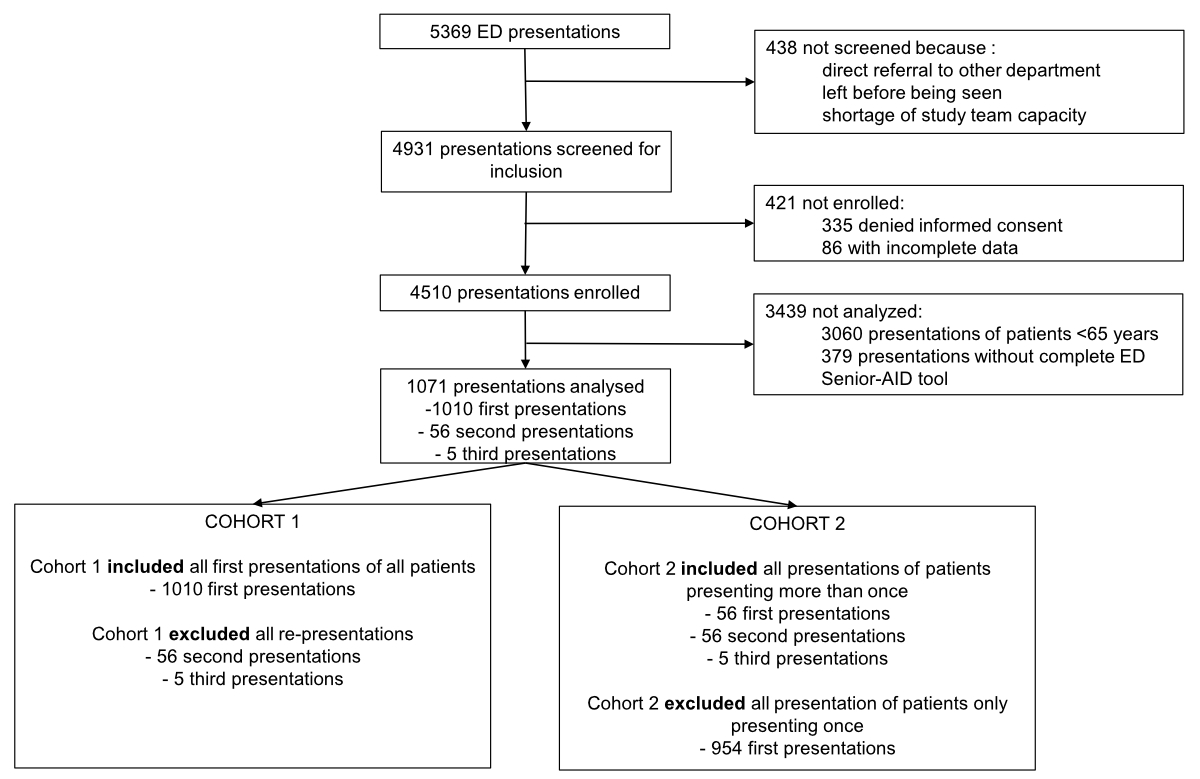
Figure 1Flow chart of the study population. The chart shows the recruitment procedure of emergency department presentations for which the Emergency Department Senior Abuse Identification (ED Senior AID) tool was used.
The Emergency Department Senior Abuse Identification tool was intended to be used in all 1450 presentations during the study period. The Emergency Department Senior Abuse Identification tool was completed for 73.9% of presentations, with 379 not assessed using the Emergency Department Senior Abuse Identification tool. For comparison, the Emergency Severity Index was missing for six presentations (i.e. a completion rate of 99.6%). In incomplete assessments, the components most often missing concerned the second step, the questions about elder mistreatment (Table S1 in the appendix).
Patients excluded from our study due to incomplete or missing data were more frail, as assessed by the CFS, had a higher mortality, and were assigned higher (more urgent) triage levels than the patients with complete data (Table S2 in the appendix).
Among the 1,010 patients with only an index presentation, the median age was 78 (interquartile range [IQR]: 72.00–85.00) years, and 525 (52.0%) were female. Twenty-nine patients (2.9%) screened positive for elder mistreatment with the Emergency Department Senior Abuse Identification tool. In addition, 589 patients (58.3%) were hospitalised; 25 of the 29 (86.2%) positively screened patients were hospitalised. The patients who screened positive had significantly higher ages, Clinical Frailty Score, the National Early Warning Score (NEWS), and cognitive impairment, as evaluated by the AMT-4 test, than those who screened negative (table 1). Mortality inside and outside of the hospital was comparable among all patients, regardless of their screening result (up to 100 days post-presentation [p = 0.861] and in-hospital [p = 0.628]).
Table 1The baseline characteristics of all index presentations. Data are presented as medians (interquartile ranges) for continuous variables and numbers (percentages) for categorical variables.
| All | Negative screen | Positive screen | ||
| n (%) | 1010 (100%) | 981 (97.1%) | 29 (2.9%) | |
| Age (years), median (IQR) | 78.00 (72.00–85.00) | 78.00 (72.00–85.00) | 84.00 (79.00) | |
| Sex (female), n (%) | 525 (52.0%) | 506 (51.6%) | 19 (65.5%) | |
| Admitted, n (%) | 589 (58.3%) | 564 (57.5%) | 25 (86.2%) | |
| National Early Warning Score, median (IQR) | 1.00 (0.00–2.00) | 1.00 (0.00–2.00) | 2.50 (0.25–4.00) | |
| Clinical Frailty Scale, median (IQR) | 3 (3–5) | 3 (3–5) | 6 (5–6) | |
| Nursing home patients, n (%) | 105 (10.4%) | 105 (100%) | 0 | |
| Correct AMT-4 answers, n (%) | 0 | 13 (1.3%) | 13 (1.3%) | 0 |
| 1 | 21 (2.1%) | 17 (1.7%) | 4 (13.8%) | |
| 2 | 42 (4.2%) | 40 (4.1%) | 2 (6.9%) | |
| 3 | 79 (7.8%) | 78 (8.0%) | 1 (3.4%) | |
| 4 | 855 (84.7%) | 833 (84.9%) | 22 (75.9%) | |
AMT-4: Abbreviated Mental Test-4; IQR: interquartile range.
In the first step, the AMT-4 was administered to all patients in Cohort 1: 855 (84.7%) responded correctly to all four questions, 79 (7.8%) to three, 42 (4.2%) to two, 21 (2.1%) to one, and 13 (1.3%) to none (table 2). Patients who screened positive had more incorrect responses than those who screened negative (p <0.001; table 1).
Table 2The Abbreviated Test-4 (AMT-4) results for the index presentations. Data are shown as the number (percentage) of all patients.
| Correct, n (%) | Incorrect, n (%) | If false, n of positive screens | |
| What is your age? | 928 (91.9%) | 82 (8.1%) | 5 |
| What is your date of birth? | 975 (96.5%) | 35 (3.5%) | 3 |
| What is this place? | 955 (94.6%) | 55 (5.4%) | 3 |
| What is the year? | 904 (89.5%) | 106 (10.5%) | 6 |
In the second step, the study team personally interviewed all patients. Of the 1,010 patients in Cohort 1, 309 (30.6%) reported needing help with at least one of the following: bathing, dressing, shopping, banking, or meals. Of these patients, 4 out of 304 (1.3%) reported that they lacked help for any of these activities of daily living; none of these patients screened positive for elder mistreatment. Of the 296 who received help, 31 (10.5%) reported that their caregiver was not always there when they were needed; 4 of these 31 patients screened positive. Psychological and emotional mistreatment was reported most often by patients in Cohort 1. Physical and financial mistreatment were reported less often (table 3).
Table 3The responses to the elder mistreatment screening questions at the index presentations. Data are shown as the number (percentage) of all patients. Missing data affects questions 1a (n = 5) and 1b (n = 4).
| No, n (%) | Yes, n (%) | If yes, n of positive screens | |
| 1. Have you needed help with bathing, dressing, shopping, banking, or meals? | 701 (69.4%) | 309 (30.6%) | 18 |
| 1a. If yes, have you had someone who helps with this? | 4 (1.3%) | 300 (98.7%) | 0 vs 17* |
| 1b. If yes, is this person always there when you need them? | 31 (10.5%) | 265 (89.5%) | 4 vs 13* |
| 2. Has anyone close to you called you names and put you down? | 980 (97.0%) | 30 (3.0%) | 4 |
| 3. Has anyone told you that you give them too much trouble? | 982 (97.2%) | 28 (2.8%) | 3 |
| 4. Has anyone close to you threatened you or made you feel bad? | 989 (97.9%) | 21 (2.1%) | 1 |
| 5. Has anyone tried to force you to sign papers or use your money against your will? | 996 (98.6%) | 14 (1.4%) | 2 |
| 6. Has anyone close to you tried to hurt you or harm you? | 1002 (99.2%) | 8 (0.8%) | 2 |
* For questions 1a and 1b, the number of positively screened patients is shown relative to both answers.
In the third step, the attending physician was interviewed about the patient’s ability to report mistreatment. Attending physicians were confident in 836 (82.8%) of all patients and not confident in 174 (17.2%) in Cohort 1, leading to a subsequent physical assessment to identify mistreatment.
The most common physical findings resulting in a positive screen in Cohort 1 were poor control of medical problems in 32/174 (18.4%) patients. Dehydration symptoms were found in 24/181 (13.3%) patients. Evidence of neglect (18/181, 9.9%), malnutrition (16/181, 8.8%), and swollen or tender areas on palpation (13/181, 7.2%) were also common (table 4). As elements were not mutually exclusive, 53 patients displayed 117 elements suggesting mistreatment, 21 displayed one, 15 displayed two, 11 displayed three, 3 displayed four, and 3 displayed five or more. After the physical assessment, the attending physician suspected mistreatment in 21 (12.1%) patients who underwent physical assessment in Cohort 1. Since the evidence for elder mistreatment increases with the number of elements, the percentage of positively screened patients increased accordingly (figure 2).
Table 4The physical assessment results for the index presentations.Data are shown as the number (percentage) of all patients. Missing data affects questions 6 (n = 3, 1.6%), 8 (n = 1, 0.6%), 9 (n = 2, 1.1%), 10 (n = 2, 1.1%), and 12 (n = 2, 1.1%). The symptoms are not mutually exclusive.
| No | Yes | If yes, n of positive screens | ||
| Elements highly suggestive of Mistreatment | 1. Bruising in unusual location, multiple bruises, or large bruises? | 170 (97.7%) | 4 (2.3%) | 2 |
| 2. Are burn patterns suggestive of intentional injury? | 174 (100%) | 0 | 0 | |
| 3. Patterned injuries? | 172 (98.9%) | 2 (1.1%) | 1 | |
| 4. Abrasions or lacerations suggestive of intentional injury? | 173 (99.4%) | 1 (0.6%) | 1 | |
| 5. Evidence of neglect? | 146 (83.9%) | 18 (16.1%) | 10 | |
| Elements which may suggest Mistreatment | 6. Evidence of dehydration? | 148 (86.5%) | 23 (13.5%) | 7 |
| 7. Evidence of poor control of medical problems? | 142 (81.6%) | 32 (18.4%) | 15 | |
| 8. Evidence of malnutrition? | 157 (90.8%) | 16 (9.2%) | 9 | |
| 9. Swollen or tender area on palpation? | 160 (93.0%) | 12 (7.0%) | 5 | |
| Specific circumstances | 10. Genital trauma or infection – evidence of sexual mistreatment? | 171 (99.4%) | 1 (0.6%) | 0 |
| 11. Fractures concerning for mistreatment? | 173 (99.4%) | 1 (0.6%) | 1 | |
| 12. The current problem has been present for a long time – is the unusual delay in seeking medical attention concerning for mistreatment? | 165 (95.9%) | 7 (4.1%) | 6 | |
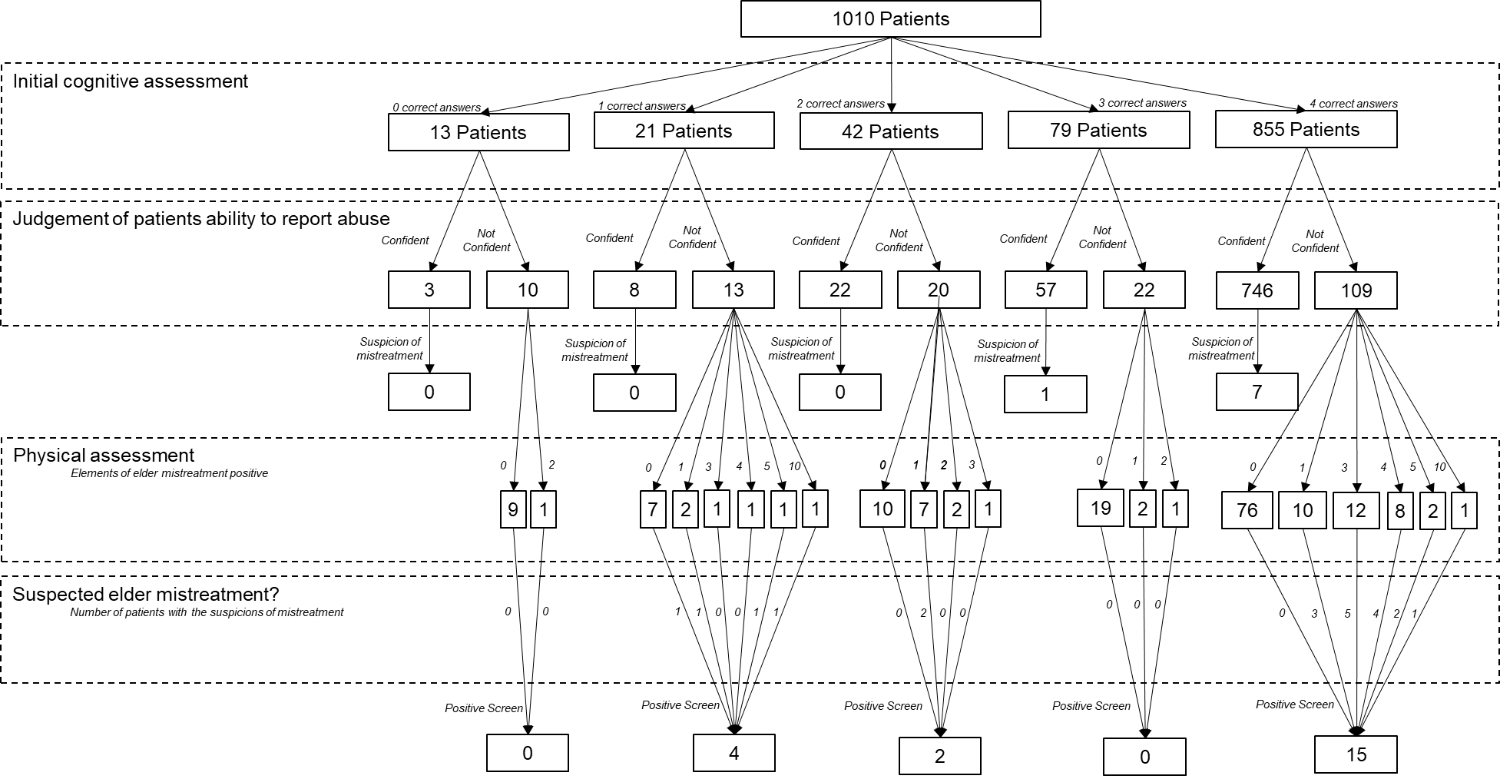
Figure 2Flow chart of the outcomes of all patients. The chart shows the Emergency Department Senior Abuse Identification (ED Senior AID) tool for every patient disaggregated by the outcomes.
Of all presenting patients, 104 (10.3%) were residents of nursing homes or long-term care facilities; none of these screened positive for elder mistreatment. Residents of nursing homes and long-term care facilities incorrectly answered questions on the AMT-4 significantly more often than community-dwelling older adults (p < 0.001). They presented fewer signs and symptoms in the physical assessment, suggesting a lower rate of mistreatment than community-dwelling older adults (p = 0.034).
Cohort 2 comprised 56 patients, of which 51 presented twice and five presented thrice during the study period. This analysis included 56 index presentations (included in Cohort 1), 56 second presentations (excluded from Cohort 1), and five third presentations (excluded from Cohort 1). Among the 56 patients in Cohort 2, the median age was 80 (IQR: 75.00–86.00) years, and 22 (39.3%) were female. No patient screened positive at their index presentation with the Emergency Department Senior Abuse Identification tool (table 5).
Table 5Baseline characteristics of individual patients stratified by number of presentations. For patients with multiple presentations to ED within study period, baseline characteristics for first presentation are presented.
| All | Single presentation | Multiple presentations | |
| n (%) | 1010 | 954 (94.5%) | 56 (5.5%) |
| Age (years), median (IQR) | 78.00 (72.00–85.00) | 78.00 (72.00–85.00) | 80.00 (75.00–86.00) |
| Sex (female), n (%) | 525 (52.0%) | 503 (52.7%) | 22 (39.3%) |
| Admitted, n (%) | 591 (58.5%) | 564 (59.1%) | 25 (44.6%) |
| National Early Warning Score, median (IQR) | 1.00 (0.00–2.00) | 1.00 (0.00–2.00) | 1.00 (0.00–2.00) |
| Clinical Frailty Scale, median (IQR) | 3.00 (3.00–5.00) | 3.00 (3.00–5.00) | 3.00 (3.00–5.00) |
| Nursing home patients, n (%) | 104 (10.3%%) | 98 (10.3%) | 6 (10.7%) |
IQR: interquartile range.
At the second visit, different attending physicians evaluated the 56 re-presenting patients and screened two (3.6%) as positive for elder mistreatment, of which one was subsequently hospitalised.
At the third visit, different attending physicians evaluated the six patients re-presenting again; none screened positive after evaluation with the Emergency Department Senior Abuse Identification tool.
In this prospective single-centre study of consecutive patients aged ≥65 years presenting to an urban emergency department, we provided a German version of the Emergency Department Senior Abuse Identification tool and assessed its performance regarding usability and positive screening rate for elder mistreatment. Twenty-nine (2.9%) of all presenting older adults screened positive for elder mistreatment. The patients who screened positive were older, frailer (as assessed by the Clinical Frailty Scale), more cognitively impaired, and assigned more urgent triage categories than those who screened negative. The positively screened patients were also hospitalised more frequently. Mortality up to 100 days after presentation was comparable regardless of the screening result.
The prevalence of elder mistreatment in the emergency department setting is not well established. A survey conducted in Singapore of 62,826 patients aged ≥65 years who presented to an emergency department between 1994 and 1997 revealed a prevalence of elder mistreatment of 0.03% [18]. A retrospective health record analysis for ICD-10 codes of six million patients aged ≥60 years in a US emergency department setting reported a prevalence of 0.01% [17]. Neither of these studies utilised a dedicated screening tool for elder mistreatment. Development and validation studies of the Emergency Department Senior Abuse Identification tool in the US reported positive screening rates for elder mistreatment in emergency departments of 4%–7% [7, 21], which can be compared to the 2.9% found in our study using the German version of the same tool. As retrospective evaluations found a substantially lower prevalence than prospective studies, the true prevalence is likely closer to the numbers reported by prospective studies using a dedicated tool.
In Switzerland, no data exists on the prevalence of elder mistreatment in the emergency department setting. The only available prevalence data focused on violence against community-dwelling older adults and were collected in 2000 via a survey by the Swiss Federal Statistical Office. This survey showed that 3.9% of community-dwelling older adults had experienced an act of violence (including robberies) over the past 12 months [30]. In subsequent years, the Swiss Federal Statistical Office removed this question from the survey [31]. Additionally, two smaller studies explored the perceptions of community-dwelling older adults and healthcare workers on elder mistreatment in Switzerland [32, 33].
Patients with more than one presentation had the same positive screening rate for elder mistreatment as those with single presentations, which is inconsistent with previous studies [13–15].
The characteristics of patients who screened positive for elder mistreatment were comparable to previous studies. They were older [34] and had greater cognitive impairment [3] and frailty [15, 34] than those who screened negative. All these factors have been suggested as risk factors for mistreatment [3, 15, 35] and institutionalisation [36].
One study suggested that patients who had experienced mistreatment were referred more often to emergency departments [14]. This observation would put emergency department personnel in a uniquely favourable position to identify potential mistreatment cases through simple routine screening in the emergency department and take appropriate actions involving social services or law enforcement early on if needed. As previously suggested, the high screening burden could be reduced by implementing a pre-screen [37].
The lower positive screening rate in our cohort compared to the original validation cohort [21] could be explained by several differences. First, elder mistreatment might occur less often due to financial issues in high-income countries. Second, institutionalised patients appear to receive high-quality care. Third, signs of elder mistreatment, such as malnutrition, might be confused as signs of “normal” ageing since they mimic chronic health conditions [38].
The usability of the Emergency Department Senior Abuse Identification tool can be assumed in our setting since almost 75% of screenings were completed. However, questions about elder mistreatment were incomplete in one-quarter of all cases, leading to exclusion from this study (table S1 in the appendix).
Previous studies have suggested that asking these types of questions might cause discomfort for healthcare providers and patients [39]. However, patients with missing data had higher morbidity, frailty, urgency, and mortality (table S2 in the appendix). Therefore, these factors could have compromised usability, particularly urgency. The comparison to the prevalence of elder mistreatment in community settings [2, 3, 17, 40] is difficult since time and resources play an important role. In the community, 10.5 home visits by nursing in-home caretakers were needed to suspect one case of mistreatment on average [41]. However, one might expect that elder mistreatment is not much rarer in emergency department presenters. Therefore, easy-to-use and standardised tools are needed for early detection [3, 42].
Despite emerging screening tools, there is a lack of evidence regarding their impact on outcomes [43, 44]. The US Preventive Services Task Force even concluded in a 2018 recommendation statement that there is insufficient evidence to assess the balance of benefits and risks of routine screening for elder mistreatment in clinical settings [44]. This recommendation statement is currently being reviewed. Therefore, gathering evidence is vital, particularly in emergency settings that tend to be a sentinel for issues of vulnerable populations.
The findings of this single-centre study conducted in Northern Switzerland during spring may not apply to different seasons or facilities in other parts of the world. The lack of a gold standard for recognising elder mistreatment makes it challenging to compare our study to others, potentially underestimating the prevalence of elder mistreatment. In addition, we were unable to investigate the interrater reliability of the ratings. The higher burden of morbidity, frailty, urgency, and mortality among patients with missing data for the Emergency Department Senior Abuse Identification tool may have led to a selection bias, potentially influencing the overall positive screening rate and usability. Since we implemented it into our study, the Emergency Department Senior Abuse Identification tool has been extended into the Elder Mistreatment Screening and Response tool, which includes a pretest to reduce the screening burden on healthcare providers [45]. The higher screening burden of the original tool might have impacted the actual prevalence and usability. Furthermore, the first multicentre validation study of the Emergency Department Senior Abuse Identification tool established a gold standard using a longitudinal, expert, all-data panel to validate all positive and 10% of randomly selected negative cases. Therefore, we did not apply this gold standard and cannot report performance criteria [21]. Lastly, we did not formally obtain feedback regarding the tool’s usability from the physicians who used it.
The presentation of an older adult to the emergency department is a sentinel event, and emergency departments are uniquely positioned to detect elder mistreatment.This study is the first to examine the prevalence of elder mistreatment in a European emergency department. Its positive screening rates and risk factors were comparable to non-European data, indicating a wider problem. Indeed, with increasing older populations, elder mistreatment could become a further challenge in healthcare globally. Therefore, implementing such elder mistreatment screening in the emergency department could potentially enhance case identification and improve patient outcomes.
Our data is currently not publicly accessible. However, it is available upon reasonable request to the corresponding author.
We would like to thank Dr. Isabelle Arnold, Ms. Anna-Zofia Szczesna, and Ms Deborah Allen for the translation and harmonization of the emergency department Senior abuse identification tool according to the ISPOR guidelines.
This research was funded by the Scientific Funds of the Emergency Department of the University Hospital Basel. There was no influence on the study design, data collection and analysis, or writing of the manuscript by the fund.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Lachs MS, Pillemer K. Elder abuse. Lancet. 2004 Oct;364(9441):1263–72. 10.1016/S0140-6736(04)17144-4
2. Yon Y, Mikton CR, Gassoumis ZD, Wilber KH. Elder abuse prevalence in community settings: a systematic review and meta-analysis. Lancet Glob Health. 2017 Feb;5(2):e147–56. 10.1016/S2214-109X(17)30006-2
3. Mercier É, Nadeau A, Brousseau AA, Émond M, Lowthian J, Berthelot S, et al. Elder Abuse in the Out-of-Hospital and Emergency Department Settings: A Scoping Review. Ann Emerg Med. 2020 Feb;75(2):181–91. 10.1016/j.annemergmed.2019.12.011
4. Simone L, Wettstein A, Senn O, Rosemann T, Hasler S. Types of abuse and risk factors associated with elder abuse. Swiss Med Wkly. 2016 Jan;146:w14273. 10.4414/smw.2016.14273
5. Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med. 2015 Nov;373(20):1947–56. 10.1056/NEJMra1404688
6. Shah SJ, Oreper S, Jeon SY, Boscardin WJ, Fang MC, Covinsky KE. Social Frailty Index: development and validation of an index of social attributes predictive of mortality in older adults. Proc Natl Acad Sci USA. 2023 Feb;120(7):e2209414120. 10.1073/pnas.2209414120
7. Platts-Mills TF, Dayaa JA, Reeve BB, Krajick K, Mosqueda L, Haukoos JS, et al.; Development of the Emergency Department Senior Abuse Identification. (ED Senior AID) tool. J Elder Abuse Negl. 2018;30(4):247–70. 10.1080/08946566.2018.1460285
8. Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev. 2011 Apr;68(2):131–55. 10.1177/1077558710379422
9. Hullick C, Carpenter CR, Critchlow R, Burkett E, Arendts G, Nagaraj G, et al. Abuse of the older person: is this the case you missed last shift? Emerg Med Australas. 2017 Apr;29(2):223–8. 10.1111/1742-6723.12756
10. Schofield MJ, Powers JR, Loxton D. Mortality and disability outcomes of self-reported elder abuse: a 12-year prospective investigation. J Am Geriatr Soc. 2013 May;61(5):679–85. 10.1111/jgs.12212
11. Dong X, Simon M, Mendes de Leon C, Fulmer T, Beck T, Hebert L, et al. Elder self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009 Aug;302(5):517–26. 10.1001/jama.2009.1109
12. Dong X, Chen R, Chang ES, Simon M. Elder abuse and psychological well-being: a systematic review and implications for research and policy—a mini review. Gerontology. 2013;59(2):132–42. 10.1159/000341652
13. Dong X, Simon MA. Association between elder abuse and use of ED: findings from the Chicago Health and Aging Project. Am J Emerg Med. 2013 Apr;31(4):693–8. 10.1016/j.ajem.2012.12.028
14. Rosen T, Zhang H, Wen K, Clark S, Elman A, Jeng P, et al.; Emergency Department and Hospital Utilization Among Older Adults Before and After Identification of Elder Mistreatment. Emergency Department and Hospital Utilization Among Older Adults Before and After Identification of Elder Mistreatment. JAMA Netw Open. 2023 Feb;6(2):e2255853–2255853. 10.1001/jamanetworkopen.2022.55853
15. Mercier E, Jones A, Brousseau A, Hirdes J, Mowbray F, Emond M, et al. Characteristics of emergency department visits by community-dwelling older adults who screened positive for elder abuse during home care assessments. CJEM. 2019;21 S1:S11–11. 10.1017/cem.2019.56
16. Dong X, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 May;173(10):911–7. 10.1001/jamainternmed.2013.238
17. Evans CS, Hunold KM, Rosen T, Platts-Mills TF; Diagnosis of Elder Abuse in U.S. Emergency Departments. Diagnosis of Elder Abuse in U.S. Emergency Departments. J Am Geriatr Soc. 2017 Jan;65(1):91–7. 10.1111/jgs.14480
18. Cham GW, Seow E. The pattern of elderly abuse presenting to an emergency department. Singapore Med J. 2000 Dec;41(12):571–4.
19. Reges ML. Forensic Nurse Identification of Elder Abuse: Implementing the Elder Assessment Instrument. 2023, Salisbury University: United States -- Maryland. p. 90.
20. Gottesman E, Elman A, Rosen T. Elder Mistreatment: Emergency Department Recognition and Management. Clin Geriatr Med. 2023 Nov;39(4):553–73. 10.1016/j.cger.2023.05.007
21. Platts-Mills TF, Hurka-Richardson K, Shams RB, Aylward A, Dayaa JA, Manning M, et al.; Investigators for the ED Senior AID Research Group. Multicenter Validation of an Emergency Department-Based Screening Tool to Identify Elder Abuse. Ann Emerg Med. 2020 Sep;76(3):280–90. 10.1016/j.annemergmed.2020.07.005
22. Kayser J, Morrow-Howell N, Rosen TE, Skees S, Doering M, Clark S, et al. Research priorities for elder abuse screening and intervention: A Geriatric Emergency Care Applied Research (GEAR) network scoping review and consensus statement. J Elder Abuse Negl. 2021;33(2):123–44. 10.1080/08946566.2021.1904313
23. Jauslin AS, Schultze L, Knuchel D, Simon NR, Nickel CH, Bingisser R. Disparities in emergency department access, resource allocation, and outcomes between migrants and the local population. Swiss Med Wkly. 2021 Nov;151(4344):w30070. 10.4414/SMW.2021.w30070
24. Prevention, C.f.D.C.a. Elder Abuse: Definitions. 2017 [cited 2018 February 2nd]; Available from: https://www.cdc.gov/violenceprevention/elderabuse/definitions.html
25. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008 Apr;61(4):344–9. 10.1016/j.jclinepi.2007.11.008
26. Prusaczyk B, Cherney SM, Carpenter CR, DuBois JM. Informed Consent to Research with Cognitively Impaired Adults: Transdisciplinary Challenges and Opportunities. Clin Gerontol. 2017;40(1):63–73. 10.1080/07317115.2016.1201714
27. Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8(2):94–104. 10.1111/j.1524-4733.2005.04054.x
28. Schofield I, Stott DJ, Tolson D, McFadyen A, Monaghan J, Nelson D. Screening for cognitive impairment in older people attending accident and emergency using the 4-item Abbreviated Mental Test. Eur J Emerg Med. 2010 Dec;17(6):340–2. 10.1097/MEJ.0b013e32833777ab
29.. Team RC. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2022.
30.. Fibbi R (Office SF, editor). Les personnes âgées en Suisse [Older persons in Switzerland]Neuchatel, Switzerland; 2000.
31. Schweizerische Gesundheitsbefragung 2017 - Telefonischer und schriftlicher Fragebogen (pdf). Schweizerische Gesundheitsbefragung 2017 - Telefonischer und schriftlicher Fragebogen (pdf). 2020. 130.
32. Roulet Schwab D, Wangmo T. Perceptions of Elder Abuse From Community-Dwelling Older Persons and Professionals Working in Western Switzerland. J Interpers Violence. 2021 Jan;36(1-2):NP135–61. 10.1177/0886260517732345
33. Wangmo T, Nordström K, Kressig RW. Preventing elder abuse and neglect in geriatric institutions: solutions from nursing care providers. Geriatr Nurs. 2017;38(5):385–92. 10.1016/j.gerinurse.2016.12.016
34. Fulmer T, Paveza G, VandeWeerd C, Fairchild S, Guadagno L, Bolton-Blatt M, et al. Dyadic vulnerability and risk profiling for elder neglect. Gerontologist. 2005 Aug;45(4):525–34. 10.1093/geront/45.4.525
35. Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, et al. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010 Feb;100(2):292–7. 10.2105/AJPH.2009.163089
36. Kojima G. Frailty as a Predictor of Nursing Home Placement Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. J Geriatr Phys Ther. 2018;41(1):42–8. 10.1519/JPT.0000000000000097
37. Makaroun LK, et al. Leveraging VA Geriatric Emergency Department Accreditation to Improve Elder Abuse Detection in Older Veterans using a Standardized Tool [n/a]. Acad Emerg Med. 2022;•••.
38. Lachs MS, Fulmer T. Recognizing elder abuse and neglect. Clin Geriatr Med. 1993 Aug;9(3):665–81. 10.1016/S0749-0690(18)30399-9
39. Nixon B, Quinlan E. Asking the Hard Questions: Psychologists’ Discomfort With Inquiring About Sexual Abuse Histories. Violence Against Women. 2022 Apr;28(5):1358–76. 10.1177/10778012211014558
40. Rovi S, Chen PH, Vega M, Johnson MS, Mouton CP. Mapping the elder mistreatment iceberg: U.S. hospitalizations with elder abuse and neglect diagnoses. J Elder Abuse Negl. 2009 Oct;21(4):346–59. 10.1080/08946560903005109
41. Friedman B, Santos EJ, Liebel DV, Russ AJ, Conwell Y. Longitudinal prevalence and correlates of elder mistreatment among older adults receiving home visiting nursing. J Elder Abuse Negl. 2015;27(1):34–64. 10.1080/08946566.2014.946193
42. Beach SR, Carpenter CR, Rosen T, Sharps P, Gelles R. Screening and detection of elder abuse: research opportunities and lessons learned from emergency geriatric care, intimate partner violence, and child abuse. J Elder Abuse Negl. 2016;28(4-5):185–216. 10.1080/08946566.2016.1229241
43. Rosen T, Elman A, Dion S, Delgado D, Demetres M, Breckman R, et al.; National Collaboratory to Address Elder Mistreatment Project Team. Review of Programs to Combat Elder Mistreatment: Focus on Hospitals and Level of Resources Needed. J Am Geriatr Soc. 2019 Jun;67(6):1286–94. 10.1111/jgs.15773
44. Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al.; US Preventive Services Task Force. Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: US Preventive Services Task Force Final Recommendation Statement. JAMA. 2018 Oct;320(16):1678–87. 10.1001/jama.2018.14741
45. Platts-Mills TF, et al. EM-SART: A Scalable Elder Mistreatment Screening and Response Tool for Emergency Departments. Generations. 2020;44(1):51–8.
Table S1Missing values across all presentations of patients aged ≥65 years during the study period (n = 1450).
| Patients aged ≥65 years, n(%) | ||
| Emergency Severity Index | 6 (0.4%) | |
| Clinical Frailty Scale | 421 (29.0%) | |
| Components of the Emergency Department Senior Abuse Identification tool | ||
| Abbreviated Mental Test-4 | What is your age? | 282 (19.4%) |
| What is your date of birth? | 281 (19.4%) | |
| What is this place? | 282 (19.4%) | |
| What is the year? | 280 (19.3%) | |
| Elder mistreatment questions | 1. Have you needed help with bathing, dressing, shopping, banking or meals? | 268 (18.5%) |
| 2. Has anyone close to you called you names and put you down? | 323 (22.3%) | |
| 3. Has anyone told you that you give them too much trouble? | 323 (22.3%) | |
| 4. Has anyone close to you threatened you or made you feel bad? | 323 (22.3%) | |
| 5. Has anyone tried to force you to sign papers or use your money against your will? | 323 (22.3%) | |
| 6. Has anyone close to you tried to hurt you or harm you? | 324 (22.3%) | |
| Decisions | Judgement of Patient`s ability to report mistreatment | 213 (14.7%) |
| Uncertain if the patient was mistreated and should receive a physical evaluation | 179 (12.3%) | |
| Elder mistreatment suspected | 212 (14.6%) | |
Table S2The baseline characteristics of all patients disaggregated by missing data. Data are presented as medians (interquartile ranges) for continuous variables and numbers (percentages) for categorical variables. No missing data represents all patients included in our analysis. Missing data represents all patients excluded because they were missing part of the Emergency Department Senior Abuse Identification tool.
| All | No missing data | Missing data | |
| n | 1450 | 1071 | 379 |
| Age (years), median (IQR) | 78.00 (72.00–85.00) | 78.00 (72.00–85.00) | 78.00 (71.50–86.00) |
| Sex (female), n (%) | 750 (51.7%) | 548 (51.2%) | 202 (53.3%) |
| Admitted, n (%) | 878 (60.6%) | 625 (58.4%) | 253 (66.8%) |
| National Early Warning Score, median (IQR) | 1 (0–2) | 1 (0–2) | 1 (0–3) |
| Clinical Frailty Scale, median (IQR) | 4 (3–4) | 3 (3–5) | 4 (3–6) |
| 1-day mortality, n (%) | 14 (1.0%) | 4 (0.4%) | 10 (2.6%) |
| 7-day mortality, n (%) | 29 (2.0%) | 7 (0.7%) | 22 (5.8%) |
| 30-day mortality, n (%) | 51 (3.5%) | 17 (1.6%) | 34 (9.0%) |
| In-hospital mortality, n (%) | 35 (2.4%) | 10 (0.9%) | 25 (6.6%) |
IQR: interquartile scale.
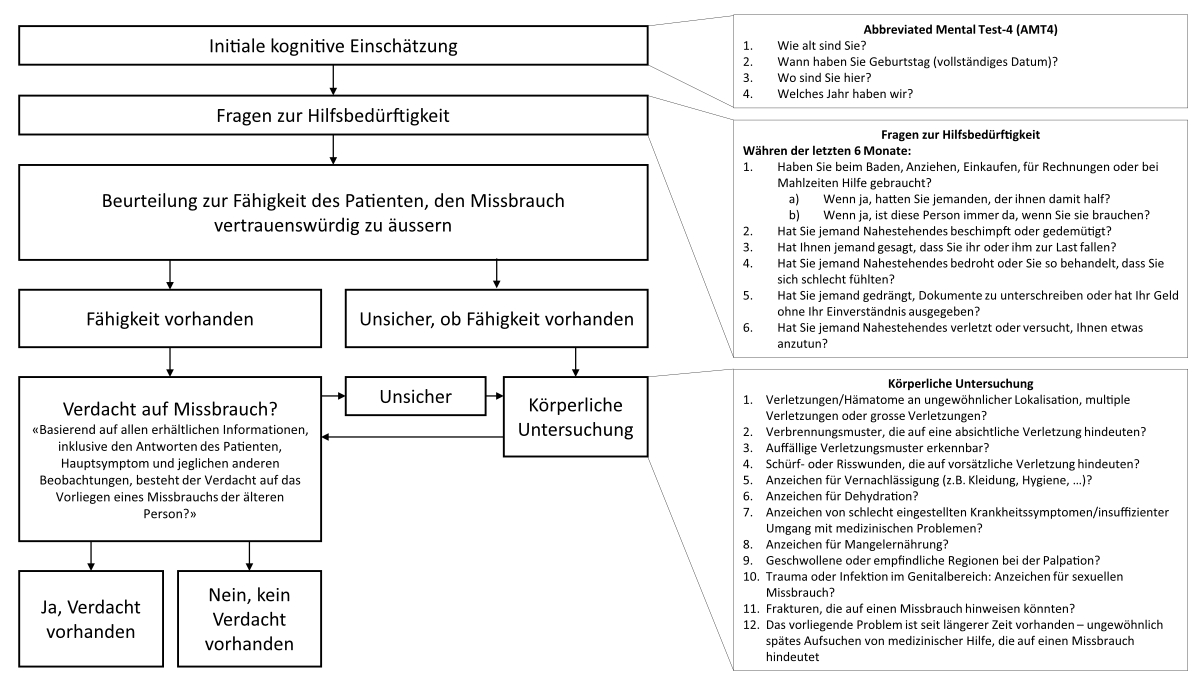
Figure S1The German translation of the Emergency Department Senior Abuse Identification (ED Senior AID) tool. The figure shows the German translation of the ED Senior AID tool used in this study to screen for elder mistreatment in our Swiss tertiary academic urban emergency department.