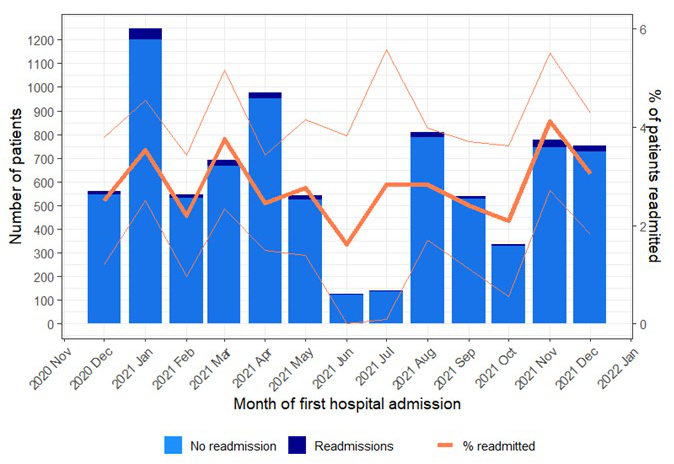
Figure 1Time trends of hospital readmission in CH-SUR. The figure shows the absolute counts of hospitalisations and readmissions on the left scale, and the percentage of readmissions on the right scale, by month of index hospitalisation. The orange line demonstrates the proportion of patients with index hospitalisation in a given month who were subsequently readmitted within 60 days after their discharge.
The characteristics of patients, overall and stratified per readmission status, are detailed in table 1.
Table 1Characteristics of all patients included in the analysis, of patients not readmitted and patients readmitted within 60 days. P-values from Chi-squared tests compare the distributions of variables between these two groups.
| All (n = 8039) | Non-readmitted (n = 7800) | Readmitted (n = 239) | ||
| Age (years) | <65 | 4411 (54.9%) | 4310 (55.3%) | 101 (42.3%) |
| ≥65 | 3628 (45.1%) | 3490 (44.7%) | 138 (57.7%) | |
| Sex | Male | 4385 (54.5%) | 4233 (54.3%) | 152 (63.6%) |
| Female | 3654 (45.5%) | 3567 (45.7%) | 87 (36.4%) | |
| Discharged to home for index hospitalisation | Yes | 6311 (78.5%) | 6106 (78.3%) | 205 (85.8%) |
| No | 1675 (20.8%) | 1643 (21.1%) | 32 (13.4%) | |
| Unknown | 53 (0.7%) | 51 (0.7%) | 2 (0.8%) | |
| Origin for index hospitalisation | Home | 7379 (91.8%) | 7161 (91.8%) | 218 (91.2%) |
| Long-term care | 129 (1.6%) | 123 (1.6%) | 6 (2.5%) | |
| Other hospital | 374 (4.7%) | 367 (4.7%) | 7 (2.9%) | |
| Other | 157 (2.0%) | 149 (1.9%) | 8 (3.3%) | |
| Unknown | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Any IMCU/ICU stay during index hospitalisation | Yes | 1337 (16.6%) | 1314 (16.8%) | 23 (9.6%) |
| No | 6685 (83.2%) | 6469 (82.9%) | 216 (90.4%) | |
| Unknown | 17 (0.2%) | 17 (0.2%) | 0 (0.0%) | |
| COVID-19 immune status (at index hospitalisation)* | Fully immunised | 908 (11.3%) | 869 (11.1%) | 39 (16.3%) |
| Not immunised | 5810 (72.3%) | 5647 (72.4%) | 163 (68.2%) | |
| Partially immunised | 284 (3.5%) | 275 (3.5%) | 9 (3.8%) | |
| Unknown | 1037 (12.9%) | 1009 (12.9%) | 28 (11.7%) | |
| Diabetes | Yes | 1615 (20.1%) | 1568 (20.1%) | 47 (19.7%) |
| No | 6405 (79.7%) | 6213 (79.7%) | 192 (80.3%) | |
| Unknown | 19 (0.2%) | 19 (0.2%) | 0 (0.0%) | |
| Hypertension | Yes | 3381 (42.1%) | 3267 (41.9%) | 114 (47.7%) |
| No | 4632 (57.6%) | 4508 (57.8%) | 124 (51.9%) | |
| Unknown | 26 (0.3%) | 25 (0.3%) | 1 (0.4%) | |
| Cardiovascular disease | Yes | 1940 (24.1%) | 1857 (23.8%) | 83 (34.7%) |
| No | 6071 (75.5%) | 5916 (75.8%) | 155 (64.9%) | |
| Unknown | 28 (0.3%) | 27 (0.3%) | 1 (0.4%) | |
| Renal disease | Yes | 1048 (13.0%) | 1004 (12.9%) | 44 (18.4%) |
| No | 6961 (86.6%) | 6767 (86.8%) | 194 (81.2%) | |
| Unknown | 30 (0.4%) | 29 (0.4%) | 1 (0.4%) | |
| Oncological pathology | Yes | 688 (8.6%) | 645 (8.3%) | 43 (18.0%) |
| No | 7311 (90.9%) | 7119 (91.3%) | 192 (80.3%) | |
| Unknown | 40 (0.5%) | 36 (0.5%) | 4 (1.7%) | |
| Obesity (body mass index ≥30 kg/m2) | Yes | 2212 (27.5%) | 2155 (27.6%) | 57 (23.8%) |
| No | 4499 (56.0%) | 4341 (55.7%) | 158 (66.1%) | |
| Unknown | 1328 (16.5%) | 1304 (16.7%) | 24 (10.0%) | |
| Respiratory disease | Yes | 1266 (15.7%) | 1214 (15.6%) | 52 (21.8%) |
| No | 6742 (83.9%) | 6555 (84.0%) | 187 (78.2%) | |
| Unknown | 31 (0.4%) | 31 (0.4%) | 0 (0.0%) | |
| Immunosuppression** | Yes | 695 (8.6%) | 648 (8.3%) | 47 (19.7%) |
| No | 7313 (91.0%) | 7121 (91.3%) | 192 (80.3%) | |
| Unknown | 31 (0.4%) | 31 (0.4%) | 0 (0.0%) | |
| Any treatment (at index hospitalisation)*** | Yes | 5139 (63.9%) | 4994 (64.0%) | 145 (60.7%) |
| No | 1140 (14.2%) | 1099 (14.1%) | 41 (17.2%) | |
| Unknown | 1760 (21.9%) | 1707 (21.9%) | 53 (22.2%) | |
| Any complication (at index hospitalisation) | Yes | 6500 (80.9%) | 6310 (80.9%) | 190 (79.5%) |
| No | 1500 (18.7%) | 1451 (18.6%) | 49 (20.5%) | |
| Unknown | 39 (0.5%) | 39 (0.5%) | 0 (0.0%) |
ICU: intensive care unit; IMCU: intermediate care unit.
*Full immunisation corresponds to having received all required doses of a vaccine or at least one dose + documented prior SARS-CoV-2 infection. Partial immunisation means having received one dose of a vaccine other than Janssen’s.
**Immunosuppression includes patients who have a haematological, rheumatological or autoimmune pathology with immunosuppression, who receive immunosuppressive treatment, or who are HIV-infected.
***Includes antiviral treatment, antibody treatment and corticosteroid treatment.
Further details of the variable definitions are provided in Appendix A.1.
Further descriptive characteristics specific to the group of readmitted patients are given in table 2.
Table 2Characteristics at readmission among patients rehospitalised within 60 days of discharge.
| Patient characteristics | Readmitted (n = 239) | |
| Time from index discharge to readmission in days, median (interquartile range) | 4 (2–8) | |
| Outcome of readmission | Discharged | 213 (89.1%) |
| Transferred outside CH-SUR | 1 (0.4%) | |
| Died | 21 (8.8%) | |
| Incomplete data | 4 (1.7%) | |
| CURB-65 score at readmission | 0 | 72 (30.1%) |
| 1 | 87 (36.4%) | |
| 2 | 52 (21.8%) | |
| 3+ | 28 (11.7%) | |
| Any IMCU/ICU stay during readmission | Yes | 41 (17.2%) |
| No | 197 (82.4%) | |
| Unknown | 1 (0.4%) | |
| Number of complications (at readmission) | 0 | 29 (12.1%) |
| 1 | 71 (29.7%) | |
| 2 | 65 (27.2%) | |
| 3+ | 72 (30.1%) | |
| Unknown | 2 (0.8%) | |
| Respiratory complication (at readmission) | Yes | 151 (63.2%) |
| No | 85 (35.6%) | |
| Unknown | 3 (1.3%) | |
| Deconditioning syndrome (at readmission) | Yes | 51 (21.3%) |
| No | 184 (77%) | |
| Unknown | 4 (1.7%) | |
| Renal complication (at readmission) | Yes | 31 (13%) |
| No | 205 (85.8%) | |
| Unknown | 3 (1.3%) | |
| Thrombosis complication (at readmission) | Yes | 32 (13.4%) |
| No | 203 (84.9%) | |
| Unknown | 4 (1.7%) | |
| Bacterial complication (at readmission) | Yes | 28 (11.7%) |
| No | 207 (86.6%) | |
| Unknown | 4 (1.7%) | |
| Any complication (at readmission) | Yes | 208 (87.0%) |
| No | 29 (12.1%) | |
| Unknown | 2 (0.8%) | |
ICU: intensive care unit; IMCU: intermediate care unit.
Figure 2 shows the overall cumulative incidence functions of readmission. Stratified cumulative incidence functions of readmission within 60 days can be found in Appendix A.2. Overall, 50% of the readmissions occurred within four days and 80% of the readmissions within ten days after index discharge.
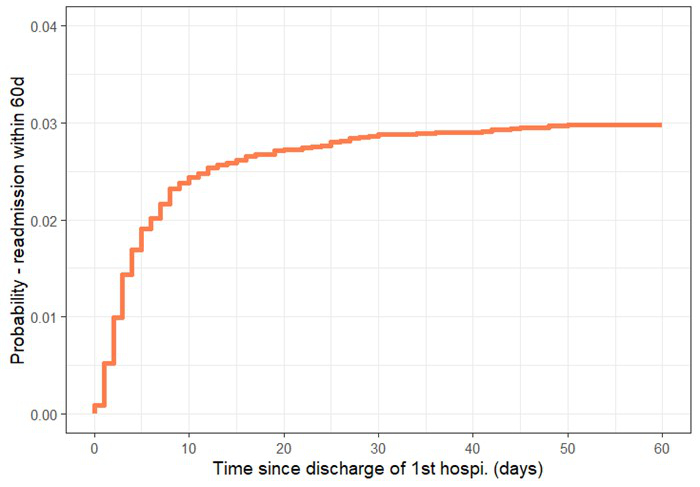
Figure 2Cumulative incidence function for hospital readmission – overall.
Figure 3 shows the distribution of time to hospital readmission, stratified per index hospitalisation duration. Among the readmitted patients, the median time to readmission was shorter for those with an index hospitalisation duration of <5 days (median of 3 days, IQR 2–4 days) than for those with an index hospitalisation duration of 5 days or longer.
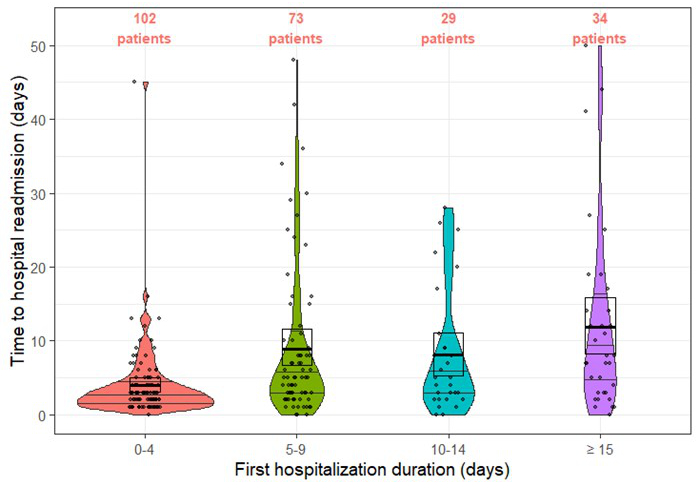
Time to hospital readmission as a function of the duration of the index hospitalisation. The shape of each plot presents the frequency of patients with a given number of days between the discharge and rehospitalisation; the box shows the median and interquartile range. Numbers in orange at the top of the figure are the number of patients readmitted for the considered index duration.
Overall 17.2% of the readmitted patients spent time in the IMCU/ICU during the subsequent hospitalisation, compared to 16.6% for the index hospitalisations among all patients. In total, 87.0% of the readmitted patients showed at least one complication during the readmission stay, and the most common complications were: respiratory complications (63.2%), deconditioning syndrome (21.3%) and thrombosis complications (13.4%) (table 2). The case fatality ratio was 9.2% (95% CI 8.6–9.7%) during the index hospitalisation and 7.1% (95% CI 3.9–10.4%) during rehospitalisation (p = 0.72).
Among the 151 patients who were readmitted and had respiratory complications at readmission, 95 (62.9%) had the same CURB-65 score at the index hospitalisation and at readmission, 37 (24.5%) had a higher CURB-65 score at readmission and 19 (12.6%) had a lower CURB-65 score at readmission (figure 4).
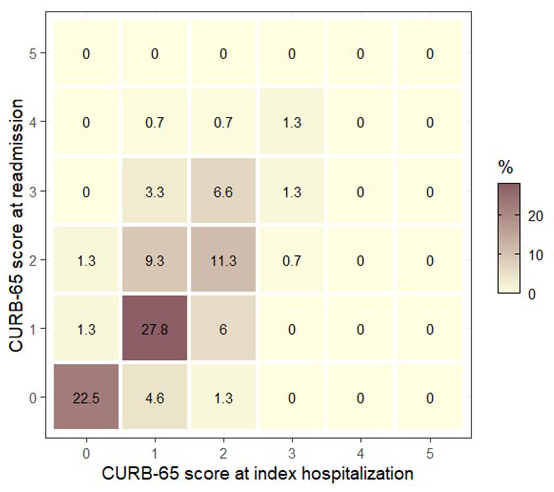
Figure 4Comparison of the severity scores at index hospitalisation and at readmission, for the patients readmitted with respiratory complications (n = 151).
Risk factors for hospital readmission within CH-SUR
Table 3 shows the odds ratios (ORs) for hospital readmission within 60 days in CH-SUR, with 95% confidence intervals (95% CIs), from the univariable logistic regression.
Table 3Odds ratios with 95% confidence intervals (95% CI) from univariable logistic regression.
| Variable | Odds ratio (95% CI) | p-value | |
| Age (years) | <65 | 1 (ref) | <0.0001 |
| ≥65 | 1.69 (1.30–2.19) | ||
| Sex | Male | 1 (ref) | 0.004 |
| Female | 0.68 (0.52–0.89) | ||
| Discharged to home for index hospitalisation | No | 1 (ref) | 0.003 |
| Yes | 1.72 (1.18–2.51) | ||
| Any IMCU/ICU stay during index hospitalisation | No | 1 (ref) | 0.002 |
| Yes | 0.52 (0.34–0.81) | ||
| COVID-19 immune status (at index hospitalisation) | Not immunised | 1 (ref) | 0.07 |
| Fully immunised | 1.55 (1.09–2.22) | ||
| Partially immunised | 1.13 (0.57–2.24) | ||
| Diabetes | No | 1 (ref) | 0.85 |
| Yes | 0.97 (0.70–1.34) | ||
| Hypertension | No | 1 (ref) | 0.07 |
| Yes | 1.27 (0.98–1.64) | ||
| Cardiovascular disease | No | 1 (ref) | 0.0002 |
| Yes | 1.71 (1.30–2.24) | ||
| Renal disease | No | 1 (ref) | 0.02 |
| Yes | 1.53 (1.09–2.13) | ||
| Oncological pathology | No | 1 (ref) | <0.00001 |
| Yes | 2.47 (1.76–3.47) | ||
| Obesity | No | 1 (ref) | 0.04 |
| Yes | 0.73 (0.53–0.99) | ||
| Respiratory disease | No | 1 (ref) | 0.01 |
| Yes | 1.50 (1.10–2.05) | ||
| Immunosuppression | No | 1 (ref) | <0.00001 |
| Yes | 2.69 (1.94–3.74) | ||
| Any treatment (at index hospitalisation) | No | 1 (ref) | 0.17 |
| Yes | 0.78 (0.55–1.11) | ||
ICU: intensive care unit; IMCU: intermediate care unit.
Please refer to table 1 and Appendix A.1 for a detailed explanation of the variables.
The model with the same eight covariables (oncological pathology, obesity, immunosuppression and any treatment, in addition to age, sex, discharge to home and ICU/IMCU stay) produced the lowest values for both AIC and SBIC and was therefore selected for the multivariable analysis. Table 4 shows the ORs and 95% CIs for hospital readmission within 60 days, from the multivariable logistic regression models using either the imputed dataset or the complete cases dataset. Of note, when limiting to cases with complete follow-up information in the multivariable analysis, the number of included patients dropped from 8039 to 5161, with 163 (3.2%) readmissions within 60 days after discharge of index hospitalisation.
Table 4Odds ratios with 95% confidence intervals (95% CI) from multivariable logistic regression on imputed data (mice), and multivariable logistic regression on complete cases (cc).
| Multivariable (mice) | Multivariable (cc) | ||||
| Variable | Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value | |
| Age (years) | <65 | 1 (ref) | 0.0005 | 1 (ref) | 0.0006 |
| ≥65 | 1.63 (1.24–2.15) | 1.55 (1.11–2.16) | |||
| Sex | Male | 1 (ref) | 0.005 | 1 (ref) | 0.06 |
| Female | 0.68 (0.52–0.89) | 0.75 (0.53–1.04) | |||
| Discharged to home for index hospitalisation | No | 1 (ref) | 0.005 | 1 (ref) | 0.002 |
| Yes | 1.77 (1.19–2.62) | 1.68 (1.08–2.69) | |||
| Any IMCU/ICU stay during index hospitalisation | No | 1 (ref) | 0.08 | 1 (ref) | 0.09 |
| Yes | 0.67 (0.43–1.05) | 0.74 (0.45–1.18) | |||
| Oncological pathology | No | 1 (ref) | 0.001 | 1 (ref) | <0.00001 |
| Yes | 1.82 (1.27–2.61) | 2.11 (1.37–3.16) | |||
| Obesity | No | 1 (ref) | 0.46 | 1 (ref) | 0.04 |
| Yes | 0.89 (0.65–1.22) | 0.73 (0.50–1.04) | |||
| Immunosuppression | No | 1 (ref) | <0.00001 | 1 (ref) | 0.001 |
| Yes | 2.34 (1.67–3.29) | 2.09 (1.36–3.12) | |||
| Any treatment (at index hospitalisation) | No | 1 (ref) | 0.21 | 1 (ref) | 0.34 |
| Yes | 0.80 (0.56–1.14) | 0.82 (0.56–1.24) | |||
ICU: intensive care unit; IMCU: intermediate care unit.
Based on our multivariable logistic regression models, factors increasing the odds of hospital readmission were age of 65 years or older (OR 1.63, 95% CI 1.24–2.15, p <0.001), being discharged to home at the end of the index hospitalisation (OR 1.77, 95% CI 1.19–2.62, p = 0.004), presence of oncological pathology (OR 1.82, 95% CI 1.27–2.61, p = 0.001) and immunosuppression (OR 2.34, 95% CI 1.67–3.29, p <0.00001). Females had lower odds of hospital readmission than males (OR 0.68, 95% CI 0.52–0.89, p = 0.005). Being admitted at least once to the IMCU/ICU during the index hospitalisation, obesity and receiving any treatment during the index hospitalisation were found to have no significant impact on the risk of hospital readmission.
The collinearity check revealed some collinearity particularly between age and other variables, but the results of the model omitting age did not essentially differ from those of the main analysis (Appendix A.3). We also conducted an analysis stratified by age (<65 vs ≥65 years) to test whether the lower readmission rate among patients who stayed at the IMCU or ICU during the index hospitalisation could be related to the younger age of these patients. The odds ratios did however not essentially differ between the two age groups, although there were some minor differences: discharge was no longer significantly associated with rehospitalisation in the younger age group, and immunosuppression was not associated with rehospitalisation in the older age group (Appendix A.3).
Discussion
In this study using Swiss COVID-19 Hospital-Based Surveillance (CH-SUR) data, we assessed the risk of hospital readmission within 60 days among COVID-19 patients discharged alive from the hospital, and investigated the risk factors for hospital readmission. Between December 2020 and December 2021, the rate of hospital readmission within 60 days among COVID-19 patients was 3.2%, with little variation observed over that time period (ranging from 1.6% to 4.6%).
Due to the growing recognition of COVID-19’s medium- and long-term health consequences, there has been significant interest in studying the post-discharge trajectory of COVID-19 patients. Reported readmission rates range between 4% [21] and 9% [13] from large sample studies in Spain and the United States, respectively, with readmissions occurring typically within the first week post-discharge. Respiratory distress was identified as the most common reason for readmission [22]. Other reasons for readmission included: pain, altered mental status, fall, fever, soft tissue infection, thrombotic event and gastrointestinal symptoms [7, 21–25]. We observed lower readmission rates than those reported previously in a systematic review [26]. However, most of the studies included were based on data collected in 2020, during the first months of the COVID-19 pandemic, when the understanding of COVID-19 and its management were still limited. Case management of hospitalised patients drastically changed with the results of the first large clinical trials during summer 2020 and the broader use of immunomodulatory drugs in patients with severe disease [27]. The disease itself and its management evolved from the beginning of the pandemic. New variants of COVID-19 appeared and co-existed, changing disease severity. The vaccine policy kept evolving, with new vaccine doses being administered to preserve immunity, leading to a beneficial impact on recovery.
The time from index hospitalisation discharge to readmission was relatively short, with a median time of four days. This may indicate that hospital readmissions within CH-SUR generally occur early enough to avoid a severe degradation of the status of the patient. We found that most of the readmitted patients had similar severity scores at index admission and at readmission. The in-hospital case fatality ratio was found to be slightly lower, although not significantly, after hospital readmission than at the end of index hospitalisation. Post-discharge, this short time span between index hospitalisation discharge and readmission could justify short-term medical surveillance for at-risk patients (males, with comorbidities, older than 65) in order to identify as quickly as possible any complication which would require further hospitalisation.
As previously reported by others [13, 14, 28], male sex and age of 65 years or over were found to increase the risk of hospital readmission within CH-SUR. Differences in the effects of COVID-19 by sex and age have been evidenced by several studies, with older patients as well as male patients being generally associated with a worse outcome [18]. This unbalanced sex-associated risk could relate to the difference in immune response to the SARS-CoV-2 virus between men and women [29,30], but it could also be associated with the higher prevalence among men than women of chronic diseases known to be COVID-19 risk factors. Likewise, the elderly population is known to have a reduced immune response, and to more likely present comorbidities that are risk factors for COVID-19 adverse events [18].
Patients with chronic cardiovascular diseases as well as immunocompromised patients had a significantly higher risk of hospital readmission compared to those without such comorbidities. Similar results have been demonstrated in other studies [21,31]. Immunosuppression, as defined in CH-SUR and in other studies, encompasses a wide range of immune dysfunctions and the risk may vary within this group. It is particularly worth noting that our definition considered all HIV-infected individuals as immunocompromised, although at present most individuals diagnosed with HIV in Switzerland are virally suppressed and with good immunological response. The increased risk of hospital readmission among patients with oncological diseases may partly be related to their immunosuppressive treatments. Another study on patients in the United States revealed significantly higher rates of cancer among readmitted compared with non-readmitted patients [32]. According to the univariable analysis, the risk of readmission was also not different among patients suffering from chronic respiratory diseases and chronic renal diseases compared to those without, similarly to other studies [33]. However, these variables were left out from the multivariable analysis as they were not considered to add information to the model.
Patients with an initially short index hospital stay had a significantly higher risk of being readmitted [14, 22]. This seems to be a common observation once sufficient sample size is considered [34]. Others describe the disease course as a biphasic phenomenon starting with a mild clinical presentation, allowing for discharge, and later evolving into a worsened state [32]. Early discharge can also be frequent in moments of hospital saturation when resources are insufficient to handle the number of patients [14]. It is known that hasty discharges before the severity peak or complete recovery favour readmissions [35]. Readmissions could also relate to post-discharge care systems. In some health facilities, management of patients after discharge can be poorer than preventive hospital measures [14]. Although administrative prioritisations aim to reduce both length of stay and readmissions, these two goals seem inversely related [22].
Discharge to home at the end of the index hospitalisation was a risk for readmission compared to discharge to medical facilities (long-term care, rehabilitation, etc.), as opposed to other findings [9, 13, 36], all based in the United States, where readmission was less frequent among patients discharged to home. In the Netherlands [6], discharge to long-term care facilities increased the risk of hospital readmission. Reasons for such differences can reside in the low-level individual differences between hospitals’ discharge decisions [37] or in the high-level differences between countries’ medical care systems. In an analysis of the health systems for Switzerland and the Netherlands [38], Switzerland’s system was described as more successful in its adaptation to changing societal constraints. Within Switzerland, quality of rehabilitation and intermediate-care facilities is ensured through an association, SwissREHA, accounting for more than 50% of all rehabilitation beds in the country [39]. As a possible proxy for COVID-19 rehabilitation, stroke rehabilitation was shown [40] to be conducted more efficiently in Switzerland than in the United States. Further studies accounting for insurance coverage of patients [14], governance and financing of healthcare systems and societal factors are necessary to learn more about this aspect.
Patients who were admitted to the IMCU or ICU during the index hospitalisation had a slightly lower risk of readmission, although the association was not statistically significant. Several other studies also found no significant association [14]. The first justification resides in a statistical bias. Due to a higher in-hospital death rate for those patients admitted to IMCU/ICU (20.2% compared to 9.1% for patients not admitted to IMCU/ICU), the readmission population is biased towards having fewer IMCU/ICU-admitted patients because a substantial proportion of them have already died during the index hospitalisation. The second explanation is that ICU admission is related to illness severity and cautions practitioners against a preemptive discharge [22]. In our data, more than 80% of patients who did not spend time in the IMCU/ICU during the index hospitalisation were discharged to home, whereas it reduced to about 40% for patients who were admitted to the IMCU/ICU.
This study investigated the effect of the immunisation status on readmission odds and concluded that there was no significant effect. From a data perspective, the proportion of patients with unknown outcome for their index hospitalisation was 6.0% overall, but the missing data rose to 10.5% when focusing on patients fully immunised. The dataset was biased towards reflecting the outcomes of patients not or partially immunised, possibly because incomplete immunisation is viewed by the practitioners as a risk factor for COVID-19 severity or recurrence. High-risk, unvaccinated patients were more likely to die in hospital and therefore would be excluded from readmission analysis, while high-risk, vaccinated individuals were more likely to survive and contribute to the analysis [43]. It is important to take into consideration the specific vaccination context of Switzerland over the year 2021. In the first six months of 2021, people at high risk of severe COVID-19 (elderly, vulnerable and immunosuppressed individuals) were vaccinated in priority: a non-negligible part of them were less prone to respond to the vaccine. Then it became clear during the last six months of the year that elderly people who did not get their booster doses were also at greater risk of severe disease caused by the Delta variant (the Delta variant became dominant in Switzerland in July 2021). Considering the previously demonstrated vaccine efficacy and the described vaccination strategy in Switzerland during the study period, the study tends to report risk factors for readmission for lower-risk unvaccinated patients and higher-risk vaccinated patients.
Limitations
The limitations of this analysis resided in its observational nature and its imputed data. The reason for readmission was not recorded in our database, limiting the understanding of risk factors. Data on competing events such as death after discharge was not available for most patients: therefore, we were unable to perform a time-to-event analysis, and the probability of rehospitalisation may be slightly biased. The study may in general be subject to some selection bias: for example, certain patients such as those admitted to the ICU or IMCU, and those without proper immunisation, were at higher risk of death and thus exclusion, which may impact the association of these variables with rehospitalisation. There may also be differences in patient characteristics between the centres that the analysis did not control for. The definitions of some variables were not optimal, for example immunocompromised patients also include HIV-infected individuals under successful antiretroviral therapy. We had to restrict the study period to one year given that the collection and definition of variables evolved substantially over time. Therefore we were not able to include the early stages of the pandemic, nor the later waves dominated by the Omicron variant. Age was identified as having strong collinearity with many other risk factors; however the analysis removing the age variable did not change the significance of the risk factors presented above (see Appendix A.3).
Conclusion
We showed that older age, male sex, immunosuppression, discharge to home instead of a facility and oncological pathology were the main risk factors for hospital readmission identified within the CH-SUR Swiss-based surveillance system. Our findings can support the development and implementation of efficient patient management strategies for discharge, as well as support services and coordinated care networks such as post-discharge telehealth monitoring, to mitigate the risk of readmission. Moreover, further studies including immunisation status for the high-risk groups and other socioeconomic factors of patients could bring further elements to fully understand the hospital readmission dynamics among COVID-19 patients.
Acknowledgments
To everyone (former and current) involved in the CH-SUR project, especially to all the study nurses for data entry and administrative coordination.
Notes
The analyses incorporated in this paper were supported by the Swiss Federal Office of Public Health, the Swiss National Science Foundation (grant No 31CA30_196270 to Olivia Keiser) and the European Union’s Horizon Europe research and innovation programme (grant agreement No 101046314).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
References
1.COVID-19 Hospitalizations. Available at: https://gis.cdc.gov/grasp/covidnet/covid19_3.html. Accessed 30 May 2022.
2.OFSP O fédéral de la santé publique. Coronavirus: monitorage. Available at: https://www.bag.admin.ch/bag/fr/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international/monitoring.html. Accessed 10 June 2022.
3.Sun BC, Hsia RY, Weiss RE, Zingmond D, Liang LJ, Han W, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013 Jun;61(6):605–611.e6. [cited 2022 Jun 22] Available from: https://linkinghub.elsevier.com/retrieve/pii/S019606441201699X doi: https://doi.org/10.1016/j.annemergmed.2012.10.026
4.Coffey LW. Savage, et al. Interventions to Promote Early Discharge and Avoid Inappropriate Hospital (Re)Admission: A Systematic Review. International Journal of Environmental Research and Public Health 2019; 16:2457. Available at: https://www.mdpi.com/1660-4601/16/14/2457. Accessed 22 June 2022.
5.Felix HC, Seaberg B, Bursac Z, Thostenson J, Stewart MK. Why do patients keep coming back? Results of a readmitted patient survey. Soc Work Health Care. 2015;54(1):1–15. [cited 2022 May 30]
6.Leijte WT, Wagemaker NM, van Kraaij TD, de Kruif MD, Mostard GJ, Leers MP, et al. [Mortality and re-admission after hospitalization with COVID-19]. Ned Tijdschr Geneeskd. 2020 Nov;164:D5423.
7.Wang X, Zhou Y, Jiang N, Zhou Q, Ma WL. Persistence of intestinal SARS-CoV-2 infection in patients with COVID-19 leads to re-admission after pneumonia resolved. Int J Infect Dis. 2020 Jun;95:433–5. [cited 2022 Jun 22] Available from: https://linkinghub.elsevier.com/retrieve/pii/S1201971220302794 doi: https://doi.org/10.1016/j.ijid.2020.04.063
8.UyaroĞlu OA, BaŞaran NÇ, ÖziŞik L, Dİzman GT, EroĞlu İ, Şahİn TK, et al. Thirty-day readmission rate of COVID-19 patients discharged from a tertiary care university hospital in Turkey: an observational, single-center study. Int J Qual Health Care. 2021 Feb;33(1):mzaa144. [cited 2022 Jun 22] Available from: https://academic.oup.com/intqhc/article/doi/10.1093/intqhc/mzaa144/5940459
9.Yeo I, Baek S, Kim J, Elshakh H, Voronina A, Lou MS, et al. Assessment of thirty-day readmission rate, timing, causes and predictors after hospitalization with COVID-19. J Intern Med. 2021 Jul;290(1):157–65. [cited 2022 Jun 22] Available from: https://onlinelibrary.wiley.com/doi/10.1111/joim.13241
10.Banerjee J, Canamar CP, Voyageur C, Tangpraphaphorn S, Lemus A, Coffey C Jr, et al. Mortality and Readmission Rates Among Patients With COVID-19 After Discharge From Acute Care Setting With Supplemental Oxygen. JAMA Netw Open. 2021 Apr;4(4):e213990. [cited 2022 Jun 22] Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2778078 doi: https://doi.org/10.1001/jamanetworkopen.2021.3990
11.Yang Z, Chen X, Huang R, Li S, Lin D, Yang Z, et al. Atypical presentations of coronavirus disease 2019 (COVID-19) from onset to readmission. BMC Infect Dis. 2021 Jan;21(1):127. [cited 2022 Jun 22] Available from: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05751-8
12.Chaudhry Z, Shawe-Taylor M, Rampling T, Cutfield T, Bidwell G, Chan XH, et al. Short durations of corticosteroids for hospitalised COVID-19 patients are associated with a high readmission rate. J Infect. 2021 Jun;82(6):276–316. [cited 2022 Jun 22] Available from: https://linkinghub.elsevier.com/retrieve/pii/S0163445321001158 doi: https://doi.org/10.1016/j.jinf.2021.03.002
13.Lavery AM, Preston LE, Ko JY, Chevinsky JR, DeSisto CL, Pennington AF, et al. Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020 Nov;69(45):1695–9. [cited 2022 Jun 22] Available from: http://www.cdc.gov/mmwr/volumes/69/wr/mm6945e2.htm?s_cid=mm6945e2_w doi: https://doi.org/10.15585/mmwr.mm6945e2
14.Jeon WH, Seon JY, Park SY, Oh IH. Analysis of Risk Factors on Readmission Cases of COVID-19 in the Republic of Korea: Using Nationwide Health Claims Data. Int J Environ Res Public Health. 2020 Aug;17(16):5844. [cited 2022 Jun 22] Available from: https://www.mdpi.com/1660-4601/17/16/5844 doi: https://doi.org/10.3390/ijerph17165844
15.Ye S, Hiura G, Fleck E, Garcia A, Geleris J, Lee P, et al. Hospital Readmissions After Implementation of a Discharge Care Program for Patients with COVID-19 Illness. J Gen Intern Med. 2021 Mar;36(3):722–9. [cited 2022 Jun 22] Available from: https://link.springer.com/10.1007/s11606-020-06340-w
16.Thiabaud A, Iten A, Balmelli C, Senn L, Troillet N, Widmer A, et al. Cohort profile: SARS-CoV-2/COVID-19 hospitalised patients in Switzerland. Swiss Med Wkly. 2021 Feb;151(708):w20475. [cited 2022 Jun 22] Available from: https://doi.emh.ch/smw.2021.20475 doi: https://doi.org/10.4414/smw.2021.20475
17.Hospital-based surveillance of COVID-19 in Switzerland. 2020; Available at: https://www.unige.ch/medecine/hospital-covid/. Accessed 30 April 2021.
18.Maximiano Sousa F, Roelens M, Fricker B, Thiabaud A, Iten A, Cusini A, et al.; Ch-Sur Study Group. Risk factors for severe outcomes for COVID-19 patients hospitalised in Switzerland during the first pandemic wave, February to August 2020: prospective observational cohort study. Swiss Med Wkly. 2021 Jul;151(2930):w20547. [cited 2021 Sep 27] Available from: https://smw.ch/article/doi/smw.2021.20547 doi: https://doi.org/10.4414/smw.2021.20547
19.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007 May;26(11):2389–430. [cited 2022 Jun 22] Available from: https://onlinelibrary.wiley.com/doi/10.1002/sim.2712
20.van Buuren S, Groothuis-Oudshoorn K. Mice : Multivariate Imputation by Chained Equations in r. J Stat Softw. 2011;45(3):1–67. [cited 2022 Jun 22] Available from: http://www.jstatsoft.org/v45/i03/ doi: https://doi.org/10.18637/jss.v045.i03
21.Parra LM, Cantero M, Morrás I, Vallejo A, Diego I, Jiménez-Tejero E, et al.; Puerta de Hierro Hospital Admission Study Group. Hospital Readmissions of Discharged Patients with COVID-19. Int J Gen Med. 2020 Dec;13:1359–66. [cited 2022 Jun 22] Available from: https://www.dovepress.com/hospital-readmissions-of-discharged-patients-with-covid-19-peer-reviewed-article-IJGM doi: https://doi.org/10.2147/IJGM.S275775
22.Somani SS, Richter F, Fuster V, De Freitas JK, Naik N, Sigel K, et al.; Mount Sinai COVID Informatics Center. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization for COVID-19. J Gen Intern Med. 2020 Oct;35(10):2838–44. [cited 2022 Jun 22] Available from: https://link.springer.com/10.1007/s11606-020-06120-6
23.Li XJ, Zhang ZW, Zong ZY. A case of a readmitted patient who recovered from COVID-19 in Chengdu, China. Crit Care. 2020 Apr;24(1):152. [cited 2022 May 30]
24.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al.; the Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020 May;323(20):2052–9. [cited 2022 May 30]
25.Wang H, Li Y, Wang F, Du H, Lu X. Rehospitalization of a Recovered Coronavirus Disease 19 (COVID-19) Child With Positive Nucleic Acid Detection. Pediatr Infect Dis J. 2020 Jun;39(6):e69–70. [cited 2022 May 30] Available from: https://journals.lww.com/pidj/Fulltext/2020/06000/Rehospitalization_of_a_Recovered_Coronavirus.21.aspx doi: https://doi.org/10.1097/INF.0000000000002690
26.Loo WK, Hasikin K, Suhaimi A, Yee PL, Teo K, Xia K, et al. Systematic Review on COVID-19 Readmission and Risk Factors: Future of Machine Learning in COVID-19 Readmission Studies. Front Public Health. 2022 May;10:898254. [cited 2022 Jun 22] Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.898254/full
27.Siemieniuk RA, Bartoszko JJ, Zeraatkar D, Kum E, Qasim A, Martinez JP, et al. Drug treatments for covid-19: living systematic review and network meta-analysis. BMJ. 2020 Jul;370:m2980. [cited 2022 Jul 27] Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.m2980
28.Ramos-Martínez A, Parra-Ramírez LM, Morrás I, Carnevali M, Jiménez-Ibañez L, Rubio-Rivas M, et al. Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients. Sci Rep. 2021 Jul;11(1):13733. [cited 2022 Jun 22] Available from: http://www.nature.com/articles/s41598-021-93076-0 doi: https://doi.org/10.1038/s41598-021-93076-0
29.Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al.; Yale IMPACT Research Team. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020 Dec;588(7837):315–20. [cited 2022 Jun 22] Available from: https://www.nature.com/articles/s41586-020-2700-3 doi: https://doi.org/10.1038/s41586-020-2700-3
30.Walter LA, McGregor AJ. Sex- and Gender-specific Observations and Implications for COVID-19. West J Emerg Med. 2020 Apr;21(3):507–9. [cited 2022 Jun 22] Available from: https://escholarship.org/uc/item/76f9p924 doi: https://doi.org/10.5811/westjem.2020.4.47536
31.Verna EC, Landis C, Brown RS Jr, et al. Factors Associated with Readmission in the US Following Hospitalization with COVID-19. 2021; ciab464. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8240865/. Accessed 31 March 2022.
32.Atalla E, Kalligeros M, Giampaolo G, Mylona EK, Shehadeh F, Mylonakis E. Readmissions among patients with COVID-19. Int J Clin Pract. 2021 Mar;75(3):e13700. [cited 2022 Jun 22] Available from: https://onlinelibrary.wiley.com/doi/10.1111/ijcp.13700
33.Townsend L, Dowds J, O’Brien K, Sheill G, Dyer AH, O’Kelly B, et al. Persistent Poor Health after COVID-19 Is Not Associated with Respiratory Complications or Initial Disease Severity. Ann Am Thorac Soc. 2021 Jun;18(6):997–1003. [cited 2022 Jun 22] Available from: https://www.atsjournals.org/doi/10.1513/AnnalsATS.202009-1175OC
34.Subramaniam A, Lim ZJ, Ponnapa Reddy M, Shekar K. Systematic review and meta-analysis of the characteristics and outcomes of readmitted COVID-19 survivors. Intern Med J. 2021 Nov;51(11):1773–80. [cited 2022 Jun 22] Available from: https://onlinelibrary.wiley.com/doi/10.1111/imj.15350
35.Xiao AT, Tong YX, Zhang S. False negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J Med Virol. 2020 Oct;92(10):1755–6. [cited 2022 Jun 22] Available from: https://onlinelibrary.wiley.com/doi/10.1002/jmv.25855
36.Huang CW, Desai PP, Wei KK, Liu IA, Lee JS, Nguyen HQ. Characteristics of patients discharged and readmitted after COVID-19 hospitalisation within a large integrated health system in the United States. Infect Dis (Lond). 2021 Oct;53(10):800–4. [cited 2022 Jun 22] Available from: https://www.tandfonline.com/doi/full/10.1080/23744235.2021.1924398
37.Krumholz HM, Wang K, Lin Z, Dharmarajan K, Horwitz LI, Ross JS, et al. Hospital-Readmission Risk - Isolating Hospital Effects from Patient Effects. N Engl J Med. 2017 Sep;377(11):1055–64. [cited 2022 Jun 22] Available from: http://www.nejm.org/doi/10.1056/NEJMsa1702321
38.Okma KG, Cheng T, Chinitz D, Crivelli L, Lim M, Maarse H, et al. Six Countries, Six Health Reform Models? Health Care Reform in Chile, Israel, Singapore, Switzerland, Taiwan and The Netherlands. J Comp Policy Anal. 2010;12(1-2):75–113. [cited 2022 Jun 22] Available from: http://www.tandfonline.com/doi/abs/10.1080/13876980903076237
39.WHO. Switzerland: Health system review. Available at: https://apps.who.int/iris/handle/10665/330252. Accessed 10 June 2022.
40.Stuart M, Ryser C, Levitt A, Beer S, Kesselring J, Chard S, et al. Stroke rehabilitation in Switzerland versus the United States: a preliminary comparison. Neurorehabil Neural Repair. 2005 Jun;19(2):139–47. [cited 2022 Jun 22] Available from: http://journals.sagepub.com/doi/10.1177/1545968305277088
41.Akbari A, Fathabadi A, Razmi M, Zarifian A, Amiri M, Ghodsi A, et al. Characteristics, risk factors, and outcomes associated with readmission in COVID-19 patients: A systematic review and meta-analysis. Am J Emerg Med. 2022 Feb;52:166–73. [cited 2022 Jun 22] Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735675721009827 doi: https://doi.org/10.1016/j.ajem.2021.12.012
42.Nematshahi M, Soroosh D, Neamatshahi M, Attarian F, Rahimi F. Factors predicting readmission in patients with COVID-19. BMC Res Notes. 2021 Sep;14(1):374. [cited 2022 Jun 22] Available from: https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-021-05782-7
43. McAlister FA, MMath YD, MHSc AC, et al. The risk of death or unplanned readmission after discharge from a COVID-19 hospitalization in Alberta and Ontario. 2022; 194:8.
Appendix
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3773.