Core stories of physicians on a Swiss internal medicine ward during the first COVID-19
wave: a qualitative exploration
DOI: https://doi.org/https://doi.org/10.57187/s.3760
Vanessa Kraegea,
Amaelle Gavinb,
Julieta Norambuenac,
Friedrich Stiefeld*,
Marie Méane*,
Céline Bourquind*
a Division of Internal medicine, Medical Directorate
and Innovation and Clinical Research Directorate, Lausanne University Hospital,
Lausanne, Switzerland
b Psychiatric Liaison Service, Lausanne
University Hospital, Lausanne, Switzerland
c Division of Internal medicine, Lausanne
University Hospital, Lausanne,Switzerland
d Psychiatric
Liaison Service, Lausanne University Hospital, and University of Lausanne, Lausanne,
Switzerland
e Division
of Internal medicine, Lausanne University Hospital, and University of Lausanne,
Lausanne, Switzerland
* This authors contributed
equally as co-last authors
Summary
INTRODUCTION: The first COVID-19 wave (2020), W1, will remain extraordinary due to
its novelty and the uncertainty on how to handle the pandemic. To understand
what physicians went through, we collected narratives of frontline physicians
working in a Swiss university hospital during W1.
METHODS: Physicians in the Division of Internal Medicine of Lausanne
University Hospital (CHUV) were invited to send anonymous narratives to an
online platform, between 28 April and 30 June 2020. The analysed material
consisted of 13 written texts and one audio record. They were examined by means
of a narrative analysis based on a holistic content approach, attempting to
identify narrative highlights, referred to as foci, in the texts.
RESULTS: Five main foci were identified: danger and threats, acquisition of
knowledge and practices, adaptation to a changing context, commitment to the
profession, and sense of belonging to the medical staff. In physicians’
narratives, danger designated
a variety of rather negative feelings and emotions, whereas threats were experienced as being
dangerous for others, but also for oneself. The acquisition of knowledge and practices focus referred to the
different types of acquisition that took place during W1. The narratives that
focused on adaptation reflected how physicians coped with W1 and private
or professional upheavals. COVID-19 W1 contributed to revealing a natural commitment
(or not) of physicians towards the profession and patients, accompanied by the
concern of offering the best possible care to all. Lastly, sense of
belonging referred to the team and its reconfiguration during W1.
CONCLUSIONS: Our study deepens the understanding of how physicians experienced
the pandemic both in their professional and personal settings. It offers
insights into how they prepared and reacted to a pandemic. The foci reflect
topics that are inherent to a physician’s profession, whatever the context. During
a pandemic, these foundational elements are particularly challenged.
Strikingly, these topics are not studied in medical school, thus raising the
general question of how students are prepared for the medical profession.
Introduction
Physicians work in an emotionally demanding
and stressful environment [1, 2], with a
lower overall quality of life compared to the general population [2–7]. Over the last
decades, studies have
shown an alarming decrease in physicians’ wellbeing [2, 3, 8, 9], which also impacts
quality and functioning of
healthcare [10–12].
The rise in health emergencies caused by
viral outbreaks such as SARS (2002), H1N1 influenza (2009–2010) and COVID-19 (since
2020) has shown that physicians involved in crisis response are particularly
exposed. Depending on the intensity of the upheaval, they can subsequently
suffer from psychological disorders [13–17].
If not properly apprehended, these disorders can become chronic [13, 14, 18]. Previous
studies have attempted
to identify stressors and coping strategies for healthcare professionals’
mental health during viral outbreaks [13, 14,
16, 19–24]. These studies mostly used multiple-choice questionnaires or
standardised forms focusing on specific outcomes, such as prevalence of
post-traumatic stress disorder [20, 25]
or coping strategies [26], burnout [20, 25, 26], anxiety or depressive symptoms
(HADS) [25], leaving little room for the
expression of personal experiences.
The first COVID-19 wave (2020), W1, will
remain extraordinary due to its novelty, the uncertainties it brought about how
to handle the pandemic and the societal upheavals it caused. Despite the
importance of comprehending what physicians and other healthcare professionals
went through, only very few qualitative studies were conducted across the
world.
We hereby briefly summarise the results of
relevant studies with regard to ours. At the very beginning of the pandemic
(February 2020), Liu et al. [27] analysed
semi-structured telephone interviews of nurses and physicians in China. They
identified three main thematic categories: the sense of tremendous professional
responsibility, having to adapt to a completely new context and associated
feelings, and the role of support in resilience. In
Italy, De Leo et al. [28] focused on
protective and risk factors in nurses and physicians and identified three
levels: a personal history level (intrinsic/ethical motivation and role
flexibility versus extrinsic
motivation and role staticity), an interpersonal level (perception of
supportive relationships with colleagues, patients and family versus poor relationships) and an organisational
level (good leadership and sustainable work purpose versus absence of managerial support and undefined or confused
tasks). In Iran, Ardebili et al. [29]
identified four main themes based on the analysis of semi-structured interviews
of a wide variety of healthcare professionals: working in the pandemic era and
associated experiences; changes in personal life and enhanced negative affect; gaining
experience, normalisation and adaptation to the pandemic; and mental health
considerations. Parsons et al. [30]
investigated Canadian physicians’ perceptions and experiences in the context of
the pandemic. They found that resources were strained by continuously evolving
pandemic conditions, which not only gave rise to safety concerns and practice
changes, but also had personal and professional implications [30]. In the United Kingdom,
Bennett et al. [31]
collected experiences of frontline NHS workers during COVID-19 W1 through a
website, where physicians, nurses and physiotherapists left a story. A central
aspect of their findings was the experience and psychological consequences of
trauma.
The main themes identified by these studies
can thus be categorised into (a) positive and negative individual experiences
and ways in which healthcare workers coped and adapted (their “inner world”), (b)
the role of relationships in this sanitary crisis (their “relational” or
“interpersonal world”), both professional and private
and (c) considerations regarding the context (institutional organisation and
healthcare system or their “outer world”).
Given that physicians’ experiences are also
influenced by the healthcare context and cultural determinants [31], we considered
it important to conduct a
qualitative study aiming to explore what frontline physicians went through
during W1, using narratives of physicians working in a Swiss university hospital.
Indeed, to the best of our knowledge, the only other Swiss qualitative study,
by Merlo et al., focused exclusively on physicians’ acceptance of triage
guidelines during the pandemic [32],
whereas other Swiss studies were mostly based on surveys [19, 33].
Methods
Setting
The study was conducted in Lausanne
University Hospital (CHUV; www.chuv.ch),
one of the five medical teaching hospitals of Switzerland. The CHUV has over 1400
beds and 45,000 hospitalisations
per year. The Division of Internal Medicine treats approximately 6200 patients
per year in non-pandemic times and has 165 beds organised in eight wards, each
staffed with one attending physician, one senior physician and up to three
medical residents. During the first wave, it had up to 216 patients simultaneously.
By 30 June 2020, 540 COVID-19 patients had been hospitalised at the CHUV, of whom
two thirds had been looked after in the Internal Medicine Division. To put
these numbers into perspective, on 26 June 2020, the five Swiss university
hospitals had a total COVID-19 bed capacity of 2423 beds and had treated 2175 COVID-19
patients [34].
Data collection
Data were collected between 28 April and 30
June 2020. During W1 of the COVID-19 pandemic, 136 physicians (i.e. residents,
senior and attending physicians) were working in the Internal
Medicine Division, where they provided care to approximately 600 COVID-19 patients
as well as non-COVID-19 patients. Whether they took care of COVID-19 patients
or not, or whether they were originally employed on the ward as internists or
had come from other specialty wards to help during the pandemic, they all
received invitations to participate in the study by email (initial email on 27 April
2020, followed by three
reminders on 8 May, 12 June and 26 June), flyers or during personal
encounters with two of the authors (VK, MM). The PENbank team (three of the authors:
AG, FS, CB)
implemented a temporary online platform, as part of a larger project (at
the time, still in development) of a permanent repository for CHUV physicians’
narratives of experience (see below) [35].
This platform served to collect internal medicine physicians’ narratives. The software
Sphinx IQ2 allowed secure and anonymous transfer
of files (narratives); participants were instructed to avoid people’s names, be
they of colleagues, patients or themselves. Physicians were invited to recount
their experiences of the COVID-19 crisis, without any other imposed themes or
guidelines on how to proceed. Several formats were possible: written texts
(typed, photographed/scanned handwritten texts), audio recordings (using a
voice changer application if desired) and artistic representations
(photographed/scanned paintings, drawings or photos). File size had to be less
than 13 Mb, which corresponds to approximately 15 to 20 minutes of audio.
Optional information included function (resident, senior or
attending physician), sex and age group.
PENbank
In brief, the PENbank project was funded by
a Spark grant from the Swiss National Science Foundation (SNSF CRSK-3_190887/1).
PENbank is a bank for narratives specifically dedicated to physicians’
experiences of medicine and of being a physician. It is a unique means to collect
and organise narrative material on a large scale and over time. PENbank
serves as an observatory providing a voice and visibility to physicians’
experiences and feedback to hospital management authorities, as well as a data
resource for researchers.
Since 2021, PENbank has taken the form of a
website (https://penbankchuv.ch/)
allowing physicians from the CHUV and Unisanté (Lausanne Center for Primary
Care and Public Health) to securely and anonymously send oral, written or
visual narratives, recounting their experiences.
Data analysis
Written data, including verbatim transcriptions
of audio recordings, were examined by means of a narrative analysis based on a
holistic content approach [36]. Lieblich
et al. developed a framework which distinguishes between holistic and categorical
analysis of narratives as well as between content and form [36, 37]. In this study, we adopted a holistic
approach putting the focus on the individual story of each participant, and
considering each story as a whole, which implies interpreting the parts within
it relative to other parts of the story [36, 37].
The “content” dimension of the approach means that attention was centred on
what was put into play in the narrative (vs on the structure of narratives) [36].
The entire interdisciplinary team – which
consisted of three internists (VK, JN, MM), a senior liaison psychiatrist (FS),
a research psychologist (AG) and a social scientist (CB) – carried out the
analysis. Following the analytical process described by Lieblich et al. [36], the
team read the material iteratively
until foci of content of the entire narratives were identified. Foci are nodal
points of the narratives or, to put it differently, the “core stories”. For
Lieblich, “A special focus is frequently distinguished by the space devoted to
the theme in the text, its repetitive nature, and the number of details the
teller provides about it. However, omissions of some aspects in the story, or
very brief reference to a subject, can sometimes also be interpreted as indicating
the focal significance of the topic” [36].
The foci were then reviewed and further described and defined, based on their
significance (repetitive nature, level of detail provided, devoted space in the
text, etc.). Team discussions, in small (FS, CB, AG) or
large groups, were conducted throughout the study, to fine-grain the analysis
and perform the interpretive work.
Informed consent
The call for narratives was accompanied by
a detailed participation information form. Participants were advised that by
submitting an anonymous narrative, they consented to their text being stored in
PENbank and used for research and in publications. The Ethics Committee of the
Canton of Vaud exempted the study from ethical review. The study protocol was
not registered in any registry.
Results
The collected material consisted of 14
photographs, 13 texts and one audio-recorded narrative in French; we
transcribed the audio-recorded narrative verbatim. As photo analysis cannot be
carried out in the same way as text analysis, nor answer the same research
questions, this material will be used as part of another study. The length of
the 14 included narratives ranged from 39 to 3556 words, with a median word count
of 248. They were more often by senior residents or attending physicians aged between
30 and 40 years and originated as much from women as from men (see table 1).
Table 1Characteristics of participating physicians
and of the narrative material.
| General characteristics |
Total
narratives received |
Excluded narratives |
Included narratives |
| Total |
28 |
14 photos |
14 (13 texts; 1 audio) |
| Sex |
Female |
20 (71%) |
13 (93%) |
7 (50%) |
| Male |
8 (29%) |
1 (7%) |
7 (50%) |
| Age |
20–30 |
2 (7%) |
0 |
2 (14%) |
| 30–40 |
20 (72%) |
8 (57%) |
12 (86%) |
| Not specified |
6 (21%) |
6 (43%) |
0 |
| Experience
level |
Students
working as residents & Residents |
6 (21%) |
1 (7%) |
5 (36%) |
| Senior
residents & Attending
Physicians |
22 (79%) |
13 (93%) |
9 (64%) |
Five main or “core” foci were identified in
the narratives: danger and threats; acquisition of knowledge and practices; adaptation
to a changing context; commitment to the profession; and sense of belonging to
the medical staff. The foci are described below, illustrated and supported by
verbatim quotes. For the purposes of this publication, one of the authors (VK),
a native English speaker, translated the narratives that appear below into English
Danger and threats
When the focus of physicians’ narratives
referred to danger, it designated a
variety of rather negative feelings and emotions, such as fear, worry, anxiety
and vulnerability. Threats were
experienced as being dangerous for others, but also for oneself. “Others” were
close relatives (family, friends) or acquaintances such as neighbours:
A plague-stricken person, who precisely because of this work is […]
at risk of being a carrier of THE virus. And therefore, a persona non grata.
It’s a very particular feeling to feel excluded, rejected, unwelcome, when one
has done nothing. (Narrative 5)
When danger concerned the narrating
physicians themselves, emotions and feelings were conveyed, triggered by
uncertainty and/or the threat, and coloured by a feeling of helplessness facing
an inevitable, unavoidable, incoming catastrophe.
So, here we go. It’s the beginning of the wave. On 23.03.2020, the
exponential hospitalisations that we had been expecting all week arrive at the
hospital: 7014 cases confirmed in the country before noon, 1676 cases in our
region, 91 hospitalised here, 14 of them in intensive care, meaning 20
hospitalisations in 24 hours. They doubled in 48 hours and we expect them to
double again in less than 12 hours.[…] We’ve been admitting patients like crazy since
this weekend.
I think it’s about time to stop fooling around and to stay home for good. Avoid
kissing your parents, because for those who will be ill in 2 weeks’ time, it
may well be tense! (Narrative 5)
Anticipatory fear and anxiety, coming from the media who convey
dramatic images from China, Italy or elsewhere... At the beginning of the
crisis, I cannot deny that there was some fear, some anxiety. One must not
forget that the media regularly reported the death of health professionals.
Thus, one could see tributes on social networks paid to these professionals who
died in combat. So many portraits, so many names of colleagues working a few
hundred kilometres from “home”. In these conditions, my fear was legitimate
because I was convinced that I would catch the disease sooner or later. (Narrative 10)
Strategies deployed by physicians to
reassure themselves and prepare to face and manage the danger, were also part
of these narratives. The analogy drawn between preparing for the arrival of the
COVID-19 virus and its patients, and getting ready for a battle, war or a
natural disaster, is reflected for instance in this story:
From that day on, there was this phase, a little bit – very strange
(.) It was as if I felt like I was some kind of army waiting for the arrival of
the enemy, we were building our trenches, we were emptying some units. […] it
was very weird to see those empty floors and – and at that point, I think at
least a week passed during which I did not see any COVID patients, I didn’t
even know what they could look like. But
(.) But I – but we – we were getting ready. And then, uh, I think it lasted a
week, a very stressful phase for me because we didn’t know what to expect, I
think that from one day to the next I said to myself “but what will we – I end up
doing… I don’t know, me, in the
overflowing floors, with patients everywhere filling the hospital, in a sort of
disaster.” (Narrative 11)
Narratives were also about warning others
of the danger:
And then – then, I think it was a phase for me when, when really,
when I said to everyone “be careful because it’s a dangerous disease, don’t try
and act smart but stay home”. For me, it was, it had become clear, it was
almost militant. (Narrative 11)
Another strategy was rationalisation, which
aimed to keep the danger at bay. In these narratives, we find statements
saying, for example, that as the situation had been anticipated, everything
would be fine, or that a sort of “Swiss invincibility” would prevail. Danger
was linked to emotions other than fear, such as anger or guilt, when faced with
the behaviour of others confronted with danger or with flaws in one’s own
behaviour or strategies:
Catching damn COVID without really knowing how, reconsidering one’s
own hospital and personal hygiene, and especially spending 10 days of
confinement being afraid of having generously gifted it to colleagues over the
last few days. (Narrative 13)
Acquisition of knowledge and practices
Acquisition
of knowledge and practices, as a focus, refers to
the different types of acquisition that took place during W1, such as learning
new daily life routines, both in professional and personal settings. For
example, priority lanes were set up for hospital staff to enter the hospital,
badge checks put into place and mask distribution introduced, together with
constant reminders of the importance of barrier gestures. At home, advanced
hygiene measures and social distancing suddenly became the new norm.
Gradually, we enter a new work routine. We carefully avoid public
transport. We observe these new rituals of tireless hand disinfection,
sometimes until they nearly burn. We put on our mask, think about what we touch
and try to avoid the unfortunate act that would make us fall sick. Rituals and
procedures repeat themselves, take time and tire us over time. They are taken
home. Clean area, dining area. Separate laundry. Separate rooms also to limit
contact with one’s own spouse, believing it possible to fall ill oneself
without contaminating one’s loved ones… Contrasting feelings: binding rituals
but also purifying. (Narrative 10)
Acquisition also concerned lessons learnt
about life in general. Narratives depicted the crisis as a revealer of usually
invisible mechanisms and behaviours, both positive and negative. They mentioned
eye-opening discoveries on unshakable age-old hospital administrative
constraints but also on colleagues’ characters. These life lessons allow for a
more informed and critical gaze at hospital organisation, co-workers and human
behaviour.
Lots of fine words at the start of the crisis, but ultimately, in
reality, the “me I” often dominated. […] Other more discreet people […] did
everything they could to help and enquire about how their colleagues were
doing. All the more touching. Certain people’s abilities and qualities were
revealed, amplified and made to stand out. On the contrary, a feeling that
others could not find their place, did not know what to do, were completely
overwhelmed, and remained as discreet and withdrawn as possible so as not to be
noticed, sometimes only to resurface with their complaints at the end of the
crisis. Amplification of incompetence / operating problems that were usually camouflaged
and ignored. (Narrative 15)
The COVID-19 experience also brought along
thoughts on societal awareness, such as the limits of globalisation,
self-introspection and priorities that guide life choices.
Deep questioning on our way of living, on the priorities that we
give (health, work, family), on the way in which the world struggles, is organised,
conducts clinical trials, publishes the results of research, on information and
disinformation. (Narrative 12)
Finally, acquisition may concern a new
personal philosophy for everyday life:
I’m living this period of time at a standstill, day by day. Alone,
of course, but day by day, and I think I appreciate it. It’s a life philosophy
that I have tried to acquire over the past few months.
Carpe Diem. Live the present day, for the past cannot be changed and
the future is filled with potential opportunities that nothing can anticipate,
despite what one would like to believe. (Narrative
5)
Adaptation to a changing context
The narratives that focus on adaptation
reflect the different ways in which physicians coped with W1 and private or
professional upheavals.
The foci adaptation and acquisition
refer to distinct phenomena. Indeed, while the acquisition of knowledge or
skills mobilise cognitive and practical processes, adaptation also depends on
psychological processes such as coping or defence mechanisms.
The stories fall between the recounting of experiences
of successful evolution and the recollection of failed adaptation. Adaptation
can be experienced as an evolution from a first phase, full of uncertainties,
stress and psychological fatigue, to one of a tamed situation, having thus
reduced stress.
A second phase, after adaptation and acceptance of constraints. I
tamed relationships through video conferences, physical distancing and changes
in interaction modes. Improving knowledge about the virus allowed me to reduce
my stress in my clinical management. (Narrative 1)
Conversely, in some stories, boredom,
intellectual understimulation, jealousy and frustration alluded to
non-adaptation or an inability to adapt.
A frustrating and uncomfortable situation, because the population
sees us a bit like heroes, while in the field, the organisational work was
intense but carried out by a small group of people. But our daily work is not
worth such applause.
Frustrating to see some colleagues working a lot in organising/reorganising
and therefore learning a lot. (Narrative 2)
Certain narratives also took a particularly
optimistic turn with the underlying idea of a certain improvement thanks to
COVID-19, with more solidarity between people, and public support for hospitals
and health professionals. Adaptation also included positive increase of
awareness due to the crisis, both as a professional and as a society, for
example in relation to the climate crisis.
Dear Coronavirus,
[…] And yet, the optimist that I am cannot help but notice the
positivity in this crisis: solidarity in my neighbourhood, support for
hospitals and, strangely enough, we could even say belatedly but also
foolishly, recognition for the daily and flawless work of healthcare teams
[...] So thank you coronavirus for having shaken up the obvious, thank you for
also questioning our economic, spiritual and ecological certainties… in the end
I think we needed it a bit. (Narrative 4)
Commitment to the profession
For some physicians, an exceptional
situation, such as COVID-19 W1, is needed to reveal a
natural/obvious/self-evident commitment (or not) towards the profession and
patients, accompanied by the concern of offering the best possible care to all.
I like my job and I do it with the same commitment whether in COVID
or non-COVID times, and, like me, hundreds of thousands of other caregivers do
so. For us, this is a certainty, but for others apparently it wasn’t... (Narrative 4)
This commitment, which seems obvious,
transcended distance: some physicians, even prior to the beginning of the
crisis, did everything they could to join their colleagues in the COVID-19
units. Commitment also transcended fear, as illustrated in this extract:
Despite the fear, I never doubted the role I had to play, I never
doubted for a second the need to commit myself on the wards, at patients’
bedside and within the teams. After all, no one else doubted. Everyone in our
teams responded, regardless of the media’s alarm signals. (Narrative 10)
Moreover, the various expressions of the public’s
gratitude expressed during W1 (applause, “Thank you” notes and gifts sent to
hospitals) as well as the accompanying heroification of health professionals,
also triggered commitment. Finally, some physicians resented being treated like
heroes, as they considered that they were only doing their job.
Sense of belonging to the medical staff
Sense of belonging refers to the team and
its reconfiguration during W1. In some narratives, the feeling of not having
been part caused frustration and envy/jealousy towards the “elected”, who
experienced the crisis intensely and learnt a lot. In other narratives, views
on team membership and roles played are more settled and less emotional,
reflecting an ability to “get on with it”.
In line with the sense of belonging or not,
some physicians felt less deserving according to the position they held, with
two different scenarios: (a) I am not deserving because I was not chosen to be
part of the frontline group, and (b) I fulfilled my tasks, but in my opinion, this
is nothing special and
I find it hard to think of myself as especially deserving.
During that time, I stay in my unit. My “usual” patients need
someone with my skills to take care of them and my role will be to stay at my
post, that’s how it is. From a distance I will see my colleagues at the front
scramble with the wave of patients and novelties,
while I am spared […] How can we welcome the applause and messages of support
if we do nothing for the collective effort? (Narrative
6)
The COVID-19 crisis also implied recalling people
who were no longer part of the team (specialists, physicians from private
practices, etc). We thus found narratives about fellowship and a galvanising
sense of collective belonging, to face this historical event together:
Returning to medicine after two years of specialty training was a
pleasure, full of nice memories, of a department that taught me so much on all
levels... It was a great pleasure to be part of this historic event in the
fight against this virus! (Narrative 3)
Discussion
Our study of accounts by frontline
physicians working during W1 in a Swiss university hospital, examined by means
of a narrative analysis based on a holistic content approach, highlights five
main foci: danger and threats; acquisition of knowledge and practices; adaptation
to a changing context; commitment to the profession; and sense of belonging to
the medical staff.
Given their different aims, designs and
methods, it is somewhat difficult to compare the findings of qualitative studies
on clinicians’ W1 COVID-19 experiences. Moreover, some studies include all
healthcare professionals, whereas others (the overwhelming majority) concentrate
on either nurses or physicians [38–43]. In
this regard, Villa et al., who examined the experience of healthcare providers
using a longitudinal approach, emphasised the importance of understanding the “profession-specific
experiences”
during the COVID-19 outbreak [44].
More specifically, some studies focus on frontline physicians
fighting the pandemic, while others on those with less contact with COVID-19
patients. There are however core areas of experiences concerning the inner, the
interpersonal and the outer world of physicians, which run through these
studies and the narratives we collected.
Indeed, we found experiences related to
physicians’ inner world (foci: danger, acquisition, adaptation and commitment);
in the literature on experiences of healthcare staff caring for patients with
COVID-19, special attention was paid to the risk of burnout and compassion
fatigue and to the need to both build resilience among professionals [45, 46] and
mitigate the repeated trauma
exposure [47]. In our study, we also
found experiences connected to the interpersonal world (focus: belonging). Existing
qualitative studies highlighted important changes in personal life due to
working in a pandemic era [48], such as
social connection deterioration and inability to manage family obligations [49]. On
a professional level, Gonzales et al. shed
light on the importance for physicians to be involved by their leadership in
the decision-making processes [50]. More
positively, studies demonstrated the impact of gratitude, solidarity and faith on
the personal and professional life of physicians [51]. At the same time, a new need
for personal fulfilment emerged [51]. Research also showed that frontline
healthcare workers’ experiences during COVID-19 resonated with experiences of
previous epidemics/pandemics [52].
However, unlike in other studies, the
institutional and healthcare contexts were rarely mentioned in our narratives,
or rather in a positive way (Swiss preparedness for the pandemic). This may be
explained by a relatively well-staffed Swiss healthcare system due to the
comfortable economic situation of the country [53].
In contrast, studies conducted for instance in Pakistan [54], Bangladesh [55] or
Jordan [45] offer lessons and address organisational/administrative
challenges for hospitals in
low- or middle-income countries. This illustrates the need to consider the
local and national context when investigating physicians’ experiences.
A specificity of our study was that all
physicians who were working in the Internal Medicine Division during W1 were
invited to participate, whether they were in charge of COVID-19 patients or
not. This is reflected in the material, as not all narratives recount
experiences of physicians overwhelmed by the gravity of patient situations and
outcomes, allowing other dimensions to emerge. An important contribution of
this study relies on the fact that data consisted of (almost)
“naturally-occurring narratives”, and were not framed by investigators’
questions, thus revealing matters of interest, satisfaction and concern of
physicians during W1. A similar approach was adopted by Lackman-Zeman et al., [46]
who used web-enabled audio diaries.
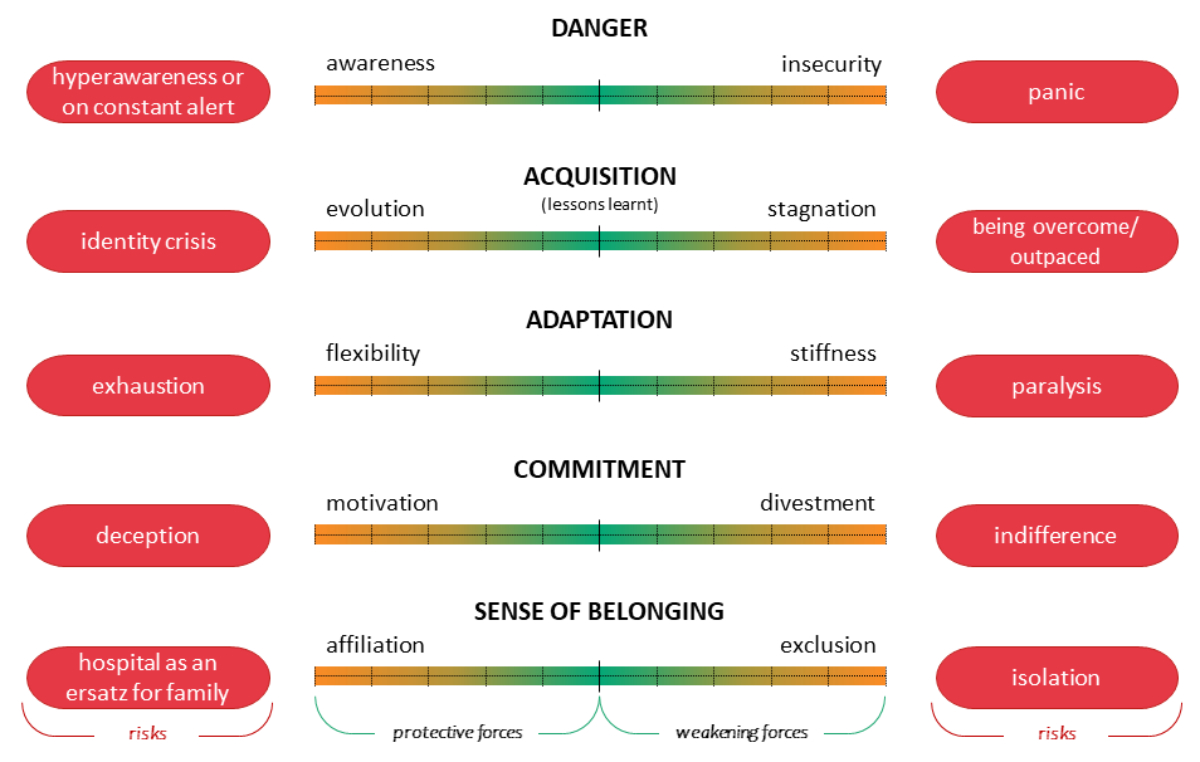
To reflect the clinical relevance of our
results and to provide field feedback to the senior staff members of the CHUV Internal
Medicine Division, a grid (see figure 1) based on the results was developed in
an attempt to situate physicians’ reactions to this crisis. The five foci were
considered to illustrate the transformational effect of the crisis on as many
levels. We also assumed that physicians’ narratives conveyed something about
the stances that they adopted or considered adopting. Seen like this, danger
oscillated between adequate awareness and a justified feeling of insecurity on
their part. Some physicians felt they were evolving by acquiring knowledge and
practical experiences, whereas others felt that they were stagnating. Challenged
by the need to adapt, physicians displayed varying levels of flexibility and of
rigidity. In some, the crisis triggered motivation, whereas in others, disengagement
prevailed. Lastly, regarding the interpersonal dimensions, physicians could
either feel increased affiliation or exclusion. These polarised stances were
represented on a spectrum in the grid.
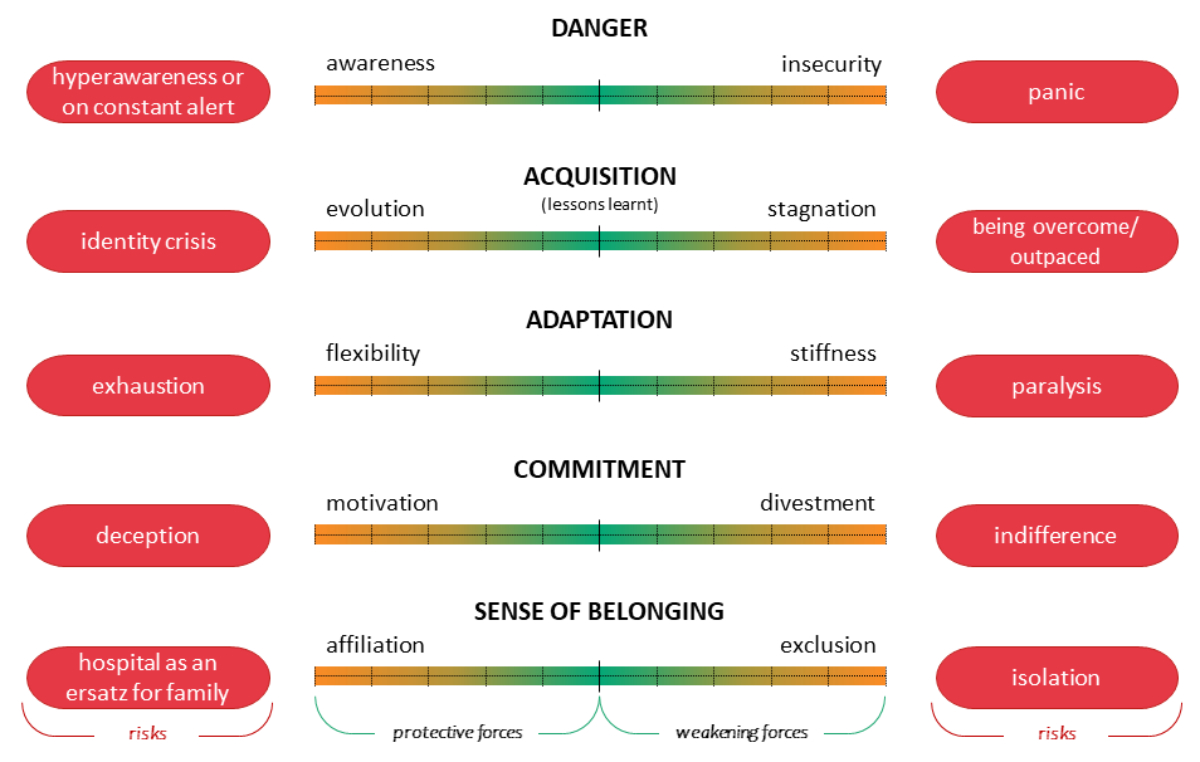
Figure 1Physicians’ experiences during the first
COVID-19 wave. The grid shows a spectrum for each of the 5 foci. The greener
the colour, the better the equilibrium. The more orange the colour, the greater
the risk of an unbalanced equilibrium, which can reach the extreme
polarisations in red.
This grid can be a means to explore the
experiences of clinicians who seem to be doing well but who may be silently
drifting towards the poles of the spectrum of one or more reactions. Indeed,
experiences that feel positive (left side of the figure) also harbour the
danger of turning into problematic attitudes (see red boxes in figure 1). This
grid could also be used to explore clinicians’ experiences in ordinary times, especially
when entering the profession and facing multiple challenges and demands.
Ultimately, the foci reflect topics that
are inherent to a physician’s profession, whatever the context, such as lifelong
never-ending learning, adjustment to every single patient or situation,
commitment to a prosocial job, feeling of belonging to a medical corporation or
guild, and care for safety and risk management, underlining the omnipresence of
danger. In times of tension, as in a pandemic, these foundational elements are
particularly challenged. Strikingly, these topics are not studied in medical
school, thus raising the general question of how students are prepared for the
medical profession, which surpasses the application of clinical skills, and how
young physicians are supervised and mentored. Conveying knowledge is of utmost
importance, but transmitting experience of how to cope with the challenges of
the profession is fundamental.
Our study presents the following
limitations. It is monocentric and focuses on “only” 14 narratives, by
physicians on an internal medicine ward during W1. However, it allowed
qualitative in-depth exploration of experiences reported by physicians at the
beginning of this unprecedented sanitary crisis. Moreover, the material was
solid, giving voice to physicians with different levels of responsibility and a
detailed description
of their experiences. Furthermore, data saturation was reached with the
collected material.
Conclusion
Our study deepens understanding of how
physicians experienced the pandemic both in professional and personal settings.
It offers insights into the manner in which they prepared for a pandemic, coped
with danger, needed to acquire new knowledge and to adapt, and felt a sense of
belonging and of commitment.
Lessons learnt from the COVID-19 pandemic
should nourish reflections about other existing and most likely accelerating
crises, such as the climate and energy crises. Indeed, whatever the crisis, fragilisation
is a consequence,
leading to polarised reactions, as we showed in this study.
Open Science
Physicians who uploaded narratives
anonymously did not consent to share them openly. We deposited the dataset with
restricted access on Zenodo [DOI: 10.5281/zenodo.8318857],
the platform used by the Faculty of Biology and
Medicine of the CHUV. Access can be requested by contacting Celine.Bourquin[at]chuv.ch.
Acknowledgments
The authors would like to thank Céline
Maglieri for her help with the bibliography.
Author contributions: Design and conception of the study: Céline Bourquin, Friedrich
Stiefel, Vanessa Kraege, Marie Méan. Methodology: Céline Bourquin, Friedrich
Stiefel, Amaelle Gavin. Analyses: Vanessa Kraege, Céline Bourquin, Friedrich Stiefel,
Amaelle Gavin, Marie Méan, Julieta Norambuena. Manuscript drafting: Vanessa
Kraege, Céline Bourquin, Amaelle Gavin, Friedrich Stiefel, Julieta Norambuena. Manuscript
revision: Vanessa Kraege, Céline Bourquin, Amaelle Gavin, Friedrich Stiefel,
Marie Méan.
Vanessa Kraege
Medical Directorate
Lausanne University Hospital
BU-21-06-247
Rue du
Bugnon 21
CH-1011
Lausanne
vanessa.kraege[at]chuv.ch
References
1.Kumar S. Burnout and Doctors: Prevalence, Prevention and Intervention. Healthcare
(Basel). 2016 Jun;4(3):37. 10.3390/healthcare4030037
2.Raj KS. Well-Being in Residency: A Systematic Review. J Grad Med Educ. 2016 Dec;8(5):674–84.
10.4300/JGME-D-15-00764.1
3.Pulcrano M, Evans SR, Sosin M. Quality of Life and Burnout Rates Across Surgical Specialties:
A Systematic Review. JAMA Surg. 2016 Oct;151(10):970–8. 10.1001/jamasurg.2016.1647
4.Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout
and career satisfaction among American surgeons. Ann Surg. 2009 Sep;250(3):463–71.
10.1097/SLA.0b013e3181ac4dfd
5.Ding J, Jia Y, Zhao J, Yang F, Ma R, Yang X. Optimizing quality of life among Chinese
physicians: the positive effects of resilience and recovery experience. Qual Life
Res. 2020 Jun;29(6):1655–63. 10.1007/s11136-020-02414-8
6.Tyssen R, Hem E, Gude T, Grønvold NT, Ekeberg O, Vaglum P. Lower life satisfaction
in physicians compared with a general population sample : a 10-year longitudinal,
nationwide study of course and predictors. Soc Psychiatry Psychiatr Epidemiol. 2009 Jan;44(1):47–54.
10.1007/s00127-008-0403-4
7.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction
with work-life balance among US physicians relative to the general US population.
Arch Intern Med. 2012 Oct;172(18):1377–85. 10.1001/archinternmed.2012.3199
8.Van Ham I, Verhoeven AA, Groenier KH, Groothoff JW, De Haan J. Job satisfaction among
general practitioners: a systematic literature review. Eur J Gen Pract. 2006;12(4):174–80.
10.1080/13814780600994376
9.Zumbrunn B, Stalder O, Limacher A, Ballmer PE, Bassetti S, Battegay E, et al. The
well-being of Swiss general internal medicine residents. Swiss Med Wkly. 2020 Jun;150(2324):w20255.
10.4414/smw.2020.20255
10.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout
and quality of healthcare in terms of safety and acceptability: a systematic review.
BMJ Open. 2017 Jun;7(6):e015141. 10.1136/bmjopen-2016-015141
11.Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence Relating
Health Care Provider Burnout and Quality of Care: A Systematic Review and Meta-analysis.
Ann Intern Med. 2019 Oct;171(8):555–67. 10.7326/M19-1152
12.Scheepers RA, Boerebach BC, Arah OA, Heineman MJ, Lombarts KM. A Systematic Review
of the Impact of Physicians’ Occupational Well-Being on the Quality of Patient Care.
Int J Behav Med. 2015 Dec;22(6):683–98. 10.1007/s12529-015-9473-3
13.Stuijfzand S, Deforges C, Sandoz V, Sajin CT, Jaques C, Elmers J, et al. Psychological
impact of an epidemic/pandemic on the mental health of healthcare professionals: a
rapid review. BMC Public Health. 2020 Aug;20(1):1230. 10.1186/s12889-020-09322-z
14.Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA,
Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare
workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020 Dec;277:347–57.
10.1016/j.jad.2020.08.034
15.Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate
psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital.
CMAJ. 2003 May;168(10):1245–51.
16. Maunder, R., et al., The experience of the 2003 SARS outbreak as a traumatic stress
among frontline health-care workers in Toronto: lessons learned. SARS: a case study
in emerging infections, 2005: p. 96-106. 10.1093/acprof:oso/9780198568193.003.0013
17.Huang CL. Underrecognition and un-dertreatment of stress-related psychiatric disorders
in physicians: Determinants, challenges, and the impact of the COVID-19 pandemic.
World J Psychiatry. 2023 Apr;13(4):131–40. 10.5498/wjp.v13.i4.131
18.Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term
psychological and occupational effects of providing hospital healthcare during SARS
outbreak. Emerg Infect Dis. 2006 Dec;12(12):1924–32. 10.3201/eid1212.060584
19.Spiller TR, Méan M, Ernst J, Sazpinar O, Gehrke S, Paolercio F, et al. Development
of health care workers’ mental health during the SARS-CoV-2 pandemic in Switzerland:
two cross-sectional studies. Psychol Med. 2022 May;52(7):1395–8. 10.1017/S0033291720003128
20.Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak
on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018 Nov;87:123–7.
10.1016/j.comppsych.2018.10.003
21.Fukuti P, Uchôa CL, Mazzoco MF, Corchs F, Kamitsuji CS, Rossi L, et al. How Institutions
Can Protect the Mental Health and Psychosocial Well-Being of Their Healthcare Workers
in the Current COVID-19 Pandemic. Clinics (São Paulo). 2020 Jun;75:e1963. 10.6061/clinics/2020/e1963
22.Zaka A, Shamloo SE, Fiorente P, Tafuri A. COVID-19 pandemic as a watershed moment:
A call for systematic psychological health care for frontline medical staff. J Health
Psychol. 2020 Jun;25(7):883–7. 10.1177/1359105320925148
23.Demartini K, Konzen VM, Siqueira MO, Garcia G, Jorge MS, Batista JS, et al. Care for
frontline health care workers in times of COVID-19. Rev Soc Bras Med Trop. 2020;53:e20200358.
10.1590/0037-8682-0358-2020
24.Ganguli I, Chang Y, Weissman A, Armstrong K, Metlay JP. Ebola risk and preparedness:
a national survey of internists. J Gen Intern Med. 2016 Mar;31(3):276–81. 10.1007/s11606-015-3493-1
25.Lancee WJ, Maunder RG, Goldbloom DS; Coauthors for the Impact of SARS Study. Prevalence
of psychiatric disorders among Toronto hospital workers one to two years after the
SARS outbreak. Psychiatr Serv. 2008 Jan;59(1):91–5. 10.1176/ps.2008.59.1.91
26.Phua DH, Tang HK, Tham KY. Coping responses of emergency physicians and nurses to
the 2003 severe acute respiratory syndrome outbreak. Acad Emerg Med. 2005 Apr;12(4):322–8.
10.1197/j.aem.2004.11.015
27.Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care
providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health.
2020 Jun;8(6):e790–8. 10.1016/S2214-109X(20)30204-7
28.De Leo A, Cianci E, Mastore P, Gozzoli C. Protective and risk factors of Italian healthcare
professionals during the COVID-19 pandemic outbreak: a qualitative study. Int J Environ
Res Public Health. 2021 Jan;18(2):453. 10.3390/ijerph18020453
29.Eftekhar Ardebili M, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H.
Healthcare providers experience of working during the COVID-19 pandemic: A qualitative
study. Am J Infect Control. 2021 May;49(5):547–54. 10.1016/j.ajic.2020.10.001
30.Parsons Leigh J, Kemp LG, de Grood C, Brundin-Mather R, Stelfox HT, Ng-Kamstra JS,
et al. A qualitative study of physician perceptions and experiences of caring for
critically ill patients in the context of resource strain during the first wave of
the COVID-19 pandemic. BMC Health Serv Res. 2021 Apr;21(1):374. 10.1186/s12913-021-06393-5
31.Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative
exploration of healthcare workers experiences of working with COVID-19. BMJ Open.
2020 Dec;10(12):e043949. 10.1136/bmjopen-2020-043949
32.Merlo F, Lepori M, Malacrida R, Albanese E, Fadda M. Physicians’ acceptance of triage
guidelines in the context of the COVID-19 pandemic: a qualitative study. Front Public
Health. 2021 Jul;9:695231. 10.3389/fpubh.2021.695231
33.Aebischer O, Weilenmann S, Gachoud D, Méan M, Spiller TR. Physical and psychological
health of medical students involved in the coronavirus disease 2019 response in Switzerland.
Swiss Med Wkly. 2020 Dec;150(4950):w20418. 10.4414/smw.2020.20418
34. Bureaux du secrétariat général Médecine Universitaire Suisse, Pandémie de coronavirus
: le bilan des cinq hôpitaux universitaires de Suisse 2020.
35.Bourquin C, Gavin A, Stiefel F. La liaison psychiatrique I : clinique. Rev Med Suisse.
2022 Feb;18(769):261–4. 10.53738/REVMED.2022.18.769.261
36.Lieblich A, Tuval-Mashiach R, Zilber T. Narrative research: Reading, analysis, and interpretation. Vol. 47. 1998: Sage. 10.4135/9781412985253
37.Beal CC. Keeping the story together: a holistic approach to narrative analysis. J
Res Nurs. 2013;18(8):692–704. 10.1177/1744987113481781
38.Copel LC, Lengetti E, McKeever A, Pariseault CA, Smeltzer SC. An uncertain time: clinical
nurses’ first impressions during the COVID-19 pandemic. Res Nurs Health. 2022 Oct;45(5):537–48.
10.1002/nur.22265
39.Deliktas Demirci A, Oruc M, Kabukcuoglu K. ‘It was difficult, but our struggle to
touch lives gave us strength’: the experience of nurses working on COVID-19 wards.
J Clin Nurs. 2021 Mar;30(5-6):732–41. 10.1111/jocn.15602
40.Firouzkouhi M, Abdollahimohammad A, Rezaie-Kheikhaie K, Mortazavi H, Farzi J, Masinaienezhad N,
et al. Nurses’ caring experiences in COVID-19 pandemic: A systematic review of qualitative
research. Health Sci Rev (Oxf). 2022 Jun;3:100030. 10.1016/j.hsr.2022.100030
41.Polinard EL, Ricks TN, Duke ES, Lewis KA. Pandemic perspectives from the frontline-The
nursing stories. J Adv Nurs. 2022 Oct;78(10):3290–303. 10.1111/jan.15306
42.Specht K, Primdahl J, Jensen HI, Elkjaer M, Hoffmann E, Boye LK, et al. Frontline
nurses’ experiences of working in a COVID-19 ward-A qualitative study. Nurs Open.
2021 Nov;8(6):3006–15. 10.1002/nop2.1013
43.Xu H, Stjernswärd S, Glasdam S. Psychosocial experiences of frontline nurses working
in hospital-based settings during the COVID-19 pandemic - A qualitative systematic
review. Int J Nurs Stud Adv. 2021 Nov;3:100037. 10.1016/j.ijnsa.2021.100037
44.Villa G, Dellafiore F, Caruso R, Arrigoni C, Galli E, Moranda D, et al. Experiences
of healthcare providers from a working week during the first wave of the COVID-19
outbreak. Acta Biomed. 2021 Oct;92 S6:e2021458.
45.Nazzal MS, Oteir AO, Jaber AF, Alwidyan MT, Raffee L. Lived experience of Jordanian
front-line healthcare workers amid the COVID-19 pandemic: a qualitative study. BMJ
Open. 2022 Aug;12(8):e057739. 10.1136/bmjopen-2021-057739
46.Lackman Zeman L, Roy S, Surnis PP, Wasserman JA, Duchak K, Homayouni R, et al. Paradoxical
experiences of healthcare workers during COVID-19: a qualitative analysis of anonymous,
web-based, audio narratives. Int J Qual Stud Health Well-being. 2023 Dec;18(1):2184034.
10.1080/17482631.2023.2184034
47.Harris S, Jenkinson E, Carlton E, Roberts T, Daniels J. “It’s Been Ugly”: A Large-Scale
Qualitative Study into the Difficulties Frontline Doctors Faced across Two Waves of
the COVID-19 Pandemic. Int J Environ Res Public Health. 2021 Dec;18(24):13067. 10.3390/ijerph182413067
48.Eftekhar Ardebili M, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H.
Healthcare providers experience of working during the COVID-19 pandemic: A qualitative
study. Am J Infect Control. 2021 May;49(5):547–54. 10.1016/j.ajic.2020.10.001
49.Mehedi N, Ismail Hossain M. Experiences of the Frontline Healthcare Professionals
Amid the COVID-19 Health Hazard: A Phenomenological Investigation. Inquiry. 2022;59:469580221111925.
10.1177/00469580221111925
50.Gonzalez CM, Hossain O, Peek ME. Frontline Physician Perspectives on Their Experiences
Working During the First Wave of the COVID-19 Pandemic. J Gen Intern Med. 2022 Dec;37(16):4233–40.
10.1007/s11606-022-07792-y
51.Adams GC, Reboe-Benjamin M, Alaverdashvili M, Le T, Adams S. Doctors’ Professional
and Personal Reflections: A Qualitative Exploration of Physicians’ Views and Coping
during the COVID-19 Pandemic. Int J Environ Res Public Health. 2023 Mar;20(7):5259.
10.3390/ijerph20075259
52.Billings J, Ching BC, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare
workers and their views about support during COVID-19 and previous pandemics: a systematic
review and qualitative meta-synthesis. BMC Health Serv Res. 2021 Sep;21(1):923. 10.1186/s12913-021-06917-z
53. OECD. Revenue Statistics, The Impact of Covid-19 on OECD Tax Revenues, 1965-2021.
Organisation for Economic Cooperation and Development; 2022.
54.Shahil Feroz A, Pradhan NA, Hussain Ahmed Z, Shah MM, Asad N, Saleem S, et al. Perceptions
and experiences of healthcare providers during COVID-19 pandemic in Karachi, Pakistan:
an exploratory qualitative study. BMJ Open. 2021 Aug;11(8):e048984. 10.1136/bmjopen-2021-048984
55.Das Pooja S, Nandonik AJ, Ahmed T, Kabir ZN. “Working in the Dark”: Experiences of
Frontline Health Workers in Bangladesh During COVID-19 Pandemic. J Multidiscip Healthc.
2022 Apr;15:869–81. 10.2147/JMDH.S357815