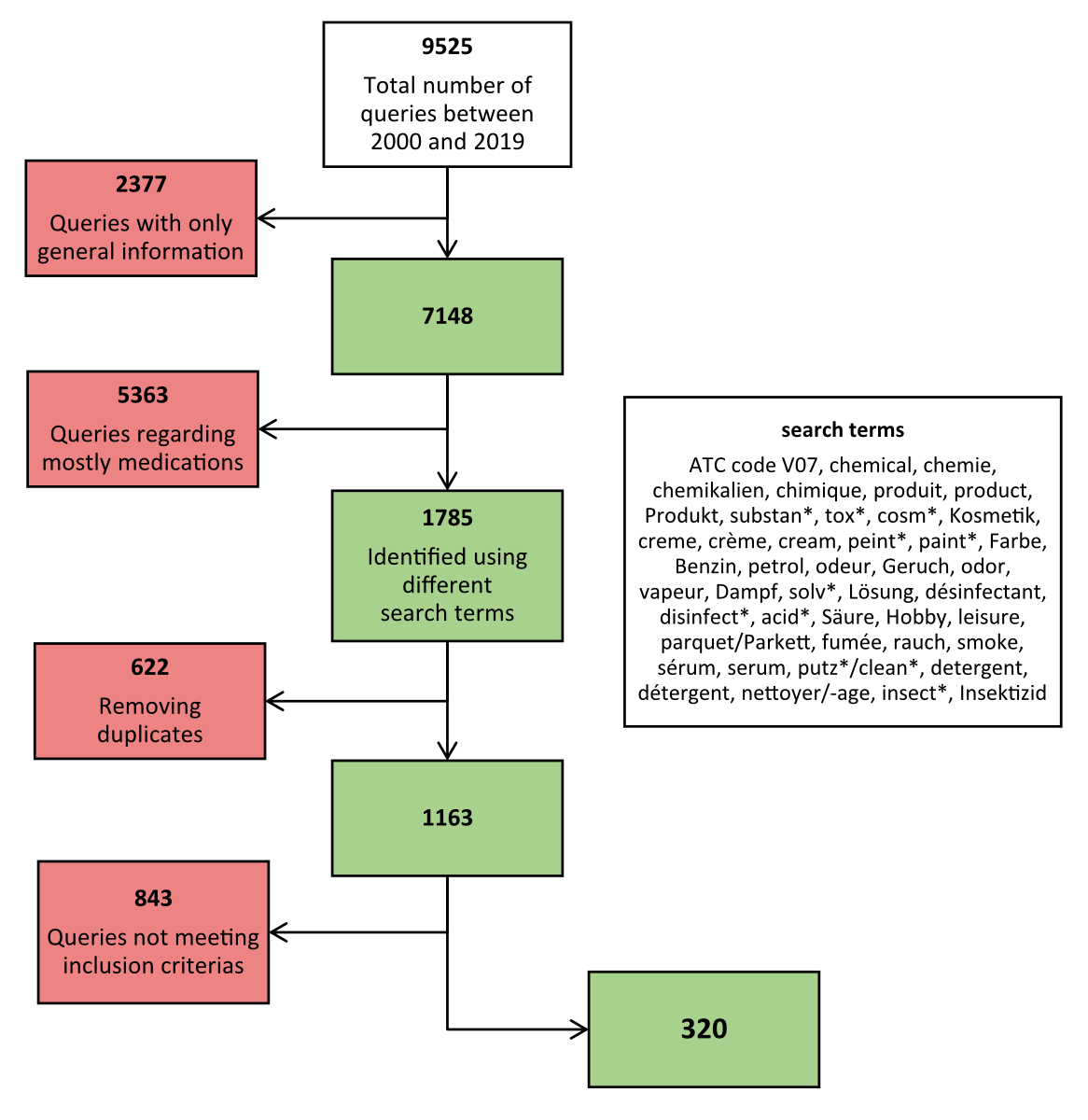
Figure 1Queries flowchart used to obtain the sample of queries analysed.
DOI: https://doi.org/https://doi.org/10.57187/s.3751
Since the thalidomide scandal of 1961/62, research and clinical attention when determining risks to intrauterine child development have predominantly centred on medications. Less attention has been given to the wide range of occupational and domestic exposures to non-therapeutic chemicals that women who are planning to conceive, pregnant or breastfeeding may encounter. Such exposures could have implications for reproductive health.
A previous analysis of the queries to Tox Info Suisse, the Swiss national poisons information centre serving both the general public and healthcare professionals, suggests that such exposures are often unintentional and in most cases related to household chemicals [1]. Research assessing risks of household chemicals in humans is scarce. Studies in humans have primarily investigated the potential impact of prenatal exposure to household cleaning products on respiratory outcomes in children. Several of these studies suggest associations between such exposures and certain health outcomes, particularly respiratory issues. However, the majority of these findings stem from observational study designs with methodological flaws, including diverse exposures, ingredient heterogeneity and reliance on self-reported outcomes, making it challenging to establish causal relationships [2–6].
This study aims to provide an overview of the queries on non-therapeutic chemicals addressed to the Swiss Teratogen Information Service (STIS) over the past two decades.
The Swiss Teratogen Information Service (STIS), located at Lausanne University Hospital (CHUV) within the Department of Clinical Pharmacology, provides evidence-based guidance to healthcare professionals. The primary focus of STIS is to support healthcare professionals in making informed decisions regarding medication use during pregnancy and breastfeeding. Additionally, STIS provides counselling on occupational and environmental exposures. STIS offers expert evidence-based information through multiple channels including telephone, email, and an online referral form, all of which are provided free of charge, to healthcare professionals across Switzerland.
This service is unique in Switzerland and maintains a database of queries, along with detailed documentation of case follow-ups [7–9]. Similar services exist in other countries, forming the European Network of Teratology Information Services (ENTIS) (see, e.g. [10]).
All queries, including relevant information such as type of enquirer, circumstances of the query (e.g. whether during pregnancy, pregnancy planning or breastfeeding), demographic and health-related data on the mothers and medications, are entered into the STIS database in a standardised manner [11]. Information about chemicals including their exact names or their respective categories based on use and composition, is entered into a free-text field. The database also systematically captures risk factors and comorbidities, such as alcohol, tobacco and illicit drug use, with an option for enquirers to list additional comorbidities as free text.
To collect follow-up information on pregnancy outcomes, a postal questionnaire is sent to the initial enquirer (both at first contact and shortly after the expected date of delivery). If there is no response, a reminder is sent. Questionnaires not returned 18 months after the estimated date of delivery are considered lost to follow-up. Information on the following pregnancy outcomes is collected: spontaneous abortion, elective termination of pregnancy, birth mode, date of end of pregnancy, and child’s sex, birth weight, length and head circumference. Additionally, the enquirer is invited to provide comments on obstetric outcomes and any observed malformations in a free-text field.
This study examined all queries (from the start of 2000 to the end of 2019) concerning maternal exposure to non-therapeutic chemicals during pregnancy, the breastfeeding period or preconception, regardless of whether the query concerned a planned exposure or was made after the maternal exposure occurred. The flowchart illustrating the process of data extraction from the STIS database is presented in figure 1. Queries were identified by searching the database for terms related to chemicals in German, French and English, and for the code V07A (the subgroup “All other non-therapeutic products” of the Anatomical Therapeutic Chemical Classification System used for standardised entry of data on medications). Queries were excluded from analysis if they did not involve chemicals, included chemical components commonly found in medications used by pregnant women, referred to chemicals in a medical treatment or diagnostics, lacked specification of the chemical substances or concerned paternal exposure.
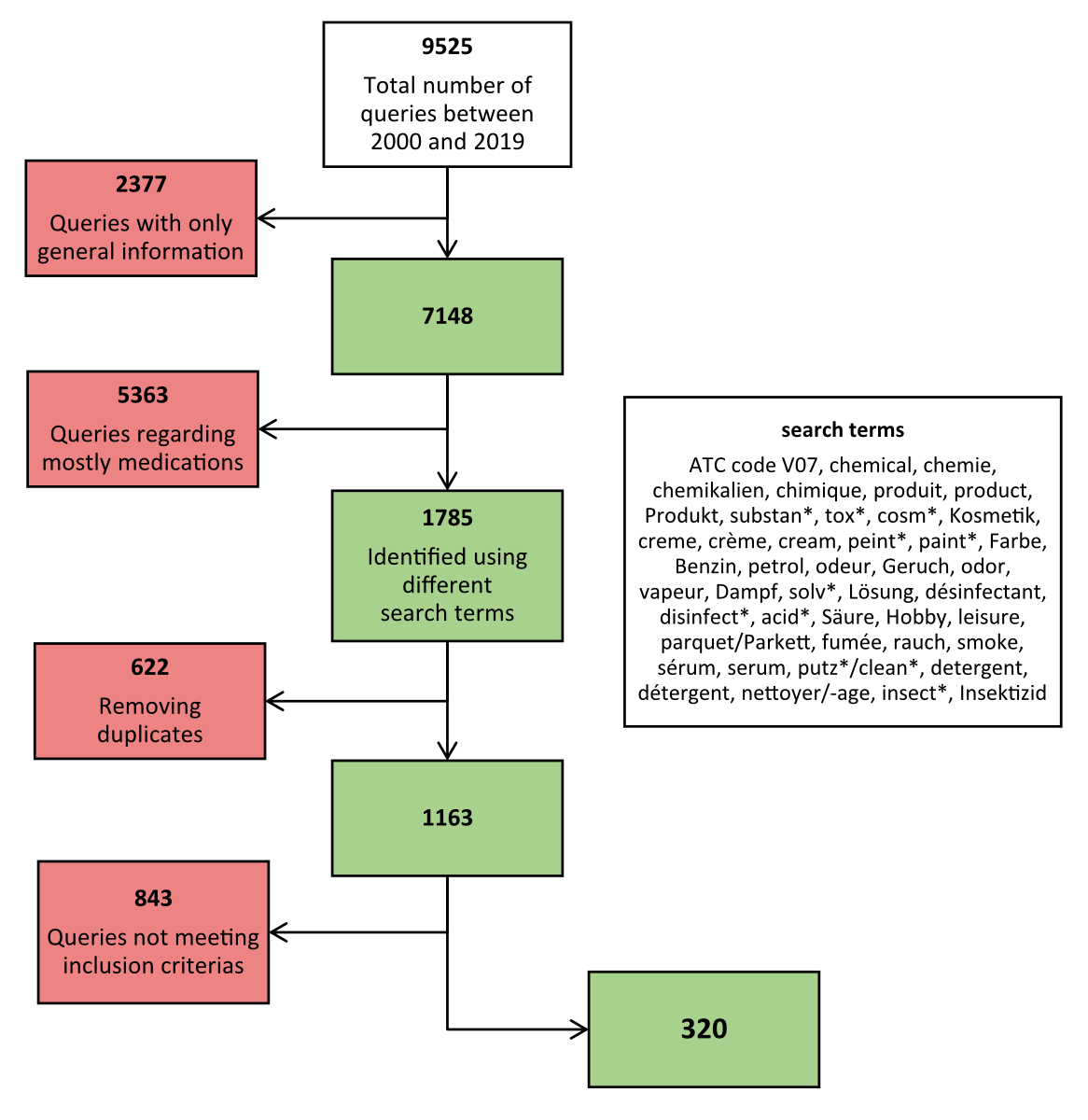
Figure 1Queries flowchart used to obtain the sample of queries analysed.
Variables obtained from the STIS database included information on the time period, details of the enquirer, geographical origin, maternal age, maternal status, use of medication (excluding folic acid), obstetric history, pregnancy risk factors, and child’s birth weight/height, head circumference, gestational age at birth, sex and circumstances related to maternal exposures and neonatal outcomes. Descriptive statistics were used to describe queries, exposures, as well as maternal and infant characteristics using absolute numbers (n) and proportions (% of total) with the number of queries meeting the study’s inclusion criteria as the denominator, unless otherwise indicated. The analyses were conducted using the programme Microsoft Excel®, version Office Professional Plus 2016, as previously described [7].
This study used anonymised data and was conducted in compliance with the Swiss Federal Law on data protection (Human Research Act, article 2). This study did not require ethical approval or informed consent [10].
Between the years 2000 and 2019, the STIS received a total of 9525 queries. From this dataset, our analysis focused specifically on 320 cases involving chemical exposures (see figure 1).
Table 1 presents the circumstances of the queries related to chemicals received by the STIS during the study period. More than half of the 320 queries were received between 2000 and 2004, with the remaining queries distributed relatively evenly over the subsequent years. The majority of the queries were made by gynaecologists or obstetricians, followed by general practitioners, paediatricians, other doctors, the women themselves, fathers of the child or midwives. Given that the STIS only began recording information about enquirers in 2009, a considerable proportion of the data regarding enquirers was missing (66.8%). Most queries originated from the Swiss cantons Vaud, Zurich, Neuchâtel, Geneva and Bern.
Table 1Circumstances of queries regarding chemicals (n = 320).
| Count | Percentage | ||
| Time period | 2000–2004 | 164 | 51.3% |
| 2005–2009 | 56 | 17.5% | |
| 2010–2014 | 49 | 15.3% | |
| 2015–2019 | 51 | 15.9% | |
| Enquirer | Gynaecologist/obstetrician | 81 | 25.3% |
| General practitioner | 9 | 2.8% | |
| Paediatrician | 7 | 2.2% | |
| Doctor of other specialty | 5 | 1.6% | |
| Patient herself | 2 | 0.6% | |
| Husband/child’s father | 2 | 0.6% | |
| Psychiatrist | 1 | 0.3% | |
| Midwife | 1 | 0.3% | |
| Missing | 212 | 66.3% | |
| Geographical origin (Swiss canton or other country) | Vaud | 69 | 21.6% |
| Zurich | 48 | 15% | |
| Neuchâtel | 27 | 8.4% | |
| Geneva | 13 | 4.1% | |
| Bern | 11 | 3.4% | |
| Aargau | 9 | 2.8% | |
| Basel Stadt | 8 | 2.5% | |
| Ticino | 8 | 2.5% | |
| St Gallen | 8 | 2.5% | |
| Fribourg | 8 | 2.5% | |
| Jura | 8 | 2.5% | |
| Valais | 5 | 1.6% | |
| Thurgau | 5 | 1.6% | |
| Schwyz | 4 | 1.3% | |
| Graubünden | 3 | 0.9% | |
| Basel Land | 3 | 0.9% | |
| Solothurn | 3 | 0.9% | |
| Lucerne | 3 | 0.9% | |
| Glarus | 1 | 0.3% | |
| Obwalden | 1 | 0.3% | |
| Appenzell Ausserrhoden | 1 | 0.3% | |
| France | 1 | 0.3% | |
| Missing | 73 | 22.8% | |
Table 2 presents the maternal characteristics. The predominant age groups among the women were 26 to 30 years (25.9%) and 31 to 35 years (29.4%). Regarding pregnancy status, over 80% of the woman were pregnant, with nearly half (45.6%) in the first trimester, 31.3% in the second trimester and 6.3% in the third trimester. A small proportion were not pregnant (6.9%) or were breastfeeding (3.8%). The use of any concomitant medications (excluding folic acid) was reported by a small proportion of women (5.0%), while the vast majority (95.0%) reported no use of medication. Among the pregnancy risk factors, tobacco use was reported by 3.1% of the women, one woman reported use of marijuana and no participants reported alcohol use.
Table 2Maternal characteristics (n = 320).
| Count | Percentage | ||
| Age | 18–20 | 7 | 2.2% |
| 21–25 | 32 | 10% | |
| 26–30 | 83 | 25.9% | |
| 31–35 | 94 | 29.4% | |
| 36–40 | 31 | 9.7% | |
| 41–45 | 9 | 2.8% | |
| >45 | 1 | 0.3% | |
| Missing | 63 | 19.7% | |
| Maternal status | 1st trimester* | 146 | 45.6% |
| 2nd trimester* | 100 | 31.3% | |
| 3rd trimester* | 20 | 6.3% | |
| Not pregnant | 22 | 6.9% | |
| Breastfeeding | 12 | 3.8% | |
| Missing | 20 | 6.3% | |
| Use of medication | Yes | 16 | 5.0% |
| No | 304 | 95.0% | |
| Pregnancy risk factors among the women | Tobacco use | 10 | 3.1% |
| Alcohol use | 0 | 0 | |
| Illicit substance abuse | 1 | 0.3% | |
* Trimester definitions: 1st trimester includes weeks 1–12 or months 1–3 of pregnancy, 2nd trimester includes weeks 13–26 or months 4–6 of pregnancy and 3rd trimester includes weeks 27 until birth or months 7 until birth.
Table 3 provides an overview of the circumstances of the exposure. The majority of exposures occurred in the workplace, representing 61.6% of the cases, followed by exposures at home with 21.3%. Other places of exposure included outdoors, swimming pools, universities, dental practices, and nail studios. Twenty-six women (8.1%) had no exposure to a given substance, the query being precautionary before potential contact with a chemical; only 6.3% of the data was missing. Respiratory exposure was the most common route (60.6%), followed by oral exposure (6.3%), respiratory and cutaneous exposure (5.9%), and cutaneous exposure alone (5.3%). Intramammary (leakage of breast implants) and subcutaneous exposures were relatively rare, each affecting only 0.3% of the women. In 9.1% of the cases, the women took protective measures during exposure (i.e. working under a fume hood or wearing gloves and/or masks).
Table 3Circumstances of exposure (n = 320).
| Count | Percentage | ||
| Place of exposure | Work | 197 | 61.6% |
| Home | 68 | 21.3% | |
| Outdoor | 3 | 0.9% | |
| Swimming pool | 2 | 0.6% | |
| University | 2 | 0.6% | |
| Dental practice | 1 | 0.3% | |
| Nail studio | 1 | 0.3% | |
| No exposure | 26 | 8.1% | |
| Missing | 20 | 6.3% | |
| Mode of exposure | Respiratory | 194 | 60.6% |
| Oral | 20 | 6.3% | |
| Respiratory and cutaneous | 19 | 5.9% | |
| Cutaneous | 17 | 5.3% | |
| Intramammary | 1 | 0.3% | |
| No exposure | 26 | 8.1% | |
| Protective measures taken during exposure | 29 | 9.1% | |
| Missing | 14 | 4.4% | |
| Pregnancy status during exposure or at query (when no exposure) | Pregnant | 284 | 88.8% |
| Before conception* | 7 | 2.2% | |
| Periconceptional | 3 | 0.9% | |
| Potential pregnancy | 14 | 4.4% | |
| Breastfeeding period | 12 | 3.8% | |
* Before conception: refers to women who reported either being exposed to a substance before conception or having a pregnancy wish with exposure but not being pregnant yet
Table 4 provides an overview of the substances most frequently referenced in the queries to the STIS. Nearly half (48.1%) of the queries addressed multiple substances, with an average of three chemicals mentioned per query. Cases that pertained solely to a single substance accounted for 40.6% of the queries, while 11.4% of the queries did not specify any particular substance (data not shown). Overall, a total of 885 chemicals were mentioned in these 320 queries. The most frequently mentioned chemicals included isopropanol, acetone, lead and naphtha.
Table 4Chemicals* most frequently mentioned in the queries to the Swiss Teratogen Information Service (n = 885).
| Count | Percentage | |
| Isopropanol | 26 | 2.9% |
| Acetone | 24 | 2.7% |
| Toluenea | 21 | 2.4% |
| Formaldehydeb | 16 | 1.8% |
| Xylene | 15 | 1.7% |
| White spirit | 14 | 1.6% |
| Lead | 13 | 1.5% |
| Naphtha | 13 | 1.5% |
| Petroleum ether | 13 | 1.5% |
| Ethanol | 12 | 1.4% |
| Ammonia | 11 | 1.2% |
| Ethyl acetate | 8 | 0.9% |
| Acetic acid | 7 | 0.8% |
| Acetonitrile | 7 | 0.8% |
| Diacetone alcohol | 7 | 0.8% |
| Dichloromethane | 7 | 0.8% |
| Turpentine | 7 | 0.8% |
| 2-butanone oxime | 6 | 0.7% |
| Bleach | 6 | 0.7% |
| Ethidium bromideb | 6 | 0.7% |
| Hydrochloric acid | 6 | 0.7% |
| Methanol | 6 | 0.7% |
| Phenolb | 6 | 0.7% |
| Trichloroethylene | 6 | 0.7% |
| Acrylamidec, d | 5 | 0.6% |
| Aliphatic hydrocarbons | 5 | 0.6% |
| Butyl acetate | 5 | 0.6% |
| Formic acid | 5 | 0.6% |
| Hydroquinoneb | 5 | 0.6% |
| Mercury | 5 | 0.6% |
| Phosphoric acid | 5 | 0.6% |
| Propylene glycol methyl ether | 5 | 0.6% |
| Sodium hydroxide | 5 | 0.6% |
| Sulphuric acid | 5 | 0.6% |
| Boraxe | 4 | 0.5% |
| Boric acid | 4 | 0.5% |
| Copper | 4 | 0.5% |
| Diethyltoluamide | 4 | 0.5% |
| Epoxy resin | 4 | 0.5% |
| Hexanef | 4 | 0.5% |
| Paraffin | 4 | 0.5% |
| Pyrethrin | 4 | 0.5% |
| Silicon dioxide | 4 | 0.5% |
| Silicone | 4 | 0.5% |
| Surfactant | 4 | 0.5% |
| Tetrachlorethylene | 4 | 0.5% |
| Other chemical mentioned less than 3 times | 375 | 42.4% |
| No particular chemical mentioned in query | 35 | 4.0% |
* including some with known hazard statement (seea-f for specification)
a suspected of damaging fertility or the unborn child (H361d)
b suspected of causing genetic defects (H341)
c may cause genetic defects (H340)
d suspected of damaging fertility or the unborn child / may presumably damage fertility (H361f)
e may damage fertility or the unborn child (H360)
f suspected of damaging fertility or the unborn child / may presumably damage fertility or the unborn child (H361fd)
Table 5 provides an overview of the product categories mentioned in the queries. The most frequently mentioned product type was solvents (16.6%), followed by cleaning products, paints and insecticides at 10.3%, 8.0% and 5.2%, respectively.
Table 5Types of products mentioned in queries (n = 349).
| Count | Percentage | |
| Solvents | 58 | 16.6% |
| Cleaning products | 36 | 10.3% |
| Paints | 28 | 8.0% |
| Insecticides | 18 | 5.2% |
| Insect repellents | 10 | 2.9% |
| Disinfectants | 10 | 2.9% |
| Metals | 9 | 2.6% |
| Photographic chemicals | 8 | 2.3% |
| Nail products | 8 | 2.3% |
| Acids | 7 | 2.0% |
| Fungicides | 7 | 2.0% |
| Glues | 7 | 2.0% |
| Descaler | 6 | 1.7% |
| Petrol | 5 | 1.4% |
| Thinners | 4 | 1.1% |
| Dental products | 3 | 0.9% |
| Pesticides | 3 | 0.9% |
| Fixatives | 3 | 0.9% |
| Parquet chemicals | 3 | 0.9% |
| Bone cement | 3 | 0.9% |
| Hair dye | 3 | 0.9% |
| Refrigerant | 3 | 0.9% |
| Floor sealer | 3 | 0.9% |
| Grout | 3 | 0.9% |
| Insulator | 3 | 0.9% |
| Paint diluters | 3 | 0.9% |
| Smoke | 3 | 0.9% |
| Inks | 2 | 0.6% |
| Thermometer mercury | 2 | 0.6% |
| Bleach | 2 | 0.6% |
| Hair products | 2 | 0.6% |
| Regenerating salt | 2 | 0.6% |
| Rodenticide | 2 | 0.6% |
| Acrylic gel | 2 | 0.6% |
| Breast implants | 2 | 0.6% |
| Hardeners | 2 | 0.6% |
| Plastics | 2 | 0.6% |
| Salts | 2 | 0.6% |
| Varnishes | 2 | 0.6% |
| Wallpaper stripper | 1 | 0.3% |
| Smoothing agent | 1 | 0.3% |
| Toy | 1 | 0.3% |
| Car paints | 1 | 0.3% |
| Paint hardeners | 1 | 0.3% |
| Light bulb | 1 | 0.3% |
| Fuel oil | 1 | 0.3% |
| Gas | 1 | 0.3% |
| Cosmetic products | 1 | 0.3% |
| Fertiliser | 1 | 0.3% |
| Gunshot residue | 1 | 0.3% |
| Oxidising agent | 1 | 0.3% |
| Proofing spray | 1 | 0.3% |
| Silicone remover | 1 | 0.3% |
| Artificial smoke | 1 | 0.3% |
| Herbicides | 1 | 0.3% |
| Plant fertiliser | 1 | 0.3% |
| Aroma | 1 | 0.3% |
| Dye for nucleic acids | 1 | 0.3% |
| e-cigarette | 1 | 0.3% |
| Polishing paste | 1 | 0.3% |
| Various chemicals | 47 | 13.5% |
Table 6 provides an overview of pregnancy outcomes. Pregnancy outcomes were available for 142 (44.4%) of the 320 cases, while the remainder were lost to follow-up. Among the 142 queries, 132 pregnancies resulted in live births, while 10 (7%) ended in miscarriages or abortions.
Table 6Pregnancy and perinatal outcomes (n = 320).
| Count | Percentage | ||
| Queries with neonatal data | 142 | 44.4% | |
| Lost to follow-up | 178 | 55.6% | |
| Time period of end of pregnancy, n = 142 | 2000–2004 | 49 | 34.5% |
| 2005–2009 | 24 | 16.9% | |
| 2010–2014 | 35 | 24.6% | |
| 2015–2019 | 25 | 17.6% | |
| Missing | 9 | 6.3% | |
| Pregnancy outcomes, n = 142 | Live birth* | 132 | 93.0% |
| Miscarriage | 8 | 5.6% | |
| Elective termination of pregnancy | 2 | 1.4% | |
| Sex of the child, n = 136** | Female | 65 | 47.8% |
| Male | 66 | 48.5% | |
| Missing | 5 | 3.7% | |
* Including 4 twin births
** Not including miscarriages and abortions
The 132 live births resulted in 136 babies, including 4 sets of twins. Of these, 65 babies were female (47.8%) and 66 male (48.5%), with only a small amount of missing data (3.7%). Birth weights were available for 133 babies and ranged from 2060 to 4350 g, with an average of 3289 ± 435 g (mean ± standard deviation). Additionally, birth heights were recorded for 125 babies and ranged from 42 to 54 cm, with an average of 49.4 ± 2.0 cm. The head circumference at birth was available for 64 babies and ranged from 30 to 38 cm, with an average of 34.7 ± 1.5 cm. The gestational age at birth was documented for 114 pregnancies and ranged from 33 to 42 weeks, with an average pregnancy duration of 38.4 ± 5.2 weeks. Ten babies were born preterm, including four twin babies.
No information on additional neonatal outcomes or on congenital malformations was available for 11 of the 136 neonates; therefore the corresponding analysis was performed on 125 neonates. Of these 125 cases, 106 (84.8%) reported a healthy outcome, with no instances of congenital malformations or abnormal neonatal adaptation noted. Of the 125 cases analysed, 19 queries (15.2%) reported various complications including neonatal jaundice, hypoglycaemia, adaptation disorders, transient tachypnoea, respiratory distress syndrome, bradycardia, low birth weight for gestational age and minor anomalies (nevus, torticollis, haemangioma, and unspecified disorders of the lower extremities). Five babies (4.0%) were diagnosed with a major congenital malformation, including congenital cardiac malformations, renal abnormalities and congenital hypertrophic pyloric stenosis.
This analysis characterises the data captured by the STIS database on non-therapeutic chemicals, spanning the years 2000 to 2019. Looking at this two decades’ worth of data, we identified 320 instances of exposure to non-therapeutic chemicals. The reported chemicals had a high degree of chemical diversity, and concerns often involved simultaneous exposures to multiple substances. The prominence of solvents and household cleaning products in the queries was expected, given that solvents are used in several industries, and household cleaning products are often used by women of reproductive age. Follow-up information on the offspring was available for a subset of cases, indicating outcomes consistent with general population expectations [12–17]. Due to the low number of cases in our study, together with the degree of chemical diversity (type and number of chemicals), no attempt was made to perform causality assessment for cases with negative pregnancy outcomes.
The majority of the exposures to chemicals documented in the STIS database were work-related. In Switzerland, a comprehensive legal framework regulates chemical use, with specific regulations for pregnant women [18–22], aiming to safeguard lives and health from potential hazards associated with chemical substances. In the context of pregnancy and breastfeeding, Swiss labour regulations including the Labour Law, its ordinances and the Ordinance on Maternity Protection at Work [23] establish criteria for categorising jobs as hazardous, outlining risk mitigation processes and defining responsibilities. Employers are required to engage occupational health specialists for workstation risk assessments. If the attending physician detects issues in the risk assessment or non-compliance with protective measures, the pregnant or breastfeeding woman is barred from the workplace and a medical certificate of incapacity may be issued. The work-related queries in the STIS database were requests from treating physicians seeking guidance on risk assessment in accordance with the Swiss Maternity Protection Ordinance. In view of the legal framework described above, we assume that following the risk assessment, security measures were implemented to safeguard potentially exposed women, although specific follow-up information is unavailable. Within this regulatory framework and in recognition of the expertise of occupational health specialists, the STIS began referring work-related chemical exposure queries to these specialists at the same hospital (Lausanne University Hospital) from 2004. This decision may have contributed to the relatively lower number of documented queries after 2004.
The handling of chemicals generally poses no risk to the mother and child when the universally applicable limit values laid down by SUVA, the Swiss National Accident Insurance Fund, are complied with (maximum workplace concentration and biological exposure limits [24]; compare with article 13 of the Ordinance on Maternity Protection at Work [23]). However, special attention is warranted for certain harmful chemicals, such as those with germ cell mutagenicity, carcinogenicity, reproductive toxicity, specific target organ toxicity, mercury compounds, mitotic inhibitors and carbon monoxide. Frequently mentioned substances in the STIS database included toluene, formaldehyde, ethidium bromide, phenol, acrylamide, hydroquinone, borax and hexane, all acknowledged for their potential harm to both maternal and foetal health (refer to the legend in table 4 for hazard statements).
Beyond the occupational context and because of the substantial involvement of women in household chores, exposures in the domestic setting can also be relevant [25]. Among the various chemicals used domestically, the constituents of household cleaning products are likely to be very commonly used. In our analysis, we found that home environments were also a prevalent context for exposures, with household cleaning products emerging prominently among the types of chemicals mentioned. According to the latest Swiss Labour Force Surveys (SLFS), women of childbearing age spend over 50 hours per week in household and family responsibilities, with 6–7 hours dedicated specifically to household cleaning tasks [25]. We are not aware of studies on exposures to non-therapeutic chemicals before, during and after pregnancy in Switzerland. In some other Western countries, however, efforts have been made to examine the use of household products during pregnancy. For instance, data from a Spanish birth cohort study (n = 2058) revealed that 20% of the pregnant women reported exposures to chemicals, primarily from cleaning products or solvents, especially when working in the industrial sector [26]. Results from a cross-sectional study from England (n = 69) indicated that cleaning products in the workplace were the most common chemical exposures during pregnancy [27]. A recent study in New York investigated the use of household cleaning products, including multi-cleaners, bleach and ammonia, among pregnant women during the COVID pandemic (n = 320) and observed an increase in the use of antimicrobial and organic cleaning products during the pandemic. Interestingly, less than 20% of these women received guidance from their obstetrician regarding the safe use of those products during pregnancy [28].
Queries to Tox Info Suisse, the Swiss national poisons information centre serving both the general public and healthcare professionals, were analysed previously. Data spanning the period 1995 to 2015 (n = 2871) showed that queries regarding household products (27.6%) exceeded those concerning medications (25.5%) [1]. Notably, questions on household products primarily originated from the general public, whereas physicians predominantly enquired about medications. The notable quantitative difference in queries between Tox Info Suisse and the STIS might partly stem from the former’s accessibility to the general public, whereas the latter specifically handles queries from healthcare professionals.
The strengths of this STIS database-based analysis are the rare and exclusive characteristics of the data used. A major limitation of the present work is that the queries to the STIS do not necessarily represent the broader landscape of exposures to chemicals during pregnancy occurring in Switzerland. Particularly in the case of widely used chemicals, such as those found in household cleaning products, the STIS database is likely to significantly underestimate the corresponding exposures occurring in Switzerland. Furthermore, the French-speaking cantons of Switzerland are slightly overrepresented among the queries, despite STIS counselling services being available not only in French, but also in German and English. This might be related to the fact that the STIS is associated with Lausanne University Hospital, which is located in the French-speaking canton Vaud. Additional limitations are the low number of queries that could be analysed (320 queries in 20 years), and the limited information available in the follow-up data. Due to the relatively short time period between birth and subsequent follow-up information, malformations and diseases that might only become evident after birth often remain undocumented in the database. To fully capture the exposures to non-therapeutic chemicals around pregnancy – i.e. in women who are planning to conceive, are pregnant or are breastfeeding – in Switzerland, further research is needed.
Our analysis of the STIS database shows that healthcare professionals in Switzerland have concerns regarding exposures to non-therapeutic chemicals before, during and after pregnancy, occurring both at work and in domestic settings. Further studies aimed at comprehensively capturing the highly heterogeneous exposures to non-therapeutic chemicals during pregnancy should extend their focus beyond professional contexts to encompass domestic environments as well.
All STIS data analysed during the current study are available from PD Dr Ursula Winterfeld upon reasonable request.
We thank the whole team at the Swiss Teratogen Information Service for their input and support, in particular the computer scientist Mr F. Veuve. We gratefully acknowledge Dr H. Murray for her language corrections. Lastly, we thank Dr Joshua Dan Itsch Csucker for his input regarding chemistry.
This research received no funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Vogel T, Lüde S, Baumgartner R, Rauber-Lüthy C, Simões-Wüst AP. Accidental or intentional exposure to potentially toxic medications, natural toxins and chemicals during pregnancy: analysis of data from Tox Info Suisse. Swiss Med Wkly. 2018 May;148:w14620. 10.4414/smw.2018.14620
2. Bably M, Arif AA, Post A. Prenatal use of cleaning and scented products and its association with childhood asthma, asthma symptoms, and mental health and developmental comorbidities. J Asthma. 2021 Jan;58(1):46–51. 10.1080/02770903.2019.1656229
3. Casas L, Zock JP, Carsin AE, Fernandez-Somoano A, Esplugues A, Santa-Marina L, et al. The use of household cleaning products during pregnancy and lower respiratory tract infections and wheezing during early life. Int J Public Health. 2013 Oct;58(5):757–64. 10.1007/s00038-012-0417-2
4. Henderson J, Sherriff A, Farrow A, Ayres JG. Household chemicals, persistent wheezing and lung function: effect modification by atopy? Eur Respir J. 2008 Mar;31(3):547–54. 10.1183/09031936.00086807
5. Tjalvin G, Svanes Ø, Igland J, Bertelsen RJ, Benediktsdóttir B, Dharmage S, et al. Maternal preconception occupational exposure to cleaning products and disinfectants and offspring asthma. J Allergy Clin Immunol. 2022 Jan;149(1):422–431.e5. 10.1016/j.jaci.2021.08.025
6. Sherriff A, Farrow A, Golding J, Henderson J. Frequent use of chemical household products is associated with persistent wheezing in pre-school age children. Thorax. 2005 Jan;60(1):45–9. 10.1136/thx.2004.021154
7. Baumgartner R, Winterfeld U, Panchaud A, Simões-Wüst AP. Queries on medication use during pregnancy: characterisation of the Swiss Teratogen Information Service database. Swiss Med Wkly. 2022 May;152(2122):w30187. 10.4414/SMW.2022.w30187
8. Weber-Schoendorfer C, Kayser A, Tissen-Diabaté T, Winterfeld U, Eleftheriou G, Te Winkel B, et al. Fetotoxic risk of AT1 blockers exceeds that of angiotensin-converting enzyme inhibitors: an observational study. J Hypertens. 2020 Jan;38(1):133–41. 10.1097/HJH.0000000000002233
9. Pauliat E, Onken M, Weber-Schoendorfer C, Rousson V, Addor MC, Baud D, et al. Pregnancy outcome following first-trimester exposure to fingolimod: A collaborative ENTIS study. Mult Scler. 2021 Mar;27(3):475–8. 10.1177/1352458520929628
10. Winterfeld U, Weber-Schöndorfer C, Schaefer C, von Elm E, Buclin T. Ethical approval for multicenter cohort studies on drug exposure during pregnancy: A survey among members of the European Network of Teratology Information Services (ENTIS). Reprod Toxicol. 2018 Sep;80:68–72. 10.1016/j.reprotox.2018.06.002
11. Swiss Teratogen Information Service S. Available from https://www.chuv.ch/en/stis/
12. EUROCAT. Prevalence charts and tables | EU RD Platform. 2020. Available from https://eu-rd-platform.jrc.ec.europa.eu/eurocat/eurocat-data/prevalence_en
13. Matas JL, Agana DF, Germanos GJ, Hansen MA, Modak S, Tanner JP, et al. Exploring classification of birth defects severity in national hospital discharge databases compared to an active surveillance program. Birth Defects Res. 2019 Nov;111(18):1343–55. 10.1002/bdr2.1539
14. Ito S. Mother and Child: Medication Use in Pregnancy and Lactation. Clin Pharmacol Ther. 2016 Jul;100(1):8–11. 10.1002/cpt.383
15. Dathe K, Schaefer C. The Use of Medication in Pregnancy. Dtsch Arztebl Int. 2019 Nov;116(46):783–90.
16. Chen LJ, Chiou JY, Huang JY, Su PH, Chen JY. Birth defects in Taiwan: A 10-year nationwide population-based, cohort study. J Formos Med Assoc. 2020 Jan;119(1 Pt 3):553–9. 10.1016/j.jfma.2019.08.006
17. Svensson E, Ehrenstein V, Nørgaard M, Bakketeig LS, Rothman KJ, Sørensen HT, et al. Estimating the proportion of all observed birth defects occurring in pregnancies terminated by a second-trimester abortion. Epidemiology. 2014 Nov;25(6):866–71. 10.1097/EDE.0000000000000163
18. The Federal Council. SR 813.1 - Federal Act of 15 December 2000 on Protection against Dangerous Substances and Preparations (Chemicals Act, ChemA) 2023. Available from https://www.fedlex.admin.ch/eli/cc/2004/724/en
19. The Federal Council. Chemicals Ordinance (ChemO). 2023. Available from https://www.anmeldestelle.admin.ch/chem/en/home/themen/recht-wegleitungen/chemikalienrecht/chemikalienverordnung.html
20. The Federal Council. Chemical Risk Reduction Ordinance (ORRChem). 2017. Available from https://www.anmeldestelle.admin.ch/chem/en/home/themen/recht-wegleitungen/chemikalienrecht/chemikalien-risikoreduktionsverordnung.html
21. Federal Administration. Federal Coordination Commission for Occupational Safety 2017. Available from https://www.ekas.ch/index-en.php?frameset = 1.
22. SUVA. 2023. Available from https://www.suva.ch/en
23. Federal Administration. 822.111.52 Verordnung des WBF über gefährliche und beschwerliche Arbeiten bei Schwangerschaft und Mutterschaft (Mutterschutzverordnung). 2015. Available from https://www.fedlex.admin.ch/eli/cc/2001/127/de
24. SUVA. Grenzwerte am Arbeitsplatz. 2023. Available from https://www.suva.ch/de-ch/services/grenzwerte#gnw-location
25. Federal Statistical Office. Housework and family work: Average time spent in hours per week [Haus- und Familienarbeit: Durchschnittlicher Zeitaufwand in Stunden pro Woche]. 2023. Available from https://www.bfs.admin.ch/bfs/de/home/statistiken/arbeit-erwerb/erwerbstaetigkeit-arbeitszeit/vereinbarkeit-unbezahlte-arbeit/haus-familienarbeit.assetdetail.17124520.html
26. García AM, González-Galarzo MC, Ronda E, Ballester F, Estarlich M, Guxens M, et al. Prevalence of exposure to occupational risks during pregnancy in Spain. Int J Public Health. 2012 Oct;57(5):817–26. 10.1007/s00038-012-0384-7
27. Zachek CM, Schwartz JM, Glasser M, DeMicco E, Woodruff TJ. A screening questionnaire for occupational and hobby exposures during pregnancy. Occup Med (Lond). 2019 Oct;69(6):428–35. 10.1093/occmed/kqz094
28. Deierlein AL, Grayon AR, Zhu X, Sun Y, Liu X, Kohlasch K, et al. Personal Care and Household Cleaning Product Use among Pregnant Women and New Mothers during the COVID-19 Pandemic [Electronic Resource]. Int J Environ Res Public Health. 2022 May;19(9):5645. 10.3390/ijerph19095645