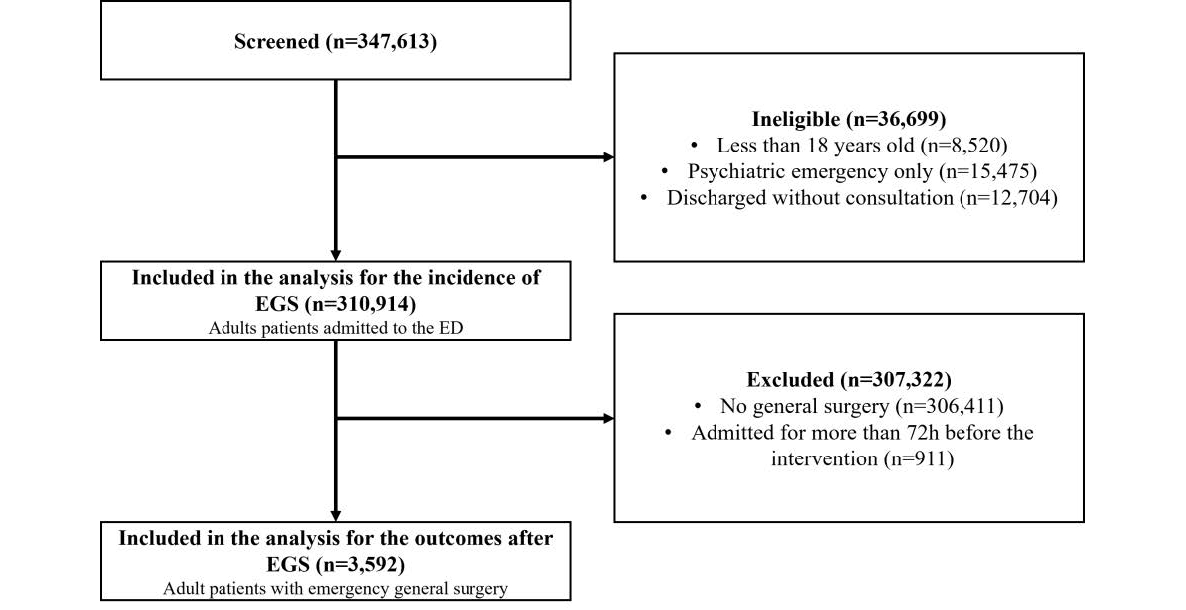
Figure 1Flowchart of patients included in the study. EGS: Emergency general surgery; ED: Emergency department.
DOI: https://doi.org/https://doi.org/10.57187/s.3729
Emergency general surgery is defined as non-elective surgery for abdominal pathologies such as appendicitis, cholecystitis, bowel perforation, bowel obstruction, or incarcerated hernia [1]. These interventions account for 28% of surgical complications and 47% of surgical deaths, yet they represent only 10% of surgical procedures performed [2]. Mortality following emergency surgery is five times higher than after elective surgery (that is, surgery planned before hospital admission) [3].
Most data regarding emergency surgery have been obtained from studies conducted in the United Kingdom (UK), Canada, or the United States of America (US). The Swiss healthcare system is quite different, with a higher density of physicians and hospitals and a lower nurse-to-bed ratio. These factors may affect the quality of care [4]. While more nurses would probably improve outcomes, a higher number of surgeons could also mean a decrease in the number of interventions performed annually per surgeon. Local studies are therefore needed to assess the burden on patients and the healthcare system and to allow international comparisons. It will also enable us to observe whether predictors of poor outcomes, such as age, that have been associated with both higher surgery rates and higher mortality rates are similar to other health settings [5, 6].
The objectives of this study were (a) to estimate the incidence of emergency general surgery in a Swiss University Hospital among patients visiting the emergency department, (b) to describe the characteristics and outcomes of patients undergoing such interventions, and (c) to study the impact of age on the outcomes.
The results of this study are being reported in line with the STROBE guidelines [7].
This study was a retrospective cohort study, analysing patients who required emergency general surgery in the Geneva University Hospital between 1 January 2015 and 31 December 2019, and was based on electronically extracted data. Geneva University Hospital is one of five university hospitals in Switzerland, with over 2100 beds. The emergency department is the only level 1 trauma centre in the area (500,000 inhabitants, 100,000 commuters) and receives more than 70,000 patient visits annually. These can be seen in an ambulatory setting (minor emergencies) or in a stretcher bay (more serious emergencies). Each year, in this hospital, surgeons perform more than 20,000 operations. Pathways to emergency general surgery can be different from one country to another, and even between hospitals. In our hospital, direct admissions to a ward are not possible. Thus, patients for whom a diagnosis requiring emergency general surgery has been made by a family physician or in a walk-in clinic are referred to our emergency department and are triaged there. After that, depending on the characteristics of the patients, the severity of the disease or the time of the admission, they are either assessed as any other patient or are “fast-tracked” by a senior emergency department physician to a surgical ward.
Medical records of all consecutive patients visiting the emergency department of the Geneva University Hospital were screened for inclusion. We excluded patients younger than 18 years old, those admitted primarily for a psychiatric reason, and those who left without consultation. This population was used to estimate the incidence of emergency general surgery. Emergency general surgery was defined as one of the following procedures: appendectomy, cholecystectomy, laparotomy, lysis of adhesions, large bowel resection, small bowel resection, or peptic ulcer repairs, that were performed on a non-elective basis during the 72 hours following the admission. These procedures were classified into low-risk (appendectomy, cholecystectomy) and high-risk (laparotomy, lysis of adhesions, large bowel resection, small bowel resection, and peptic ulcer repairs) [8]. Patients were identified using CHOP (Swiss Operations Classification) codes (table S1 in the appendix). We then excluded patients who did not undergo emergency general surgery, to study the characteristics and outcomes only among surgical patients.
Baseline patient characteristics include demographic information (age and sex), previous health care use (number of hospitalisations and emergency department visits in the previous year), emergency department features (day and time of admission, triage scale [life/limb threatening (level 1) to non-urgent (level 4)] [9], vital signs including shock index (ratio of heart rate over systolic blood pressure higher than 1), and laboratory results (creatinine, haemoglobin, leukocytes, C-reactive protein (CRP), albumin). We also collected co-morbidities and diagnoses (using a billing coding based on the ICD-10 classification). The time before surgery, defined as the time between emergency department admission and operating room (OR) admission, and the type of surgery were also collected. The type of surgery was classified as a low-risk procedure (appendectomy and cholecystectomy) or a high-risk procedure (large bowel resection, lysis of adhesions, small bowel resection, peptic ulcer repair and laparotomy for other reasons).
The primary outcome was the incidence of emergency general surgery among patients assessed in the emergency department. Secondary outcomes included admission to the intensive care unit (ICU), ICU length of stay, 30-day, 90-day and one-year mortality, hospital length of stay, and dependence at discharge. Mortality was ascertained from the hospital database. Therefore, these outcomes were missing for patients discharged alive and without any ambulatory visit or hospital admission after 30 days, 90 days or one year. Hospital length of stay was measured from admission to discharge from the acute care hospital (without rehabilitation). ICU length of stay was the sum of every ICU stay during the hospitalisation. Dependence at discharge was defined as a transfer to any place except home (rehabilitation, long-term care facility, or new admission to a nursing home). Patients who were not alive at discharge or who were already in a nursing home before hospitalisation were excluded from the analysis of this outcome.
Variables were collected using electronic data extraction from the hospital data warehouse (table S1 in the appendix). Briefly, all data routinely collected for clinical purposes (e.g. physician and nursing notes, laboratory results and diagnostic imaging results) are recorded in the electronic health record of the patient. These data are structured and can be extracted for quality evaluation or research projects, subject to approval by the Ethics Committee. Linkage between different subsets of the database is performed using an individual number attributed to each care episode.
For the primary objective, we first calculated the incidence of emergency general surgery among emergency department patients, with a 95% confidence interval (CI). A priori subgroup analyses were planned with stratified estimates: sex (male versus female), age (<65 versus ≥65 years old), and the area in the emergency department in which the patient was initially assessed (minor emergencies versus stretcher bay). Unadjusted associations between age and incidence of emergency general surgery were graphically represented using restricted cubic splines.
For the second objective, we described the baseline characteristics of patients with emergency general surgery using means and standard deviations (medians and interquartile ranges [IQR] if skewed) or frequency and proportion. The frequency of surgical interventions was also reported, both for the overall population and for different subgroups. Finally, the outcomes after surgery were described. Binary outcomes such as mortality or intensive care unit admission were reported as proportions, together with their 95% CI. Continuous outcomes with skewed distributions (e.g. ICU length of stay) were log-transformed and described using the geometric mean with 95% CI. Stratified estimates were reported for different subgroups: sex (male versus female) and age (<65 versus ≥65). This cut-off was chosen a priori, since it is an age cut-off that has been commonly used in the geriatric literature and in previous studies [10, 11].
For the third objective, unadjusted associations between age and intensive care unit admission, dependence at discharge and one-year mortality were graphically represented using restricted cubic splines. The number of knots was based on Akaike information criteria and their placement was decided using recommended quantiles [12]. To study the adjusted associations between older age and these outcomes, multivariable log-binomial regression models were used to estimate adjusted risk ratios (aRR) and their 95% CI [13]. Covariates used for multivariable models were sex, admission by ambulance, level of emergency department triage (1 and 2 versus 3 and 4) and the type of procedure (high risk versus low risk). These were chosen on the basis of their clinical importance (based on the authors’ judgement and on previous studies). Relationships modelled with restricted cubic splines were presented as RR, comparing older patients (75th percentile of age) with younger patients (25th percentile) [12]. Two sensitivity analyses were performed. First, we excluded patients visiting the emergency department following a trauma. Secondly, to explore the potential impact of missing data, we identified characteristics associated with missing one-year mortality data using multivariable logistic regression. Factors associated with "missingness" (p <0.1) were then included in our model. Due to non-convergence of the model when using log-binomial regression, the sensitivity analysis used logistic regression and computed odds ratios (OR) and their 95% CI.
For all tests, a 5% level of significance was accepted. Stata (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC) was used for statistical analyses. Based on an anticipated incidence of 1%, a sample size of about 150,000 emergency department patients was calculated to be required to estimate this incidence with an error margin of ± 0.05%.
The study was conducted at the Geneva University Hospital in accordance with Good Clinical Practice (Declaration of Helsinki 2002). This study was approved on 23 August 2021 by the Institutional Ethics Committee of Geneva, Switzerland (Project 2021-01498). Patient consent was waived by this committee. There was neither patient nor public involvement in the project.
Between 1 January 2015 and 31 December 2019, 347,613 patients visited the emergency department. After exclusion of patients less than 18 years old (n = 8520), patients admitted for a psychiatric emergency only (n = 15,475) and patients who left the emergency department without consultation (n = 12,704), 310,914 patients remained.
Among the available emergency department visits, 3592 required emergency general surgery in the 72 hours following their emergency department admission (figure 1). Surgery was performed on 3594 different patients. The incidence of emergency general surgery was 116 per 10,000 emergency department visits (95% CI: 112–119). In our subgroup analysis, the incidence of emergency general surgery per 10,000 emergency department visits was 127 for female patients and 105 for male patients; 121 for patients younger than 65 years old and 102 for patients of 65 or older; 187 in the stretcher bay sector and 4 in the ambulatory setting. Figure 2 shows the relationship between patient age and incidence of emergency general surgery per 10,000 emergency department visits.
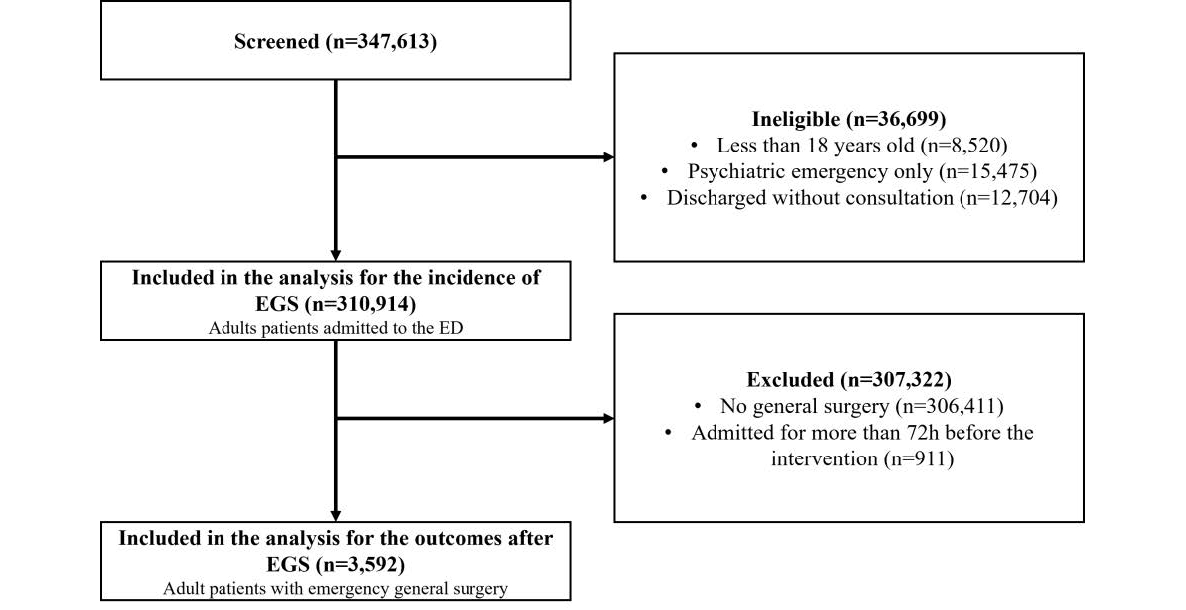
Figure 1Flowchart of patients included in the study. EGS: Emergency general surgery; ED: Emergency department.
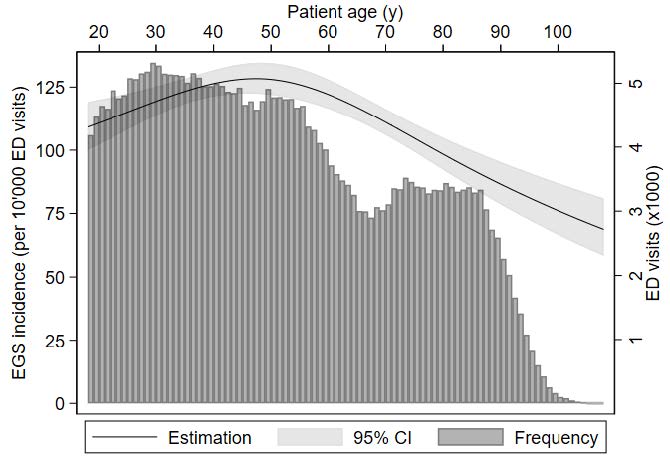
Figure 2Incidence of emergency general surgery by age among emergency department (ED) patients. The curve represents the unadjusted estimation of the incidence of emergency general surgery (EGS) (left vertical axis) while the vertical bars represent the number of patients admitted to the emergency department (right vertical axis).
Table 1 presents the characteristics of patients undergoing emergency general surgery during the first 72 hours of their stay. For baseline characteristics, no variable had more than 10% of missing data, except for body mass index (BMI) (26%). Patients had a mean age of 50 (SD = 20) years, with a similar proportion of females and males. Very few patients were living in a nursing home before hospitalisation. Patients were mainly admitted during the day (60.5%). Triage level was 1 (highest acuity) for 105 patients (2.9%), 2 for 1250 patients (34.8%) and 3 for 2211 patients (61.6%). The majority of patients (72.5%) were attending the emergency department for abdominal pain. One in ten patients had fever on admission and less than 5% presented with a positive shock index. More than half of the patients presented with a high leucocyte count and about 60% had an elevated CRP level. The median length of stay in the emergency department was 6.7 hours (IQR: 3.9–10.5). Finally, the median time between the emergency department admission and the operating theatre admission was 14 hours: 990 patients (27.6%) went directly from the emergency department to the operating theatre, while 72.7% and 91.1% of patients had their intervention during the 24 and the 48 first hours, respectively. Age influenced the time between emergency department admission and OR admission, with older patients spending an extra 4.1 hours (95% CI: 2.9–5.4) in the emergency department.
Table 1Patient characteristics of those undergoing surgery. IQR: interquartile range; SD: standard deviation.
| All patients (n = 3592) | ||
| Female – n (%) | 1846 (51.5) | |
| Age (years) – median (IQR) | 49 (33–65) | |
| Age ≥65 years old – n (%) | 926 (25.8) | |
| Place of living before hospitalisation – n (%) | Home | 3532 (98.3) |
| Nursing home | 60 (1.7) | |
| Acute hospitalisation in the previous year – n (%) | 0 | 2795 (77.8) |
| 1–2 | 629 (17.5) | |
| >2 | 168 (4.7) | |
| Emergency department visits in the previous year – n (%) | 0 | 2477 (69.0) |
| 1–2 | 896 (24.9) | |
| >2 | 219 (6.1) | |
| Admission by ambulance or equivalent – n (%) | 907 (25.3) | |
| Emergency department triage level – n (%) | 1 (highest acuity) | 105 (2.9) |
| 2 | 1250 (34.8) | |
| 3 | 2211 (61.6) | |
| 4 (lowest acuity) | 21 (0.6) | |
| Missing | 5 (0.1) | |
| Trauma patients – n (%) | 23 (0.6) | |
| Night admission (6 PM – 7 AM )– n (%) | 1357 (37.8) | |
| Week-end admission – n (%) | 846 (23.6) | |
| Body mass index (kg/m2) – mean ± SD [missing] | 26.6 ± 5.9 [947] | |
| Emergency department vital signs [missing] | Systolic blood pressure (mm Hg) – mean (±SD) | 131 ± 21 [53] |
| Diastolic blood pressure (mm Hg) – mean (±SD) | 81 ± 14 [62] | |
| Mean arterial pressure <65 mm Hg – n (%) | 49 (1.4) [62] | |
| Heart rate (min–1) – mean (±SD) | 86 ± 18 [51] | |
| Temperature (°C) – mean (±SD) | 37.0 ± 0.8 [110] | |
| Laboratory values – median (IQR) [missing] | Creatinine (μmol/l) | 75 (63–90) [216] |
| Haemoglobin (g/l) | 139 (128–151) [182] | |
| Leucocytes (G/l) | 11.6 (8.7–15.3) [196] | |
| C-reactive protein (mg/l) | 26.4 (5.7–92.1) [301] | |
| Emergency department length of stay (hours) – median (IQR) | 6.7 (3.9–10.5) | |
| Diabetes – n (%) | 243 (6.8) | |
| Hypertension – n (%) | 693 (19.3) | |
| History of myocardial infarction – n (%) | 133 (3.7) | |
| Chronic obstructive pulmonary disease – n (%) | 75 (2.1) | |
| Cognitive impairment – n (%) | 64 (1.8) | |
| Time to operating theatre (hours) – median (IQR) | 14.0 (7.3–26.3) | |
Overall, the main intervention performed was appendectomy (45.2%) (table 2). Among young patients, this represented more than half of the interventions, while in older patients, cholecystectomy was the most frequent surgery.
Table 2Main intervention performed, stratified by risk category – n (%).
| Total | Male | Female | 18–64 years | ≥65 years | ||
| Low risk | 2794 (77.8) | 1353 (77.6) | 1441 (77.9) | 2294 (86.0) | 500 (54.0) | |
| Appendectomy | 1625 (45.2) | 842 (48.3) | 783 (42.4) | 1485 (55.7) | 140 (15.1) | |
| Cholecystectomy | 1169 (32.5) | 511 (29.3) | 658 (35.6) | 809 (30.4) | 360 (38.9) | |
| High risk | 798 (22.2) | 390 (22.4) | 408 (22.4) | 372 (14.0) | 426 (46.0) | |
| Large bowel resection | 259 (7.2) | 127 (7.3) | 132 (7.1) | 95 (3.6) | 164 (17.7) | |
| Lysis of adhesions | 216 (6.0) | 84 (4.8) | 132 (7.1) | 107 (4.0) | 109 (11.8) | |
| Small bowel resection | 152 (4.2) | 68 (3.9) | 84 (4.6) | 68 (2.6) | 84 (9.1) | |
| Peptic ulcer repair | 79 (2.2) | 55 (3.2) | 24 (1.3) | 47 (1.8) | 32 (3.5) | |
| Laparotomy for another reason | 92 (2.6) | 56 (3.2) | 36 (2.0) | 55 (2.1) | 37 (4.0) |
A total of 191 patients (5.3%) were admitted to the ICU during their stay, of whom 160 (83.8%) were admitted directly from the emergency department or the operating theatre (table 3). Their mean length of stay in the ICU was 6.5 days. Among those alive at discharge and not living in a nursing home before hospitalisation, 270 (7.8%) patients were discharged from acute care as dependent. Data regarding mortality were missing for 633 (17.6%), 708 (19.7%), and 1088 (30.3%) patients at 30 days, 90 days, and one year, respectively. At 30 days, 49 of 2959 (1.7%) patients with follow-up had died; at 90 days and one year, mortality rates were 78 of 2884 (2.7%) and 121 of 2504 (4.8%) patients, respectively.
Table 3Outcomes after emergency general surgery. ICU: intensive care unit.
| Total | Male | Female | 18–64 years | ≥65 years | |
| ICU admission – n (%) | 191 (5.3) | 128 (7.3) | 63 (3.4) | 79 (3.0) | 112 (12.1) |
| ICU length of stay (d) – mean (95% CI) | 3.7 (3.2–4.3) | 3.8 (3.2–4.6) | 3.4 (2.5–4.5) | 4.2 (3.3–5.2) | 3.4 (2.7–4.2) |
| Hospital length of stay (d) – mean (95% CI) | 4.6 (4.4–4.7) | 4.7 (4.5–4.9) | 4.5 (4.3–4.7) | 3.6 (3.5–3.7) | 9.2 (8.7–9.8) |
| Dependent at discharge* – n (%) | 270 (7.8) | 123 (8.2) | 147 (7.3) | 42 (1.6) | 228 (27.5) |
| 30-day mortality** – n (%) | 49 (1.7) | 30 (2.1) | 19 (1.2) | 9 (0.4) | 40 (4.9) |
| 90-day mortality** – n (%) | 78 (2.7) | 50 (3.7) | 28 (1.9) | 19 (0.9) | 59 (7.4) |
| One-year mortality** – n (%) | 121 (4.8) | 74 (6.4) | 47 (3.5) | 29 (1.6) | 92 (13.0) |
* Among patients alive at discharge and not in a nursing home before hospitalisation (n = 3468).
** Data were missing for 633, 708 and 1088 patients at 30 days, 90 days and 1 year, respectively.
Figure 3 shows the unadjusted associations between age and ICU admission, dependence at discharge and one-year mortality. After adjusting for sex, admission by ambulance, triage level and the risk of the intervention, older patients were more often admitted to the ICU (aRR = 2.9 [95% CI: 1.5–5.4]), were more frequently dependent at discharge (aRR = 15.3 [95% CI 5.5–42.4]) and had a higher one-year mortality (aRR = 5.4 [95% CI: 2.2–13.4]) (table 4).
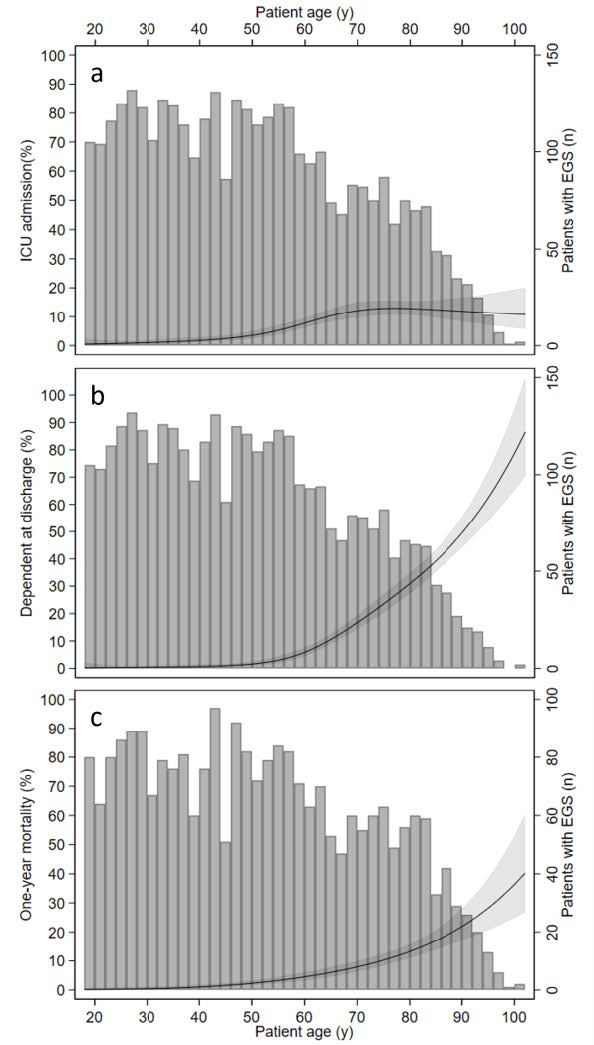
Figure 3Outcomes after emergency general surgery by age: (A) Intensive care unit (ICU) admission; (B) dependent at discharge; (C) one-year mortality. In each figure, the curve represents the estimation of the incidence of the outcome (left vertical axis) while the vertical bars represent the number of patients who underwent emergency general surgery (EGS) and were considered for the outcome (right vertical axis).
Table 4Outcomes after emergency general surgery. Age was modelled using restricted cubic splines. Emergency triage levels were based on the Swiss Emergency Triage Scale (from level 1 [life/limb threatening] to level 4 [non-urgent]). High-risk procedures include large bowel resection, lysis of adhesions, small bowel resection, peptic ulcer repair and laparotomy for another reason. ICU: intensive care unit.
| ICU admission | Dependent at discharge | One-year mortality | ||||
| Risk ratio | 95% confidence interval | Risk ratio | 95% confidence interval | Risk ratio | 95% confidence interval | |
| Age (75th vs 25th percentile) | 2.9 | 1.5–5.4 | 15.3 | 5.5–42.4 | 5.4 | 2.2–13.4 |
| Male | 2.0 | 1.5–2.6 | 1.0 | 0.8–1.2 | 1.7 | 1.3–2.4 |
| Arrived with ambulance | 2.5 | 1.8–3.3 | 1.9 | 1.5–2.4 | 1.6 | 1.1–2.3 |
| Emergency triage level 1–2 | 2.2 | 1.6–3.1 | 1.3 | 1.1–1.6 | 1.3 | 0.9–1.8 |
| High-risk procedure | 5.3 | 3.7–7.6 | 2.7 | 2.1–3.5 | 4.65 | 3.0–7.3 |
Excluding patients with trauma (n = 24) from the analysis of one-year mortality increased the risk ratio. Factors associated with missing data for mortality at one year were sex, number of previous hospitalisations and emergency department visits, admission by ambulance, diabetes, history of myocardial infarction, type of surgery and ICU admission (table S2 in the appendix). After adjusting for factors associated with “missingness” in our analysis of one-year mortality, the association between age and mortality remained statistically significant but slightly decreased from OR = 5.2 [95% CI: 2.1–12.6] to OR = 3.6 [95% CI 1.5 to 8.6].
Our 5-year retrospective study showed that 116 per 10,000 emergency department patients had emergency general surgery and that, following surgery, ICU admission rates and one-year mortality rates were both about 5%. Additionally, it appears that, compared to young patients, older patients had a lower emergency general surgery incidence, but with a higher ICU admission rate and a higher mortality rate, and were more frequently dependent at discharge.
Emergency general surgical diagnoses are frequently an indication for patients to present to the emergency department. Indeed, emergency general surgery occurs 3 to 10 times more frequently than other serious conditions such as acute myocardial infarction, stroke, or pulmonary embolism [14, 15]. We also observed a reduction in the incidence of emergency general surgery with increasing age, which can be explained in several ways. First, other diagnoses such as heart failure, pneumonia or hip fracture are more frequent as patients become older [16]. Secondly, for a given surgical condition, non-operative management is known to be more frequently performed in older than in younger patients, probably because outcomes after surgery are worse. Hutchings et al. recently demonstrated that, for appendicitis and cholecystitis, older patients had lower odds of being surgically treated, after adjustment for co-morbidities and frailty [17].
We estimated a mortality rate at 30 days of about 2%, slightly lower than previous studies that reported a mortality rate between 4.5% and 9% [18–20]. While the study populations can differ based on the inclusion criteria, the difference in the setting should also be considered. In Switzerland, the density of nurses and physicians is usually higher than in other countries, and this can increase the quality of care and affect mortality rates [4]. Ozdemir et al. found that fewer general surgical doctors and lower nursing staff ratios were associated with higher mortality [20]. Nevertheless, studies on emergency general surgery in Switzerland are scarce. One study, focusing on colorectal cancer surgery, showed an in-hospital mortality of 8.4% [21]. In patients undergoing laparoscopic cholecystectomy, postoperative complications were more likely after emergency surgery, when compared with elective procedures [22]. A single-centre retrospective study conducted on older patients (80 years or older) showed an in-hospital mortality of 16.4%; there was an association between age and mortality and an association between intensive care unit admission and loss of independence [21]. However, this last study focused on older patients, and results can therefore not be applied to younger patients. In our study, we demonstrated a strong association between patient age and mortality, with the mortality rate in patients aged 65 years or older being four times higher than for younger patients. Wohlgemut et al. [23] reported an adjusted odds ratio of 15 for one-year mortality for patients older than 60, compared to younger patients. More recently, in a very similar setting, Magyar et al. found an odds ratio for in-hospital mortality 4 times higher in older patients and showed that the performance of quick Sequential Organ Failure Assessment (qSOFA) was increased when age was considered [24]. Different explanations can be put forward to explain this association. First, older patients more often have co-morbidities and are therefore more prone to complications. However, some authors have adjusted for co-morbidities and have still found an association between age and mortality [25]. Another explanation could be the severity of the disease, with older patients more seriously ill than younger patients. Finally, higher-risk interventions, such as bowel resection or lysis of adhesions, were more frequently performed in older patients, and this could bias the association [8].
Overall, 7.5% of patients were dependent at discharge. In the US, Paredes reported a lower proportion, about 4%, who were not discharged home [26]. Our rate is, however, lower than that which we find with internal medicine patients in our hospital, among whom up to 25% are not discharged home [27]. Surgical patients are usually younger and fitter than medical patients, and this may explain the difference. In our study, we found that older patients were much more likely not to be discharged than younger patients. Older patients were more likely to have high-risk and longer interventions. Their capacity to recover after this type of intervention might be slower and might justify their transfer to a rehabilitation unit.
Important limitations should be acknowledged. First, since this was a retrospective study on routinely collected data, we had some missing data. In our hospital, there was no possibility of matching hospital data with the death registry, and deaths outside the hospital could therefore be missed. This could bias the estimation of the mortality. In younger patients, this is likely an overestimation, as death outside the hospital is extremely rare. For older patients, the bias could be in either direction. Another limitation is the risk of residual confounding, since some important predictors such as frailty were not available [11]. We also chose a restricted definition of emergency general surgery, excluding diagnostic laparoscopy and incarcerated hernia, and this might affect the results. Finally, it was a single-centre study performed in a tertiary hospital, making the results less generalizable: the incidence of emergency general surgery might indeed differ between regions, even in Switzerland, since it depends on the number and the type of hospitals, emergency departments and primary care facilities in the surrounding area. For patient outcomes, generalisations should also be made with caution, since the management and procedures of the emergency departments and surgical wards can be very different.
This study also had some strengths. While it was a single-centre study, the sample size was large and allowed for stratified estimates of different subgroups, such as sex and age, with enough power to observe statistically significant differences. Most studies on emergency general surgery are from the surgical perspective, and this study is one of the first to examine outcomes from the perspective of the emergency physician. It is important, in our opinion, that emergency general surgery management starts in the emergency department and involves emergency physicians.
From a clinical perspective, this study gives information that can be shared with patients before surgery, such as mortality rate, ICU admission rate and orientation at discharge. This could help patients to understand the risks related to proposed interventions and could improve the shared decision-making process. Some patients might benefit from non-operative care, which could reduce non-beneficial and unwanted surgical care [28]. Emergency department management could also be improved on the basis of our results, with the implementation of risk-stratification tools.
This study also engenders additional research questions, especially among older patients, such as the association between frailty and outcomes in the Swiss healthcare system. It would be interesting to examine diagnoses rather than procedures, to see whether emergency general surgeries are performed less frequently on older than younger patients with a similar diagnosis. Future studies should focus on predictors of independence at discharge and quality of life, since these outcomes might be as important as mortality for those patients [29]. Qualitative studies among patients could help to understand their decision-making process regarding therapeutic options. Finally, the stratification by sex showed some interesting differences, such as a decrease in ICU admission among female patients. A future study that specifically examines sex differences could be performed to determine whether these differences are due to differences in management or potentially due to confounding.
Emergency department visits resulting in emergency general surgery are frequent but decrease with age. However, mortality, ICU admission and dependence at discharge following emergency general surgery are more frequent in older patients. Given the risk for older patients, a shared decision-making process is appropriate to make a more informed decision about their care options.
The data that support the findings are publicly available on the Open Science Framework (OSF, https://www.doi.org/10.17605/OSF.IO/TRU4N).
We would like to thank Jimison Iavindrasana for his help in the data extraction.
Authors’ contributions (based on CREDIT taxonomy): Conceptualisation: CAF, MT, DIM, DE, JJP. Data curation: CAF. Formal analysis: CAF. Investigation: CAF. Methodology: CAF. Project administration: JJP. Supervision: MT, DIM, DE, JJP. Visualisation: CAF. Writing – original draft: CAF. Writing – review & editing: CAF, MT, DIM, LS, EA, AD, FR, DE, JJP.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Shafi S, Aboutanos MB, Agarwal S Jr, Brown CV, Crandall M, Feliciano DV, et al.; AAST Committee on Severity Assessment and Patient Outcomes. Emergency general surgery: definition and estimated burden of disease. J Trauma Acute Care Surg. 2013 Apr;74(4):1092–7. 10.1097/TA.0b013e31827e1bc7
2. To KB, Kamdar NS, Patil P, Collins SD, Seese E, Krapohl GL, et al.; Michigan Surgical Quality Collaborative (MSQC) Emergency General Surgery Study Group and the MSQC Research Advisory Group. Acute Care Surgery Model and Outcomes in Emergency General Surgery. J Am Coll Surg. 2019 Jan;228(1):21–28.e7. 10.1016/j.jamcollsurg.2018.07.664
3. Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, et al. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015 Feb;78(2):306–11. 10.1097/TA.0000000000000517
4. OECD. Health Care Resources 2019. [cited 2020; Available from: https://stats.oecd.org/index.aspx?DataSetCode=HEALTH_REAC#
5. Fowler AJ, Abbott TE, Prowle J, Pearse RM. Age of patients undergoing surgery. Br J Surg. 2019 Jul;106(8):1012–8. 10.1002/bjs.11148
6. Al-Temimi MH, Griffee M, Enniss TM, Preston R, Vargo D, Overton S, et al. When is death inevitable after emergency laparotomy? Analysis of the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg. 2012 Oct;215(4):503–11. 10.1016/j.jamcollsurg.2012.06.004
7. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007 Oct;370(9596):1453–7. 10.1016/S0140-6736(07)61602-X
8. Feeney T, Castillo-Angeles M, Scott JW, Nitzschke SL, Salim A, Haider AH, et al. The independent effect of emergency general surgery on outcomes varies depending on case type: A NSQIP outcomes study. Am J Surg. 2018 Nov;216(5):856–62. 10.1016/j.amjsurg.2018.03.006
9. Rutschmann OT, Kossovsky M, Geissbühler A, Perneger TV, Vermeulen B, Simon J, et al. Interactive triage simulator revealed important variability in both process and outcome of emergency triage. J Clin Epidemiol. 2006 Jun;59(6):615–21. 10.1016/j.jclinepi.2005.11.003
10. Bloom DE, Mitgang E, Osher B. Demography of global ageing, in Oxford Textbook of Geriatric Medicine, J.-P. Michel, et al., Editors. 2017, Oxford University Press. p. 0. 10.1093/med/9780198701590.003.0001
11. Parmar KL, et al. Frailty in Older Patients Undergoing Emergency Laparotomy: Results From the UK Observational Emergency Laparotomy and Frailty (ELF) Study. Ann Surg. 2019.
12. Harrell FE. General Aspects of Fitting Regression Models, in Regression Modeling Strategies. 2015, Springer International Publishing. p. 13-44. 10.1007/978-3-319-19425-7_2
13. Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012 May;184(8):895–9. 10.1503/cmaj.101715
14. Pendyal A, Rothenberg C, Scofi JE, Krumholz HM, Safdar B, Dreyer RP, et al. National Trends in Emergency Department Care Processes for Acute Myocardial Infarction in the United States, 2005 to 2015. J Am Heart Assoc. 2020 Oct;9(20):e017208. 10.1161/JAHA.120.017208
15. Kline JA, Garrett JS, Sarmiento EJ, Strachan CC, Courtney DM. Over-Testing for Suspected Pulmonary Embolism in American Emergency Departments: The Continuing Epidemic. Circ Cardiovasc Qual Outcomes. 2020 Jan;13(1):e005753. 10.1161/CIRCOUTCOMES.119.005753
16. Ukkonen M, Jämsen E, Zeitlin R, Pauniaho SL. Emergency department visits in older patients: a population-based survey. BMC Emerg Med. 2019 Feb;19(1):20. 10.1186/s12873-019-0236-3
17. Hutchings A, Moler Zapata S, O’Neill S, Smart N, Cromwell D, Hinchliffe R, et al. Variation in the rates of emergency surgery amongst emergency admissions to hospital for common acute conditions. BJS Open. 2021 Nov;5(6):zrab094. 10.1093/bjsopen/zrab094
18. Chana P, Joy M, Casey N, Chang D, Burns EM, Arora S, et al. Cohort analysis of outcomes in 69 490 emergency general surgical admissions across an international benchmarking collaborative. BMJ Open. 2017 Mar;7(3):e014484. 10.1136/bmjopen-2016-014484
19. Sangji NF, Bohnen JD, Ramly EP, Yeh DD, King DR, DeMoya M, et al. Derivation and validation of a novel Emergency Surgery Acuity Score (ESAS). J Trauma Acute Care Surg. 2016 Aug;81(2):213–20. 10.1097/TA.0000000000001059
20. Ozdemir BA, Sinha S, Karthikesalingam A, Poloniecki JD, Pearse RM, Grocott MP, et al. Mortality of emergency general surgical patients and associations with hospital structures and processes. Br J Anaesth. 2016 Jan;116(1):54–62. 10.1093/bja/aev372
21. Lavanchy JL, Holzgang MM, Haltmeier T, Candinas D, Schnüriger B. Outcomes of emergency abdominal surgery in octogenarians: A single-center analysis. Am J Surg. 2019 Aug;218(2):248–54. 10.1016/j.amjsurg.2018.11.023
22. Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krähenbühl L; Swiss Association of Laparoscopic and Thoracoscopic Surgery (SALTS) Study Group. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 2006 Nov;203(5):723–8. 10.1016/j.jamcollsurg.2006.07.018
23. Wohlgemut JM, Ramsay G, Bekheit M, Scott NW, Watson AJ, Jansen JO. Emergency general surgery: impact of distance and rurality on mortality. BJS Open. 2022 Mar;6(2):zrac032.
24. Magyar CT, Haltmeier T, Dubuis JB, Osterwalder A, Winterhalder S, Candinas D, et al. Performance of quick sequential organ failure assessment and modified age disease adjusted qadSOFA for the prediction of outcomes in emergency general surgery patients. J Trauma Acute Care Surg. 2022 Oct;93(4):558–65. 10.1097/TA.0000000000003742
25. Castillo-Angeles M, Cooper Z, Jarman MP, Sturgeon D, Salim A, Havens JM. Association of Frailty With Morbidity and Mortality in Emergency General Surgery By Procedural Risk Level. JAMA Surg. 2020. 10.1001/jamasurg.2020.5397
26. Paredes AZ, Malik AT, Cluse M, Strassels SA, Santry HP, Eiferman D, et al. Discharge disposition to skilled nursing facility after emergent general surgery predicts a poor prognosis. Surgery. 2019 Oct;166(4):489–95. 10.1016/j.surg.2019.04.034
27. Fehlmann C, Louis Simonet M, Reny JL, Stirnemann J, Blondon K. Associations between early handoffs, length of stay and complications in internal medicine wards: A retrospective study. Eur J Intern Med. 2019 Sep;67:77–83. 10.1016/j.ejim.2019.07.003
28. Baimas-George M, Yelverton S, Ross SW, Rozario N, Matthews BD, Reinke CE. Palliative Care in Emergency General Surgery Patients: Reduced Inpatient Mortality And Increased Discharge to Hospice. Am Surg. 2021 Jul;87(7):1087–92. 10.1177/0003134820956942
29. Rubin EB, Buehler AE, Halpern SD. States Worse Than Death Among Hospitalized Patients With Serious Illnesses. JAMA Intern Med. 2016 Oct;176(10):1557–9. 10.1001/jamainternmed.2016.4362
Table S1Institutional databases and codes.
| Type of variables | Variable | Database | Codes (if applicable) |
| Inclusion | Care episode starting in the emergency department | SILEX | Start of the care episode in the emergency department |
| Exclusion | Age <18 | DPA, SILEX | Start date: birthday <18 years old |
| Psychiatric emergency only | DPI | FLAG_QUEU388 | |
| Discharged without consultation | DPI | FLAG_REPSANSCONS | |
| Outcomes | Emergency general surgery | DPICodage | CHOP (Z44.40, Z44.41, Z44.42, Z45.6, Z45.7, Z45.8, Z47.0, Z51.2, Z54.1, Z54.5) |
| Death date | DPA | DT_DECES, DERNIER_EDS | |
| ICU admission | SILEX | OCLSI-US, OPERASI-US | |
| Dependent at discharge | DPA, SILEX | DESTINATION | |
| Confounders | Comorbidity | DPICodage | ICD10 (I11, I12, I13, I14, I15, I21, I22, I23, I24, I25, E10, E11, E12, E13, E14, F01, F02, F03, F06.7, U51.1, U51.2, J42, J43, J44) |
| Sex | DPA | PATIENT_SEXE | |
| Arrived by ambulance | DPI | MODE_ARRIVEE | |
| High risk | DPICodage | ||
| Triage level | DPI | NIVEAU_URGENCE | |
| Others | |||
| Laboratory | Unilab2 |
Table S2Factors associated with missing data for one-year mortality.
| Odds ratio | 95% conficence interval | p value | ||||
| Male | 1.39 | 1.19 | – | 1.62 | 0.000 | |
| 65 years or older | 0.88 | 0.71 | – | 1.10 | 0.265 | |
| Living in a nursing home | 0.92 | 0.46 | – | 1.83 | 0.802 | |
| Acute hospitalisation in the previous year | 0 | |||||
| 1–2 | 0.62 | 0.48 | – | 0.80 | 0.000 | |
| >2 | 0.16 | 0.06 | – | 0.42 | 0.000 | |
| Emergency department visits in the previous year | 0 | |||||
| 1–2 | 0.58 | 0.47 | – | 0.71 | 0.000 | |
| >2 | 0.34 | 0.19 | – | 0.62 | 0.000 | |
| Admission by ambulance or equivalent | 1.46 | 1.20 | – | 1.77 | 0.000 | |
| Triage level 1 or 2 | 1.00 | 0.85 | – | 1.19 | 0.956 | |
| Abdominal pain as triage motive | 1.04 | 0.87 | – | 1.24 | 0.651 | |
| Trauma | 1.46 | 0.40 | – | 5.41 | 0.569 | |
| Weekend admission | 1.13 | 0.94 | – | 1.34 | 0.185 | |
| Night admission | 0.92 | 0.79 | – | 1.08 | 0.304 | |
| Hypertension | 0.94 | 0.74 | – | 1.21 | 0.646 | |
| Diabetes | 0.70 | 0.48 | – | 1.02 | 0.062 | |
| History of myocardial infarction | 0.59 | 0.33 | – | 1.05 | 0.074 | |
| Chronic obstructive pulmonary disease | 1.09 | 0.56 | – | 2.11 | 0.810 | |
| Cognitive impairment | 1.06 | 0.48 | – | 2.36 | 0.889 | |
| Fever | 0.94 | 0.72 | – | 1.22 | 0.628 | |
| High-risk intervention | 0.75 | 0.60 | – | 0.95 | 0.015 | |
| ICU admission | 0.49 | 0.30 | – | 0.80 | 0.004 | |