Economic evaluation in the treatment of unruptured intracranial aneurysms in the Swiss
healthcare system: a retrospective cost evaluation
DOI: https://doi.org/https://doi.org/10.57187/s.3727
Ulf C. Schneiderabc,
Stephan Bohlhaltercde,
Florian Wüthrichf,
Dirk Lehnickb,
Alexander von Hesslingbcg
a Department of Neurosurgery, Cantonal Hospital
of Lucerne, Lucerne, Switzerland
b Faculty of Health Sciences and Medicine,
University of Lucerne, Lucerne, Switzerland
c Neurocenter, Cantonal Hospital of Lucerne,
Lucerne, Switzerland
d Department of Neurology and
Neurorehabilitation, Cantonal Hospital of Lucerne, Lucerne, Switzerland
e Department of Neurology, University of Zurich, Zurich, Switzerland
f Div. Med. Controlling and Coding, Cantonal
Hospital of Lucerne, Lucerne, Switzerland
g Section of Neuroradiology, Cantonal
Hospital of Lucerne, Lucerne, Switzerland
Summary
The choice of modality of treatment for unruptured
intracranial aneurysms is based on various clinical aspects and the patient’s
preference. Financial considerations should not be among these. To evaluate any
financial variations between endovascular and microsurgical treatment of unruptured
intracranial aneurysms in the Swiss healthcare system, we retrospectively
reviewed 100 consecutive aneurysm cases treated as inpatients in our
institution.
Case-based financial data were collected
(revenues, costs, net earnings) and compared between the treatments.
Among 100 consecutive aneurysm cases
treated at our institution (2021–2023), 58 were unruptured intracranial
aneurysm. Treatment was endovascular in 33, microsurgery in 23 and conservative/antibiotic
in 2 cases. Length of stay (but not duration in the intensive care unit) was
longer after microsurgical treatment. Total median revenues (public insurance,
private insurance, material reimbursement) were Swiss Francs (CHF) 30,012.25
with a maximum of CHF 125,337.20 and a minimum of CHF 9543.25. No marked
difference was found between the treatment groups (endovascular and
microsurgery). Despite the fact that median net earnings per patient were
positive (CHF 3655.03), more than one third of all cases led to a net loss for
the hospital with a tendency for more stable net earnings in microsurgery cases.
The only factor associated with a higher risk of net loss per case was higher implant
costs in endovascular cases.
Reimbursement within the Swiss healthcare
system does not promote financial bias for decision-making in treatment
modality for unruptured intracranial aneurysm. The fact that one third of all
cases does not result in positive net earnings (even in the highly paid unruptured
intracranial aneurysm sector), although overall net earnings were positive, should
be monitored – especially in times of rising costs.
Introduction
Decision-making for the modality of treatment
of unruptured intracranial aneurysms may be based on various aspects. Medical arguments,
usually foremost, comprise the durability of the treatment; the configuration, size
and location of the unruptured intracranial aneurysm; comorbidities; treatment complexity;
invasiveness; need for anti-aggregation or invasive follow-up diagnostics, etc.
Even though counselling should primarily be based on medical factors, non-medical
considerations might also play a role in deciding whether endovascular or
microsurgical treatment of an unruptured intracranial aneurysm is recommended. These
may include personal preferences or beliefs (held by the treating professional or
the patient) or financial considerations [1–4].
In 2015, Swiss healthcare costs had risen
to 11.7% of Gross Domestic Product (GDP) [5], the second highest in Europe. According
to 2013 Organisation for Economic Co-operation and Development (OECD)
statistics, annual healthcare expenditure per capita exceeded US$ 5500 and was
ranked second highest among 27 countries evaluated [6]. According to the same data,
the density of
nurses and psychiatrists in Switzerland is the highest among OECD countries, while
the number of physicians per capita is among the highest. Thus, the Swiss
healthcare system can be considered excellent although expensive [7].
In common with many other healthcare
systems worldwide, reimbursement for in-hospital treatments in the Swiss
healthcare system is based on diagnosis-related groups (DRGs). The final amount
reimbursed for a treatment is therefore dependent on various factors, such as the
primary diagnosis, secondary illnesses or pre-conditions, complications
throughout the stay and the method of treatment. In Switzerland, the method of
treatment is based on the Swiss (CH) Operation Classification (CHOP), which was
derived from the international statistical classification of diseases and
related health problems (ICD). The reimbursement for a given disease may vary as
it depends on the particular treatment method / CHOP code used. Usually, operative
CHOP codes contribute to higher reimbursements than non-operative codes (www.bfs.admin.ch
or www.swissdrg.org).
As in most European healthcare facilities,
financial controlling in Swiss hospitals is carried out by economists or
accountants, who regularly update the leading physicians on relevant numbers including
Earnings Before Interest, Taxes, Depreciation and Amortisation (EBITDA) and the
corresponding margin.
Whenever monetary considerations play into
medical decision-making, risks of bias arise.
To closely monitor eventual monetary bias risks
for medical decision-making and to detect potential risk factors for negative net
earnings, we evaluated the treatment of unruptured intracranial aneurysm in
particular as it is, on the one hand, a high-volume business (in terms of costs
and earnings) and, on the other hand, a highly discussed medical decision
process.
Methods
We reviewed the treatment costs of 100 consecutive
cases with intracranial aneurysms admitted for inpatient treatment at our
hospital within the past two years (23 February 2021 – 30 March 2023), of which
58 were unruptured.
Rationale of local multidisciplinary
decision-making at our institution: Our hospital is a tertiary care centre in
central Switzerland within an area of coverage of approximately 800,000 people.
We have a dedicated neurovascular decision and treatment team, on on-call and off-call
duty, that consists of two neurosurgeons trained in neurovascular microsurgery
and three interventional neuroradiologists trained in endovascular procedures. All
microsurgical and endovascular techniques for the treatment of unruptured
intracranial aneurysm are thus offered at our institution.
All elective procedures are routinely
processed within a weekly neurovascular board. Treatment recommendations are
mutually made and brought to the patients, mainly taking into account standard considerations
like patient
characteristics (age, comorbidities, medication, preferences), aneurysm
characteristics (size, accessibility, aspect ratio, shape) and treatment
characteristics (durability, need for additional devices/medication). Non-elective
procedures, which require immediate action, are decided bilaterally (neurosurgery
and interventional neuroradiology). Re-evaluation of these decisions is
regularly done through post hoc discussion in the board.
Net earnings and revenues of the 58 cases
of unruptured intracranial aneurysm treated in the corresponding time period were
reviewed on an individual case basis; revenues were further divided into general
revenue by public insurance, additional revenue by private insurance and implant
revenue. Treatment costs per case were further divided into facility costs/interests/depreciation,
general costs of treatment and direct case costs, the last item comprising
implant costs. This definition – as set by our local controlling
persons – divides everything that goes into one individual patient (e.g. implants,
medication, etc; direct
case costs) from costs that arise during treatment and can only be attributed by
time or area used (e.g. cost of nursing staff, operating theatre time,
physician costs, anaesthesia, room capacity, etc; general costs of treatment). The
following patient and treatment characteristics were obtained from our patient information
system (EPIC System Corporation, Verona, WI, USA): Unruptured intracranial
aneurysm treatment (microsurgery, endovascular), discharge (home,
rehabilitation, nursing care, death), duration of stay (days), number of intensive
care unit (ICU) hours, complexity of care in ICU (Nine Equivalents of nursing Manpower
Score or NEMS [8] and Simplified Acute Physiology Score or SAPS [9]).
Treatment decisions were completely
independent of this evaluation.
Statistical analysis was done using Stata 18
(StatCorp LLC, Texas, USA). Data are not normally distributed. Values are given
as median and interquartile ranges (Q1–Q3), whenever appropriate. For two-sample
comparison, the Wilcoxon rank-sum test (Mann-Whitney) was applied. Currency is
CHF (Swiss Francs).
Due to the retrospective nature of the
study, a protocol was not prepared. Trial registration was not applicable.
Results
Over the 105-week period, 100 cases of
intracranial aneurysms received inpatient treatment at our institution, of
which 58 were unruptured.
Of these 58 cases, 23 were treated
microsurgically, 33 were treated endovascularly and 2 were treated
conservatively (one received antibiotic treatment, the other anti-seizure
medication). In 55 cases, only one aneurysm was treated at the time. In 3 cases
(all microsurgery), 2 aneurysms were treated concurrently. Given that treatment
decisions, as well as costs and revenues, were completely different in the two
conservatively treated cases, these were not included in further analyses.
Hence all analyses comprise 56 treated patients.
Patient
characteristics showed a higher percentage of endovascular treatment in the
posterior circulation, but otherwise did not differ markedly between
microsurgically and endovascularly treated cases. Of the 56 patients, 48 were
discharged home directly, while 6 went to rehabilitation before returning home
(4 after microsurgery and 2 after endovascular therapy). One patient was
discharged to a nursing home and another died in hospital, both after
endovascular treatment (table 1).
Table 1Patient characteristics (total case number of 56: 33 endovascular cases plus 23
microsurgical cases – 2 conservative cases were excluded from further
analysis).
|
Endovascular (n = 33) |
Microsurgery (n = 23) |
| Age (years, mean±SD) |
58±12 |
60±8 |
| Gender (f:m:d) |
22:11:0 |
15:8:0 |
| Aneurysm location |
Anterior |
25 (76%) |
22 (96%) |
| Posterior |
8 (24%) |
1 (4%) |
| Discharge |
Home |
29 (88%) |
19 (83%) |
| Rehabilitation |
2 (6%) |
4 (17%) |
| Nursing Care |
1 (3%) |
0 (0%) |
| Death |
1 (3%) |
0 (0%) |
Mean treatment characteristics of both
groups are summarised in table 2. Patients stayed in hospital for a
median (Q1–Q3) of 4 (2–7) days for their treatment. Length of stay was longer in
microsurgery cases: 6 (4–8) vs 3 (2–5). Median duration of stay in the ICU was
volatile, but without obvious differences between the two groups (combined: 20 [18–24];
microsurgery: 21 [19–25]; endovascular: 19 [18–23]). It is therefore noteworthy
that the SAPS scores were higher in the endovascular cases, but the NEMS scores
were higher in microsurgery cases (SAPS: approx. 25% difference; NEMS: approx. 50%
difference, when comparing the medians) (table 2).
Table 2Treatment characteristics (total of 56 cases: 33 endovascular plus 23
microsurgical cases – 2 conservative cases were excluded from further
analysis). Results indicated as median and interquartile range (Q1–Q3).
|
Total (n = 56) |
Endovascular (n = 33) |
Microsurgery (n = 23) |
| Length of stay (days) |
4 (2–7) |
3 (2–5) |
6 (4–8) |
| Time on ICU (hours) |
20 (18–24) |
19 (18–23) |
21 (19–25) |
| SAPS points |
20 (15–23) |
20 (17–25) |
16 (14–19) |
| NEMS points |
60 (42–78) |
48 (39–42) |
72 (63–78) |
Median (Q1–Q3) total revenue per case was
CHF 30,012.25 (24,235.05–40,563.28) with a maximum of CHF 125,337.20 and a
minimum of CHF 9543.25. No marked difference was found between the treatment
groups, with CHF 29,102.28 (22,206.52–42,702.28) for the microsurgery vs CHF 30,012.25
(25,468.02–38,246.25) for the endovascular cases, respectively (p = 0.94). Median
(Q1–Q3) revenues by public insurances and additional revenues by private
insurances were, respectively, CHF 23,859.71 (22,022.49–29,102.28) and CHF 0 (0–0);
there were no visible differences for microsurgery vs endovascular cases,
either for public insurances (CHF 29,102.2 [22,019.13–38,257.64] vs CHF 23,859.71
[22,728.76–27,307.42]; p = 0.41) or private insurances (CHF 0 [0–10,585.00] vs
CHF 0 [0–0]; p = 0.14). Additional implant reimbursements were CHF 1435.06 (0–6152.54),
being, as expected, almost exclusively attributable to endovascular cases: CHF 0
(0–0) and CHF 3204.14 (1793.83–6457.50) in microsurgery and endovascular cases,
respectively; p = 0.00001.
Total costs were CHF 26,226.89 (23,058.24–33,251.15)
and comparable between the groups: CHF 26,223.10 (19,559.13–33,838.19) and CHF 26,230.69
(23,565.75–30,161.02) for microsurgery and endovascular groups, respectively (p
= 0.72).
Direct case costs were lower and less
volatile in microsurgery cases: CHF 4261.22 (3586.20–4780.25) and CHF 16,653.82
(15,004.93–18,432.49) in microsurgery and endovascular cases, respectively; p =
0.0001. Implant costs were substantially higher in endovascular cases and contributed
substantially to direct case costs: CHF 1052.79 (836.09–1372.98) and 13,212.33
(10,467.78–13,757.82) in microsurgery and endovascular cases, respectively; p =
0.0001. Conversely, general costs of treatment were substantially higher in
microsurgery cases: CHF 19,866.94 (14,650.47–25,154.77) and CHF 8966.79 (7403.24–11,439.67)
in microsurgery and endovascular cases, respectively; p = 0.0001. Facility
costs/interest/depreciation did contribute to total costs, but were as low as
CHF 2334.36 (1533.92–2773.44) and 1106.79 (745.37–1444.93) for microsurgery and
endovascular cases, respectively (p = 0.001); as expected, they were higher in microsurgery
cases due to longer duration of stay.
The most pronounced difference was thus
seen in the weighting of direct case costs and general costs of treatment,
which showed anticipated differences between the two groups, that, in the end,
were balanced in the total costs.
Given higher median total revenues than
total costs per case, median net earnings per case could be achieved and were
as high as CHF 3655.03 (%1310.69–9267.88) with a tendency for a lower risk of net
losses in microsurgery cases at CHF 5818.62 (−372.22–12,261.83)
vs 1145.27 (−2851.13–6925.50) for endovascular cases, p = 0.08 (figure 1).

Figure 1Graphical display of net earnings
and revenues (left) and costs (right) per case, divided into microsurgery cases
(blue) and endovascular cases (red). All revenues and costs showed high
volatility. Median total revenues were higher than median total costs thus net
earnings per case could be obtained (far left). Total revenues (2nd
from left) are divided into revenues by public insurance (3rd from
left) plus additional implant revenues (whenever feasible, 4th from
left) plus additional revenues by private insurance (in 14 cases, 5th
from left). The differences on the side of earnings were higher additional
implant revenues in endovascular cases (p = 0.00001) and a tendency to higher
additional revenues from private insurances in microsurgery cases (p = 0.14).
Total costs (leftmost) derive from facility costs/interest depreciation (2nd
from left), general costs of treatment (3rd from left) and direct
case costs (4th from left). The latter comprise implant costs (far
right column, separated). Higher facility costs/depreciation/interest were
documented in microsurgery cases (p = 0.001), while higher implant costs arose
in endovascular cases (p = 0.0001). All data given as median and interquartile
ranges. Monetary values are displayed in CHF (Swiss Francs). EVT: endovascular
treatment.
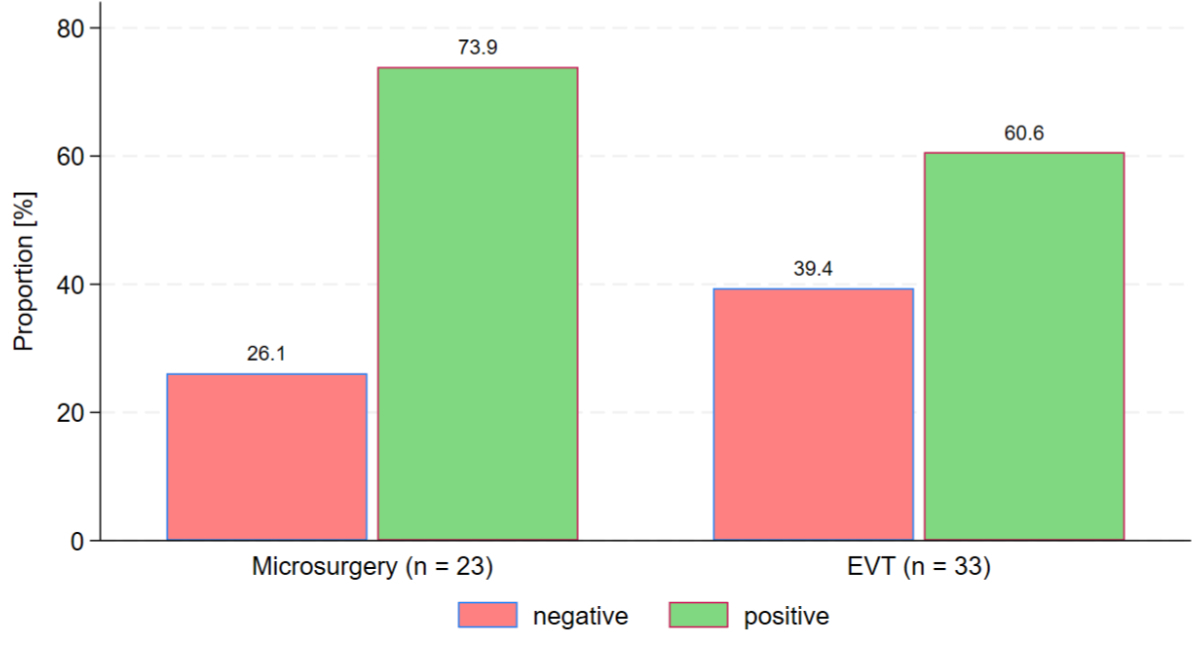
Nevertheless, far from all cases closed
with positive net earnings. In fact, 19 of the 56 cases (33.9%) closed with a
loss of money, due to higher costs than revenue; specifically, 13 of the 33
endovascular cases (39.4%) and 6 of the 23 microsurgery cases (26.1%) were not closed
with positive net earnings (p = 0.23) (figure 2).
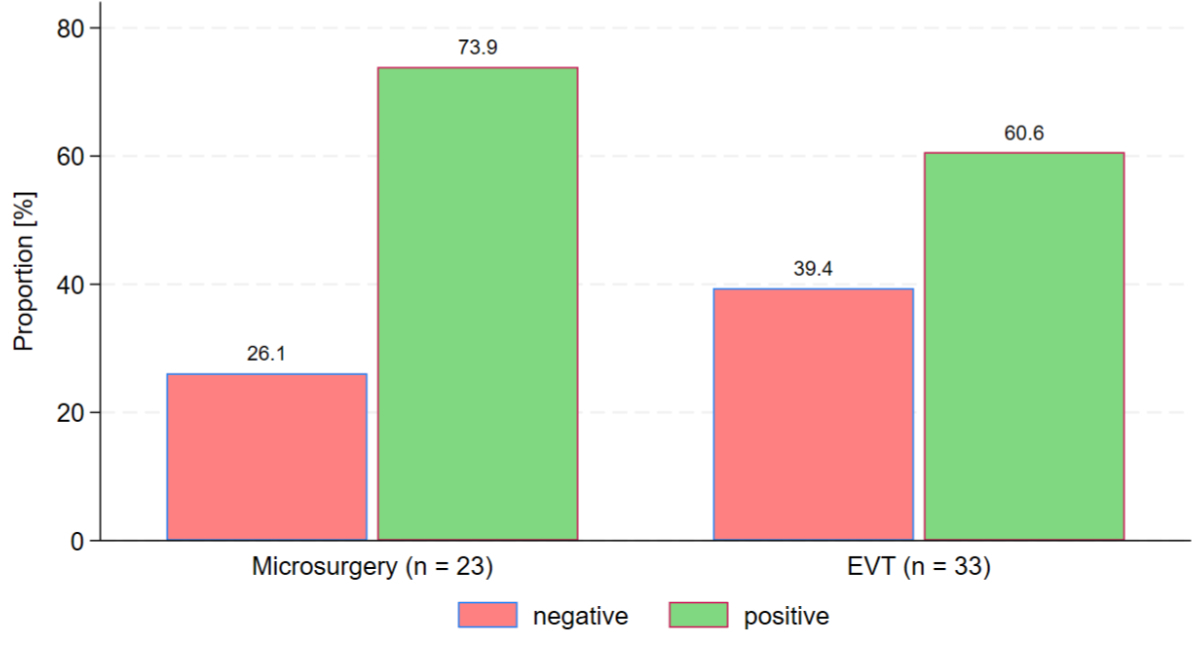
Figure 2Net earnings. A total of 34% of all cases led to a
net loss for the hospital. By group, 6 of 23 microsurgery cases (26%) but 13 of
34 endovascular cases (39%) did not close with positive net earnings (p = 0.23).
EVT: endovascular treatment.
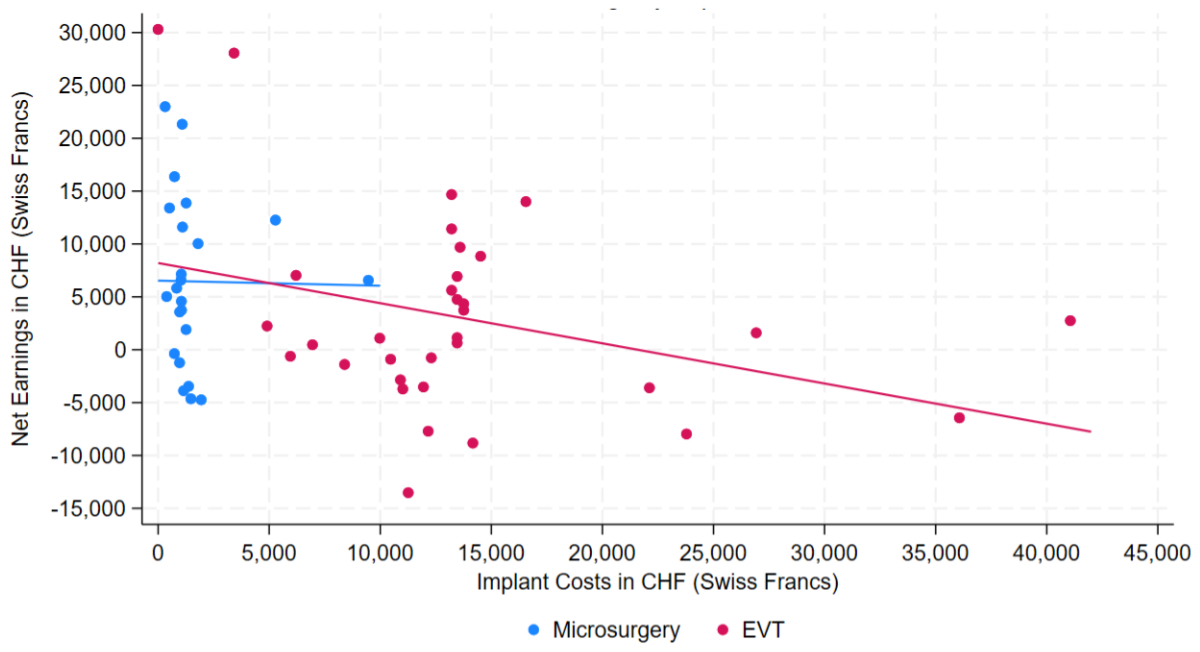
To determine which factors contributed to
lower net earnings or even losses in certain cases, we looked at the
relationship between net earnings and the variables total length of stay, hours
in the ICU and implant costs. Neither a longer duration of stay nor more time in
the ICU was correlated with negative net earnings (data not shown). The only
factor that tended to cause higher risks of net losses was higher implant costs,
which (as pointed out previously) were only of relevance in endovascular cases
(figure 3).
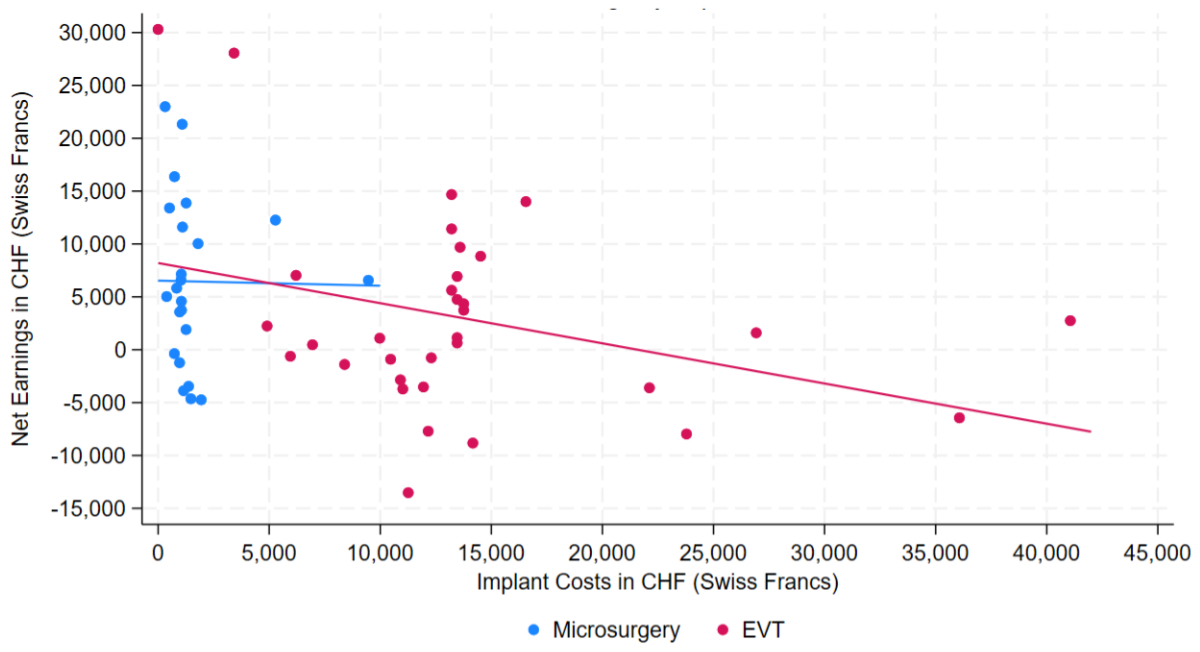
Figure 3Several factors were evaluated for their
correlation with net earnings per case. Single-case net earnings are displayed
as dots (blue for microsurgery and red for endovascular) on the Y-axis and
correlated with implant costs (on the X-axis). Implant costs in endovascular
cases were much more volatile than in microsurgery cases and led to a negative
correlation with net earnings (blue regression line). Monetary values are
displayed in CHF (Swiss Francs). EVT: endovascular treatment.
Discussion
The decision concerning the treatment
modality for unruptured intracranial aneurysm in the Swiss healthcare system should
obviously be made without bias related to monetary matters. Overall revenues,
net earnings, rates of non-profitable cases did not display marked differences
between the two treatment modalities (microsurgical clipping and endovascular
treatment). Nevertheless, we found distinct differences in cost distribution –
which were not unexpected. Direct case costs (everything that goes “into the
patient”, e.g. implants, medication, …) were higher in endovascular cases,
while general treatment costs (costs that are attributed to a certain case per
time interval or per area used, e.g. medical staff, operating theatre minutes,
ICU time, …) were higher in microsurgery cases. As total costs were comparable
between the treatment groups, we consider this difference in cost distribution to
be due to technical reasons and do not see any influence on the treatment
decision.
Microsurgically treated patients had longer
stays and thus higher facility usage costs. Yet, due to slightly higher
revenues, the latter were equalised. This points to fair and realistic revenue policies
as conducted by the Swiss
healthcare system, minimising the risk of financial bias in medical decision-making.
Treatment of unruptured intracranial
aneurysm seems to be a highly reimbursed procedure, independent of treatment
method. Approximately two thirds of our cases were closed with positive net earnings.
Yet, the risk of a case closing with a loss seemed to be higher in the
endovascular group (approx. 40% of endovascular cases closed with negative net
earnings vs approx. 26% of microsurgery cases). We saw a tendency for cases
with higher implant costs to lead to a decline in net earnings. Implant costs
were almost exclusively attributed to endovascular treatment. Depending on the
implants used, additional reimbursement for certain implants can be requested
in these cases. However, our findings suggest that these additional
reimbursements did not offset the higher implant costs and may have resulted in
a higher risk of negative net earnings. Therefore, based on these findings, further
negotiations with the authorities are warranted.
Beyond implant costs, we could not identify
factors contributing to net losses in certain cases.
Although almost two thirds of our cases
yielded positive net earnings at discharge, we remain with more than a third of
all unruptured intracranial aneurysm cases that did not yield a profit but led
to a loss of money for our neurocentre and the hospital.
One might assume that there should not be a
single case that leads to a loss of money for the hospital or the corresponding
treatment unit. This assumption is not necessarily correct. No data exist in
the scientific literature that support or contradict the assumption that each
case should leave a small profit for the hospital to cover developmental costs.
Common sense tells us that there will always be profitable cases and unprofitable
cases, and that the latter have to be balanced by the profitable ones. Ultimately,
there must be sufficient surplus for the healthcare institutions to cover infrastructure,
renovation, depreciation, interest and development.
Good care and close monitoring are required
for each individual treatment group. The reimbursement should be adequate to
prevent substantial loss for hospitals and caregivers. Otherwise there is a
risk that gaps in the healthcare will arise as hospitals might no longer be
able to provide highly specialised treatments.
On the other hand, close monitoring of highly
profitable treatments must be preserved. If certain treatments or diseases
regularly lead to high net revenues, individual institutions could “specialise”
in them in order to regularly generate high net earnings, which they – in the worst-case
scenario – pay out to their shareholders or investors to the detriment of the general
public, leaving the less lucrative treatments to public providers.
A theoretical discussion point remains: As
endovascularly treated patients had significantly shorter lengths of stay (3.8
vs 7.4 days, approx. 95% longer after microsurgery), one could argue that for
every microsurgically treated case, we could instead treat two cases
endovascularly to optimise total revenue volume, and thus total earnings. This
theory is based on one of the pillars of the DRG system, namely payment by case
rather than per time, which provides an incentive for a higher case load. However
unlikely this mathematical model seems, it would hold true on a computational
basis, given that all aforementioned factors would stay the same if free
treatment choice were abolished and all unruptured intracranial aneurysms
received endovascular treatment.
Revenue scenarios vary substantially
between different healthcare systems so our results do not necessarily reflect
a generalisable point of view and must be compared to systems in other
countries. In 2009, Hoh et al. evaluated treatment costs of unruptured
intracranial aneurysm at the University of Florida and concluded that
microsurgical treatment was associated with lower hospital costs and higher
surgeons’ revenues as compared to endovascular treatment [10]. A year later, Drazin
et al. came to the
same conclusion in their analysis of cases in New York [11]. This finding, from two
independent studies,
is especially noteworthy, given that in most places in the United States it is
the same person who provides microsurgical and endovascular treatment
(neurovascular hybrid). A higher personal revenue for a distinct treatment
modality might cause significant bias in medical decision-making.
The problem of cases that do not close with
positive net earnings has also been addressed before by Brinjikji et al. in the
United States. Hospital costs for both treatment methods for unruptured
intracranial aneurysm had not been covered by reimbursement from public
insurance in almost every single case [4]. Although these numbers might ameliorate
our 34% of cases that led to a net loss at discharge, the distinct differences
of the two healthcare systems must be addressed; especially the question of who
bears the loss of the underpayment
found in that study. A hint to that can be found in a study by Lan et al., who
concluded that net revenue by private insurance is significantly higher than by
public insurance for endovascular unruptured intracranial aneurysm treatment at
Vanderbilt University (Nashville, Tennessee, United States) [12].
While in microsurgical clipping, implant
costs are usually low (a typical clip in Switzerland costs around CHF 200–300) in
relation to the overall costs, implant costs in endovascular treatment vary
substantially, depending on the implants used. This is, on the one hand, the
type of material (coil, stent/flowdiverter woven endobridge device, etc…), and,
on the other hand, the amount used, which depends on the size and complexity of
the unruptured intracranial aneurysm. In our data, we saw a high volatility of
implant costs in endovascular cases and assume that both aforementioned factors
influence the costs. Several studies (one from Mexico, one from Thailand and
one from the United States) have addressed this question and found that depending
on the type and amount of material used for embolisation, larger or more
complex aneurysms had higher implant costs, as expected [1, 13, 14]. As we also saw
a tendency towards
higher rates of non-profitable cases with rising implant costs, close care must
be taken and discussions must follow the implementation of new (or more
expensive) devices, for dedicated reimbursement in selected cases, if justified.
Our study did not look at follow-up costs,
but at primary treatment costs. Primary treatment costs might have been a
decision criterion for the recommendation of a distinct treatment option.
Fortunately, within the Swiss healthcare system, this does not seem to be the
case. Yet, costs for revision interventions, follow-up images or complication
management must also be considered, especially in a population where cure rates
(and follow-up costs) might differ between the treatment modalities. Assuming
that re-intervention rates are higher in endovascular cases, the cost-balance
for a single lesion might additionally be affected in favour of microsurgical
treatment. Yet these distinct follow-up costs pose a different question and
might be addressed by a different dataset in the future.
From a critical point of view, the rates of
patients being discharged to rehabilitation or nursing homes might seem high
(17% after microsurgical treatment and 9% after endovascular treatment). However,
we routinely offer rehabilitation programmes (also including Kur-Klinik) to
patients who receive intracranial (mainly operative) procedures. Thus, a rate
of 17% of patients who are reluctant to take advantage of this kind of therapy
is well expected after microsurgery. Also, we had three patients in our dataset
who had been diagnosed with unruptured intracranial aneurysm during a hospital
stay due to other neurological diseases and had therefore been recommended
rehabilitation after treatment. The one patient who had died had a previously
coiled giant aneurysm of the basilar artery that had already elicited midbrain
compression. Re-treatment was associated with intraprocedural bleeding from the
aneurysm. Given the poor overall prognosis, therapy goals were changed to
comfort therapy after multiprofessional conversations and care for the patient
and relatives.
Of course, further treatment (like
rehabilitation, Kur-Klinik, etc) do also raise the total costs for the healthcare
or even the social system. Yet, they could not be assessed objectively in our
dataset.
Conclusion
Our data show that within the Swiss
healthcare system, patients do not have to worry about a financial bias in
medical decision-making concerning unruptured intracranial aneurysm treatment.
This is reassuring and stresses the well-balanced reimbursement features in
this country, whose healthcare system is considered excellent but expensive. Nevertheless,
there are threats even for well-balanced and well-financed healthcare systems. Rising
costs may lead to imbalanced net earnings or even losses and result in reduced supply
of the non-profitable treatments. Also, unequal reimbursements that promote
certain treatments or methods can facilitate “cherry picking” which in turn may
encourage individual institutions to only carry out well-paid treatments and
leave less lucrative treatments to others. We see initial signs of an imbalance
with a higher risk for negative net earnings in endovascular cases – probably
due to higher and volatile implant costs. This issue is of course highly
dependent on the local healthcare system and can even vary within a country (by
multiple healthcare options). In any event, two points seem valid across countries:
A significant number of
cases (even in the high-revenue segments) cannot be closed with positive net earnings.
The reasons seem variable, but high implant costs do surely contribute and
should therefore be closely monitored.
Data sharing statement
Open science code
CHEERS 2022 Checklist items 1–28 were met
where applicable.
Dedicated applicability per item can be received upon sound and adequate
request addressed to ulf.schneider[at]luks.ch and will be available for five years
from publication of the study.
Will the individual dataset be available? Yes
What data in particular will be shared: Individual
data that underlie the results reported in this article, after deidentification.
What other documents will be available: Not
applicable.
When will data be available: Immediately
following publication and ending five years following article publication.
With whom: Researchers who provide a
methodologically sound proposal.
For what types of analyses: To achieve the aim
in the approved proposal.
By what mechanism will data be available: Proposals
should be addressed to ulf.schneider[at]luks.ch. To gain data access, data requesters
will have to sign a data access agreement. Data are available for five years.
Prof. Dr. Ulf C. Schneider
Chairman
Department Neurosurgery
Neurocenter
Cantonal Hospital of Lucerne
Spitalstrasse
CH-6000 Lucerne 16
ulf.schneider[at]luks.ch
References
1. Figueroa-Sanchez JA, Ferrigno AS, Hinojosa-González DE, Salgado-Garza G, Martinez HR,
Caro-Osorio E, et al. Cost analysis of materials used in the endovascular treatment
of unruptured intracranial aneurysms in Mexico. Interv Neuroradiol. 2020 Aug;26(4):476–82.
doi: https://doi.org/10.1177/1591019920920954
2. Maud A, Lakshminarayan K, Suri MF, Vazquez G, Lanzino G, Qureshi AI. Cost-effectiveness
analysis of endovascular versus neurosurgical treatment for ruptured intracranial
aneurysms in the United States. J Neurosurg. 2009 May;110(5):880–6. doi: https://doi.org/10.3171/2008.8.JNS0858
3. Takao H, Nojo T, Ohtomo K. Cost-effectiveness of treatment of unruptured intracranial
aneurysms in patients with a history of subarachnoid hemorrhage. Acad Radiol. 2008 Sep;15(9):1126–32.
doi: https://doi.org/10.1016/j.acra.2008.02.017
4. Brinjikji W, Kallmes DF, Lanzino G, Cloft HJ. Hospitalization costs for endovascular
and surgical treatment of unruptured cerebral aneurysms in the United States are substantially
higher than medicare payments. AJNR Am J Neuroradiol. 2012 Jan;33(1):49–51. doi: https://doi.org/10.3174/ajnr.A2739
5. Ballas D, Dorling D, Hennig B. The Human Atlas of Europe. Bristol: Policy Press; 2017.
p. 79.
6. Stats OE. Health Care Resources: Physician Density 2013. OECD Stats; 2015.
7. Bjoernberg A, Phang AY. Euro Health Consumer Index 2018. 2019 Feb. Available from:
https://healthpowerhouse.com/media/EHCI-2018/EHCI-2018-report.pdf
8. Reis Miranda D, Moreno R, Iapichino G. Nine equivalents of nursing manpower use score
(NEMS). Intensive Care Med. 1997 Jul;23(7):760–5. doi: https://doi.org/10.1007/s001340050406
9. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS
II) based on a European/North American multicenter study. JAMA. 1993 Dec;270(24):2957–63.
doi: https://doi.org/10.1001/jama.1993.03510240069035
10. Hoh BL, Chi YY, Dermott MA, Lipori PJ, Lewis SB. The effect of coiling versus clipping
of ruptured and unruptured cerebral aneurysms on length of stay, hospital cost, hospital
reimbursement, and surgeon reimbursement at the university of Florida. Neurosurgery.
2009 Apr;64(4):614–9. doi: https://doi.org/10.1227/01.NEU.0000340784.75352.A4
11. Drazin D, Dalfino JC, Donovan M, Friedlich D, Feustel PJ, Popp AJ, et al. Surgonomics
of unruptured intracranial aneurysms. J Neurointerv Surg. 2010 Jun;2(2):168–70. doi: https://doi.org/10.1136/jnis.2009.001065
12. Lan M, Liles C, Patel PD, Gannon SR, Chitale RV. Impact of insurance type on national
variation in cost of endovascular treatment for unruptured cerebral aneurysms. J Neurointerv
Surg. 2021 Jul;13(7):661–8. doi: https://doi.org/10.1136/neurintsurg-2020-016676
13. Wang C, Hui FK, Spiotta AM, Rasmussen PA. The cost of coils implanted in aneurysms:
2 years of clinical data. J Neurointerv Surg. 2014 Jan;6(1):72–5. doi: https://doi.org/10.1136/neurintsurg-2012-010600
14. Duangthongphon P, Kitkhuandee A, Munkong W, Limwattananon P, Waleekhachonloet O, Rattanachotphanit T,
et al. Cost-effectiveness analysis of endovascular coiling and neurosurgical clipping
for aneurysmal subarachnoid hemorrhage in Thailand. J Neurointerv Surg. 2022 Sep;14(9):942–7.
doi: https://doi.org/10.1136/neurintsurg-2021-017970