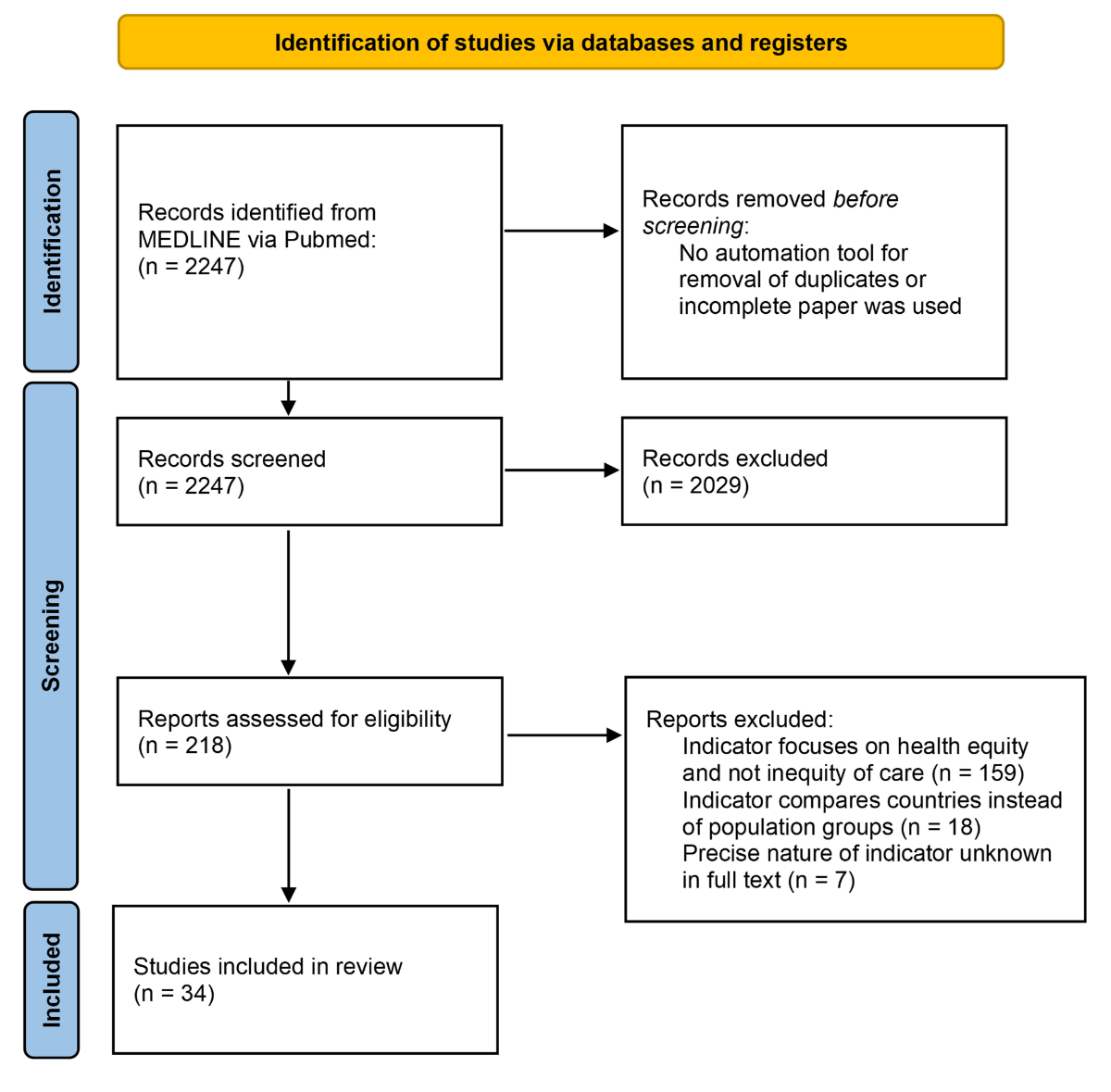
Figure 1Flowchart of the literature review.
DOI: https://doi.org/https://doi.org/10.57187/s.3714
Health equity has been receiving growing attention internationally as a key component of quality of care [1, 2]. In its 2001 report, the US Institute of Medicine (IoM) recommended that any healthcare system that aspires to quality should aim for six goals: safety, effectiveness, timeliness, efficiency, patient-centredness and equity [3]. Since the seminal report of IoM in 2001, the Organisation for Economic Co-operation and Development (OECD), the American College of Physicians, the UK’s National Health Service and the Canadian Institute for Health Information have all added equity to their definitions of quality of care [2, 4]. In Switzerland, quality of care is increasingly seen as an important objective, as demonstrated by the 2019 National Report on Health Quality, which led to the creation of the Swiss Commission for Quality [5].
Evidence has long shown that the ethnicity, sex, sexual orientation and socioeconomic status of patients affect their use of preventive care and access to care [6–9]. While striving for equity is a major deontological, ethical and moral imperative [10], it is also an economic imperative since inequities impose a high cost for the community. For example, between 2002 and 2006 in the US, ethnic inequities represented 230 billion USD in direct medical costs and productivity losses [11]. From a public health perspective, the COVID pandemic highlighted the consequences of having vulnerable groups acting as reservoirs for communicable diseases [12, 13].
A credible consideration of equity as a central objective of healthcare systems requires tools to measure and reveal inequities [14]. Specifically, healthcare systems need to monitor equity using a set of diverse indicators, at structure, process and outcome levels [15]. Structure indicators assess the availability of resources and are complementary to process indicators, which assess treatments and clinical pathways [15, 16]. These evaluate, in a relatively direct manner, the current state of equity in the delivery of healthcare services. Outcome indicators focus on patient-relevant outcomes and allow the evaluation of the effectiveness of equity improvement programmes. However, outcome indicators do not only reflect healthcare equity as they are also influenced by patient characteristics and health inequalities (e.g. low socioeconomic status patients have on average more comorbidities, and thereby a higher risk of hospital readmission) [17]. Equity of care improvement aims to reduce healthcare inequalities. Identifying those inequalities hence presupposes not only indicators but also stratifier variables that enable comparisons across vulnerability groups, such as migrants, elderly or foreign-language speakers.
In order to gain attractiveness, be routinely implemented and induce changes in practice, these equity indicators need to be precise, easy to implement and standardised, yet adapted to the local context [18, 19]. Indicators with high precision and accuracy would allow for reliable identification of inequities. For instance, geography-based indicators, like post codes or the Swiss Neighbourhood Index of socioeconomic position are available but lack precision because they group people with drastically different access to healthcare [20, 21]. Indicators should be easy to implement, limiting any burden on either patients or healthcare professionals. For example, self-reported indicators in questionnaires are known to have low completion rates when they are long and time-consuming [22]. Ease of implementation or, even better, automatic and generalised assessment of indicators also reduce the risk of measuring the indicators in potentially non-representative samples. Finally, standardisation of a set of indicators has two major advantages. First, it provides a more objective picture of the actual state of care equity, avoiding potential cherry-picking of an indicator by stakeholders that would overemphasise a specific local positive aspect. For example, cities hosting international institutions like Geneva and Zurich have an abundance of culturally competent interpreters in comparison with other Swiss cities [23]. Second, standardised indicators enable benchmarking and comparisons between hospitals, a driver for progress using the example of successful healthcare institutions [24].
Indicators also need to be adapted to the local context. In this study, we will focus on Switzerland, a country with a population of 9 million, a large proportion (39%) of non-Swiss citizens and 4 national languages [25]. Previous Swiss studies have proposed indicators of inequities in access and quality of care with, for example, indicators for hospital equity focused on potentially avoidable or potentially inappropriate hospitalisations [26]. Another study on outpatients, the Swiss Primary Care Active Monitoring initiative, developed 56 priority quality indicators, including 2 dedicated to equity in access to care [27]. Similarly, the Swiss Migrant Friendly Hospitals Project, an initiative led by the Swiss Federal Office of Public Health (FOPH), aimed to turn some hospitals into centres of excellence for the treatment of patients with a migratory background and relied on interpreter availability as an indicator of equity in healthcare [28]. However, none of the proposed indicators have been widely adopted by healthcare institutions in Switzerland, precluding comparison and benchmarking between different hospitals. Our aims were therefore to bring together existing initiatives and experts to reach consensus on a set of easily implementable healthcare equity indicators for populations at risk of inequities and to test their implementation potential and feasibility in three Swiss hospitals. In order to improve the internal validity of our indicators, we restricted our focus to the hospital setting, excluding private practices.
A set of equity indicators was selected in three phases: first, a large set of potential indicators in the context of the Swiss healthcare system was generated; then the most useful indicators were selected using a Delphi process; and finally the feasibility of implementing the chosen indicators was tested in three hospitals [29].
To recruit experts, a brochure presenting the project was distributed to various parties interested in equity, including national institutions, private and public healthcare stakeholders as well as patient associations. Our aim was to have experts from the three linguistic regions of Switzerland, from university and non-university settings, with several professions included, and with at least one patient partner. Eighteen experts were recruited (self-reported sex: 12 men, 6 women) from the three main linguistic regions of Switzerland and comprised 7 physicians (5 internists and 2 psychiatrists), 3 epidemiologists, 2 sociologists and 6 researchers and professionals working in the field of quality of care, including a patient representative. All experts had previous interests or had produced research in equity and worked in universities, university hospitals, either in outpatient or inpatient care, or had functions in healthcare institutions.
The initial set of indicators for the Delphi process came from two sources: a scoping review of the medical literature and a list of indicators proposed by the expert group. In addition to indicators, we also identified vulnerability stratifiers, which could lead to differences in quality of care. For instance, the indicator could be “waiting time in the emergency room” for patients presenting at the emergency department. The stratifier could be, for instance, sex, whereby women would have a longer “waiting time in the emergency room” on average than men. All experts’ input was collected using the REDCap electronic data capture tool hosted at University Hospitals of Geneva [30, 31].
The review included articles that described inequities in care or in access to care in Switzerland, or studies about programmes to improve healthcare equity in Switzerland. The literature search included publications from 1980 to 2021, concerning outpatient or inpatient care. We searched MEDLINE with the search terms “(Swiss OR Switzerland) and (Equity OR Inequity)” on 17 November 2021. This strategy yielded a total of 2247 citations. One author (CB) read each title and abstract to select articles using indicators and then extracted the definitions of the indicators and stratifiers from the full text of the articles.
The expert group met twice and went through four rounds of votes. During the first meeting, the experts agreed upon which criteria should be used to evaluate all proposed indicators. Validity, feasibility, patient coverage and actionability were retained. Validity is an estimation of whether an indicator measures what it purports to measure. Validity was the core criterion for selecting appropriate indicators and was the selection criterion for the first Delphi round. Feasibility describes the difficulty of obtaining the indicator, notably through data availability and extra work required to obtain it. Patient coverage describes the proportion of patients concerned by the indicator and actionability describes the capacity of the indicator to change after a quality improvement project [32].
For the first Delphi round, each indicator and stratifier were rated by the expert group on a scale from 0 to 10 for each criterion. After the first Delphi round, indicators with a mean validity rating >7 and for which ≥60% of the experts gave a validity score ≥7 were retained. During the votes, experts had the opportunity to suggest additional indicators or stratifiers.
Before the second round, indicators selected in the first round were organised in themes, reporting on a similar healthcare topic, from structural issues to process differences and unequal outcomes.
Each theme was assigned to either outpatient or inpatient care. Stratifiers were kept as a separate category. An example of a theme would be: “inpatient rehospitalisation” with the following theory: available social workers and information about treatment reduces delays in hospital care, which in turn leads to shorter length of stay as well as lower risk of transition of care issues without impacting early readmissions.
The experts were then asked to rank the themes and the stratifiers from best to worst, focusing on both feasibility and actionability.
Once the definitive set of indicators was selected, a feasibility study was conducted in three public hospitals: Hôpitaux Universitaire de Genève (HUG), Universitätsspital Zürich (USZ) and Ente Ospedaliero Cantonale in Mendrisio (EOC). These three hospitals are located in each of the three linguistic regions of Switzerland (French-, German- and Italian-speaking, respectively) and also represent university and non-academic settings. To operationalise the indicators and allow the hospital information system to extract them, we produced indicator sheets specifying in full detail how and with which variables each indicator should be calculated. Computation of the indicators was tested on all inpatient and outpatient consultations in 2021. Availability of structure indicators at the hospital level was assessed via a questionnaire sent to heads of quality of care in each hospital.
The funding source had no involvement in the study design; in the collection, analysis or interpretation of data; in the writing of the report; nor in the decision to submit the paper for publication.
According to the Swiss law (Federal Act on Research involving Human Beings), this study falls under the scope of quality improvement activities and hence is exempt from ethics review. Furthermore, data were provided by each hospital in aggregated form, i.e. anonymised, another reason for exemption from ethics review.
The initial literature review yielded 34 articles (see figure 1), with 32 individual indicators previously used in Switzerland. The full list of retained articles is available in supplementary file 1 available for download at https://doi.org/10.57187/s.3714.
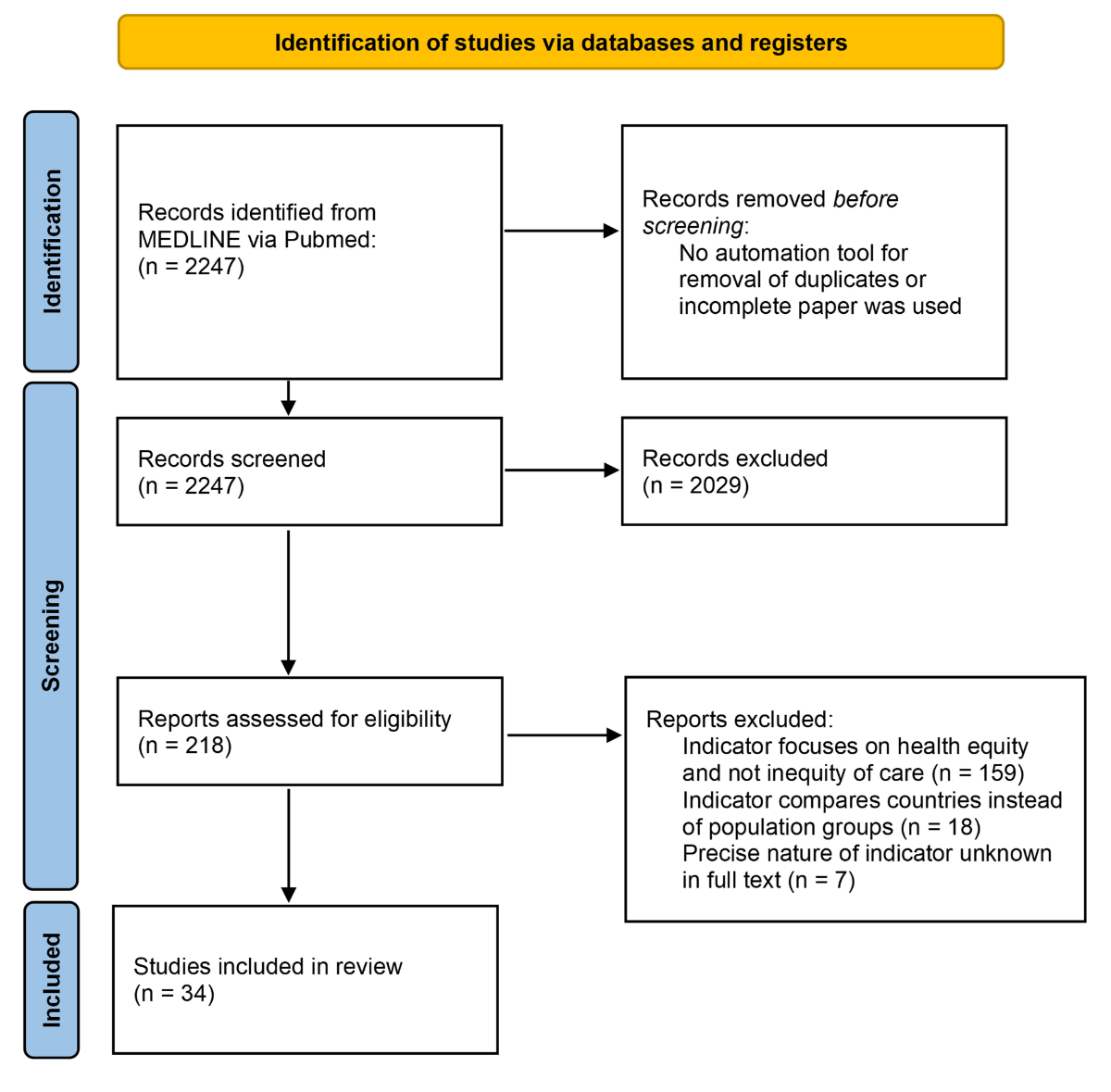
Figure 1Flowchart of the literature review.
Experts added 195 indicators to the 32 original ones. After removing duplicates, an initial set of 159 indicators was split into structure, process, outcome and inpatient/outpatient care, as well as 15 stratifiers (see supplementary file 2 for the full list and mean [standard deviation] ratings on all four criteria). Based on the validity criterion of the first Delphi round (mean rating >7 and ≥ 60% of scores >7), we retained 35 indicators and eight stratifiers grouped into three outpatient care themes and three inpatient care themes (table 1). One indicator did not fit into the themes (“Entrance of hospitals adapted for patients with a physical disability”).
Table 1Themes with indicators of outcome, process and structure. Bolded themes (3 and 5) denote the themes.
| Target | Theme | Outcome | Process | Structure |
| Inpatient themes | 1: Inpatient rehospitalisation | Early readmission rate | Length of stay | Availability of social workers |
| Availability of documents in simple and clear language | ||||
| 2: Inpatient admission | Emergency admission rate | Urgent care access time | Ongoing/continuous training offer for employees on cross-cultural skill | |
| Preventable hospital admissions rate | Healthcare renunciation for financial reasons rate | |||
| 3: Inpatient satisfaction | Patient satisfaction | Delay in care | Availability of social workers | |
| Proportion of foreign-language speaker patients receiving interpreting services | Availability of documents in simple and clear language | |||
| Availability of interpreters | ||||
| Existence/activity of an institutional referent for issues related to migration | ||||
| Outpatient themes | 4: Outpatient economic constraint | Proportion of people with self-declaring unmet needs for dental care services due to financial barrier | Healthcare renunciation for financial reasons rate | Existence of outpatient care structure for people without legal documents to live in the country |
| Availability of documents of information and consent in several languages | ||||
| 5: Outpatient language barriers | Patient satisfaction | Proportion of foreign-language speaker patients receiving interpreting services | Ongoing/continuous training offer for employees on cross-cultural skills | |
| Availability of interpreters | ||||
| Existence of outpatient care structure for people without legal documents to live in the country | ||||
| 6: Outpatient prevention care | Cervical cancer screening rate | Healthcare renunciation for financial reasons rate | ||
| Colorectal cancer testing for males >50 years old | Emergency room visit rate | |||
| Dental check-up rate | ||||
| Mammography screening |
“Economic constraint” is an example of an outpatient theme that follows the theory: the existence of an outpatient care structure for people without legal documents and health insurance helps to reduce healthcare renunciations for financial and administrative reasons, which in turn reduces the proportion of people having unmet healthcare needs (table 1).
In the second Delphi round, the experts ranked the themes in terms of feasibility and actionability, and only the best ranking themes in each of inpatient and outpatient care were retained: patient satisfaction for inpatients and language barriers for outpatients. The experts also voted to exclude the single indicator not included in the themes from the final set. This corresponded to a final set of 11 indicators presented in bold in table 1. The five stratifiers, retained on feasibility and actionability criteria, were: sex, foreign-language speaker, migration status, age category and homelessness.
The 11 indicators and 5 stratifiers were then operationalised with specific definitions to make them implementable in the pilot study. For example, the outpatient indicator “availability of interpreters” was defined as “the number of languages available in translation services in person or on the phone for outpatients divided by the total number of languages officially recorded as being spoken at home in Switzerland according to the 2019 “Language, religion and culture survey” (ELRC) of the Federal Statistical Office (FSO)”. These operationalisations are described for the 11 indicators and the 5 stratifiers in the indicators sheets available in supplementary file 3 (indicator sheets). The final operationalised indicators and stratifiers were approved by the expert group.
Patient-level data were extracted for the year 2021 in all three pilot hospitals. Availability was evaluated on two levels: whether the variables necessary to compute the indicator existed in the electronic patient records (“Available”: Yes/No) and the percentage of non-missing data for the actual set of patients’ records (figure 2).
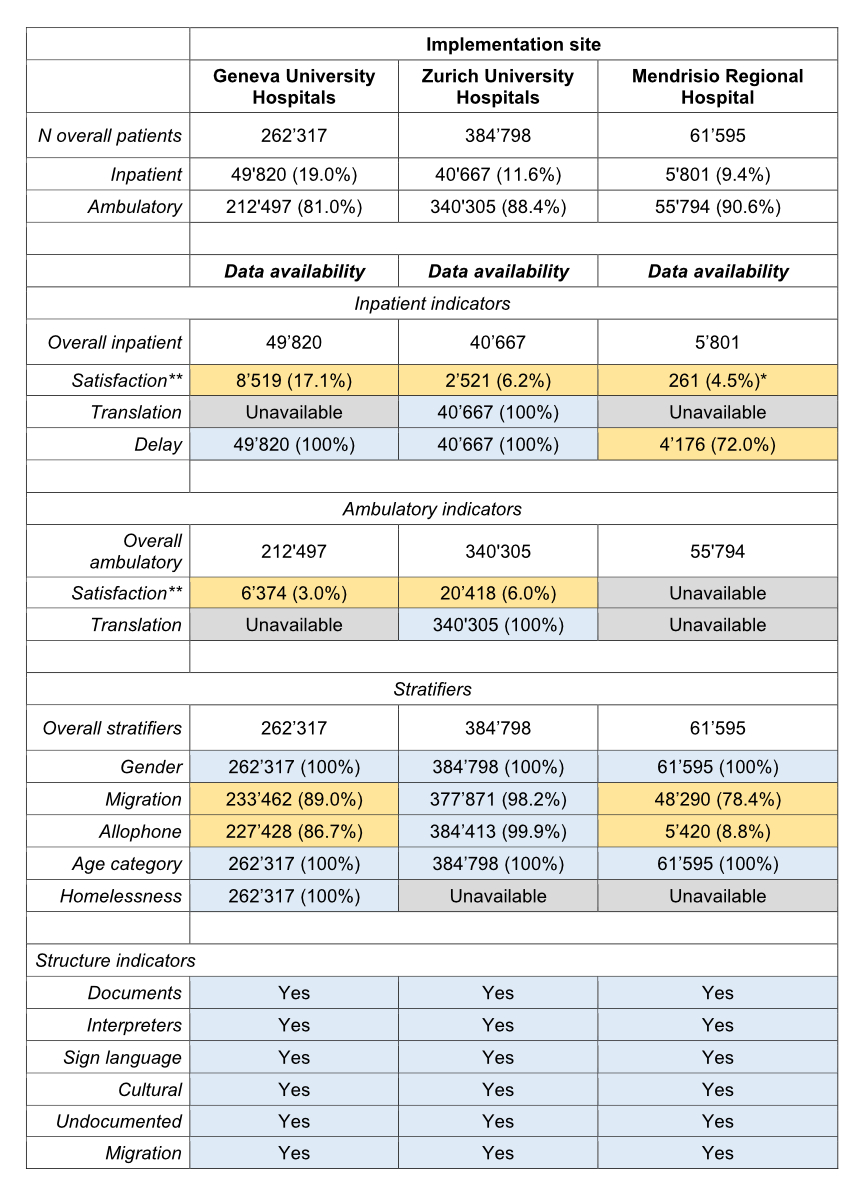
Figure 2Availability of indicators and stratifiers by implementation site. Data availability displays the percentage of non-missing data for the actual set of patients’ records. Level of availability is represented by colours: blue = largely available (>90%), yellow = partially available (>0–90%), grey = unavailable: Variable didn’t exist in the hospital’s Electronic Health Record (EHR). Indicators and stratifiers are presented in their shortened titles. Full titles and detailed definitions are available in supplementary file 2 (available for download as a separate file).
* Satisfaction data at Mendrisio is unavailable in the institution but collected by the Swiss National Association for Quality Development in Hospitals and Clinics (ANQ).
** Satisfaction questionnaire at Zurich University Hospitals was only available in German.
Overall, variables were more often available for inpatient than for outpatient indicators. University hospitals HUG and USZ had higher indicator availability overall than EOC. Interestingly, the availability of patient satisfaction differed between hospitals. Patient satisfaction was often collected at the hospital level at HUG and USZ. Another source of patient satisfaction data is the Swiss National Association for Quality Development in Hospitals and Clinics (ANQ), which collects patient satisfaction data at the national level. However, the patient satisfaction data collected by ANQ are only associated with minimal patient characteristics, and thus cannot be stratified.
To summarise, this feasibility study showed three levels of availability for the proposed indicators. First, indicators based on routine data such as “Delay in care”, or “Translation” at USZ were largely available (>90%, in green in table 1). Second, indicators requiring extra effort to be assessed were partially available (>0–90%, in yellow in figure 2). The availability of patient satisfaction data, for instance, depends in large part on the survey response rate. Lastly, some indicators were fully unavailable (in grey in figure 2), usually due to a lack of required variables in the information system, such as “receiving a translation” at HUG and EOC.
For stratifiers, age categories and sex were almost always available. Sex was stored in as a dichotomous variable at EOC but existed in three categories at USZ and HUG. However, at HUG, despite the availability of three options (male, female, undetermined), only the “male” and “female” options were used. Migration status was not directly available, but was operationalised based on nationality, country of residence, insurance type and residence permit (details in supplementary file 3). Finally, homelessness status, was only available at HUG, since homeless patients in HUG are assigned the address of the cantonal court. Other hospitals could not provide such approximation of homeless status.
A taskforce of Swiss experts produced 11 indicators of equity that would allow comparison and benchmarking at the national level and to shed light on inequities in healthcare. The taskforce concurrently selected five stratifiers assessing groups potentially vulnerable to inequity of care. The proposed indicators are valid, have high patient coverage and are focused on inequities in the healthcare system that are actionable through improvement projects. A feasibility study at three hospitals, representative of different linguistic regions and hospital types in Switzerland, showed three different levels of availability: available, partially available and unavailable.
Many of the selected indicators have already been used, which supports their face validity, since it will facilitate their acceptance by hospital administrators and policymakers. Taking the example of patient satisfaction, previous use has shown interesting results, such as a difference between sexes in terms of the importance of the dimensions of patient satisfaction. However, it has also highlighted potential limitations, such as a ceiling effect that limits its use for benchmarking already well-performing hospitals, and a positive correlation with age limiting its ability to reveal age-related inequities [33, 34]. Most patient satisfaction questionnaires divide satisfaction into dimensions such as patient information, wellbeing, respect of the patient or friends, and family involvement [35, 36]. Focusing on the specific aspects of satisfaction instead of global satisfaction is a potential solution to better evaluate contextual satisfaction. For instance, for outpatients, the dimension of patient information may have a stronger connection with the availability of interpreters. Taking the example of the availability of interpreters and sign language interpreters, their use as structure indicators has warned us that the availability of interpreters translates poorly into actual interpreting for patients [37]. This supports the division of indicators into structure, process and outcome themes, which should allow the whole process to be documented through the actual improvement in equity of care for patients. This study paves the way for future investigation of the proposed indicators’ criterion validity.
The indicators that are highly available could be implemented on a large scale immediately without substantial efforts from health institutions. The existence of these variables and their high availability are encouraging, and the indicators should be assessed across stratifiers to reveal existing inequities across Switzerland. The results would provide healthcare researchers studying inequities and public health practitioners with the tools to explore individual hospital policies. Large national infrastructures such as the Swiss Personalized Health Network (SPHN) could facilitate the assessment of these indicators using deidentified data, thus enabling quality improvement projects to address inequities in health [38].
Partial availability of some indicators or stratifiers emphasises the required effort for extensive documentation of processes and outcomes. A partial image of the situation may lead to a biased appreciation of the situation, for instance if only unsatisfied patients respond to a satisfaction survey [39, 40]. In Switzerland, satisfaction is measured by the National Association for Quality Development in Hospitals and Clinics (ANQ) over one month every two years. The survey is anonymous and collects some patient characteristics, such as sex (dichotomous), year of birth and insurance class, which can be used for stratification. It would be valuable to include more patient information in the ANQ survey. The best solution would entail combining already collected patient data with satisfaction surveys, without compromising the patient’s right to confidentiality of their satisfaction survey response.
Finally, completely unavailable stratifiers, such as homelessness status in the USZ and EOC, will require work to be implemented. Though more information on stratifiers could help to detect inequitable care, their implementation may also raise ethical questions. In the feasibility study, sex was mostly measured as a static binary, unchangeable and far from the gender spectrum with which patients from the LGBTQIA+ communities identify themselves. However, the collection of information not necessarily relevant for patients’ care, may actually lead to discrimination at a personal level. This risk should be weighed against the benefit of shedding light on inequities at a systemic level and discussed with members of the concerned communities. Numerous studies in the USA have shown that LGBTQIA+ patients overwhelmingly support the collection of gender-specific data in healthcare. A consultation with European patients may be necessary to rule out cultural differences in the approach to data safety [41–43].
One limitation of this study is its focus on feasibility. The aim was to produce an easily implementable set of indicators and stratifiers, sometimes to the detriment of potentially more valid indicators or stratifiers that would cover larger parts of the population. However, all the proposed indicators and all results of the Delphi votes are available in supplementary file 3. We hope that other researchers and institutions will use this full list of indicators to examine topics not included here, such as screening rates in preventive medicine or stratifiers by socioeconomic status.This focus on feasibility may explain the absence of ethnicity-based stratifiers. Data on racial or ethnic origin are considered sensitive in the Swiss Federal Act on Data Protection, which largely limits their collection. Since the proposed stratifiers aimed to be easy to implement, experts proposed using surrogate variables such as migration or foreign-language speaker status, which cover neighbouring vulnerable groups. Another limitation is that the test implementation only investigated data availability and not data quality. For example, some of the authors working in the field of quality of care have reported that the variable “foreign-language speaker” at USZ often correlates poorly with the actual patients’ spoken language. Further research into the quality of the selected variables would make it possible to quantify the potential gap between reality in the clinic and the reported variable in the electronic health record. Furthermore, the selected indicators were conceived as measurement tools at institutional level, which might not transfer well at patient level [44]. Finally, we were limited by the representativeness of the group of experts. Despite their large number, experts could not represent all important stakeholders. Specifically, there was only one patient representative, no representatives of private healthcare institutions or experts with a nursing care background. Nevertheless, before the publication of any report, a large panel of stakeholders were contacted to provide feedback on a preliminary report on the process and results, including private healthcare providers, patient organisations and associations representing the interests of specific communities such as migrant, disabled or LGBTQIA+ patients. Their feedback was encouraging, recognising the validity of the proposed set of indicators and vulnerability criteria, with good patient coverage and actionability, despite some expressed doubts about the ease of implementation due to technical and cost reasons.
With the growing recognition of the importance of quality of care, the implementation of equity indicators in as many institutions as possible will allow an estimation of the extent of inequity, highlight effective policies in specific institutions and support improvement projects. This is particularly crucial when considering that public health interventions using a population approach have been shown to be more effective in low-risk groups, which can inadvertently increase health inequalities. To enhance overall population health and reduce disparities between social groups, there is a need to integrate both population approaches and vulnerable population approaches, which necessitates the use of equity indicators [45]. The indicators provided in this study are a first step towards more equitable health care, and the indicator sheets should facilitate the rapid and standardised deployment of these indicators in Switzerland and international settings.
All the data relative to the selection process of the indicators are available as supplementary files (available for download at https://doi.org/10.57187/s.3714). For the test implementation of indicators, the hospital shared aggregated data as patient data are not available for confidentiality reasons.
The authors would like to thank their colleagues for making the collection, the analysis and the representation of the data possible: Dr Sébastien Courvoisier; Arnaud Iseli; Dr Denis Mongin; Liudmila Pagnamenta, MSc; Dr Anne-Marie Rassinoux, as well as the data and decision support IT team of HUG.
Authors contributions: DC, JM, PB, and YJ were responsible for the study design. DC, CB, AD, KO and FG managed data collection. DC an CB produced the data analysis. All co-authors equally contributed to data interpretation. DC and CB wrote the first draft and all co-authors reviewed and edited the final article.
The authors’ work was supported by a grant (reference: 142004508 / 224-78/49) from the Swiss Federal Office of Public Health (FOPH).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Doherty R, Cooney TG, Mire RD, Engel LS, Goldman JM; Health and Public Policy Committee and Medical Practice and Quality Committee of the American College of Physicians. Envisioning a Better U.S. Health Care System for All: A Call to Action by the American College of Physicians. Ann Intern Med. 2020 Jan;172(2 Suppl):S3–6. doi: https://doi.org/10.7326/M19-2411
2. Health D of. The NHS Plan: a plan for investment, a plan for reform. The Stationery Office Parliamentary Press, Mandela Way, London, SE1 5SS, customer.services@tso.co.uk; 2000. Available from: https://webarchive.nationalarchives.gov.uk/ukgwa/+mp_/http://www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_4002960
3. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC). US: National Academies Press; 2001.
4. Health Care Quality and Outcomes Indicators - OECD. Available from: https://www.oecd.org/health/health-care-quality-outcomes-indicators.htm
5. Vincent C, Staines A. Enhancing the quality and safety of swiss healthcare. Federal Office of Public Health on quality and safety of healthcare in Switzerland; 2019.
6. Achieving Health Equity. A Guide for Health Care Organizations | IHI - Institute for Healthcare Improvement. Available from: http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Health-Equity.aspx. https://www.ihi.org/resources/white-papers/achieving-health-equity-guide-health-care-organizations
7. Bosworth B. Increasing Disparities in Mortality by Socioeconomic Status. Annu Rev Public Health. 2018 Apr;39(1):237–51. doi: https://doi.org/10.1146/annurev-publhealth-040617-014615
8. Akinade T, Kheyfets A, Piverger N, Layne TM, Howell EA, Janevic T. The influence of racial-ethnic discrimination on women’s health care outcomes: A mixed methods systematic review. Soc Sci Med. 2023 Jan;316:114983. doi: https://doi.org/10.1016/j.socscimed.2022.114983
9. Burton-Jeangros C, Cullati S, Manor O, Courvoisier DS, Bouchardy C, Guessous I. Cervical cancer screening in Switzerland: cross-sectional trends (1992-2012) in social inequalities. Eur J Public Health. 2017 Feb;27(1):167–73.
10. Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–45. doi: https://doi.org/10.2190/986L-LHQ6-2VTE-YRRN
11. LaVeist TA, Gaskin D, Richard P. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv. 2011;41(2):231–8. doi: https://doi.org/10.2190/HS.41.2.c
12. Yi H, Ng ST, Farwin A, Pei Ting Low A, Chang CM, Lim J. Health equity considerations in COVID-19: geospatial network analysis of the COVID-19 outbreak in the migrant population in Singapore. J Travel Med. 2021 Feb;28(2):28. doi: https://doi.org/10.1093/jtm/taaa159
13. Riou J, Panczak R, Althaus CL, Junker C, Perisa D, Schneider K, et al. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: a population-based analysis. Lancet Public Health. 2021 Sep;6(9):e683–91. doi: https://doi.org/10.1016/S2468-2667(21)00160-2
14. World Health Organization website. Health topic: Equity. World Health Organization website. Available from: https://www.who.int/health-topics/health-equity
15. Donabedian A. The quality of care. How can it be assessed? JAMA. 1988 Sep;260(12):1743–8. doi: https://doi.org/10.1001/jama.1988.03410120089033
16. Lorini C, Porchia BR, Pieralli F, Bonaccorsi G. Process, structural, and outcome quality indicators of nutritional care in nursing homes: a systematic review. BMC Health Serv Res. 2018 Jan;18(1):43. doi: https://doi.org/10.1186/s12913-018-2828-0
17. Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyongying P, Stieglitz H, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013 Feb;28(2):269–82. doi: https://doi.org/10.1007/s11606-012-2235-x
18. Anderson AC, O’Rourke E, Chin MH, Ponce NA, Bernheim SM, Burstin H. Promoting Health Equity And Eliminating Disparities Through Performance Measurement And Payment. Health Aff (Millwood). 2018 Mar;37(3):371–7. doi: https://doi.org/10.1377/hlthaff.2017.1301
19. Dover DC, Belon AP. The health equity measurement framework: a comprehensive model to measure social inequities in health. Int J Equity Health. 2019 Feb;18(1):36. doi: https://doi.org/10.1186/s12939-019-0935-0
20. Wolkin A, Collier S, House JS, Reif D, Motsinger-Reif A, Duca L, et al. Comparison of National Vulnerability Indices Used by the Centers for Disease Control and Prevention for the COVID-19 Response. Public Health Rep. 2022;137(4):803–12. doi: https://doi.org/10.1177/00333549221090262
21. Panczak R, Galobardes B, Voorpostel M, Spoerri A, Zwahlen M, Egger M; Swiss National Cohort and Swiss Household Panel. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health. 2012 Dec;66(12):1129–36. doi: https://doi.org/10.1136/jech-2011-200699
22. Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002 May;324(7347):1183. doi: https://doi.org/10.1136/bmj.324.7347.1183
23. Bischoff A, Tonnerre C, Eytan A, Bernstein M, Loutan L. Addressing language barriers to health care, a survey of medical services in Switzerland. Soz Praventivmed. 1999;44(6):248–56. doi: https://doi.org/10.1007/BF01358973
24. Kounev S, Lange KD, von Kistowski J. Standardization. In: Kounev S, Lange KD, von Kistowski J, editors. Systems Benchmarking: For Scientists and Engineers. Cham: Springer International Publishing; 2020. pp. 203–27.
25. Oesch D. La structure économique et sociale de la Suisse. LIVES Working papers. 2022;94. Available from: http://dx.doi.org/
26. Spycher J, Morisod K, Eggli Y, et al. Indicators on Healthcare Equity in Switzerland. New Evidence and Challenges. Rapport sur mandat de l’Office fédéral de la santé publique OFSP. 2021.
27. Ebert ST, Pittet V, Cornuz J, Senn N. Development of a monitoring instrument to assess the performance of the Swiss primary care system. BMC Health Serv Res. 2017 Nov;17(1):789. doi: https://doi.org/10.1186/s12913-017-2696-z
28. Hudelson P, Dominice Dao M, Perneger T, Durieux-Paillard S. A “migrant friendly hospital” initiative in Geneva, Switzerland: evaluation of the effects on staff knowledge and practices. PLoS One. 2014 Sep;9(9):e106758. doi: https://doi.org/10.1371/journal.pone.0106758
29. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000 Oct;32(4):1008–15. doi: https://doi.org/10.1046/j.1365-2648.2000.t01-1-01567.x
30. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al.; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019 Jul;95:103208. doi: https://doi.org/10.1016/j.jbi.2019.103208
31. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–81. doi: https://doi.org/10.1016/j.jbi.2008.08.010
32. Kallen MC, Roos-Blom MJ, Dongelmans DA, Schouten JA, Gude WT, de Jonge E, et al. Development of actionable quality indicators and an action implementation toolbox for appropriate antibiotic use at intensive care units: A modified-RAND Delphi study. PLoS One. 2018 Nov;13(11):e0207991. doi: https://doi.org/10.1371/journal.pone.0207991
33. Hekkert KD, Cihangir S, Kleefstra SM, van den Berg B, Kool RB. Patient satisfaction revisited: a multilevel approach. Soc Sci Med. 2009 Jul;69(1):68–75. doi: https://doi.org/10.1016/j.socscimed.2009.04.016
34. Mpinga EK, Chastonay P. Satisfaction of patients: a right to health indicator? Health Policy. 2011 May;100(2-3):144–50. doi: https://doi.org/10.1016/j.healthpol.2010.11.001
35. Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002 Oct;14(5):353–8. doi: https://doi.org/10.1093/intqhc/14.5.353
36. Thayaparan AJ, Mahdi E. The Patient Satisfaction Questionnaire Short Form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Med Educ Online. 2013 Jul;18(1):21747. doi: https://doi.org/10.3402/meo.v18i0.21747
37. Bischoff A, Hudelson P. Access to healthcare interpreter services: where are we and where do we need to go? Int J Environ Res Public Health. 2010 Jul;7(7):2838–44. doi: https://doi.org/10.3390/ijerph7072838
38. Touré V, Krauss P, Gnodtke K, Buchhorn J, Unni D, Horki P, et al. FAIRification of health-related data using semantic web technologies in the Swiss Personalized Health Network. Sci Data. 2023 Mar;10(1):127. doi: https://doi.org/10.1038/s41597-023-02028-y
39. Tyser AR, Abtahi AM, McFadden M, Presson AP. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016 Aug;16(1 a):350. doi: https://doi.org/10.1186/s12913-016-1595-z
40. Perneger TV, Peytremann-Bridevaux I, Combescure C. Patient satisfaction and survey response in 717 hospital surveys in Switzerland: a cross-sectional study. BMC Health Serv Res. 2020 Mar;20(1):158. doi: https://doi.org/10.1186/s12913-020-5012-2
41. Deutsch MB, Plasencia N. Patient Attitudes on Collection of Sexual Orientation and Gender Identity Data in a Women’s Health Clinic with an Embedded Transgender Medicine Program. LGBT Health. 2023 Oct;10(7):552–9. doi: https://doi.org/10.1089/lgbt.2021.0381
42. Haider A, Adler RR, Schneider E, Uribe Leitz T, Ranjit A, Ta C, et al. Assessment of Patient-Centered Approaches to Collect Sexual Orientation and Gender Identity Information in the Emergency Department: the EQUALITY Study. JAMA Netw Open. 2018 Dec;1(8):e186506. doi: https://doi.org/10.1001/jamanetworkopen.2018.6506
43. Cahill S, Singal R, Grasso C, King D, Mayer K, Baker K, et al. Do ask, do tell: high levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS One. 2014 Sep;9(9):e107104. doi: https://doi.org/10.1371/journal.pone.0107104
44. Garg A, LeBlanc A, Raphael JL. Inadequacy of Current Screening Measures for Health-Related Social Needs. JAMA. 2023 Sep;330(10):915–6. doi: https://doi.org/10.1001/jama.2023.13948
45. Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008 Feb;98(2):216–21. doi: https://doi.org/10.2105/AJPH.2007.114777
The supplementary files are available for download as separate files at https://doi.org/10.57187/s.3714