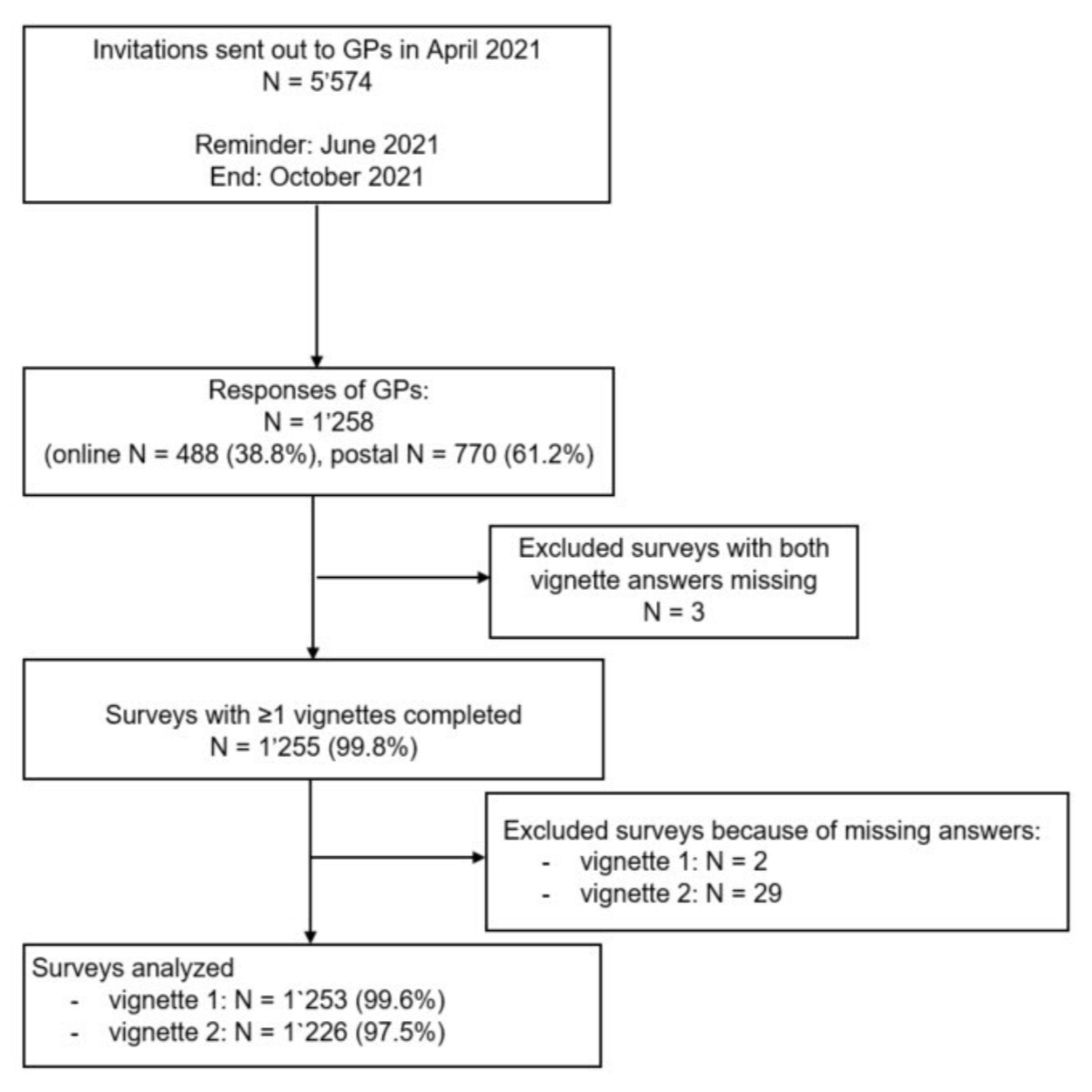
Figure 1Study flow. GPs: general practitioners.
DOI: https://doi.org/https://doi.org/10.57187/s.3697
Low back pain has been the leading reason for pain-related disability worldwide for many years [1–3]. The lifetime prevalence of low back pain in the global population is reported to be up to 80% [4]. Low back pain is one of the most frequent reasons for primary care visits. In the majority of cases presenting with acute low back pain, a specific underlying cause explaining the pain cannot be identified; thus it is non-specific [2, 5]. The prevalence of a serious spinal disease in patients presenting with acute low back pain to the general practitioners (GP) office is <1% [6]. Within six weeks, over 60% of patients with acute low back pain will have recovered without specific treatments [7]. However, in a low proportion of patients, chronic pain develops, resulting in individual pain and disability. Although low back pain is considered a benign condition, the impact in terms of direct medical costs and indirect costs worldwide is substantial [2]. The national annual costs range from $259 million in Sweden to nearly $150 billion in the USA [8].In Switzerland, the total economic burden of low back pain to Swiss society was estimated to be between 1.6% and 2.3% of the gross domestic product (GDP) in 2005 [9]. With an ageing population, the individual burden of low back pain and the associated costs are expected to further increase [10].
Due to a substantial spontaneous recovery during the acute low back pain phase, no further diagnostic work-up is recommended in acute low back pain without red flags [11, 12]. Current guidelines recommend to focus on pain control, reassurance and education on staying active and avoiding bed rest [5, 11–14]. The main reason against recommending early imaging is that studies showed no impact on low back pain management and outcome [15, 16] but potential unintended consequences such as overdiagnosis and overtreatment with higher healthcare utilisation, poor patient wellbeing and delayed return to work [17–20]. Further, inadequate and ineffective management may increase the risk for chronic low back pain [7, 21].
Healthcare professionals worldwide are asked to avoid ineffective or low-value care, and to improve the management of low back pain [1, 2]. The overuse of imaging and inadequate treatment suggests a gap between evidence and clinical practice [22, 23].
Therefore, the aim of this study was to assess whether current clinical practice of GPs across Switzerland is in line with practice guidelines for the management of patients with acute non-specific low back pain. The main outcomes of interest were the percentage of GPs prescribing imaging (magnetic resonance imaging [MRI] and/or X-ray), long-acting strong opioids and/or any activity restrictions. We further assessed whether management differed between female and male GPs and between French-/Italian-speaking and German-speaking regions of Switzerland.
We hypothesised that a substantial proportion of GPs do not follow the current guideline recommendations. We further hypothesised that there would be no or minimal differences between sexes and language regions, given that current guidelines like “Choosing Wisely Switzerland” are endorsed by the national medical association (FMH) and continuous education training for GPs in Switzerland does not differ between sexes.
In April 2021, we sent a letter to all physicians registered as GPs in the membership database of the Swiss Medical Association (FMH) inviting them to complete a survey of two clinical cases with acute low back pain. Reminders were sent in June 2021. The last surveys were returned in October 2021. Participation was voluntary, anonymous and confidential.
Switzerland has a compulsory universal health insurance coverage [24]. Although GPs are often the first contact for patients with acute low back pain [25], patients may also seek advice from specialists if permitted to do so by their health plan. Further, the organisation of local services varies due to the highly decentralised nature of the healthcare system with 26 administrative regions (cantons). Thus, a reliable figure for the number of physicians actively working as GPs is not available. We invited 5574 physicians (3993, 1397 and 184 from the German-, French- and Italian-speaking regions, respectively) registered in the membership database. According to a study in the canton of Bern, only 44% of physicians registered as GPs in this database were working as GPs [26]. The main reasons for physicians not working as GPs in the study were retirement / death (42%), working as a specialist (28%) and not having a licence to practice / changed profession (10%) [26]. Assuming that 50% of the contacted GPs were actively working, we expected potential responses from approximately 2800 GPs. In total, 1258 GPs (23% of those registered and 45% of our estimated number of active GPs) completed the survey (figure 1).
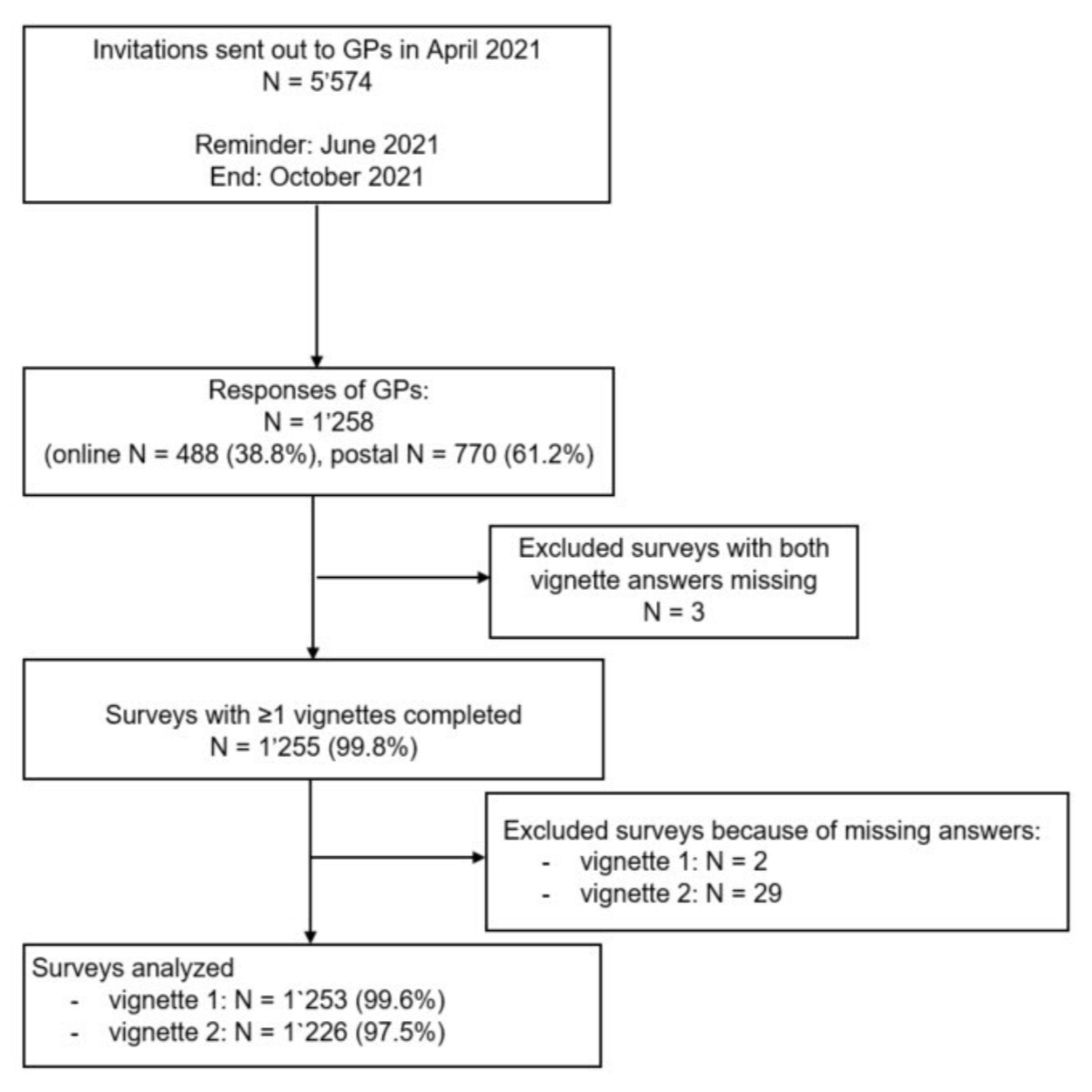
Figure 1Study flow. GPs: general practitioners.
We developed within a multidisciplinary research team (three physicians specialised in internal medicine, two physical therapists and one methodologist) two clinical vignettes of two patients with acute non-specific low back pain without red flags. The development of the vignettes was inspired by an earlier study exploring physicians’ recommendations in chronic low back pain using three vignettes [27]. We followed the current recommendations for the development and use of vignettes with clinical cases [28]. The vignettes were developed in German and translated into French and Italian by a physician (IJG) with proficiency in all three national languages. The vignettes were pilot-tested by five physicians not involved in the study. Based on their feedback, the vignettes were improved and retested for clinicians until all members of the research team agreed on the final version.
The main differences between the vignettes were sex (male vs female), age (35 vs 54 years), profession (warehouse operator vs IT specialist), pain duration (10 days vs 3–4 weeks) and medical history (none vs degenerative spine changes and disc protrusion in an MRI scan 8 years ago). Neither of the case vignettes included red flags or neurological deficits. According to current guideline recommendations, diagnostic tests are not required in either case, and the recommended treatments are pain control and advice to stay active.
Vignette 1: A 35-year-old male warehouse operator presented with acute severe low back pain that started 10 days after lifting heavy boxes in the store and increased steadily over time. There were no red flags in his personal history and clinical examination, with non-specific findings.
Vignette 2: A 54-year-old female IT specialist presented with a history of 3–4 weeks of low back pain with worsening of pain over the previous 2 days. The intermittent use of painkillers (non-steroidal anti-inflammatory drugs [NSAIDs] or paracetamol) improved her pain for short periods. The patient had a history of a previous low back pain episode 8 years ago with disc protrusion and degenerative changes on MRI. She was worried that the disc protrusion may have progressed and asked for a spinal injection. The clinical presentation suggested a non-specific low back pain in absence of red flags.
An English translation of the vignettes, with the complete questions and the corresponding response options is provided in appendix 1.
GPs received by post a paper version of the survey and a QR code to access the online version. They were thus able to either return the paper version of the survey or to complete the survey online. Of 1258 GPs who completed the survey, 770 (61.2%) returned the paper version by post and 488 (38.8%) completed the survey online (figure 1).
GPs were asked to rate for each vignette how they would proceed in the clinical situation with diagnostic options (none, imaging, laboratory tests, referral to a specialist), pharmacological options (none, non-opioids, weak opioids, short-acting strong opioids, long-acting strong opioids, muscle relaxants, oral steroids, homeopathy, spinal injection) and non-pharmacological options (none, massage, active physical therapy, manual therapy, acupuncture). We further assessed recommendations about activity (stay in bed/avoid any activity; avoid painful and stressful activities; stay active as usual) and work (issue sickness certificate due to pain; continue working with limitations; continue as usual). We asked GPs whether they believed that a disc herniation was the cause of the current pain.
GPs were not aware of the research question. After completing the two vignettes, we asked GPs general information about their age, sex, years in clinical practice, type of employment (employed or own practice, full-time or part-time), and knowledge about current guideline recommendations and “Smarter Medicine – Choosing Wisely” recommendations [29]. GPs characteristics and questions about whether they knew the guidelines for low back pain were asked at the end of the survey to avoid bias in the responses.
We defined low-value care as diagnostic tests and management not in agreement with current guidelines. We used guidelines from the National Institute for Health and Care Excellence (NICE) in England [14], the American College of Physicians (ACP) [30] and Choosing Wisely recommendations [29]. We also consulted systematic reviews of clinical guidelines on management of low back pain published in The Lancet [11, 13], European Spine Journal [12] and European Journal of Pain [31, 32]. Appendix 1 summarises the detailed definitions and cut-offs of guideline adherence and low-value care for diagnostic approaches, pharmacological and non-pharmacological treatments, referral to specialist and recommendations for activity and work. Since there were no red flags and no neurological deficits in both vignettes and both patients had no previous treatment, we considered responses as guideline-adherent if GPs “never or rarely” performed imaging studies, laboratory tests, referred the patient to a specialist, prescribed muscle relaxants, steroids, long-acting opioids, spinal injection, homeopathy, massage and acupuncture. We considered the use of NSAIDs and metamizole as guideline-adherent for pain control. Guideline recommendations for paracetamol changed over time and paracetamol was no longer recommended as a first-line therapy or monotherapy for pain [33]. Thus, we defined as guideline-adherent if it was never, rarely or occasionally considered. Because our response options did not allow to assess whether a pain medication was prescribed in combinations or as-needed, we assessed co-prescription of paracetamol with NSAIDs that had been shown to be potentially beneficial [34]. The guidelines recommend active physical and manual therapy in selected patients [13]. We defined as guideline-adherent if active physical and manual therapy were considered occasionally or more in both vignettes because some evidence indicates that manual and active physical therapy may help to rapidly decrease pain and educate the patients [35]. In both vignettes, risk factors for chronification (lifting heavy weights, previous episode of low back pain) [36, 37] were present and therefore active physical and manual therapy were considered appropriate. We considered advice to stay active without any restrictions and to continue to work as guideline-adherent.
The online survey was set up using a web-based survey tool. All questionnaires returned by post were entered into the web-based survey tool by two researchers (MT and VH). A third researcher (NT), otherwise not involved in the study, checked the data quality in a random sample of 45 respondents (with 1080 responses in total) and found a very low error rate (2 errors or 0.2%). Missing responses were rare (2% of the returned questionnaires: 2 missing responses to vignette 1, 29 missing responses to vignette 2). Missing data is reported for each variable in the corresponding tables. 45 respondents (with 1080 responses in total) and found a very low error rate (2 errors or 0.2%). Missing responses were rare (2% of the returned questionnaires: 2 missing responses to vignette 1, 29 missing responses to vignette 2). Missing data is reported for each variable in the corresponding tables.
We calculated descriptive statistics, medians and interquartile ranges for continuous variables, absolute numbers and percentages the number for categorical variables. We assessed guideline adherence by calculating the proportion of responses in agreement with current guideline recommendations. We compared differences in responses for subgroups (female vs male GPs; GPs working in French- and Italian-speaking regions vs German-speaking region) by using the chi-square test for categorical data. The level of significance was set at p <0.05. Statistical analyses were performed using R version 4.0.3 [38].
The study and all methods were carried out in accordance with relevant guidelines and regulations. According to the Swiss Human Research Act, article 2.2c [39], Institutional Review Board (IRB) approval is not required for research that uses anonymously collected data. In this study, data collection was fully anonymised. Furthermore, physicians were informed about the content of the survey and the study goals, study participation was voluntary and GPs were able to withdraw from the survey at any time. All physicians who returned the questionnaire by post or completed the survey online confirmed their informed consent by completing the survey.
Of the 1258 surveys received, 934, 278 and 46 were from GPs working in German-, French- and Italian-speaking regions, respectively. Figure 2 depicts the GP distribution across Swiss cantons. After the exclusion of three surveys with no answers to any of the vignettes, we analysed 1253 surveys for vignette 1 and 1226 for vignette 2 (29 surveys had no answers to vignette 2; see also study flow in figure 1).
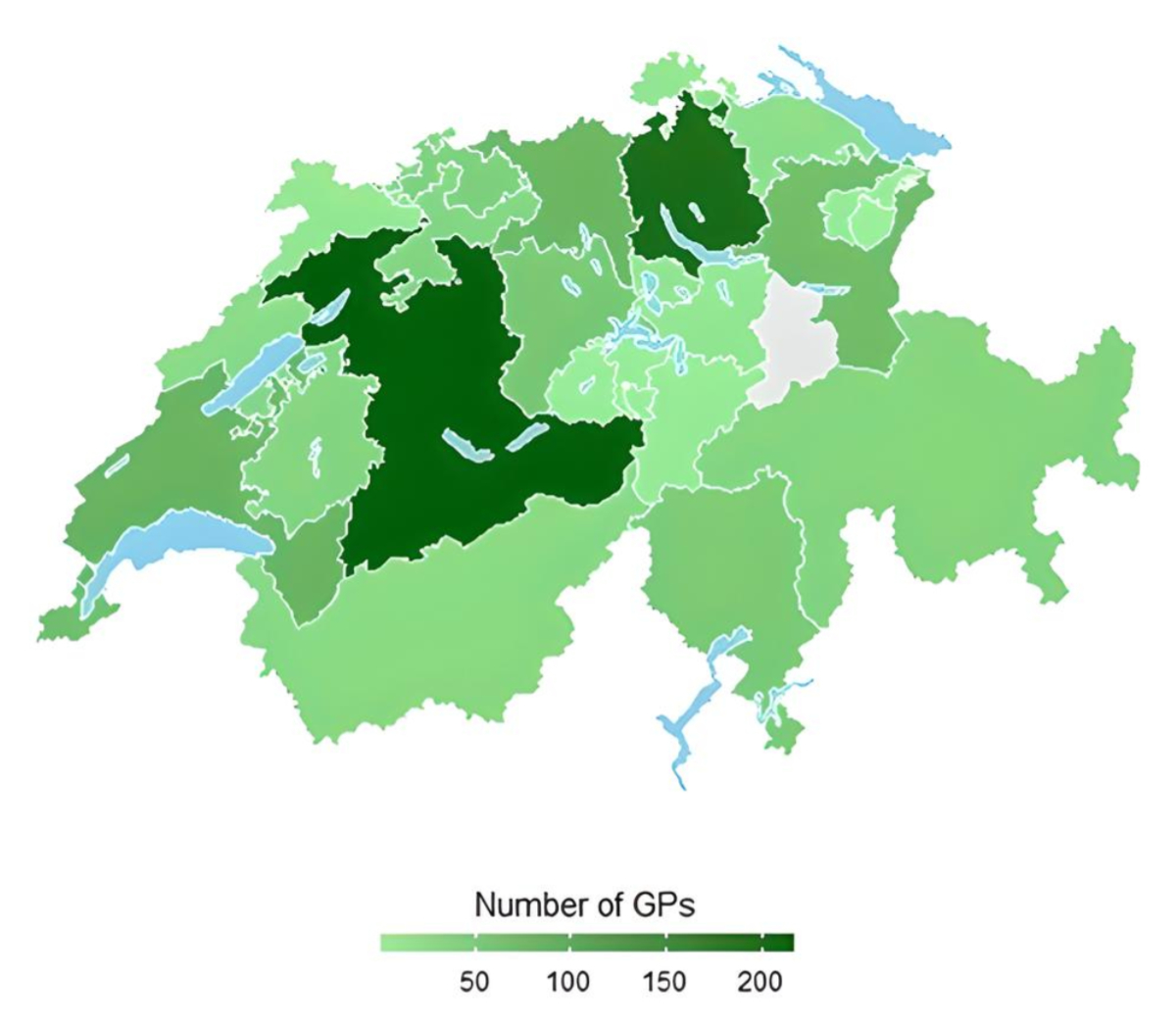
Figure 2Distribution of participating general practitioners (GPs) across Swiss cantons.
GPs were mainly male (53%), aged over 50 years (50%), worked part-time (60%) and in their own office (66%), and had >8 years of experience (60%) (table 1). Female GPs were younger than their male colleagues (50% vs 65% aged over 50 years) and were more likely to work part-time (84% vs 42%). Most GPs scheduled between 15 and 30 minutes per patient (69%), and only 5% scheduled fewer than 15 minutes to see a patient. GPs working in the French-/Italian-speaking regions more often had their own office compared to GPs working in the German-speaking regions (84 vs 63%).
Table 1Baseline characteristics of the general practitioners (GPs) in the study.
| All (n = 1255) | Female (n = 567)* | Male (n = 645)* | p-value | ||
| Age (years) | <0.001 | ||||
| <40 | 231 (18%) | 145 (26%) | 85 (13%) | ||
| 41–50 | 357 (29%) | 213 (38%) | 142 (22%) | ||
| >50 | 632 (50%) | 209 (37%) | 418 (65%) | ||
| Missing | 35 (3%) | 0 (0%) | 0 (0%) | ||
| Language | <0.001 | ||||
| German | 932 (74%) | 432 (76%) | 475 (74%) | ||
| French | 277 (22%) | 127 (22%) | 135 (21%) | ||
| Italian | 46 (4%) | 8 (1%) | 35 (5%) | ||
| Missing | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Work schedule | <0.001 | ||||
| Full-time | 463 (37%) | 90 (16%) | 370 (58%) | ||
| Part-time | 752 (60%) | 475 (84%) | 273 (42%) | ||
| Missing | 40 (3.2%) | 2 (0%) | 2 (0%) | ||
| Practice type | <0.001 | ||||
| Employed in GP office | 325 (26%) | 207 (37%) | 118 (18%) | ||
| Own GP office | 830 (66%) | 331 (59%) | 491 (77%) | ||
| Hospital – outpatients | 21 (2%) | 6 (1%) | 15 (2%) | ||
| Other | 36 (3%) | 19 (3%) | 17 (3%) | ||
| Missing | 43 (3.4%) | 4 (0.7%) | 4 (0.6%) | ||
| Graduation year | <0.001 | ||||
| 1–7 years ago | 18 (1%) | 9 (2%) | 9 (1%) | ||
| 8–20 years ago | 453 (36%) | 273 (49%) | 179 (28%) | ||
| >20 years ago | 735 (59%) | 277 (50%) | 452 (71%) | ||
| Missing | 49 (3.9%) | 8 (1.4%) | 5 (0.8%) | ||
| Work experience (years) | <0.001 | ||||
| ≤1 | 13 (1%) | 8 (1%) | 5 (1%) | ||
| >1 to 7 | 183 (15%) | 114 (20%) | 68 (11%) | ||
| ≥8 | 1009 (84%) | 436 (78%) | 567 (89%) | ||
| Missing | 50 (4.0%) | 9 (1.6%) | 5 (0.8%) | ||
| Length of visit (minutes) | <0.001 | ||||
| 10–15 | 63 (5%) | 19 (3%) | 43 (7%) | ||
| 15–20 | 441 (35%) | 167 (30%) | 273 (43%) | ||
| 20–30 | 555 (44%) | 287 (52%) | 264 (42%) | ||
| >30 | 140 (11%) | 84 (15%) | 54 (9%) | ||
| Missing | 56 (4.5%) | 10 (1.8%) | 11 (1.7%) | ||
| In-house X-ray | <0.001 | ||||
| No | 352 (28%) | 194 (34%) | 155 (24%) | ||
| Yes | 863 (69%) | 370 (66%) | 489 (76 %) | ||
| Missing | 40 (3.2%) | 3 (0.5%) | (0%) | ||
* Number of surveys with answer to sex question (missing 3.4%, n = 43).
Most GPs considered the two case vignettes to be representative of the cases they see in their clinical practice (93%). A majority reported that they knew the current clinical guidelines (61%), considered them reasonable (81%) and were aware of the “Smarter Medicine – Choosing Wisely Switzerland” recommendations (76%).
Although both cases presented without red flags or neurological deficits, uncertainty about the likelihood of an underlying disc herniation was high: 40% of GPs rated a disc herniation as possible or likely for vignette 1, and 55% for vignette 2. There were no differences in the likelihood of an underlying disc herniation between female and male GPs (table S1 in the appendix). GPs working in the French-/Italian-speaking parts of Switzerland were more likely to assume an underlying disc herniation than GPs working in the German-speaking regions (60% vs 34% for vignette 1, 77 vs 54% for vignette 2, p <0.001; table S2 in the appendix).
X-rays were recommended in vignette 1 by 18% of respondents and in vignette 2 by 32%; MRI imaging by 31% in vignette 1 and by 62% in vignette 2 (table 2). Figure 3 depicts the proportion of GPs in agreement with the guideline’s recommendations and the proportion using low-value diagnostic tests.
Table 2Proportion of general practitioners (GPs) managing patients with non-specific low back pain in agreement with clinical guidelines (vignette 1, n = 1253; vignette 2, n = 1226).
| Guideline recommendation (response categories)* | Vignette 1 | Vignette 2 | ||||
| All, n = 1253 (100%) | Missing (%) | All, n = 1226** (100%) | Missing (%) | |||
| Diagnostic measure | No further diagnostic measures recommended | 786 (63%) | 113 (9%) | 474 (39%) | 113 (9%) | |
| Avoid laboratory tests | 987 (79%) | 141 (11%) | 836 (68%) | 93 (8%) | ||
| Avoid X-ray | 896 (72%) | 129 (10%) | 743 (61%) | 90 (7%) | ||
| Avoid MRI | 750 (60%) | 116 (9%) | 414 (34%) | 48 (4%) | ||
| Pharmacological treatment | No medication | 185 (15%) | 342 (27%) | 160 (13%) | 323 (26%) | |
| No use of paracetamol | 405 (32%) | 144 (12%) | 422 (34%) | 100 (8%) | ||
| Use of NSAIDs | 1208 (96%) | 34 (3%) | 1184 (97%) | 31 (2%) | ||
| Co-prescription of paracetamol and NSAID*** | 670 (95%) | 652 (93%) | ||||
| Use of metamizole | 1078 (86%) | 102 (8%) | 1075 (88%) | 70 (6%) | ||
| No use of muscle relaxants | 228 (18%) | 51 (4%) | 245 (20%) | 40 (3%) | ||
| No use of weak opioids | 1021 (82%) | 96 (8%) | 952 (78%) | 79 (6%) | ||
| No use of short-acting strong opioids | 1127 (90%) | 116 (9%) | 1105 (90%) | 100 (8%) | ||
| No use of long-acting strong opioids | 1040 (83%) | 114 (9%) | 996 (81%) | 101 (8%) | ||
| No use of steroids | 836 (67%) | 91 (7%) | 749 (61%) | 75 (6%) | ||
| No homeopathy | 1038 (83%) | 149 (12%) | 1013 (83%) | 149 (12%) | ||
| No spinal injections | 813 (65%) | 91 (7%) | 638 (52%) | 78 (6%) | ||
| Non-pharmacological treatment | Start active physical therapy | 1182 (94%) | 21 (2%) | 1171 (96%) | 25 (2%) | |
| Consider manual therapy | 826 (66%) | 67 (5%) | 758 (62%) | 66 (5%) | ||
| No massage recommended as first-line therapy | 652 (52%) | 110 (9%) | 644 (53%) | 117 (10%) | ||
| No acupuncture recommended as first-line therapy | 895 (71%) | 111 (9%) | 842 (69%) | 123 (10%) | ||
| Referral | No referral to a rheumatologist | 996 (80%) | 159 (13%) | 857 (70%) | 85 (7%) | |
| No referral to a spine surgeon | 957 (76%) | 157 (13%) | 830 (68%) | 90 (7%) | ||
| Recommendations | Allow all activities/recommend to remain active | 215 (17%) | 7 (1%) | 342 (28%) | 7 (0.6%) | |
| Stay at work/no sickness certificate due to pain | 67 (5%) | 4 (0.3%) | 554 (45%) | 12 (1%) | ||
* Definition of guideline adherence and low-value care is provided in appendix 1.
** Number of surveys with at least one question answered.
*** Co-prescription of paracetamol and NSAID in GPs who often or always prescribed paracetamol.
Figure 3Agreement with guideline recommendations and the proportion of low-value care in the diagnostic management of two acute non-specific low back pain vignettes (vignette 1, n = 1253; vignette 2, n = 1226). Low-value care: any additional diagnostic test often or always performed; laboratory tests, X-rays or MRI occasionally, often or always performed. Questions, response options and the definitions of low-value care / disagreement with guidelines are provided in appendix 1.
Most GPs prescribed NSAIDs, paracetamol and/or metamizole for pain management (table 2; figure 4). GPs who considered paracetamol did so in 95% by co-prescribing with NSAIDs in vignette 1 and in 93% in vignette 2. Low-value pharmacological treatments included muscle relaxants (78% in vignette 1 and 77% in vignette 2), a short course of oral steroids (26% and 33%), spinal injections (28% and 42%) and long-acting strong opioids (8% and 11%).
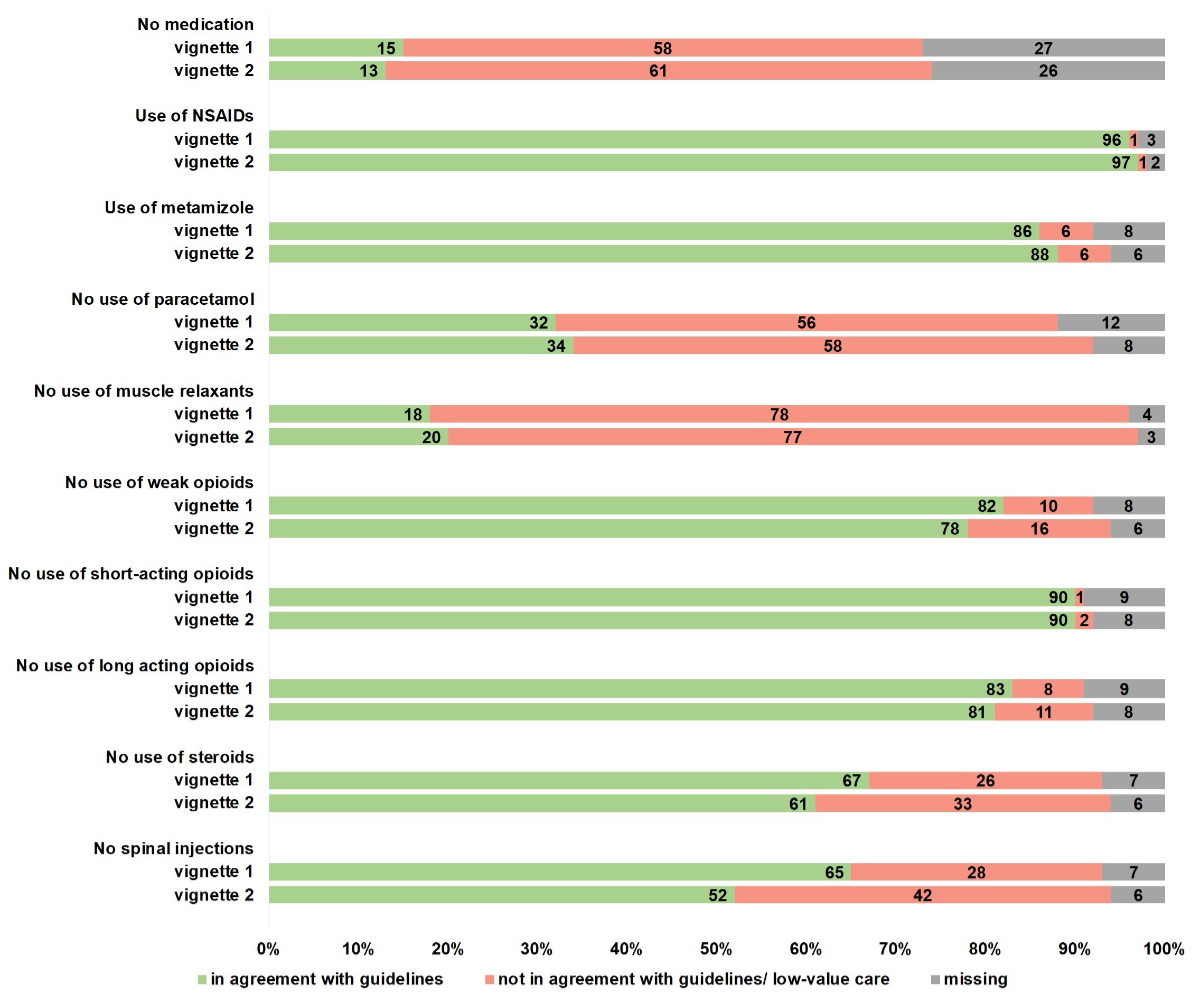
Figure 4Agreement with guideline recommendations and the proportion of low-value pharmacological therapy in two acute non-specific low back pain vignettes (vignette 1, n = 1253; vignette 2, n = 1226). Low-value care for NSAID: never, rarely used. Low-value care for muscle relaxants, steroids, long-acting strong opioids, homeopathy, spinal injection: occasionally, often or always used. Low-value care for paracetamol, weak and short-acting strong opioids: often or always used. Questions, response options and the definitions of low-value care / disagreement with guidelines are provided in appendix 1.
The majority of GPs advised active physical therapy (over 90%, table 2; figure 5) and manual therapy (over 60%). Low-value non-pharmacological treatments were recommended by a relevant proportion of GPs: massage by nearly 40%, acupuncture by 20% and 25% considered referral to a specialist (spine surgeon or rheumatologist) in both vignettes.
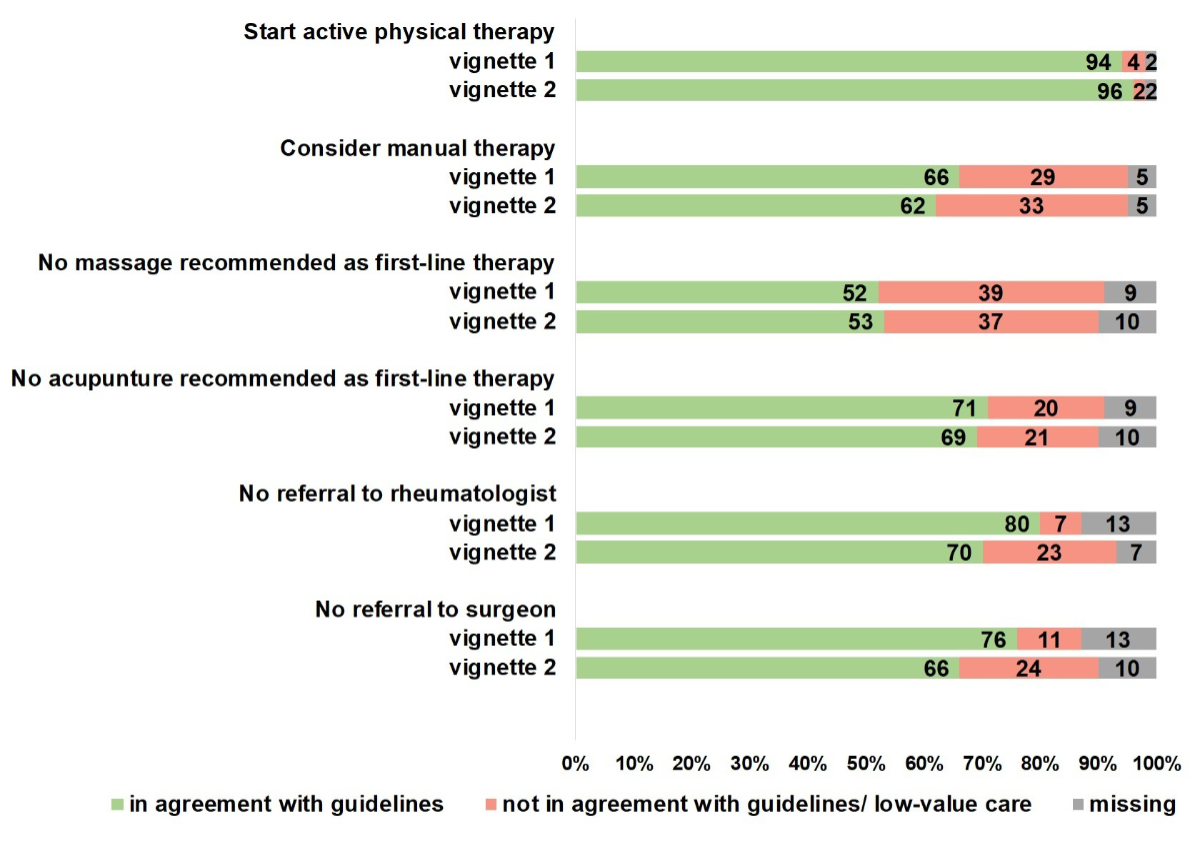
Figure 5Agreement with guideline recommendations and the proportion of low-value non-pharmacological care in two acute non-specific low back pain vignettes (vignette 1, n = 1253; vignette 2, n = 1226). Low-value care for active physical therapy and manual therapy: never or rarely used. Low-value care for massage and acupuncture: occasionally, often or always used. Low-value care for referral to a rheumatologist or spinal surgeon: occasionally, often or always. Questions, response options and the definitions of low-value care / disagreement with guidelines are provided in appendix 1.
Low-value care included activity restrictions, which were recommended by 82% in vignette 1 and 71% in vignette 2 (table 2; figure 6). Most GPs recommended avoiding painful activities (68% in vignette 1 and 57% in vignette 2). Bed rest/avoidance of any activity was recommended by 3% in vignette 1 and 2% in vignette 2. A work-sickness certificate was issued by 95% of the GPs in vignette 1 and by 54% in vignette 2.
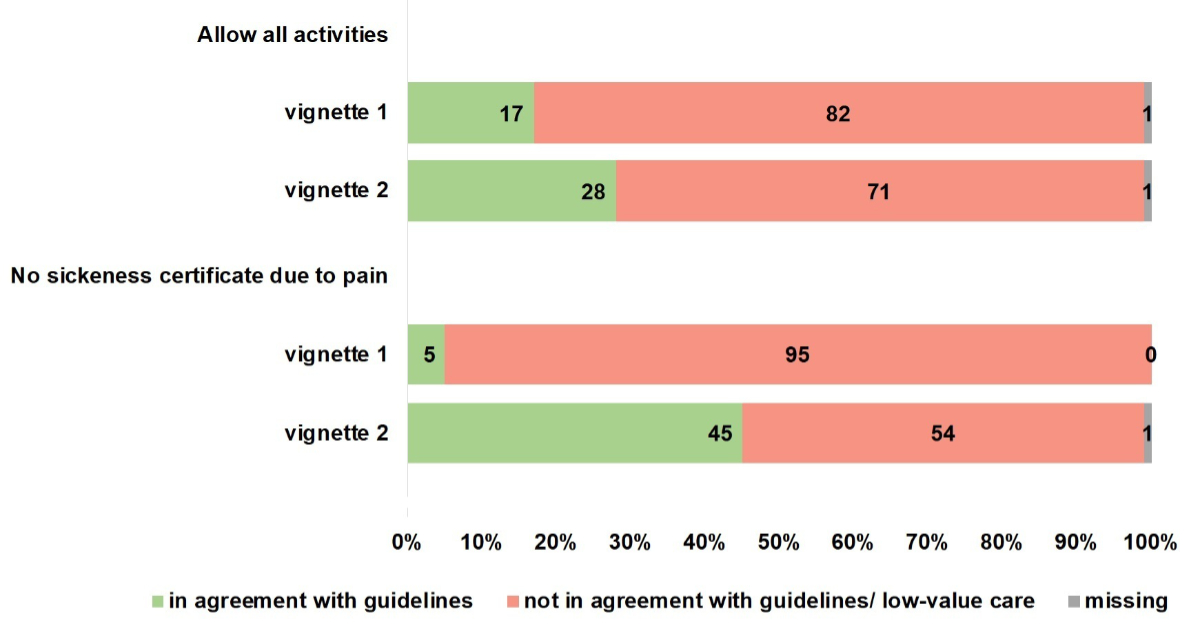
Figure 6Recommendations for activity and work in two acute non-specific low back pain vignettes (vignette 1, n = 1253; vignette 2, n = 1226). Low-value care for activity recommendations: any restrictions. Low-value care to work recommendations: issue sickness certificate. Questions, response options and the definitions of low-value care / disagreement with guidelines are provided in appendix 1.
The main difference by sex is that female GPs included a higher use of MRI in vignette 1 (44% vs 36% of male GPs, p = 0.04, table S1 in the appendix), muscle relaxants in vignette 2 (84% vs 76%, p = 0.01), non-pharmacological treatments (manual therapy, acupuncture) and referral to a specialist in vignette 2. Female GPs were less likely to use long-acting opioids in both vignettes (vignette 1, 14% vs 19%, p <0.001; vignette 2, 17% vs 20%, p <0.001), weak opioids (vignette 1, 16% vs 20%, p = 0.03) and a short course of oral steroids (vignette 1, 22% vs 32%, p <0.001).
GPs working in the German-speaking regions of Switzerland were more likely to adhere to guideline recommendations for no additional diagnostic tests (both vignettes) and no MRI in vignette 2 (36 vs 29%, p = 0.02, table S2 in the appendix). Whereas GPs in German-speaking regions used more metamizole (vignette 1, 91% vs 72%; vignette 2, 93% vs 72%; p <0.001), GPs in the French-/Italian-speaking regions were more likely to use paracetamol (vignette 1, 83% vs 63%; vignette 2, 83% vs 61%; p <0.001) and weak opioids (vignette 1, 27% vs 15%; vignette 2, 35% vs 18%; p <0.001).
Low-value care was more common among GPs in French-/Italian-speaking regions for the use of muscle relaxants (vignette 1, 88% vs 79%; vignette 2, 84% vs 78%; p <0.001), corticosteroid use in vignette 1 (38% vs 32%, p = 0.004) and spinal injections in vignette 2 (54% vs 46%, p = 0.002). GPs in French-/Italian-speaking regions were also more likely to prescribe low-value non-pharmacological treatments such as massage (vignette 1, 54% vs 46%, p = 0.003; vignette 2, 54% vs 44%; p <0.001) and acupuncture (vignette 1, 34% vs 23%; vignette 2, 41% vs 28%; p <0.001) and to recommend activity restrictions in vignette 1 (87% vs 81%, p = 0.04) compared to German-speaking GPs. They were also more likely to refer the patient in vignette 2 to a specialist (rheumatologist: 35% vs 28%, p = 0.003; spine surgeon: 37% vs 31%, p = 0.01).
In this survey completed by 1253 GPs, we observed substantial disagreement between current clinical practice and guideline recommendations. Most patients with an episode of non-specific low back pain as described in the two case vignettes recover spontaneously within 6 weeks [7]. In the current study, we found potential harmful practices in the use of diagnostic studies, pharmacological treatments and activity restriction recommendations to patients with acute low back pain which may result in unintended and costly consequences. Although no neurological deficits or red flags were present in either clinical vignette, a substantial proportion of GPs seemed not to be aware of the benign nature of the condition. Further, the presence of risk factors for chronic pain resulted in increased use of imaging studies and inappropriate treatments, GPs considered performing an MRI in up to 62% and/or an X-ray in up to 32% in vignette 2. Treatments of unknown benefit and/or potential harm in this patient population included muscle relaxants (up to 78%), long-acting strong opioids (8% and 11%), short course of corticosteroids (26% and 33%) and spinal injections (28% and 42%). The majority of GPs suggested activity restrictions, including bed rest or avoidance of all painful activities (82% and 71%), which conflicts with guideline recommendations.
Studies showed that early MRI in acute low back pain did not result in improved outcomes or better management [16, 18]. Despite efforts (e.g. Choosing Wisely campaign) to reduce the use of X-rays and MRIs [29, 40, 41], 1 in 4 patients presenting to GPs received imaging [40]. The use of MRI has been shown to increase the likelihood of prescription of strong opioids [42] and to increase the risk of invasive overtreatment (e.g. disc degeneration or herniation not related to the symptoms [5, 11]), worse wellbeing and delayed return to work [15, 17–19]. Although opioid use may be harmful, as recently confirmed in the OPAL trial [43], the prescription of opioids for low back pain remains high in primary care [23, 42, 44, 45]. The increasing use of strong opioids in minor musculoskeletal injuries over time indicates more liberal prescribing practice among primary care physicians – a worrying trend [46]. Further, there is a widespread use of non-recommended treatments such as muscle relaxants [47], oral steroids [48] and spinal injections [49]. Finally, activity restrictions may be harmful, supporting fear avoidance and catastrophising with increased risk of chronic low back pain [50], lower efficacy of treatment and recovery rates with more disability [51, 52].
Systematic application of guideline-adherent practices has been shown to be effective and improve care [53]. Although physicians appear to have high awareness of the guidelines and recommendations [41, 54], several barriers and factors may limit their readiness to implement them [54, 55]. Guidelines that are accepted by peers need to be based on high-quality evidence from clinical studies [56], that may increase the acceptance or agreement with the guidelines [57]. Changing recommendations, missing evidence and limited generalisability of clinical studies may limit adherence to recommendations.
Other potential barriers include overestimation of risk and fear of missing serious disease, habits in previous practice and personal beliefs. For example, physicians with high personal fear–avoidance beliefs were more likely to prescribe activity restrictions and bed rest [58–60]. Additional external barriers are uncertainty due to clinical manifestation, age of the patient and duration of symptoms, professional dignity, easy access to radiology services, patients’ experience and expectations, and desire to maintain a harmonious relationship with the patient [57, 61]. Whether interventions to improve GPs adherence to guidelines are effective is under debate [62]. In a recently published qualitative study, GPs made decisions about pain medications largely based on previous experience, also their own experience of low back pain, rather than guidelines [63].
Due to a growing shortage of GPs [26, 64], patients may increasingly seek care in emergency departments, which could lead to a further deterioration of the quality of care [65], additional referral to specialists and for imaging [56, 57, 61], thus resulting in unnecessary treatments. These emerging changes in healthcare provision call for new approaches. Tools intended to inform and educate patients during the physician-patient encounter may help [66]. Additionally, involving employers and running public media campaigns to increase awareness, educate and improve guideline adherence have been shown to be effective in reducing unnecessary visits to GPs and emergency departments [66–69].
GPs’ attitudes towards activity restriction are of concern [58]. According to a national survey, 1 in 5 Swiss people with acute low back pain were absent from work for a week and 1 in 12 for up to a month [70]. This perception can be further reinforced by the attitude of GPs. Only a minority of patients seeking care received advice to stay activeand return to work as soon as possible [23, 44]. Regional sociocultural patterns may additionally play a role. GPs in French-/Italian-speaking regions were more likely to refer patients to specialists, to recommend activity restrictions and to prescribe low-value non-pharmacological options. Other studies confirmed such differences with lower rates in elective surgeries such as hip and knee replacement, vertebroplasty, implantable cardiac devices [71–73], and differences in practice style, patients’ and physicians’ preferences [74, 75] in the French-/Italian-compared to the German-speaking regions.
There are several limitations that need to be discussed. First, we cannot exclude a selection of GPs that responded to the survey (response bias). If we hypothesise that GPs more interested in the treatment of acute low back pain responded to the survey, we would expect an even higher proportion of non-adherence with guideline recommendations in non-respondents. Second, although clinical vignettes to assess choices in medical practice are well established [76] and although we used accepted methods for them [28], they do not objectively assess real-time clinical care, and thus management may be different than reported in our study. However, 95% of GPs rated the clinical vignettes to be representative of their real low back pain patients. Third, we used cut-offs for agreement with guidelines/low-value care that may not be in agreement with all guidelines. For example, the use of paracetamol has changed over time and no evidence-based recommendations for metamizole exist. Different and changing guideline recommendations may influence current clinical practice and the delay between the publication of new evidence and its adoption into clinical practice may explain some of the variation observed in the current study. Finally, we cannot exclude chance findings due to multiple testing.
Future studies should assess the efficacy of interventions to improve guideline adherence by GPs, health literacy in patients and the impact of quality improvement interventions. In future studies, factors associated with the use of low-value care may help to design targeted interventions to train physicians. Many interventions, particularly those by policymakers, may have good intentions but not result in improved care. Further, our study suggests that interventions need to address regional/cultural differences and may require different approaches for French-, Italian- and German-speaking regions.
GPs need to be aware of the potential harmful effects of early imaging, ineffective treatments and recommendations that promote avoidance. Because GPs are under time pressure, information material, such as information for patients provided by the “Smarter Medicine – Choosing Wisely” campaign may facilitate the discussion with patients [29]. GPs could collaborate with physical therapists or other healthcare professionals with a high expertise in evidence-based care of patients with low back pain. Considering the increasing GP shortage, physical therapists may assist patients with self-management strategies, helping them to stay active and resume work early [77]. While GPs currently are often the first contact of patients with acute low back pain in Switzerland, new strategies such as facilitating direct contact with physical therapists might reduce costs and the burden for society through less imaging, medication, injections and surgery, as shown in retrospective studies [78].
Training programmes should include evidence-based management of low back pain in residents to improve care. A growing female GP workforce may be relevant to how patients with acute low back pain are managed. Although studies showed that female physicians were more likely to follow recommendations [79], female GPs were more likely to perform MRI studies and refer patients to specialists and, consistent with another study, male GPs were more likely to prescribe opioids [80] and corticosteroids. Thus, sex-specific aspects may be relevant in the training of the workforce.
Although GPs reported being aware of current guideline recommendations, management of acute non-specific low back pain was not in line with these recommendations. A substantial proportion of GPs considered imaging, treatments (e.g. muscle relaxants, long-acting strong opioids), activity and work restrictions with potentially harmful consequences.
The anonymised data and datasets analysed during the current study are available from the corresponding author upon reasonable request.
The authors would like to thank the primary care clinicians who took time to answer the survey, to share their decisions and their views of guidelines for care for low back pain. The authors would like to thank Nicholas Thalmann, research student, for testing the random sample for errors.
Author contributions: MT, MAT and MMW conceived and designed the study. All authors commented on the study design, the methods and case vignettes. MMW obtained research funding, supervised the conduct of the trial. Data collection and analysis was accomplished by MT and VH in collaboration with MRB and MMW. MRB and MT conducted the statistical analysis, compiled the tables and figures. MT and MMW wrote the first draft of the manuscript. All authors had access to the data, interpreted the study results and commented on the first draft. All authors reviewed the manuscript and approved the final version.
This research was supported by the Bernese Foundation for General Medicine (Berner Stiftung zur Förderung der Hausarztmedizin [HaST]) and the Swiss Foundation of Smarter Medicine – Choosing Wisely Switzerland.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al.; Lancet Low Back Pain Series Working Group. Low back pain: a call for action. Lancet. 2018 Jun;391(10137):2384–8. doi: https://doi.org/10.1016/S0140-6736(18)30488-4
2. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al.; Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention. Lancet. 2018 Jun;391(10137):2356–67. doi: https://doi.org/10.1016/S0140-6736(18)30480-X
3. Disease GB, Injury I, Prevalence C; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018 Nov;392(10159):1789–858. doi: https://doi.org/10.1016/S0140-6736(18)32279-7
4. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012 Feb;379(9814):482–91. doi: https://doi.org/10.1016/S0140-6736(11)60610-7
5. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017 Feb;389(10070):736–47. doi: https://doi.org/10.1016/S0140-6736(16)30970-9
6. Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009 Oct;60(10):3072–80. doi: https://doi.org/10.1002/art.24853
7. da C Menezes Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012 Aug;184(11):E613–24. doi: https://doi.org/10.1503/cmaj.111271
8. Zemedikun DT, Kigozi J, Wynne-Jones G, Guariglia A, Roberts T. Methodological considerations in the assessment of direct and indirect costs of back pain: A systematic scoping review. PLoS One. 2021 May;16(5):e0251406. doi: https://doi.org/10.1371/journal.pone.0251406
9. Wieser S, Horisberger B, Schmidhauser S, Eisenring C, Brügger U, Ruckstuhl A, et al. Cost of low back pain in Switzerland in 2005. Eur J Health Econ. 2011 Oct;12(5):455–67. doi: https://doi.org/10.1007/s10198-010-0258-y
10. Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014 Jun;73(6):968–74. doi: https://doi.org/10.1136/annrheumdis-2013-204428
11. Knezevic NN, Candido KD, Vlaeyen JW, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021 Jul;398(10294):78–92. doi: https://doi.org/10.1016/S0140-6736(21)00733-9
12. Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018 Nov;27(11):2791–803. doi: https://doi.org/10.1007/s00586-018-5673-2
13. Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al.; Lancet Low Back Pain Series Working Group. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018 Jun;391(10137):2368–83. doi: https://doi.org/10.1016/S0140-6736(18)30489-6
14. National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management, NICE Guideline, No. 59. 2020. Available from: https://www.nice.org.uk/guidance/ng59
15. Chou R, Qaseem A, Owens DK, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011 Feb;154(3):181–9. doi: https://doi.org/10.7326/0003-4819-154-3-201102010-00008
16. Gillan MG, Gilbert FJ, Andrew JE, Grant AM, Wardlaw D, Valentine NW, et al.; Scottish Back Trial Group. Influence of imaging on clinical decision making in the treatment of lower back pain. Radiology. 2001 Aug;220(2):393–9. doi: https://doi.org/10.1148/radiology.220.2.r01au06393
17. Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine. 2013 Oct;38(22):1939–46. doi: https://doi.org/10.1097/BRS.0b013e3182a42eb6
18. Ash LM, Modic MT, Obuchowski NA, Ross JS, Brant-Zawadzki MN, Grooff PN. Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. AJNR Am J Neuroradiol. 2008 Jun;29(6):1098–103. doi: https://doi.org/10.3174/ajnr.A0999
19. Lemmers GP, van Lankveld W, Westert GP, van der Wees PJ, Staal JB. Imaging versus no imaging for low back pain: a systematic review, measuring costs, healthcare utilization and absence from work. Eur Spine J. 2019 May;28(5):937–50. doi: https://doi.org/10.1007/s00586-019-05918-1
20. Rajasekaran S, Dilip Chand Raja S, Pushpa BT, Ananda KB, Ajoy Prasad S, Rishi MK. The catastrophization effects of an MRI report on the patient and surgeon and the benefits of ‘clinical reporting’: results from an RCT and blinded trials. Eur Spine J. 2021 Jul;30(7):2069–81. doi: https://doi.org/10.1007/s00586-021-06809-0
21. Stevans JM, Delitto A, Khoja SS, Patterson CG, Smith CN, Schneider MJ, et al. Risk Factors Associated With Transition From Acute to Chronic Low Back Pain in US Patients Seeking Primary Care. JAMA Netw Open. 2021 Feb;4(2):e2037371. doi: https://doi.org/10.1001/jamanetworkopen.2020.37371
22. Scott NA, Moga C, Harstall C. Managing low back pain in the primary care setting: the know-do gap. Pain Res Manag. 2010;15(6):392–400. doi: https://doi.org/10.1155/2010/252695
23. Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain. 2020 Apr;161(4):694–702. doi: https://doi.org/10.1097/j.pain.0000000000001751
24. Biller-Andorno N, Zeltner T. Individual Responsibility and Community Solidarity—The Swiss Health Care System. N Engl J Med. 2015 Dec;373(23):2193–7. doi: https://doi.org/10.1056/NEJMp1508256
25. Höglinger M, Knöfler F, Schaumann-von Stosch R, Scholz-Odermatt SM, Eichler K. Recent trends and variations in general practitioners’ involvement in accident care in Switzerland: an analysis of claims data. BMC Fam Pract. 2020 Jun;21(1):99. doi: https://doi.org/10.1186/s12875-020-01170-5
26. Stierli R, Rozsnyai Z, Felber R, Jörg R, Kraft E, Exadaktylos AK, et al. Primary Care Physician Workforce 2020 to 2025 - a cross-sectional study for the Canton of Bern. Swiss Med Wkly. 2021 Sep;151(3536):w30024. doi: https://doi.org/10.4414/SMW.2021.w30024
27. Rainville J, Carlson N, Polatin P, Gatchel RJ, Indahl A. Exploration of physicians’ recommendations for activities in chronic low back pain. Spine. 2000 Sep;25(17):2210–20. doi: https://doi.org/10.1097/00007632-200009010-00012
28. Evans SC, Roberts MC, Keeley JW, Blossom JB, Amaro CM, Garcia AM, et al. Vignette methodologies for studying clinicians’ decision-making: Validity, utility, and application in ICD-11 field studies. Int J Clin Health Psychol. 2015;15(2):160–70. doi: https://doi.org/10.1016/j.ijchp.2014.12.001
29. Smarter Medicine - Choosing Wisely Switzerland. Top Five List for "Choosing Wisely" Switzerland in Inpatient Sector. Published online first: 2016. Available from: https://www.smartermedicine.ch
30. Qaseem A, Wilt TJ, McLean RM, Forciea MA, Denberg TD, Barry MJ, et al.; Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017 Apr;166(7):514–30. doi: https://doi.org/10.7326/M16-2367
31. Corp N, Mansell G, Stynes S, Wynne-Jones G, Morsø L, Hill JC, et al. Evidence-based treatment recommendations for neck and low back pain across Europe: A systematic review of guidelines. Eur J Pain. 2021 Feb;25(2):275–95. doi: https://doi.org/10.1002/ejp.1679
32. Wong JJ, Côté P, Sutton DA, Randhawa K, Yu H, Varatharajan S, et al. Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. 2017 Feb;21(2):201–16. doi: https://doi.org/10.1002/ejp.931
33. Williams CM, Maher CG, Latimer J, McLachlan AJ, Hancock MJ, Day RO, et al. Efficacy of paracetamol for acute low-back pain: a double-blind, randomised controlled trial. Lancet. 2014 Nov;384(9954):1586–96. doi: https://doi.org/10.1016/S0140-6736(14)60805-9
34. Ostojic P, Radunovic G, Lazovic M, Tomanovic-Vujadinovic S. Ibuprofen plus paracetamol versus ibuprofen in acute low back pain: a randomized open label multicenter clinical study. Acta Reumatol Port. 2017;42(1):18–25.
35. Chiarotto A, Koes BW. Nonspecific Low Back Pain. N Engl J Med. 2022 May;386(18):1732–40. doi: https://doi.org/10.1056/NEJMcp2032396
36. Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014 Oct;14(10):2299–319. doi: https://doi.org/10.1016/j.spinee.2014.01.026
37. Steffens D, Ferreira ML, Latimer J, Ferreira PH, Koes BW, Blyth F, et al. What triggers an episode of acute low back pain? A case-crossover study. Arthritis Care Res (Hoboken). 2015 Mar;67(3):403–10. doi: https://doi.org/10.1002/acr.22533
38. Team, R.C., R: A language and environment for statistical computing. 2013.
39. The Federal Assembly of the Swiss Confederation. Federal Act on Research involving Human Beings (Human Research Act, HRA). Art. 2. Published Online First: 2011.; Available from: https://fedlex.data.admin.ch/eli/cc/2013/617
40. Downie A, Hancock M, Jenkins H, Buchbinder R, Harris I, Underwood M, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med. 2020 Jun;54(11):642–51. doi: https://doi.org/10.1136/bjsports-2018-100087
41. Selby K, Cornuz J, Cohidon C, Gaspoz JM, Senn N. How do Swiss general practitioners agree with and report adhering to a top-five list of unnecessary tests and treatments? Results of a cross-sectional survey. Eur J Gen Pract. 2018 Dec;24(1):32–8. doi: https://doi.org/10.1080/13814788.2017.1395018
42. Di Gangi S, Bagnoud C, Pichierri G, Rosemann T, Plate A. Treatment Patterns in Patients with Diagnostic Imaging for Low Back Pain: A Retrospective Observational Study. J Pain Res. 2021 Oct;14:3109–20. doi: https://doi.org/10.2147/JPR.S328033
43. Jones CM, Day RO, Koes BW, Latimer J, Maher CG, McLachlan AJ, et al.; OPAL Investigators Coordinators. Opioid analgesia for acute low back pain and neck pain (the OPAL trial): a randomised placebo-controlled trial. Lancet. 2023 Jul;402(10398):304–12. doi: https://doi.org/10.1016/S0140-6736(23)00404-X
44. Williams CM, Maher CG, Hancock MJ, McAuley JH, McLachlan AJ, Britt H, et al. Low back pain and best practice care: A survey of general practice physicians. Arch Intern Med. 2010 Feb;170(3):271–7. doi: https://doi.org/10.1001/archinternmed.2009.507
45. Di Gangi S, Pichierri G, Zechmann S, Rosemann T, Plate A. Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis. J Clin Med. 2021 Mar;10(7):1366. doi: https://doi.org/10.3390/jcm10071366
46. Müller D, Scholz SM, Thalmann NF, Trippolini MA, Wertli MM. Increased Use and Large Variation in Strong Opioids and Metamizole (Dipyrone) for Minor and Major Musculoskeletal Injuries Between 2008 and 2018: An Analysis of a Representative Sample of Swiss Workers. J Occup Rehabil. 2024 Mar;34(1):157–68.
47. Soprano SE, Hennessy S, Bilker WB, Leonard CE. Assessment of Physician Prescribing of Muscle Relaxants in the United States, 2005-2016. JAMA Netw Open. 2020 Jun;3(6):e207664. doi: https://doi.org/10.1001/jamanetworkopen.2020.7664
48. Chou R, Pinto RZ, Fu R, Lowe RA, Henschke N, McAuley JH, et al. Systemic corticosteroids for radicular and non-radicular low back pain. Cochrane Database Syst Rev. 2022 Oct;10(10):CD012450.
49. Oliveira CB, Maher CG, Ferreira ML, Hancock MJ, Oliveira VC, McLachlan AJ, et al. Epidural Corticosteroid Injections for Sciatica: An Abridged Cochrane Systematic Review and Meta-Analysis. Spine. 2020 Nov;45(21):E1405–15. doi: https://doi.org/10.1097/BRS.0000000000003651
50. Vlaeyen JW, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016 Aug;157(8):1588–9. doi: https://doi.org/10.1097/j.pain.0000000000000574
51. Wertli MM, Burgstaller JM, Weiser S, Steurer J, Kofmehl R, Held U. Influence of catastrophizing on treatment outcome in patients with nonspecific low back pain: a systematic review. Spine. 2014 Feb;39(3):263–73. doi: https://doi.org/10.1097/BRS.0000000000000110
52. Wertli MM, Rasmussen-Barr E, Weiser S, Bachmann LM, Brunner F. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. Spine J. 2014 May;14(5):816–36.e4. doi: https://doi.org/10.1016/j.spinee.2013.09.036
53. Bruns D, Mueller K, Warren PA. Biopsychosocial law, health care reform, and the control of medical inflation in Colorado. Rehabil Psychol. 2012 May;57(2):81–97. doi: https://doi.org/10.1037/a0028623
54. Epstein-Sher S, Jaffe DH, Lahad A. Are They Complying? Physicians’ Knowledge, Attitudes, and Readiness to Change Regarding Low Back Pain Treatment Guideline Adherence. Spine. 2017 Feb;42(4):247–52. doi: https://doi.org/10.1097/BRS.0000000000001714
55. Fullen BM, Baxter GD, O’Donovan BG, Doody C, Daly LE, Hurley DA. Factors impacting on doctors’ management of acute low back pain: a systematic review. Eur J Pain. 2009 Oct;13(9):908–14. doi: https://doi.org/10.1016/j.ejpain.2008.11.013
56. Traeger AC, Buchbinder R, Elshaug AG, Croft PR, Maher CG. Care for low back pain: can health systems deliver? Bull World Health Organ. 2019 Jun;97(6):423–33. doi: https://doi.org/10.2471/BLT.18.226050
57. Slade SC, Kent P, Patel S, Bucknall T, Buchbinder R. Barriers to Primary Care Clinician Adherence to Clinical Guidelines for the Management of Low Back Pain: A Systematic Review and Metasynthesis of Qualitative Studies. Clin J Pain. 2016 Sep;32(9):800–16. doi: https://doi.org/10.1097/AJP.0000000000000324
58. Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002 Dec;12(4):223–32. doi: https://doi.org/10.1023/A:1020218422974
59. Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012 Jan;16(1):3–17. doi: https://doi.org/10.1016/j.ejpain.2011.06.006
60. Buchbinder R, Staples M, Jolley D. Doctors with a special interest in back pain have poorer knowledge about how to treat back pain. Spine. 2009 May;34(11):1218–26. doi: https://doi.org/10.1097/BRS.0b013e318195d688
61. Espeland A, Baerheim A. Factors affecting general practitioners’ decisions about plain radiography for back pain: implications for classification of guideline barriers—a qualitative study. BMC Health Serv Res. 2003 Mar;3(1):8. doi: https://doi.org/10.1186/1472-6963-3-8
62. Suman A, Schaafsma FG, van de Ven PM, Slottje P, Buchbinder R, van Tulder MW, et al. Effectiveness of a multifaceted implementation strategy compared to usual care on low back pain guideline adherence among general practitioners. BMC Health Serv Res. 2018 May;18(1):358. doi: https://doi.org/10.1186/s12913-018-3166-y
63. Ferreira GE, Zadro J, Jones C, Ayre J, Lin C, Richards B, et al. General practitioners’ decision-making process to prescribe pain medicines for low back pain: a qualitative study. BMJ Open. 2023 Oct;13(10):e074380. doi: https://doi.org/10.1136/bmjopen-2023-074380
64. Pahud O. Ärztinnen und Ärzte in der Grundversorgung - Situation in der Schweiz und im internationalen Vergleich. Schweizerisches Gesundheitsobservatorium (Obsan) 2019; Available from: https://www.obsan.admin.ch/de/publikationen/
65. Jermini-Gianinazzi I, Blum M, Trachsel M, Trippolini MA, Tochtermann N, Rimensberger C, et al. Management of acute non-specific low back pain in the emergency department: do emergency physicians follow the guidelines? Results of a cross-sectional survey. BMJ Open. 2023 Aug;13(8):e071893. doi: https://doi.org/10.1136/bmjopen-2023-071893
66. Fifer SK, Choundry NK, Brod M, Hsu E, Milstein A. Improving adherence to guidelines for spine pain care: what tools could support primary care clinicians in conforming to guidelines? BMJ Open Qual. 2022 Aug;11(3):e001868. doi: https://doi.org/10.1136/bmjoq-2022-001868
67. Coenen P, de Wind A, van de Ven P, de Maaker-Berkhof M, Koes B, Buchbinder R, et al. The slow de-implementation of non-evidence-based treatments in low back pain hospital care-Trends in treatments using Dutch hospital register data from 1991 to 2018. Eur J Pain. 2023 Feb;27(2):212–22. doi: https://doi.org/10.1002/ejp.2052
68. Lambeek LC, van Tulder MW, Swinkels IC, Koppes LL, Anema JR, van Mechelen W. The trend in total cost of back pain in The Netherlands in the period 2002 to 2007. Spine. 2011 Jun;36(13):1050–8. doi: https://doi.org/10.1097/BRS.0b013e3181e70488
69. Suman A, Armijo-Olivo S, Deshpande S, Marietta-Vasquez J, Dennett L, Miciak M, et al. A systematic review of the effectiveness of mass media campaigns for the management of low back pain. Disabil Rehabil. 2021 Dec;43(24):3523–51. doi: https://doi.org/10.1080/09638288.2020.1743777
70. Rheumaliga. Rueckenreport Schweiz 2020. Published Online First: 2021. Available from: https://saez.ch/article/doi/saez.2021.19449
71. Wertli MM, Schlapbach JM, Haynes AG, Scheuter C, Jegerlehner SN, Panczak R, et al. Regional variation in hip and knee arthroplasty rates in Switzerland: A population-based small area analysis. PLoS One. 2020 Sep;15(9):e0238287. doi: https://doi.org/10.1371/journal.pone.0238287
72. Frei AN, Gellad WF, Wertli MM, Haynes AG, Chiolero A, Rodondi N, et al. Trends and regional variation in vertebroplasty and kyphoplasty in Switzerland: a population-based small area analysis. Osteoporos Int. 2021 Dec;32(12):2515–24. doi: https://doi.org/10.1007/s00198-021-06026-x
73. Bolt L, Wertli MM, Haynes AG, Rodondi N, Chiolero A, Panczak R, et al. Variation in regional implantation patterns of cardiac implantable electronic device in Switzerland. PLoS One. 2022 Feb;17(2):e0262959. doi: https://doi.org/10.1371/journal.pone.0262959
74. OECD. Switzerland: Geographic Variations in Health Care: Whrat Do We Know and What Can Be Done to Improve Health System Performance? OECD Health Policy Studies. Paris: OECD Publishing; 2014. doi:. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/geographic-variations-in-health-care_9789264216594-en
75. Eggli Y, Stadelmann P, Piaget-Rossel R, Marti J. Heterogeneity in The drivers of health expenditures financed by health insurance in a fragmented health system: the case of Switzerland. Health Policy. 2019 Dec;123(12):1275–81. doi: https://doi.org/10.1016/j.healthpol.2019.10.010
76. Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000 Apr;283(13):1715–22. doi: https://doi.org/10.1001/jama.283.13.1715
77. Fritz JM, Magel JS, McFadden M, Asche C, Thackeray A, Meier W, et al. Early Physical Therapy vs Usual Care in Patients With Recent-Onset Low Back Pain: A Randomized Clinical Trial. JAMA. 2015 Oct;314(14):1459–67. doi: https://doi.org/10.1001/jama.2015.11648
78. Garrity BM, McDonough CM, Ameli O, Rothendler JA, Carey KM, Cabral HJ, et al.; Unrestricted Direct Access to Physical Therapist Services Is Associated With Lower Health Care Utilization and Costs in Patients With New-Onset Low Back Pain. Unrestricted Direct Access to Physical Therapist Services Is Associated With Lower Health Care Utilization and Costs in Patients With New-Onset Low Back Pain. Phys Ther. 2020 Jan;100(1):107–15. doi: https://doi.org/10.1093/ptj/pzz152
79. Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of Hospital Mortality and Readmission Rates for Medicare Patients Treated by Male vs Female Physicians. JAMA Intern Med. 2017 Feb;177(2):206–13. doi: https://doi.org/10.1001/jamainternmed.2016.7875
80. Tamblyn R, Girard N, Boulet J, Dauphinee D, Habib B. Association of clinical competence, specialty and physician country of origin with opioid prescribing for chronic pain: a cohort study. BMJ Qual Saf. 2022 May;31(5):340–52. doi: https://doi.org/10.1136/bmjqs-2021-013503
The appendix is available in the pdf version of the article at https://doi.org/10.57187/s.3697.