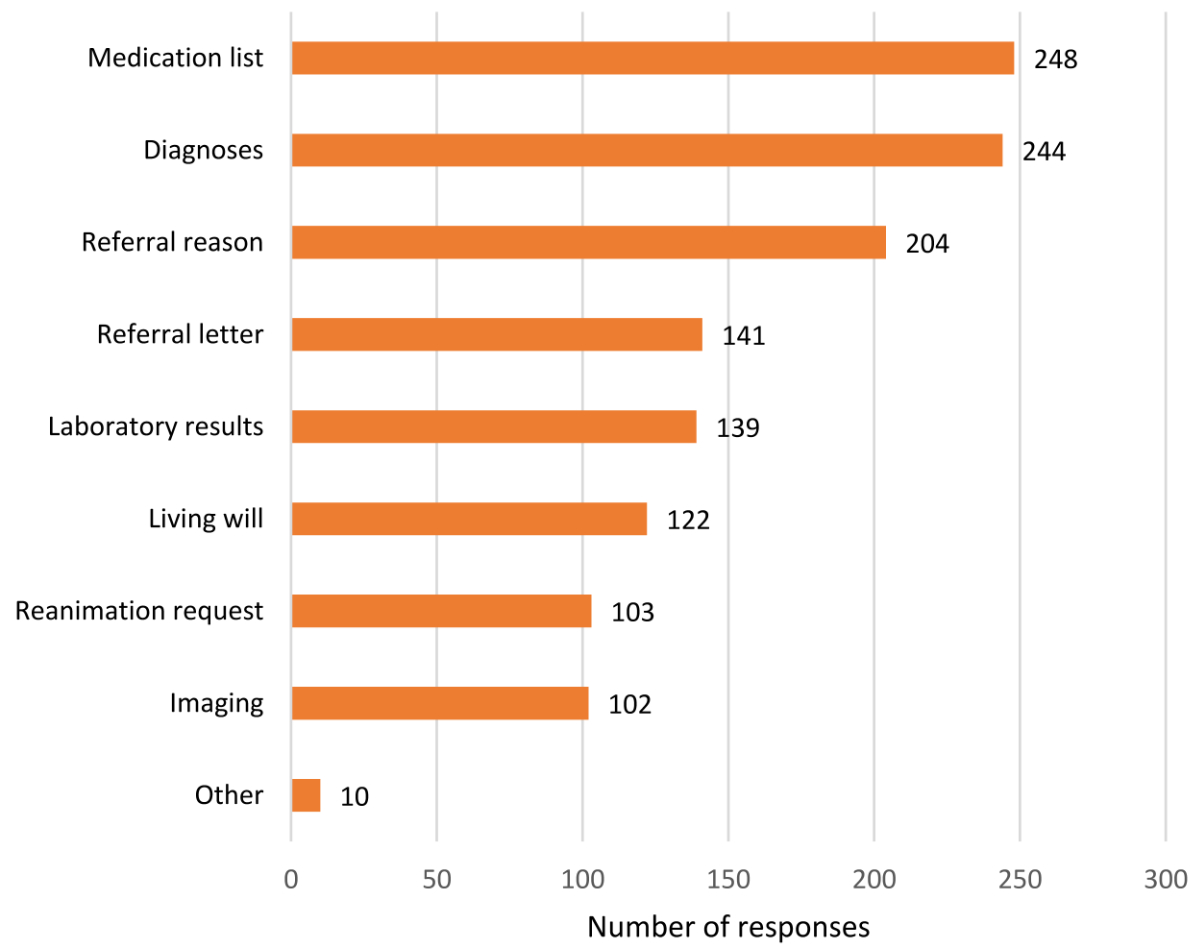
Figure 1Information that hospitalists most preferred in referrals from PCPs.
DOI: https://doi.org/https://doi.org/10.57187/s.3643
Effective communication and information exchange, especially during transitions of care, have a significant impact on patient safety and continuity of care [1]. Understanding and satisfaction among patients and healthcare providers, as well as the use of limited resources in the medical setting, are also positively affected [2, 3].
A systematic review on provider-to-provider communication during transition from outpatient to acute care found that delayed or incomplete transmission of patients’ medical records led to omitted or incorrect assessments, ultimately resulting in longer hospital stays and increased risk of morbidity and mortality [4]. Given the increasing complexity of health care [4] and the resulting rise in healthcare costs due to insufficient information exchange [5], effective and secure transmission of patient data is of great importance [4]. A survey assessing mutual communication between primary care physicians (PCPs) and specialists in the Netherlands showed that they disagreed on several aspects of their communication [5]. Hence, it is important to recognise and understand differences and needs of different provider groups in order to improve communication [6].
To our knowledge, there have been no Swiss studies to date examining the perspective of hospitalists on communication with PCPs. The present study focuses on hospitalists’ views of their communication with PCPs in the region of Central Switzerland. Our primary objective was to assess satisfaction with mutual communication with PCPs. The secondary objectives of this study were to gather information about the referral process and communication with PCPs. This included identifying the required information in the referral letter and the preferred communication channel of the hospitalists. Additionally, regarding mutual communication, the views of hospitalists and those of PCPs from a previous cross-sectional study were compared based on seven similar questions [7].
A cross-sectional survey was conducted in six hospitals in the Central Switzerland region to investigate what hospitalists consider important in their communication with PCPs. The survey was in German and contained 17 questions (see supplementary material). In this study, a hospitalist is a physician of any specialty working in a hospital, be it with inpatients, with outpatients or in a mixed setting.
For this cross-sectional survey, a structured questionnaire was created using Google Forms. The questionnaire addressed the satisfaction of communication between hospitalists and PCPs from the hospitalists’ perspective. Our study adhered to the consensus-based Checklist for Reporting Of Survey Studies (CROSS) [8]. There was no study protocol.
Hospitalists from six hospitals in the cantons of Lucerne and Nidwalden were asked directly and anonymously about their opinion regarding communication with PCPs by means of a questionnaire. Prior to sending out the questionnaire, contact was made with the respective management of the collaborating hospitals to ensure that the survey reached the target physicians. Four of the six included hospitals were part of the Lucerne Cantonal Hospital (LUKS): Lucerne, Wolhusen, Stans and Sursee. The other two participating hospitals were the Hirslanden Clinic St Anna and the Swiss Paraplegic Centre in Nottwil. Thus, the definition of the sample size was geographical and not by power calculation.
The questionnaire was developed in a two-step process and then sent to the target group by email. The survey was anonymous, and participation was voluntary. The development process included literature research on effective provider-to-provider communication and direct communication with providers by means of a questionnaire. The authors did not pilot-test the questionnaire, but instead relied on expert assessment by experienced hospitalists and PCPs.
The questionnaire contained (1) five closed-ended questions on demographics, profession and work setting, with the option of free-text entries on work location, work setting and profession if none of the options applied, (2) two closed-ended questions using a 5-point Likert item to investigate the satisfaction of communication between hospitalists and PCPs, (3) five Likert item questions on the frequency of information exchange between hospitalists and PCPs, (4) most important data that hospitalists would like to have when receiving referral letters from PCPs, (5) which information channel hospitalists prefer and (6) three open-ended questions seeking suggestions on how to improve interdisciplinary communication, handoffs between shifts and internal patient triage. All questions had to be answered except for the open-ended questions. The questionnaire language was German.
The target population consisted of hospitalists, categorised into residents and specialists, working at one of the six included hospitals and who are in regular contact with PCPs, i.e. mainly internists and surgeons (n = 1134). All physicians employed by a hospital and having patient contact were regarded as hospitalists. A resident physician is a physician who graduated from medical school and is being trained for specialty board certification. An attending physician is a doctor with board certification.
Data collection started at the end of October 2021 and the last emails were sent out by the research team or hospital administration at the beginning of February 2022. Each site reminded the hospitalists of the questionnaire approximately one month after the first email was sent. Hospitalists who had already filled in the questionnaire were told to ignore the reminder in order to prevent double entries.
In two cases, information given for the year of birth was not reasonable because the value to be entered was not predefined. These unreasonable values were imputed by using the mean value of all years of birth, in each case grouped by either residents or attending physicians.All hospitalists who reported working in a specialty other than internal medicine or surgery were assigned to the “Others” group. All respondents who stated that they worked in the emergency setting were assigned to the “Mixed” group, as they work in both inpatient and outpatient settings. In the mixed group, no further distinctions were made regarding the relative proportions of inpatient and outpatient work.
In a previous cross-sectional study among PCPs in Central Switzerland, PCPs’ views regarding communication with hospitalists were assessed [7]. As a secondary objective of our study, the responses of hospitalists and PCPs to similar questions were juxtaposed and compared.
Categorical variables are presented as counts and percentages, continuous variables with non-normal distribution as medians and first and third quartiles (expressed as interquartile ranges [IQR]). Chi-square tests were used to compare categorical variables between groups, the Kruskal-Wallis test to compare continuous variables. Potential associations between hospitalists’ characteristics and responses were analysed by exploratory multivariable logistic regression models. We also analysed a potential association between age and sex of hospitalists. For regression analyses, results are reported as odds ratios (OR) and 95% confidence intervals (95% CI). To dichotomise the Likert-scale item responses, responses categorised as responses 1 (never; very dissatisfied; strongly disagree), 2 (rarely; dissatisfied; disagree) and 3 (sometimes; neutral) were placed in one group, while responses 4 (often; satisfied; agree) and 5 (always; very satisfied; strongly agree) were placed in another. Multivariable logistic regression analyses were also performed to compare the responses of hospitalists and PCPs. For table 1, stratification according to age group quartiles was done. Free-text responses on suggestions for improvement were summarised according to their frequencies. The data were processed and analysed using R (version 4.2.1).
A total of 276 completed questionnaires were received from the 1134 hospitalists included in the survey, corresponding to a response rate of 24.3%.
Table 1 illustrates the demographic characteristics of the participants stratified by age quartiles. Most participants were specialists (73.5%, 203/276); most participants worked in internal medicine (56.5%, 156/276).
An adjusted logistic regression showed that younger physicians tend to be female and older ones male (OR 3.33; 95% CI 1.85–6.10; see also supplementary tables).
Table 1Characteristics of hospitalists, stratified by age quartiles.
| Age 26–34 | Age 35–44 | Age 45–52 | Age 53–72 | Overall | |
| Number of hospitalists | 70 | 71 | 70 | 65 | 276 |
| Age in years – median [IQR] | 30 [29–32] | 39 [37–42] | 47.5 [46–50] | 59 [56–61] | 44 [33.8–52] |
| Male – n (%) | 26 (37.7%) | 34 (46.6%) | 46 (66.7%) | 52 (80.0%) | 158 (57.2%) |
| Participants per hospital | |||||
| Hospital A – n (%) | 41 (59.4%) | 52 (71.2%) | 48 (69.6%) | 34 (52.3%) | 175 (63.4%) |
| Hospital B – n (%) | 7 (10.1%) | 5 (6.8%) | 4 (5.8%) | 8 (12.3%) | 24 (8.7%) |
| Hospital C – n (%) | 9 (13.0%) | 3 (4.1%) | 2 (2.9%) | 6 (9.2%) | 20 (7.2%) |
| Hospital D – n (%) | 4 (5.8%) | 4 (5.5%) | 4 (5.8%) | 5 (7.7%) | 17 (6.2%) |
| Hospital E – n (%) | 5 (7.2%) | 6 (8.2%) | 7 (10.1%) | 1 (1.5%) | 19 (6.9%) |
| Hospital F – n (%) | 6 (8.7%) | 4 (5.5%) | 5 (7.2%) | 11 (16.9%) | 26 (9.4%) |
| Professional background – n (%) | |||||
| Attending physician, internal medicine | 5 (7.2%) | 30 (41.1%) | 39 (56.5%) | 32 (49.2%) | 106 (38.4%) |
| Attending physician, surgery | 3 (4.3%) | 28 (38.4%) | 19 (27.5%) | 29 (44.6%) | 79 (28.6%) |
| Attending physician, other specialty | 1 (1.4%) | 6 (8.2%) | 7 (10.1%) | 4 (6.2%) | 18 (6.5%) |
| Resident, internal medicine | 40 (58.0%) | 7 (9.6%) | 3 (4.3%) | 0 (0.0%) | 50 (18.1%) |
| Resident, surgery | 16 (23.2%) | 2 (2.7%) | 0 (0.0%) | 0 (0.0%) | 18 (6.5%) |
| Resident, other specialty | 4 (5.8%) | 0 (0.0%) | 1 (1.4%) | 0 (0.0%) | 5 (1.8%) |
| Work setting – n (%) | |||||
| Inpatient setting | 33 (47.1%) | 23 (32.4%) | 19 (27.1%) | 16 (24.6%) | 91 (33.0%) |
| Mixed setting | 29 (41.4%) | 29 (40.8%) | 29 (42.0%) | 31 (47.7%) | 120 (43.5%) |
| Outpatient setting | 8 (11.4%) | 19 (26.8%) | 20 (29.0%) | 18 (27.7%) | 65 (23.6%) |
The majority of participants were satisfied with the general communication with PCPs and patient referrals (figure 2, questions 6 and 7; table S2 in the appendix).
Most hospitalists reported that they rarely inform PCPs about their patients’ emergency admissions and that PCPs rarely contact the hospitalists when they learn about such admissions. However, most hospitalists agreed with the statement that hospitals should inform PCPs of their patients’ emergency admissions in a timely manner.
The analysis revealed that the information hospitalists most urgently needed in referrals from PCPs were the medication list (89.9%, 248/276), the diagnoses (88.4%, 244/276) and the reason for referral (73.9%, 204/276) (see figure 1 for further results). The preferred communication channels for referral letters were email (76.8%, 212/276) and electronic portals (65.5%, 181/276).
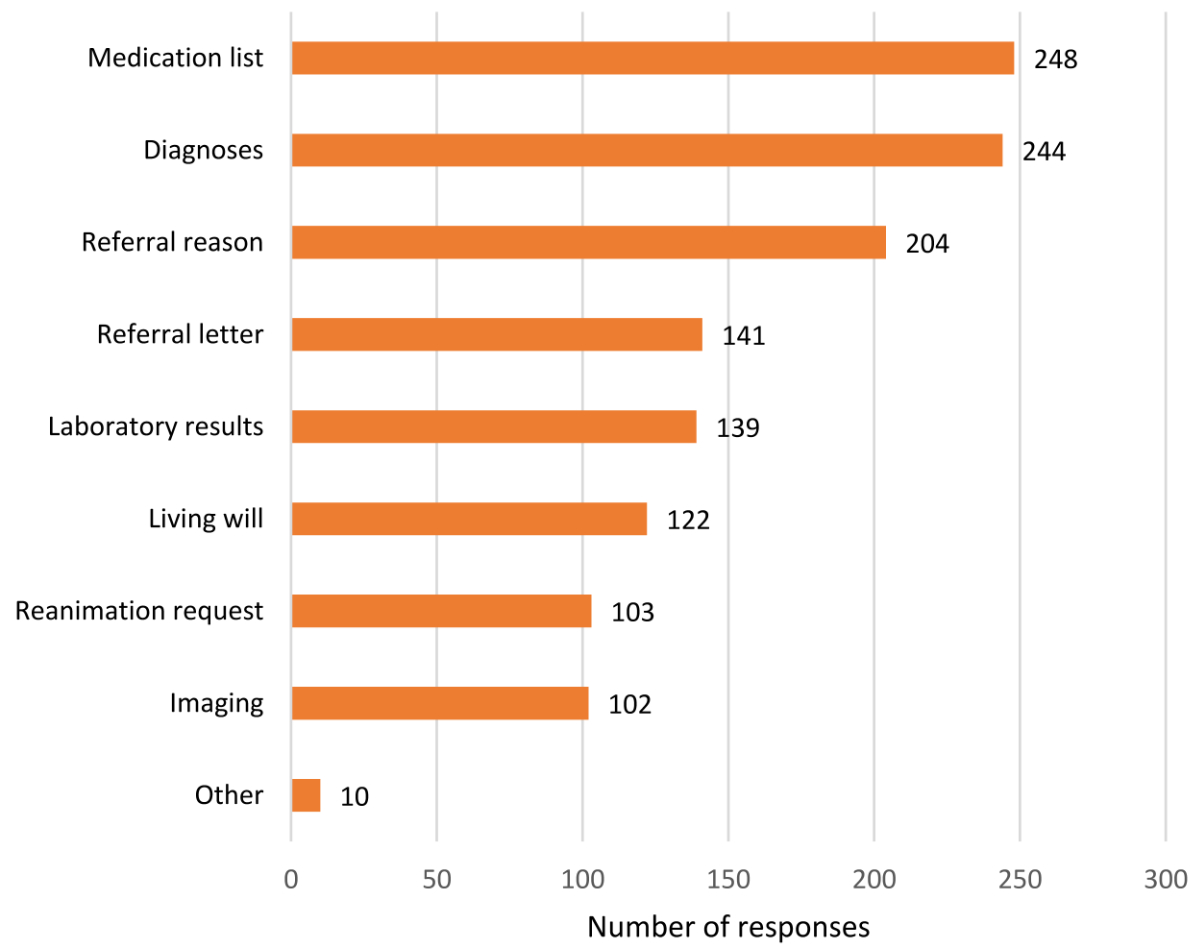
Figure 1Information that hospitalists most preferred in referrals from PCPs.
On multivariable regression, compared to other clinicians, internists independently favoured informing PCPs of emergency admissions of their patients in a timely manner (OR 2.04; 95% CI 1.21–3.49).
Compared to other clinicians, a positive association between internists and the frequency of wanting Advance Care Planning (ACP) in the referral was found (OR 1.88; 95% CI 1.11– 3.22).
Although email was popular among hospitalists, they were less likely to prefer email in a hospital with an electronic communication portal (OR 0.20; 95% CI 0.05–0.61) compared to hospitals without electronic communication portals. Furthermore, with increasing clinician age, telephone, mail by post and fax were more preferred communication channels for referrals, independently of other factors (OR 2.52; 95% CI 1.47–4.36).
Free-text responses provided insight into hospitalists’ opinions on improving interdisciplinary communication. When asked about suggestions for improving communication between hospitalists and PCPs, “access for everyone and simplification of the software” was mentioned most frequently; a standardised design of the communication software was explicitly requested. There was also a call for a “clear line on how and via which system to communicate [...]” for mutual communication.
No statistically significant difference in satisfaction with communication in general (OR 1.40; 95% CI 0.89–2.18) and with referrals (OR 1.05; 95% CI 0.67–1.63) was found in multivariable regression comparing PCPs and hospitalists. Figure 2 compares hospitalists’ and PCPs’ responses to seven similar questions.
Among both hospitalists (76.8%, 212/276) and PCPs (97.2%, 106/109), email emerged as the favoured channel for information. However, in contrast to PCPs (18.3%, 20/109), substantially more hospitalists (65.6%, 181/276) chose electronic portals as an additional preferred communication channel (see regression result in the “Patient referrals” section above).
When asked how often hospitalists inform PCPs after treatment (question 9), respectively how often PCPs are informed by hospitalists, 79.4% (219/276) of hospitalists indicated that they often to always inform PCPs after the patient’s stay, 45.9% (50/109) of the latter answered that they are never or rarely informed. In contrast to PCPs, hospitalists perceived that they inform the PCPs regarding the hospital stay (OR 8.64; 95% CI 5.23–14.59).
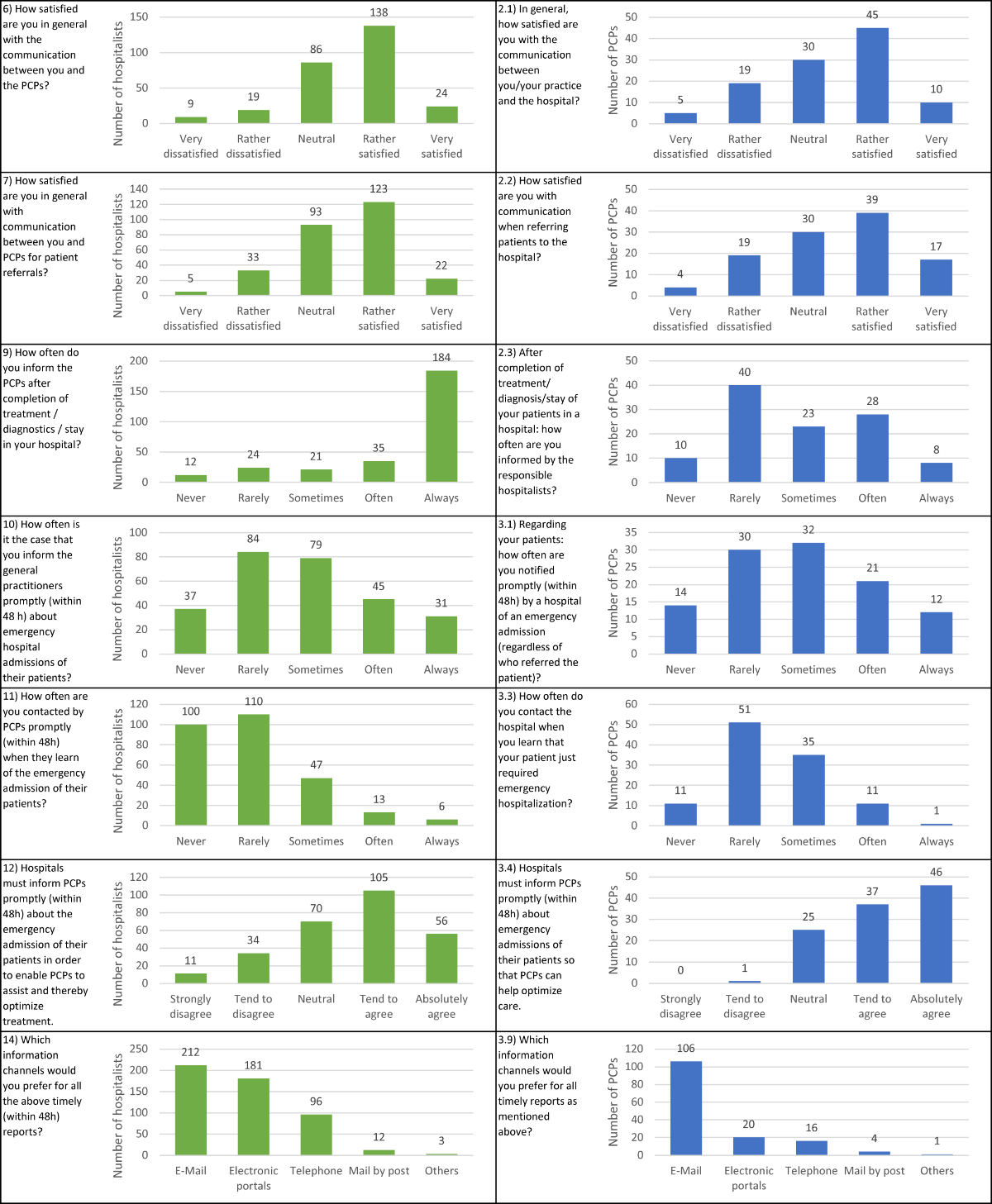
Figure 2Direct comparisons of hospitalists’ (left side) and PCPs’ (right side) responses to seven similar questions.
For relative numbers, please refer to table S2 in the appendix.
This cross-sectional survey was conducted with the objective of evaluating satisfaction with communication between hospitals and PCPs in Central Switzerland, as perceived by the local hospitalists, with a focus on determining the preferred content and communication channels for referral letters.
Our results revealed the following: (1) Hospitalists are mostly satisfied with communication with PCPs. However, there is a discrepancy between hospitalists’ and PCPs’ perceptions regarding the flow of information after the hospital stay is completed. (2) According to the crude numbers, communication via email is popular among hospitalists. On regression however, we found that the availability of an electronic communication portal is statistically significantly associated with a lower favourability of emails. (3) The three most important items of information hospitalists need in a referral letter from PCPs in a timely manner are the medication list, the diagnoses and the reason for referral. (4) The majority of hospitalists agree with the statement that it is necessary for hospitals to inform PCPs of their patients’ emergency admissions in a timely manner so that they can help to optimise care. (5) The most frequently mentioned suggestions about improving the communication between hospitals and PCPs were an easily accessible software for both parties and a consistent communication style and channel.
In the present study, hospitalists were asked what they require in a referral letter from PCPs. The three most common answers were the medication list, the diagnoses and the reason for referral. A survey of hospitalists and PCPs conducted in the Netherlands found that hospitalists believe referral letters from PCPs often contain inadequate or incomplete information or do not always state a specific reason for referral [5]. Therefore, the consensus, especially in relation to reason for referral by PCPs, shows that this problem also exists internationally.
In this study, compared to surgeons and other physicians, internists more frequently selected that they would like to have information on ACPs in referral letters. This could be explained by the higher proportion of critically ill inpatients for whom ACPs are available. This is also reflected in a Swiss survey of physicians on ACPs for elective cardiovascular surgery: nearly 60% of respondents stated that the optimal moment to establish ACP is when the patient experiences a serious illness or comorbidity which is often the reason for hospitalisation [10].
Most hospitalists and PCPs agreed with the statement that hospitals must inform PCPs as soon as possible about the hospitalisation of their patients so that they can contribute to improved treatment. However, compared with PCPs, significantly more hospitalists disagreed with this statement regardless of sex and age. Most hospitalists reported that they only sometimes contact PCPs to inform them of their patients’ hospitalisation. In addition, most hospitalists stated that they are very rarely contacted by PCPs when they refer their patients to the emergency department. This contradiction between attitudes regarding the involvement of PCPs in treatment and the actual behaviour of hospitalists can be explained by several factors, for instance, the greater workload in reaching out to PCPs and lack of time [11]. A study from Switzerland also emphasises the uncertainty regarding the best strategy for communication between hospitalists and PCPs, as PCPs want to be informed about the hospitalisation or discharge of their patients from hospital on the one hand, but do not want to be called so as not to be disturbed on the other [12].
It is increasingly important that relevant information from the inpatient to the outpatient setting is not only concise but complete, relevant and timely [13]. In the present study, the majority of hospitalists said they would always or often inform PCPs after completion of their patient’s hospital stay, while nearly half of PCPs said they never or rarely receive such information from the hospitalists. This discrepancy was also demonstrated in other studies between PCPs and specialists [5, 14]. According to another study, PCPs indicated that they often did not know when patients were hospitalised and also did not have hospital recommendations for post-hospitalisation appointments [11]. We believe that hospitalists actually do inform PCPs, and that the discrepancy in perception may be explained by the time taken, several days or even weeks, for the discharge summary to reach the PCPs. One study found that the strongest predictor of discharge letter availability in the follow-up setting was direct access to inpatient data [13]. However, the fragmented digitalisation of outpatient healthcare is likely to hinder effective communication between hospitalists and PCPs [12]. Furthermore, a systematic review found that well-designed IT solutions can improve communication, coordination and storage of information, leading to better patient outcomes [15]. Well-designed electronic portals for data interchange may therefore play an increasingly important role in informing PCPs sooner [11].
According to the crude numbers, email was chosen as the most preferred information channel by both hospitalists and PCPs, closely followed by electronic portals for hospitalists. However, on multivariable regression analysis of the responses of hospitalists, we found that a hospital’s provision of an electronic communication portal is independently associated with a lower favourability of emails. Another study also examined communication preferences during care transitions between hospitalists and PCPs using electronic medical records (EMR). It was found that PCPs preferred direct communication at discharge through a message within the EMR, while hospitalists preferred a message through EMR and email. These results show the potential of EMR for future communication between the two provider groups [16].
An association was found in the study between increasing age and preference for older communication channels such as telephone or mail by post. However, one study demonstrated that it is hardly feasible to implement a standardised process for communication to PCPs by telephone, because either the hospitalists lacked time or had problems reaching the PCPs [17].
One goal of this study was to suggest opportunities for improvement in communication between hospitalists and PCPs. A study has shown that a referral template leads to higher-quality referrals [18]. The results of the present study on the content of referral letters desired by hospitalists and the data on the electronic referral portal and its functionality provide potentially more efficient communication processes. Further studies are needed to evaluate the introduction of electronic support to improve referrals and discharge reporting.
There are some limitations that should be considered when interpreting the results of our study. Although it involved a large heterogeneous sample, bias in the sampling strategy may still have occurred. For example, this survey was conducted online, and it is possible that participants with IT skills were more inclined to answer the web-based questionnaires. In addition, the study is based on self-reporting, which may encourage desirability bias, whereby individuals change their answers in a survey to be viewed favourably by others. However, participants were informed in advance that the surveys were voluntary and anonymous. There could also be a selection bias due to non-responses. Generalisation to other regions or countries may not be warranted and may show different results. As the survey was conducted in hospitals in Central Switzerland, it may not be applicable to the whole of Switzerland or other countries.
Another limitation of our study is that the questionnaire was developed using face validity and expert assessments without pretest nor a sample size calculation, which might have affected the internal validity of the study.
A strength of the study is its multicentre design. Although the results may not be applicable to the whole of Switzerland, the coverage of the survey (Central Switzerland and six hospitals) makes this study of fundamental value and a sound basis for further surveys. However, in terms of sample repetitiveness, some observations in this study align well with the Swiss landscape: the median age of our hospitalists was 44 (IQR 33.8–52), which is in line with a recent statistic by the Swiss Medical Association. And, unsurprisingly, our study confirms known demographic changes among physicians in Switzerland [9]: with decreasing age, it is more likely that the physician is female.
Most hospitalists are satisfied with the communication with PCPs, and vice versa. What needs to be improved are the timely transmission of patient information and the use of electronic communication channels. Electronic data interchange may be the key for future improvements of timely notifications sent from hospitalists to PCPs and vice versa.
We thank all physicians who responded to our survey questions.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007 Feb;297(8):831–41. 10.1001/jama.297.8.831
2. Situation, Background, Assessment, Recommendation (SBAR) Communication Tool for Handoff in Health Care – A Narrative Review | Safety in Health | Full Text, https://safetyinhealth.biomedcentral.com/articles/10.1186/s40886-018-0073-1 (accessed 13 October 2022).
3. Sheehan J, Laver K, Bhopti A, Rahja M, Usherwood T, Clemson L, et al. Methods and Effectiveness of Communication Between Hospital Allied Health and Primary Care Practitioners: A Systematic Narrative Review. J Multidiscip Healthc. 2021 Feb;14:493–511. 10.2147/JMDH.S295549
4. Luu NP, Pitts S, Petty B, Sawyer MD, Dennison-Himmelfarb C, Boonyasai RT, et al. Provider-to-Provider Communication during Transitions of Care from Outpatient to Acute Care: A Systematic Review. J Gen Intern Med. 2016 Apr;31(4):417–25. 10.1007/s11606-015-3547-4
5. Berendsen AJ, Kuiken A, Benneker WH, Meyboom-de Jong B, Voorn TB, Schuling J. How do general practitioners and specialists value their mutual communication? A survey. BMC Health Serv Res. 2009 Aug;9(1):143. 10.1186/1472-6963-9-143
6. Berendsen AJ, Benneker WH, Schuling J, Rijkers-Koorn N, Slaets JP, Meyboom-de Jong B. Collaboration with general practitioners: preferences of medical specialists—a qualitative study. BMC Health Serv Res. 2006 Dec;6(1):155. 10.1186/1472-6963-6-155
7. Tomaschek R, Beeler PE, Grgičević K, Müller LS, Merlo C, Hug BL. Communication and information exchange between practices and hospitals: a survey among primary care practitioners in Central Switzerland. Swiss Med Wkly. (submitted).
8. Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med. 2021 Oct;36(10):3179–87. 10.1007/s11606-021-06737-1
9. Hostettler S, Kraft E. Jeder vierte Arzt ist 60 Jahre alt oder älter. Schweiz Arzteztg. 2022;103(13):414–9.
10. Gigon F, Merlani P, Ricou B. Swiss physicians’ perspectives on advance directives in elective cardiovascular surgery. Minerva Anestesiol. 2015 Oct;81(10):1061–75.
11. Jones CD, Vu MB, O’Donnell CM, Anderson ME, Patel S, Wald HL, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015 Apr;30(4):417–24. 10.1007/s11606-014-3056-x
12. Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021 May;11(5):e049872. 10.1136/bmjopen-2021-049872
13. Robelia PM, Kashiwagi DT, Jenkins SM, Newman JS, Sorita A. Information Transfer and the Hospital Discharge Summary: National Primary Care Provider Perspectives of Challenges and Opportunities. J Am Board Fam Med. 2017;30(6):758–65. 10.3122/jabfm.2017.06.170194
14. Vermeir P, Vandijck D, Degroote S, Ommeslag D, Van De Putte M, Heytens S, et al. Mutual perception of communication between general practitioners and hospital-based specialists. Acta Clin Belg. 2015 Oct;70(5):350–6. 10.1179/2295333715Y.0000000032
15. Newnham H, Barker A, Ritchie E, Hitchcock K, Gibbs H, Holton S. Discharge communication practices and healthcare provider and patient preferences, satisfaction and comprehension: A systematic review. Int J Qual Health Care. 2017 Oct;29(6):752–68. 10.1093/intqhc/mzx121
16. Munchhof A, Gruber R, Lane KA, Bo N, Rattray NA. Beyond Discharge Summaries: Communication Preferences in Care Transitions Between Hospitalists and Primary Care Providers Using Electronic Medical Records. J Gen Intern Med. 2020 Jun;35(6):1789–96. 10.1007/s11606-020-05786-2
17. Enzinger L, Dumanoir P, Boussat B, Couturier P, Francois P. Direct phone communication to primary care physician to plan discharge from hospital: feasibility and benefits. BMC Health Serv Res. 2021 Dec;21(1):1352. 10.1186/s12913-021-07398-w
18. Wåhlberg H, Valle PC, Malm S, Broderstad AR. Impact of referral templates on the quality of referrals from primary to secondary care: a cluster randomised trial. BMC Health Serv Res. 2015 Aug;15(1):353. 10.1186/s12913-015-1017-7
Table S1Stratified by hospital.
| Hospital A | Hospital B | Hospital C | Hospital D | Hospital E | Hospital F | |
| n Hospitalists | 175 | 24 | 20 | 17 | 19 | 26 |
| Age – median (IQR) | 44 (34, 50) | 44 (32, 56) | 38.5 (32, 53.5) | 45 (34, 56) | 40 (33, 49.5) | 50.5 (35.25, 58.75) |
| Male (%) | 101 (57.7) | 13 (54.2) | 8 (40.0) | 12 (70.6) | 8 (42.1) | 20 (76.9) |
| Setting (%) | ||||||
| Inpatient setting | 59 (33.7) | 6 (25.0) | 6 (30.0) | 1 (5.9) | 6 (31.6) | 13 (50.0) |
| Mixed | 71 (40.6) | 14 (58.3) | 10 (50.0) | 14 (82.4) | 11 (57.9) | 4 (15.4) |
| Outpatient setting | 45 (25.7) | 4 (16.7) | 4 (20.0) | 2 (11.8) | 2 (10.5) | 9 (34.6) |
| Professional background (%) | ||||||
| Attending physician in other subject | 7 (4.0) | 3 (12.5) | 2 (10.0) | 4 (23.5) | 5 (26.3) | 13 (50.0) |
| Attending physician of a medical subject | 68 (38.9) | 9 (37.5) | 7 (35.0) | 1 (5.9) | 9 (47.4) | 6 (23.1) |
| Attending physician of a surgical subject | 53 (30.3) | 6 (25.0) | 6 (30.0) | 9 (52.9) | 4 (21.1) | 7 (26.9) |
| Resident in a medical subject | 28 (16.0) | 6 (25.0) | 4 (20.0) | 1 (5.9) | 1 (5.3) | 0 (0.0) |
| Resident in a surgical subject | 16 (9.1) | 0 (0.0) | 1 (5.0) | 2 (11.8) | 0 (0.0) | 0 (0.0) |
| Resident in other subject | 3 (1.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Overall | 175 | 24 | 20 | 17 | 19 | 26 |
Table S2Questions with Likert item classification.
| Question | Mean | Median | Most frequent answer | Response | n (%) | |
| 6 | How satisfied are you in general with the communication between you and the primary care physicians? | 3.5 | Satisfied (4) | Satisfied (4 | Very dissatisfied (1) | 9 (3.3) |
| Dissatisfied (2) | 19 (6.9) | |||||
| Neutral (3) | 86 (31.2) | |||||
| Satisfied (4) | 138 (50) | |||||
| Very satisfied (5) | 24 (8.7) | |||||
| Total | 276 (100) | |||||
| 7 | How satisfied are you with the communication between you and the primary care physicians regarding patient referrals? | 3.5 | Satisfied (4) | Satisfied (4) | Very dissatisfied (1) | 5 (1.8) |
| Dissatisfied (2) | 33 (12) | |||||
| Neutral (3) | 93 (33.7) | |||||
| Satisfied (4) | 123 (44.6) | |||||
| Very satisfied (5) | 22 (8.0) | |||||
| Total | 276 (100) | |||||
| 8 | How often do you receive a referral letter (letter or email) when patients are referred to you by primary care physicians? | 3.9 | Often (4) | Often (4) | Never (1 | 11 (4) |
| Rarely (2) | 19 (6.9) | |||||
| Sometimes (3) | 45 (16.3) | |||||
| Often (4) | 117 (42.4) | |||||
| Always (5) | 84 (30.4) | |||||
| Total | 276 (100) | |||||
| 9 | How often do you inform the primary care physicians after completion of treatment/diagnostics/ stay in your hospital? | 4.3 | Always (5) | Always (5) | Never (1) | 12 (4.4) |
| Rarely (2) | 24 (8.7) | |||||
| Sometimes (3) | 21 (7.6) | |||||
| Often (4) | 35 (12.7) | |||||
| Always (5) | 184 (66.7) | |||||
| Total | 276 (100 | |||||
| 10 | How often do you inform the primary care physicians promptly (within 48 hours) about emergency hospital admissions of their patients? | 2.8 | Sometimes (3) | Rarely (2) | Never (1) | 37 (13.4) |
| Rarely (2) | 84 (30.4) | |||||
| Sometimes (3) | 79 (28.6) | |||||
| Often (4) | 45 (16.3) | |||||
| Always (5) | 31 (11.2) | |||||
| Total | 276 (100) | |||||
| 11 | How often are you contacted by the primary care physicians in a timely manner (within 48 hours) when they learn of the emergency admission of their patients? | 2 | Rarely (2) | Rarely (2 | Never (1) | 100 (36.2) |
| Rarely (2) | 110 (39.9) | |||||
| Sometimes (3) | 47 (17) | |||||
| Often (4) | 13 (4.7) | |||||
| Always (5) | 6 (2.2) | |||||
| Total | 276 (100) | |||||
| 12 | Hospitals must inform primary care physicians promptly (within 48 hours) about the emergency admission of their patients in order to enable primary care physicians to assist and thus optimize treatment. | 3.6 | Agree (4) | Agree (4) | Strongly disagree (1) | 11 (4) |
| Disagree (2) | 34 (12.3) | |||||
| Neutral (3) | 70 (25.4) | |||||
| Agree (4) | 105 (38) | |||||
| Strongly agree (5) | 56 (20.3) | |||||
| Total | 276 (100) | |||||
Model 1Unadjusted regression model for association with male sex.
| Variable | OR | (95% CI) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 1.56 | (0.80, 3.06) |
| Physicians aged 45–52 | 3.24 | (1.64, 6.57) |
| Physicians aged 53–72 | 6.77 | (3.18, 15.18) |
Model 1Adjusted regression model for association with male sex.
| Variable | OR | (95% CI) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 1.67 | (0.63, 4.57) |
| Physicians aged 45–52 | 3.75 | (1.34, 10.99) |
| Physicians aged 53–72 | 7.68 | (2.50, 24.85) |
| Other clinicians | Ref. | |
| Internists | 0.71 | (0.41, 1.24) |
| Attendings | Ref. | |
| Residents | 1.02 | (0.40, 2.67) |
| Inpatient setting | Ref. | |
| Mixed setting | 0.90 | (0.48, 1.66) |
| Outpatient setting | 0.50 | (0.24, 1.02) |
Model 1Adjusted regression model for association with male sex.
| Variable | OR | (95% CI) |
| Physicians aged 26–44 | Ref. | |
| Physicians aged 45–72 | 3.33 | (1.85, 6.10) |
| Other clinicians | Ref. | |
| Internists | 0.69 | (0.40, 1.19) |
| Attendings | Ref. | |
| Residents | 0.70 | (0.36, 1.36) |
| Inpatient setting | Ref. | |
| Mixed setting | 0.91 | (0.49, 1.66) |
| Outpatient setting | 0.52 | (0.26, 1.05) |
Model 2Unadjusted regression model for association with advance healthcare directives.
| Variable | OR | (95% CI) |
| Other clinicians | Ref. | |
| Internists | 2.08 | (1.28, 3.42) |
Model 2Adjusted regression model for association with advance healthcare directives.
| Variable | OR | (95% CI) |
| Male sex | Ref. | |
| Female sex | 1.38 | (0.80, 2.36) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 1.12 | (0.55, 2.28) |
| Physicians aged 45–52 | 1.01 | (0.49, 2.09) |
| Physicians aged 53–72 | 0.89 | (0.41, 1.93) |
| Other clinicians | Ref. | |
| Internists | 1.88 | (1.11, 3.22) |
| Inpatient setting | Ref. | |
| Mixed setting | 0.37 | (0.21, 0.66) |
| Outpatient setting | 0.41 | (0.20, 0.80) |
Model 3Unadjusted regression model for association with e-mail.
| Variable | OR | (95% CI) |
| Hospital without communication portal | Ref. | |
| Hospital with communication portal | 0.21 | (0.05, 0.59) |
Model 3Adjusted regression model for association with e-mail.
| Variable | OR | (95% CI) |
| Female sex | Ref. | |
| Male sex | 0.80 | (0.41, 1.55) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 0.09 | (0.02, 0.26) |
| Physicians aged 45–52 | 0.20 | (0.04, 0.67) |
| Physicians aged 53–72 | 0.11 | (0.02, 0.37) |
| Other clinicians | Ref. | |
| Internists | 1.07 | (0.56, 2.03) |
| Inpatient setting | Ref. | |
| Mixed setting | 0.82 | (0.38, 1.72) |
| Outpatient setting | 0.67 | (0.29, 1.56) |
| Hospital without communication portal | Ref. | |
| Hospital with communication portal | 0.20 | (0.05, 0.61) |
Model 4Unadjusted regression model for association with older communication channels (telephone, fax).
| Variable | OR | (95% CI) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 0.85 | (0.41, 1.78) |
| Physicians aged 45–52 | 2.20 | (1.11, 4.46) |
| Physicians aged 53–72 | 2.13 | (1.06, 4.35) |
Model 4Adjusted regression model for association with older communication channels (telephone, fax).
| Variable | OR | (95% CI) |
| Female sex | Ref. | |
| Male sex | 0.77 | (0.44, 1.33) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 0.88 | (0.41, 1.89) |
| Physicians aged 45–52 | 2.37 | (1.14, 5.02) |
| Physicians aged 53–72 | 2.34 | (1.08, 5.16) |
| Other clinicians | Ref. | |
| Internists | 1.06 | (0.62, 1.82) |
| Inpatient setting | Ref. | |
| Mixed setting | 1.88 | (1.04, 3.46) |
| Outpatient setting | 1.07 | (0.52, 2.20) |
Model 4Adjusted regression model for association with older communication channels (telephone, fax).
| Variable | OR | (95% CI) |
| Female sex | Ref. | |
| Male sex | 0.76 | (0.44, 1.31) |
| Physicians aged 26–44 | Ref. | |
| Physicians aged 45–72 | 2.52 | (1.47, 4.36) |
| Other clinicians | Ref. | |
| Internists | 1.07 | (0.63, 1.84) |
| Inpatient setting | Ref. | |
| Mixed setting | 1.88 | (1.04, 3.45) |
| Outpatient setting | 1.05 | (0.52, 2.14) |
Model 5Unadjusted regression model for association with agreeing or strongly agreeing that hospitals must inform PCPs promptly about the emergency admission of their patients (question 12).
| Variable | OR | (95% CI) |
| Other clinicians | Ref. | |
| Internists | 1.84 | (1.13, 2.99) |
Model 5Adjusted regression model for association with agreeing or strongly agreeing that hospitals must inform PCPs promptly about the emergency admission of their patients (question 12).
| Variable | OR | (95% CI) |
| Female sex | Ref. | |
| Male sex | 1.18 | (0.69, 2.01) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 0.89 | (0.45, 1.78) |
| Physicians aged 45–52 | 1.73 | (0.84, 3.60) |
| Physicians aged 53–72 | 1.51 | (0.71, 3.24) |
| Inpatient setting | Ref. | |
| Mixed setting | 1.26 | (0.70, 2.25) |
| Outpatient setting | 0.99 | (0.50, 1.97) |
| Other clinicians | Ref. | |
| Internists | 2.04 | (1.21, 3.49) |
Model 6Unadjusted regression model for association with the general satisfaction in communication between PCPs and hospitalists (question 6).
| Variable | OR | (95% CI) |
| Primary care providers | Ref. | |
| Hospitalists | 1.40 | (0.89, 2.18) |
Model 6Adjusted regression model for association with the general satisfaction in communication between PCPs and hospitalists (question 6).
| Variable | ||
| Male sex | Ref. | |
| Female sex | 0.94 | (0.62, 1.44) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 1.00 | (0.56, 1.79) |
| Physicians aged 45–52 | 0.69 | (0.39, 1.23) |
| Physicians aged 53–72 | 0.74 | (0.41, 1.34) |
| Primary care providers | Ref. | |
| Hospitalists | 1.38 | (0.88, 2.16) |
Model 7Unadjusted regression model for association with the general satisfaction in communication regarding patient referrals between PCPs and hospitalists (question 7).
| Variable | OR | (95% CI) |
| Primary care providers | Ref. | |
| Hospitalists | 1.05 | (0.67, 1.63) |
Model 7Adjusted regression model for association with the general satisfaction in communication regarding patient referrals between PCPs and hospitalists (question 7).
| Variable | OR | (95% CI) |
| Male sex | Ref. | |
| Female sex | 0.96 | (0.63, 1.47) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 1.61 | (0.91, 2.87) |
| Physicians aged 45–52 | 0.96 | (0.54, 1.68) |
| Physicians aged 53–72 | 1.20 | (0.67, 2.15) |
| Primary care providers | Ref. | |
| Hospitalists | 1.06 | (0.68, 1.66) |
Model 8Unadjusted regression model for association of how often the hospitalists informing the PCPs (question 9) results: PCPs vs hospitalists.
| Variable | OR | (95% CI) |
| Primary care providers | Ref. | |
| Hospitalists | 7.79 | (4.79, 12.90) |
Model 8Adjusted regression model for association of how often the hospitalists informing the PCPs (question 9) results: PCPs vs hospitalists.
| Variable | OR | (95% CI) |
| Male sex | Ref. | |
| Female sex | 0.80 | (0.49, 1.31) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 2.16 | (1.10, 4.30) |
| Physicians aged 45–52 | 2.35 | (1.20, 4.69) |
| Physicians aged 53–72 | 1.59 | (0.81, 3.15) |
| Primary care providers | Ref. | |
| Hospitalists | 8.64 | (5.23, 14.59) |
Model 9Unadjusted regression model for association with agreeing or strongly agreeing that hospitals must inform PCPs promptly about the emergency admission of their patients (question 12) results: PCPs vs hospitalists.
| Variable | OR | (95% CI) |
| Primary care providers | Ref. | |
| Hospitalists | 0.44 | (0.26, 0.72) |
Model 9Adjusted regression model for association with agreeing or strongly agreeing that hospitals must inform PCPs promptly about the emergency admission of their patients (question 12) results: PCPs vs hospitalists.
| Variable | OR | (95% CI) |
| Male sex | Ref. | |
| Female sex | 0.74 | (0.48, 1.15) |
| Physicians aged 26–34 | Ref. | |
| Physicians aged 35–44 | 0.62 | (0.34, 1.12) |
| Physicians aged 45–52 | 1.30 | (0.71, 2.39) |
| Physicians aged 53–72 | 1.20 | (0.64, 2.25) |
| Primary care providers | Ref. | |
| Hospitalists | 0.43 | (0.26, 0.71) |