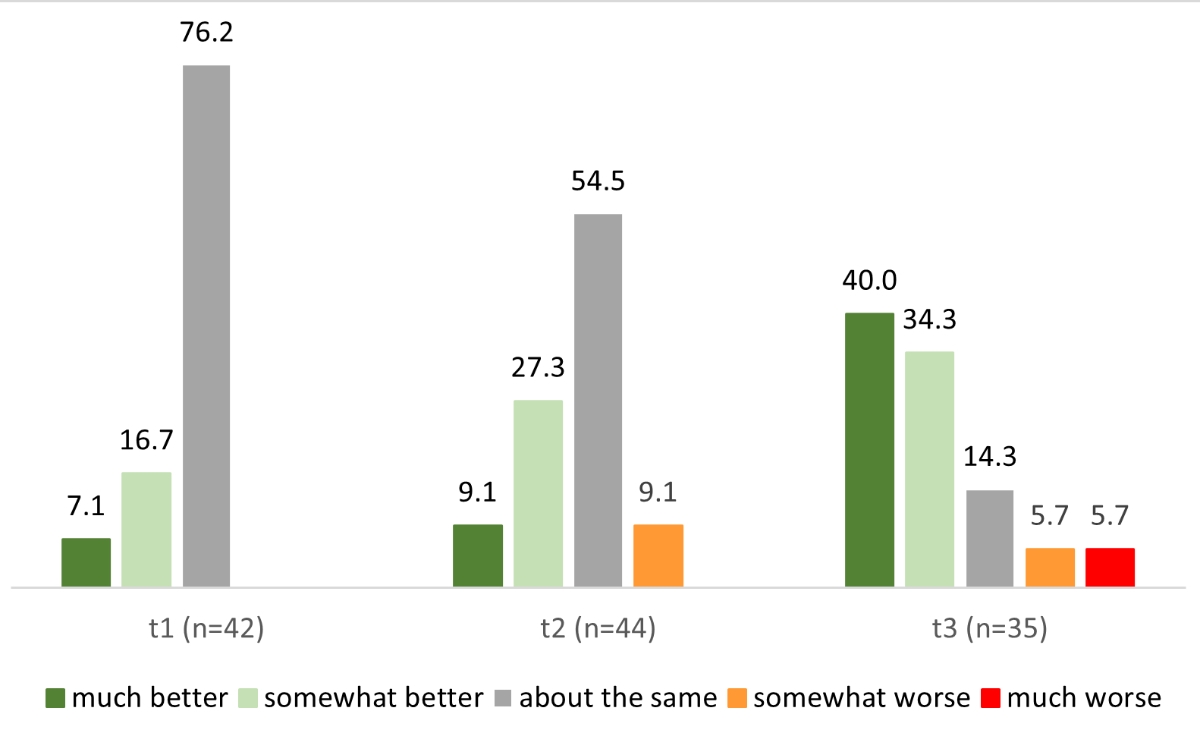
Figure 1Current state of health compared to before consultation. Numbers represent percentages.
DOI: https://doi.org/https://doi.org/10.57187/s.3622
The epidemiological and clinical characteristics of patients with acute COVID-19 as well as the therapeutic principles underlying their treatment have already been researched and described [1, 2]. The following definitions have become established [3]:
According to a global analysis of pandemic data at the end of 2021, which also included data from the Swiss Corona Immunitas Study, around 15% of people with COVID worldwide showed persistent pulmonary, neurological, cardiovascular or other physical symptoms/complications for more than 12 months [1, 5]. Despite the high number of cases worldwide, the aetiology, prevalence and risk factors for post-COVID are still unclear. However, the probability of developing post-COVID has not been shown to be related to the severity of the acute COVID [3].
Post-COVID is characterised by a diverse complex of symptoms and complaints affecting the organ system (e.g. pulmonary, cardiovascular, endocrine, haematological, renal, gastrointestinal and hepatobiliary, dermatological) or neuropsychiatric (e.g. fatigue, myalgia, cognitive impairment) [6] that can have a major impact on the quality of life of COVID survivors [7]. The most common symptoms of post-COVID are fatigue (51%, exhaustion often combined with physical pain, depression or anxiety), respiratory (60%, persistent cough or shortness of breath) and cognitive (35%, e.g. forgetfulness, “brain fog”). Some 38% of patients show several of these symptom complexes [5]. Other known common symptoms include headaches, musculoskeletal pain, sleep problems and dizziness [8].
At the beginning of 2021, the Department of Pneumology at the Cantonal Hospital Winterthur initiated a multidisciplinary post-COVID outpatient clinic for patients with persistent complaints and symptoms after COVID disease. At that time, there were no studies on post-COVID from the patient perspective. There are now systematic reviews of qualitative or mixed-methods studies showing that people with post-COVID face complex psychological, physical and social challenges [9, 10]. The support of medical professionals is of great relevance in this context. Data on this subject were mainly published in Great Britain, Italy and Denmark [9, 10]. The perspective of patients with post-COVID in Switzerland, in the context of their medical care, has not yet been systematically examined. Therefore, the aim of this study was to record patient satisfaction with the consultation, interventions and measures initiated at the multidisciplinary post-COVID outpatient clinic at Cantonal Hospital Winterthur, and to explore and describe the course of the complaints longitudinally.
At the multidisciplinary post-COVID outpatient clinic of the Cantonal Hospital Winterthur, pulmonologists record patients’ medical histories and clinical examinations. Patients are also evaluated using the instruments listed in table 1. According to the clinical findings and individual preferences, a multidisciplinary team of pulmonologists, psychologists, physiotherapists, pain experts and members of a specialised home care team determines a treatment plan. The success of the treatment is evaluated regularly and necessary adjustments made.
Table 1Outcomes collected at each time point.
| Time point | t1 consultation | t2 follow-up I | t3 follow-up II | |
| Day 0–7 | Week 4–8 | Month 4–6 | ||
| Questionnaire | Questionnaire and interview | Questionnaire and interview | ||
| Data | ||||
| Sociodemographic characteristics | Age, sex, education, employment, workload, inability to work | X | ||
| Clinical examination | Body Mass Index, comorbidities, pulmonary function status, laboratory analysis in the context of COVID-19, functional walking test, date of first symptoms of the COVID-19 infection, inpatient treatment (if yes, duration), intensive care unit treatment (if yes, duration), HADS, PCFS, Chalder Fatigue scale, post-COVID Visual Analogue Scale, specific treatment of COVID-19 | X | X | |
| Patient perspective | Reasons for consulting the multidisciplinary post-COVID outpatient clinic, most challenging symptoms, satisfaction with multidisciplinary post-COVID outpatient clinic, satisfaction with therapeutic measures | X | X | X |
HADS: Hospital Anxiety and Depression Scale; PCFS: post-COVID-19 Functional Status.
This is an observational study with a mixed-methods design. Specifically, quantitative data from questionnaires and clinical examinations, and qualitative data from semi-structured interviews were combined in a triangulation design [11].
All patients with post-COVID syndrome who visited the multidisciplinary post-COVID outpatient clinic at the Cantonal Hospital Winterthur between 1 November 2021 and 25 October 2022, were invited to participate. Exclusion criteria included insufficient written and/or spoken German, age under 18 years and unwillingness to participate. The target sample size was 50 patients.
From this total sample, a consecutive subsample was selected for two interviews per person at two time points. A sample of ten people would allow us to consider different levels of illness severity (according to the Post-COVID Functional Scale [PCFS] [12]), different groups of main symptoms (i.e. fatigue or respiratory limitation), as well as variation in sex and age of participants.
Data collection used both quantitative and qualitative methods (table 1).
Quantitative data were collected via a questionnaire completed at three time points post-consultation: 0–7 days (t1), 4–8 weeks (t2) and 4–6 months (t3). The questionnaire consisted of two parts: customised questions specific to the clinic (yes/no answers, Likert scales and free-text fields) and standardised questionnaires, including the Hospital Anxiety and Depression Scale (HADS) [13], the Chalder Fatigue Scale (CFS) [14], the PCFS [12] and the post-COVID Visual Analogue Scale (PC-VAS).
Data were managed using REDCap electronic data capture tools hosted at Zurich University of Applied Sciences (ZHAW). REDCap provides an intuitive interface for validated data capture, audit trails for tracking data manipulation and export procedures, automated export procedures for seamless data downloads to statistical packages, and integration and interoperability with external sources [15].
Qualitative data were collected at time points t1 and t3 through semi-structured interviews focusing on:
Interview guidelines were tested and refined for redundancy with feedback from a patient and a Cantonal Hospital Winterthur staff member before data collection began. The questionnaires and interview guidelines are available in the appendix.
The first patient was included in the study on 1 November 2021, and the last inclusion was on 25 October 2022. The final interview was conducted in April 2023. After agreement to participate, patients received the first questionnaire on paper directly after their consultation at the multidisciplinary post-COVID outpatient clinic. They were asked to complete it within one week and return it to Zurich University of Applied Sciences, the independent evaluator for this project. The survey was repeated at two additional time points with slightly modified questionnaires (table 1); for these subsequent surveys, participants could choose to complete the questionnaires electronically via REDCap or on paper. Paper responses were entered into REDCap upon receipt. The dispatch and receipt of the questionnaires were tracked and documented in a spreadsheet. Participants who did not respond were reminded to do so via email, phone or in writing. Data collection was regularly checked for completeness and plausibility using REDCap’s evaluation functions.
The interviews were conducted face-to-face in a separate room at the Cantonal Hospital Winterthur by two researchers from Zurich University of Applied Sciences (AKR, a female physiotherapist PhD; SEK: a female psychologist MSc). SEK conducted the first 10 interviews, and AKR, after listening to audiotapes of these interviews, conducted the next ten. Researchers and interviewees met for the first time during the interviews, which lasted 27–66 minutes for the first round and 8–45 minutes for the second. No field notes were taken.
Only study staff requiring access for their tasks had access to identifying participant information, which was otherwise pseudonymised with a consecutive ID.
The quantitative data from the questionnaires were analysed exploratively. Cochran’s Q-test was employed to examine disparities in the distribution of binary-coded variables across multiple time points (e.g. differences in the number of individuals affected by a specific symptom at t1, t2 and t3). This test evaluates the null hypothesis that the proportion of affected individuals remains consistent across all three time points against the alternative hypothesis that it differs at least at one time point. The Q-statistic is calculated as the sum of squared differences between the proportions of observations within each category across the time points, divided by the total number of observations minus the number of groups. The Q-statistic follows a chi-squared distribution. If the calculated Q-statistic exceeds the critical value, the null hypothesis is rejected.
The Friedman test was used to assess disparities in the distribution of metric variables across multiple time points (e.g. differences in symptom intensity at t1, t2 and t3). This nonparametric method does not require a normal distribution and operates by ranking the data rather than using the measured values directly. The resulting test statistic is compared against the critical value from the chi-squared distribution, determined by the degrees of freedom.
Missing data were handled by specifying the exact number of participants who provided values and calculating relative frequencies based on this precise sample size. Analyses were conducted using IBM SPSS Statistics (version 28.0.1.0 for Windows).
The qualitative interviews were audio-recorded and then transcribed. Interpretative Phenomenological Analysis (IPA) [16] was used to analyse the interviews, aiming to capture subjective meanings and individual attributions of meaning [17]. Coding was inductive for the t1 interviews and deductive for the t3 interviews. One researcher performed the coding, but the process and findings were discussed within the group. The analysis was conducted using MAXQDA Analytics Pro 2022 (release 22.01). Interviewees were not involved in the data analysis of the qualitative data.
This research project was approved by the Cantonal Ethics Committee, Zurich, on 5 October 2021 (BASEC 2021-01589). All study procedures adhered to the Declaration of Helsinki guidelines.
Some participants did not provide a response at all time points. Fifty patients answered the questionnaires at t1, 46 at t2 and 43 at t3. All questionnaires at each time point were answered by 35 patients and these were included in the longitudinal analysis (see figure S1 in the appendix). None of the interviewees was lost to follow-up.
The study included 66.0% women and 34.0% men. Their sociodemographic and work-related characteristics are detailed in table 2. The median age was 47 years (IQR: 36–55) and the median Body Mass Index was 23.5 (IQR: 21.1–26.7). Most participants had either higher vocational education (32.0%) or higher education (32.0%), and 88.0% reported being employed or self-employed.
Table 2Sample characteristics recorded at t1 (n = 50).
| n (%), median (IQR) | ||
| Male | 17 (34.0%) | |
| Female | 33 (66.0%) | |
| Age | 50 (100%), 47 (36–55) | |
| BMI (kg/m2) | 50 (100%), 23.5 (21.1–26.7) | |
| Highest completed education | Compulsory school | 1 (2.0%) |
| Basic vocational education | 10 (20.0%) | |
| General education (e.g. grammar school) | 7 (14.0%) | |
| Higher vocational education | 16 (32.0%) | |
| Higher education (e.g. Bachelor, Master, Doctorate) | 16 (32.0%) | |
| Missing | 0 | |
| Employment status | (Self-)Employed | 44 (88.0%) |
| Employment level (%) | 80.0 (58–100) | |
| Unemployed, retired | 5 (10%) | |
| Missing | 1 (2%) | |
At t1, 12.0% of participants reported being in inpatient treatment for their acute COVID-19 illness for a median of 13 days (IQR: 10–35), with one patient in intensive care for 19 days. Regarding comorbidities, 66.0% reported having no other diseases, while 34.0% had one or more concomitant diseases, with asthma being the most frequently mentioned. During the study, 14.0% reported a new COVID-19 infection, and 28.0% had other diseases (infections 10.0%, other lung disease 6.0%, musculoskeletal pain 4.0%, psychiatric or neurological problems 4.0%, eye disease 2.0%, sleep disorder 2.0%). The interviewed participants did not differ from the total sample.
The median interval between first COVID-19 symptoms and clinic attendance was 201 days (IQR: 135–357), and 200 days (IQR: 122–372) from a positive COVID-19 test (table 3). Most patients (82.0%) attended the clinic on their family doctor’s advice. Other routes included self-referral (8.0%), referral from other Cantonal Hospital Winterthur wards (4.0%) and support group counselling (2.0%).
Table 3Circumstances for attending the multidisciplinary post-COVID outpatient clinic at t1 (n = 50).
| n (%), median (IQR) | ||
| Timing | Days since first symptoms of COVID-19 infection | 30 (60.0%), 201 (135–357) |
| Days since positive COVID-19 test | 32 (64.0%), 200 (122–372) | |
| Awareness of the multidisciplinary post-COVID outpatient clinic through: | General practitioner | 41 (82.0%) |
| Specialist doctor | 8 (16.0%) | |
| Recommendation from family, friends, acquaintances | 6 (12.0%) | |
| Public media (e.g. newspaper, television) | 5 (10.0%) | |
| Altea network* | 3 (6.0%) | |
| Social media (e.g. Facebook, Instagram) | 2 (4.0%) | |
| Physiotherapist | 1 (2.0%) | |
| Other | 7 (14.0%) | |
| Missing | 0 | |
| Reasons for attending the multidisciplinary post-COVID outpatient clinic | Tiredness, exhaustion, fatigue | 47 (94.0%) |
| Reduced physical capacity | 41 (82.0%) | |
| Pain | 16 (32.0%) | |
| Breathing difficulties | 14 (28.0%) | |
| Concern that lungs have been damaged by COVID-19 | 13 (26.0%) | |
| Search for advice/information | 13 (26.0%) | |
| Medical check | 11 (22.0%) | |
| Other | 12 (24.0%) | |
| Missing | 0 | |
* Swiss network for patients with COVID-19 and their healthcare professionals.
The most common reasons for consulting a doctor were persistent tiredness, exhaustion or fatigue (94.0%) and persistent reduced physical capacity (82.0%). Other reasons included physical complaints (12.0%), cognitive limitations (8.0%) and altered sense of smell/taste (4.0%).
In qualitative interviews, most patients did not express high expectations for treatment, given the novelty and unexplored nature of post-COVID symptomatology. “Covid is still new. I don’t think anyone can help me because science doesn’t have this knowledge.” (TN35_1). However, they clearly expressed a need to understand their symptoms or to have confirmation that they were affected and not faking it, especially regarding fatigue and reduced physical capacity. “I simply wish that when I come here, I would feel better at some point. Physically and mentally.” (TN102_1). Some patients also expressed a desire to regain their pre-illness health and sought support in managing the disease to strengthen their self-efficacy. “It was important for me to have guidance on how to proceed. What I can do to minimise or eliminate the symptoms.” (TN72_1).
At t1, half of the patients were unable to work, with nine (18.0%) completely unable to work. At t2, 43.2% (19/44) were still unable to work; by t3, this proportion had fallen to 34.3% (12/35). These changes were not statistically significant (p = 0.150, appendix table S1).
Qualitative interviews revealed a lack of understanding and support from their environment regarding post-COVID complaints, causing significant burden: “Many saying ‘Yes, I am also tired’ showing a lack of understanding, (…) my wife saying ‘Yes, but … you can't see anything.’, this is difficult for me.” (TN45_2); “At work, (…) it was never recognised. Even people who collapsed. It was always blamed as (…) burnout (…). And that disappoints me.” (TN72_2).
Table 4 shows the prevalence of symptoms at the three survey points. Tiredness, exhaustion and fatigue were the most reported symptoms. Their prevalence remained high over time: 94.0% (47/50) at t1, 88.6% (39/44) at t2 and 88.6% (31/35) at t3 (p = 0.819). In contrast, significantly fewer people reported reduced physical capacity over time (65.7% or 23/35 at t3) compared to the time of consultation (82.0% or 41/50; p = 0.023).
Table 4Symptoms.
| t1 (n = 50) | t2 (n = 44) | t3 (n = 35) | Test statistics | ||
| Tiredness, exhaustion, fatigue | n (%) | 47 (94.0%) | 39 (88.6%) | 31 (88.6%) | Cochran-Q(2) = 0.4; p = 0.819 |
| VAS mean [SD] | 7.0 [1.8] | 6.7 [2.6] | 5.8 [2.6] | χ2 (2) = 10.086; p = 0.006 | |
| Reduced physical capacity | n (%) | 41 (82.0%) | 36 (81.8%) | 23 (65.7%) | Cochran-Q(2) = 7.5; p = 0.023 |
| VAS mean [SD] | 6.9 [1.9] | 5.7 [3.0] | 4.8 [2.9] | χ2 (2) = 11.5; p = 0.003 | |
| Pain | n (%) | 16 (32.0%) | 18 (40.9%) | 9 (25.7%) | Cochran-Q(2) = 2.9; p = 0.236 |
| VAS mean [SD] | 7.5 [1.8] | 2.7 [2.6] | 2.1 [2.6] | χ2 (2) = 11.6;p = 0.003 | |
| Breathing difficulties | n (%) | 14 (28.0%) | 14 (31.8%) | 9 (25.7%) | Cochran-Q(2) = 1.3; p = 0.513 |
| VAS mean [SD] | 6.9 [2.0] | 1.9 [2.5] | 1.5 [1.9] | χ2 (2) = 10.7; p = 0.005 | |
| Concern, damaged lungs | n (%) | 13 (26.0%) | 9 (20.5%) | 10 (28.6%) | Cochran-Q(2) = 0.4; p = 0.819 |
| VAS mean [SD] | 6.3 [2.6] | 1.9 [2.7] | 2.2[2.9] | χ2 (2) = 8.6; p = 0.013 | |
| Other symptoms | n (%) | 12 (24.0%) | 27 (61.4%) | 14 (40.0%) | Cochran-Q(2) = 7.4; p = 0.025 |
| VAS mean [SD] | 7.0 [1.7] | 5.5[2.6] | 3.6 [3.0] | χ2 (2) = 1.5; p = 0.465 | |
| Cognitive impairment* | n (%) | 3 (6.0%) | 12 (27.3%) | 10 (28.6%) | Cochran-Q(2) = 5.3; p = 0.069 |
| VAS mean [SD] | 8.3 [1.5] | 5.6[2.8] | 5.1 [2.3] | χ2 (2) = n.a.** |
VAS: Visual Analogue Scale
* Cognitive impairment was not specified as a category in the questionnaire but was often given as a burdensome symptom in the free-text field.
** Too few observations
Patients assessed the intensity of their symptoms using a Visual Analogue Scale (VAS). Over time, there were statistically significant changes in the intensity of tiredness, exhaustion, fatigue, reduced physical capacity, pain, breathing difficulties and concern about lung damage.
Compared to before the consultation, most participants rated their health as “about the same” at t1 (76.2% or 32/42) and at t2 (54.5% or 24/44). At t3, more patients rated their condition as “much better” (40.0% or 14/35) or “somewhat better” (34.3% or 12/35) (figure 1).
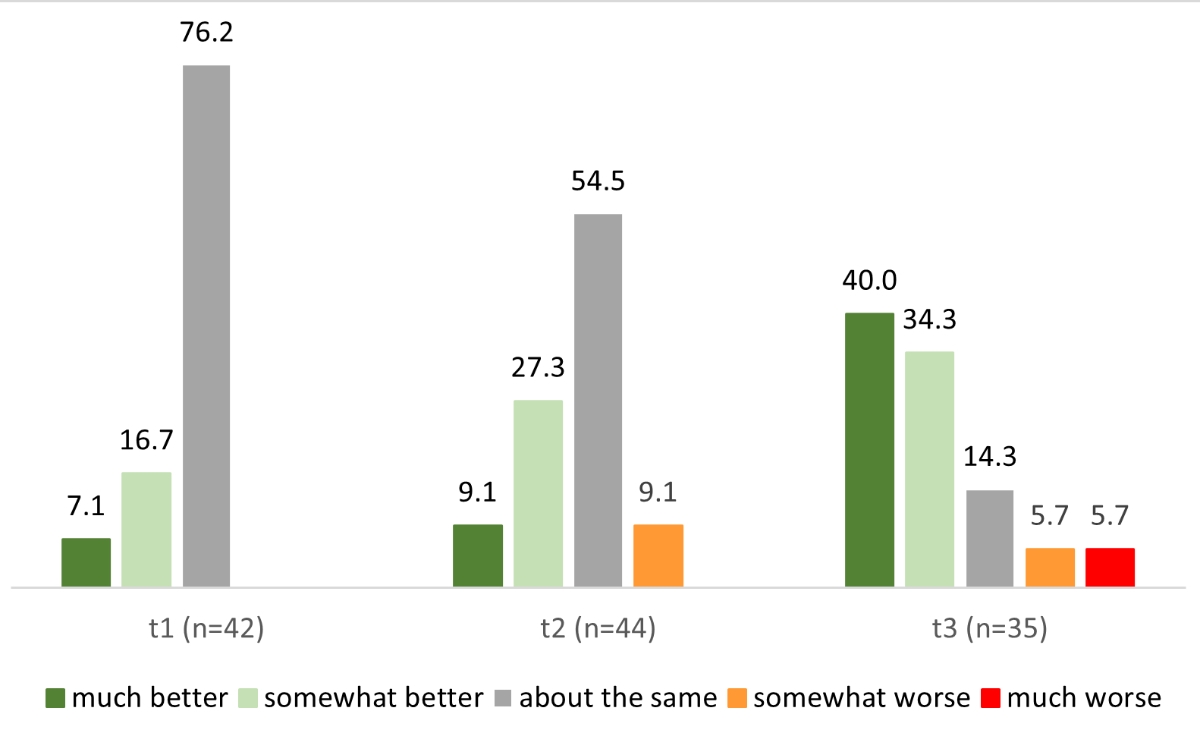
Figure 1Current state of health compared to before consultation. Numbers represent percentages.
The changes described in the free-text fields of the questionnaire after attending the multidisciplinary post-COVID outpatient clinic are summarised in categories (appendix table S2). The most frequent mentions at both t2 (34.1%) and t3 (42.9%) time points were related to improved physical capacity (n = 15/44 and 15/35 respectively). At time t2, patients also described negative changes, such as increased pain (9.1% or 4/44) or persistent fatigue (11.4% or 5/44).
In the qualitative interviews, patients reported very different strategies for dealing with the complaints. For example, the following were useful strategies mentioned: communication with other patients, psychological support as early as possible, or reduction of stress at work and at home. “I still go to psychotherapy, once a week, which helps me a lot.” (TN49_4); “I try to listen to by body.” (TN59_1).
Four standardised questionnaires showed statistically significant changes over time: HADS Anxiety (p = 0.015), HADS Depression (p = 0.002), CFS (p = 0.048) and PCFS (p <0.001) (figure 2). The PC-VAS showed significant improvement on the subscale “health today” (p = 0.023). At t3, 77.1% (27/35) had noticeable fatigue symptoms (CFS ≥4), compared to 96.0% (48/50) at t1. The degree of restriction due to COVID symptoms, represented by the PCFS, decreased from a mean of 2.6 ± 0.7 to 1.7 ± 1.0 (p <0.05, appendix table S3).
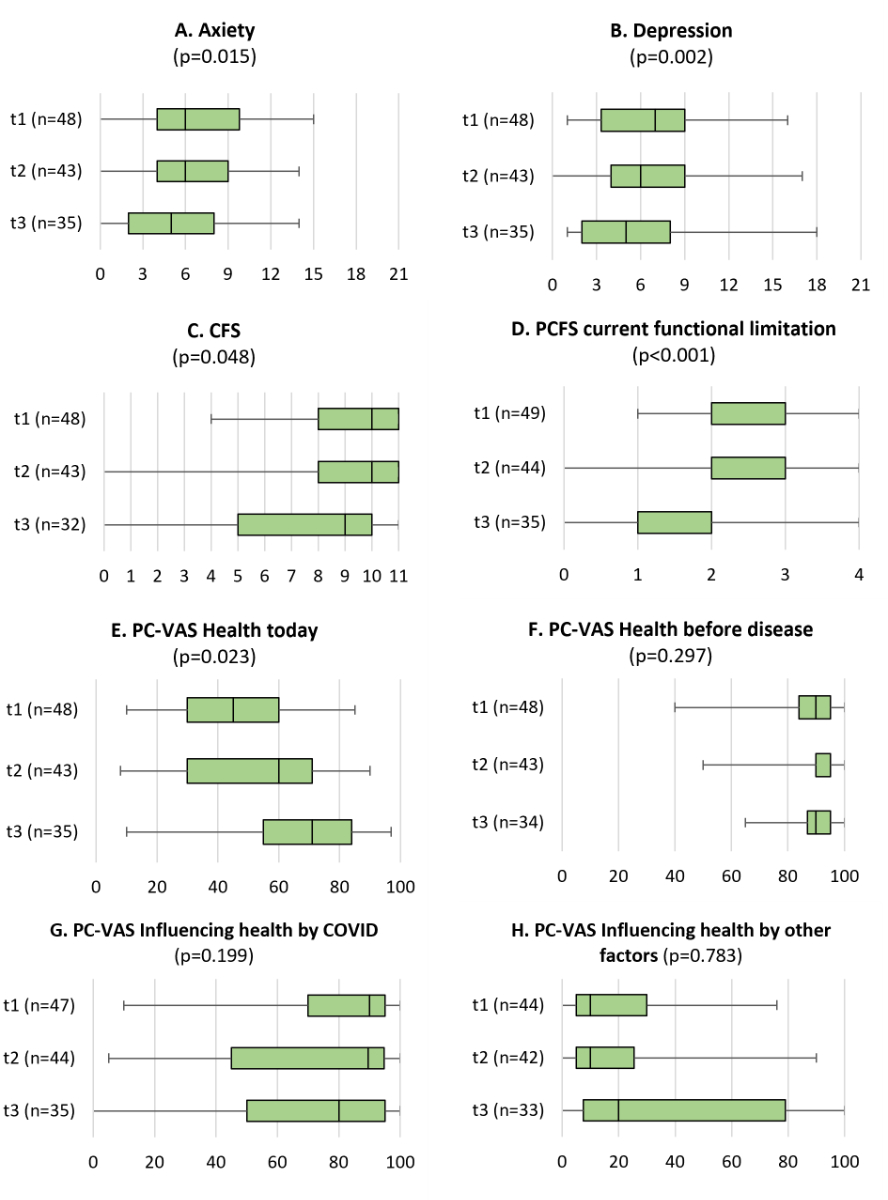
Figure 2Standardised questionnaires. The line dividing the box in two represents the median value. Boxes represent interquartile ranges, the whiskers encompass each 25% of the lower and upper values of the distribution. CFS: Chalder Fatigue Scale; HADS: Hospital Anxiety and Depression Scale; n.s.: (statistically) non-significant; PCFS: post-COVID Functional Status; PC-VAS: Post-COVID Visual Analogue Scale.
At t1, 82.0% (41/50) reported starting post-COVID-specific treatments. At t2, referrals were mainly for psychological counselling (43.2% or 19/44) and physiotherapy (29.5% or 13/44). Further diagnostic clarifications were reported at t2 (47.7% or 21/44) and t3 (37.1% or 13/35), most frequently for pulmonary (n = 9), cardiological (n = 7) and neurological (n = 5) examinations. At t2, most treatments involved drug therapy (72.7% or 32/44) or physical activity (59.1% or 26/44). Some participants (n = 13) reported using complementary therapies like acupuncture or osteopathy.
In qualitative interviews, patients valued the confirmation of their post-COVID diagnosis but found it difficult to accept when no pathological findings were raised.
“… can be anything and it can be nothing (…) I find that a bit unsatisfactory for me and certainly also for the doctors treating me. All examinations are fine, great, and I still feel the way I feel. From that point of view, yes, it’s still difficult to understand” (TN72_ 1); “…that you’re not somehow strange or that it’s your imagination (…). It also helps to have a diagnosis” (TN68_2).
Patients emphasised the importance of understanding their illness and feeling taken seriously. Recognition of symptoms by medical staff was beneficial, while lack of recognition caused frustration. Some patients wanted coordinated care with outside professionals to reduce travel burden. Better communication about post-COVID illness among professionals and patients was also noted. The potential benefit of a self-help group for networking among affected individuals was mentioned.
Of the included patients, 91.5% (43/47) fully or rather agreed that the multidisciplinary post-COVID outpatient clinic met their expectations. The majority of patients (95.9% or 47/49) confirmed or rather confirmed that they felt well looked after at all times and that they would recommend the clinic to others (appendix figure S2).
Regarding specific aspects of the clinic, the majority of patients indicated high satisfaction with their ability to co-decide the further course of action, with 59.2% (29/49) being very satisfied and 30.6% (15/49) rather satisfied. Similarly, 58.0% (29/50) were very satisfied and 38.0% (19/50) were rather satisfied with the information they received about the examination outcomes (figure 3).
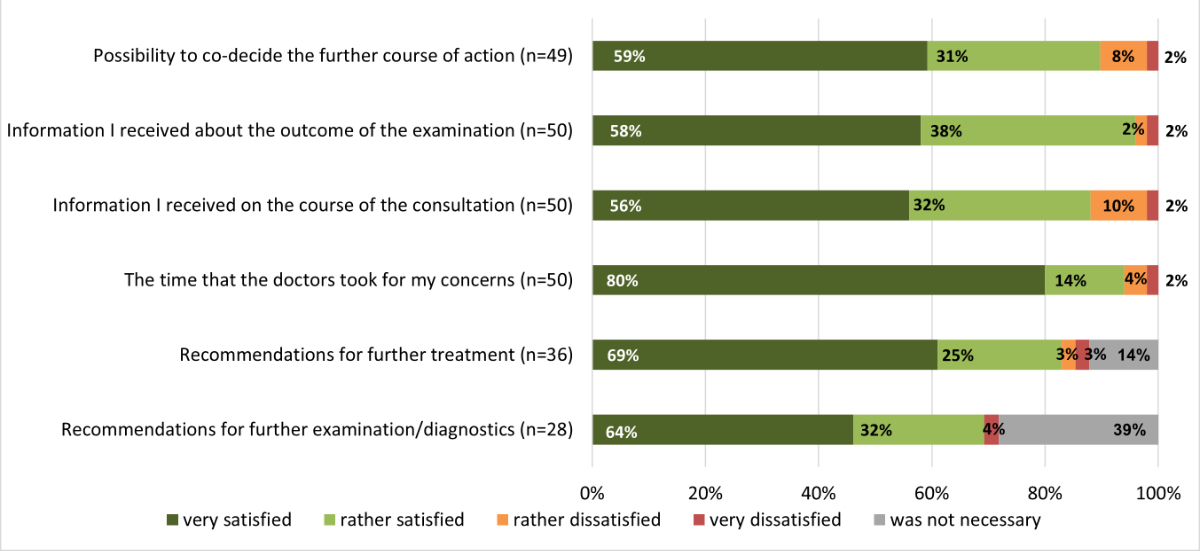
Figure 3Satisfaction with aspects of the multidisciplinary post-COVID outpatient clinic.
In the free-text responses, patients highlighted several helpful aspects of their consultation: attention from doctors and other professionals; being taken seriously; understanding; inclusion; not being alone (36.0% or 18/50); being given a perspective for the future and being able to take action (22.0% or 11/50); referral for concrete therapies (16.0% or 8/50); assessment of the situation based on detailed diagnosis and feedback on symptoms (14% or 7/50); and knowing more about post-COVID and classification of the disease (10.0% or 5/50).
Participants expressed dissatisfaction with certain aspects: specific therapy options or recommendations for symptoms seem limited; there is no new information or clinical research (10.0% or 5/50); waiting times are too long and postponements of examinations (10.0% or 5/50); and results were not sufficiently or individually discussed (4.0% or 2/50).
The most frequently mentioned suggestion for improvement was an increase in the number of consultation hours.
In the qualitative interviews, waiting times were perceived differently. Some patients found the waiting time acceptable given their long-term symptoms, while others found it stressful, especially with acute symptoms. Patients also expressed the need for faster contact with experts and better scheduling of diagnostic and therapeutic appointments.
In retrospect, the average general satisfaction with the multidisciplinary post-COVID outpatient clinic was also high in surveys t1 and t2 (figure 4).
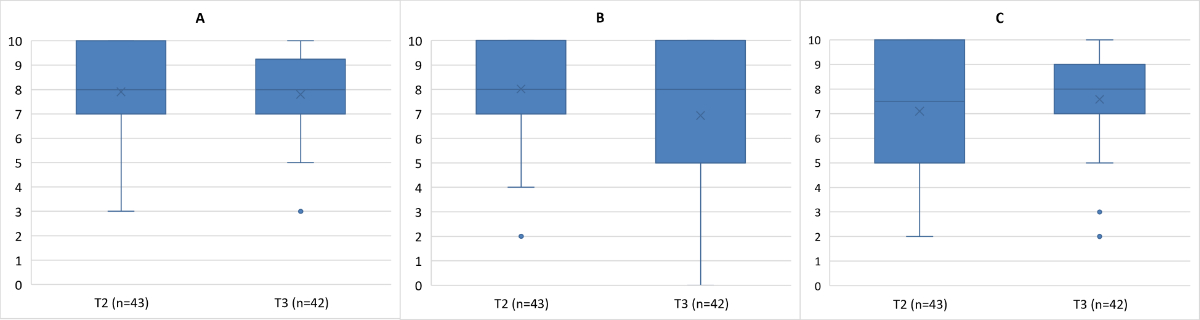
Figure 4Retrospective satisfaction with the multidisciplinary post-COVID outpatient clinic on a scale from 0 (totally dissatisfied) to 10 (totally satisfied) regarding: (A) general; (B) initiated treatments; and (C) diagnostic procedures. The line dividing the box in two represents the median value, X represent means. Boxes represent interquartile ranges, the whiskers encompass each 25% of the lower and upper values of the distribution, dots mark outliers.
The aim of this study was to evaluate the multidisciplinary post-COVID outpatient clinic for individuals affected by post-COVID syndrome. This clinic, available at the Pneumology Department of the Cantonal Hospital Winterthur since 2021, emphasises the patient perspective during data collection. The study employed a combined methodological approach, comprising quantitative questionnaire surveys at three time points and qualitative, semi-structured individual interviews at two time points. The main finding is that patients benefited most from having their complaints taken seriously through attentive listening and the multidisciplinary treatment approach.
The target size of the study was achieved in the first survey. However, not all participants responded to the subsequent surveys, resulting in 35 complete datasets for evaluation. In May 2023, a study from the USA by Bailey et al. was published with a similar evaluation, documenting 1802 patients [18]. A comparison of the two samples shows similarity in terms of sex (proportion of females: 64.6% in Bailey et al. vs 66.0% in the Cantonal Hospital Winterthur), age (47.0 vs 43.7 years) and time since first symptoms (8 vs 7 months). Differences were exhibited in the BMI (28.3 vs 24.4) and the number of participants being hospitalised during the acute phase (19.4% vs 12.0%). Compared to the overall sample in our study, males were slightly overrepresented in the subsample for the qualitative interviews (34% vs 50%). It cannot be assumed that this caused a bias in the qualitative findings, since they were not based on statistical power and were of a representative nature, but on “the sufficient representation and maximum variation of characteristics that may have an influence on the topic of interest”. A special feature of the study sample is the low proportion of participants who reported changes in taste or olfactory function.
Participants reported various subjective health-related and/or functional limitations. Standardised questionnaire indicators showed stable values between t1 and t2 and noticeable recovery between t2 and t3, likely due to the longer second intervening period. The subjectively perceived physical capacity showed the most improvement. It is not possible to make a statement about the reasons for this because the improvements could have been a natural course of recovery or due to the targeted therapy measures. Despite observed recoveries, COVID-19’s influence on health remained stable over the entire observation period. The level of assessed health was clearly limited.
In most cases, the referral to the multidisciplinary post-COVID outpatient clinic was made by the family doctor. However, this referral channel was further augmented, e.g. with targeted information to GPs and further training events. The need for only a few further diagnostic measures indicates that the referrals were appropriate.
General satisfaction with the post-COVID outpatient clinic was high, with only a few patients being less satisfied. Patients appreciated having opportunities to co-decide their treatment course and receiving consultation information. The high need for information was evident in interviews, with many patients seeking professional guidance for coping strategies.
It can be assumed that expectations were relatively high due to the long course of the disease and the relatively little or unclear information available at the same time. The interviews were inconclusive in this respect. On the one hand, patients expected to regain the state of health they had had before the disease, while, on the other hand, some patients displayed low expectations regarding successful therapy. There was understanding expressed for this subject because of the existence of little research in this area. A great, frequently mentioned need was to be taken seriously. A few patients also stated that there was potential to improve the consultation hours. These mainly concerned organisational issues, such as shorter waiting times for an appointment. The focus of criticism on organisational topics can also be interpreted as a further indication of the high level of satisfaction with the content of the multidisciplinary post-COVID outpatient clinic. Or, to put it another way, patient satisfaction can be best improved by investing time in organisational issues rather than in costly additional diagnostic examinations or other content.
The recognition of the illness and its symptoms by doctors was perceived as very comforting and with full confidence. In the interviews, many emphasised the importance of early access to consultations and psychotherapy to increase self-management. Improvement proposals, such as the promotion of knowledge transfer to external doctors (general practitioners) and other healthcare professionals (e.g. psychotherapists, physiotherapists), as well as the opportunity to communicate with other affected individuals, were suggested multiple times. This should certainly be seen in the context that new knowledge on COVID was developing very dynamically.
The majority of the quantitative survey results were confirmed by the interviews. Very satisfied and very dissatisfied people were interviewed. Even though the survey showed that the general satisfaction seemed to be quite high, some people reported a more nuanced picture in the interview, of unfulfilled or only very low expectations. Qualitative data saturation might not be reached; however, the spectrum of data was broad. Thus, the mixed-methods approach was beneficial in complementing the questionnaire data with the interviews and in obtaining more in-depth information [11].
Both the questionnaire and the interview guide were developed by the research team based on the available literature at the time of planning and in consultation with the medical staff of the Cantonal Hospital Winterthur.
The questionnaire asked for the patients’ perspectives on the course of their treatment, the services offered by the clinic and on their recovery status. The combination of closed and open questions not only allowed a comparison of the statements between people and over time, but also offered the opportunity to introduce further topics and concerns on the part of the patients. The questionnaires at the three time points allowed for a direct comparison between the three data collection points for many constructs, but not for all.
The interview guide was tested in a mock interview. All interviews at t1 were conducted by one researcher and those at t2 by a different researcher. All participants could be contacted again for an interview at time t3.
For various reasons, there were participants lost to follow-up, resulting in complete datasets being available for only 35 participants. More datasets are available for the individual time points. The loss of observations requires examination with regard to the descriptive evaluations, because such losses are especially critical in the event that they bias conclusive evaluations [19].
This study focused on one specific centre. Accordingly, the results cannot be generalised in a scientific sense. Nevertheless, the results can be helpful for comparing the design of other programmes. It should also be noted that it is not sufficient to judge the quality of a medical facility solely based on satisfaction data collected from the patient’s perspective. Although this is an essential element, other objective criteria should also be taken into account to determine the quality of care [20].
The study data show that patients with post-COVID syndrome felt best supported through attentive interprofessional coaching. Early access to consultation and psychotherapy was crucial for enhancing self-management. The promotion of knowledge transfer to external doctors (general practitioners) and healthcare professionals (e.g. psychotherapists, physiotherapists), as well as the opportunity to communicate with other patients, were also suggested as necessary themes. These insights are contextualised by the rapidly evolving knowledge about COVID-19 at the time of data collection.
Upon reasonable request, the data from this study will be shared in anonymised form.
The authors would like to thank Sandra Egli-Künzle (SEK), Rachel Bärtsch and Leah Reicherzer for their help with data collection and analysis, Christa Wachter for administrative support and Michelle Haas for assistance with the REDCap survey.
This study was financially supported by the Lung Association Zurich (Verein Lunge Zürich) and the Cantonal Hospital Winterthur (KSW).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Coronavirus disease (COVID-19) – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
2. Products - COVID-19 | Topic | NICE. NICE; 2023. https://www.nice.org.uk/guidance/conditions-and-diseases/respiratory-conditions/covid19/products?ProductType = Guidance&Status = Published
3. COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (UK); 2020. (National Institute for Health and Care Excellence: Clinical Guidelines). http://www.ncbi.nlm.nih.gov/books/NBK567261/
4. Emergency use ICD codes for COVID-19 disease outbreak. https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak
5. Hanson SW, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, et al. A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv. 2022 May 27;2022.05.26.22275532.
6. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021 Apr;27(4):601–15. doi: https://doi.org/10.1038/s41591-021-01283-z
7. Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. Madeddu G, editor. PLoS ONE. 2020 Dec 11;15(12):e0243882.
8. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. Infectious Diseases (except HIV/AIDS); 2021 Jan. http://medrxiv.org/lookup/doi/10.1101/2021.01.27.21250617
9. Hossain MM, Das J, Rahman F, Nesa F, Hossain P, Islam AM, et al. Living with “long COVID”: A systematic review and meta-synthesis of qualitative evidence. PLoS One. 2023 Feb;18(2):e0281884. doi: https://doi.org/10.1371/journal.pone.0281884
10. Macpherson K, Cooper K, Harbour J, Mahal D, Miller C, Nairn M. Experiences of living with long COVID and of accessing healthcare services: a qualitative systematic review. BMJ Open. 2022 Jan;12(1):e050979. doi: https://doi.org/10.1136/bmjopen-2021-050979
11. Creswell JW, Clark VL. Designing and conducting mixed methods research. Thousand Oaks, CA, US: Sage Publications, Inc; 2007. xviii, 275 p.
12. Klok FA, Boon GJ, Barco S, Endres M, Geelhoed JJ, Knauss S, et al. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020 Jul;56(1):2001494. doi: https://doi.org/10.1183/13993003.01494-2020
13. Stern AF. The hospital anxiety and depression scale. Occup Med (Lond). 2014 Jul;64(5):393–4. doi: https://doi.org/10.1093/occmed/kqu024
14. Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–53. doi: https://doi.org/10.1016/0022-3999(93)90081-P
15. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al.; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019 Jul;95:103208. doi: https://doi.org/10.1016/j.jbi.2019.103208
16. Smith JA, Osborn M. Interpretative phenomenological analysis as a useful methodology for research on the lived experience of pain. Br J Pain. 2015 Feb;9(1):41–2. doi: https://doi.org/10.1177/2049463714541642
17. Flick U. Qualitative Sozialforschung: eine Einführung. 10. Auflage, Originalausgabe. Reinbek bei Hamburg: rowohlts enzyklopädie im Rowohlt Taschenbuch Verlag; 2021. 623 p. (Rororo Rowohlts Enzyklopädie).
18. Bailey J, Lavelle B, Miller J, Jimenez M, Lim PH, Orban ZS, et al.; Northwestern Medicine Comprehensive COVID Center Investigators. Multidisciplinary Center Care for Long COVID Syndrome-A Retrospective Cohort Study. Am J Med. 2023 May;(May):S0002934323003285. doi: https://doi.org/10.1016/j.amjmed.2023.05.002
19. Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol. 2004;19(8):751–60. doi: https://doi.org/10.1023/B:EJEP.0000036568.02655.f8
20. Berger B, Lenz M, Mühlhauser I. Patient zufrieden, Arzt gut? Inwiefern ist Patientenzufriedenheit ein Indikator für die Qualität der hausärztlichen Versorgung? Eine systematische Ubersichtsarbelt. Z Evid Fortbild Qual Gesundhwes. 2008;102(5):299–306. doi: https://doi.org/10.1016/j.zgesun.2008.01.004
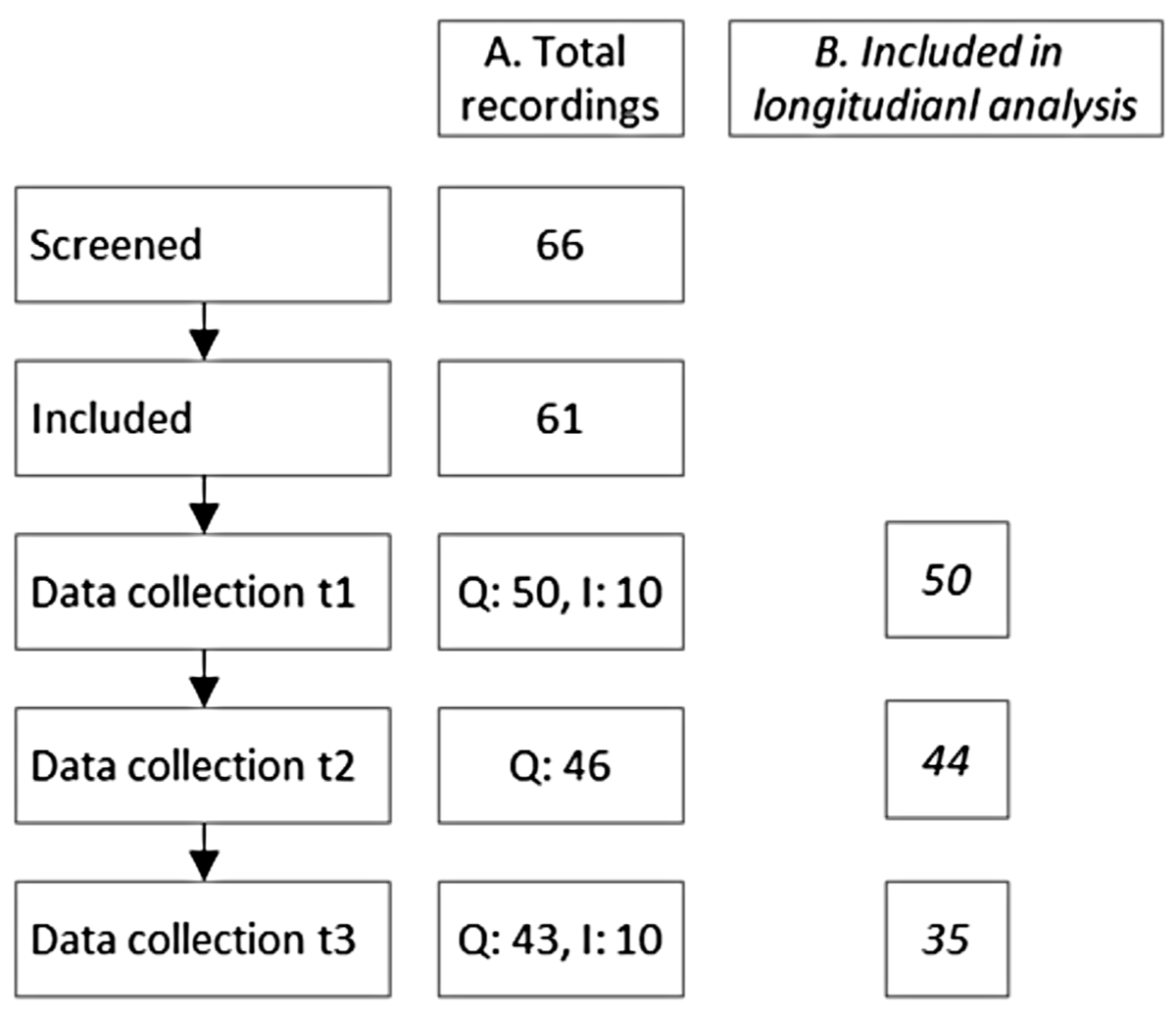
Figure S1Flowchart of the recruitment. The numbers correspond to (A) all responses received at the respective time points and (B) all participants for whom data from previous time points are available and who could be evaluated longitudinally. I: interviews; Q: Questionnaire survey.
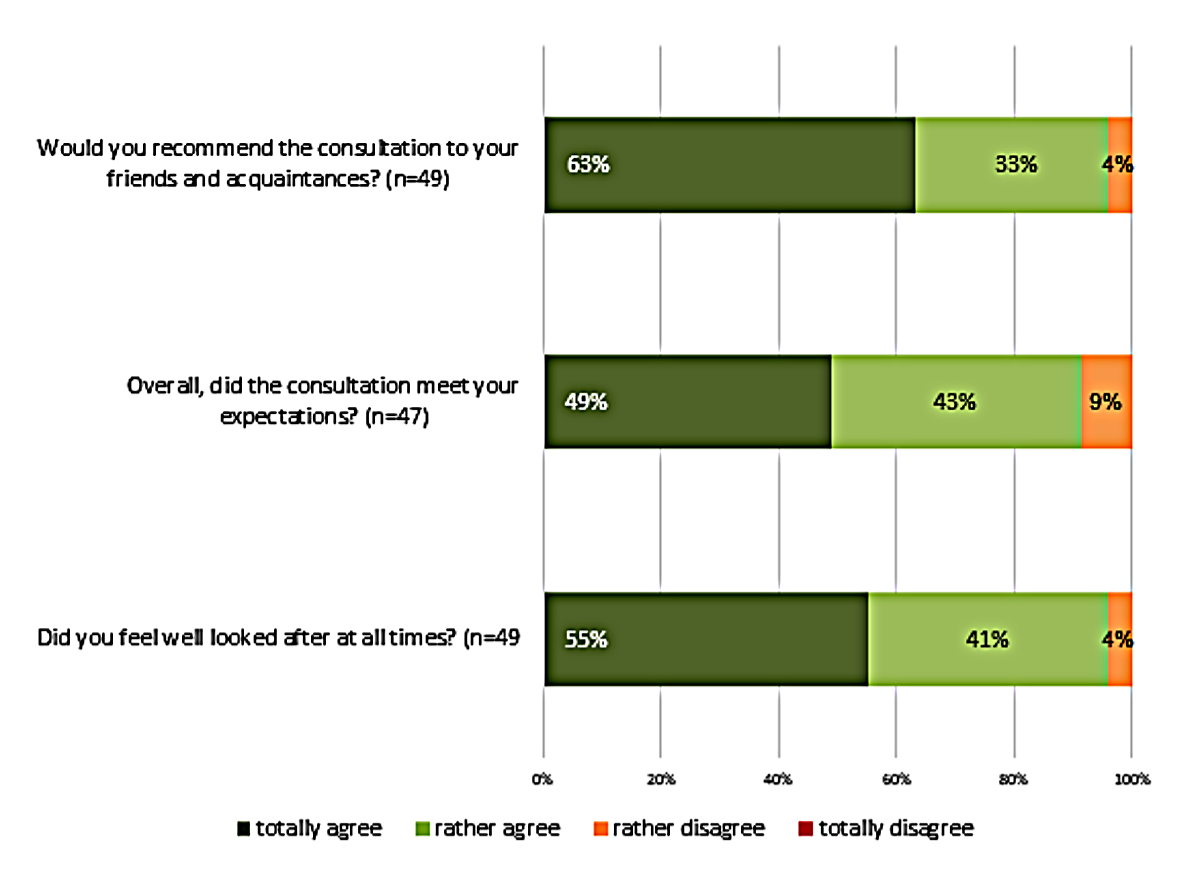
Figure S2General satisfaction with the post-COVID consultation at t1.
Table S1Inability to work over the whole observation period.
| t1 (n = 50) | t2 (n = 44) | t3 (n = 35) | Test statistics | ||
| Inability to work | n (%) | 25 (50.0%) | 19 (43.2%) | 12 (34.3%) | Cochran-Q (2) = 3.8; p = 0.150 |
| 100% unable, n (%) | 9 (18.0%) | 0 (0%) | 11 (31.4%) | ||
| Extent of inability to work | n (%), mean [SD] | 22 (44.0%), 68.0 [30.1] | 5 (11.4%), 30.0 [12.2] | 11 (31.4%), 66.4 [29.8] | n.a.* |
Table S2Changes after attending the consultation described in the free-text fields of the questionnaire.
| t2 (n = 44) | t3 (n = 35) | |
| Improvements | Physical capacity (n = 15) | Physical capacity (n = 15). Improved mental state (n = 1) |
| Breathing (n = 4) | Breathing(n = 6) | |
| Altered sensory perceptions (n = 2) | Decreased pain (n = 3) | |
| Better emotional support (n = 1) | Improved cognitive performance (n = 3) | |
| Improved mental state (n = 1) | ||
| Deteriorations | Persistent fatigue (n = 5) | Decreased physical capacity (n = 2) |
| Increased pain (n = 4) | Weakened immune system (n = 1) | |
| Cognitive impairment (n = 3) | ||
| Psychological issues (n = 2) | ||
| Increased coughing (n = 1) |
Table S3Standardised questionnaires.
| t1 (n = 50) | t2 (n = 44) | t3 (n = 35) | Test statistics | |||
| HADS | Anxiety (0–21): | mean [SD] | 6.6 [3.7] | 6.2 [3.4] | 5.3 [3.7] | χ2 (2) = 8.3; p = 0.015 |
| min, Q0.25, Q0.5, Q0.75, max | 0, 4.0, 6.0, 9.8, 15 | 0, 4.0, 6.0, 9.0, 14 | 0, 2.0, 5.0, 8.0, 14 | |||
| unobtrusive(0–7): n (%) | 29 (58.0%) | 28 (63.6%) | 26 (74.3%) | |||
| suspect (8–10): n (%) | 11 (22.0%) | 12 (27.3%) | 6 (17.1%) | |||
| conspicuous (≥11): n (%) | 8 (16.0%) | 3 (6.8%) | 3 (8.6%) | |||
| Depression (0–21): | mean [SD] | 6.8 [3.8] | 6.8 [4.0] | 5.5 [4.0] | χ2 (2) = 12.6; p = 0.002 | |
| min, Q0.25, Q0.5, Q0.75, max | 1, 3.3, 7.0, 9.0, 16 | 0, 4.0, 6.0, 9.0, 17 | 1, 2.0, 5.0, 8.0, 18 | |||
| unobtrusive (0–7):n (%) | 27 (54.0%) | 26 (59.1%) | 24 (68.6%) | |||
| suspect (8–10): n (%) | 14 (28.0%) | 9 (20.5%) | 7 (20.0%) | |||
| conspicuous (≥11): n(%) | 7 (14.0%) | 8 (18.2%) | 4 (11.4%) | |||
| CFS (0–11) | Bimodal score | mean [SD] | 9.2 [1.9] | 8.6 [2.8] | 7.4 [3.5] | χ2 (2) = 6.1; p = 0.048 |
| min, Q0.25, Q0.5, Q0.75, max | 4, 8.0, 10.0, 11.0, 11 | 0, 8.0, 10.0, 11.0, 11 | 0, 5.0, 9.0, 10.0, 11 | |||
| unobtrusive (<4): n (%) | 0 (0.0%) | 3 (6.8%) | 5 (14.3%) | |||
| conspicuous (≥4): n (%) | 48 (96.0%) | 40 (90.9%) | 27 (77.1%) | |||
| PCFS (0–4) | Current functional limitation | mean [SD] | 2.6 [0.7] | 2.1 [0.9] | 1.7 [1.0] | χ2 (2) = 21.8; p <0.001 |
| min, Q0.25, Q0.5, Q0.75, max | 1, 2.0, 3.0, 3.0, 4 | 0, 2.0, 2.0, 3.0, 4 | 0, 1.0, 2.0, 2.0, 4 | |||
| Functional limitation before disease | mean [SD] | 0.7 [1.0] | 0.7 [0.9] | 0.5 [0.8] | χ2 (2) = 3.7; p = 0.156 | |
| min, Q0.25, Q0.5, Q0.75, max | 0, 0.0, 0.0, 1.0, 4 | 0, 0.0, 0.0, 1.0, 3 | 0, 0.0, 0.0, 1.0, 3 | |||
| PC-VAS (0–100) | Health today | mean [SD] | 55.8 [18.3] | 54.1 [22.8] | 66.7 [22.3] | χ2 (2) = 7.5; p = 0.023 |
| min, Q0.25, Q0.5, Q0.75, max | 20, 40.3, 55.0, 70.0, 95 | 8, 30.0, 60.0, 71.0, 90 | 10, 55.0, 71.0, 84.0, 97 | |||
| Healthbefore disease | mean [SD] | 87.1 [10.8] | 89.0 [10.5] | 90.0 [8.6] | χ2 (2) = 2.4; p = 0.297 | |
| min, Q0.25, Q0.5, Q0.75, max | 40, 84.3, 90.0, 94.5, 100 | 50, 90.0, 90.0, 95.0, 100 | 65, 86.8, 90.0, 95.0, 100 | |||
| Influencing health by COVID | mean[SD] | 78.5 [24.0] | 71.7 [30.6] | 68.3 [32.7] | χ2 (2) = 3.2; p = 0.199 | |
| min, Q0.25, Q0.5, Q0.75, max | 10, 70, 90.0, 95.0, 100 | 5, 45.0, 89.5, 94.8, 100 | 0, 50.0, 80.0, 95.0, 100 | |||
| Influencing health by other | mean [SD] | 20.5 [22.0] | 21.6 [25.7] | 36.1 [35.8] | Χ2 (2) = 0.5; p = 0.783 | |
| min, Q0.25, Q0.5, Q0.75, max | 0, 5.0, 10.0, 30.0, 76 | 0, 5.0, 10.0, 25.3, 90 | 0, 7.5, 20.0, 79.0, 100 | |||
CFS: Chalder Fatigue Scale; HADS: Hospital Anxiety and Depression Scale; PCFS: post-COVID Functional Status; PC-VAS: Post-COVID Visual Analogue Scale.