Changes in diagnostic patterns and resource utilisation in Swiss adult ICUs during
the first two COVID-19 waves: an exploratory study
DOI: https://doi.org/https://doi.org/10.57187/s.3589
Marco
Previsdominia*,
Andreas Perrenabc*,
Alessandro Chiesaa,
Mark Kaufmannd,
Hans Parggerd,
Roger Ludwige,
Bernard Ceruttif
a Intensive Care
Unit, Department of Intensive Care Medicine - Ente Ospedaliero Cantonale,
Ospedale Regionale Bellinzona e Valli, Bellinzona, Switzerland
b Faculty of
Medicine, University of Geneva, Geneva, Switzerland
c Faculty of
Biomedical Sciences, Università Svizzera Italiana, Lugano, Switzerland
d Intensive
Care Unit, Department Acute Medicine, University Hospital and University Basel,
Basel, Switzerland
e Department
of Intensive Care Medicine, Inselspital Bern, Bern University Hospital, Bern,
Switzerland
f Unit of
Development and Research in Medical Education, Faculty of Medicine, University
of Geneva, Geneva, Switzerland
* these
authors have contributed equally
Summary
BACKGROUND AND AIM: The coronavirus disease
2019 (COVID-19) outbreak deeply affected intensive care units (ICUs). We aimed
to explore the main changes in the distribution and characteristics of Swiss
ICU patients during the first two COVID-19 waves and to relate these figures
with those of the preceding two years.
METHODS: Using the national ICU registry,
we conducted an exploratory study to assess the number of ICU admissions in Switzerland
and their changes over time, characteristics of the
admissions, the length of stay (LOS) and its trend over time, ICU mortality and
changes in therapeutic nursing workload and hospital resources in 2020 and
compare them with the average figures in 2018 and 2019.
RESULTS: After analysing 242,935 patient
records from all 84 certified Swiss ICUs, we found a significant decrease in
admissions (–9.6%, corresponding to –8005 patients) in 2020 compared to 2018/2019,
with an increase in the proportion of men admitted (61.3% vs 59.6%; p <0.001).
This reduction occurred in all Swiss regions except Ticino. Planned admissions
decreased from 25,020 to 22,021 in 2020 and mainly affected the
neurological/neurosurgical (–14.9%), gastrointestinal (–13.9%) and
cardiovascular (–9.3%) pathologies. Unplanned admissions due to respiratory
diagnoses increased by 1971 (+25.2%), and those of patients with acute
respiratory distress syndrome (ARDS) requiring isolation reached 9973 (+109.9%).
The LOS increased by 20.8% from 2.55 ± 4.92 days (median 1.05) in 2018/2019 to
3.08 ± 5.87 days (median 1.11 days; p <0.001), resulting in an additional 19,753
inpatient days. The nine equivalents of nursing manpower use score (NEMS) of
the first nursing shift (21.6 ± 9.0 vs 20.8 ± 9.4; p <0.001), the total NEMS
per patient (251.0 ± 526.8 vs 198.9 ± 413.8; p <0.01) and mortality (5.7% vs
4.7%; p <0.001) increased in 2020. The number of ICU beds increased from 979
to 1012 (+3.4%), as did the number of beds equipped with mechanical ventilators
(from 773 to 821; +6.2%).
CONCLUSIONS: Based on a comprehensive
national data set, our report describes the profound changes triggered by COVID-19
over one year in Swiss ICUs. We observed an overall decrease in admissions and
a shift in admission types, with fewer planned hospitalisations, suggesting the
loss of approximately 3000 elective interventions. We found a substantial
increase in unplanned admissions due to respiratory diagnoses, a doubling of
ARDS cases requiring isolation, an increase in ICU LOS associated with
substantial nationwide growth in ICU days, an augmented need for
life-sustaining therapies and specific therapeutic resources and worse
outcomes.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has strained
health services worldwide. In selected areas, the rapid increase of COVID-19
patients requiring hospitalisation overburdened acute healthcare systems,
including intensive care units (ICUs), as seen in northern Italy, Madrid and
New York [1–3]. Even in less affected
jurisdictions, the
anticipation of a potential surge in ICU admissions and the diversion of human
resources forced government and healthcare administrators to transiently limit
elective interventional and outpatient activity [4–6]. Interestingly, while some districts
had to expand
ICU capabilities to meet the need for ICU beds, the incidence of some acute
conditions routinely managed in ICUs (e.g. acute coronary syndrome,
intracranial haemorrhage, stroke and major trauma) declined drastically during
the first wave of the pandemic [7–11], leading to an overflow of vacant ICU beds
in other regions. Consequently, regional, national and sometimes international
coordination bodies for intensive care had to be established [1, 12–14].
In a study conducted in Alberta, Canada,
where the ICU bed base was 9.7 ICU beds per 100,000 population and where there
were 2335 COVID-19 cases per 100,000 population in 2020, the number of ICU admissions,
the ICU length of stay (LOS) and mortality decreased during the lockdown
compared to non-lockdown periods [15]. In Japan,
where there were approximately five ICU beds per 100,000 population and 192 COVID-19
cases per 100,000
population in 2020, ICU admissions and organ support procedures declined
substantially, while mortality and LOS remained stable compared to non-pandemic
periods [16].
Switzerland reported its first coronavirus case on 20
February 2020. On 16
March 2020, given the rapid rise of COVID-19 cases, the Swiss
government put the nation into a semi-lockdown until 11 May 2020 to prevent the
collapse of the healthcare system [17, 18]. By
the end of the year, the country had accumulated 452,296 laboratory-confirmed
cases (5232/100,000 inhabitants), 18,630 hospitalisations (215.5/100,000
inhabitants) and 7082 deaths (81.9/100,000 inhabitants) associated with severe acute
respiratory syndrome
coronavirus 2 (SARS-CoV-2) infection [19].
Given the different levels of pressure imposed on
Switzerland by COVID-19, examining how the national critical care system
responded to the pandemic will help future critical care planning. We hypothesised
that ICU admissions, diagnostic patterns, human resource utilisation and
outcomes changed during the first year of the COVID-19 pandemic, albeit with
possible regional variation. Accordingly, we conducted a nationwide registry-based
study to explore the characteristics of all patients admitted to certified ICUs
in Switzerland in 2020 and compare them with a historical cohort from the
previous two years (2018 and 2019).
Materials and methods
Design, setting and population
We performed a retrospective cohort study
involving all patients aged ≥ 16 years admitted to any of the 84 certified
Swiss ICUs. Given the type of study, no protocol was prepared. Switzerland
(2021 population: ~8.7 million [20])
has an ICU bed base of approximately 11.4 per 100,000 inhabitants. ICUs operate
with a “closed” model and are staffed with certified intensivists.
Inter-hospital ICU transfers could occur in response to limited ICU capacity
(e.g. no available beds) due to the need for specialised services (e.g. extracorporeal
life support) or to centralise COVID-19 patients in designated ICUs (e.g.
Ticino).
Data source
The Swiss ICU Registry (Minimal Dataset for
ICUs, MDSi) systematically collects essential variables describing the structural
characteristics of all certified Swiss ICUs (once a year) and a set of process data
for every patient admitted, such as
information on admission (e.g. time, whether planned or unplanned, etc.),
the severity of illness, the diagnostic group, interventions, daily process
variables and discharge details. Submitting this information to the MDSi is
mandatory; consequently, the data reflect the situation at the national level [21].
The data quality of the MDSi has recently
been assessed, and the results have been published [22]. The expansion of the pandemic
did not allow timely mapping of
COVID-19 in MDSi. Therefore, we used the combination of acute respiratory
distress syndrome (ARDS) plus isolation during the ICU stay as a surrogate for
severe COVID-19 pneumonia [23].
Objectives
Our study aimed to explore COVID-19-induced
changes in Swiss ICUs over one year by comparing the data from 2020 with the
average of figures from 2018 and 2019. We divided the objectives of our study
into four groups: (a) to analyse the impact on admissions and patient
characteristics, including the number of daily ICU admissions and its weekly
moving average and the number of daily unplanned admissions with respiratory
diagnoses and its weekly moving average; (b) to investigate whether patients
had a different LOS in 2020 compared to the previous years; (c) to analyse
whether mortality changed in 2020 and (d) to explore the impact of COVID-19 on
the use of hospital resources, i.e. staffing and equipment.
We extracted the following data from the
Swiss ICU Registry for the years 2018, 2019 and 2020 (1 January to 31 December):
- Number of admissions at the
national level and in the seven major regions defined by the Swiss Federal
Statistical Office [24].
- Patient characteristics: age,
sex, diagnosis group according to the Swiss ICU Registry regulations
(cardiovascular, gastrointestinal, metabolic, neurological, respiratory, trauma
or other) [21], occurrence of ARDS and
isolation (yes or no), early readmission status (within 48 hours), planned and
unplanned admission status, treatment restrictions (present from admission to
the ICU or decided during or at the end of the ICU stay), severity of acute
illness (determined by the Simplified Acute Physiology Score II, SAPS II [25]) and
destination on discharge from the
ICU (general ward, step-down unit, inter-hospital ICU transfer, intra-hospital
ICU-transfer, acute rehabilitation, home or other).
- LOS in days: overall, of the unplanned
admissions with respiratory diagnoses and of the admissions with ARDS and
isolation. LOS time-trend analysis: mean and median LOS by day of admission and
its weekly moving average.
- ICU mortality: overall, of the unplanned
admissions with respiratory diagnoses and of the admissions with ARDS and
isolation.
- Use of hospital resources: nine
equivalents of nursing
manpower use score (NEMS [26]) of the first and the last nursing shifts, total NEMS
per patient,
total NEMS per patient from the unplanned respiratory diagnosis group, number
of nursing shifts per NEMS item, number of full-time equivalents (FTEs) per
professional category (specialised ICU nurses, other clinical nurses, nursing
assistants, non-clinical nurses, specialised ICU physicians and non-specialised
ICU physicians), number of ICU beds and number of ICU beds with mechanical
ventilation.
Statistical analysis
Statistical analysis was performed in compliance with the
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist
[27]. The sample size was determined by the number of patients
aged ≥ 16
years admitted
during 2020 to the 84 certified Swiss ICUs. As a control group, we used a
historical cohort of patients aged ≥16 years admitted to the certified Swiss
ICUs in the previous two years (2018/2019). We used descriptive statistics to
analyse demographic, structural and procedural characteristics. Results were given
as number of
observations (or percentages), mean ± standard deviation (SD), median and interquartile
range (IQR) for continuous variables (age and LOS). Both daily and weekly
moving averages were used for the time series (number of admissions and LOS by
day of admission). Total NEMS per patient served to assess therapeutic nursing workload.
Unless specified, all p-values refer to χ2 tests associated with
contingency tables, a Student’s t-test for the comparison of two groups
of continuous observations or a Wilcoxon rank test for highly asymmetric
distributions such as that of LOS. No adjustment was made for multiple comparisons.
All analyses were conducted using R version 4.1.1 (R Foundation for Statistical
Computing, Vienna, Austria).
Ethics approval and consent to participate
The Ethics Committee from Northwestern
Switzerland – corresponding to the legal location of the Swiss Society for
Intensive Care Medicine – approved the research project (EKNZ UBE-15/47). It
was unnecessary to obtain the consent of the included patients due to the
retrospective and registry-based study design.
Results
Admissions and patient characteristics
We analysed 242,935 patient records from
all 84 certified Swiss ICUs. In 2020, there was a 9.6% reduction in admissions
(84,266 in 2018, 83,027 in 2019 and 75,642 in 2020) affecting all major Swiss
regions equally, except Ticino, where the number of patients admitted remained
stable compared to the average of 2018 and 2019 (p <0.001). The usual net
decrease in hospitalisations during the Christmas holidays was followed in 2020
by a substantial reduction during the two COVID-19 waves (figure 1). Low-risk
admissions (i.e. SAPS II <20 points) decreased by 16%. In 2020, patients
were slightly younger and had a higher acuity, and the proportion of male
patients was slightly higher compared to in previous years (table 1). Planned admissions
(e.g. following a scheduled inpatient procedure) decreased more than unplanned
admissions (–12% vs –8.5%), from 25,020 to 22,021, and this mainly affected the
neurological/neurosurgical (–14.9%), gastrointestinal (–13.9%) and
cardiovascular (–9.3%) diagnosis groups. The overall reduction in admissions did
not affect the respiratory group, whose admissions increased substantially. More
patients required unplanned admission to intensive care due to respiratory
diagnoses during the two COVID-19 waves of 2020, with two peaks (about 60
admissions per day) twice as prominent as in previous winter flu seasons (figure
2). In 2020, the subgroup of patients with ARDS requiring isolation reached 9973
and more than doubled compared to the 2018/2019 average.
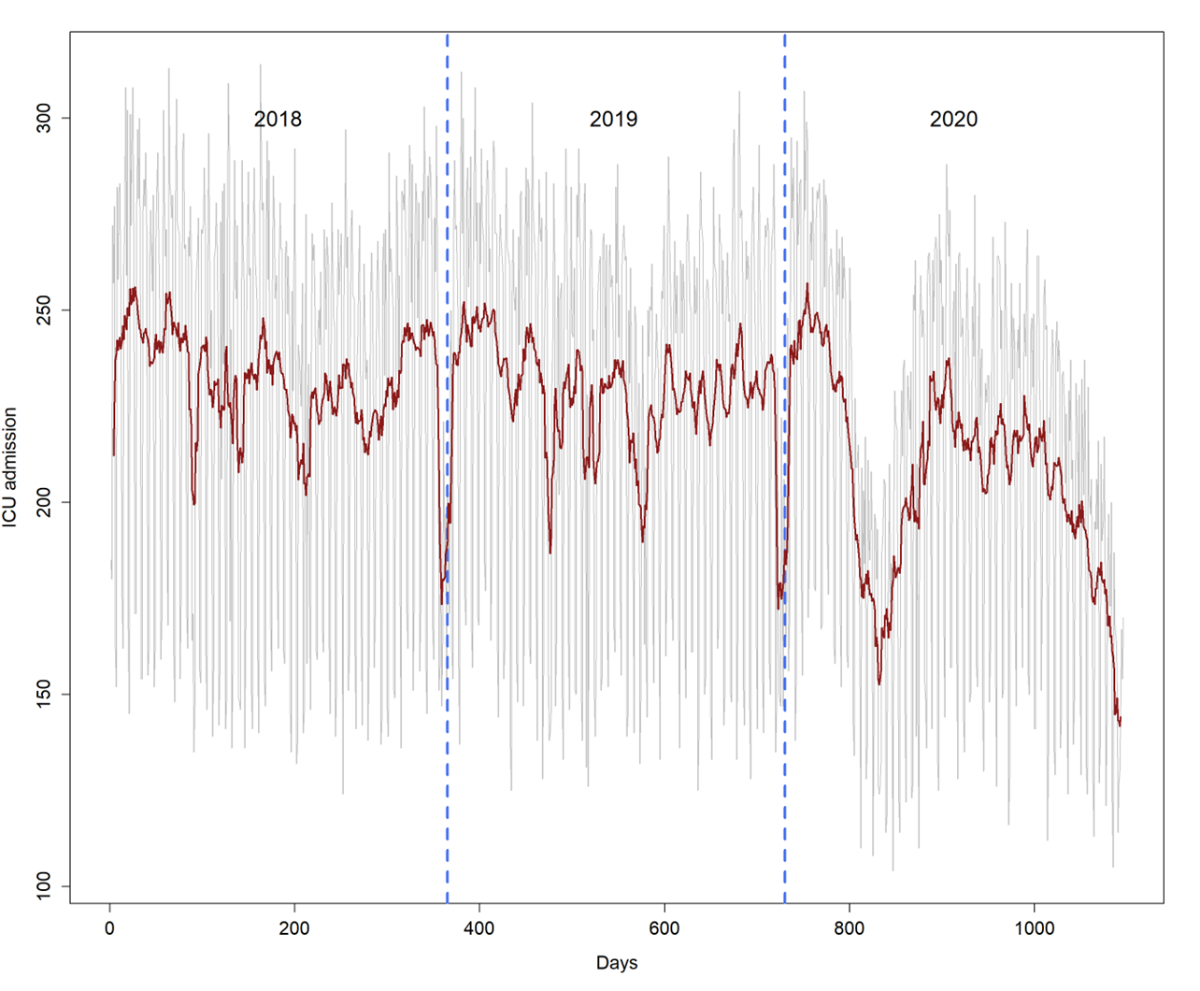
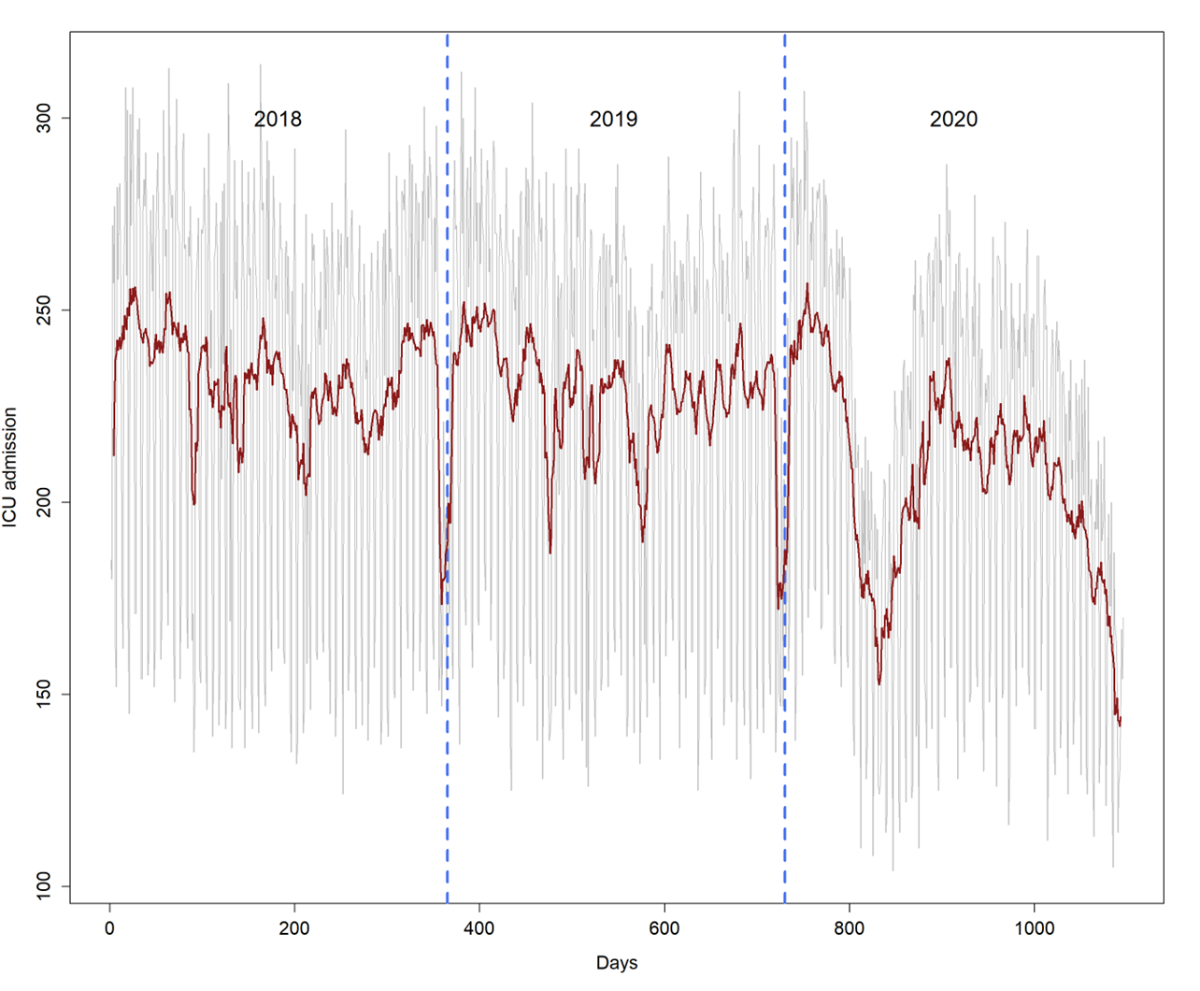
Figure 1Number of daily intensive care unit (ICU)
admissions (grey) and its weekly moving average (red) during the study period.
The dashed vertical blue lines indicate the calendar year changes. The usual
net decrease in hospitalisations during the Christmas holidays (also
recognisable during the weeks after Easter and Whitsun) was followed in 2020 by
a massive drop during the two COVID-19 waves.
Patient transfers between ICUs increased slightly
in 2020, while the locations of the follow-up treatments of the patients after
ICU stays remained unchanged. The 48-hour readmission rate was similar between
the two periods.
Table 1Patient characteristics and outcomes.
| |
Mean
2018/2019 |
2020 |
Difference |
p-value |
| n |
83,647 |
75,642 |
–9.6% |
|
| Age, years |
Mean (SD) |
65.2
(17.1) |
65.0
(16.8) |
|
0.005** |
| Median (IQR) |
69
(56–78) |
68
(56–77) |
|
| Male sex |
% |
59.6 |
61.3 |
|
<0.001# |
| Planned admissions |
n |
25,020 |
22,021 |
–12.0% |
<0.001# |
| Unplanned admissions |
n |
58,627 |
53,621 |
–8.5% |
|
| Unplanned admissions, respiratory |
n |
7807 |
9778 |
+25.2% |
<0.001# |
| SAPS II |
Mean (SD) |
32.1
(17.3) |
32.7
(16.9) |
|
<0.001** |
| Median (IQR) |
29
(21–40) |
30 (21–41) |
|
| SAPS II <20 (low risk) |
n (%) |
17,780
(21.3%) |
14,984
(19.8%) |
–15.7% |
<0.001# |
| Diagnosis group* |
<0.001## |
| |
Cardiovascular |
n (%) |
26,878
(32.1%) |
22,969
(30.4%) |
–14.5% |
|
| Gastrointestinal |
n (%) |
10,855
(13.0%) |
9608
(12.7%) |
–11.5% |
|
| Metabolic |
n (%) |
5350
(6.4%) |
4594
(6.1%) |
–14.1% |
|
| Neurological |
n (%) |
12,432
(14.9%) |
10,860
(14.4%) |
–12.6% |
|
| Respiratory |
n (%) |
10,501
(12.6%) |
12,306
(16.3%) |
+17.2% |
|
| Respiratory: ARDS requiring isolation |
n (%) |
4751
(5.7%) |
9973
(13.2%) |
+109.9% |
<0.001# |
| Trauma |
n (%) |
4969
(5.9%) |
4484
(5.9%) |
–9.8% |
|
| Other |
n (%) |
12,662
(15.1%) |
10,821
(14.3%) |
–14.5% |
|
| Length of stay |
Overall, days |
Mean (SD) |
2.5
(4.9) |
3.1
(5.9) |
+20.8% |
<0.001*** |
| Median (IQR) |
1.0
(0.7–2.4) |
1.1
(0.8–2.8) |
|
| Unplanned admissions, respiratory |
Mean (SD) |
4.1
(6.5) |
7.2
(10.0) |
+76.4% |
<0.001*** |
| Median (IQR) |
2.0
(0.9–4.6) |
3.2
(1.2–8.9) |
|
| ARDS requiring isolation |
Mean (SD) |
6.6
(11.2) |
6.0
(9.3) |
–9.6% |
<0.001*** |
| Median (IQR) |
2.8
(1.2–6.9) |
2.6
(1.1–6.7) |
|
| Cumulative ICU days |
n |
213,238 |
232,991 |
+19,753 (+9.3%) |
|
| Discharge route |
|
<0.001### |
| General ward |
n (%) |
61,625
(73.7%) |
54,554
(72.1%) |
–11.5% |
|
| Step-down unit |
n (%) |
6052
(7.2%) |
5522
(7.3%) |
–8.8% |
|
| Inter-hospital ICU transfer |
n (%) |
2676
(3.2%) |
2901
(3.8%) |
+8.4% |
|
| Intra-hospital ICU transfer |
n (%) |
233
(0.3%) |
300
(0.4%) |
+28.8% |
|
| Inter-hospital transfer |
n (%) |
3256
(3.9%) |
2831
(3.7%) |
–13.1% |
|
| Acute rehabilitation |
n (%) |
115
(0.1%) |
184
(0.2%) |
+60% |
|
| Home |
n (%) |
3634
(4.3%) |
3216
(4.3%) |
–11.5% |
|
| Other |
n (%) |
2097
(2.5%) |
1778
(2.4%) |
–15.2% |
|
| Readmission rate |
n (%) |
1965
(2.3%) |
1702
(2.3%) |
–13.4% |
0.13# |
| ICU mortality |
Overall |
n (%) |
3961
(4.7%) |
4315
(5.7%) |
+8.9% |
<0.001# |
| Women |
n (%) |
1540
(4.6%) |
1532
(5.2%) |
–0.5% |
|
| Men |
n (%) |
2421
(4.9%) |
2783
(6.0%) |
+15.0% |
|
| Unplanned admissions, respiratory |
n (%) |
634
(8.1%) |
1301
(13.3%) |
+105.2% |
<0.001# |
| ARDS requiring isolation |
n (%) |
471
(9.9%) |
1053
(10.6%) |
+123.6% |
0.14# |
| Treatment restrictions |
n (%) |
13,100
(15.7%) |
12,336
(16.3%) |
–5.8% |
<0.001# |
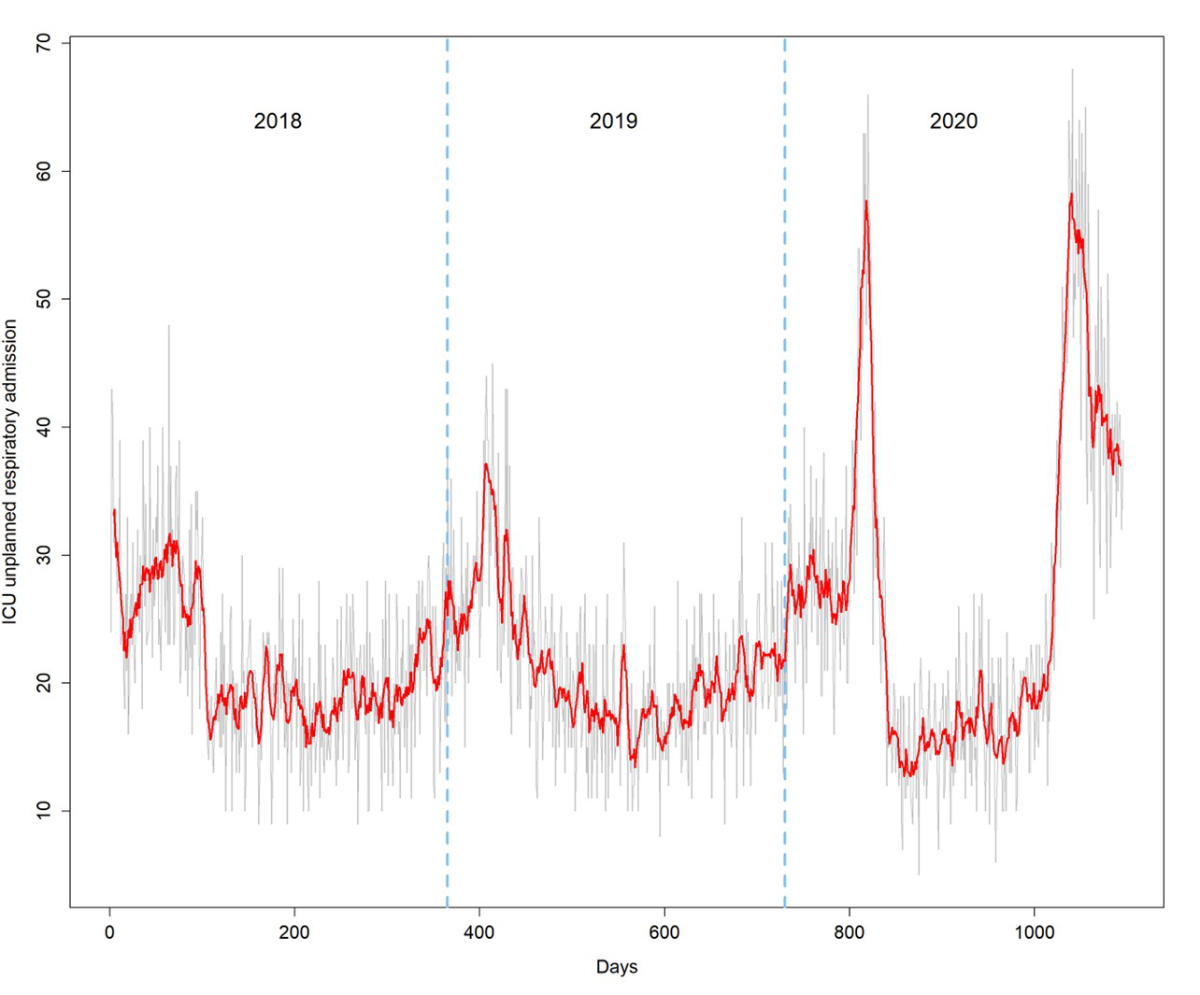
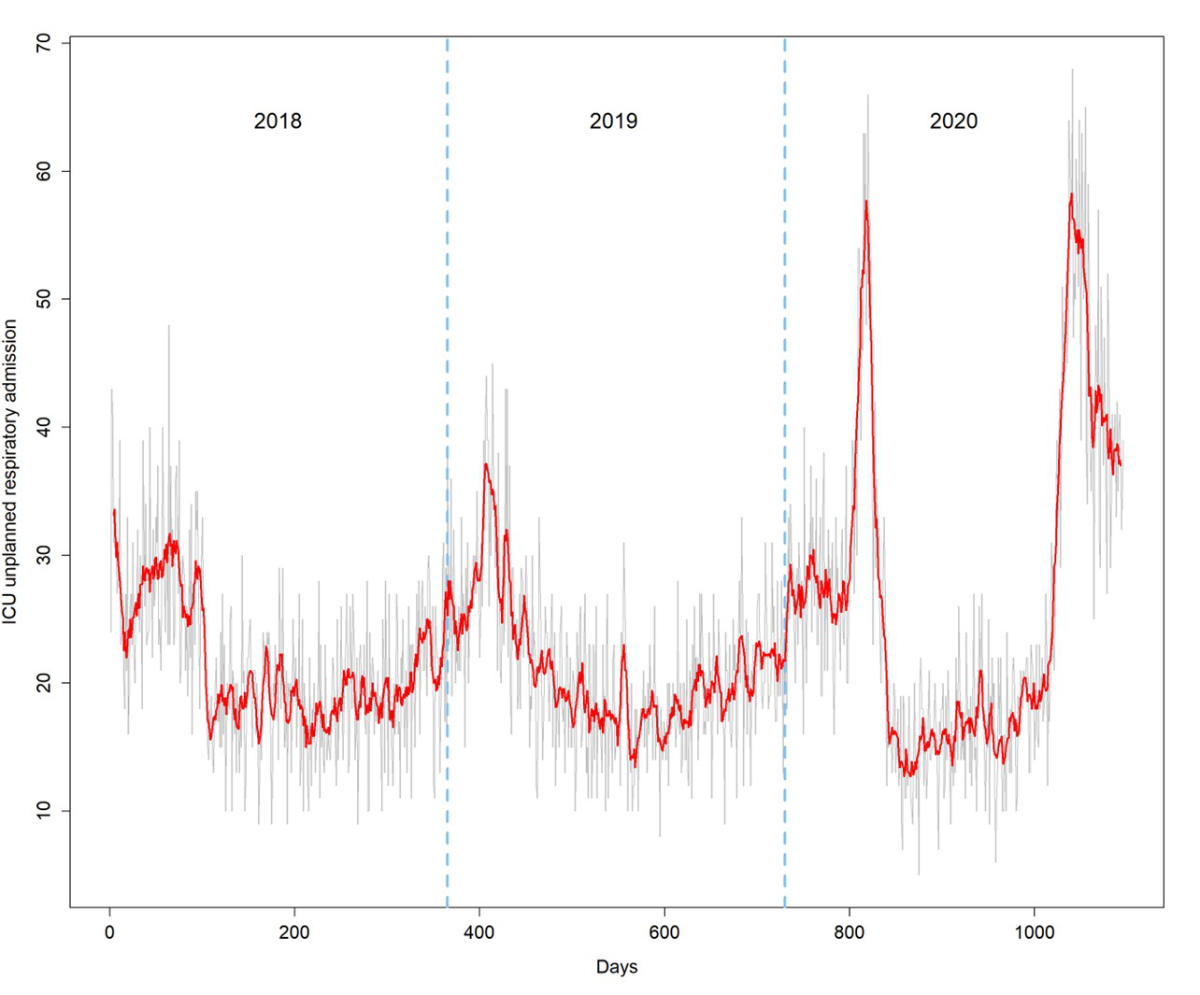
Figure 2Figure 2: Daily unplanned ICU
admissions with a respiratory diagnosis (grey) and its weekly moving average
(red) during the study period. The dashed vertical blue lines indicate the
calendar year changes.
Length of stay (ICU LOS)
The mean ICU LOS increased by 20.8%,
generating an increase of 19,753 days of stay (+9.3%) in Swiss ICUs despite the
reduction in admissions. This increase was mainly generated by patients with unplanned
admissions and respiratory diagnoses (median LOS 3.2 days, IQR 1.2–8.9, vs 2.0
days, IQR 0.9–4.6; p <0.001), who showed a substantial but short-lived peak in
ICU LOS during the first wave of COVID-19 and a milder but longer-lasting increase
during the second wave (figure 3). The increase in LOS of all other admissions was
not significant (median LOS 1.0 days, IQR 0.7–2.2, vs 1.0 days, IQR 0.7–2.1; p =
0.07).
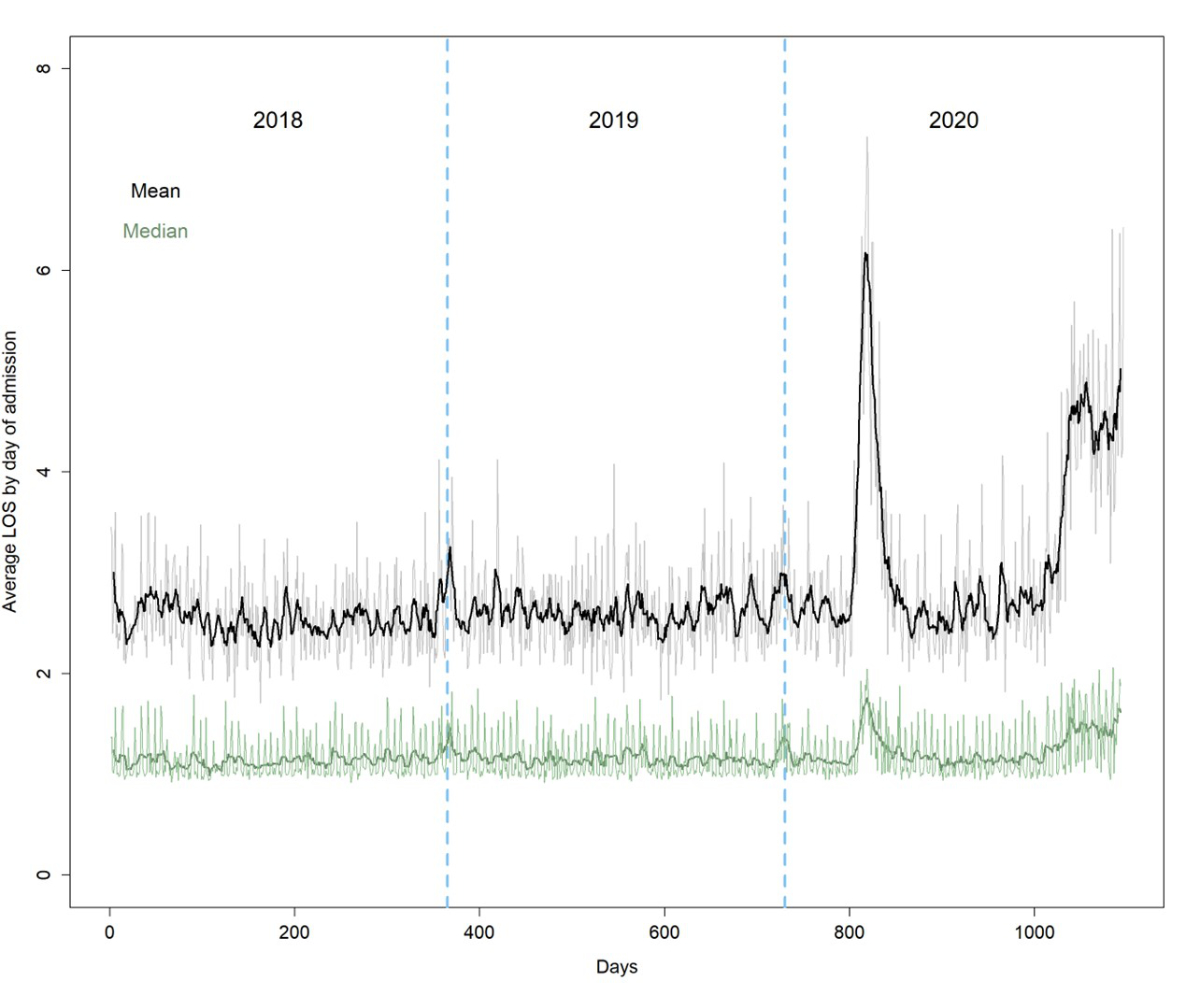
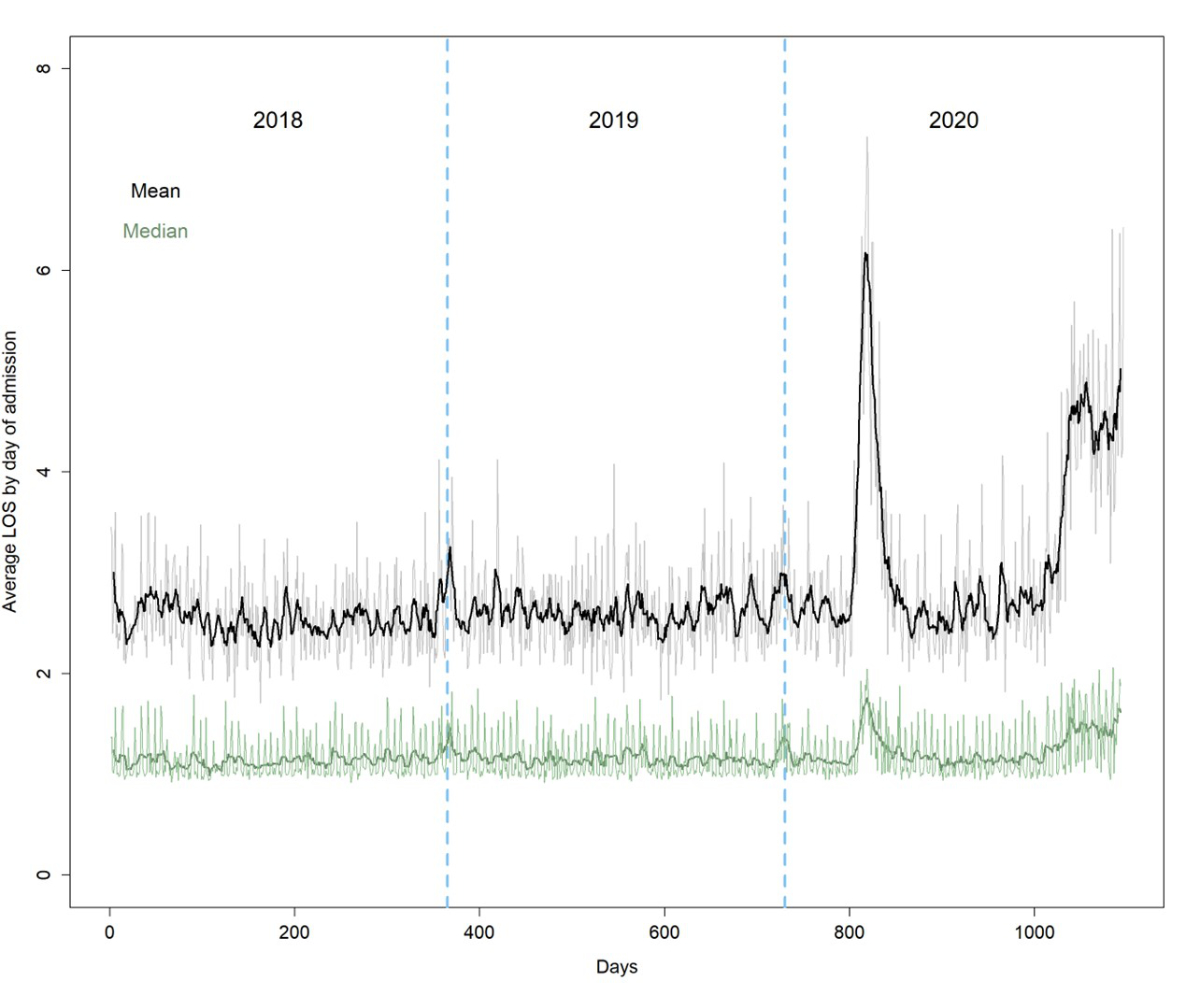
Figure 3Mean (black) and median (dark green) length of
stay (LOS) by day of admission and its weekly moving average (bold lines). The dashed
vertical blue lines indicate the calendar year changes.
Mortality in ICUs
The proportion of patients with treatment
restrictions was slightly higher in 2020 compared to the average in 2018 and
2019 (16.3 vs 15.7%; p <0.001). However, mean mortality increased
significantly from 4.7% in 2018/2019 to 5.7% in 2020. This increase was driven mainly
by a considerable increase in deaths among patients with unplanned admissions and
respiratory diagnoses (13.3% vs
8.1% in 2018/2019; p <0.001).
Therapeutic hospital resources and staffing
The NEMS (± SD) of the first shift increased
from 20.8 ± 9.4 in 2018/2019 to 21.6 ± 9.0 in 2020 (p <0.001), while
the NEMS of the last shift remained nearly stable (table 2). In contrast, the
total NEMS per patient was significantly higher in 2020, mainly due to the vast
contribution from unplanned admissions with respiratory diagnoses (238.5, IQR
92–747, vs 148, IQR 72–332; p <0.001).
Breaking down the therapeutic workload by NEMS
items, we found a significant increase in shifts with mechanical ventilation,
single vasoactive drugs and dialysis techniques in 2020. At the same time,
Swiss ICUs employed more human resources from all professional categories except
staff with administrative duties: specialised nurses went from 2393 to 2468 FTE
(+3.1%), other clinical nurses from 988 to 1127 FTE (+14.1%), nursing
assistants from 464 to 549 FTE (+18.4%), non-clinical nurses from 465 to 454 FTE
(–2.3%), specialised ICU physicians from 364 to 405 FTE (+11.2%) and
non-specialised physicians from 666 to 727 FTE (+9.2%). The number of ICU beds
increased from 979 (2018/2019 average) to 1012, representing a 3.4% gain during
the 2020 COVID-19 pandemic. The number of beds with mechanical ventilation
increased from 773 (2018/2019 average) to 821 (+6.2%).
Table 2Therapeutic workload and employment of human resources in Swiss ICUs.
Values represent mean (± SD) and median (IQR)
in nursing shifts and percent change during the 2020 COVID-19 pandemic compared
to the previous period.
P-values were obtained using a Wilcoxon
rank sum test comparing 2020 data and 2018/2019 data.
| |
Average
2018/2019 |
2020 |
Difference |
p-value |
| NEMS |
| First shift |
Mean (SD) |
20.8 (9.4) |
21.6 (9.0) |
+3.8% |
|
| Median (IQR) |
18 (15–25) |
18 (15–27) |
|
<0.001 |
| Last shift |
Mean (SD) |
17.4 (6.0) |
17.3 (6.7) |
–0.6% |
|
| Median (IQR) |
18 (15–18) |
18 (15–18) |
|
<0.001 |
| Total, all |
Mean (SD) |
198.9 (413.8) |
251.0 (526.8) |
+26.2% |
|
| Median (IQR) |
84 (54–172) |
88 (54–198) |
|
<0.001 |
| Total, unplanned admissions, respiratory |
Mean (SD) |
324.4 (551.7) |
617.7 (918.4) |
+90.4% |
|
| Median (IQR) |
148 (72–332) |
239 (92–747) |
|
<0.001 |
| Total, all except unplanned admissions, respiratory |
Mean (SD) |
186.0
(394.7) |
196.6
(413.0) |
+5.7% |
|
| Median (IQR) |
79 (54–159) |
81 (54–162) |
|
0.014 |
| Resource use according to NEMS |
| Basic monitoring |
Mean (SD) |
8.6 (14.7) |
10.2 (17.5) |
+18.4% |
|
| Median (IQR) |
4 (3–8) |
4 (3–9) |
|
<0.001 |
| Total shifts |
719,947 |
771,145 |
+7.1% |
|
| Intravenous medication |
Mean (SD) |
7.7 (13.7) |
9.3 (16.8) |
+20.1% |
|
| Median (IQR) |
4 (3–7) |
4 (3–9) |
|
<0.001 |
| Total shifts |
648,118 |
704,101 |
+8.6% |
|
| Mechanical ventilation |
Mean (SD) |
2.7 (10.2) |
4.2 (13.9) |
+55.1% |
|
| Median (IQR) |
0 (0–1) |
0 (0–2) |
|
<0.001 |
| Total shifts |
228,531 |
320,441 |
+40.2% |
|
| Supplementary ventilatory care |
Mean (SD) |
4.2 (6.8) |
4.4 (7.0) |
+4.2% |
|
| Median (IQR) |
3 (1–5) |
3 (1–5) |
|
0.01 |
| Total shifts |
351,224 |
331,017 |
–5.8% |
|
| Single vasoactive drug |
Mean (SD) |
2.2 (6.5) |
3.3 (9.0) |
+46.4% |
|
| Median (IQR) |
0 (0–2) |
0 (0–3) |
|
<0.001 |
| Total shifts |
185,814 |
246,076 |
+32.4% |
|
| Multiple vasoactive drugs |
Mean (SD) |
0.6 (2.9) |
0.6 (3.0) |
+3.8% |
|
| Median (IQR) |
0 (0–0) |
0 (0–0) |
|
0.48 |
| Total shifts |
46,104 |
43,265 |
–6.2% |
|
| Dialysis techniques |
Mean (SD) |
0.5 (4.8) |
0.7 (5.4) |
+35.3% |
|
| Median (IQR) |
0 (0–0) |
0 (0–0) |
|
<0.001 |
| Total shifts |
40,350 |
49,401 |
+22.4% |
|
| Specific intervention in the ICU |
Mean (SD) |
0.6 (2.4) |
0.7 (2.8) |
+18.8% |
|
| Median (IQR) |
0 (0–0) |
0 (0–0) |
|
<0.001 |
| Total shifts |
50,410 |
54,079 |
+7.3% |
|
| Specific intervention outside the ICU |
Mean (SD) |
0.4 (1.1) |
0.4 (1.2) |
+5.0% |
|
| Median (IQR) |
0 (0–0) |
0 (0–0) |
|
0.40 |
| Total shifts |
32,628 |
30,991 |
–5.0% |
|
Discussion
The present study describes the utilisation
of ICUs in Switzerland at a national level before and during the first year of
the COVID-19 pandemic and presents several key findings: (a) an overall
decrease in the number of admissions, including planned admissions; (b) fewer
admissions of low-risk cases (SAPS II <20 points); (c) an increase in
unplanned admissions due to respiratory diagnoses and related mortality rates; (d)
a nationwide 9.3% increase in ICU bed-days; (e) an increased need for
ICU-specific therapies (e.g. mechanical ventilation, vasopressor therapy and
renal replacement therapy) and human resources and (f) a significantly higher
total NEMS per patient, reflecting longer ICU stays and increased use of ICU-specific
therapies.
The countries hardest hit by the pandemic
faced a sudden and disproportionate number of hospitalisations. Due to its
proximity to Lombardy, the first area outside of China to be
overwhelmed by the SARS-CoV-2 epidemic [28], Ticino was the Swiss region that suffered
most during the first
wave, while the regions north of the Alps saw a much less aggressive spread of
cases. This delay allowed the social distancing measures imposed by the
government to mitigate the impact of the disease and thus avoid overburdening
hospitals and ICUs in large parts of the country. In parallel, on government instructions,
hospitals rapidly reduced and finally ceased elective surgical/interventional
activities and created additional ad hoc ICU beds to provide a buffer to
absorb the increase in patients with COVID-19. Under these circumstances, we
found an absolute 9.6% reduction in ICU admissions in 2020. There were 14.5%
fewer patients in the cardiovascular diagnosis group. Reports from different
countries during the first pandemic wave describe a substantial reduction in ICU
admissions for acute coronary syndromes [29–35]. This reduction was partly related
to patients’ reluctance to
present to the hospital for fear of contracting COVID-19 or violating social
distancing regulations and misinterpretation of heart attack symptoms rather
than being a beneficial effect of lifestyle changes during the pandemic
lockdown [36]. In addition, a
survey conducted by the European Association of Percutaneous Coronary
Interventions showed that catheterisation laboratories reduced their activity
due to the unavailability of staff and to decrease the risk of infection, thereby
admitting fewer patients to ICU for post-procedural monitoring [37].
Cardiac surgical volumes displayed an even stronger decrease, with 30–90%
reductions as a result of discontinuing all elective or deferrable surgeries [6, 38–40],
and only a partial recovery after
the surge [39–42]. In Switzerland,
two major tertiary centres confirmed that the overall incidence of patients
with acute coronary syndromes undergoing percutaneous coronary interventions was
significantly lower, whereas the incidence of transmural myocardial infarction did
not differ considerably from that of previous years [43,
44].
In this context, we observed 16% fewer
low-risk ICU admissions in 2020, probably due to the reduction of ICU admissions
for monitoring patients with acute coronary syndrome or after elective surgery
and, in addition, the need to allocate ICU beds to severely ill emergency patients.
The reduction in planned ICU admissions from 25,020 (2018/2019) to 22,021
(2020), mainly to the neurological/neurosurgical, gastrointestinal and
cardiovascular diagnosis groups, suggests a loss of about 3,000 elective interventions.
As reported by several authors, there was a reduction in referrals for
evaluation of brain tumours during the lockdown. Some patients with malignant
brain tumours changed their initial treatment strategy and often received only
simple diagnostic biopsy [45, 46]. In general, about 10% of patients with several
solid cancer types did
not receive their planned surgical treatment, and those awaiting surgery in a
complete lockdown for more than six weeks had an increased likelihood of
non-operation. The effect of these changes in therapeutic approach on outcomes
has not been reported [5]. In
situations with several treatment options (e.g. coronary artery disease), the
least invasive option might have been selected to reduce hospital time and
avoid intensive care. However, no statistically significant change in
in-hospital mortality was demonstrated [40,
41].
In contrast, we observed a 17% increase in
respiratory diagnoses and a doubling of ARDS cases requiring isolation.
Although data from our registry do not allow tracing the exact aetiology, it is
likely that many of these admissions were due to COVID-19, which explains the
higher mortality over the year and the significantly worse outcomes among patients
with unplanned admissions and respiratory diagnoses compared to the 2018/2019
control group.
The previous studies in Japan and Alberta,
Canada, where the critical care surge of COVID-19 did not exceed the ICU bed
capacity, showed a substantial decline in ICU admissions during the first
COVID-19 pandemic year and the COVID-19 lockdown, respectively [15, 16]. Despite fewer
admissions in 2020, Swiss
ICUs recorded about 20,000 more inpatient days due to a significant increase in
ICU LOS, mainly driven by unplanned respiratory admissions. On average, such
patients remained in the ICU for seven days, almost twice as long as in
2018/2019, while their median LOS increased from 2.0 to 3.2 days. In contrast,
the median LOS of patients with ARDS requiring isolation decreased from 2.8 to
2.6 days in 2020, which is significantly shorter than the 9.0 days described in
a meta-analysis of studies involving critically ill COVID-19 patients [47]. This difference
can have several explanations.
First, our cohort might, to some extent, include patients with different
characteristics (i.e. aetiology and severity), which the constraints of the
Swiss ICU Registry mentioned above do not allow us to identify precisely. Second,
management of COVID-19 patients different from that published may result in
earlier transfer to a step-down unit or general ward. Finally, the lower LOS
could be due to higher early mortality. However, this hypothesis is unlikely to
explain the difference, given that patients with unplanned respiratory
admissions and those with ARDS requiring isolation in our cohort had a
substantially lower ICU mortality (13% and 10.6%, respectively, vs 32%) than those
of the meta-analysis of COVID-19 cases [47].
During the pandemic, in 2020, patients were
found to require more supportive care and invasive ICU-specific therapies over
a longer period of time, as evidenced by an increase in ICU LOS. They required
more mechanical ventilation (+55%), more renal replacement therapies (+35%) and
more vasopressors (+46%) than in 2018/2019. In addition to indicating greater
patient severity, this translated into a 26% increase in the total NEMS.
During the pandemic, Swiss ICUs employed
more human resources from all professional categories except staff with
administrative duties. However, as they were able to recruit only 3% more intensive
care nurses, critical care departments had to mitigate staff shortages by
reallocating non-specialised nurses and nursing assistants from other
departments. Furthermore, due to reduced elective activity and the closure of operating
theatres for scheduled and deferrable operations, it was possible to redeploy medical
personnel (i.e. anaesthetists and other specialists with some ICU expertise)
and thus substantially increase staffing levels. This experience will help in
future emergency planning. For example, it has demonstrated the value of
preserving the expertise of physicians with specialities other than critical
care but with experience in this area and of promoting regular ICU rotations.
Furthermore, it has encouraged the establishment of critical care training
courses for anaesthesia, emergency room and intermediate care nurses to facilitate
flexible work assignments in a crisis such as a pandemic. Finally, given the
increase in ICU bed-days, the reduction in elective admissions and the uneven
distribution of patients across Swiss regions, the pandemic experience has
shown that central coordination is essential to ensure optimal use of resources
and equal accessibility to all categories of patients while respecting
distributive justice.
The main strengths of our study are its
nationwide design, its large sample size within the setting of a homogeneous
healthcare system and the good data quality of the Swiss ICU Registry.
Nevertheless, there are some limitations. First, this was a retrospective study
of registry-based data with possible variation in coding among people and
institutions. Second, as the rapid expansion of the pandemic did not allow for
a timely mapping of COVID-19 patients in the MDSi, we had to use a combination
of two variables (ARDS and isolation) to define this patient group. However,
even with this limitation, we were able to illustrate substantial changes in
Swiss ICUs that occurred during the COVID-19 pandemic. Third, there might have
been some missing data (e.g. additional beds ± mechanical ventilators or
inaccurate scoring). Accordingly, structural and procedural data might have been
under- or overestimated. Furthermore, the structural data represent the average
over the year and do not reflect the fluctuations in beds and staff during
waves of the pandemic. Fourth, the Swiss ICU Registry provides only ICU mortality
data. Due to different ICU admission and discharge practices in various
hospitals, the mortality data need to be interpreted accordingly. Nonetheless,
excess mortality in Switzerland during the pandemic year 2020 was in line with
that of other European countries [48].
Fifth, unimportant differences might become statistically significant in
large-scale registry-based studies. Consequently, we focused on results with
clinical and public health relevance. Sixth, our results may not be generalised
to other countries because of different approaches and strategies for managing the
crisis. Finally, this study was mainly exploratory and used an extensive
database to generate hypotheses for further research.
Conclusions
Our report describes the nationwide changes
in ICU needs and resource use triggered by the COVID-19 pandemic in 2020: an
overall decrease in the number of admissions and a shift in admission types,
with fewer planned admissions, suggesting the loss of about 3,000 elective
interventions; fewer admissions of low-risk cases; an increase in patients with
unplanned admissions due to respiratory diagnoses and related mortality rates;
a nationwide 9.3% increase in ICU bed-days and a significantly higher total
NEMS per patient, reflecting the increased ICU LOS and the increased use of
ICU-specific therapies. In future emergencies, a national body should allocate
patients requiring intensive care in a coordinated manner to optimise resource
use while respecting distributive justice. In the meantime, the expertise of
doctors with past ICU experience should be preserved, and training courses for
“multi-specialised” nurses in the “resuscitation” area should be developed to
obtain a reserve of sufficiently
qualified personnel. Furthermore, it is necessary to invest in infrastructure, which
must be maintained, to be prepared for future emergencies.
Availability of data and materials
The
datasets analysed during the current study are available from the corresponding
author upon reasonable request.
Acknowledgments
Authors’ contributions: AP, MP and BC conceived the study, edited the data and
developed the methodology. BC performed the formal analysis. MP and AP drafted,
edited and reviewed the original manuscript (equal contributions). AC, MK, HP
and RL helped to develop the methodology and participated in drafting the
manuscript. All authors approved the final version.
Marco
Previsdomini
Intensive Care Unit
Ospedale Regionale Bellinzona e Valli (EOC)
Via A. Gallino 12
CH-6500 Bellinzona
Marco.Previsdomini[at]eoc.ch
References
1. Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak
in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA.
2020 Apr;323(16):1545–6. 10.1001/jama.2020.4031
2. Puerta JL, Torrego-Ellacuría M, Del Rey-Mejías Á, Bienzobas López C. Capacity and
organisation of Madrid’s community hospitals during first wave of COVID-19 pandemic.
J Healthc Qual Res. 2022;37(5):275–82. 10.1016/j.jhqr.2022.02.002
3. Uppal A, Silvestri DM, Siegler M, Natsui S, Boudourakis L, Salway RJ, et al. Critical
Care And Emergency Department Response At The Epicenter Of The COVID-19 Pandemic.
Health Aff (Millwood). 2020 Aug;39(8):1443–9. 10.1377/hlthaff.2020.00901
4. Kursumovic E, Cook TM, Vindrola-Padros C, Kane AD, Armstrong RA, Waite O, et al. The
impact of COVID-19 on anaesthesia and critical care services in the UK: a serial service
evaluation. Anaesthesia. 2021 Sep;76(9):1167–75. 10.1111/anae.15512
5. Glasbey J, Ademuyiwa A, Adisa A, AlAmeer E, Arnaud AP, Ayasra F, et al.; COVIDSurg
Collaborative. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for
15 tumour types in 61 countries: an international, prospective, cohort study. Lancet
Oncol. 2021 Nov;22(11):1507–17. 10.1016/S1470-2045(21)00493-9
6. George I, Salna M, Kobsa S, Deroo S, Kriegel J, Blitzer D, et al. The rapid transformation
of cardiac surgery practice in the coronavirus disease 2019 (COVID-19) pandemic: insights
and clinical strategies from a centre at the epicentre. European J Cardio-thoracic
Surg Official J European Assoc Cardio-thoracic Surg. 2020;58(4):ezaa228.
7. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, et al. COVID-19 pandemic
and admission rates for and management of acute coronary syndromes in England. Lancet.
2020 Aug;396(10248):381–9. 10.1016/S0140-6736(20)31356-8
8. Esenwa C, Parides MK, Labovitz DL. The effect of COVID-19 on stroke hospitalizations
in New York City. J Stroke Cerebrovasc Dis. 2020 Oct;29(10):105114–105114. 10.1016/j.jstrokecerebrovasdis.2020.105114
9. Abdulazim A, Ebert A, Etminan N, Szabo K, Alonso A. Negative Impact of the COVID-19
Pandemic on Admissions for Intracranial Hemorrhage. Front Neurol. 2020 Sep;11:584522.
10.3389/fneur.2020.584522
10. Walline JH, Hung KK, Yeung JH, Song PP, Cheung NK, Graham CA. The impact of SARS and
COVID-19 on major trauma in Hong Kong. Am J Emerg Med. 2021 Aug;46:10–5. 10.1016/j.ajem.2021.02.030
20. Office FS. [Internet]. Population. 2021;2023(Mar): [cited 2023 Jun 13] Available from:
https://www.bfs.admin.ch/bfs/en/home/statistics/population.assetdetail.24625451.html
21. Minimaler Datensatz der SGI – MDSi [Internet]. 2021. Available from: https://www.sgi-ssmi.ch/de/datensatz.html
22. Perren A, Cerutti B, Kaufmann M, Rothen HU; Swiss Society of Intensive Care Medicine.
A novel method to assess data quality in large medical registries and databases. Int
J Qual Health Care. 2019 Aug;31(7):1–7. 10.1093/intqhc/mzy249
23. Fumeaux T, von Arx F, Perren A, Kaufmann M, Kleger GR, Balmer M, et al. COVID-19:
Administrative Belange der Intensivmedizin. Schweiz Arzteztg. 1718;2020(101):576–8.
24. Major Regions in Switzerland [Internet]. 2000 [cited 2022 Jul 26]. Available from:
https://www.bfs.admin.ch/bfs/en/home/statistics/catalogues-databases.assetdetail.1031445.html
25. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS
II) based on a European/North American multicenter study. JAMA. 1993 Dec;270(24):2957–63.
10.1001/jama.1993.03510240069035
26. Reis Miranda D, Moreno R, Iapichino G. Nine equivalents of nursing manpower use score
(NEMS). Intensive Care Med. 1997 Jul;23(7):760–5. 10.1007/s001340050406
27. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)
statement: guidelines for reporting observational studies. PLoS Med. 2007 Oct;4(10):e296.
10.1371/journal.pmed.0040296
28. Trentini F, Marziano V, Guzzetta G, Tirani M, Cereda D, Poletti P, et al. The pressure
on healthcare system and intensive care utilization during the COVID-19 outbreak in
the Lombardy region: a retrospective observational study on 43,538 hospitalized patients.
Am J Epidemiol. 2022 Jan;191(1):137–46. 10.1093/aje/kwab252
29. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al.; Società
Italiana di Cardiologia and the CCU Academy investigators group. Reduction of hospitalizations
for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020 Jun;41(22):2083–8.
10.1093/eurheartj/ehaa409
30. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction
in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United
States During COVID-19 Pandemic. J Am Coll Cardiol. 2020 Jun;75(22):2871–2. 10.1016/j.jacc.2020.04.011
31. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary
syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response
causes cardiac collateral damage. Eur Heart J. 2020 May;41(19):1852–3. 10.1093/eurheartj/ehaa314
32. Abdi S, Salarifar M, Mortazavi SH, Sadeghipour P, Geraiely B. COVID-19 sends STEMI
to quarantine!? Clin Res Cardiol. 2020 Dec;109(12):1567–8. 10.1007/s00392-020-01664-3
33. Nef HM, Elsässer A, Möllmann H, Abdel-Hadi M, Bauer T, Brück M, et al.; CoVCAD –Study
Group. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization
activity during the lockdown in central Germany: an observational study. Clin Res
Cardiol. 2021 Feb;110(2):292–301. 10.1007/s00392-020-01780-0
34. Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, et al. The Covid-19 Pandemic
and the Incidence of Acute Myocardial Infarction. N Engl J Med. 2020 Aug;383(7):691–3.
10.1056/NEJMc2015630
35. Sokolski M, Gajewski P, Zymliński R, Biegus J, Berg JM, Bor W, et al. Impact of Coronavirus
Disease 2019 (COVID-19) Outbreak on Acute Admissions at the Emergency and Cardiology
Departments Across Europe. Am J Med. 2021 Apr;134(4):482–9. 10.1016/j.amjmed.2020.08.043
36. Tsigkas G, Koufou EE, Katsanos K, Patrinos P, Moulias A, Miliordos I, et al. Potential
Relationship Between Lifestyle Changes and Incidence of Hospital Admissions for Acute
Coronary Syndrome During the COVID-19 Lockdown. Front Cardiovasc Med. 2021 Feb;8:604374.
10.3389/fcvm.2021.604374
37. Roffi M, Capodanno D, Windecker S, Baumbach A, Dudek D. Impact of the COVID-19 pandemic
on interventional cardiology practice: results of the EAPCI survey. EuroIntervention.
2020 Jun;16(3):247–50. 10.4244/EIJ-D-20-00528
38. Mohamed MO, Banerjee A, Clarke S, de Belder M, Patwala A, Goodwin AT, et al. Impact
of COVID-19 on cardiac procedure activity in England and associated 30-day mortality.
Eur Heart J Qual Care Clin Outcomes. 2021 May;7(3):247–56. 10.1093/ehjqcco/qcaa079
39. Nägele F, Engler C, Graber M, Remmel N, Hirsch J, Pölzl L, et al. Lockdown surgery:
the impact of coronavirus disease 2019 measures on cardiac cases. Interact Cardiov
Th. 2022;35(1):ivac060. 10.1093/icvts/ivac060
40. Nguyen TC, Thourani VH, Nissen AP, Habib RH, Dearani JA, Ropski A, et al. The Effect
of COVID-19 on Adult Cardiac Surgery in the United States in 717'103 Patients. Ann
Thorac Surg. 2022 Mar;113(3):738–46. 10.1016/j.athoracsur.2021.07.015
41. Yong CM, Spinelli KJ, Chiu ST, Jones B, Penny B, Gummidipundi S, et al. Cardiovascular
procedural deferral and outcomes over COVID-19 pandemic phases: A multi-center study.
Am Heart J. 2021 Nov;241:14–25. 10.1016/j.ahj.2021.06.011
42. Beckmann A, Meyer R, Lewandowski J, Markewitz A, Gummert J. German Heart Surgery Report
2020: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular
Surgery. Thorac Cardiovasc Surg. 2021 Jun;69(4):294–307. 10.1055/s-0041-1730374
43. Perrin N, Iglesias JF, Rey F, Benzakour L, Cimci M, Noble S, et al. Impact of the
COVID-19 pandemic on acute coronary syndromes. Swiss Med Wkly. 2020 Dec;150(5153):w20448.
10.4414/smw.2020.20448
44. Boeddinghaus J, Nestelberger T, Kaiser C, Twerenbold R, Fahrni G, Bingisser R, et
al. Effect of COVID-19 on acute treatment of ST-segment elevation and Non-ST-segment
elevation acute coronary syndrome in northwestern Switzerland. Int J Cardiol Heart
Vasc. 2020 Dec;32:100686. 10.1016/j.ijcha.2020.100686
45. Price SJ, Joannides A, Plaha P, Afshari FT, Albanese E, Barua NU, et al.; COVID-CNSMDT
study group. Impact of COVID-19 pandemic on surgical neuro-oncology multi-disciplinary
team decision making: a national survey (COVID-CNSMDT Study). BMJ Open. 2020 Aug;10(8):e040898.
10.1136/bmjopen-2020-040898
46. Dannhoff G, Cebula H, Chibbaro S, Ganau M, Todeschi J, Mallereau CH, et al. Investigating
the real impact of COVID-19 pandemic on the daily neurosurgical practice? Neurochirurgie.
2021 Apr;67(2):99–103. 10.1016/j.neuchi.2021.01.009
47. Serafim RB, Póvoa P, Souza-Dantas V, Kalil AC, Salluh JI. Clinical course and outcomes
of critically ill patients with COVID-19 infection: a systematic review. Clin Microbiol
Infect. 2021 Jan;27(1):47–54. 10.1016/j.cmi.2020.10.017
48. Konstantinoudis G, Cameletti M, Gómez-Rubio V, Gómez IL, Pirani M, Baio G, et al. Regional
excess mortality during the 2020 COVID-19 pandemic in five European countries. Nat
Commun. 2022 Jan;13(1):482. 10.1038/s41467-022-28157-3