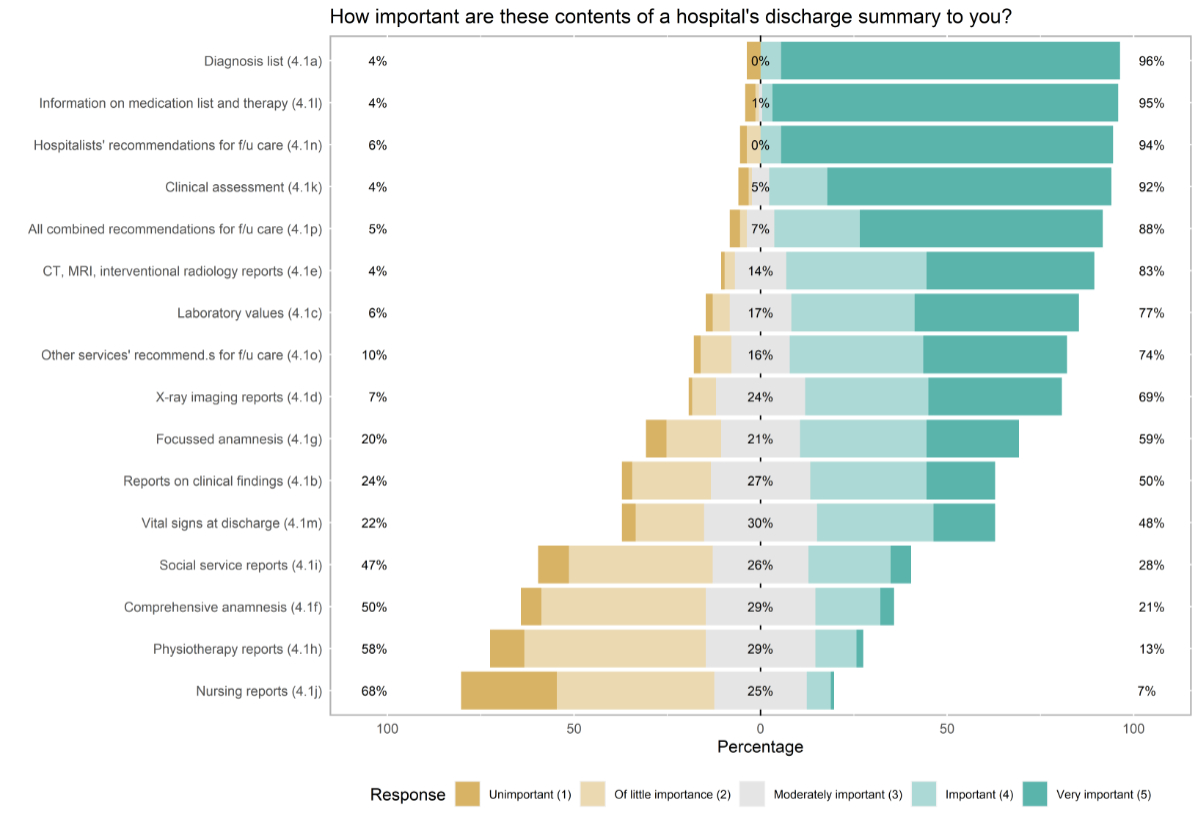
Figure 1Primary care physicians’ rating of the importance of included topics in the hospital’s discharge summary.
DOI: https://doi.org/https://doi.org/10.57187/s.3585
An increasing prevalence of multimorbidity in patients necessitates well-coordinated and timely information exchange among healthcare providers [1]. Hospitals must provide information regarding a patient’s health status, diagnosis, treatment, and medication to the primary care physicians (PCPs) who plan follow-up care. The absence of communication has contributed to an increase in emergency department visits and hospitalisations among patients [2]. Some studies have indicated that delayed or incomplete transfer of patient records can lead to missed or duplicate assessments and longer hospital stays [2–4]. However, high workloads, personnel shortages, and a lack of standardisation prevent healthcare professionals from communicating effectively [5, 6].
Digital tools are utilised to improve communication and information exchange among healthcare professionals. These tools aim to improve the efficiency and timeliness of information sharing and vary in their approach [7–9]. In Switzerland, the regulatory framework and conditions for healthcare system digitisation are currently being established [10, 11]. The Cantonal Hospital of Lucerne was the first to implement the Epic software system in a German-speaking country in 2019. Epic is widely adopted by large healthcare organisations and academic hospitals and is one of the leading electronic health record systems [9]. Before the introduction of the new portal, primary care physicians could define how they wanted to receive reports (e.g. discharge reports or surgery reports) from one of the following options: secured e-mail, InBasket messages, or letters. The primary care physicians’ preference, e-mail, was then incorporated. Before the software was launched, information events and workshops were held. The former was well attended by primary care physicians. If required or requested, personal training was provided in the primary care physician’s practice. The implementation in the cantonal hospital in Lucerne allows:
Understanding perceptions regarding technology utilisation, as well as its barriers and facilitators, may help enhance the experience and application of technology [15]. Therefore, this study aimed to provide insights into primary care physicians’ perceptions, satisfaction of the quality and the timeliness of regional hospitals’ communication in Central Switzerland, particularly in the canton of Lucerne. Secondarily, it assessed primary care physicians’ preferences of included topics in the hospitals’ discharge summaries, as well as the experiences with and utilisation of a regionally implemented electronic health record portal.
We performed an online survey of primary care physicians to assess their perceptions of the quality of communication with all regional hospitals and evaluate the role of an electronic health record portal in primary care. This cross-sectional study design aimed to identify perspectives of and possibilities for improvement in provider-to-provider communication. The reporting of this study followed the Checklist for Reporting Of Survey Studies (CROSS), which can be found in table S1 in the appendix 3 [16].
A structured questionnaire was specifically developed for this study and its setting, considering the literature on provider-to-provider communication. It was designed as an online survey using the Google Forms platform. The questionnaire was compiled using the literature and adding several questions of our own.
The questionnaire consists of 26 questions in five parts: (1) demographics and type of practice, (2) quality of communication, (3) information exchange and notifications, (4) discharge letter, and (5) software. All questions were closed-ended with multiple-choice answers. Satisfaction, preferences, levels of agreement, and frequencies were explored with items rated on a five-point Likert scale. For all Likert scales, a score of 1 was the lowest or most negative response, and a score of 5 was the highest or most positive response. Additionally, two free-text questions were included at the end of the survey to solicit improvement suggestions for communication between primary care physicians and hospitalists and to primary care physician portals. Responses were mandatory, except for items 5.2–5.4.
The target study population was primary care physicians practising in the canton of Lucerne. We sampled all 323 primary care physicians enlisted as members of the cantonal medical society in Lucerne, representing 97% of all primary care physicians in the canton, according to the respective office’s estimate. Lucerne is a German-speaking canton with roughly 400,000 inhabitants [17].
All primary care physicians practising in the canton of Lucerne received the link to the online survey via e-mail and could access it between 28 October 2021 and 7 January 2022. Reminder e-mails were sent to the primary care physicians one month and two months after the initial distribution.
This study did not require ethical approval according to Swiss law, and it conformed to the ethical review and research policies. Participants were informed about the study’s objectives in the introduction of the survey. Respondents provided electronic consent by agreeing to a consent paragraph before starting the survey. All responses were anonymous and confidential.
Data preparation, statistical analyses, and the creation of charts and tables were carried out using R version 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria). Table 1 and figure 1 were prepared using the R packages “tableone” (version 0.13.2) and “likert” (version 1.3.5), respectively. Categorical variables are presented as counts and percentages, and numerical variables with non-normal distributions are presented as medians and interquartile ranges (IQRs), where appropriate. In table 1, to compare primary care physicians stratified by age groups, chi-square tests were used for categorical variables, and the Kruskal-Wallis test was used for numerical variables. For numerical Likert item responses presented in the tables, the mean, median, statistical mode (response peak), fraction of the participants who responded, and all counts and proportions for each response are shown. In addition, potential associations between primary care physicians’ characteristics and responses were analysed by exploratory multivariable logistic regression models, reporting odds ratios (ORs) and 95% confidence intervals (CIs). For table 1 and the regression analyses, tertiles were considered a reasonable quantile to group the primary care physicians by age. The analysed dataset (except free text responses) is available as online supplementary material, and all models are published online alongside this article as supplementary tables (see appendices). A study protocol was not prepared.
Table 1Characteristics of surveyed primary care physicians.
| Aged 32–45 | Aged 47–58 | Aged 59–69 | p | Overall | ||
| n = 35 | n = 38 | n = 36 | n = 109 | |||
| Age, median (IQR) | 41 (37.50, 43) | 54 (52, 57) | 62 (61, 64.25) | <0.001 | 54 (43, 61) | |
| Females, n (%) | 19 (54) | 18 (47) | 10 (28) | 0.063 | 47 (43) | |
| Males, n (%) | 16 (46) | 20 (53) | 26 (72) | 0.063 | 62 (57) | |
| Years of experience, n (%) | <0.001 | |||||
| <1 year | 2 (6) | 0 (0) | 0 (0) | 2 (2) | ||
| 1–5 years | 14 (40) | 0 (0) | 0 (0) | 14 (13) | ||
| 5–10 years | 14 (40) | 9 (24) | 2 (6) | 25 (23) | ||
| 10–20 years | 5 (14) | 14 (37) | 2 (6) | 21 (19) | ||
| >20 years | 0 (0) | 15 (39) | 32 (89) | 47 (43) | ||
| Work in own practice, n (%) | 24 (69) | 33 (87) | 28 (78) | 0.17 | 85 (78) | |
| Primary care physicians working in practice, n (%) | 0.001 | |||||
| One | 2 (6) | 11 (29) | 12 (33) | 25 (23) | ||
| Two | 5 (14) | 13 (34) | 10 (28) | 28 (26) | ||
| Three or more | 28 (80) | 14 (37) | 14 (39) | 56 (51) | ||
| Location of practice, n (%) | 0.074 | |||||
| Urban | 5 (14) | 16 (42) | 15 (42) | 36 (33) | ||
| Suburban | 13 (37) | 12 (32) | 11 (31) | 36 (33) | ||
| Small town | 3 (9) | 4 (11) | 4 (11) | 11 (10) | ||
| Rural | 14 (40) | 6 (16) | 6 (17) | 26 (24) | ||
| Refer to hospital A, n (%) | 21 (60) | 27 (71) | 30 (83) | 0.093 | 78 (72) | |
| Refer to hospital B, n (%) | 17 (49) | 23 (61) | 24 (67) | 0.29 | 64 (59) | |
| Refer to hospital C, n (%) | 11 (31) | 7 (18) | 9 (25) | 0.437 | 27 (25) | |
| Refer to hospital D, n (%) | 7 (20) | 8 (21) | 9 (25) | 0.865 | 24 (22) | |
| Refer to hospital E, n (%) | 4 (11) | 4 (11) | 5 (14) | 0.9 | 13 (12) | |
| Refer to other hospitals, n (%) | 1 (3) | 2 (5) | 4 (11) | 0.343 | 7 (6) | |
| Use/are familiar with EpicCare Link, n (%) | 30 (86) | 30 (79) | 29 (81) | 0.741 | 89 (82) | |
The answers to the two free-text questions on improvement suggestions were analysed using thematic content analysis with MAXQDA 2022. Major themes answering the questions were coded deductively and summarised [18]. In the results, quotes were selected to illustrate common themes and provide context for the quantitative data.
A total of 109 primary care physicians completed the online survey, yielding a response rate of 34%. Table 1 presents the characteristics of respondents and their primary care practices. The mean age of the respondents was 54 years, and 57% were male. Roughly half of the primary care physicians (51%) worked in a group practice with three other primary care physicians or more. Most primary care physicians (81%) were familiar with the electronic health record portal.
Overall, half of the primary care physicians were satisfied or very satisfied with general communication with the hospital, including communication related to referrals (51%). Table 2 provides information about primary care physicians’ satisfaction with and frequency of communication with hospitals.
Table 2Primary care physicians’ answer distributions regarding satisfaction with and frequency of communication with hospitals.
| Question | Mean | Median | Statistical mode (peak) | Number of responses | Percent of total | Response | Number of responses | Proportion of who responded (%) | |
| 2.1 | In general, how satisfied are you with the communication between you/your practice and the hospital? | 3.3 | 4 | Satisfied (4) | 109 | 100 | Very dissatisfied (1) | 5 | 5 |
| Dissatisfied (2) | 19 | 17 | |||||||
| Neutral (3) | 30 | 28 | |||||||
| Satisfied (4) | 45 | 41 | |||||||
| Very satisfied (5) | 10 | 9 | |||||||
| 2.2 | How satisfied are you with communication when referring patients to the hospital? | 3.4 | 4 | Satisfied (4) | 109 | 100 | Very dissatisfied (1) | 4 | 4 |
| Dissatisfied (2) | 19 | 17 | |||||||
| Neutral (3) | 30 | 28 | |||||||
| Satisfied (4) | 39 | 36 | |||||||
| Very satisfied (5) | 17 | 16 | |||||||
| 3.4 | Hospitals must inform primary care physicians promptly (within 48 hours) about emergency admissions of their patients so that primary care physicians can help optimise care. | 4.2 | 4 | Strongly agree (5) | 109 | 100 | Strongly disagree (1) | 0 | 0 |
| Disagree (2) | 1 | 1 | |||||||
| Neutral (3) | 25 | 23 | |||||||
| Agree (4) | 37 | 34 | |||||||
| Strongly agree (5) | 46 | 42 | |||||||
| 3.1 | Regarding your patients, how often are you notified promptly (within 48 hours) by a hospital of an emergency admission (regardless of who referred the patient, incl. self-referral)? | 2.9 | 3 | Sometimes (3) | 109 | 100 | Never (1) | 14 | 13 |
| Rarely (2) | 30 | 28 | |||||||
| Sometimes (3) | 32 | 29 | |||||||
| Often (4) | 21 | 19 | |||||||
| Always (5) | 12 | 11 | |||||||
| 3.3 | How often do you contact the hospital when you learn that your patient just required emergency hospitalisation? | 2.4 | 2 | Rarely (2) | 109 | 100 | Never (1) | 11 | 10 |
| Rarely (2) | 51 | 47 | |||||||
| Sometimes (3) | 35 | 32 | |||||||
| Often (4) | 11 | 10 | |||||||
| Always (5) | 1 | 1 | |||||||
| 3.7 | How often are you notified by the hospital of your patients’ deaths in a timely manner (within 48 hours)? | 3.5 | 4 | Often (4) | 109 | 100 | Never (1) | 5 | 5 |
| Rarely (2) | 18 | 17 | |||||||
| Sometimes (3) | 26 | 24 | |||||||
| Often (4) | 41 | 38 | |||||||
| Always (5) | 19 | 17 | |||||||
| 2.3 | After completion of treatment/diagnosis/stay of your patients in a hospital, how often are you informed by the responsible hospital physicians? | 2.9 | 3 | Rarely (2) | 109 | 100 | Never (1) | 10 | 9 |
| Rarely (2) | 40 | 37 | |||||||
| Sometimes (3) | 23 | 21 | |||||||
| Often (4) | 28 | 26 | |||||||
| Always (5) | 8 | 7 | |||||||
Most primary care physicians (76%) agreed that they should be notified of patients’ emergency admissions within 48 hours. However, 40% of primary care physicians reported that they were never or rarely notified. Table S2 in the appendix 3 illustrates whether primary care physicians’ believed they were notified of such emergency admissions by regional hospitals. Regarding the communication channel, some primary care physicians wanted to be notified about emergency admissions with a short e-mail (40%), others with a detailed admission report sent via e-mail (39%), and a smaller proportion via an e-mail including a web link to the electronic health record portal (17%).
A total of 55% of primary care physicians reported that they preferred to receive an admission report within 48 hours of a patient’s admission, and 88% of primary care physicians reported that they preferred to receive a discharge report within 48 hours of discharge. After discharge, 33% of primary care physicians perceived that they were always or often informed by the hospital about a patient’s hospitalisation. Figure 1 depicts which content is most relevant to primary care physicians in discharge summaries.
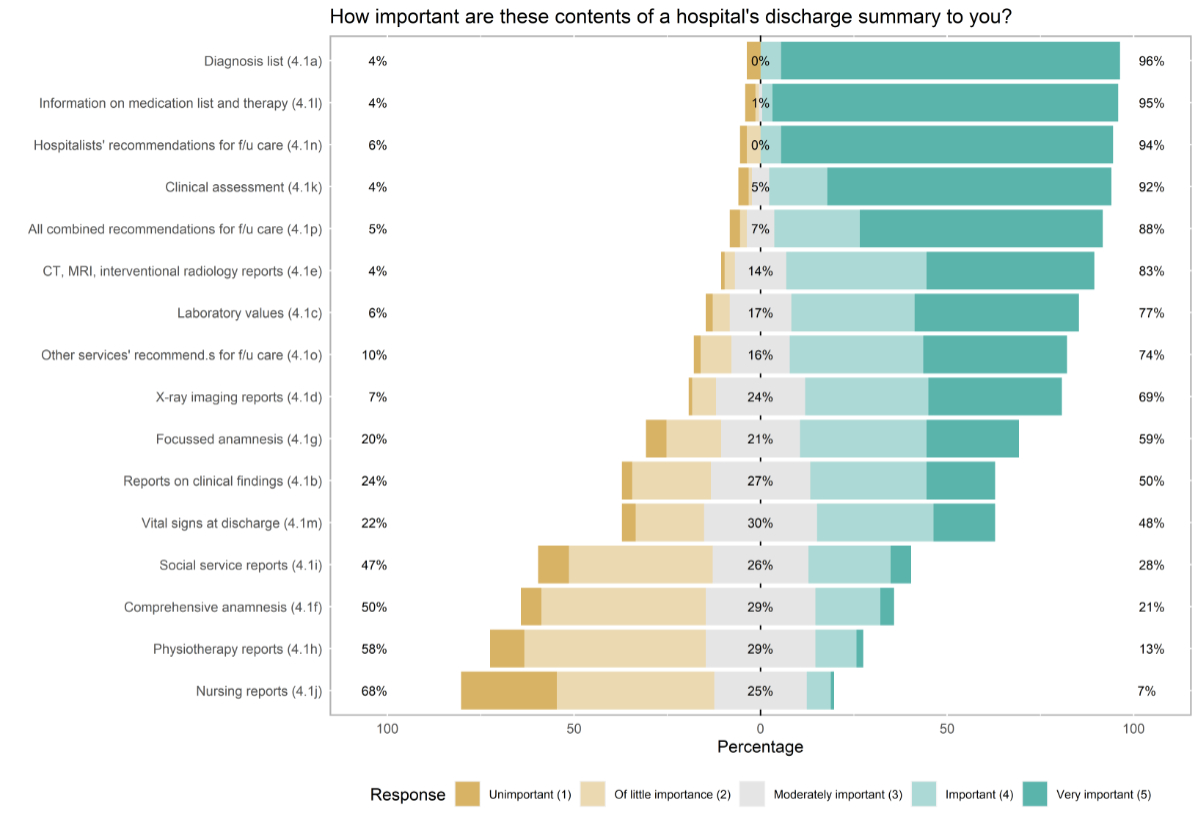
Figure 1Primary care physicians’ rating of the importance of included topics in the hospital’s discharge summary.
Table 3 provides information on the primary care physicians’ experiences using the electronic health record portal. The results showed that 82% of primary care physicians regularly retrieved hospital information from the electronic health record portal. Half of primary care physicians considered the portal useful for their patient management, and one-quarter disagreed. Most primary care physicians (81%) never used portals for patient referrals, and half of them would benefit from training on the use of the portal. The preferred learning methods were YouTube videos for self-study, suggested by 43% of primary care physicians; online training with an instructor, suggested by 37% of primary care physicians; and training with colleagues, suggested by 33% of primary care physicians.
Table 3Experiences with the electronic health record portal.
| Question | Mean | Median | Statistical mode (peak) | Number responses | Percent of total | Response | Number responses | Percentage of all who responded | |
| 5.2 | From your perspective as a primary care physician, the electronic health record portal has a positive influence on your patient management. | 3.3 | 4 | Agree (4) | 95 | 87 | Strongly disagree (1) | 10 | 11 |
| Disagree (2) | 14 | 15 | |||||||
| Neutral (3) | 21 | 22 | |||||||
| Agree (4) | 34 | 36 | |||||||
| Strongly agree (5) | 16 | 17 | |||||||
| 5.3 | The electronic health record portal is easy to use, and it provides information and patient data collected at the hospital in an appealing and useful way. | 2.8 | 3 | Agree (4) | 95 | 87 | Strongly disagree (1) | 13 | 14 |
| Disagree (2) | 26 | 27 | |||||||
| Neutral (3) | 25 | 26 | |||||||
| Agree (4) | 27 | 28 | |||||||
| Strongly agree (5) | 4 | 4 | |||||||
| 5.4 | How often do you use the electronic health record portal for patient referrals to the hospital? | 1.2 | 1 | Never (1) | 95 | 87 | Never (1) | 77 | 81 |
| Rarely (2) | 15 | 16 | |||||||
| Sometimes (3) | 2 | 2 | |||||||
| Often (4) | 0 | 0 | |||||||
| Always (5) | 1 | 1 | |||||||
| 5.5 | The electronic health record portal requires a sound introduction with training opportunities as well as an offer of regular information, e.g. on innovations. | 3.5 | 3 | Neutral (3) | 109 | 100 | Strongly disagree (1) | 3 | 3 |
| Disagree (2) | 14 | 13 | |||||||
| Neutral (3) | 38 | 35 | |||||||
| Agree (4) | 34 | 31 | |||||||
| Strongly agree (5) | 20 | 18 | |||||||
Regression showed that female primary care physicians were likely not to work in their own practice (OR 0.15; 95% CI 0.04–0.50) and not in a rural setting (OR 0.19; 95% CI 0.04–0.70). Consistent with these findings, male primary care physicians were associated with the 59–69 age group (OR 4.94; 95% CI 1.44–18.92), and they were more likely to work in their own practice (OR 6.72; 95% CI 2.02–25.67) and in a rural setting (OR 5.22; 95% CI 1.43–22.32). When analysing associations with urban practices, regression showed that older primary care physicians, namely those in the 47–58 age group (OR 5.65; 95% CI 1.74–21.19) and 59–69 age group (OR 6.61; 95% CI 1.95–26.02), tended to work in urban settings, independent of sex, whether they worked in their own practice, and the number of primary care physicians working there.
Regarding preferred communication channels, regression revealed that the channel group phone, fax, or postal mail was significantly associated with the 47–58 age group (OR 7.24; 95% CI 1.46–55.59) and 59–69 age group (OR 6.31; 95% CI 1.18–50.86).
Regression revealed an independent, statistically significant association indicating that the 59–69 age group did not find the electronic health record portal easy to use (OR 0.17; 95% CI 0.03–0.77). In addition, primary care physicians working in their own practice were not associated with group trainings (OR 0.24; 95% CI 0.06–0.84).
Free-text answers provided insights into primary care physicians’ suggestions for improving information exchange. Some primary care physicians wished that hospitalists increased contact via phone, such as for “occasional calls for complex problems” (PCP90) or “calls about admission and discharge from the ward’s case manager to the primary care physician” (PCP98). Regarding the electronic health record portal, primary care physicians suggested user-friendliness improvements: “Ideally, the interface allows you to highlight and drag text from the documents into our patient records or to import images into our database without downloading beforehand.” (PCP61) Furthermore, some primary care physicians suggested a decrease in complexity by providing a better overview or visibility of relevant information. “Improve clarity and make it more user-friendly. How do I find laboratories’ results? […] Is a chronological order of information not possible?” (PCP70) Other suggestions highlighted the primary care physicians’ need for update notifications in patients’ electronic health records, as illustrated by the following quote: “An automatic, clearly visible notification about new messages or changes to the patient’s record from the electronic health record portal to my computer is necessary” (PCP54).
This study examined how primary care physicians perceive communication and information exchange between primary care physician practices and hospitals in the canton of Lucerne. Overall, primary care physicians were satisfied with communication in general and specifically for referrals. However, they reported that information provided after patients’ hospitalisation, discharge, or death is not provided in a timely manner by hospitals. Primary care physicians requested that they be notified of their patients’ emergency hospitalisation within 48 hours via e-mail. In discharge summaries sent within 48 hours, primary care physicians expect information on the diagnosis, medication and therapies, clinical assessments, and hospitalists’ recommendations for follow-up care.
The self-reported data obtained from this survey suggest a selective utilisation of the regionally implemented electronic health record portal. A high proportion of primary care physicians deemed the electronic health record portal beneficial for their patient management, specifically for retrieving patient information. However, almost none of the primary care physicians reported using the electronic health record portal for patient referrals. User friendliness seems to be the main barrier to the portal’s utilisation, and opportunities for self-study or group trainings could support primary care physicians.
In our study, primary care physicians reported a lack of timely information from hospitals about patients’ emergency admissions, deaths, and discharges, which aligns with the existing literature.
Our study did not evaluate the effect on patient care, but notifications to primary care physicians about emergency encounters have been shown to play a vital role in maintaining continuity of care [19]. However, encounter notifications may vary in the amount of information provided to primary care physicians and the communication channel [20, 21]. Most of our primary care physicians seemed satisfied with a simple e-mail notification of a patient’s admission. Several primary care physicians requested that the reason for the encounter be included in the notification. Although the older primary care physicians surveyed preferred non-electronic communication channels, they reported mainly using e-mail. It appears that e-mail has become the accepted communication channel in Swiss primary care, as even in 2010, 80% of primary care physicians in a survey reported using email for communication [11].
Similar to our findings, several studies have reported issues with discharge summaries. The findings of Kripilani et al. demonstrated that receiving discharge summaries significantly influenced primary care physician satisfaction [22]. Weetman et al. listed several reasons for unsatisfactory discharge letters, such as incomplete and insufficient information, unclear follow-up plans, delayed letter delivery, and inadequate medication information [23]. For the most part, our primary care physicians had uniform expectations about the contents of a discharge letter and its timeliness. Electronic discharge summaries are implemented in several European countries, and they may mitigate the lack of timely information transfer between providers [6] and increase primary care physician satisfaction [24].
Despite the perceived benefits of using the electronic health record portal, primary care physicians seemed to encounter challenges in utilisation. A qualitative study from the Italian-speaking part of Switzerland identified the availability of complete patient documentation as one of the main challenges in using electronic health records [25]. Primary care physicians in our study reported a confusing data architecture, and it appears that they have difficulty finding relevant information. According to similar studies, electronic health record portals may lack intuitive navigation [15, 26, 27]. Price et al. conducted an evaluation of the Epic system in an emergency department setting and concluded that it requires adaptation to physicians’ workflows, following extensive training [9]. In their review, O’Donnell and colleagues identified challenges in adapting to new digital workflows and a lack of necessary training, especially among older primary care physicians [28]. Consistently, the older primary care physician age groups in our study requested self-study material for using the regionally implemented electronic health record portal. Lastly, studies have reported that the large number of InBasket messages from electronic health record portals no longer help simplify communication; rather, they are overwhelming for everyday clinical practice [29]. As part of the electronic health record portal, which is the subject of this study, primary care physicians are informed by email about unread InBasket messages if they are one of the following four specific message types: Community Messages, Employee Messages, Patient Files, or New Patient Event Monitor. For all other information about their patients, primary care physicians do not receive separate e-mail notifications (e.g. emergency admission to hospital). Instead, primary care physicians must log in to check whether new InBasket messages have arrived.
The limitations of our study must be considered in the interpretation of the results and their implications. Our study sample was restricted to primary care physicians practising in the canton of Lucerne, Central Switzerland, limiting the generalisability of our findings. However, we achieved a relatively high response rate and reached a broad variety of primary care physicians in terms of demographics and locations. The sample’s characteristics are representative of primary care physicians in this region. Since the survey was disseminated by e-mail, the primary care physicians’ preference to be notified via this channel may be biased; however, this preference is in line with preferences reported in the literature. Finally, although three regional hospitals provide patient information electronically on a specific electronic health record portal for primary care physicians, other regional hospitals may offer different solutions not investigated by this study. As our data were collected in 2022, this study might not reflect the most recent developments in electronic information exchange. However, we believe that any changes since the time of data collection can be considered negligible.
This study provides valuable insights into primary care physicians’ perceptions and expectations for provider-to-provider communication. The suggestions for improving communication, information exchange, and the electronic health record portal’s user-friendliness provide opportunities to strengthen the local healthcare system and ensure continuity of care for patients. To our knowledge, this is the first study conducted in a German-speaking country to assess primary care physicians’ perceptions of this electronic health record portal (EpicCare Link).
Primary care physicians provided their expectations for timely communication and the content of discharge summaries: the diagnosis list, information on medications and therapies, and hospitalists’ recommendations for follow-up care. This information may be used to develop standardised templates for discharge summaries.
This study includes specific suggestions for electronic health record portals from the perspective of primary care physicians. The results showed that older primary care physicians were more likely to use non-digital channels for their information exchange and did not find the electronic health record portal easy to use. Although this finding is not surprising, measures to make benefits more apparent and digital tools easier to use should be developed, as this age group of primary care physicians currently comprise a large part of all primary care physicians. Regarding electronic health record portals, research on log files could provide beneficial information about utilisation; hospitals and software developers should understand how their tools are used to improve them. Lastly, we published the results of a similar survey from the perspective of the hospitals; a comparison of the results reveals interesting differences in perceptions of information exchange and should open discussions between the two user groups [30].
Half of primary care physicians were satisfied with communication with regional hospitals. We identified room for improvement regarding timely notifications on emergency admissions, deaths, and discharges. Primary care physicians valued the regionally implemented electronic health record portal for patient management but offered suggestions to enhance user-friendliness.
The (a) questionnaire used, (b) data collected (with data dictionary), and (c) additional tables are available as online supplementary materials (see appendices).
The R code of this study is available from the corresponding author upon reasonable request.
We would like to thank all physicians who participated in this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003 Aug;18(8):646–51. doi: https://doi.org/10.1046/j.1525-1497.2003.20722.x
2. Murtagh S, McCombe G, Broughan J, Carroll Á, Casey M, Harrold Á, et al. Integrating Primary and Secondary Care to Enhance Chronic Disease Management: A Scoping Review. Int J Integr Care. 2021 Feb;21(1):4. doi: https://doi.org/10.5334/ijic.5508
3. Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ. 2017 Feb;356:j84. doi: https://doi.org/10.1136/bmj.j84
4. Sheehan J, Laver K, Bhopti A, Rahja M, Usherwood T, Clemson L, et al. Methods and Effectiveness of Communication Between Hospital Allied Health and Primary Care Practitioners: A Systematic Narrative Review. J Multidiscip Healthc. 2021 Feb;14:493–511. doi: https://doi.org/10.2147/JMDH.S295549
5. Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015 Nov;69(11):1257–67. doi: https://doi.org/10.1111/ijcp.12686
6. Luu NP, Pitts S, Petty B, Sawyer MD, Dennison-Himmelfarb C, Boonyasai RT, et al. Provider-to-Provider Communication during Transitions of Care from Outpatient to Acute Care: A Systematic Review. J Gen Intern Med. 2016 Apr;31(4):417–25. doi: https://doi.org/10.1007/s11606-015-3547-4
7. Gagnon MP, Légaré F, Labrecque M, Frémont P, Pluye P, Gagnon J, et al. Interventions for promoting information and communication technologies adoption in healthcare professionals. Cochrane Database Syst Rev. 2009 Jan;2010(1):CD006093. doi: https://doi.org/10.1002/14651858.CD006093.pub2
8. Holmgren AJ, Adler-Milstein J. Health Information Exchange in US Hospitals: The Current Landscape and a Path to Improved Information Sharing. J Hosp Med. 2017 Mar;12(3):193–8. doi: https://doi.org/10.12788/jhm.2704
9. Price C, Kwok ES, Cheung WJ, Thiruganasambandamoorthy V, Clapham G, Nemnom MJ, et al. Physician experience with the Epic electronic health record (EHR) system: longitudinal findings from an emergency department implementation. CJEM. 2022 Sep;24(6):630–5. doi: https://doi.org/10.1007/s43678-022-00354-5
10. Zürcher Hochschule für Angewandte Wissenschaften (ZHAW). Digital Health Report 21/22. 2021. Available from: https://www.zhaw.ch/storage/hochschule/medien/news/2021/210914-digital-health-report-2021.pdf
11. Rosemann T, Marty F, Bhend H, Wagner J, Brunner L, Zoller M. Utilisation of information technologies in ambulatory care in Switzerland. Swiss Med Wkly. 2010 Sep;140(3738):w13088. doi: https://doi.org/10.4414/smw.2010.13088
12. Reich J, Canakis A, Shankar D, Harrington J, Apte M, Weinberg J, et al. The Use of An EHR Patient Portal (Mychart-Epic) in Patients With Inflammatory Bowel Disease. Crohns Colitis 360. 2019 Oct;1(3):otz039. doi: https://doi.org/10.1093/crocol/otz039
13. Hwang AB, Schuepfer G, Pietrini M, Boes S. External validation of EPIC’s Risk of Unplanned Readmission model, the LACE+ index and SQLape as predictors of unplanned hospital readmissions: A monocentric, retrospective, diagnostic cohort study in Switzerland. Provenzano M, editor. PLOS ONE. 2021 Nov 12;16(11):e0258338. https://doi.org/
14. Cross DA, McCullough JS, Banaszak-Holl J, Adler-Milstein J. Health information exchange between hospital and skilled nursing facilities not associated with lower readmissions. Health Serv Res. 2019 Dec;54(6):1335–45. doi: https://doi.org/10.1111/1475-6773.13210
15. Eden KB, Totten AM, Kassakian SZ, Gorman PN, McDonagh MS, Devine B, et al. Barriers and facilitators to exchanging health information: a systematic review. Int J Med Inform. 2016 Apr;88:44–51. doi: https://doi.org/10.1016/j.ijmedinf.2016.01.004
16. Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med. 2021 Oct;36(10):3179–87. doi: https://doi.org/10.1007/s11606-021-06737-1
17. Bundesamt für Statistik. Luzern. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/regionalstatistik/regionale-portraets-kennzahlen/kantone/luzern.html
18. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14. doi: https://doi.org/10.1016/j.npls.2016.01.001
19. Afilalo M, Lang E, Léger R, Xue X, Colacone A, Soucy N, et al. Impact of a standardized communication system on continuity of care between family physicians and the emergency department. CJEM. 2007 Mar;9(2):79–86. doi: https://doi.org/10.1017/S1481803500014834
20. Dixon BE, Embi PJ, Haggstrom DA. Information technologies that facilitate care coordination: provider and patient perspectives. Transl Behav Med. 2018 May;8(3):522–5. doi: https://doi.org/10.1093/tbm/ibx086
21. Gutteridge DL, Genes N, Hwang U, Kaplan B, GEDI WISE Investigator T, Shapiro J. GEDI WISE Investigator T, Shapiro J. Enhancing a Geriatric Emergency Department Care Coordination Intervention Using Automated Health Information Exchange-Based Clinical Event Notifications. EGEMS (Wash DC). 2014 Aug;2(3):6. doi: https://doi.org/10.13063/2327-9214.1095
22. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007 Feb;297(8):831–41. doi: https://doi.org/10.1001/jama.297.8.831
23. Weetman K, Spencer R, Dale J, Scott E, Schnurr S. What makes a “successful” or “unsuccessful” discharge letter? Hospital clinician and General Practitioner assessments of the quality of discharge letters. BMC Health Serv Res. 2021 Apr;21(1):349. doi: https://doi.org/10.1186/s12913-021-06345-z
24. O’Leary KJ, Liebovitz DM, Feinglass J, Liss DT, Evans DB, Kulkarni N, et al. Creating a better discharge summary: improvement in quality and timeliness using an electronic discharge summary. J Hosp Med. 2009 Apr;4(4):219–25. doi: https://doi.org/10.1002/jhm.425
25. Centemero NS, Rechel B. Barriers and facilitators to a health information exchange system between general practitioners and hospitals: a qualitative study in Southern Switzerland. Swiss Med Wkly. 2021 Oct;151(4142):w30063. doi: https://doi.org/10.4414/SMW.2021.w30063
26. Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform. 2009 Jan;78(1):22–31. doi: https://doi.org/10.1016/j.ijmedinf.2008.06.005
27. Ajami S, Bagheri-Tadi T. Barriers for Adopting Electronic Health Records (EHRs) by Physicians. Acta Inform Med. 2013;21(2):129–34. doi: https://doi.org/10.5455/aim.2013.21.129-134
28. O’Donnell A, Kaner E, Shaw C, Haighton C. Primary care physicians’ attitudes to the adoption of electronic medical records: a systematic review and evidence synthesis using the clinical adoption framework. BMC Med Inform Decis Mak. 2018 Nov;18(1):101. doi: https://doi.org/10.1186/s12911-018-0703-x
29. Fogg JF, Sinsky CA. In-Basket Reduction: A Multiyear Pragmatic Approach to Lessen the Work Burden of Primary Care Physicians. NEJM Catal. 2023 Apr;4(5). doi: https://doi.org/10.1056/CAT.22.0438
30. Käufeler M, Beeler PE, Müller LS, Gemperli A, Merlo C, Hug BL. Hospitalists’ perception of their communication with primary care providers - survey results from six hospitals in Central Switzerland. Swiss Med Wkly. 2024 Jul;154(7):3643. doi: https://doi.org/10.57187/s.3643
The appendices are available for download as separate files at https://doi.org/10.57187/s.3585.