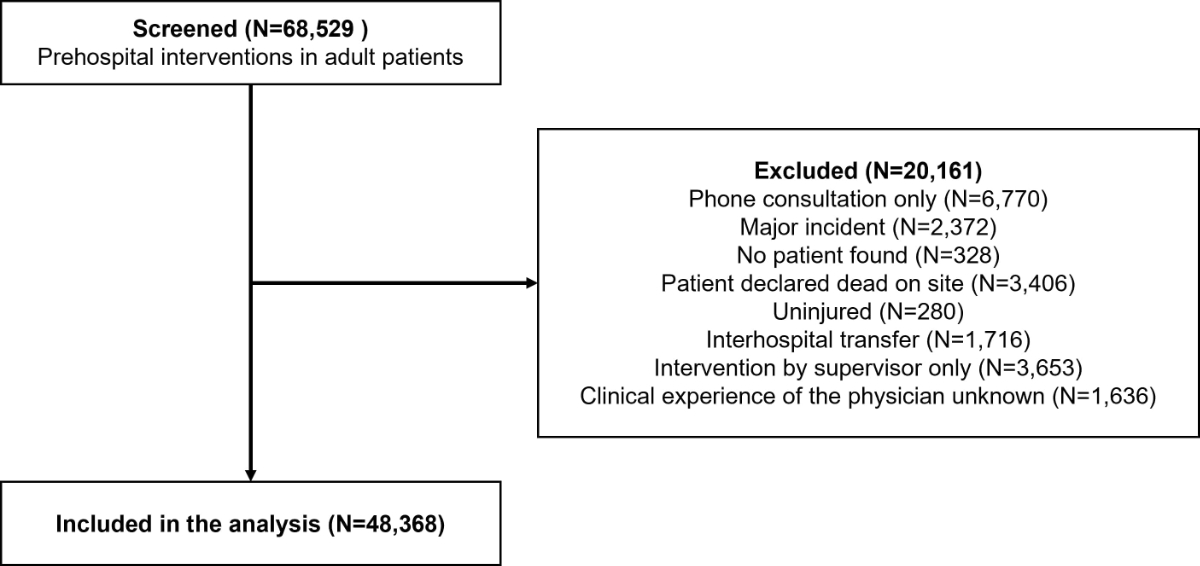
Figure 1Flowchart of patient inclusion.
DOI: https://doi.org/https://doi.org/10.57187/s.3533
The clinical experience and expertise of prehospital providers vary according to the regional setting [1, 2]. Prehospital physicians can help improve patient outcomes in several cases, such as cardiac arrests [3] and polytrauma [4]. In addition to these specific outcomes, a specialised medical evaluation can be helpful when making appropriate clinical and medicolegal decisions [5]. The impact of these decision-making skills has already been demonstrated in several other settings, including radiological exam prescription[6], futility assessment [7], readmission [8] and mortality [9]. The appropriateness of these decisions and the magnitude of their impact are affected by clinical experience [10]. This also holds true in the prehospital setting, where the impact of clinical experience has been demonstrated on critical outcomes such as endotracheal intubation success rates [1]. The impact of clinical experience on the probability of discharging patients at scene has been little studied. Our hypothesis was that experienced prehospital physicians should be more likely to discharge patients at scene since they should be more confident in their clinical evaluation skills. Therefore, our objective was to determine whether the discharge at scene rate was associated with clinical experience.
This retrospective cohort study was carried out in the prehospital unit of HUG (Hôpitaux universitaires de Genève, Geneva University Hospitals) [11]. In Geneva, a single emergency medical call centre receives all medical emergency calls arising from the canton, totalling more than 68,000 calls per year [12]. The response is decided according to an evaluation performed by professional emergency medical dispatchers, most of whom are either nurses or former paramedics. Mobile medical units (Service mobile d’urgence et de reanimation [SMUR]) are dispatched whenever emergency medical dispatchers identify life-threatening emergencies, along with an advanced life support ambulance. These ambulances are staffed by two paramedics who graduated after a 3-year curriculum [13]. Alternatively, paramedics can request backup by an SMUR unit, either to help with a difficult clinical condition or to resolve a problematic medicolegal situation. Physicians working in these SMUR units have different levels of clinical experience and most of them are residents in the middle or at the end of their training. Since there is no emergency medicine residency programme in Switzerland, these residents mostly come from internal medicine and anaesthesia departments [14]. A senior prehospital specialist physician provides both remote and on-scene supervision around the clock. After each intervention, a computerised medical file is filled in by the prehospital physician. These files are reviewed by supervisors on a daily basis for teaching and quality control purposes [11].
After assessing the patient and initiating prehospital treatment if necessary, SMUR physicians have three options: accompany the patient in the ambulance; hand the patient over to paramedics; or discharge the patient at scene. Discharged patients are usually uninjured patients, those not requiring further investigations and those who can be referred to their general practitioner or to an outpatient medical centre. There are also less-obvious reasons underlying non-transport decisions (such as advance care planning or refusal by patient with preserved decision-making capacity). Physicians can also choose to discharge patients at scene when further treatment is deemed futile, even in the presence of a life-threatening condition, provided that there are sufficient resources on site to cope with the situation. There are no protocols or standardised operating procedures to guide prehospital physicians, and these decisions are made based on clinical judgement alone.
The analysis included all prehospital files reporting interventions in which an SMUR unit attended to an adult patient (i.e. aged 18 years or over) between 1 January 2010 and 31 December 2019. It excluded: phone consultations; major incidents with multiple casualties; interventions in which patients were uninjured, were not found or died at the scene; and secondary interventions (inter-hospital transfers). Interventions performed by senior specialist physicians only were also excluded since these supervisors are usually only dispatched if a regular SMUR unit is unavailable, and dispatch criteria are therefore more restrictive in such cases. Finally, interventions carried out by a physician whose level of experience could not be determined were also excluded.
The study was conducted at Geneva University Hospitals in accordance with Good Clinical Practice (Declaration of Helsinki 2002). It was approved on 27 August 2020 by the institutional ethics committee of Geneva, Switzerland (Project ID 2020-01807). Patient consent was waived by this committee.
The main exposure was the clinical experience of the prehospital physician at the time of the intervention, in number of years since graduation.
The main outcome was the rate of discharge at scene. This information was prospectively collected for all patients as part of the administrative data required to validate the prehospital file. Secondary outcomes were the rates of handover to paramedics (non-medicalised transportation) and of supervised interventions. All these variables are mandatory fields in the prehospital files.
Other variables collected were patient age and sex, time and place of intervention, main pathology, vital signs and severity status as a NACA (National Advisory Committee for Aeronautics) score [15] assessed at the scene by the SMUR physician with paramedics. Severely ill patients were defined as patients with a NACA ≥4. These values are also reviewed by the supervisors and corrected if necessary.
The data used for this study are publicly available on the Open Science Framework (OSF, https://www.doi.org/10.17605/OSF.IO/STPQY).
Patient characteristics and outcomes were analysed using descriptive statistics. Then interventions performed by physicians with experience of less than 1 year or greater than 15 years were excluded as they were performed by an extremely low number of physicians who were thus considered outliers. Restricted cubic splines (5 knots) were used to obtain a graphical representation of associations. This allowed us to determine that the linearity assumption was not meaningfully violated. Mixed-effect logistic regression with a random intercept on physicians was used to study the association between clinical experience and outcomes, adjusting for patient’s sex and age, night and weekend interventions, illness severity and physician’s sex. We reported odds ratios (OR) and their 95% confidence intervals (CI). To test for a potential modification according to illness severity, we added an interaction between level of experience and illness severity in our model. The rationale for this analysis was that leaving patients at scene because treatment was either refused by the patient or considered futile by the physician (higher NACA scores) does not require the same skill set as declining transport when further medical investigation or treatment in the emergency department (ED) are deemed unnecessary (lower NACA scores). Missing data were reported and treated as such. The primary and secondary outcomes are all mandatory fields and must be recorded to validate the prehospital files. Therefore, there could be no missing values for these outcomes.
Two prespecified sensitivity analyses were performed for the main outcome. First, supervised interventions were excluded because the presence of a supervisor can markedly influence transportation decisions. Second, a dichotomisation was performed on the exposure, with two different cut-offs (three years and five years).
Analyses were performed using Stata 17.0 (StataCorp, College Station, TX, USA).
During the research period, 68,529 prehospital interventions involving adult patients were performed (figure 1). A total of 20,161 interventions were excluded. The three main reasons for exclusion were phone consultations (n = 6770), interventions performed by supervisors alone (n = 3653) and interventions in which patients were declared dead at scene (n = 3406). Hence 48,368 interventions were included in the analysis.
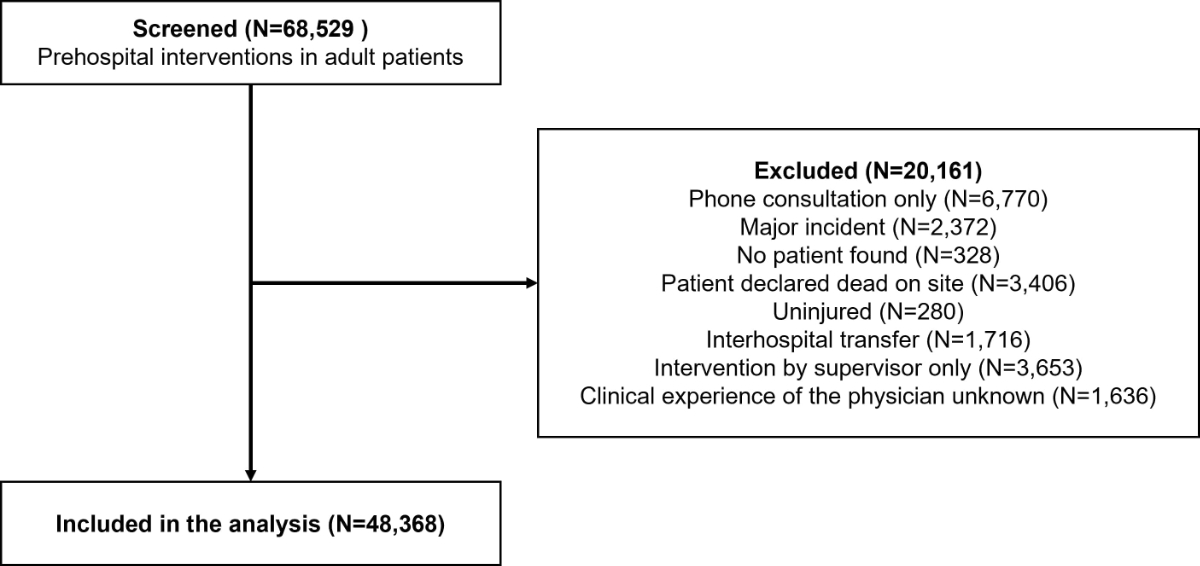
Figure 1Flowchart of patient inclusion.
The interventions were performed by 219 different physicians, 181 (82.7%) of whom graduated from a medical school in Switzerland and 118 (53.9%) of whom were male. The mean level of experience at the time of intervention was 5.2 years (standard deviation [SD]: 3.3), and the median was 4.6 (interquartile range [IQR]: 3.4–6.0). The median number of interventions by physician was 193 (IQR: 139–281).
Table 1 presents the characteristics of the patients. Patients were mostly male (54.4%) and had a mean age of 62.2 years (SD: 21.2). Most interventions took place at the patient’s home (63.1%). Night interventions were less frequent (40.0%) and patients were predominantly severely ill (68.5%). A total of 1234 (2.6%) interventions were performed by physicians with a level of experience less than 1 year (745 interventions by 3 physicians) or greater than 15 years (489 interventions by 2 physicians).
Table 1Patient characteristics.
| Overall (n = 48,368) | ||
| Male – n (%) | 26,337 (54.5%) | |
| Age (years) – mean±SD | 62.2 ± 21.2 | |
| Intervention site – n (%) | Home | 30,497 (63.1%) |
| Public place | 11,310 (23.4%) | |
| Healthcare place | 6561 (13.6%) | |
| Intervention periode | Weekend– n (%) | 12,668 (73.8%) |
| Night – n (%) | 19,333 (40.0%) | |
| Heart rate (/min) – mean ± SD | 94 ± 28 | |
| Missing | 3318 (6.5%) | |
| Systolic blood pressure (mm Hg) – mean ± SD | 139 ± 31 | |
| Missing | 4193 (8.7%) | |
| Respiratory rate (/min) – mean ± SD | 21.9 ± 8.4 | |
| Missing | 6485 (13.4%) | |
| Oxygen saturation (%) – median [IQR] | 97% [94–99%] | |
| Missing | 4086 (8.5%) | |
| Glasgow coma scale – n (%) | 15 | 23,904 (48.4%) |
| <15 | 11,415 (23.6%) | |
| Missing | 13,049 (27.0%) | |
| Pathology – n (%) | Medical | 41,234 (85.2%) |
| Traumatic | 5796 (12.0%) | |
| Cardiac arrest | 962 (2.0%) | |
| Missing | 376 (0.8%) | |
| NACA – n (%) | 1 | 793 (1.6%) |
| 2 | 3264 (6.8%) | |
| 3 | 11,175 (23.1%) | |
| 4 | 24,996 (51.8%) | |
| 5 | 6970 (14.4%) | |
| 6 | 1087 (2.3%) | |
| Missing | 83 (0.2%) | |
The outcomes are presented in table 2. The overall discharge at scene rate was 7.8%. This rate differed widely between physicians (median: 7.3%, IQR: 5.5–9.1), including among physicians with a similar level of experience.
Table 2Outcomes.
| Overall – n (%) | ||
| Main outcome | Discharge at scene | 3794 (7.84%) |
| Secondary outcomes | Handover to paramedics* | 15,560 (34.9%) |
| Supervision | 6184 (12.8%) | |
* Only applies to transported patients. Those who were discharged at scene were excluded.
After adjusting for potential confounders, there was no association between level of experience and discharge at scene (table 3). There was an effect by severe illness (p for interaction = 0.003): the association was slightly stronger for severely ill patients (adjusted OR [aOR]: 1.06 [95% CI: 0.98–1.03]) than for non-severely ill patients (aOR: 1.02 [95% CI: 1.02–1.10]). In our sensitivity analyses, level of experience was not associated with discharge at scene when supervised interventions were excluded (aOR: 1.02 [95% CI: 0.99–1.04]) or when level of training was dichotomised at three years (aOR: 0.96 [95% CI: 0.83–1.11]) or five years (aOR: 1.02 [95% CI: 0.92–1.13]).
Table 3Multivariable regression models for each outcome.
| Discharge at scene | Handover to paramedics | Supervision | ||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Level of experience (years)* | 1.01 (0.98–1.03) | 1.17 (1.13–1.21) | 0.85 (0.82–0.88) | |
| Severely ill** | 0.06 (0.05–0.07) | 0.02 (0.02–0.02) | 1.40 (1.19–1.64) | |
| Interaction*** | 1.06 (1.02–1.10) | 1.06 (1.03–1.09) | 1.02 (0.99–1.05) | |
| Patient sex | Male | Ref. | Ref. | Ref. |
| Female | 1.11 (1.03–1.20) | 1.15 (1.09–1.22) | 0.85 (0.80–0.90) | |
| Patient age (10 y) | 1.02 (1.01–1.04) | 1.06 (1.05–1.07) | 0.81 (0.80–0.82) | |
| Weekend intervention | 1.09 (1.01–1.18) | 1.05 (0.99–1.12) | 0.95 (0.89–1.01) | |
| Night intervention | 1.26 (1.17–1.35) | 1.09 (1.03–1.15) | 0.74 (0.70–0.78) | |
| Physician sex | Male | Ref | Ref | Ref |
| Female | 0.95 (0.85–1.06) | 0.92 (0.72–1.17) | 1.05 (0.93–1.19) | |
* Level of experience was modelled as a linear variable, therefore the ORs represent the change by one additional year of experience.
** Severely ill patients were defined as those having a NACA ≥4.
*** The interaction coefficient indicates how much the effect of experience depended on the severity of the illness.
The rate of handover to paramedics was 34.9% and was associated with level of clinical experience (aOR: 1.17 [95% CI: 1.13–1.21]) (table 3). It differed according to illness severity (p for interaction <0.001): the association was stronger for severely ill patients (aOR: 1.27) than for non-severely ill patients (aOR: 1.06). There was no major change when supervised interventions were excluded (aOR: 1.17 [95% CI: 1.14–1.20]), but the association was stronger when level of training was dichotomised at three years (aOR: 1.51 [95% CI: 1.24–1.85]) or five years (aOR: 1.66 [95% CI: 1.43–1.92]).
Finally, the rate of supervision was 12.8%. Level of clinical experience was associated with supervision (aOR: 0.85 [95% CI: 0.82–0.88]) (table 3). This association did not differ according to illness severity (p for interaction = 0.290).
The associations are graphically presented in figure 2. Discharge at scene and handover to paramedics seem to increase with experience while supervision seems to decrease.
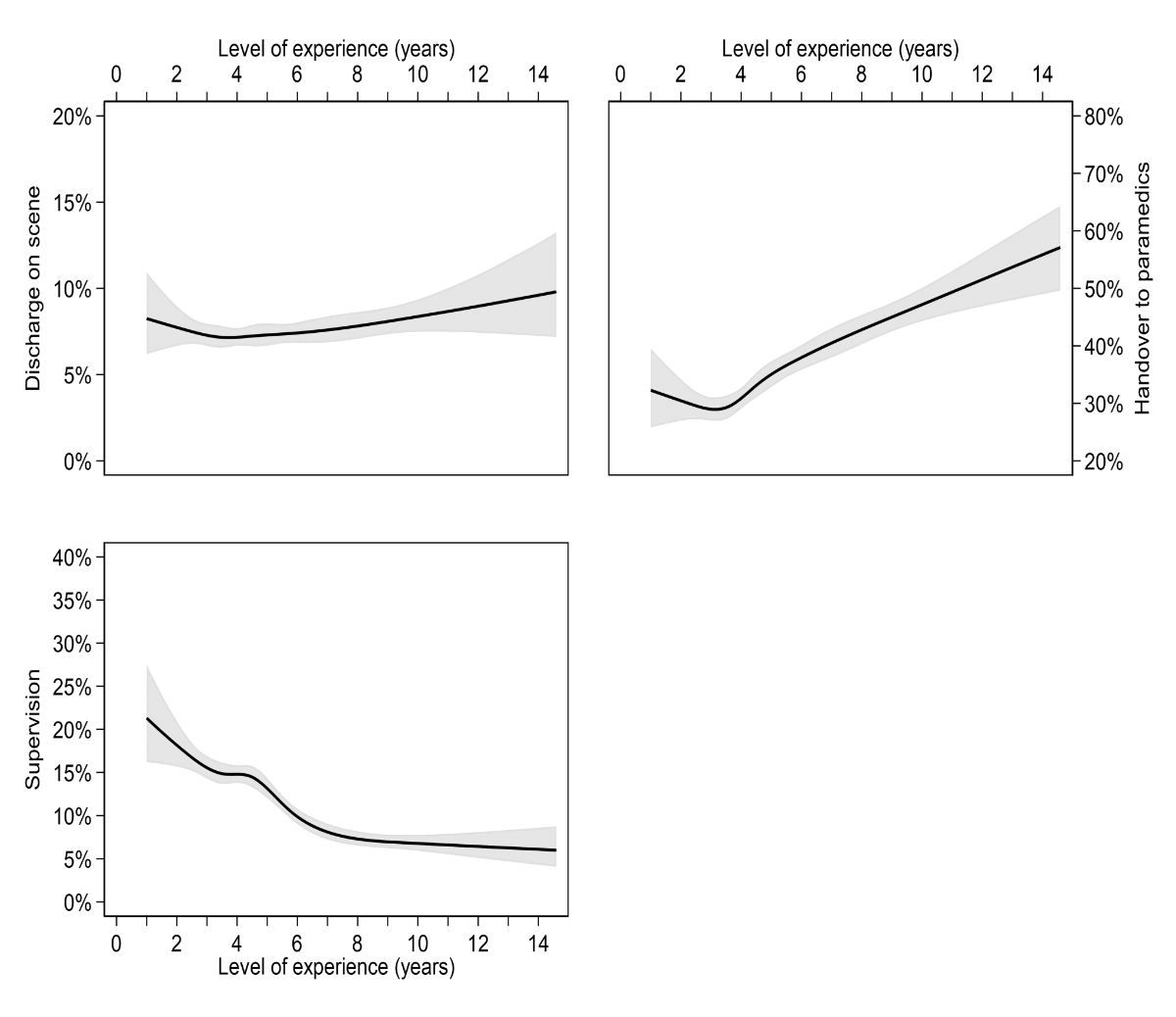
Figure 2Associations between level of clinical experience and outcomes, modelled using restricted cubic splines and logistic regression.
In this retrospective study, clinical experience was significantly associated with patient disposition and supervision outcomes. Even though an association between level of experience and overall discharge at scene rate could not be proved, a trend was seen on the graphical representation in figure 2. Experienced physicians were also more likely to discharge severely ill patients at the scene.
Assessing the factors influencing patient disposition in the prehospital setting is of particular importance since prehospital resources are not always allocated appropriately in spite of the progressive improvement of dispatching procedures. In 2020, a prospective observational study showed that approximately 20% of patients evaluated by a nurse in the prehospital setting are ultimately discharged at scene [16]. While we were unable to identify other prehospital articles studying the effect of clinical experience of prehospital physicians on disposition, similar results were obtained by studies conducted in non-physician-staffed prehospital systems [17–20]. Therefore, the experience of paramedics might have acted as an unmeasured confounder in this study, but any difference should have been smoothed by the sheer number of interventions analysed as there is no relation between the experiences of the physician and the paramedic teams dispatched by the emergency medical call centre.
The association between illness severity and patient disposition is of particular importance. There may be many reasons to choose not to transport severely ill patients, among which patient refusal and futility are paramount [21]. In case of acute illness, patients may refuse transportation either because of a prior informed decision or because of an acute lack of decision-making capacity [22]. Experienced clinicians should be able to determine more readily the reason behind such a refusal than their younger colleagues [23], thereby allowing them to take more relevant decisions and preserve patient autonomy [24].
Experienced physicians were more likely to hand patients over to paramedics (figure 2), even when they were more severely affected. Three hypotheses could explain this phenomenon. First, by virtue of their more thorough clinical knowledge, experienced physicians might feel more confident in their ability to predict patient evolution [25]. Second, these physicians should have more comprehensive knowledge of the skills and aptitudes of paramedics and be more confident in their ability to manage expected or unexpected events which may arise during transport[26]. The rate of handover to paramedics followed a U-shaped curve, with the lowest rates reported among physicians with approximatively 3 years of clinical experience. The early drop may be related to a waning of the Dunning-Kruger effect, while the later rise is probably the result of increased confidence in the abilities of paramedics. Finally, since many physicians with a high level of experience also work as ED registrars, their decisions regarding patient disposition may be affected by their concern to prevent ED overcrowding.
Supervision rates were affected by clinical experience but generally remained higher than 10% regardless of the level of experience. These rather high rates are easily explained by the specificities of the prehospital setting [27], which even otherwise experienced clinicians might not be used to. In addition, physicians who are considered as experienced in some fields might still require assistance in managing specific conditions seldom encountered in their usual practice (e.g. airway management procedures). Enabling these physicians to call upon the help of senior prehospital specialists has been shown to allow high endotracheal intubation success rates [28]. Finally, supervision enabled the physicians with lower level of clinical experience to achieve discharge at scene rates similar to those obtained by their more experienced colleagues. While it could be argued that there would be less need for supervision if only highly experienced physicians operated in the prehospital setting, it should be acknowledged that prehospital rotations have been shown to help senior residents acquire important non-technical skills, such as leadership and communication [14].
Some limitations must be acknowledged, especially regarding the main variable. First, using years since graduation as an exposure may not be optimal for defining experience, as the postgraduate curriculum often differs from one physician to another [29]. And although strong methods were used to assess the date of graduation of each physician, this study was retrospective so inaccuracies cannot be ruled out, especially for physicians who graduated abroad. Moreover, our method did not allow us to take into account the unlikely but conceivable possibility that some physicians took long leaves of absence or undertook several months of non-clinical activity. In addition, prior knowledge of the regional setting could also act as a confounder. However, this effect should be minimal as both beginners and more advanced physicians could perform their first prehospital rotation in this setting. Similarly, emergency medical dispatcher performance may have influenced our results, as less experienced emergency medical dispatchers may have overtriaged. Nevertheless, the schedule of SMUR physicians is totally independent to that of the emergency medical dispatchers, and any such effect should have been smoothed, particularly when considering the rather broad timeframe of this study. Another limitation is that even though the increased proportion of patients handed over to paramedics was considered suitable, the retrospective design of the study prevented us from determining whether paramedics felt comfortable transporting these patients, and prospective studies assessing this outcome should therefore be considered. At the same line, we must also acknowledge that the appropriateness of the decisions, which would have been an interesting outcome, was not assessed in the course of this study because of the many potential confounders which can hardly be determined by means of a retrospective study. Finally, while the overall level of experience seems similar to some other settings [30], an important number of prehospital medical units are staffed with more-experienced physicians, and the generalisation to such systems should be done with caution.
Despite these limitations, this study also has some strengths, among which the high quality of the data and the high number of cases could be cited. The fact that different analyses were carried out using the main exposure both as a categorical and continuous variable reinforces the internal validity of our study.
The impact of clinical experience on patient disposition in the prehospital setting deserves further study. Prospective trials should now be designed to determine whether prehospital disposition decisions are safe and appropriate. Such studies should also assess the parameters experienced clinicians take into account when assessing futility. In the meantime, prehospital systems employing less-experienced clinicians could aim to reinforce their supervision mechanisms to support their decision-making processes.
In this retrospective study, there was no association between the level of experience and the overall rate of discharge at scene. However, greater clinical experience was associated with higher rates of handover to paramedics and lower supervision rate. Further studies are required to determine whether such decisions are taken adequately and their impact on patient outcomes such as mortality.
The protocol has not been published and is not publicly accessible. The data that support the findings are publicly available on the Open Science Framework (OSF, https://www.doi.org/10.17605/OSF.IO/STPQY).
Authors’ contributions: Conceptualisation: R Betend, L Suppan, M Chan, S Regard, F Sarasin, CA Fehlmann. Data curation: R Betend, CA Fehlmann. Formal analysis: CA Fehlmann. Investigation: R Betend, L Suppan, M Chan, CA Fehlmann. Methodology: CA Fehlmann. Project administration: L Suppan, CA Fehlmann. Supervision: L Suppan, CA Fehlmann. Visualiszation: R Betend, CA Fehlmann. Writing – original draft: R Betend, CA Fehlmann. Writing – review and editing: R Betend, L Suppan, M Chan, S Regard, F Sarasin, CA Fehlmann.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Bossers SM, Schwarte LA, Loer SA, Twisk JW, Boer C, Schober P. Experience in prehospital endotracheal intubation significantly influences mortality of patients with severe traumatic brain injury: A systematic review and meta-analysis. PLoS One. 2015 Oct;10(10):e0141034. 10.1371/journal.pone.0141034
2. Crewdson K, Lockey DJ, Røislien J, Lossius HM, Rehn M. The success of pre-hospital tracheal intubation by different pre-hospital providers: a systematic literature review and meta-analysis. Crit Care. 2017 Feb;21(1):31. 10.1186/s13054-017-1603-7
3. Goto Y, Funada A, Goto Y. Impact of prehospital physician-led cardiopulmonary resuscitation on neurologically intact survival after out-of-hospital cardiac arrest: A nationwide population-based observational study. Resuscitation. 2019 Mar;136:38–46. 10.1016/j.resuscitation.2018.11.014
4. Fukuda T, Ohashi-Fukuda N, Kondo Y, Hayashida K, Kukita I. Association of prehospital advanced life support by physician with survival after out-of-hospital cardiac arrest with blunt trauma following traffic collisions Japanese registry-based study. JAMA Surg. 2018 Jun;153(6):e180674. 10.1001/jamasurg.2018.0674
5. Schmutz T, Guechi Y, Gendre G, Ariosa J, Ribordy V. [SMUR or not SMUR?]. Rev Med Suisse. 2021 Aug;17(746):1367–9. 10.53738/REVMED.2021.17.746.1367
6. Young GJ, Flaherty S, Zepeda ED, Mortele KJ, Griffith JL. Effects of Physician Experience, Specialty Training, and Self-referral on Inappropriate Diagnostic Imaging. J Gen Intern Med. 2020 Jun;35(6):1661–7. 10.1007/s11606-019-05621-3
7. Neville TH, Wiley JF, Holmboe ES, Tseng CH, Vespa P, Kleerup EC, et al. Differences between attendings’ and fellows’ perceptions of futile treatment in the intensive care unit at one academic health center: implications for training. Acad Med. 2015 Mar;90(3):324–30. 10.1097/ACM.0000000000000617
8. Glette MK, Kringeland T, Røise O, Wiig S. Exploring physicians’ decision-making in hospital readmission processes - a comparative case study. BMC Health Serv Res. 2018 Sep;18(1):725. 10.1186/s12913-018-3538-3
9. Chen TM, Chang TM, Huang PT, Tsai MH, Lin LF, Liu CC, et al. Management and patient survival in hepatocellular carcinoma: does the physician’s level of experience matter? J Gastroenterol Hepatol. 2008 Jul;23(7 Pt 2 7pt2):e179–88. 10.1111/j.1440-1746.2008.05341.x
10. Kirby R, Robinson RD, Dib S, Mclarty D, Shaikh S, Cheeti R, et al. Emergency Medicine Resident Efficiency and Emergency Department Crowding. Runde DP, editor. AEM Educ Train. 2019 Jul 27;3(3):209–17. 10.1002/aet2.10327
11. Gartner BA, Fehlmann C, Suppan L, Niquille M, Rutschmann OT, Sarasin F. Effect of noninvasive ventilation on intubation risk in prehospital patients with acute cardiogenic pulmonary edema: a retrospective study. Eur J Emerg Med. 2020 Feb;27(1):54–8. 10.1097/MEJ.0000000000000616
12. Chappuis VN, Deham H, Cottet P, Gartner BA, Sarasin FP, Niquille M, et al. Emergency physician’s dispatch by a paramedic-staffed emergency medical communication centre: sensitivity, specificity and search for a reference standard. Scand J Trauma Resusc Emerg Med. 2021 Feb;29(1):31. 10.1186/s13049-021-00844-y
13. Schmutz T, Guechi Y, Denereaz S, Ozainne F, Nuoffer M, Exadaktylos A, et al. Paramedics in Switzerland: A Mature Profession. Int J Environ Res Public Health. 2022 Jul;19(14):8429. 10.3390/ijerph19148429
14. Suppan L, Chan M, Gartner B, Regard S, Campana M, Chatellard G, et al. Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey. Healthcare (Basel). 2020 Dec;9(1):24. 10.3390/healthcare9010024
15. Weiss M, Bernoulli L, Zollinger A. Der NACA-Index. Anaesthesist. 2001 Mar;50(3):150–4. 10.1007/s001010170030
16. Magnusson C, Herlitz J, Axelsson C. Patient characteristics, triage utilisation, level of care, and outcomes in an unselected adult patient population seen by the emergency medical services: a prospective observational study. BMC Emerg Med. 2020 Jan;20(1):7. 10.1186/s12873-020-0302-x
17. Jensen JL, Travers AH, Bardua DJ, Dobson T, Cox B, McVey J, et al. Transport outcomes and dispatch determinants in a paramedic long-term care program: a pilot study. CJEM. 2013 Jul;15(4):206–13. 10.2310/8000.2012.120965
18. van der Pols H, Mencl F, de Vos R. The impact of an emergency motorcycle response vehicle on prehospital care in an urban area. Eur J Emerg Med. 2011 Dec;18(6):328–33. 10.1097/MEJ.0b013e32834624e8
19. O’Cathain A, Jacques R, Stone T, Turner J. Why do ambulance services have different non-transport rates? A national cross sectional study. Gabbe BJ, editor. PLoS One. 2018 Sep 21;13(9):e0204508.
20. Tohira H, Williams TA, Jacobs I, Bremner A, Finn J. The impact of new prehospital practitioners on ambulance transportation to the emergency department: a systematic review and meta-analysis. Emerg Med J. 2014 Oct;31 e1:e88–94. 10.1136/emermed-2013-202976
21. Follette C, Halimeh B, Chaparro A, Shi A, Winfield R. Futile trauma transfers: an infrequent but costly component of regionalized trauma care. J Trauma Acute Care Surg. 2021 Jul;91(1):72–6. 10.1097/TA.0000000000003139
22. ERBAY H. Some Ethical Issues in Prehospital Emergency Medicine. Turk J Emerg Med. 2014 Dec;14(4):193–8. 10.5505/1304.7361.2014.32656
23. Hermann H, Trachsel M, Mitchell C, Biller-Andorno N. Medical decision-making capacity: knowledge, attitudes, and assessment practices of physicians in Switzerland. Swiss Med Wkly. 2014 Oct;144:w14039. 10.4414/smw.2014.14039
24. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997 Mar;44(5):681–92. 10.1016/S0277-9536(96)00221-3
25. Çalis M, Sener K, Kaya A, Sari S, Polat M, Yolcu S. The prediction levels of emergency clinicians about the outcome of the ambulance patients and outpatients. Am J Emerg Med. 2020 Jul;38(7):1463–5. 10.1016/j.ajem.2020.02.050
26. Smith MW, Bentley MA, Fernandez AR, Gibson G, Schweikhart SB, Woods DD. Performance of experienced versus less experienced paramedics in managing challenging scenarios: a cognitive task analysis study. Ann Emerg Med. 2013 Oct;62(4):367–79. 10.1016/j.annemergmed.2013.04.026
27. Wilson MH, Habig K, Wright C, Hughes A, Davies G, Imray CH. Pre-hospital emergency medicine. Lancet. 2015 Dec;386(10012):2526–34. 10.1016/S0140-6736(15)00985-X
28. Chan M, Fehlmann CA, Pasquier M, Suppan L, Savoldelli GL. Endotracheal Intubation Success Rate in an Urban, Supervised, Resident-Staffed Emergency Mobile System: An 11-Year Retrospective Cohort Study. J Clin Med. 2020 Jan;9(1):238. 10.3390/jcm9010238
29. Elstad EA, Lutfey KE, Marceau LD, Campbell SM, von dem Knesebeck O, McKinlay JB. What do physicians gain (and lose) with experience? Qualitative results from a cross-national study of diabetes. Soc Sci Med. 2010 Jun;70(11):1728–36. 10.1016/j.socscimed.2010.02.014
30. Bollinger M, Mathee C, Shapeton AD, Thal SC, Russo SG. Differences in training among prehospital emergency physicians in Germany. Notf Rettmed. 2022;25(S2 Suppl 2):23–30. 10.1007/s10049-022-01021-z