Figure 1Study flowchart.
DOI: https://doi.org/https://doi.org/10.57187/s.3515
Healthcare access is crucial in maintaining good health and a high quality of life [1]. In Switzerland, mandatory health insurance ensures basic healthcare coverage for every resident [2]. This system is supported by the Federal Office of Public Health (FOPH), whose missions include promoting and ensuring equitable healthcare access for all residents of Switzerland [3].
As in many other countries [4], population ageing implies the growing healthcare needs of an older population [5]. As individuals age, the prevalence of chronic conditions and the incidence of acute health events tend to increase [6], resulting in a higher demand for healthcare services. This raises questions about individuals’ ability to meet their healthcare needs. Specifically, individuals may face challenges in recognising and seeking appropriate treatments as well as in the self-management of their health conditions, which can lead to poor health outcomes, unnecessary healthcare use and spending. In Switzerland, general practitioners are an important resource for the population as they are essential in providing primary care [7]. As highlighted in a survey of 1201 general practitioners in Switzerland, these professionals are integral to patients’ end-of-life experiences, maintaining family connections and serving as liaisons for coordinated care among fellow physicians [8]. Additionally, a study involving 1154 general practitioners and their patients in Switzerland emphasised the dedicated role of general practitioners in preventive care. Both general practitioners and patients acknowledged this significance [9].
Individuals’ ability to assess their healthcare needs and to find, understand and utilise health-related information and services to maintain their health in the best condition is commonly referred to as health literacy [10]. Subjective instruments measuring health literacy aim to capture a comprehensive health literacy assessment in the general population, encompassing individuals’ capacities to seek, comprehend, evaluate and utilise health-related information in their daily lives [11]. The latter argument is particularly relevant in the context of effective healthcare consumption since the population’s self-perception of their health literacy could potentially influence their decision concerning healthcare use. For instance, an incorrect evaluation of personal health needs could lead to incorrect healthcare utilisation.
Poor health literacy has been linked to poor health behaviours and unfavourable health outcomes; some examples include suboptimal adherence to physical activity guidelines [12], poor medication management [13] and lower levels of preventive care use [14]. Moreover, some previous cross-sectional studies found a significant negative association between health literacy and healthcare utilisation [15–18]. Other examples include cross-sectional studies focusing on the North American population, which found that low health literacy was associated with higher rates of healthcare use [19], higher use of emergency departments and higher frequency of medical consultations [20]. Similar research was also conducted in European countries, which generally showed that low levels of health literacy are associated with a higher frequency of doctor consultations among the German population [21] and greater use of health services in Italy [22]. Previous studies in Switzerland were generally limited to specific population groups rather than looking at broader population strata. For example, one study found that immigrants in Switzerland with lower health literacy levels had higher healthcare use [23]. Further examples include a study on individuals with multimorbidity, revealing a positive association between limited health literacy and an increased treatment burden [24], and another study focusing on people with diabetes found that elevated levels of health literacy corresponded to reduced medical costs and fewer medical visits [25]. Our research complements the existing literature by providing evidence on the association between health literacy and healthcare utilisation in the older population in Switzerland based on a population-based national sample of adults aged 58 and older. In addition, this paper adds to the literature on health literacy using data from the Survey of Health, Aging and Retirement in Europe (SHARE). Previous research on the subject found that older adults with low health literacy are more likely to suffer from multiple chronic diseases [26], and that certain population groups are particularly vulnerable due to inadequate health literacy levels. Specifically, men and individuals with low education, financial difficulties or poor self-assessed health status were at a higher risk of inadequate health literacy [27].
To the best of our knowledge, to date there have been no studies exploring the complex association between health literacy and healthcare utilisation in the general older adult population in Switzerland. Understanding this relationship could provide important insights for policymakers to optimise healthcare access for the increasingly ageing population. For instance, understanding the direction of this relationship could help assess whether individuals with lower health literacy are limited in their healthcare access or, conversely, exhibit propensities for excessive healthcare utilisation. In either case, the findings of this study hold promise in shedding light on this intricate relationship, thus assisting policymakers in identifying necessary interventions to ensure equitable access to the entire population and, ultimately, cultivate a healthier society.
Importantly, better health literacy could enable individuals to make more efficient decisions regarding their usage of healthcare [28]. By empowering individuals with better tools to improve their health literacy, the older population might become more efficient in their healthcare choices and consumption as well as in their proactive preventive behaviours.
This paper aims to close the aforementioned gap in the literature and shed light on the association between individuals’ health literacy and healthcare utilisation. Specifically, we focus on the relationship between health literacy and the number of consultations with general practitioners and healthcare specialists within a sample of the older Swiss population (58+ years). This study serves as an important progression in aligning healthcare supply and demand with the varying health literacy levels of older adults, ultimately promoting more effective and equitable healthcare access.
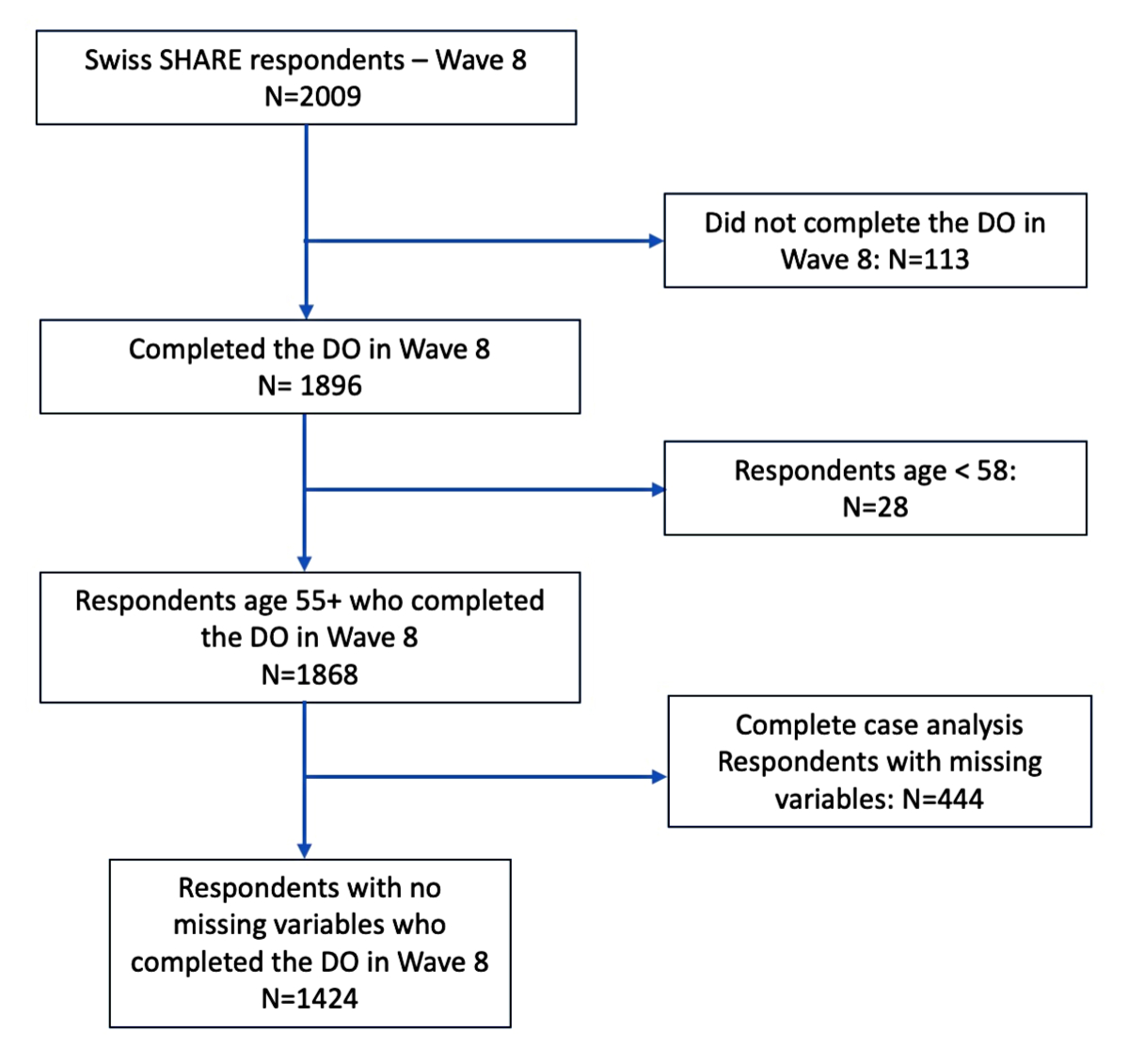
We used cross-sectional data from SHARE (Survey of Health, Aging and Retirement in Europe), a longitudinal study conducted every two years starting from 2004 [29]. SHARE collects comprehensive information on the health, socioeconomic status and social networks of individuals aged 50 and above in 28 European countries and Israel. The survey employs computer-assisted personal interviews as the primary data collection method, supplemented by country-specific paper-and-pencil drop-off questionnaires. The Swiss SHARE sample of wave 8 (October 2019 to March 2020) included 2009 participants who were either targeted respondents or their partners. Among them, 1896 individuals completed the drop-off questionnaire, which included an assessment of respondents’ subjective health literacy [29], resulting in a conditional completion rate of 94.4%. However, it is important to note that our study focused solely on respondents aged 58 or older. As the most recent refreshment sample for SHARE Switzerland occurred in 2011, survey participants aged 50 to 58 in 2019/2020 could only enter SHARE as partners of target respondents and they are therefore not representative of the general population aged 50–58. After excluding 28 individuals aged below 58 and 444 with one or more missing answers on the outcome, exposure variables or covariates, our final analysis sample consisted of 1424 participants (figure 1).
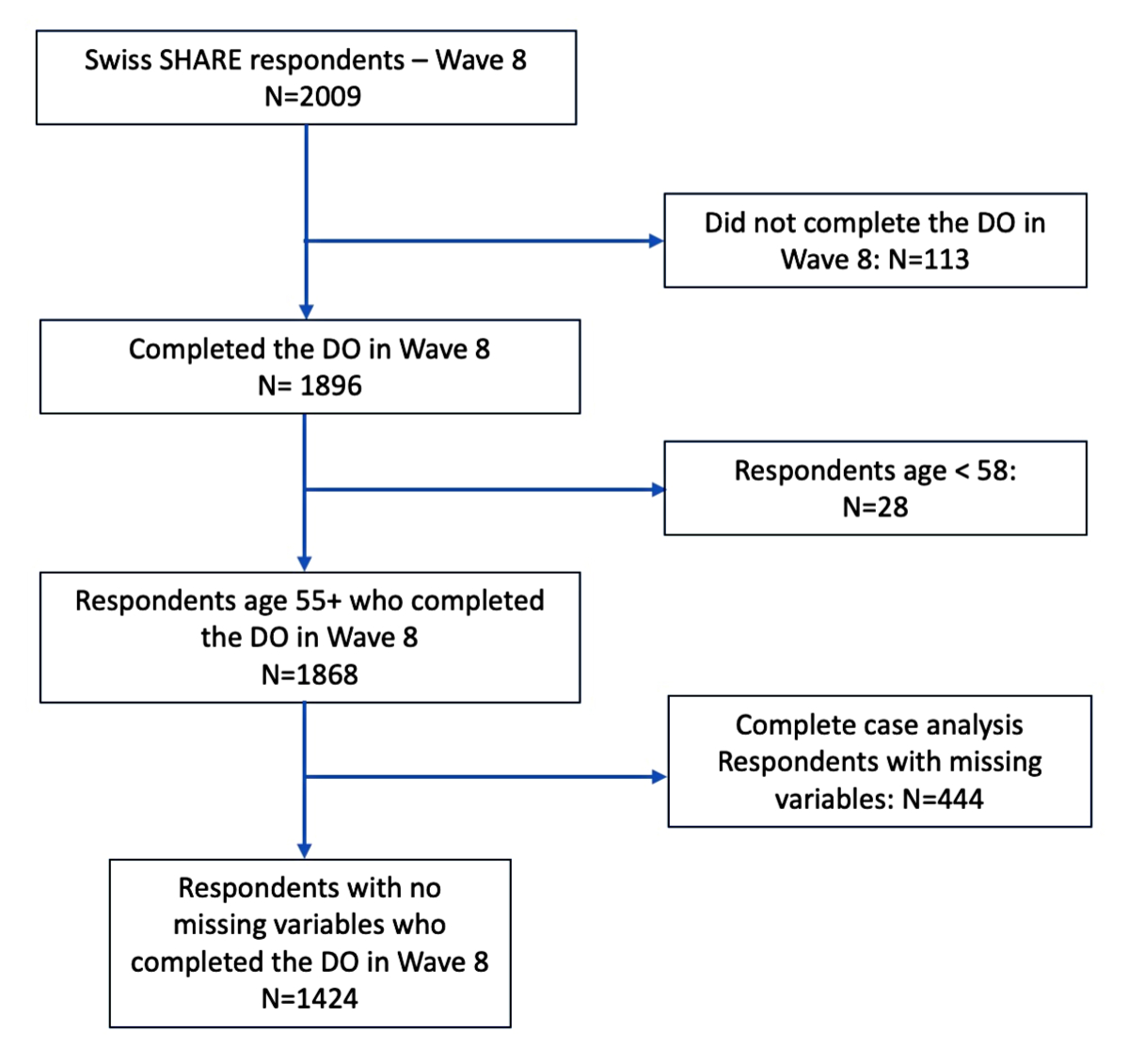
Figure 1Study flowchart.
Our analysis uses two primary outcome variables: the reported number of consultations with general practitioners and the reported number of consultations with healthcare specialists in the year prior to the interview. During the main interview, respondents were asked how many times in the 12 months prior to the interview they had been in contact with a medical doctor and/or a qualified nurse for reasons related to their health. Furthermore, they were asked to specify how many of these contacts were with a general practitioner or a doctor at their healthcare centre, and how many were with a specialist, excluding dentists and emergency visits [29]. Healthcare specialists include, among others, ophthalmologists, gynaecologists, cardiologists, psychiatrists, rheumatologists, orthopaedists, ear, nose and throat (ENT) specialists, geriatricians, neurologists, gastroenterologists and radiologists [29].
Our main exposure variable is a subjective measure of health literacy, measured with the HLS-EU-Q16. The drop-off questionnaire administered in Switzerland included the short version of the European Health Literacy Survey questionnaire, which was developed by the HLS-EU consortium [30]. This scale comprises 16 items, which are listed in table S1 in the appendix, covering various aspects of health literacy. For example, measurements include respondents’ self-perceived difficulties in finding information on treatments, comprehending medical advice, making informed health decisions and assessing the reliability of health-related information from different sources, such as doctors, media and family members. Respondents were asked to rate each item on a 4-point Likert scale, with response options ranging from “very easy” to “very difficult” [31]. To simplify the analysis, the answers were dichotomised as follows: “fairly difficult” and “very difficult” were assigned a value of 0 while “very easy” and “fairly easy” were assigned a value of 1. Based on the methodology employed in previous research [27], if the overall number of item non-responses did not exceed two, missing item values were imputed as 0, and only respondents with no more than two missing values on the items were included in the final health literacy score [27]. The development of the HLS-EU-Q16 underwent a rigorous process, which relied on Item Response Theory and Rasch Analysis [30]. Furthermore, previous research by our research group within the same study population demonstrated excellent internal consistency for the entire health literacy scale, as indicated by a Cronbach’s alpha of 0.91 [32]. The resulting health literacy score ranged from 0 to 16 and was categorised as inadequate (0–8), problematic (9–12) or sufficient (13–16) [27]. Both continuous scores and categorised variables are used in our analysis.
In the present study, the selection of key covariates – including sociodemographic, regional and health-related variables – was mainly informed by the findings of a prior publication [27], which assessed the association between social, regional and health characteristics and health literacy levels within the same sample of older adults living in Switzerland. These covariates included sex (male or female) and age group, classified into three categories: 58–64 years, 65–74 years and 75+ years. Education levels were grouped into three categories (low, medium, high) based on the International Standard Classification of Education (ISCED) of 2017 [33]. Partnership status was measured with a binary variable indicating whether individuals had a partner or not, accounting for all types of partnerships. To assess the subjective financial situation of households, respondents were asked about their capacity to cover essential expenses with their income. This was measured through a question on their “ability to make ends meet”, where respondents could indicate whether they manage their financial obligations “easily”, “fairly easily” or “with difficulty”. The language respondents used to answer the questionnaire (German, French, Italian) served as a proxy for capturing regional and cultural differences, and the variable indicating respondents’ living area was dichotomised as either urban or rural. Furthermore, a set of health-related control variables was included. These variables include limitations in activities of daily living and the count of chronic conditions (0, 1, 2, 3+) measured in SHARE. Limitations in activities of daily living follow the established definition put forth by Katz [34, 35].
We used unweighted number counts to assess the frequencies of all variables in our analysis sample; from these, we obtained the socioeconomic and health-related characteristics of our sample. We examined the distribution of the number of general practitioner and specialist consultations for each level of health literacy (inadequate, problematic, sufficient) and compared medians across groups with Kruskal-Wallis tests. As the distribution of both outcome variables suggests the presence of overdispersion (variance larger than the mean) and heteroscedasticity (unequal dispersion of residuals), multivariable analysis was performed using generalised Poisson regression models. The atanh-delta (hyperbolic tangent of the delta) constant parameter resulting from the generalised Poisson regression model confirms the presence of overdispersion. This modelling approach offers flexibility in accounting for various dispersion patterns, as it does not assume a specific distribution for the random component that connects the mean and variance [36]. Average marginal effects with their corresponding standard errors were calculated to examine the partial associations between health literacy (continuous and categorical variables) and healthcare utilisation. For the continuous health literacy score, the average marginal effects represent the average difference in the expected number of general practitioner or specialist visits for every one-point increase in the health literacy score, keeping all other covariates constant. When examining the levels of health literacy, the average marginal effects indicate the average difference in the expected number of general practitioner or specialist visits when comparing inadequate or problematic levels to the reference level (sufficient), holding all other covariates constant.
The standard errors are clustered at the household level to account for linear dependencies among respondents from the same household participating in the SHARE study. Statistical analyses were conducted using STATA/SE 17.0 (STATA Corporation, College Station, TX, USA). Two-sided p-values <0.05 were considered statistically significant.
Our study obtained ethical approval number 66/14 from the ethics committee of the canton of Vaud, Switzerland, in March 2014. Informed consent was obtained from all individual participants included in the study.
Table 1 presents descriptive statistics of the 1424 respondents who comprise our study sample. The proportion of men in our sample was 46.9%. The age distribution of the respondents was as follows: 41.1% were aged between 65 and 74 years, 35.3% were 75 years or older and the remaining 23.7% were between 58 and 64 years old. The majority of the sample had a secondary education level (62.6%), whereas 19.9% had a tertiary education level and 17.6% had a low education level. Three quarters (74.7%) of the sample reported being in a relationship. Concerning their subjective financial situation, 54.9% reported that they were able to make ends meet easily, 31.8% fairly easily and 13.3% with difficulty, which indicates some financial challenges among some respondents. The majority of respondents resided in rural areas (53.4%), with the remaining 46.6% living in urban areas. Furthermore, the majority of respondents were from the German-speaking part of Switzerland (70.2%), while 26.9% were from the French-speaking part and 2.9% were from the Italian-speaking region. Regarding health, 25.7% of the respondents reported having no chronic diseases, 31.8% reported having one chronic disease, 22.3% reported having two chronic diseases and 20.6% reported having three or more chronic diseases. Additionally, 92.5% of respondents reported living without limitations in their activities of daily living.
Table 1Descriptive statistics of analysis sample, adults aged 58+, Survey of Health, Ageing, and Retirement in Europe (SHARE) Switzerland, 2019/2020, n = 1424.
| Frequency | Sample % | ||
| Sex | Men | 669 | 47.0% |
| Women | 755 | 53.0% | |
| Age group of the respondent | 58–64 years | 337 | 23.7% |
| 65–74 years | 585 | 41.1% | |
| ≥75 years | 502 | 35.3% | |
| Education level | Low | 250 | 17.6% |
| Secondary | 891 | 62.6% | |
| Tertiary | 283 | 19.9% | |
| Partnership status | Has a partner | 1063 | 74.7% |
| No partner | 361 | 25.4% | |
| Ability to make ends meet | Easily | 782 | 54.9% |
| Fairly easily | 453 | 31.8% | |
| With difficulty | 189 | 13.3% | |
| Living area | Urban | 663 | 46.6% |
| Rural | 761 | 53.4% | |
| Linguistic region | German | 1000 | 70.2% |
| French | 383 | 26.9% | |
| Italian | 41 | 2.9% | |
| Number of chronic diseases | 0 | 360 | 25.3% |
| 1 | 453 | 31.8% | |
| 2 | 318 | 22.3% | |
| 3+ | 293 | 20.6% | |
| Limitations to activities of daily living | No limitations | 1317 | 92.5% |
| One or more limitations | 107 | 7.5% | |
| Health literacy index, by category | Sufficient | 976 | 68.5% |
| Problematic | 335 | 23.5% | |
| Inadequate | 113 | 7.9% | |
| Health literacy score, continuous score | 0 | 5 | 0.4% |
| 1 | 1 | 0.1% | |
| 2 | 2 | 0.1% | |
| 3 | 6 | 0.4% | |
| 4 | 7 | 0.5% | |
| 5 | 9 | 0.6% | |
| 6 | 14 | 1.0% | |
| 7 | 33 | 2.3% | |
| 8 | 36 | 2.5% | |
| 9 | 42 | 3.0% | |
| 10 | 74 | 5.2% | |
| 11 | 105 | 7.4% | |
| 12 | 114 | 8.0% | |
| 13 | 154 | 10.8% | |
| 14 | 185 | 13.0% | |
| 15 | 176 | 12.4% | |
| 16 | 461 | 32.4% | |
Our classification of health literacy based on the HLS-EU-Q16 questionnaire resulted in 976 (68.5%) respondents with a sufficient level of health literacy, while 335 (23.5%) had a problematic level and 113 (7.9%) had an inadequate level of health literacy. Within our analysis sample, 5 respondents (5.7%) had one missing item in the HLS-EU-Q16, while 24 respondents (2.1%) had two missing items, which were treated by imputing them as 0.
In our analysis sample, the median number of general practitioner consultations in the year prior to the interview was 2 with an interquartile range (IQR) of 1, while the median number of specialist consultations was 1 with an IQR of 1 too.
The distribution of healthcare utilisation across different health literacy levels is displayed in figures 2 and 3. Figure 2 displays the boxplot of general practitioner consultations in the year prior to the interview for groups of respondents with different levels of health literacy (sufficient, problematic, inadequate) while figure 3 shows these descriptive results for specialist consultations. For general practitioner consultations, the median number of consultations in the year prior to the interview varied significantly by health literacy level: respondents with sufficient health literacy had a median of 2 consultations, those with problematic health literacy had a median of 3 and individuals with inadequate health literacy had the highest median at 4 consultations. The statistical test confirmed that these between-group differences were significant (p <0.001). In contrast, for specialist consultations, all health literacy groups – sufficient, problematic and inadequate – reported a median of 1 consultation in the year prior to the interview. The differences in the number of specialist consultations across health literacy levels did not reach statistical significance (p = 0.80). Importantly, the boxplots reveal the presence of observations outside the upper fence (= Q3 + [1.5 × IQR]), where IQR is defined as Q3−Q1. This suggests the presence of outliers (n = 84 and n = 111 for general practitioner consultations and specialist consultations, respectively). However, our results remain consistent with a sensitivity analysis, in which the distribution was capped at the 90th percentile for extreme values (table S2 in the appendix).
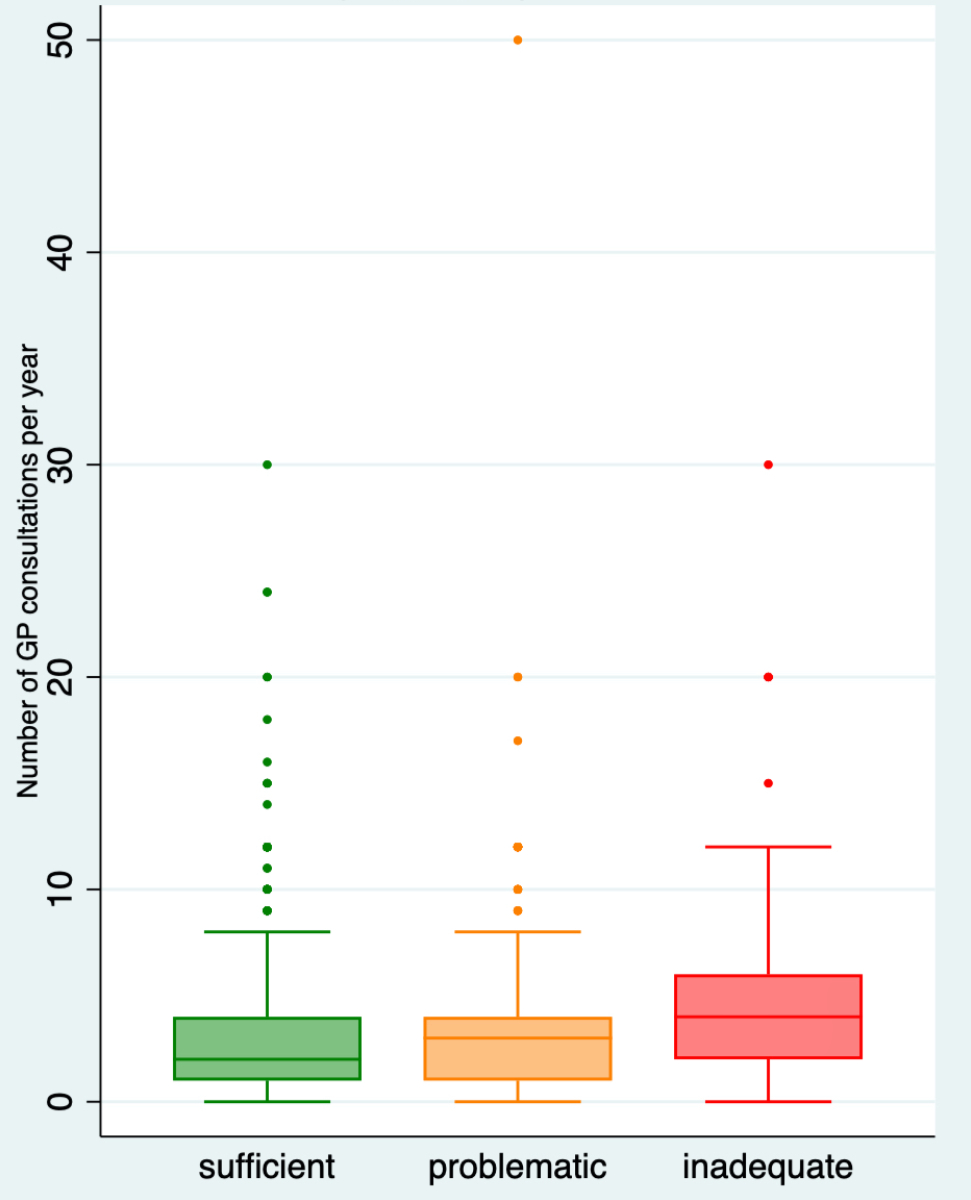
Figure 2Distribution of General Practitioner (GP) consultations by health literacy level. Adults aged 58+, SHARE Switzerland, 2019/2020, n = 1424. Boxplot of GP consultations by health literacy level. The medians are 2 for the sufficient category (n = 976), 3 for the inadequate category (n = 335) and 4 for the problematic category (n = 113). The Kruskal-Wallis test indicates a significant difference between medians (p <0.001).
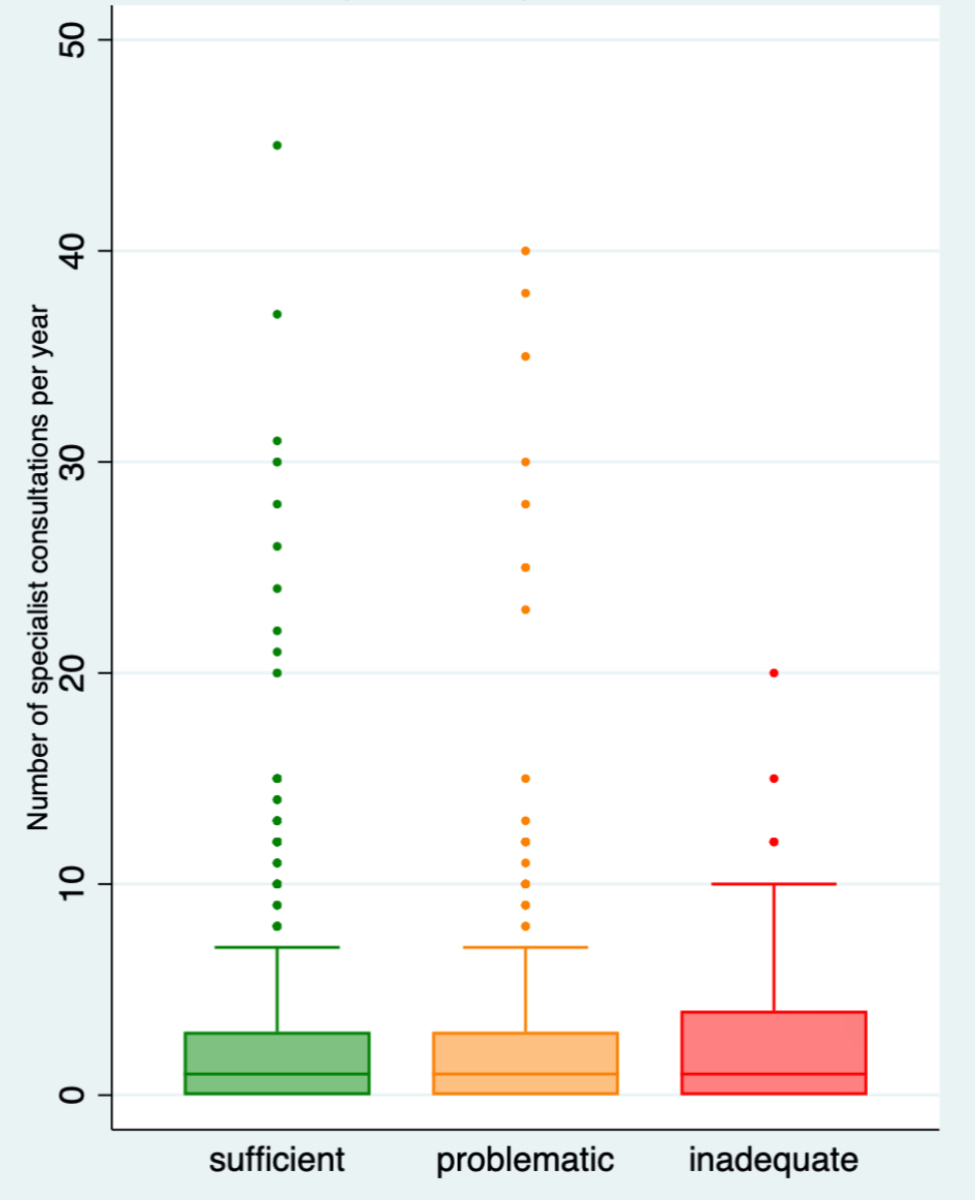
Figure 3Distribution of specialist consultations by health literacy level*. Adults aged 58+, Survey of Health, Ageing, and Retirement in Europe (SHARE) Switzerland, 2019/2020, n = 1424. Boxplot of specialist consultations by health literacy level. The medians are 1 for the sufficient category (n = 974), 1 for the inadequate category (n = 334) and 1 for the problematic category (n = 113). The Kruskal-Wallis test indicates no significant difference between medians (p = 0.80). *To enhance legibility, three outliers are omitted from the figure: two observations within the category of sufficient health literacy (100 and 160 specialist consultations) and one within the inadequate health literacy category (95 specialist consultations).
Table 2 displays the results from multivariate analyses in the form of average marginal effect and standard errors based on two models for two outcome variables: general practitioner consultations and specialist consultations. Both models utilise generalised Poisson regression and include sociodemographic, regional and health-related control variables and health literacy. In model 1, health literacy is categorised into three levels (sufficient, problematic, inadequate), while in model 2 health literacy is treated as a continuous variable measured on a scale of 0–16.
Table 2Partial associations of health literacy scores and categories on general practitioner and specialist consultations controlling for respondents’ sociodemographic characteristics and health status variables, adults aged 58+, Survey of Health, Ageing, and Retirement in Europe (SHARE) Switzerland, 2019/2020, n = 1424. The table shows average marginal effects and standard errors (in brackets) from two separate models for the count of general practitioner consultations and the count of healthcare specialist consultations. Both models control for sex, age, partnership status, linguistic region, education level, subjective financial situation, living area, activities of daily living limitations and the number of chronic conditions. Model 1 uses categorical health literacy while model 2 uses its continuous score. SHARE wave 8.
| Model 1 – general practitioner consultations | Model 2 – general practitioner consultations | Model 1 – Specialist consultations | Model 2 – Specialist consultations | |||
| Health literacy, 3 categories (vs sufficient) | problematic | 0.05 | −0.01 | |||
| (0.05) | (0.07) | |||||
| inadequate | 0.26** | −0.01 | ||||
| (0.08) | (0.12) | |||||
| Health literacy - continuous | Health literacy score | −0.03** | 0.01 | |||
| (0.01) | (0.01) | |||||
| Constant | 0.68** | 1.04** | 0.45* | 0.36 | ||
| (0.09) | (0.12) | (0.15) | (0.20) | |||
| atanhdelta constant | 0.38** | 0.38** | 0.71** | 0.71** | ||
| (0.02) | (0.02) | (0.05) | (0.05) | |||
| Observations | 1424 | 1424 | 1424 | 1424 | ||
atanhdelta refers to the inverse hyperbolic tangent of the dispersion parameter (delta). This transformation is used to map the dispersion parameter into a bounded range, ensuring model stability and interpretability. It controls overdispersion (delta >0) or underdispersion (delta <0) in count data.
* p <0.01
** p <0.001
Model 1 shows that, on average, individuals with inadequate health literacy reported a significantly higher number of general practitioner consultations in the 12 months prior to the interview (average marginal effect = 0.26, p = 0.0013). This result indicates that individuals would, on average, report 0.26 additional general practitioner consultations when having inadequate health literacy compared to individuals with sufficient health literacy levels. Similar to model 1, model 2 shows that respondents with a higher health literacy score reported on average a lower number of general practitioner consultations in the 12 months prior to the interview (average marginal effect = –0.03, p = 0.0011). This result shows that for each additional point on the health literacy score, the person would report 0.03 fewer general practitioner consultations, highlighting that the association between health literacy and use of general practitioners does not critically depend on the specific health literacy category. In contrast, we found no statistically significant associations between health literacy and specialist consultations in either model 1 (p = 0.8526) or 2 (p = 0.3828).
This paper uses a population-based sample of 1424 adults aged 58 or older living in Switzerland to study the association between health literacy and use of general practitioners and healthcare specialists. After controlling for sociodemographic, regional and health-related variables, older adults with inadequate health literacy had a significantly higher number of general practitioner consultations, whereas no such association was observed for specialist consultations. These results are consistent with previous research showing a significant association between health literacy and healthcare utilisation [15–18]. This paper adds to this literature by utilising a setting that comprises the general older population in Switzerland and allows us to extrapolate some important information regarding the healthcare utilisation of older adults with varying levels of health literacy in the Swiss context. While there are some studies investigating the relationship between health literacy and healthcare utilisation in Switzerland, they are generally based on smaller samples and target specific population groups. One previous study showed that immigrants with lower health literacy had higher use of healthcare services than immigrants with higher health literacy levels [23]. Other studies in the Swiss context have focused on patients with multimorbidity [24] or diabetes [25], and both found that lower health literacy levels are associated with higher healthcare use. While previous research has explored the association between health literacy and sociodemographic characteristics [27] or individuals’ health conditions [26] using SHARE data, the present study is, to the best of our knowledge, the first to investigate its relationship with healthcare utilisation in this large population-based ageing survey in Switzerland.
Our findings suggest that poor health literacy is associated with increased healthcare utilisation irrespective of health status and socioeconomic position. This may indicate higher healthcare needs for older adults with inadequate levels of health literacy in Switzerland. Specifically, the documented inequality in general practitioner consultations may not reflect inequities in healthcare use but rather show that general practitioners have an important role in care coordination and care management for patients with lower levels of health literacy [9–37]. In this case, the reported inequalities in healthcare use by health literacy level may be fair. By contrast, our finding is also consistent with a higher incidence of complications or other needs for medical intervention among older adults with low health literacy, even if we do not see a similar association between health literacy and specialist care. In either case, our findings highlight that low health literacy does not seem to constitute a major barrier to accessing healthcare in the Swiss health system.
The absence of a significant association between health literacy and the number of consultations with a healthcare specialist might be explained by specific organisational aspects of the Swiss healthcare system. In Switzerland, general practitioners play a crucial role in providing basic healthcare services, administering initial treatments and, when needed, referring patients to specialists [37]. While patients have the option to directly contact specialists, certain health insurance plans require a prior visit to a general practitioner before seeking specialist care. General practitioners therefore often serve as gatekeepers [38]. Additionally, at least a basic understanding of the different disciplines of medicine, and hence a higher level of health literacy, may be required for patients to access specialist care directly, which may explain our documented absence of inequalities in specialist care by health literacy level.
Health insurance plans in Switzerland vary in the amount of deductibles and/or co-payments, with higher-deductible plans being associated with lower premiums [2]. Also, extra coverage may be purchased separately, and income-related premium assistance is provided for those in need [39]. The healthcare system characteristics described above may impact healthcare utilisation. Although the SHARE main interview includes questions about long-term care insurances, supplementary insurance and about respondent’s satisfaction with their basic insurance coverage [29], there is no information available about personal insurance plans (i.e. size of deductibles or premiums) within the older population in Switzerland. However, one study examining access to care in various countries including a weighted sample of 1306 adults from Switzerland found that only a small proportion of individuals in Switzerland encounter challenges in accessing care or face financial difficulties in paying for healthcare services [40].
Our findings suggest that individuals with inadequate health literacy may compensate for their lack of knowledge by seeking guidance and advice from a general practitioner. One study using population-based cross-sectional health survey data interviewed 1025 adult individuals in Switzerland (median age of 52) and found that the vast majority were registered with a general practitioner [37]; this finding underscores the importance of general practitioners for health advice in the Swiss healthcare system and highlights the broader role of general practitioners as comprehensive health advisors rather than just providers of disease-centred care.
While general practitioners acting as health advisors may help to compensate for some disadvantages of people with low health literacy, improving health literacy in the population may provide further health benefits and also save resources in the system. Switzerland’s ageing population is associated with an increase in the development of chronic diseases and multimorbidity [41], which is leading to a higher resource utilisation in terms of healthcare [42, 43]. Given that our findings suggest that individuals with lower health literacy are more likely to seek consultations with general practitioners compared to those with higher health literacy levels, enhancing overall health literacy within the population could potentially ease the strain on healthcare resource utilisation, particularly in the context of general practitioners. In fact, improving health literacy could provide the population with the tools to better manage their healthcare needs, reducing the need to frequently consult general practitioners for basic information and coordination of care. Moreover, better health literacy might increase awareness of how one’s own actions affect personal health, encouraging more proactive preventive behaviours [44] and self-management [45], potentially resulting in a healthier population [46] and a more cost-effective healthcare system [47].
Actions may be taken in order to empower the population with higher health literacy. National interventions and communication campaigns could be an effective way to reach the population [48]. Developing health literacy strategies at a national level might include cross-sector public policies, including healthcare services, professionals, organisations and policymakers to reach the different strata of the population [49]. Focusing on communities, social contacts or older adults’ families could serve as an informal pathway for enhancing health literacy, potentially triggering a ripple effect within the community [50]. The consideration of cultural differences and vulnerable populations is a crucial part in policymaking, necessitating the tailoring of health information to diverse cultural nuances. A previous study in the same study population revealed significant disparities in health literacy across linguistic regions in Switzerland [27], underscoring some important regional differences. This study also reported that lower education, limited financial resources and poor health status were associated with a higher risk of disadvantaged access to health services. In public health policies, employing health literacy measures like the European Health Literacy Survey questionnaire may be important for targeting affected individuals. Interventions should include simplified health information and user-friendly eHealth tools [48]. However, the challenge of digitisation is particularly acute for older adults, who often face difficulties accessing digital information due to their lower levels of digital health literacy [51]. Collaboration with official media channels may be essential for the accurate dissemination of health information. Simultaneously, it appears critical to monitor informal channels, like social media, for their potential to spread fake or misleading information, as underscored by a study on Swiss news consumption during the COVID-19 pandemic that highlighted the potentially harmful impact of misinformation on public health during emergencies [52]. Ultimately, advancing health literacy should be viewed as a collaborative effort between healthcare consumers and professionals rather than solely an individual’s responsibility [53]. In this context, healthcare professionals may need training and support to enhance their communication skills, ensuring that medical information is delivered in a comprehensive and actionable manner for patients with varying levels of health literacy. By improving communication, healthcare providers can empower patients to actively participate in their healthcare decisions and improve health outcomes [54]. Additionally, a greater emphasis on preventive care and promotion of a broader understanding of health beyond disease-centred care can provide individuals with the tools and knowledge to make informed choices about their health, leading to more effective healthcare utilisation. By integrating these principles into healthcare policy and practice, policymakers can foster a healthcare system that focuses on holistic well-being and empowers individuals to actively manage their health. In the context of older adults, healthcare providers may take the time to educate them about their health conditions, potential treatment options and lifestyle modifications. Patients would be encouraged to actively participate in decision-making related to their health. Therefore, they would be more likely to feel empowered and confident in their ability to manage their health effectively. As a result, they may be more proactive in adhering to their care plans, making healthier lifestyle choices and seeking help when needed.
Our study has some limitations. First, we rely on self-reported data for the number of general practitioner and specialist consultations, which may lead to inaccuracies in measurement and introduce potential recall biases. Additionally, the subjective nature of our health literacy instrument (i.e. the HLS-EU-Q16) may introduce reporting bias, whereby respondents might over- or underestimate their actual health literacy skills, which could result in bias when trying to measure the association between actual objectively measured health literacy and healthcare use. However, the short version of the HLS-EU-Q16 questionnaire is commonly used in the literature as it is a validated instrument that offers many advantages in general health survey settings such as convenience and shorter completion times, especially for older adults [30]. Further, the representativeness of the SHARE dataset and the presence of missing data may result in additional biases. Selection effects and attrition within the study could result in the underrepresentation of certain groups, such as very old adults, those in poor health or immigrants with limited proficiency in any of the official languages of Switzerland, who may have lower literacy, less education and be less willing to participate in a survey like SHARE. Additionally, conducting interviews in nursing homes can be challenging and may result in additional selection effects. However, missing data were not a significant concern in our study, as the number of respondents who did not participate in the drop-off questionnaire was relatively low. Additionally, our analysis, which included regressing indicators for item non-response on a set of covariates, did not reveal any significant biases, indicating no substantial selection issues. Finally, the cross-sectional nature of our data limits our ability to infer any causal relationship, which would require further research. Nonetheless, our descriptive studies already provide important diagnostics for the functioning of the healthcare system in Switzerland, even if the interpretation of our regressions remains strictly non-causal.
Our study shows that in Switzerland, older adults with lower levels of health literacy use more general practitioner care than those with higher levels of health literacy. These findings, however, should not necessarily be interpreted as excessive care use among older adults with low levels of health literacy but may rather highlight the role of general practitioners as health advisors helping older adults with low levels of health literacy navigate the healthcare system. At the same time, improving health literacy in the older population may help reduce the need for general practitioners to act as healthcare advisors and may, therefore, result in improved health and lower costs for the health system. Our findings underscore the need to prioritise health literacy improvements as a fundamental component of healthcare policy and practice. This approach seeks to enhance healthcare access and improve health outcomes by encouraging older adults in Switzerland to make more informed and conscious decisions about their health.
This paper uses data from Börsch-Supan A (2020) Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. Release version: 1.0.0. SHARE-ERIC. Dataset. DOI: 10.6103/SHARE.w8.100. The datasets generated and/or analysed during this study are accessible for scientific research following a formal data request application to the SHARE study (https://share-eric.eu/data/become-a-user).
Analytical codes related to this research can be obtained upon request to: giuliano.pigazzini[at]ehl.ch
The authors are grateful to Dr Carmen Borrat-Besson and Dr Sarah Vilpert for developing the Swiss drop-off questionnaire in collaboration with Prof. Jürgen Maurer, Prof. Gian-Domenico Borasio and Prof. Ralf J. Jox, and to other members of the Swiss SHARE team for their valuable advice and discussions.
SNSF funding for the end-of-life project. Healthy Ageing in the Face of Death: Preferences, Communication, Knowledge, and Behaviors Regarding End of Life and End-of-life Planning Among Older Adults in Switzerland (grant number: 10001C_188836).
This paper uses data from Survey of Health, Ageing, and Retirement in Europe (SHARE) Waves 8 (10.6103/SHARE.w8.800); see Börsch-Supan et al. (2013) for methodological details [1]. The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782, SHARE-COVID19: GA N°101015924) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332 and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see https://share-eric.eu).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Federal Office of Public Health FOPH. Assessing Equity. Available from https://www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitsstrategien/gesundheitliche-chancengleichheit/chancengleichheit-in-der-gesundheitsversorgung/chancengerechtigkeit-messen.html
2. Federal Office of Public Health FOPH. Health insurance. Available from https://www.bag.admin.ch/bag/en/home/versicherungen/krankenversicherung.html
3. Federal Office of Public Health FOPH. Taking health to heart. Available from: https://www.bag.admin.ch/bag/en/home/das-bag/auftrag-ziele.html
4. OECD. Health at a Glance 2021: OECD Indicators. Health at a Glance. OECD; 2021.
5. Federal Statistical Office. Ageing in Switzerland. Available from https://www.bfs.admin.ch/bfs/en/home/statistiken/querschnittsthemen/aelter-werden-schweiz.html
6. Jaul E, Barron J. Age-Related Diseases and Clinical and Public Health Implications for the 85 Years Old and Over Population. Front Public Health. 2017 Dec;5:335. doi: https://doi.org/10.3389/fpubh.2017.00335
7. Djalali S, Meier T, Hasler S, Rosemann T, Tandjung R. Primary care in Switzerland gains strength. Fam Pract. 2015 Jun;32(3):348–53. doi: https://doi.org/10.1093/fampra/cmv005
8. Schnakenberg R, Goeldlin A, Boehm-Stiel C, Bleckwenn M, Weckbecker K, Radbruch L. Written survey on recently deceased patients in germany and switzerland: how do general practitioners see their role? BMC Health Serv Res. 2016 Jan;16(1):22. doi: https://doi.org/10.1186/s12913-016-1257-1
9. Cohidon C, Imhof F, Bovy L, Birrer P, Cornuz J, Senn N. Patients’ and General Practitioners’ Views About Preventive Care in Family Medicine in Switzerland: A Cross-sectional Study. J Prev Med Public Health. 2019 Sep;52(5):323–32. doi: https://doi.org/10.3961/jpmph.19.184
10. Santana S, Brach C, Harris L, Ochiai E, Blakey C, Bevington F, et al. Updating Health Literacy for Healthy People 2030: Defining Its Importance for a New Decade in Public Health. J Public Health Manag Pract. 2021 Nov-Dec;27(6 Suppl 6):S258–64. doi: https://doi.org/10.1097/PHH.0000000000001324
11. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al.; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012 Jan;12(1):80.
12. Geboers B, de Winter AF, Luten KA, Jansen CJ, Reijneveld SA. The association of health literacy with physical activity and nutritional behavior in older adults, and its social cognitive mediators. J Health Commun. 2014;19(sup2 Suppl 2):61–76. doi: https://doi.org/10.1080/10810730.2014.934933
13.Easton P, Entwistle VA, Williams B. Health in the ‘hidden population’ of people with low literacy. A systematic review of the literature. BMC Public Health. 2010 Aug;10(1):459. doi: https://doi.org/10.1186/1471-2458-10-459
14. Chen JZ, Hsu HC, Tung HJ, Pan LY. Effects of health literacy to self-efficacy and preventive care utilization among older adults. Geriatr Gerontol Int. 2013 Jan;13(1):70–6. doi: https://doi.org/10.1111/j.1447-0594.2012.00862.x
15. Viktorsson L, Yngman-Uhlin P, Törnvall E, Falk M. Healthcare utilisation and health literacy among young adults seeking care in Sweden: findings from a cross-sectional and retrospective study with questionnaire and registry-based data. Prim Health Care Res Dev. 2019 Dec;20:e151. doi: https://doi.org/10.1017/S1463423619000859
16. MacLeod S, Musich S, Gulyas S, Cheng Y, Tkatch R, Cempellin D, et al. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr Nurs. 2017;38(4):334–41. doi: https://doi.org/10.1016/j.gerinurse.2016.12.003
17. Y. I. Cho, S.-Y. D. Lee, A. M. Arozullah, and K. S. Crittenden. Effects of health literacy on health status and health service utilization amongst the elderly. Soc. Sci. Med. 1982, vol. 66, no. 8, pp. 1809–1816, Apr. 2008. doi: https://doi.org/10.1016/j.socscimed.2008.01.003
18. Hardie NA, Kyanko K, Busch S, Losasso AT, Levin RA. Health literacy and health care spending and utilization in a consumer-driven health plan. J Health Commun. 2011;16(sup3 Suppl 3):308–21. doi: https://doi.org/10.1080/10810730.2011.604703
19. Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health Literacy Impact on National Healthcare Utilization and Expenditure. Int J Health Policy Manag. 2015 Aug;4(11):747–55. doi: https://doi.org/10.15171/ijhpm.2015.151
20. Griffey RT, Kennedy SK, D’Agostino McGowan L, Goodman M, Kaphingst KA. Is low health literacy associated with increased emergency department utilization and recidivism? Acad Emerg Med. 2014 Oct;21(10):1109–15. doi: https://doi.org/10.1111/acem.12476
21. Berens EM, Vogt D, Messer M, Hurrelmann K, Schaeffer D. Health literacy among different age groups in Germany: results of a cross-sectional survey. BMC Public Health. 2016 Nov;16(1):1151. doi: https://doi.org/10.1186/s12889-016-3810-6
22. Palumbo R, Annarumma C, Adinolfi P, Musella M, Piscopo G. The Italian Health Literacy Project: insights from the assessment of health literacy skills in Italy. Health Policy. 2016 Sep;120(9):1087–94. doi: https://doi.org/10.1016/j.healthpol.2016.08.007
23. Mantwill S, Schulz PJ. Low health literacy and healthcare utilization among immigrants and non-immigrants in Switzerland. Patient Educ Couns. 2017 Nov;100(11):2020–7. doi: https://doi.org/10.1016/j.pec.2017.05.023
24. N’Goran AA, Pasquier J, Deruaz-Luyet A, Burnand B, Haller DM, Neuner-Jehle S, et al. Factors associated with health literacy in multimorbid patients in primary care: a cross-sectional study in Switzerland. BMJ Open. 2018 Feb;8(2):e018281. doi: https://doi.org/10.1136/bmjopen-2017-018281
25. Franzen J, Mantwill S, Rapold R, Schulz PJ. The relationship between functional health literacy and the use of the health system by diabetics in Switzerland. Eur J Public Health. 2014 Dec;24(6):997–1003. doi: https://doi.org/10.1093/eurpub/ckt202
26. Wieczorek M, Meier C, Vilpert S, Reinecke R, Borrat-Besson C, Maurer J, et al. Association between multiple chronic conditions and insufficient health literacy: cross-sectional evidence from a population-based sample of older adults living in Switzerland. BMC Public Health. 2023 Feb;23(1):253. doi: https://doi.org/10.1186/s12889-023-15136-6
27. Meier C, Vilpert S, Borrat-Besson C, Jox RJ, Maurer J. Health literacy among older adults in Switzerland: cross-sectional evidence from a nationally representative population-based observational study. Swiss Med Wkly. 2022 Apr;152(1314):w30158. doi: https://doi.org/10.4414/SMW.2022.w30158
28. Sykes S, Wills J, Rowlands G, Popple K. Understanding critical health literacy: a concept analysis. BMC Public Health. 2013 Feb;13(1):150. doi: https://doi.org/10.1186/1471-2458-13-150
29. Börsch-Supan A. (2022). Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. Release version: 8.0.0. SHARE-ERIC. Data set. DOI: ”
30. Okan O, Bauer U, Levin‐Zamir D, Pinheiro P, Sørensen K. International Handbook of Health Literacy: Research, practice and policy across the lifespan. Policy Press; 2019. https://library.oapen.org/handle/20.500. 12657/24879.
31. Pelikan J, Ganahl K, Van den Broucke S, Sorensen K. Measuring health literacy in Europe: Introducing the European Health Literacy Survey Questionnaire (HLS-EU-Q). 2019. https://www.degruyter.com/document/doi/10.56687/9781447344520-011/html
32. Ryser VA, Meier C, Vilpert S, Maurer J. Health literacy across personality traits among older adults: cross-sectional evidence from Switzerland. Eur J Ageing. 2023 Jun;20(1):28. doi: https://doi.org/10.1007/s10433-023-00774-x
33. Hoffmeyer-Zlotnik JH, Wolf C, editors. Advances in Cross-National Comparison: A European Working Book for Demographic and Socio-Economic Variables. Boston (MA): Springer US; 2003. pp. 195–220. doi: https://doi.org/10.1007/978-1-4419-9186-7
34. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983 Dec;31(12):721–7. doi: https://doi.org/10.1111/j.1532-5415.1983.tb03391.x
35. Edemekong PF, Bomgaars DL, Sukumaran S, et al. Activities of Daily Living. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan., Available from https://www.ncbi.nlm.nih.gov/books/NBK470404/
36. Cameron AC, Trivedi PK. Regression Analysis of Count Data, 2nd ed. in Econometric Society Monographs. Cambridge: Cambridge University Press, 2013. ISBN 9781139013567. doi: https://doi.org/10.1017/CBO9781139013567
37. Giezendanner S, Bretschneider W, Fischer R, Diaz Hernandez L, Zeller A. The ecology of medical care in Switzerland: prevalence of illness in the community and healthcare utilisation in Switzerland. Swiss Med Wkly. 2020 May;150(1920):w20221. doi: https://doi.org/10.4414/smw.2020.20221
38. Böhlert I, Adam I, Robra BP. [The Swiss gatekeeper system—a model for improving capacity development and economic effectiveness]. Gesundheitswesen. 1997;59(8-9):488–94.
39. De Pietro C, Camenzind P, Sturny I, Crivelli L, Edwards-Garavoglia S, Spranger A, et al. Switzerland: health system review. Health Syst Transit. 2015;17(4):1–288.
40. Schoen C, Osborn R, Squires D, Doty MM, Pierson R, Applebaum S. How health insurance design affects access to care and costs, by income, in eleven countries. Health Aff (Millwood). 2010 Dec;29(12):2323–34. doi: https://doi.org/10.1377/hlthaff.2010.0862
41. Fabbri E, Zoli M, Gonzalez-Freire M, Salive ME, Studenski SA, Ferrucci L. Aging and Multimorbidity: New Tasks, Priorities, and Frontiers for Integrated Gerontological and Clinical Research. J Am Med Dir Assoc. 2015 Aug;16(8):640–7. doi: https://doi.org/10.1016/j.jamda.2015.03.013
42. Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015 Jan;15(1):23. doi: https://doi.org/10.1186/s12913-015-0698-2
43. Aubert CE, Fankhauser N, Marques-Vidal P, Stirnemann J, Aujesky D, Limacher A, et al. Multimorbidity and healthcare resource utilization in Switzerland: a multicentre cohort study. BMC Health Serv Res. 2019 Oct;19(1):708. doi: https://doi.org/10.1186/s12913-019-4575-2
44. Aaby A, Friis K, Christensen B, Rowlands G, Maindal HT. Health literacy is associated with health behaviour and self-reported health: A large population-based study in individuals with cardiovascular disease. Eur J Prev Cardiol. 2017 Nov;24(17):1880–8. doi: https://doi.org/10.1177/2047487317729538
45. Mackey LM, Doody C, Werner EL, Fullen B. Self-Management Skills in Chronic Disease Management: What Role Does Health Literacy Have? Med Decis Making. 2016 Aug;36(6):741–59. doi: https://doi.org/10.1177/0272989X16638330
46. Ezzati M, Hoorn SV, Rodgers A, Lopez AD, Mathers CD, Murray CJ; Comparative Risk Assessment Collaborating Group. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003 Jul;362(9380):271–80. doi: https://doi.org/10.1016/S0140-6736(03)13968-2
47. Eichler K, Wieser S, Brügger U. The costs of limited health literacy: a systematic review. Int J Public Health. 2009;54(5):313–24. doi: https://doi.org/10.1007/s00038-009-0058-2
48. Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018 Dec;18(1):1414. doi: https://doi.org/10.1186/s12889-018-6331-7
49. Osborne RH, Elmer S, Hawkins M, Cheng CC, Batterham RW, Dias S, et al. Health literacy development is central to the prevention and control of non-communicable diseases. BMJ Glob Health. 2022 Dec;7(12):e010362. doi: https://doi.org/10.1136/bmjgh-2022-010362
50. Samerski S. Health literacy as a social practice: social and empirical dimensions of knowledge on health and healthcare. Soc Sci Med. 2019 Apr;226:1–8. doi: https://doi.org/10.1016/j.socscimed.2019.02.024
51. De Gani SM, Jaks R, Bieri U, Kocher JP. Health Literacy Survey Schweiz 2019-2021. Schlussbericht im Auftrag des Bundesamtes für Gesundheit BAG. Zürich, Careum Stiftung. 2021. Available from: https://www.bag.admin.ch/bag/en/home/strate-gie-und-politik/nationale-gesundheitspolitik/gesundheitskompetenz.html
52. Liu Z, Shan J, Delaloye M, Piguet JG, Glassey Balet N. The Role of Public Trust and Media in Managing the Dissemination of COVID-19-Related News in Switzerland. J Med. 2020 Dec;1(1):1. doi: https://doi.org/10.3390/journalmedia1010010
53. van der Heide I, Poureslami I, Mitic W, Shum J, Rootman I, FitzGerald JM. Health literacy in chronic disease management: a matter of interaction. J Clin Epidemiol. 2018 Oct;102:134–8. doi: https://doi.org/10.1016/j.jclinepi.2018.05.010
54. Mata ÁN, de Azevedo KP, Braga LP, de Medeiros GC, de Oliveira Segundo VH, Bezerra IN, et al. Training in communication skills for self-efficacy of health professionals: a systematic review. Hum Resour Health. 2021 Mar;19(1):30. doi: https://doi.org/10.1186/s12960-021-00574-3
Table S1List of items from the European Health Literacy Survey questionnaire (HLS-EU-Q16).
| First, we would like to ask you how comfortable you feel when dealing with health-related information. | |
| For you, how easy or difficult is it to… | |
| Answer categories | Very easy |
| Fairly easy | |
| Fairly difficult | |
| Very difficult | |
| 1. | Find information on treatments of illnesses that concern you? |
| 2. | Find out where to get professional help when you are ill? |
| 3. | Understand what your doctor says to you? |
| 4. | Understand your doctor or pharmacist’s instruction on how to take prescribed medicine? |
| 5. | Use the information the doctor gives you to make decisions about your illness? |
| 6. | Judge when you may need to get a second opinion from another doctor? |
| 7. | Follow instructions from your doctor or pharmacist? |
| 8. | Find information on how to manage mental health problems like stress or depression? |
| 9. | Understand health warnings about behaviour such as smoking, low physical activity, and excessive drinking? |
| 10. | Understand why you need health screenings? |
| 11. | Judge if the information on health risks in the media is reliable? |
| 12. | Decide how you can protect yourself from illness based on information in the media? |
| 13. | Understand information in the media on how to be healthier? |
| 14. | Find out about activities that benefit your mental well- being? |
| 15. | Understand advice on health from family members or friends? |
| 16. | Judge which everyday behaviour is related to your health? |
Table S2Sensitivity analysis of the generalised Poisson regression coefficients and statistical significance after imputation of the 90th percentile to outliers. Partial associations of health literacy scores and categories on general practitioner and specialist consultations after imputing the 90th percentile to extreme values, controlling for respondents’ sociodemographic characteristics and health status variables, adults aged 58+, SHARE Switzerland, 2019/2020, n = 1424. The table shows average marginal effects and standard errors (in brackets) from two separate models for the count of general practitioner consultations and the count of healthcare specialist consultations. Both models control for sex, age, partnership status, linguistic region, education level, subjective financial situation, living area, activities of daily living limitations and the number of chronic conditions. Model 1 uses categorical health literacy while model 2 uses its continuous score. SHARE wave 8.
| Model 1 – general practitioner consultations | Model 2 – general practitioner consultations | Model 1 – specialist consultations | Model 2 – specialist consultations | ||
| Health literacy, 3 categories (vs sufficient) | Problematic | 0.04 (0.04) | −0.01 (0.07) | ||
| Inadequate | 0.20** (0.06) | −0.01 (0.12) | |||
| Health literacy, continuous | Health literacy score | −0.02** (0.01) | 0.01 (0.01) | ||
| Constant | 0.52** (0.08) | 0.81** (0.10) | 0.45* (0.15) | 0.36 (0.20) | |
| Atanhdelta constant | 0.12** (0.01) | 0.12** (0.01) | 0.71** (0.05) | 0.71** (0.05) | |
| Observations | 1424 | 1424 | 1424 | 1424 | |
* p <0.01
** p <0.001