The funding of specialised paediatric palliative care in Switzerland: a conceptualisation
and modified Delphi study on obstacles and priorities
DOI: https://doi.org/https://doi.org/10.57187/s.3498
Stefan
Mitterera,
Karin
Zimmermannab,
Günther Finkc,
Michael Simona,
Anne-Kathrin
Gerbera,
Eva
Bergsträsserb
a Institute of Nursing Science, Department of Public Health, University
of Basel, Basel, Switzerland
b Paediatric
Palliative Care and Children’s Research Center, University Children’s Hospital
Zurich, Zurich, Switzerland
c Swiss Tropical and Public Health Institute, University of Basel, Basel,
Switzerland
Summary
BACKGROUND: Effective
funding models are key for implementing and sustaining critical care delivery
programmes such as specialised paediatric palliative care (SPPC). In
Switzerland, funding concerns have frequently been raised as primary barriers
to providing SPPC in dedicated settings. However, systematic evidence on
existing models of funding as well as primary challenges faced by stakeholders
remains scarce.
AIMS: The
present study’s first aim was to investigate and conceptualise the funding of
hospital-based consultative SPPC programmes
in Switzerland. Its second aim was to identify obstacles to and priorities for
funding these programmes sustainably.
METHODS: A 4-step process, including a document analysis, was used to conceptualise
the funding of hospital-based consultative SPPC programmes in Switzerland. In
consultation with a purposefully selected panel of experts in the subject, a 3-round
modified Delphi study was conducted to identify funding-relevant obstacles and
priorities regarding SPPC.
RESULTS: Current
funding of hospital-based consultative specialised paediatric palliative care
programmes is complex and fragmented, combining funding from public, private
and charitable sources. Overall, 21 experts participated in the first round of
the modified Delphi study, 19 in round two and 15 in round three. They identified
23 obstacles and 29 priorities. Consensus (>70%) was obtained for 12
obstacles and 22 priorities. The highest level of consensus (>90%) was achieved
for three priorities: the development of financing solutions to ensure
long-term funding of SPPC programmes; the provision of funding and support for
integrated palliative care; and sufficient reimbursement of inpatient service
costs in the context of high-deficit palliative care patients.
CONCLUSION: Decision-
and policy-makers hoping to further develop and expand SPPC in Switzerland should
be aware that current funding models are
highly complex and that SPPC funding is impeded by many obstacles. Considering
the steadily rising prevalence of children with life-limiting conditions and
the proven benefits of SPPC, improvements in funding models are urgently needed
to ensure that the needs of this highly vulnerable population are adequately
met.
Introduction
The prevalence
of children (aged 0–19 years) with life-limiting conditions has been rising steadily
in recent years [1, 2]. Extrapolating from hospital admission data from England
[2], an estimated 11,400 such children currently live in Switzerland. However,
if more comprehensive data from Germany are applied, this number could be as
high as 42,400 [3]. While advances in life-extending medical care and
technology can partially explain the steady increase [4, 5], improvements in
medical coding practice may also have had an effect [2]. Many of these children
and their families can benefit from paediatric palliative care (PPC). Generally,
palliative care aims to improve the quality of life of patients with severe
health-related suffering across all ages, as well as that of their families and
caregivers [6]. As a needs-based approach, PPC includes physical, emotional,
social and spiritual elements that continue throughout the patient’s life and
beyond [6, 7].
Although
new paediatric palliative care programmes have been implemented in recent
years, nationwide access remains limited in Switzerland [8, 9]. Recognising the
complexity of care involved, the Swiss Federal Office of Public Health defines PPC
as
specialised palliative care [10]. Commonly provided by consultative
hospital-based programmes, specialised paediatric palliative care (SPPC) is
delivered in dedicated settings, i.e. the team works exclusively in PPC [11]. Ideally,
these teams are comprised of physicians, nurses, therapists and other
professionals specialised in PPC [11, 12].
Specialised
paediatric palliative care offered within a consultative model of care
contributes to primary care provision and incorporates elements of medical
treatment, care coordination, psychosocial support and other consultative services
[13]. Care and support is offered as and where necessary – both in and out of
hospitals (mobile services such as home visits), through the phases of
palliation, end of life and bereavement to patients, their families, primary
care teams and other healthcare professionals [13]. The level of mobile support
offered varies between programmes, depending on service mandates and available
resources [14]. Additionally, SPPC teams may engage in paediatric palliative
care-related education, training and research [13].
Although
federal healthcare laws and regulations apply [15, 16] and most cantons have
formally recognised the promotion and provision of palliative care [17], specialised
paediatric palliative care is currently much less established than adult palliative
care [8]. In the context of the Swiss healthcare system’s complexity, for which
federal and cantonal bodies assume different tasks, ongoing resource shortages are
likely to challenge the full provision of SPPC. In the Swiss healthcare
system, resources to pay for eligible services, including palliative care, are
collected mostly through compulsory insurance premiums and taxes [18]. In
addition, patients who use insured services are subject to cost-sharing in the
form of deductibles and co-payments [18]. And while patients under the age of
18 are exempt from deductible payments, their families are still liable for co-payments
[19].
Activity-based
funding is the dominant payment method for reimbursing healthcare providers in
Switzerland [18]. While inpatient services are reimbursed via Diagnosis-Related
Group (DRG) payments, outpatient medical services are reimbursed via the tarif
médical (TARMED), a fee-for-service system [18]. Reimbursement of inpatient
costs is subject to cost-sharing between cantons (at least 55%) and health
insurers (at most 45%) [18]. Under certain circumstances, e.g. when a child has
a birth defect, Swiss disability insurance covers part of the related
healthcare expenses [20]: it reimburses 80% of inpatient treatment costs, with
the canton of residence bearing the remaining 20% [21]. Payments for medical
devices and items, laboratory and diagnostic services and medications are
specified in standard fee schedules (i.e. so-called positive lists) [18]. Although reimbursement via standardised
payment systems, e.g. SwissDRG and TARMED, may work well in most healthcare
settings, this is not always the case for hospital-based consultative specialised
paediatric palliative care programmes. Considering the complexity of these
programmes, with care and support provided in various settings and across the
phases of palliation, end of life and bereavement, adequate reimbursement of
related costs may constitute a major challenge.
Information
on models of specialised paediatric palliative care funding and their practical
implementation remains scarce. Even in adult palliative care, few studies
describe such models [22]. The available evidence suggests both that
reimbursement mechanisms tend to undervalue care input and that funding models
are often characterised by a combination of public, private and philanthropic
funding [22]. However, it has been recognised that analyses of payment and
financial strategies based on programme types and funding systems are highly
important to this field’s progress [23]. Therefore, this study’s primary aim
was to develop a conceptual model describing the funding of hospital-based
consultative specialised paediatric palliative care programmes in Switzerland.
Its second aim was to identify obstacles to and priorities for funding these
programmes sustainably.
Materials and methods
In this
study, two separate methodological approaches were employed to address each of
the study’s objectives. First, to develop a conceptual model describing the
funding of hospital-based consultative SPPC programmes in Switzerland, we
followed a 4-step conceptualisation process, including a document analysis.
Second, to identify obstacles and priorities regarding SPPC funding, we
conducted a 3-round modified Delphi study.
Conceptualisation
process
Conceptual models
provide visual illustrations of causal linkages (often visualised as arrows) among
sets of concepts (often visualised as boxes) believed to relate to particular target
points [24, 25]. To conceptualise the funding of hospital-based consultative specialised
paediatric palliative care programmes in Switzerland, we used a 4-step process:
(1) define a target point, (2) choose a conceptual basis, (3) conduct a literature
search and (4) propose a conceptual model [24].
Target point
For this conceptualisation,
we decided to set the focus on hospital-based consultative SPPC programmes, as
they are a common model for providing paediatric palliative care and have been implemented
at several children’s hospitals throughout Switzerland [8, 9].
Conceptual basis
Deber et al.’s
blended service and funding flow model [26] provided the theoretical basis upon
which we conceptualised the funding of hospital-based consultative SPPC
programmes in Switzerland. Their model illustrates the complex relationship
between provider organisations, service providers, service recipients and
third-party payers, all of which are connected by payment and reimbursement
structures [26]. To design our model, we focused on assessing the current
sources of funding, systems of payment and mechanisms of reimbursement in terms
of direct financial flows and funding arrangements.
Document analysis
To explore
and describe the funding of Swiss specialised paediatric palliative care
programmes, we performed a document analysis. Such analyses are widely used in
health policy research to review documents, provide context and supplement
other data types [27]. The aim of the document analysis was to identify funding
sources, payment systems and reimbursement mechanisms and to uncover areas
where challenges to SPPC programmes’ funding are encountered.
Due to the
limited number of specialised paediatric palliative care-specific documents and
the fact that healthcare financing policies do not distinguish between palliative
care for children and adults, we widened our search to include documents on the
funding of palliative care in general. The READ approach (Ready materials;
Extract data; Analyse data; and Distil findings) for document analysis in
health policy research provided the necessary methodology for this document
analysis [28].
Documents
were identified by conducting web searches (Google search engine) for grey
literature, browsing for documents on institutions’ and non-governmental
organisations’ web pages and tracking references. The search was conducted in
German between 6and 20 August 2021 by the first author (SM) and
discussed with two other authors (KZ and EB). Documents about palliative care
funding in Switzerland were included if they reported funding sources, payment
systems and reimbursement mechanisms and/or areas where challenges to that
funding are encountered. To account for the implementation of SwissDRG, documents
had to be published in 2012 or later. Documents reporting solely on the funding
of non-hospital-based palliative care programmes (e.g. geriatric long-term
care, home care agencies) were excluded. Included documents were analysed using
qualitative content analysis [27]. Information was coded, summarised and
tabulated into three predefined categories: funding sources; payment systems
and reimbursement mechanisms; and challenging areas.
Conceptual model
The findings
of the document analysis were used to visualise the funding of hospital-based
consultative specialised paediatric palliative care programmes in Switzerland.
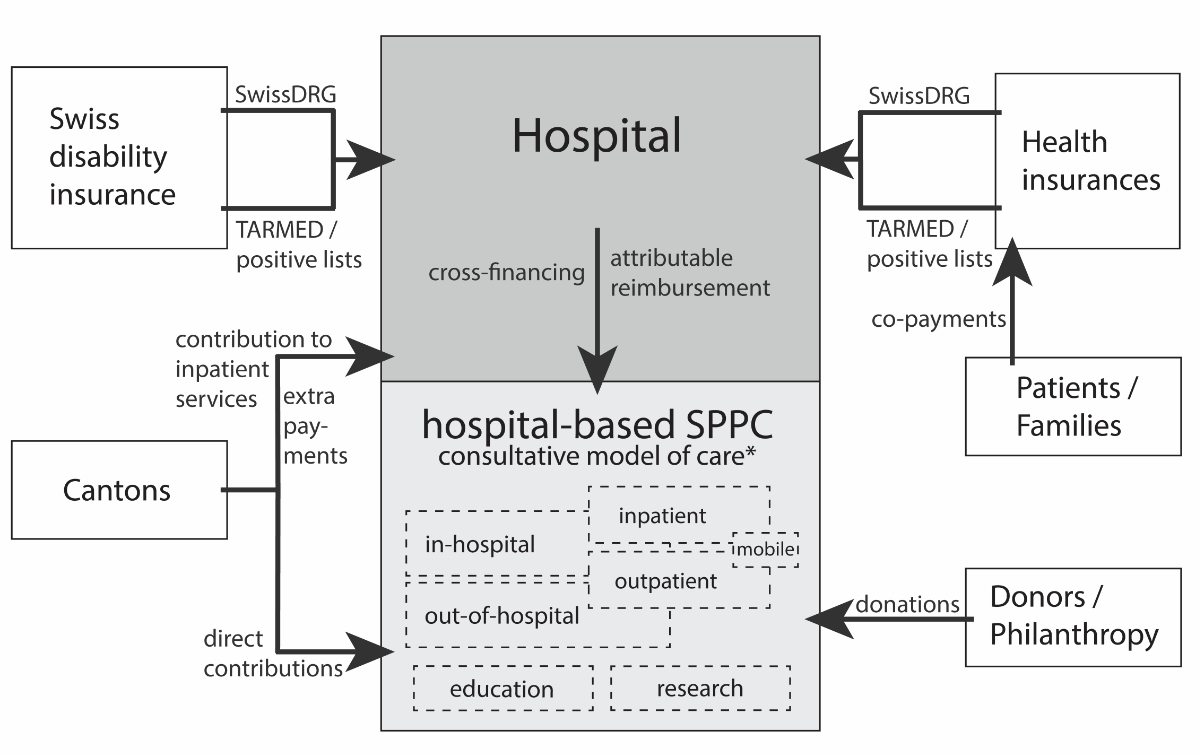
The resulting conceptual model is presented in figure 1.
Figure 1Conceptualisation
of direct financial flows and funding arrangements regarding hospital-based
consultative specialised paediatric palliative care programmes in Switzerland.
* The consultative model of care refers to the provision of medical treatment,
care coordination, psychosocial support and other consultative services that
contribute to primary care provision. Care and support is provided to families,
primary care teams and other professionals in and out of hospitals, i.e.
inpatient, outpatient/mobile services. Specialised paediatric palliative care
teams may engage in paediatric palliative care-related research and education.
Modified Delphi
study
To identify
obstacles and priorities in the funding of Swiss SPPC programmes, we used a 3-round
modified Delphi approach [29]. The Delphi technique is a well-established,
iterative series of steps to survey experts on a particular issue and develop
individual opinions into a group consensus [30–34]. Since its inception in the
1950s, numerous versions of the Delphi technique have been developed, differing
mainly in how consensus was reached or measured [35]. In this study, consensus
was measured by asking participating experts to indicate their agreement or
disagreement with specific statements on a 4-point Likert scale.
Procedures
Before
study start, we purposefully compiled an initial list of experts. We selected potential
participants based on two inclusion criteria: either they had professional
experience in establishing, managing or leading Swiss SPPC programmes (e.g.
programme directors) or they had direct professional knowledge about sources of
funding, payment systems or reimbursement mechanisms related to palliative care
funding in Switzerland (e.g. researchers, health economists, public health
officials, insurance professionals). All eligible experts were first invited via
e-mail to participate in this study, then asked to name two to three other
experts who might also qualify for participation. The modified Delphi study
took place between 23 May and 3 October 2022. Online questionnaires were
provided in German via Google Forms. Reminders were sent towards the end of
each round.
Round one
All experts
who had consented to study participation received a link to an online
questionnaire. This asked them to provide minimal demographic data (i.e.
profession, affiliation) and, using free-text fields, to list and describe
obstacles and priorities regarding SPPC funding. To provide the necessary
context for their responses, challenging areas identified via the document analysis
were provided. In discussion with two study team members (KZ and EB), the first
author (SM) compiled, summarised and merged the expert’s answers into two
lists, one of obstacles, the other of priorities.
Round
two
In round
two, the generated and anonymised lists were sent to everyone who had participated
in round one. Experts were encouraged to comment on identified obstacles and
priorities, as well as specify any more that might have emerged or occurred to
them during the second round. Their answers were again compiled, summarised and
merged. The results were used to update the lists of obstacles and priorities.
Round
three
To measure
consensus, the updated lists were sent to all experts who had participated in the
first two rounds. In the third questionnaire, experts were asked to indicate
their agreement or disagreement with each identified obstacle and priority on a
4-point Likert scale: strongly agree, agree, disagree, strongly disagree. In
cases where participating experts did not feel adequately informed on a topic
to indicate agreement or disagreement, they were given the option to answer
“Don’t know”. In addition, each respondent was asked to indicate what they
considered the three most pressing obstacles and the three most urgent priorities.
Data
analysis
Descriptive
statistics (i.e. counts and percentages) were used to provide an overview of
the characteristics of participating experts and to analyse consensus. Analyses
were performed in Microsoft Excel. The thresholds of consensus vary widely between
Delphi studies, with 75% being the median [36]. Considering the diversity of our
participants, we chose a slightly lower cut-off, defining consensus as >70%
agreement (“Strongly agree” and “Agree”).
Ethical
considerations
As no
health-related personal data were collected, the study was not under the
jurisdiction of the Swiss Human Research Act and no ethical approval was
obtained.
Results
Document analysis
and conceptual model
We included
a total of 15 documents in our analysis: 10 reports [8, 9, 14, 16, 17, 37–41],
three technical articles [42–44], one directive [45] and one review [46].
Twelve were obtained through web searches and three by backward reference
tracking. Only two were paediatric-specific; the other 13 focused on palliative
care in general. An overview of included documents is provided as a supplementary
resource (see appendix). Figure 1 shows our conceptual model of hospital-based
consultative specialised paediatric palliative care programme funding in
Switzerland.
Funding sources
Figure 1
illustrates how the Swiss disability insurance fund, health insurance funds,
cantons, donors and philanthropists, patients (i.e. their families) and
hospitals all hold stakes in the funding of hospital-based consultative specialised
paediatric palliative care programmes [8, 9, 14, 16, 17, 41]. Alongside
curative and preventive services, compulsory health insurance covers inpatient
and outpatient palliative care services, at least partially [16]. Depending on
patient characteristics (e.g. age, diagnosis) and service type (e.g. medical
aid, treatment), certain costs are reimbursed (partially) either by the Swiss
disability insurance fund or by health insurers [14, 16].
In addition
to partially reimbursing inpatient service costs and providing financial grants
to service providers (e.g. extra payments, deficit coverage), some cantons
provide direct financial contributions to fund palliative care [8, 9, 14, 16, 17].
In these cantons, special service mandates with hospitals regulate palliative
care provision and related cantonal funding [17]. For instance, the canton of Vaud
commissioned a cantonally funded consultative mobile specialised paediatric
palliative care programme to provide care in various settings, e.g. hospitals,
long-term care institutions, patients’ homes [8, 9, 16].
Very
limited information is reported about payments made by patients or families (in
case of children). Leaving aside their tax payments and insurance premiums,
however, they are also involved in the financing of palliative care services
through their co-payments [14].
For
hospital-based palliative care programmes, hospitals act as both funders and
distributors of funds generated through service provision [41], i.e. payments
made by the Swiss disability insurance fund, health insurance funds and cantons
are collected at the hospital level and distributed under the sovereignty of
the hospital [41]. Our document analysis showed budget deficits of palliative
care programmes had to be either cross-financed by their operating hospitals [37,
46] or covered by donations and philanthropic contributions [8, 17, 37, 46].
Payment systems and reimbursement mechanisms
In terms of
the payment systems and reimbursement mechanisms outlined in figure 1, the reviewed
documents primarily reported on SwissDRG and TARMED. The responsibility for
further developing, adjusting and maintaining the SwissDRG system belongs to SwissDRG
AG, a nonprofit public organisation and joint institution of healthcare
provider associations, health insurers and cantons [42]. Within the National
Strategy for Palliative Care 2010–2015 [40], SwissDRG AG was commissioned to
develop a national tariff structure for reimbursing inpatient palliative care
services [42]. Via a multiyear process, they developed Swiss Classification of
Operations (CHOP) codes for palliative care procedures [16, 41–43, 46]. In this
context, to ensure uniform, high-quality service provision, minimum structural
and personnel requirements were set as performance criteria [16, 41–43]. Only
when these criteria are met can a hospital code and bill for the associated palliative
care procedure codes [41, 42].
Despite
these provisions, analyses showed that certain characteristics of palliative
care patients were not being considered optimally regarding reimbursement [42].
For instance, in terms of length of stay, treatment costs and number of
hospitalisations, palliative care patients differed significantly from other
patients in the same DRGs [42]. Therefore, SwissDRG AG conducted a fundamental
“grouper” restructuring and classified palliative care as a pre-Major
Diagnostic Category [9, 16, 42]. By the end of 2016, palliative care had been
allocated a separate diagnosis group – one independent of the patient’s main
diagnosis, with its own DRG codes (codes A97A–G) – defined in terms of medical
treatment, procedure, length of stay and other criteria [42–44]. Concerns about
adverse incentives regarding inappropriately shortened hospital stays were
addressed by a two-pronged strategy: on the one hand, additional payments were
allowed for extended hospitalisations [45]; on the other, case consolidations
were prevented by recognising readmissions as new, separate hospitalisations [16,
43].
Outpatient
medical palliative care services are reimbursed on a fee-for-service basis via TARMED
[14, 41]. Services listed in this tariff structure are covered by compulsory
healthcare insurance. However, our document analysis suggests that certain palliative
care services, e.g. care coordination and case management, are not fully reimbursable
via TARMED [16, 41]. Alongside TARMED, standard fee schedules – positive lists – regulate
and ensure
the reimbursement of diagnostic and laboratory services, medical devices and
items, medications and other expenses (e.g. therapies) [16]. Our document
analysis also drew our attention to essential palliative care services, including
support and relief for relatives and social counselling, that were not covered
by formal payers [14, 16, 41]. Instead, these services must be financed by
public service contracts, grants, donations or cross-financing [14].
Challenging areas
The reviewed
documents indicate that funding challenges are a major barrier to the implementation,
sustainability and further development of specialised paediatric palliative
care programmes [8, 40]. Difficulties attached to charging for services/covering
costs lead to deficits and funding gaps [8, 9, 17, 46]. Areas where funding challenges
are encountered include both the SwissDRG and the TARMED system [9, 14, 16, 37,
38, 40, 41, 43, 44]. Our document analysis suggests that variations between
cantonal funding regulations hinder the provision of inter-cantonal mobile palliative
care services [17, 37, 40]. In addition, dependencies on external funding (e.g.
donations, philanthropic contributions) pose a risk to long-term financial
stability [17, 41].
Modified Delphi study
Thirty-one
experts were invited for study participation, of whom 22 had been purposefully
identified by the study team and 9 recommended by initially contacted experts. Overall,
21 experts participated in the first Delphi round (68% response rate), 19 in
the second (10% dropout rate) and 15 in the third (21% dropout rate). Demographic
characteristics of the original 21 participating experts are presented in table
1. The participants were mostly female (n = 11, 52%), aged 50–69 years (n = 11,
52%) and working in (university) hospitals, clinics or other healthcare
providers (n = 14, 67%). Ten (48%) worked in medical/clinical professions,
including specialised paediatric palliative care programme leadership.
Table 1Demographic characteristics of participating
experts.
| Characteristics |
Experts, n = 21 |
| Sex, no (%) |
Female |
11 (52%) |
| Male |
10 (48%) |
| Age, no (%) |
30–49 |
10 (48%) |
| 50–69 |
11 (52%) |
| Primary
profession, no (%) |
Medical, clinical, specialised paediatric palliative
care programme leadership |
10
(48%) |
| Health policy, health economics, public health |
5
(24%) |
| Specialist in medical coding, payment systems,
service reimbursement |
4
(19%) |
| Research |
2
(10%) |
| Primary place of employment, no (%) |
(University) hospital, clinic, healthcare provider |
14
(67%) |
| Federal office, (semi-)governmental organisation |
3
(14%) |
| Association
(e.g. hospital / insurance association) |
2
(10%) |
| Other |
2
(10%) |
At the end
of round one, one list each of obstacles (n = 22) and priorities (n = 28)
regarding the funding of specialised paediatric palliative care programmes was
generated. After additional obstacles and priorities suggested in round two, round
three began with lists of 23 obstacles and 29 priorities. Obstacles and priorities
were grouped inductively into six categories: (1) Political and structural, (2)
Funding and tariff structures in general, (3) Inpatient tariff structures, (4) Outpatient
tariff structures, (5) Mobile palliative care and (6) Other. All identified obstacles
and priorities are presented in tables 2 and 3 respectively.
Table 2List of obstacles encountered in the funding of specialised
paediatric palliative care, sorted by category and most-to-least pressing.
| Category |
Obstacles encountered in the funding of specialised paediatric palliative care |
Most-to-least pressing |
| Political and structural |
1. No holistic health policy approach to the financing and funding of palliative care* |
6× |
| 2. Fragmentation of palliative care* funding rendering the establishment and maintenance
of integrated and well-performing treatment pathways more difficult |
4× |
| 3. Lack of guaranteed funding to develop and implement specialised paediatric palliative
care programms |
4× |
| 4. Lack of legal definition of palliative care* (e.g. services, providers and funding
needed to meet patients' palliative care*demand) |
3× |
| 5. Dependency on charitable funding, compromising long-term continuity and sustainability
of specialised paediatric palliative care programmes |
2× |
| 6. Cantonal differences regarding palliative care* service mandates and cost coverage
(e.g. financial contributions, coverage of residual costs) |
1× |
| Funding and tariff structures in general |
7. Gaps in palliative care* funding when patients transition between care settings
(e.g. inpatient, outpatient, home, rehabilitation) |
3× |
| 8. Insufficient compensation, billing limitations and lack of tariffs regarding certain
palliative care* services (e.g. roundtable meetings, case management, care coordination,
support for relatives) |
2× |
| 9. Patient classification and reimbursement difficulties arising from existing tariff
structures that fail to recognise the heterogeneity, multimorbidity and complexity
of the palliative care* population |
– |
| Inpatient tariff structures |
10. Insufficient reimbursement of inpatient service costs in the context of hight-deficit
palliative care* cases or palliative care* patients with complex case constellations
(i.e. high-deficit outliers) |
1× |
| 11. Difficulties in meeting the minimum criteria required for the palliative care
Complex Codes of the Swiss Classification of Operations (CHOPs) |
1× |
| 12. Funding challenges due to gaps between remuneration and hospital operating costs
in view of above-average operating costs, non-optimised processes, low base rates
or gaps in tariff structures |
– |
| Outpatient tariff structures |
13. Lack of palliative care*-specific reimbursement codes in outpatient tariff structures |
2× |
| 14. No reimbursement of bereavement support services or follow-up home visites to
bereaved families and caregivers |
2× |
| 15. Time limitations in the reimbursement of outpatient palliative care* services
(i.e. consultation time limits in TARMED for cases not reimbursed via the Swiss disability,
accident or military social insurance funds) |
– |
| 16. Lack of clarity on whether TARDOC, as a potential successor of TARMED, will improve
palliative care* service reimbursement (TARDOC contains tariff positions for palliative
care services provided by general practitioners and paediatricians) |
– |
| Mobile palliative care |
17. Difficulties in funding mobile palliative care* services, particularly non-direct
patient services (e.g. care coordination, consultations with other healthcare professionals) |
3× |
| Other |
18. Lack of financial support and relief for families and informal caregivers |
3× |
| 19. Challenges to palliative care* service reimbursement in long-term and home-care
settings |
2× |
| 20. Inconsistent definitions of palliative care cases and populations (e.g. neonates,
children, adolescents, adults, elderly) in discussions of funding issues |
1× |
| 21. Lack of educational and training opportunities in specialised paediatric palliative
care |
1× |
| 22. Insufficient evidence on specialised paediatric palliative care's (cost-)effectiveness
in the Swiss setting |
1× |
| 23. Lack of national regulations about the inclusion, status and funding of (paediatric)
hospices |
– |
Table 3List of priorities in the funding of specialised
paediatric palliative care, sorted by category and most-to-least urgent.
| Category |
Priorities in the funding of specialised paediatric palliative care |
Most-to-least urgent |
| Political and structural |
1. Harmonisation of palliative care* regulations (e.g. service mandates, financing)
and closer inter-cantonal cooperation and coordination in palliative care* provision |
5× |
| 2. Funding and support for integrated palliative care* programmes, well-performing
treatment pathways and closer cooperation and coordination among service providers |
4× |
| 3. Development of specific, feasible and viable funding solutions to ensure long-term
funding of specialised paediatric palliative care programmes |
4× |
| 4. Legislative integration of palliative care* into the Swiss Federal Health Insurance
Act (KVG) and the Swiss Health Care Benefits Ordinance (KLV) |
4× |
| 5. Initiation of a nationwide working group (including decision-making bodies) for
securing long-term funding in specialised paediatric palliative care |
3× |
| 6. Provision of financial resources (initial funding, core funding) to establish specialised
paediatric palliative care programmes and facilitate nationwide coverage |
2× |
| 7. Comprehensive analysis of palliative care* demand, supply and funding, including
the identification and disclosure of potential gaps |
2× |
| 8. Establishment of a legal framework for the reimbursement of consultative palliative
care* services |
1× |
| Funding and tariff structures in general |
9. Amendment of palliative care* services (including psychosocial, spiritual services)
as standard benefits in the Swiss Statutory Health Insurance (OKP) scheme |
1× |
| 10. Clarification of open questions regarding the reimbursement of palliative care*
services provided when patients transition between care settings (e.g. inpatient,
outpatient, home, rehabilitation) |
1× |
| 11. Revision, further development and supplementation of services provided in the
patient’s absence in established tariff structures (e.g. interprofessional meetings,
case management, care coordination) |
– |
| 12. A comprehensive, palliative care-specific revision of payment systems and reimbursement
mechanisms to improve palliative care* funding conditions in the medium term |
– |
| 13. A flexible application of tariff rules, explicitly approved by formal payers,
to improve palliative care* funding conditions in the short term (e.g. via analogous
positions)
|
– |
| Inpatient tariff structures |
14. Sufficient reimbursement of inpatient service costs in the context of high-deficit
palliative care* cases or palliative care* patients with complex case constellations
(i.e. high-deficit outliers) |
1× |
| 15. Assuring the quality of data supplied by service providers to SwissDRG AG (when
adequate data becomes available, palliative care* patient and service classification
improvements in inpatient tariff structures can be realised through system maintenance) |
– |
| 16. Broader application of palliative care DRG complex codes through the respective
certification (quality label) of specialised paediatric palliative care programmes |
– |
| 17. Consideration of structural factors not currently considered regarding SwissDRG
at the hospital and patient level in setting base rates |
– |
| Outpatient tariff structures |
18. Sufficient, cost-covering reimbursement of outpatient palliative care* services
(e.g. interprofessional meetings, travel time for home visits) |
2× |
| 19. Reduction of quantity and time limitations in the reimbursement of outpatient
palliative care* services (e.g. reduction of consultation time limits in TARMED) |
2× |
| 20. Introduction of palliative care*-specific counselling and coordination fees in
outpatient tariff structures (i.e. tariff codes for palliative care* case management) |
1× |
| 21. Reimbursement for bereavement support services provided to families and caregivers |
1× |
| Mobile palliative care |
22. Establishment of mobile palliative care* funding regulations in all cantons |
– |
| 23. Funding of mobile palliative care* services based on the area’s palliative care*
demand, not contingent on fluctuating case numbers |
– |
| Other |
24. Establishment of a valid nationwide database on palliative care* provision, in
coordination with the Spitalstationäre Gesundheitsversorgung (SpiGes) project of the Federal Office of Public Health and the Federal Statistical
Office |
4× |
| 25. Financial support/relief for palliative care* patients’ families and informal
caregivers |
3× |
| 26. Development of educational and training opportunities in the field of palliative
care* (including medical curricula) |
2× |
| 27. Facilitation of research on specialised paediatric palliative care's (cost-)effeciveness |
1× |
| 28. Furthering knowledge and understanding of tariff structures to optimise the coding
and billing of palliative care*services |
1× |
| 29. Ensuring cost-covering financing of palliative care* services in non-hospital
settings (e.g. hospices, psychiatric clinics, long-term institutions) |
– |
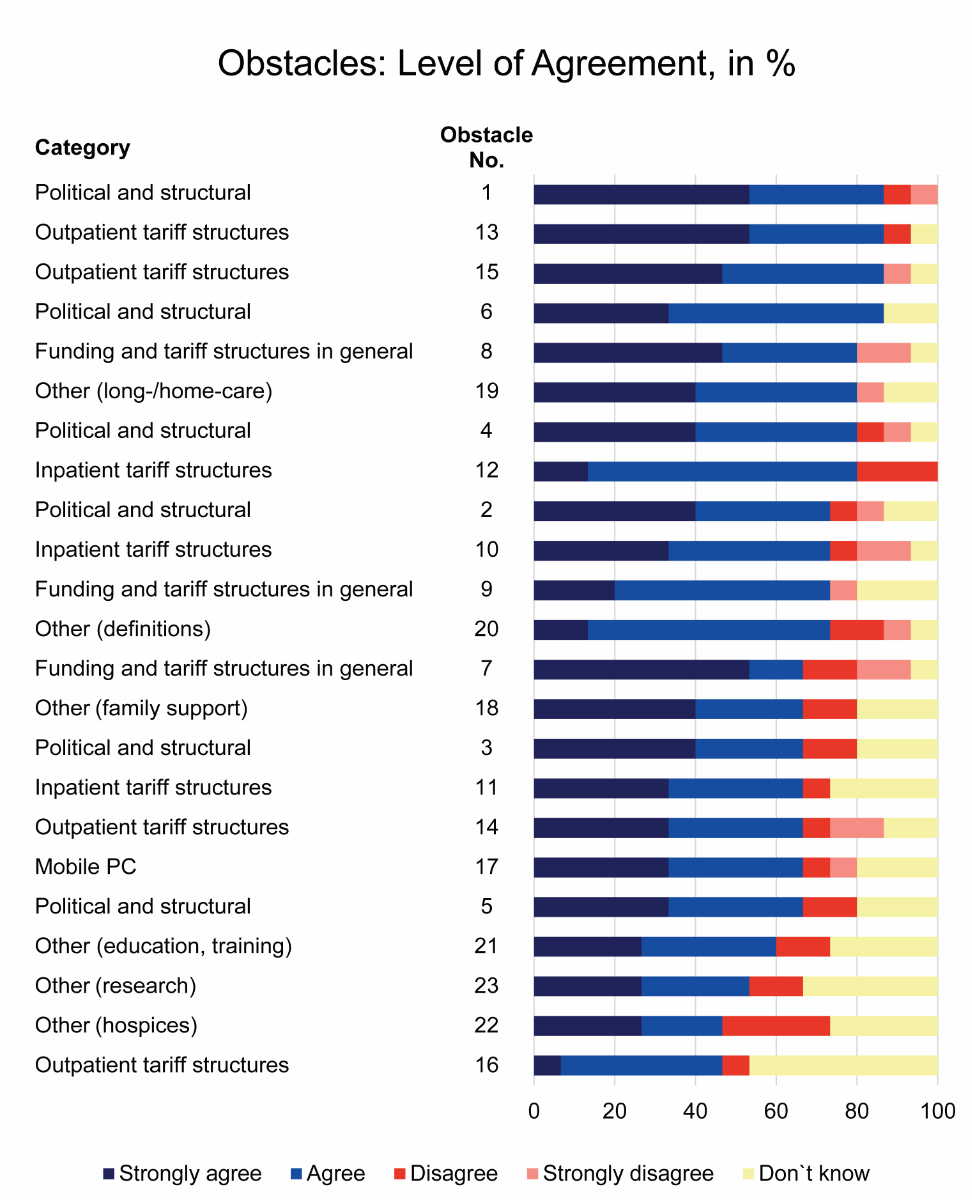
Obstacles
Using our
predefined consensus definition of >70% of experts either strongly agreeing
or agreeing (level of agreement), consensus was obtained on 12 of the 23 identified
obstacles. A level of agreement of >85% was obtained for four obstacles: “Absence
of a holistic health policy approach”, “Cantonal differences in service
mandates and cost coverage”, “Lack of palliative care-specific reimbursement
codes in outpatient tariff structures” and “Existent consultation time
limitations in the reimbursement of certain palliative care outpatient services
in TARMED”. Zero disagreement was recorded regarding difficulties arising from
cantonal differences in palliative care service mandates and cost coverage. The
distribution of the level of agreement of identified obstacles is shown in figure
2.
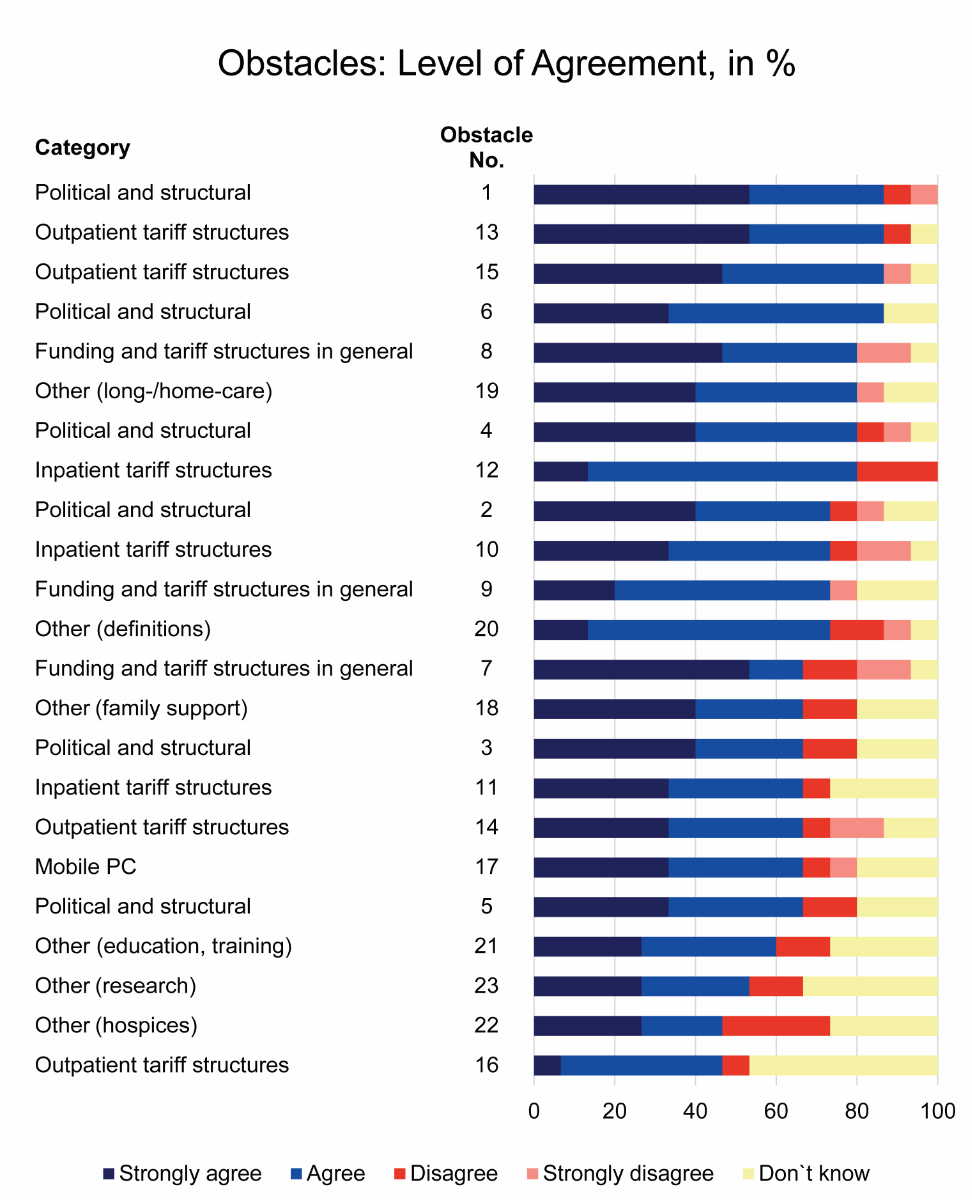
Figure 2Distribution
of the level of agreement of identified obstacles encountered in specialised
paediatric palliative care funding in Switzerland, sorted by level of
agreement. Obstacle numbers refer to the numbered obstacles provided in table
2. PC: palliative
care.
Asked to
indicate the three most pressing obstacles, participating experts indicated 18
obstacles as most pressing at least once. The obstacle most frequently named – six
times – was “Absence of a holistic health policy approach”. “Fragmentation of palliative
care funding” and “Lack of guaranteed funding for developing and implementing new
specialised paediatric palliative care programmes” were indicated four times each.
Obstacles indicated as one of the most pressing fell predominantly within the
political and structural category (table 2).
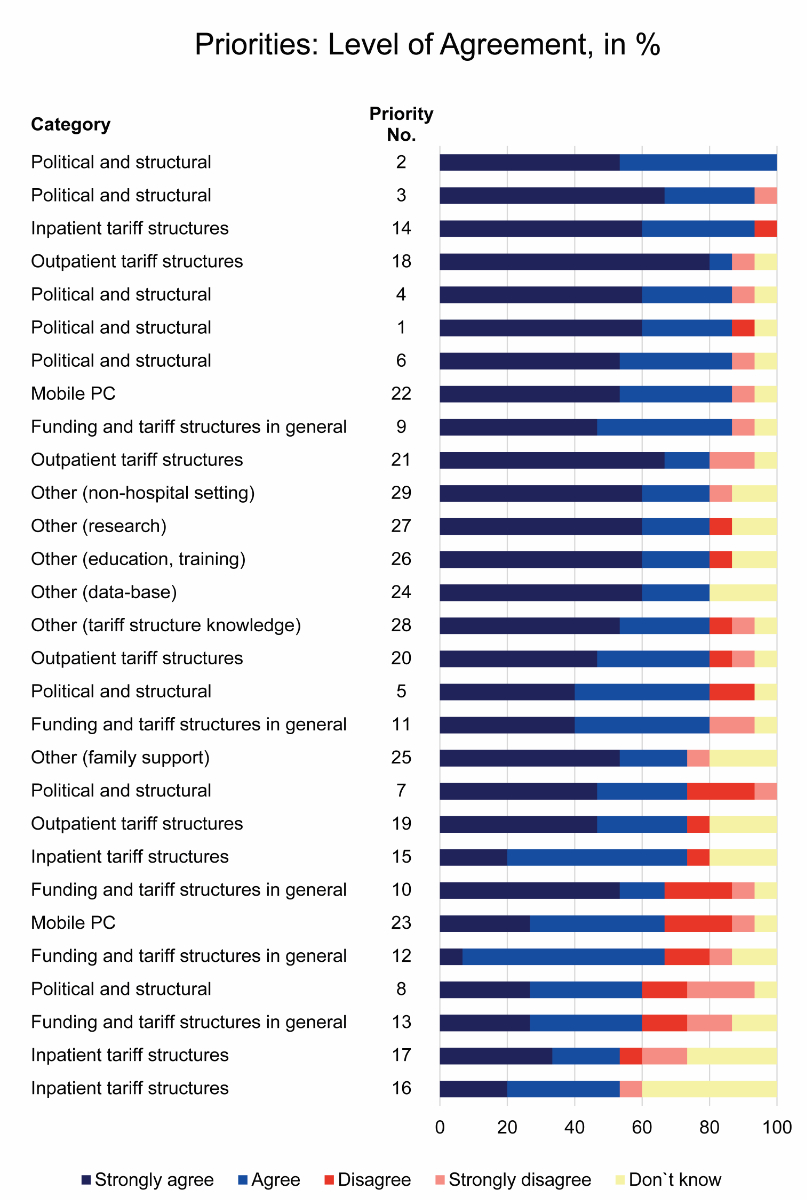
Priorities
A level of
agreement >70% was measured for 22 of the 29 identified priorities. Three priorities
had consensus rates of >90%: “The development of financing solutions to
ensure the long-term funding of specialised paediatric palliative care
programmes”, “The provision of funding and support for integrated palliative
care programmes” and “Sufficient reimbursement of inpatient service costs in
the context of high-deficit palliative care cases”. Zero disagreement was
recorded for two priorities: “Establishing a valid nationwide database on palliative
care provision and offering funding and support for integrated palliative care
programmes, well-performing treatment pathways” and “Closer cooperation and
coordination among service providers”. The distribution of agreement levels of
identified priorities is shown in figure 3.
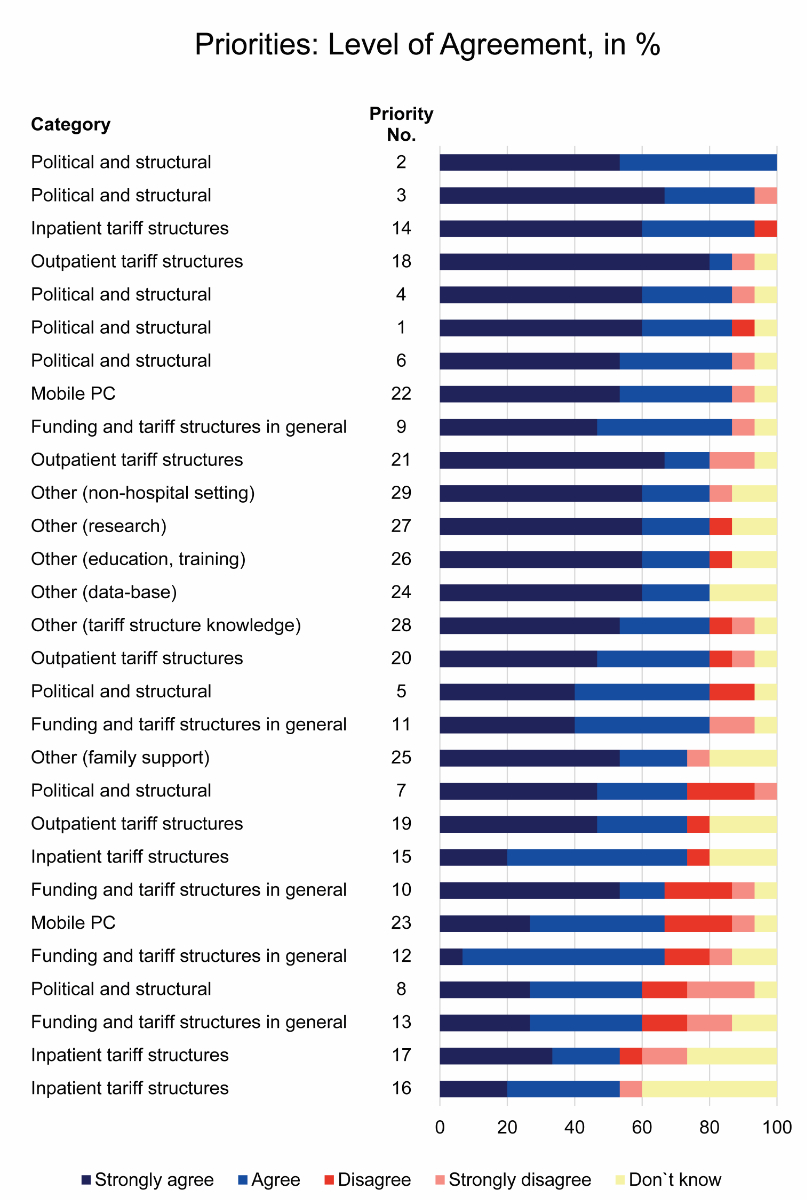
Figure 3Distribution
of the level of agreement of identified priorities for specialised paediatric
palliative care funding in Switzerland, sorted by level of agreement. Priority
numbers refer to the numbered priorities provided in table 3. PC: palliative
care.
When asked
to indicate what they considered the three most urgent priorities, participating
experts noted a wide range of priorities (n = 20). Most experts’ top priorities
fall within the political and structural category: “Inter-cantonal harmonisation
of palliative care regulations” was indicated five times; “Development of
financing solution to ensure long-term funding of specialised paediatric
palliative care services”, “Legislative integration of palliative care” and “Financing
and support of integrated palliative care programmes” were indicated four times
each. Additionally, experts indicated four times that they considered the
establishment of a valid nationwide database on palliative care provision one
of the most urgent priorities (table 3).
Discussion
Our
conceptualisation of the funding of hospital-based consultative specialised
paediatric palliative care programmes in Switzerland (figure 1) shows that funding
flows and financial arrangements surrounding the provision of SPPC are highly fragmented.
In many cases, donations and philanthropic contributions are required to
supplement funding from formal structures. Several obstacles impede the funding
of SPPC. Overall, our modified Delphi study identified 23 obstacles and 29 priorities
regarding SPPC funding. Consensus was reached on 12 of the obstacles and 22 of
the priorities. The large numbers of both identified obstacles and priorities are
notable, as both lists are samples of issues encountered in the funding of
hospital-based consultative SPPC programmes. The contributing experts considered
many of both lists as very pressing, suggesting that, while no single specific
obstacle or priority emerged as most important, a set of each require urgent
action.
This study’s
findings also bolster the results of a previous investigation on funding models
in palliative care [22]. It was shown that a high degree of fragmentation in
funding sources can increase administrative complexities and create ambiguity
in responsibilities [22]. The fragmentation in funding sources, payment systems
and reimbursement mechanisms has several important implications for the
development, implementation and sustainability of specialised paediatric
palliative care programmes.
First, high
levels of administrative complexity associated with SPPC funding are likely to hinder
the development and implementation of new SPPC programmes and may, at least
partially, explain why nationwide coverage of SPPC has not yet been achieved in
Switzerland [8, 9]. Stable funding, with a streamlined system of payment and
reimbursement, may greatly facilitate the establishment of new programmes [47].
Second,
reliance on annual grants to cover operating costs can actually endanger a
programme’s long-term survival. For example, as both charitable foundations’
and cantonal governments’ budgets can freeze or dry up, dependence on either
can pose serious risks to the long-term sustainability of SPPC programmes.
Third, fragmentation
and complexity in funding of specialised paediatric palliative care programmes may
make it more difficult to estimate how and where funding sources, payment
systems and reimbursement mechanisms act as policy levers. Palliative care
funding has recently become the focus of growing political attention in
Switzerland [41]. In June 2021, parliamentary motion no 20.4264 on palliative
care financing was passed, instructing the Federal Council to establish a statutory
basis to guarantee needs-based palliative and end-of-life treatment and care
for all people [48].
Politically
and structurally, the findings of our modified Delphi study suggest that
further legislative integration and specification regarding palliative care
funding is needed. Parliamentary motion no 20.4264 [48] provides a unique
opportunity to clarify open legal questions. Moreover, participating experts
agreed that a nationwide working group should initiate work on securing
long-term funding for SPPC. When executing parliamentary motion no
20.4264 [48], the Federal Office of Public Health established two dedicated
working groups: one for palliative care supply and demand, the other for palliative
care financing. Ideally, these groups will commission a comprehensive analysis
of SPPC demand, supply and funding. In addition to identifying potential gaps
in SPPC supply, such an analysis would facilitate development of viable
long-term funding solutions.
Additionally,
experts participating in our modified Delphi study agreed that differences in
service mandates and funding regulations among Swiss cantons are an obstacle. Although
most cantons have established legislation to promote palliative care [17], the
details of these measures are rather heterogenous. Therefore, even though tailored
canton-level solutions for specialised paediatric palliative care funding may
provide flexibility in establishing new programmes, local differences may hamper
the provision of inter-cantonal SPPC services (e.g. mobile SPPC teams).
Our
findings also indicate that charitable sources contribute disproportionately to
the current funding of hospital-based consultative specialised paediatric
palliative care programmes in Switzerland: a recent report suggests that donations
and philanthropic contributions cover up to 50% of annual SPPC programme budgets
[8]. In our study, participating experts warned that reliance on donations and
philanthropic contributions compromises long-term continuity and sustainability.
Regarding
inpatient tariff structures, participating experts agreed that, in the context
of high-deficit palliative care cases, i.e. high-deficit outliers, improvements
in the reimbursement of inpatient stay costs are required. Generally, compared
with the total number of hospitalised patients, high-deficit outliers are a
small number of patients that cause a substantial proportion of total inpatient
stay costs [49–51]. Considering that specialised paediatric palliative care cases
are often highly complex [52], high-deficit outliers can be expected to be more
prevalent in this patient population. Sufficient reimbursement of these
patients’ treatment costs should thus be ensured.
Several
obstacles and priorities identified in this study further indicate that certain
palliative care activities are reimbursed insufficiently. These include but are
not limited to care coordination, case management, consultations of other
healthcare professionals and psychosocial and spiritual support. Previous
research suggests that insufficient financing mechanisms constrain access to specialised
paediatric palliative care [53, 54]. This issue is particularly evident in
outpatient palliative care. One identified obstacle is that certain palliative
care services are only partially billable, if at all, via outpatient tariff
structures. Besides the services outlined above, those provided to family
members and other informal caregivers, including psychosocial and bereavement
support, are especially prone to reimbursement failures. Related issues regarding
these services have also been documented previously [14, 16, 38, 41]. Whether
TARDOC, as a potential successor of TARMED, will improve the reimbursement of
outpatient services provided by hospital-based consultative SPPC programmes
remains unclear.
Strengths and
limitations
The
conceptual model developed provides a systemic understanding of how
hospital-based consultative specialised paediatric palliative care programmes are
funded. While informing clinical and administrative leaders regarding the
development and implementation of new SPPC programmes, it serves as a point of
reference regarding funding issues, e.g. how to address them through policies
and regulations. Given that, with high levels of agreement among experts, we
have identified a broad spectrum of obstacles, we believe that our findings accurately
reflect the issues encountered in SPPC funding. Initiatives aiming to improve SPPC
funding models should focus on addressing the priorities identified above.
Several
notable limitations affect this study. First, it was not always possible to
strictly distinguish between specialised paediatric palliative care and overall
palliative care information. Therefore, we included documents on the funding of
both SPPC and palliative care in general in our document analysis. Second, several
experts participating in the modified Delphi study were experts not in SPPC but
in palliative care funding. Third, our approach to conducting the modified
Delphi study precluded us from defining the identified obstacles and priorities
in greater detail. As a result, a number of obstacles and priorities are stated
rather broadly. In addition, as this study aimed to quantify neither funding
flows nor the financial impacts of identified obstacles and priorities, we
recommend both topics as the subjects of further research. Future research may
also explore funding issues in other paediatric palliative care settings, e.g.
home care or children’s hospices.
Conclusion
Current
funding of hospital-based consultative SPPC programmes in Switzerland is highly
fragmented and characterised by a complex combination of public, private and charitable
funding. With new SPPC programmes currently being developed and implemented, a comprehensive
review of current funding structures and actual funding requirements is
urgently needed.
We hope
that the obstacles and priorities identified in this study will help
researchers and policymakers develop funding and reimbursement schemes that
will appropriately support specialised paediatric palliative care provision in
the future.
Data sharing
statement
The data
that support the findings of this study are available on request from the first
author, stefan.mitterer [at]unibas.ch.
Acknowledgments
We warmly
thank all the experts who participated in our modified Delphi study for their
valuable time and expertise. Furthermore, we would like to thank Chris Shultis
for his editorial assistance.
Karin
Zimmermann, PhD, RN
Institute
of Nursing Science
Department
of Public Health
University
of Basel
CH-4000 Basel
karin.zimmermann[at]unibas.ch
References
1. Fraser LK, Miller M, Hain R, Norman P, Aldridge J, McKinney PA, et al. Rising national
prevalence of life-limiting conditions in children in England. Pediatrics. 2012 Apr;129(4):e923–9.
10.1542/peds.2011-2846
2. Fraser LK, Gibson-Smith D, Jarvis S, Norman P, Parslow RC. Estimating the current
and future prevalence of life-limiting conditions in children in England. Palliat
Med. 2021 Oct;35(9):1641–51. 10.1177/0269216320975308
3. Jennessen S, Burgio NM. Erhebung der Prävalenz von Kindern und Jugendlichen mit lebensbedrohlichen
und lebensverkürzenden Erkrankungen in Deutschland (PraeKids). 2022. https://doi.org/10.18452/24740. accessed 08.11.2022. https://edoc.hu-berlin.de/handle/18452/25451
4. Norman P, Fraser L. Prevalence of life-limiting conditions in children and young people
in England: time trends by area type. Health Place. 2014 Mar;26:171–9. 10.1016/j.healthplace.2014.01.002
5. Nageswaran S, Hurst A, Radulovic A. Unexpected Survivors: Children With Life-Limiting
Conditions of Uncertain Prognosis. Am J Hosp Palliat Care. 2018 Apr;35(4):690–6. 10.1177/1049909117739852
6. Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, Bhatnaghar S, et al. Redefining Palliative
Care-A New Consensus-Based Definition. J Pain Symptom Manage. 2020 Oct;60(4):754–64.
10.1016/j.jpainsymman.2020.04.027
7. World Health Organization. Integrating palliative care and symptom relief into paediatrics:
a WHO guide for health-care planners, implementers and managers. 2018. pp. 5–9. [],
https://apps.who.int/iris/handle/10665/274561
8. Gesundheitsobservatorium S. Gesundheit in der Schweiz - Kinder, Jugendliche und junge
Erwachsene: Nationaler Gesundheitsbericht 2020. 2020: p. 323. accessed 29.03.2022.
https://www.bfs.admin.ch/bfs/de/home.assetdetail.14147105.html
9. Amstad H. Palliative Care für vulnerable Patientengruppen: Konzept zuhanden der Plattform
Palliative Care des Bundesamtes für Gesundheit. 2020. accessed 14.04.2022. https://www.plattform-palliativecare.ch/arbeiten/zugang-zu-palliative-care-fuer-vulnerable-gruppen-verbessern
10. Bundesamt für Gesundheit und Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen
und -direktoren, Rahmenkonzept Palliative Care Schweiz. Eine definitorische Grundlage
für die Umsetzung der «Nationalen Strategie Palliative Care». 2014. accessed 09.01.2023.
https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/strategie-palliative-care/grundlagen-zur-strategie-palliative-care/rahmenkonzept-palliative-care.html
11. Benini F, Papadatou D, Bernadá M, Craig F, De Zen L, Downing J, et al. International
Standards for Pediatric Palliative Care: From IMPaCCT to GO-PPaCS. J Pain Symptom
Manage. 2022 May;63(5):e529–43. 10.1016/j.jpainsymman.2021.12.031
12. Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, et al. Pediatric palliative
care programs in children’s hospitals: a cross-sectional national survey. Pediatrics.
2013 Dec;132(6):1063–70. 10.1542/peds.2013-1286
13. Bergsträsser E, Abbruzzese R, Marfurt K, and Hošek M, Konzept Pädiatrische Palliative
Care University Children’s Hospital Zurich. 2010. Version 2015. accessed 17.10.2022.
https://docplayer.org/29201365-Konzept-paediatrische-palliative-care-autoren-palliative-care-pd-dr-med-eva-bergstraesser-und-ppc-team.html
14. Wächter M, Bommer A. Mobile Palliative-Care-Dienste in der Schweiz - Eine Bestandsaufnahme
aus der Perspektive dieser Anbieter. 2014. accessed 21.09.2021. https://www.palliative.ch/de/fachbereich/aktuell/grundlagendokumente/
15. Bundesamt für Gesundheit und Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen
und -direktoren, Nationale Strategie Palliative Care 2010–2012. 2009. accessed 12.01.2022.
https://www.bag.admin.ch/dam/bag/de/dokumente/nat-gesundheitsstrategien/strategie-palliative-care/nationale-strategie-palliative-care-2010-2012.pdf.download.pdf/10_D_Nationale_Strategie_Palliative_Care_2010-2012.pdf
16. Furrer MT, Grünig A, Coppex P. Finanzierung der Palliative-Care-Leistungen der Grundversorgung
und der spezialisierten Palliative Care (ambulante Pflege und Langzeitpflege). 2013.
accessed 06.08.2021. https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/strategie-palliative-care/versorgung-und-finanzierung-in-palliative-care/finanzierung-der-palliative-care.html
17. Liechti L, Künzi K. Stand und Umsetzung von Palliative Care in den Kantonen: Ergebnisse
der Befragung der Kantone und Sektionen von palliative ch 2018. 2019. accessed 06.08.2021.
https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/strategie-palliative-care/grundlagen-zur-strategie-palliative-care/befragung-der-kantone-zu-palliative-care.html
18. De Pietro C, Camenzind P, Sturny I, Crivelli L, Edwards-Garavoglia S, Spranger A,
et al. Switzerland: health system review. Health Syst Transit. 2015;17(4):1–288.
19. Bundesamt für Gesundheit. Health insurance: Co-payment for persons resident in Switzerland. 2020 accessed 14.01.2022; Available from: https://www.bag.admin.ch/bag/en/home/versicherungen/krankenversicherung/krankenversicherung-versicherte-mit-wohnsitz-in-der-schweiz/praemien-kostenbeteiligung/kostenbeteiligung.html
20. Invalidenversicherung, Leistungen der Invalidenversicherung (IV) für Kinder und Jugendliche.
2022. 4.16-22/01-D. accessed 14.01.2022. https://www.ahv-iv.ch/p/4.16.d
21. Bundesgesetz über die Invalidenversicherung. Art. 14 Kostenvergütung für stationäre
Behandlungen. 1959 (01.01.2022). accessed 14.01.2022. https://www.fedlex.admin.ch/eli/cc/1959/827_857_845/de
22. Groeneveld EI, Cassel JB, Bausewein C, Csikós Á, Krajnik M, Ryan K, et al. Funding
models in palliative care: lessons from international experience. Palliat Med. 2017 Apr;31(4):296–305.
10.1177/0269216316689015
23. Feudtner C, Faerber JA, Rosenberg AR, Kobler K, Baker JN, Bowman BA, et al. Prioritization
of Pediatric Palliative Care Field-Advancement Activities in the United States: Results
of a National Survey. J Pain Symptom Manage. 2021 Sep;62(3):593–8. 10.1016/j.jpainsymman.2021.01.007
24. Earp JA, Ennett ST. Conceptual models for health education research and practice.
Health Educ Res. 1991 Jun;6(2):163–71. 10.1093/her/6.2.163
25. Brady SS, Brubaker L, Fok CS, Gahagan S, Lewis CE, Lewis J, et al.; Prevention of
Lower Urinary Tract Symptoms (PLUS) Research Consortium. Development of Conceptual
Models to Guide Public Health Research, Practice, and Policy: Synthesizing Traditional
and Contemporary Paradigms. Health Promot Pract. 2020 Jul;21(4):510–24. 10.1177/1524839919890869
26. Deber R, Hollander MJ, Jacobs P. Models of funding and reimbursement in health care:
a conceptual framework. Can Public Adm. 2008;51(3):381–405. 10.1111/j.1754-7121.2008.00030.x
27. Bowen GA. Document analysis as a qualitative research method. Qual Res J. 2009;9(2):27–40.
10.3316/QRJ0902027
28. Dalglish SL, Khalid H, McMahon SA. Document analysis in health policy research: the
READ approach. Health Policy Plan. 2021 Feb;35(10):1424–31. 10.1093/heapol/czaa064
29. Okoli C, Pawlowski SD. The Delphi method as a research tool: an example, design considerations
and applications. Inf Manage. 2004;42(1):15–29. 10.1016/j.im.2003.11.002
30. Dalkey N, Helmer O. An experimental application of the Delphi method to the use of
experts. Manage Sci. 1963;9(3):458–67. 10.1287/mnsc.9.3.458
31. Barrett D, Heale R. What are Delphi studies? Evid Based Nurs. 2020 Jul;23(3):68–9.
10.1136/ebnurs-2020-103303
32. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique.
J Adv Nurs. 2000 Oct;32(4):1008–15. 10.1046/j.1365-2648.2000.t01-1-01567.x
33. Loughlin KG, Moore LF. Using Delphi to achieve congruent objectives and activities
in a pediatrics department. J Med Educ. 1979 Feb;54(2):101–6. 10.1097/00001888-197902000-00006
34. Whitman NI. The committee meeting alternative. Using the Delphi technique. J Nurs
Adm. 1990;20(7-8):30–6. 10.1097/00005110-199007000-00008
35. McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv
Nurs. 1994 Jun;19(6):1221–5. 10.1111/j.1365-2648.1994.tb01207.x
36. Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining
consensus: a systematic review recommends methodologic criteria for reporting of Delphi
studies. J Clin Epidemiol. 2014 Apr;67(4):401–9. 10.1016/j.jclinepi.2013.12.002
37. Degen E, Liebig B, Reeves E, Schweighoffer R. Palliative Care in der Schweiz. Die
Perspektive der Leistungserbringenden. 2020. accessed 13.08.2021. https://www.palliative.ch/fileadmin/user_upload/palliative/fachwelt/B_Aktuell/200608_Palliative_Care_in_der_Schweiz_-_die_Perspektive_der_Leistungserbringenden.pdf
38. Bundesamt für Gesundheit und Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen
und -direktoren, Stand und Umsetzung von Palliative Care in den Kantonen Ende 2011.
2012. accessed 21.09.2021. https://www.bag.admin.ch/bag/de/home/suche.html#kantone%20stand%20umsetzung%20palliative%20care%202012
39. Wyss N, Coppex P. Stand und Umsetzung von Palliative Care in den Kantonen 2013. 2013.
accessed 21.09.2021. https://www.bag.admin.ch/bag/de/home/suche.html#kantone%20stand%20umsetzung%20palliative%20care%202012
40. Bundesamt für Gesundheit und Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen
und -direktoren, Nationale Strategie Palliative Care 2013–2015. 2012. accessed 13.08.2021.
https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/strategie-palliative-care.html#-163315092
41. Bundesamt für Gesundheit. Bessere Betreuung und Behandlung von Menschen am Lebensende:
Bericht des Bundesrates in Erfüllung des Postulates 18.3384 der Kommission für soziale
Sicherheit und Gesundheit des Ständerats (SGK-SR) vom 26. April 2018. 2020. accessed
06.08.2021. https://www.bag.admin.ch/dam/bag/de/dokumente/cc/bundesratsberichte/2020/bessere-betreuung-am-lebensende.pdf.download.pdf/200918_Bericht_Po_183384_Lebensende.pdf
42. Franziska S. Das SwissDRG-System und die Finanzierung der palliativmedizinischen Versorgung.
palliative ch - Finanzierung, 2016. 2-2016. accessed 13.08.2021. https://www.palliative.ch/de/fachbereich/zeitschrift/archiv/
43. Gudat H. Ist das Vergütungssystem der SwissDRG AG für spezialisierte Palliative Care
geeignet? Die Pro-Position. palliative ch - Finanzierung, 2016. 02-2016. accessed
13.08.2021. https://www.palliative.ch/de/fachbereich/zeitschrift/archiv/
44. Borasio GD. Ist das Vergütungssystem der SwissDRG AG für spezialisierte Palliative
Care geeignet? Die Kontra-Position. palliative ch - Finanzierung, 2016. 2-2016. accessed
13.08.2021. https://www.palliative.ch/de/fachbereich/zeitschrift/archiv/
45. Swiss DR. Beschluss des Verwaltungsrats der SwissDRG AG: Abbildung der palliativmedizinischen
Behandlung im SwissDRG Tarifsystem. 2016. accessed 13.08.2021. https://www.swissdrg.org/de/ueber-uns/verwaltungsrat/kommunikation
46. Gudat H. Der Wert des Lebensendes: am Beispiel der Finanzierung der stationären spezialisierten
Palliative Care in der Schweiz. Ther Umsch. 2018 Jul;75(2):127–34. 10.1024/0040-5930/a000978
47. Pelant D, McCaffrey T, Beckel J. Development and implementation of a pediatric palliative
care program. J Pediatr Nurs. 2012 Aug;27(4):394–401. 10.1016/j.pedn.2011.06.005
48. Motion 20.4264. Für eine angemessene Finanzierung der Palliative Care. 2020. accessed
13.10.2022. https://www.parlament.ch/de/ratsbetrieb/suche-curia-vista/geschaeft?AffairId=20204264
49. Pirson M, Dramaix M, Leclercq P, Jackson T. Analysis of cost outliers within APR-DRGs
in a Belgian general hospital: two complementary approaches. Health Policy. 2006 Mar;76(1):13–25.
10.1016/j.healthpol.2005.04.008
50. Cots F, Mercadé L, Castells X, Salvador X. Relationship between hospital structural
level and length of stay outliers. Implications for hospital payment systems. Health
Policy. 2004 May;68(2):159–68. 10.1016/j.healthpol.2003.09.004
51. Mehra T, Müller CT, Volbracht J, Seifert B, Moos R. Predictors of High Profit and
High Deficit Outliers under SwissDRG of a Tertiary Care Center. PLoS One. 2015 Oct;10(10):e0140874.
10.1371/journal.pone.0140874
52. Baumann F, Hebert S, Rascher W, Woelfle J, Gravou-Apostolatou C. Clinical Characteristics
of the End-of-Life Phase in Children with Life-Limiting Diseases: Retrospective Study
from a Single Center for Pediatric Palliative Care. Children (Basel). 2021 Jun;8(6):523.
10.3390/children8060523
53. Haines ER, Frost AC, Kane HL, Rokoske FS. Barriers to accessing palliative care for
pediatric patients with cancer: A review of the literature. Cancer. 2018 Jun;124(11):2278–88.
10.1002/cncr.31265
54. Williams-Reade J, Lamson AL, Knight SM, White MB, Ballard SM, Desai PP. Paediatric
palliative care: a review of needs, obstacles and the future. J Nurs Manag. 2015 Jan;23(1):4–14.
10.1111/jonm.12095
Appendix: Overview of included documents
| Type (year) |
Publisher; author(s) |
Title |
Content category |
| Funding sources |
Payment
systems and reimbursement mechanisms |
Areas of challenges |
| Report (2020) |
Swiss Health Observatory; Peter C.,
Diebold M., Delgrande Jordan M., Dratva J., Kickbusch I., Stronski S. |
Gesundheit in der Schweiz – Kinder,
Jugendliche und junge Erwachsene: Nationaler Gesundheitsbericht 2020 [8] |
X |
|
X |
| Report (2020) |
Amstad H. |
Palliative Care für vulnerable
Patientengruppen: Konzept zuhanden der Plattform Palliative Care des
Bundesamtes für Gesundheit [9] |
X |
X |
X |
| Report / Strategy Paper (2012) |
Bundesamt für Gesundheit BAG,
Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und
-direktoren GDK |
Nationale Strategie Palliative Care
2013–2015: Bilanz «Nationale Strategie Palliative Care 2010–2012» und
Handlungsbedarf 2013–2015 [40] |
|
|
X |
| Report (2020) |
Bundesamt für Gesundheit BAG |
Bessere Betreuung und Behandlung von
Menschen am Lebensende: Bericht des Bundesrates in Erfüllung des Postulates
18.3384 der Kommission für soziale Sicherheit und Gesundheit des Ständerats
(SGK-SR) [41] |
X |
X |
X |
| Report (2019) |
Bundesamts für Gesundheit; Liechti L.,
Künzi K., Büro für arbeits- und sozialpolitische Studien BASS |
Stand und Umsetzung von Palliative Care
in den Kantonen: Ergebnisse der Befragung der Kantone und Sektionen von
palliative ch 2018 [17] |
X |
|
X |
| Report (2013) |
Bundesamt für Gesundheit BAG,
Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und
-direktoren GDK; Furrer M.T., Grünig A., Coppex P. |
Finanzierung der
Palliative-Care-Leistungen der Grundversorgung und der spezialisierten
Palliative Care (ambulante Pflege und Langzeitpflege) [16] |
X |
X |
X |
| Review (2018) |
Gudat H. |
Der Wert des Lebensendes: am Beispiel der
Finanzierung der stationären spezialisierten Palliative Care in der Schweiz [46] |
X |
X |
X |
| Directive (2016) |
SwissDRG AG |
Beschluss des Verwaltungsrats der
SwissDRG AG: Abbildung der palliativmedizinischen Behandlung im SwissDRG
Tarifsystem [45] |
|
X |
|
| Report (2020) |
Degen E., Liebig B., Reeves E.,
Schweighoffer R. |
Palliative Care in der Schweiz: Die
Perspektive der Leistungserbringenden [37] |
X |
X |
X |
| Article (2016) |
palliative ch; Schlägel F. |
Das SwissDRG-System und die Finanzierung
der palliativmedizinischen Versorgung [42] |
|
X |
|
| Article (2016) |
palliative ch; Gudat H. |
Ist das Vergütungssystem der SwissDRG AG
für spezialisierte Palliative Care geeignet? Die Pro-Position [43] |
|
X |
X |
| Article (2016) |
palliative ch; Borasio G.D. |
Ist das Vergütungssystem der SwissDRG AG
für spezialisierte Palliative Care geeignet? Die Kontra-Position [44] |
|
X |
X |
| Report (2014) |
Wächter M., Bommer A. |
Mobile Palliative-Care-Dienste in der
Schweiz - Eine Bestandsaufnahme aus der Perspektive dieser Anbieter [14] |
X |
X |
X |
| Report (2012) |
Bundesamt für Gesundheit BAG,
Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und
-direktoren GDK |
Stand und Umsetzung von Palliative Care
in den Kantonen Ende 2011 [38] |
|
|
X |
| Report (2013) |
Bundesamt für Gesundheit BAG,
Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und
-direktoren GDK; Wyss N., Coppex P. |
Stand und Umsetzung von Palliative Care in
den Kantonen 2013 [39] |
|
|
X |