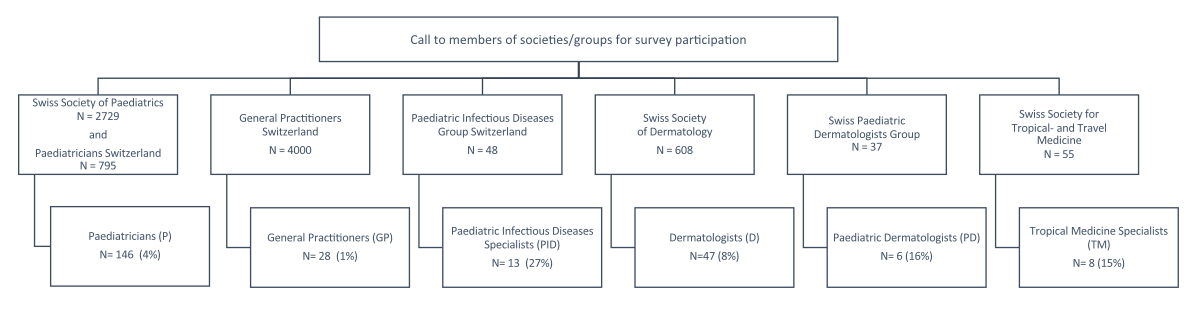
Figure 1Participation flowchart. Societies and groups with the number of members contacted through electronic mail. The number and percentage of survey participants by speciality.
DOI: https://doi.org/https://doi.org/10.57187/smw.2023.40129
Scabies, caused by infestation with the mite Sarcoptes scabiei var. hominis, is a contagious ectoparasitic dermatosis affecting all age groups, but particularly children [1, 2]. The global prevalence of scabies was estimated at 175 million across all age groups in 2017 [3]. Scabies-associated disability-adjusted life-years (DALYs) are highest in children aged 1–4 years [4]. In Europe, it is currently believed that scabies prevalence is rising mainly due to the influx of migrant populations. However, many countries, including Switzerland, lack national surveillance systems to formally monitor scabies [5–7].
Effective scabies management is challenging in children. The clinical presentation of scabies varies with age [2]. Infants often present with severe and widespread skin involvement. The presence of crusted nodules in the axillary area and on the back and the involvement of palmoplantar surfaces, the face, and the scalp may help differentiate scabies from atopic dermatitis and other inflammatory skin disorders in this age group [8]. In high-income countries, delays in diagnosing scabies may be due to reduced familiarity with this disorder among non-dermatologists. This diagnostic delay can lead to outbreaks in daycare facilities, schools, and other institutions [9]. The International Alliance for the Control of Scabies (IACS) recently developed international consensus diagnostic criteria and guidelines for common scabies [10].
Topical 5% permethrin cream (Scabi-med® Crème 5%; Permamed AG) is the only registered scabies treatment in Switzerland. Topicals are cumbersome since they require meticulous application to all skin areas for 8–12 hours of exposure [11]. Permethrin cream must be reapplied 7–10 days later, often resulting in poor treatment adherence, leading to persistent infection, further spreading, particularly in overcrowded settings, and increasing risk of drug resistance [12]. Other scabicides such as benzyl benzoate, topical ivermectin, crotamiton, and oral ivermectin must be imported from abroad and used off-label. Often, health insurance companies decline to cover these treatment options, resulting in a significant financial burden for affected families.
Oral ivermectin is generally effective in patients weighing >15 kg, including those with refractory infestations or immunocompromised [13, 14]. It is also reported to be safe and effective in children weighing <15 kg [15]. Since ivermectin is not ovicidal, repeat administration is required to ensure successful treatment. In France, following the recommendation of the French Medicines Regulatory Agency, oral ivermectin is used in children <1 year if topical 5% permethrin treatment fails [16].
A national surveillance system for scabies does not exist in Switzerland. One study concluded that most scabies cases were treated by general practitioners and paediatricians [17]. Swiss data on the review of infectious diseases in arriving asylum-seeking minors show that scabies is a relevant and common skin infection [18, 19]. To our knowledge, data on diagnostic and treatment strategies for scabies in Swiss children do not exist.
We aimed to survey the management of children infected with scabies by different Swiss healthcare providers to identify knowledge gaps and research needs to optimise the diagnosis and treatment of children with scabies.
Pre-survey discussions with expert colleagues from dermatology, paediatric infectious diseases, tropical medicine, and adult and paediatric generalists revealed that scabies is a frequently encountered dermatosis associated with management uncertainties in Switzerland. A literature search of the PubMed database (search terms: scabies AND Switzerland; Filters: child [birth to 18 years], human), focusing on articles describing diagnostic and treatment strategies for scabies in children in Switzerland, identified only two reports of single-centre experiences with multiple infectious and dermatological diseases that only mentioned the number of scabies cases [18, 19]. Therefore, we initiated a survey among dermatologists and non-dermatologists to describe the current situation regarding scabies in Switzerland and to generate research questions. We formulated 36 survey questions reviewing the general management of scabies cases, the approximate number of cases seen by age group during a 16-month period (January 2019 to April 2020), treatment practices, oral ivermectin use, treatment failures, and research priorities. Survey questions were formulated in German, English, and French (supplemental material see appendix 1: English version). They were pretested by medical students, paediatric infectious disease specialists, paediatric dermatologists, and paediatric generalists. Improvement suggestions were integrated to create the final version. A completion time of 15–20 minutes was proposed. The surveys were hosted at Unipark QuestBack (https://www.unipark.com).
In Switzerland, the following healthcare providers manage scabies in children: paediatricians, dermatologists, general practitioners, paediatric dermatologists, tropical medicine specialists, and paediatric infectious disease specialists. The following professional societies were contacted to motivate their members to participate in the survey: Swiss Society of Paediatrics (SSP; 2729 members), General Paediatricians Switzerland (“Kinderärzte Schweiz”; 795 members), General Practitioners (GP) and Paediatricians (“Haus- und Kinderärzte Schweiz - mfe”; 4000 general practitioners and 500 paediatricians), Paediatric Infectious Disease Group of Switzerland (PIGS; 48 members), Swiss Society of Dermatology (608 members), Swiss Group for Paediatric Dermatology (SGPD; 37 members), and the Swiss Society for Tropical and Travel Medicine (55 members) (figure 1). A call for participation with the link to the survey was sent on 25th May 2020, with a reminder sent on 25th June 2020. The survey was inactivated on 8th August 2020. Participation was anonymous. Statements regarding diagnostic criteria used were compared with the IACS Consensus Criteria for the Diagnosis of Scabies (confirmed: visualisation of mites, eggs, and faeces with an optical device; clinical: visualisation of burrows at typical anatomic areas/distribution including two history features; suspected: typical lesions with one history feature or atypical lesions with two history features; history features include itch and/or positive contact history) [20].
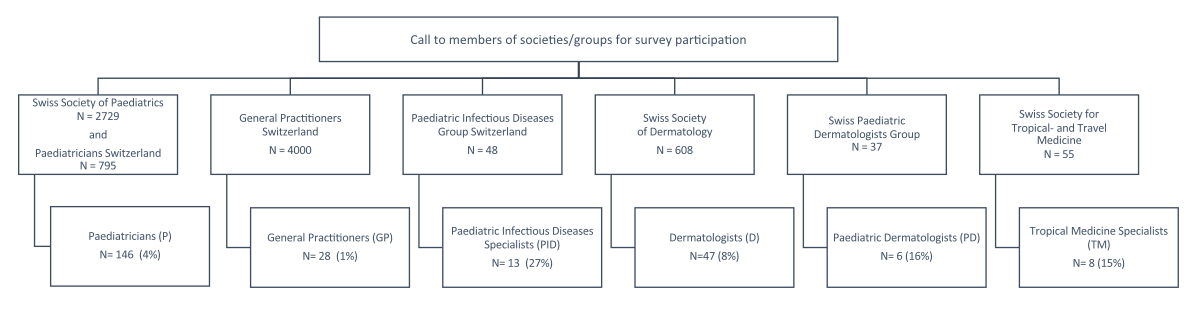
Figure 1Participation flowchart. Societies and groups with the number of members contacted through electronic mail. The number and percentage of survey participants by speciality.
Furthermore, we contacted 15 cantonal hospital pharmacies throughout Switzerland, asking about trends in ivermectin prescriptions/consumption for 2018 and 2019. Permamed AG was contacted, enquiring about trends for orders of Scabi-med® 5%. Statistics were descriptive. Analyses were conducted by calculating the frequencies and percentages of the survey answers provided by the different clinicians. No statistical software was used.
The project synopsis was approved by the ethics committee (EKNZ) (ID: Req-2020-00681).
The 36 survey questions were completed by 248 clinicians: 146 (59%) paediatricians, 47 (19%) dermatologists, 28 (11%) general practitioners, 6 (2%) paediatric dermatologists, 13 (5%) paediatric infectious diseases specialists, and 8 (3%) tropical medicine specialists. Among the responding clinicians, 70%, 27%, and 2% were from the German-, French-, and Italian-speaking cantons of Switzerland, respectively.
By specialisation, the following proportions of clinicians had been practising for >5 years since their Swiss Medical Association (FMH) board qualification: 94% of paediatricians, 96% of general practitioners, 83% of dermatologists, 100% of paediatric dermatologists, 82% of paediatric infectious diseases specialists, and 86% of tropical medicine specialists. Among respondents, 20% worked in a hospital, 65% in a private practice, and 15% in both settings. Among the dermatologists, 60% of dermatologists and 34% of paediatric dermatologists worked in private practice. Non-paediatricians (general practitioners, dermatologists, and tropical medicine specialists) stated that up to 25% of children with scabies were aged <5 years. When asked to estimate which age group was particularly affected by scabies, 78% of paediatricians, 89% of paediatric infectious diseases specialists, and 80% of paediatric dermatologists considered children aged <5 years the most affected group compared to 67% of non-paediatricians (dermatologists, general practitioners, and tropical medicine specialists); 5% of respondents did not answer this question. Scabies was perceived to affect the Swiss local population and children with a migrant background at similar rates between January 2019 and April 2020 (table 1).
Table 1Approximate numbers of scabies cases seen in children aged <5 years during a 16-month period (01/2019–04/2020) by group/speciality expressed in percentages.
| Scabies case range consulted | 1–5 | 6–10 | 11–25 | 26–35 | 35–50 | >50 | Non-responders | |||||||
| Population | Swiss | Migrant | Swiss | Migrant | Swiss | Migrant | Swiss | Migrant | Swiss | Migrant | Swiss | Migrant | Swiss | Migrant |
| Paediatricians (paediatrician + paediatric infectious disease specialist), n = 159 | 90% | 87% | 7% | 12% | 2% | 2% | 0% | 0% | 0% | 0% | 0% | 0% | 1% | 1% |
| Dermatologists (dermatologist + paediatric dermatologist), n = 53 | 92% | 80% | 1% | 13% | 4% | 4% | 3% | 3% | 0% | 0% | 0% | 0% | 4% | 4% |
| General practitioners, n = 28 | 79% | 86% | 7% | 0% | 0% | 4% | 7% | 0% | 7% | 9% | 0% | 0% | 8% | 8% |
| Tropical medicine specialists, n = 8 | 67% | 75% | 33% | 25% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 14% |
The management and treatment results are summarised in table 2. Most non-dermatologists (i.e. general practitioners, paediatricians, paediatric infectious diseases specialists, and tropical medicine specialists) relied on history (itchy skin lesions plus contact history) and suggestive skin findings (skin lesions, distribution, and burrows) alone to diagnose scabies, which would correspond to the IACS diagnosis category “clinical scabies”. Diagnostic criteria, including tools used by the different clinicians, are shown in figure 2. Dermoscopy was frequently used by dermatologists (dermatologists and paediatric dermatologists) and less often by non-dermatologists. Dermatologists were also more likely to use laboratory tests, including skin scrapings, to visualise mites, eggs, or faeces than non-dermatologists. These diagnostic modalities correspond to the IACS criteria for “confirmed scabies” and suggest that dermatologists rely on the most specific criteria.
Table 2Summary of the results for scabies diagnosis and management in children by clinical group. The non-dermatologist group included general practitioners (n = 28), paediatricians (n = 146), paediatric infectious diseases specialists (n = 13), and tropical medicine specialists (n = 8).
| Non-dermatologists | Dermatologists | Paediatric dermatologists | ||||
| n = 195 | n = 47 | n = 6 | ||||
| Scabies diagnosis | Non-responder | Non-responder | Non-responder | |||
| Rely on history and suggestive skin findings (IACS criteria: clinical scabies) | 155 (80%) | 0 (0%) | 14 (30%) | 1 (2%) | 0 (0%) | 0 (0%) |
| Use dermoscopy (IACS criteria: confirmed scabies) | 47 (24%) | 17 (9%) | 42 (89%) | 1 (2%) | 6 (100%) | 0 (0%) |
| Use PCR testing (skin sample) | 3 (2%) | 17 (9%) | 0 (0%) | 1 (2%) | 0 (0%) | 0 (0%) |
| Use burrow ink test | 2 (1%) | 17 (9%) | 3 (6%) | 1 (2%) | 0 (0%) | 0 (0%) |
| Refer to a dermatologist for a second opinion | 20 (10%)* | 0 (0%) | ||||
| Treatment and complications | ||||||
| Use ivermectin off-label in children weighing <15 kg | 20 (10%)** | 18 (9%) | 8 (17%) | 3 (6%) | 4 (67%) | 0 (0%) |
| Use of a single ivermectin cycle at 200 μg/kg | 17 (9%) | 108 (55%) | 7 (15%) | 9 (19%) | 0 (0%) | 0 (0%) |
| Use of two ivermectin cycles at 200 μg/kg | 46 (24%) | 108 (55%) | 15 (32%) | 9 (19%) | 6 (100%) | 0 (0%) |
| Use of adjuvant therapy (emollient and topical steroids from the first treatment day) | 27 (14%) | 18 (9%) | 20 (43%) | 1 (2%) | 3 (50%) | 0 (0%) |
| Co-treat all close contacts | 115 (59%) | 1 (1%) | 43 (91%) | 1 (2%) | 6 (100%) | 0 (0%) |
| 5% Permethrin cream | ||||||
| Observe treatment failure: age (1 month–5 years) | 111 (57%) | 38 (19%) | 35 (81%) | 3 (6%) | 6 (100%) | 0 (0%) |
| Observe treatment failure: age (>5–16 years) | 91 (47%) | 38 (19%) | 37 (86%) | 3 (6%) | 4 (67%) | 0 (0%) |
| Observe burning/stinging/redness | 24 (12%) | 0 (0%) | 18 (38%) | 0 (0%) | 3 (50%) | 0 (0%) |
| Oral Ivermectin | ||||||
| Observe treatment failure: age (1 month–5 years) | 39 (20%) | 39 (20%) | 12 (48%) | 6 (13%) | 6 (100%) | 0 (0%) |
| Observe treatment failure: age (>5–16 years) | 46 (24%) | 39 (20%) | 24 (59%) | 6 (13%) | 5 (83%) | 0 (0%) |
| Fear of adverse events when used in children | 69 (35%)*** | 17 (9%) | 18 (38%) | 3 (6%) | 1 (17%) | 0 (0%) |
| Observe stomachache/diarrhoea/vomiting | 9 (5%) | 5 (3%) | 1 (2%) | 1 (2%) | 0 (0%) | 1 (17%) |
IACS: International Alliance for the Control of Scabies; PCR: polymerase chain reaction.
* Refer patient to a dermatologist for a second opinion: 5/28 general practitioners, 15/146 paediatricians, 0/13 paediatric infectious diseases specialists, and 0/8 tropical medicine specialists.
** Use ivermectin in patients weighing <15 kg: 0/28 general practitioners, 16/146 paediatricians, 4/13 paediatric infectious diseases specialists, and 0/8 tropical medicine specialists.
*** Fear of adverse events when oral ivermectin is used in children: 12/28 general practitioners, 51/146 paediatricians, 1/13 paediatric infectious diseases specialists, and 5/8 tropical medicine specialists.
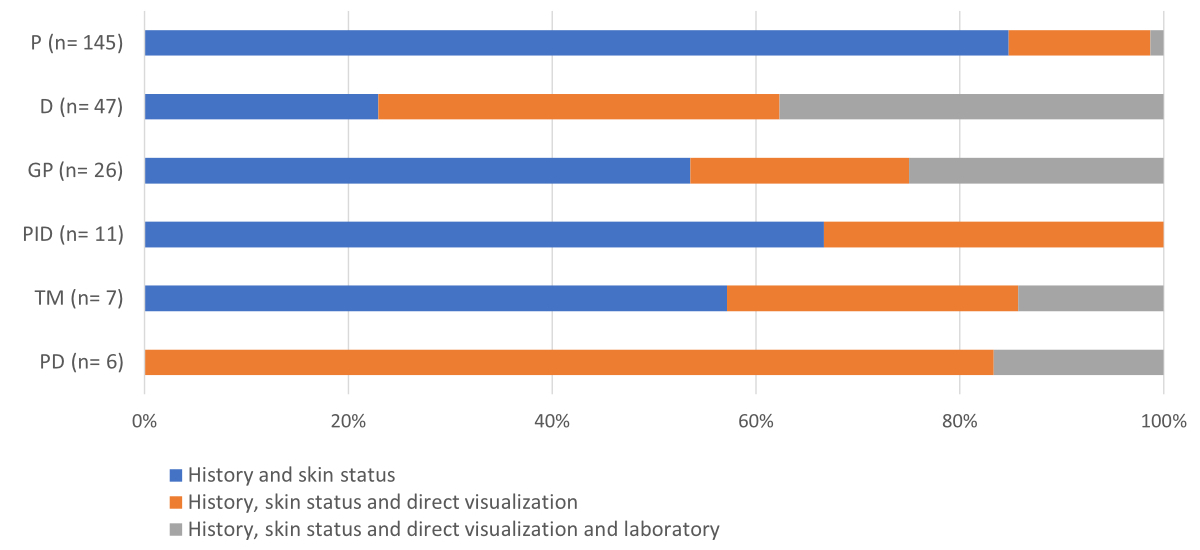
Figure 2Diagnostic criteria used by clinicians to diagnose scabies in children. History (itchy lesions plus contact history and family members with itching), skin status (skin lesions, distributions, and burrows), direct visualisation (dermoscopy), and laboratory test (scrapings for parasitology). P: paediatrician; D: dermatologist; GP: general practitioner; PID: paediatric infectious disease specialist; TM: tropical medicine specialist; PD: paediatric dermatologist.
Topical 5% permethrin and oral ivermectin were the treatment options most frequently prescribed. Children aged <5 years were most frequently treated with 5% permethrin, with ivermectin use steadily increasing with age (figure 3). Paediatric dermatologists were the most frequent off-label prescribers of oral ivermectin in children weighing <15 kg. Most dermatologists used two treatment cycles of oral ivermectin. Non-dermatologists rarely prescribed adjuvant therapy (emollient and topical steroids from the first treatment day). Around a third of non-dermatologists feared adverse events when using ivermectin in children (table 2).
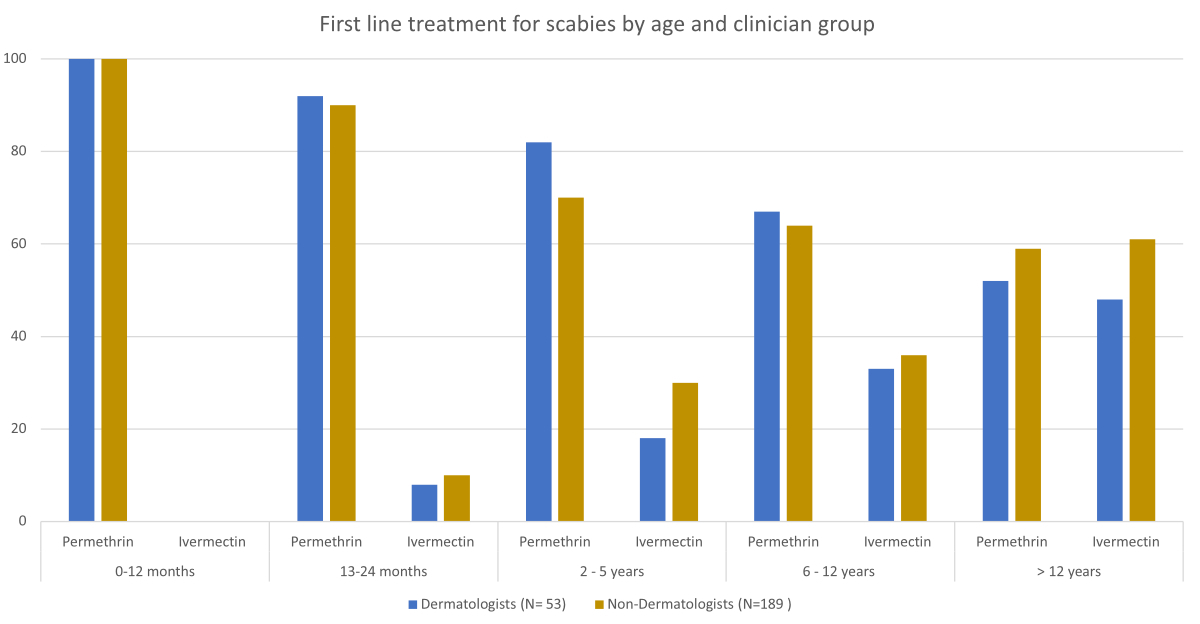
Figure 3First-line treatment modalities dermatologists and non-dermatologists used to treat scabies by age group. N: the number of clinicians (grouped) who answered the question; X-axis: percentage.
Most clinicians recommend washing clothes and bedlinen at 60°C (100% dermatologists, 69% non-dermatologists). Most clinicians considered oral ivermectin, followed by topical permethrin, the most effective treatment (figure 4). The question “In your opinion, which treatment is the most effective?” was not answered by 18% of general practitioners, 7% of paediatricians, and 6% of dermatologists.
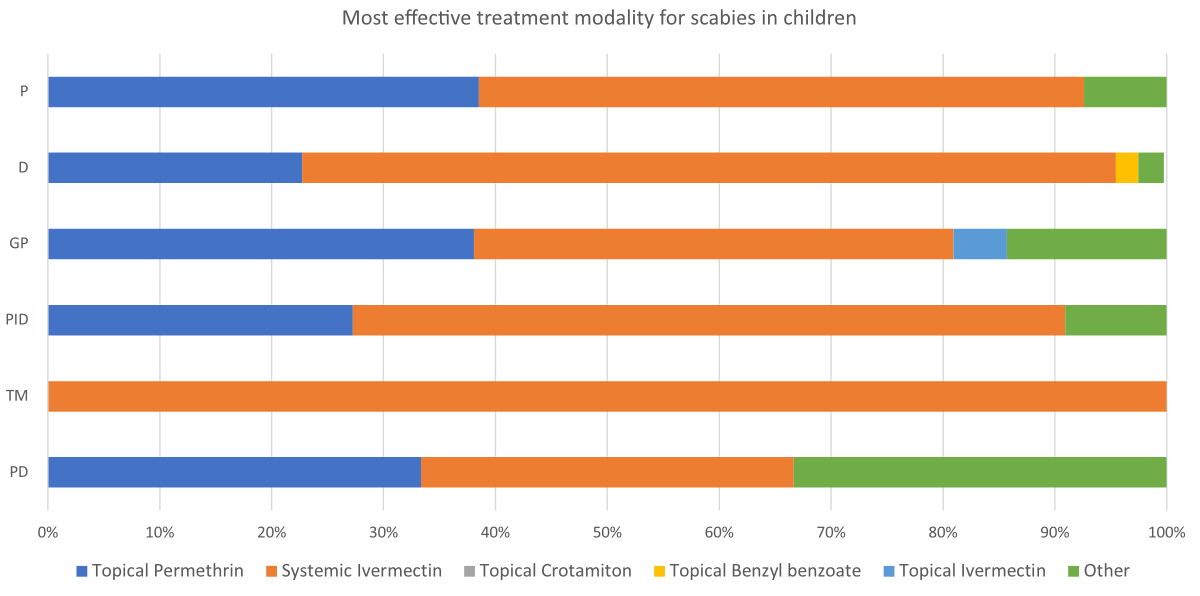
Figure 4The treatment modality clinicians found the most effective for scabies in children.
GP: general practitioner; P: paediatrician; PID: paediatric infectious diseases specialist; D: dermatologist; PD: paediatric dermatologist; TM: tropical medicine specialist.
All clinicians reported treatment failures with topical permethrin in children and adolescents. However, the dermatologists reported the highest numbers. Clinicians who used oral ivermectin for scabies reported fewer treatment failures in children and adolescents (table 2). Most participating clinicians mentioned that “communication problems”, “compliance issues”, “inadequate hygienic measures”, and “severe form of scabies” were contributing factors to treatment failure.
Around a third of dermatologists but fewer non-dermatologists reported adverse events with topical permethrin (“burning/stinging/redness of the skin”) in children aged one month to five years. Both dermatologists and non-dermatologists rarely observed “stomachache/diarrhoea/vomiting” with oral ivermectin treatment (table 2).
When asked to consider “persistent scabies if itching and eczematous lesions persist”, 43% of dermatologists (dermatologists and paediatric dermatologists) and 8% of non-dermatologists responded that this depends on further diagnostics, such as dermoscopy or microscopy. While 2% of respondents did not answer this question, 13% of dermatologists and 13% of non-dermatologists suspected recurrent or persistent scabies when symptoms remained two weeks post-treatment, increasing to 26% and 31% at four weeks, respectively. However, 20% of non-dermatologists did not know when to consider persistent or recurrent scabies. When persistent scabies was suspected, 33% of paediatric dermatologists, 23% of dermatologists, and 17% of non-dermatologists would switch from permethrin cream to oral ivermectin. In addition, 66% of paediatric dermatologists, 43% of dermatologists, and 12% of non-dermatologists would start combination treatment with permethrin cream and oral ivermectin.
The most relevant research priorities for dermatologists, paediatric infectious disease specialists, and tropical medicine specialists were studies examining the safety and efficacy of using ivermectin in infants and toddlers. The most relevant research priority for paediatricians and general practitioners was easier diagnostic tools for scabies (table 3).
Table 3Research priorities for scabies management suggested by the clinicians. Multiple answers were allowed. Respondents answered each question on a scale from 0 (irrelevant) to 6 (very relevant). Only highly relevant answers (scores of 5–6) are shown.
| Highly relevant (Score of 5–6) | Ivermectin use in infants and toddlers (safety and efficacy studies) | New dosages and treatment protocols for ivermectin | New drug agents for scabies | Easier diagnostic tools for scabies | Research regarding scabies resistance | Non-responders |
| Paediatricians (n =146) | 53% | 43% | 30% | 59% | 26% | 0% |
| Dermatologists (n = 47) | 57% | 51% | 38% | 43% | 51% | 0% |
| General practitioners (n = 28) | 15% | 19% | 38% | 35% | 27% | 0% |
| Paediatric infectious disease specialists (n = 13) | 82% | 64% | 27% | 45% | 18% | 0% |
| Tropical medicine specialists (n =8) | 86% | 57% | 71% | 57% | 57% | 0% |
| Paediatric dermatologists (n = 6) | 100% | 33% | 50% | 17% | 83% | 0% |
The following 9 of 15 contacted Swiss hospital pharmacies reported that prescriptions for ivermectin tablets increased from 2018 to 2019: Thurgau (80 to 430 tablets), Zug (30 to 36 tablets), Basel City (adults: 572 to 1848 tablets; children: 0 to 12 tablets), Basel Country (2040 to 2440 tablets), Ticino (1275 to 3022 tablets), St Gallen (172 to 372 tablets), Bern (adults: 1372 to 1736 tablets; children: 0 to 40 tablets), Chur (adults: 20 to 28 tablets), and Aarau (500 to 550 tablets). Permamed AG reported an increase in 5% permethrin cream prescriptions from 10,779 to 24,895 packs.
Infants and children with scabies may present to clinicians with differing expertise and in different settings in high-income countries. There is limited data on scabies management across specialities. Previous surveys involved only single groups, such as paediatricians [21], general practitioners [22] and dermatologists [23, 24] and contained only a few questions on management. We included a diverse group of clinicians nationwide and reviewed many aspects of their scabies management, including research priorities.
No precise epidemiological data are available since scabies is not a notifiable disease in Switzerland. Scabies is one of the most prevalent dermatoses in the migrant population [6, 19]. However, within our national survey, most clinicians reported similar numbers in the local population and children with a migrant background. An increase in scabies or scabicide consumption has been reported in countries with a high sociodemographic index [5, 7, 25, 26]. A recent study in the Netherlands reported a more than threefold increase in incidence from 2011 to 2020 [27]. In Spain, 5% permethrin cream prescriptions for scabies increased sixfold from 2008 to 2021 [28]. In Switzerland, hospital pharmacies and Permamed AG reported that scabicide prescriptions increased from 2018 to 2019, indicating a similar trend to those in other European countries. The findings from our and other studies indicate that scabies is not a rare disease in high-income countries but rather an increasing problem.
The scabies burden in low- and middle-income countries is highest among children aged <5 years [4], which was also confirmed in our survey. Scabies management in very young children frequently challenges clinicians in Switzerland.
Few national guidelines on managing scabies in children exist in Europe. These guidelines are often not harmonised, particularly regarding diagnostic and therapeutic modalities [11, 29–31]. The IACS has recently developed practical guidelines for categorising scabies diagnoses into confirmed, clinical, and suspected scabies that are appropriate for use in all income settings [10]. Our survey showed that most non-dermatologists rely only on history and suggestive skin findings. Almost all dermatologists and paediatric dermatologists used dermoscopy, and some used adjunctive diagnostics such as skin scrapings. A recent survey among dermatologists in Italy found that dermoscopy was only used in half of suspected cases [24].
Regarding the IACS criteria, most Swiss non-dermatologists would diagnose “clinical” or “suspected” scabies. Using less specific diagnostic criteria may result in misdiagnosis since there are several differential diagnoses mimicking scabies, resulting in the spread of scabies in families or institutions or the application of incorrect treatment modalities (e.g. steroids for presumed eczema in young children with scabies leading to crusted scabies [32]). Our survey showed that almost all dermatologists correctly treat close contacts simultaneously [11, 33]. However, up to 40% of non-dermatologists do not follow this critical management step. Not treating contacts of index patients risks spread or recurrence [12, 34].
Dermatologists readily prescribe emollients and topical steroids as adjuvant treatment from the first day of treatment, while non-dermatologists are reluctant to use topical steroids. They are safe to use as adjunct first-line treatment and can help control the eczematous and inflammatory components of scabies [2, 35]. Inflammation may last 4–6 weeks after treatment initiation [2, 36].
This survey revealed that approximately a third of non-dermatologists consider the “recurrent scabies” diagnosis, but only if itching and eczematous lesions persist at four weeks post-treatment, and only 6% use further diagnostic tools to support their diagnosis. This gap in optimal treatment and follow-up diagnostics may explain overdiagnosing “recurrent scabies” or “treatment failure” [37, 38].
In Switzerland, the younger the patient, the more likely permethrin will be prescribed. Conversely, the older the patient, the more likely oral ivermectin will be prescribed. A study in France made similar observations [21]. However, most clinicians in our survey felt that oral ivermectin was the most effective treatment modality.
Dermatologists observed treatment failures with permethrin cream in 46–90% of cases involving children aged <5 years. In contrast, non-dermatologists observed treatment failure in nearly a third of such cases. Our study did not provide information on patient education (treatment application and duration). Furthermore, our survey did not ask whether the heads of children aged <5 years were included when applying permethrin. These factors (incorrect application of topical treatment) may potentially contribute to permethrin treatment failure. A recent Italian survey among dermatologists reported similar numbers (52%) of permethrin failure, but this was not specified by age group [24]. However, these observations may have a particular bias since most children are primarily seen by paediatricians and general practitioners, starting with the first-line treatment. They may refer particularly difficult cases to dermatologists for further management. However, studies by Mazzatenta et al. [39] and Balestri et al. [38] suggest that permethrin is becoming less effective against scabies. In vitro resistance studies on scabies mites are rare [40], and, to our knowledge, conclusive resistance data are not yet available in Europe.
Permethrin cream adherence issues are multifactorial, particularly in families with many children. Risk factors for treatment failure include communication problems in migrant families, treatment of all family members, and difficult housing settings. These factors may reflect the cumbersome process of applying cream to all skin areas, making this topical treatment modality prone to incorrect application. An oral treatment modality such as ivermectin could reduce these risk factors.
Interestingly, up to 23% of clinicians, particularly dermatologists, use oral ivermectin regularly off-label in children weighing <15 kg. Ivermectin is an off-label treatment modality in this young age group due to its limited pharmacokinetic, safety, and efficacy data. In recent years, increasing studies on post-off-label treatment observations have been reported, concluding that oral ivermectin is safe and has no significant adverse events [15, 41–44]. However, data from randomised controlled trials on ivermectin’s safety, pharmacokinetics, and efficacy in children weighing <15 kg are currently unavailable. This aspect is a research priority, particularly for the clinicians who participated in our survey. Other priorities for clinicians are new user-friendly diagnostic tools, treatment protocols, child-friendly dosage forms, and clinical research regarding scabies treatment resistance. This finding aligns with recently reported research priorities discussed in the IACS and the World Health Organization [45].
It should be noted that our survey results are based on the answers provided by a limited number of clinicians who were reached by mail through their societies and could participate. Our low number of respondents may reflect that our survey fell within the initial months of the lockdown during the COVID-19 pandemic, during which many physicians were preoccupied with other tasks and overwhelmed by electronic mail. In addition, some clinicians did not answer all questions. It can be hypothesised that only clinicians who have been in contact with paediatric scabies and experienced management problems were keen to participate, and the findings from our survey may be biased towards the answers of these clinicians and, therefore, not generalisable. Some questions were unanswered due to time constraints or unfamiliarity with the topic, which may add bias and reduce generalisability. However, being key players in managing children with dermatologic problems, paediatricians and dermatologists were the largest group of clinicians to provide answers on their management of scabies, providing a perspective on potential gaps and shortcomings of scabies diagnosis and treatment in children. Nevertheless, our findings can guide necessary management and research topics to focus on in the future.
In Switzerland, scabies is a frequently observed dermatosis in migrant and Swiss children aged <5 years. While accessible, optimal diagnostics are underutilised, and treatment is suboptimal. There is indirect evidence that resistance to permethrin may be an increasing problem. Up to two-thirds of dermatologists regularly use oral ivermectin off-label in children weighing <15 kg. Clinical studies on ivermectin use in children weighing <15 kg, user-friendly diagnostic tools, new treatment protocols, and child-friendly dosage forms are needed.
The data presented in this manuscript are available from the corresponding author upon reasonable request.
We would like to thank all participating clinicians for supporting this project and taking their time answering the survey questions.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Chandler DJ, Fuller LC. A Review of Scabies: An Infestation More than Skin Deep. Dermatology. 2019;235(2):79–90. 10.1159/000495290
2. Chosidow O. Clinical practices. Scabies. N Engl J Med. 2006 Apr;354(16):1718–27. 10.1056/NEJMcp052784
3. Disease GB, Injury I, Prevalence C; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018 Nov;392(10159):1789–858. 10.1016/S0140-6736(18)32279-7
4. Karimkhani C, Colombara DV, Drucker AM, Norton SA, Hay R, Engelman D, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017 Dec;17(12):1247–54. 10.1016/S1473-3099(17)30483-8
5. Sunderkötter C, Aebischer A, Neufeld M, Löser C, Kreuter A, Bialek R, et al. Increase of scabies in Germany and development of resistant mites? Evidence and consequences. J Dtsch Dermatol Ges. 2019 Jan;17(1):15–23. 10.1111/ddg.13706
6. Di Meco E, Di Napoli A, Amato LM, Fortino A, Costanzo G, Rossi A, et al.; INMP Team. Infectious and dermatological diseases among arriving migrants on the Italian coasts. Eur J Public Health. 2018 Oct;28(5):910–6. 10.1093/eurpub/cky126
7. Zhang W, Zhang Y, Luo L, Huang W, Shen X, Dong X, et al. Trends in prevalence and incidence of scabies from 1990 to 2017: findings from the global Burden of disease study 2017. Emerg Microbes Infect. 2020 Dec;9(1):813–6. 10.1080/22221751.2020.1754136
8. Boralevi F, Diallo A, Miquel J, Guerin-Moreau M, Bessis D, Chiavérini C, et al.; Groupe de Recherche Clinique en Dermatologie Pédiatrique. Clinical phenotype of scabies by age. Pediatrics. 2014 Apr;133(4):e910–6. 10.1542/peds.2013-2880
9. Brockman R, Leitenberger S. Review of Scabies Infestation and Selected Common Cutaneous Infections. Pediatr Rev. 2021 Jan;42(1):21–32. 10.1542/pir.2018-0305
10. Engelman D, Yoshizumi J, Hay RJ, Osti M, Micali G, Norton S, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol. 2020 Nov;183(5):808–20. 10.1111/bjd.18943
11. Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017 Aug;31(8):1248–53. 10.1111/jdv.14351
12. Aussy A, Houivet E, Hébert V, Colas-Cailleux H, Laaengh N, Richard C, et al.; investigators from the Normandy Association of Medical Education in Dermatology. Risk factors for treatment failure in scabies: a cohort study. Br J Dermatol. 2019 Apr;180(4):888–93. 10.1111/bjd.17348
13. Chosidow A, Gendrel D. [Safety of oral ivermectin in children]. Arch Pediatr. 2016 Feb;23(2):204–9. 10.1016/j.arcped.2015.11.002
14. Rosumeck S, Nast A, Dressler C. Evaluation of Ivermectin vs Permethrin for Treating Scabies-Summary of a Cochrane Review. JAMA Dermatol. 2019 Jun;155(6):730–2. 10.1001/jamadermatol.2019.0279
15. Levy M, Martin L, Bursztejn AC, Chiaverini C, Miquel J, Mahé E, et al.; Groupe de Recherche de la Société Française de Dermatologie Pédiatrique. Ivermectin safety in infants and children under 15 kg treated for scabies: a multicentric observational study. Br J Dermatol. 2020 Apr;182(4):1003–6. 10.1111/bjd.18369
16. Berthe-Aucejo A, Prot-Labarthe S, Pull L, Lorrot M, Touratier S, Trout H, et al. [Treatment of scabies and Ascabiol(®) supply disruption: what about the pediatric population?]. Arch Pediatr. 2014 Jun;21(6):670–5. 10.1016/j.arcped.2014.03.001
17. Wenk C, Itin PH. Epidemiology of pediatric dermatology and allergology in the region of Aargau, Switzerland. Pediatr Dermatol. 2003;20(6):482–7. 10.1111/j.1525-1470.2003.20605.x
18. Genton PC, Wang J, Bodenmann P, Ambresin AE. Clinical profile and care pathways among unaccompanied minor asylum seekers in Vaud, Switzerland. Int J Adolesc Med Health. 2019 Sep;34(3):20190140. 10.1515/ijamh-2019-0140
19. Pohl C, Mack I, Schmitz T, Ritz N. The spectrum of care for pediatric refugees and asylum seekers at a tertiary health care facility in Switzerland in 2015. Eur J Pediatr. 2017 Dec;176(12):1681–7. 10.1007/s00431-017-3014-9
20. Engelman D, Fuller LC, Steer AC, panel IAftCoSD. Consensus criteria for the diagnosis of scabies: A Delphi study of international experts. 2018. e0006549.
21. Lê MS, Richard MA, Baumstarck K, Hesse S, Gaudy-Marqueste C, Grob JJ, et al.; le groupe de recherche en dermatologie pédiatrique de la Société Française de Dermatologie. [Evaluation of practices in the management of scabies in children]. Ann Dermatol Venereol. 2017 May;144(5):341–8.
22. Schmidt-Guerre AR, Aranda-Hulin B, Maumy-Bertrand M, Aubin F. [Diagnosis and treatment of scabies by general practitioners: A survey of practices in France]. Ann Dermatol Venereol. 2018 Feb;145(2):89–94. 10.1016/j.annder.2017.09.591
23. Thomas C, Rehmus W, Chang AY. Treatment practices in the management of scabies in infants younger than two months. Pediatr Dermatol. 2021 Mar;38(2):431–5. 10.1111/pde.14523
24. Bassi A, Mazzatenta C, Piccolo V. Diagnosis and management of pediatric scabies: results from a survey on 317 Italian dermatologists. Travel Med Infect Dis. 2022;50:102461. 10.1016/j.tmaid.2022.102461
25. Amato E, Dansie LS, Grøneng GM, Blix HS, Bentele H, Veneti L, et al. Increase of scabies infestations, Norway, 2006 to 2018. Euro Surveill. 2019 Jun;24(23):24. 10.2807/1560-7917.ES.2019.24.23.190020
26. Aždajić MD, Bešlić I, Gašić A, Ferara N, Pedić L, Lugović-Mihić L. Increased Scabies Incidence at the Beginning of the 21st Century: What Do Reports from Europe and the World Show? Life (Basel). 2022 Oct;12(10):12.
27. van Deursen B, Hooiveld M, Marks S, Snijdewind I, van den Kerkhof H, Wintermans B, et al. Increasing incidence of reported scabies infestations in the Netherlands, 2011-2021. PLoS One. 2022 Jun;17(6):e0268865. 10.1371/journal.pone.0268865
28. Martinez-Garcia E, Grau-Perez M, Buendia-Eisman A, Garcia-Doval I. Prescriptions for scabies are rapidly increasing in Spain: an ecological study with national prescription data, 2008-2021. J Eur Acad Dermatol Venereol. 2022.
29. Executive Committee of Guideline for the D. Treatment of S. Guideline for the diagnosis and treatment of scabies in Japan (third edition): Executive Committee of Guideline for the Diagnosis and Treatment of Scabies. J Dermatol. 2017;44; 991-1014.
30. Banerji A; Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee. Scabies. Paediatr Child Health. 2015 Oct;20(7):395–402. 10.1093/pch/20.7.395
31. Sunderkötter C, Mayser P, Fölster-Holst R, Maier WA, Kampen H, Hamm H. Scabies. J Dtsch Dermatol Ges. 2007 May;5(5):424–30. 10.1111/j.1610-0387.2007.06298.x
32. Lima FC, Cerqueira AM, Guimarães MB, Padilha CB, Craide FH, Bombardelli M. Crusted scabies due to indiscriminate use of glucocorticoid therapy in infant. An Bras Dermatol. 2017;92(3):383–5. 10.1590/abd1806-4841.20174433
33. Sunderkötter C, Wohlrab J, Hamm H. Scabies: Epidemiology, Diagnosis, and Treatment. Dtsch Arztebl Int. 2021 Oct;118(41):695–704.
34. Anderson KL, Strowd LC. Epidemiology, Diagnosis, and Treatment of Scabies in a Dermatology Office. J Am Board Fam Med. 2017 Jan;30(1):78–84. 10.3122/jabfm.2017.01.160190
35. Johnston G, Sladden M. Scabies: diagnosis and treatment. BMJ. 2005 Sep;331(7517):619–22. 10.1136/bmj.331.7517.619
36. Golant AK, Levitt JO. Scabies: a review of diagnosis and management based on mite biology. Pediatr Rev. 2012 Jan;33(1):e1–12. 10.1542/pir.33.1.e1
37. Ständer S, Ständer S. Itch in Scabies-What Do We Know? Front Med (Lausanne). 2021 Feb;8:628392. 10.3389/fmed.2021.628392
38. Balestri R, Magnano M, Infusino SD, Rizzoli L, Girardelli CR, Rech G. Scabies is becoming less sensitive to permethrin therapy. J Eur Acad Dermatol Venereol. 2021 Dec;35(12):e889–91. 10.1111/jdv.17538
39. Mazzatenta C, Piccolo V, Argenziano G, Bassi A. Is Scabies becoming less sensitive to permethrin therapy? J Eur Acad Dermatol Venereol. 2021 Sep;35(9):e607–9. 10.1111/jdv.17339
40. Yürekli A. Is there a really resistance to scabies treatment with permethrin? In vitro killing activity of permethrin on Sarcoptes scabiei from patients with resistant scabies. Dermatol Ther. 2022 Mar;35(3):e15260. 10.1111/dth.15260
41. Jittamala P, Monteiro W, Smit MR, Pedrique B, Specht S, Chaccour CJ, et al. A systematic review and an individual patient data meta-analysis of ivermectin use in children weighing less than fifteen kilograms: is it time to reconsider the current contraindication? PLoS Negl Trop Dis. 2021 Mar;15(3):e0009144. 10.1371/journal.pntd.0009144
42. Nicolas P, Maia MF, Bassat Q, Kobylinski KC, Monteiro W, Rabinovich NR, et al. Safety of oral ivermectin during pregnancy: a systematic review and meta-analysis. Lancet Glob Health. 2020 Jan;8(1):e92–100. 10.1016/S2214-109X(19)30453-X
43. King CL. Is ivermectin safe in pregnancy? Lancet Glob Health. 2020 Jan;8(1):e12–3. 10.1016/S2214-109X(19)30490-5
44. Wilkins AL, Steer AC, Cranswick N, Gwee A. Question 1: is it safe to use ivermectin in children less than five years of age and weighing less than 15 kg? Arch Dis Child. 2018 May;103(5):514–9. 10.1136/archdischild-2017-314505
45. Engelman D, Cantey PT, Marks M, Solomon AW, Chang AY, Chosidow O, et al. The public health control of scabies: priorities for research and action. Lancet. 2019 Jul;394(10192):81–92. 10.1016/S0140-6736(19)31136-5