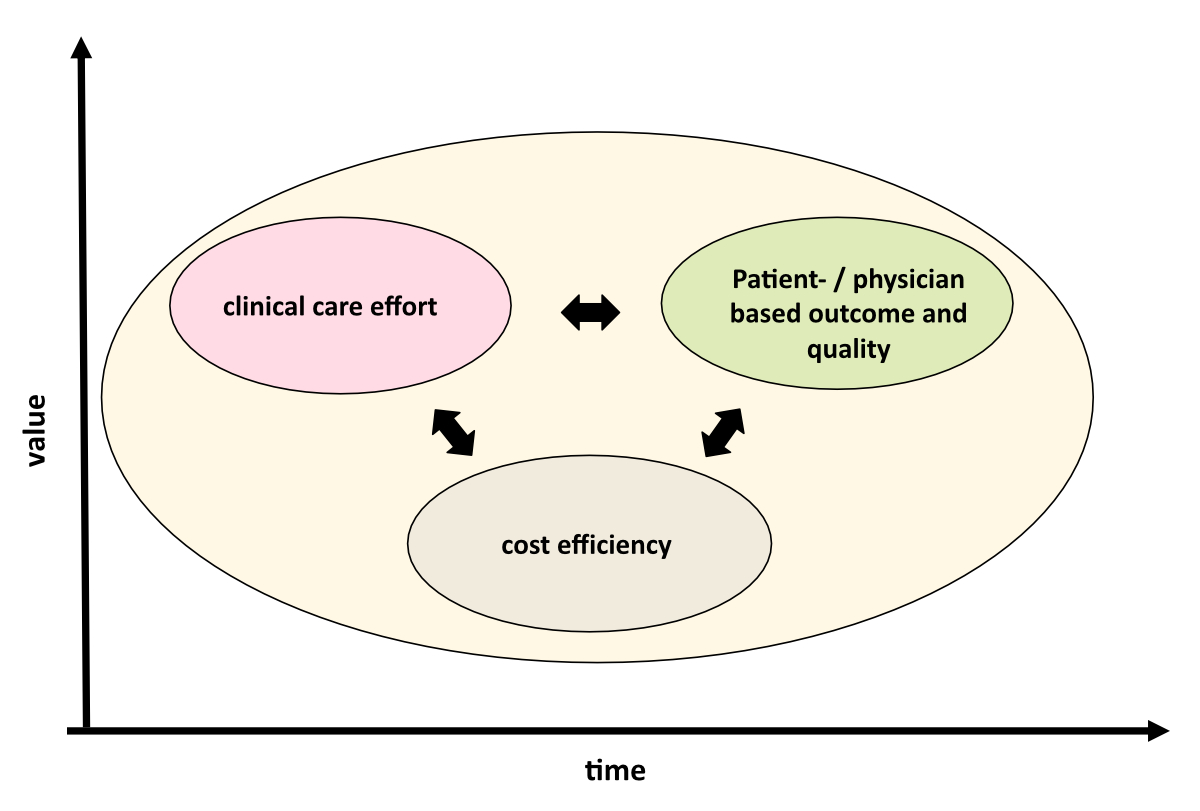
Figure 1The sustainable healthcare triad aligns the clinical effort with outcome and quality, as well as cost efficiency. The goal is to benchmark these parameters over time to establish shared value.
DOI: https://doi.org/https://doi.org/10.57187/s.3473
Healthcare organisations worldwide are facing significant challenges, including labour shortages, cost containment and capital contraction, leading to unsustainable workloads, staff shortages and burnout. The projected workforce shortages of both nurses and physicians have prompted the need to rethink healthcare delivery [1]. Hiring workers from other organisations to address staffing gaps ultimately creates a zero-sum game. A global survey highlighted the importance of intrinsic motivators, such as professional development opportunities, that may have been overlooked in the past [1]. There is unanimous agreement that financial expenditure exceeds medical capabilities. In Switzerland, concerns about the sustainability of the healthcare system existed before the COVID-19 pandemic due to sociodemographic changes, such as the retirement of the baby boomer generation and the smaller zoomer generation taking over, resulting in reduced healthcare capital [2–5]. This impending contraction of capital will further challenge the financial situation of hospitals.
There is unanimous agreement that a fundamental shift in healthcare delivery is necessary due to dwindling financial resources and staffing. Meyer et al. suggested that the healthcare system should be more integrated, preventive, transparent, outpatient-based and data-driven [6]. Many recognise the importance of digital transformation, although Switzerland is still in the early stages of developing electronic health records and embracing digitisation. Physicians have historically been resistant to defining quality of care due to its complexity, but defining it is crucial. Nearly two decades ago, Porter et al. introduced the concept of value-based healthcare, which involves assessing the quality and outcomes of care based on both patient and physician evaluations and considering the total costs incurred throughout the healthcare cycle [7]. The Swiss Sarcoma Network has proposed an adapted approach for developing a value-based healthcare delivery model specifically for sarcoma patients [8, 9].
The sustainable healthcare triad emphasises the interconnectedness of clinical care, outcomes and quality measures, and cost efficiency. Currently, the fee-for-service system does not consider the quality or cost control of medical procedures, such as surgeries. However, the new ecosystem-based triad necessitates coordinated, multidisciplinary interventions evaluated for their quality, outcome and costs. This approach integrates key parameters from the patient’s perspective and identifies key performance indicators for individual physicians. Aligning patient and physician views on cost efficiency is crucial for establishing a sustainable healthcare system, including also an objective and transparent definition of variable physician salaries.
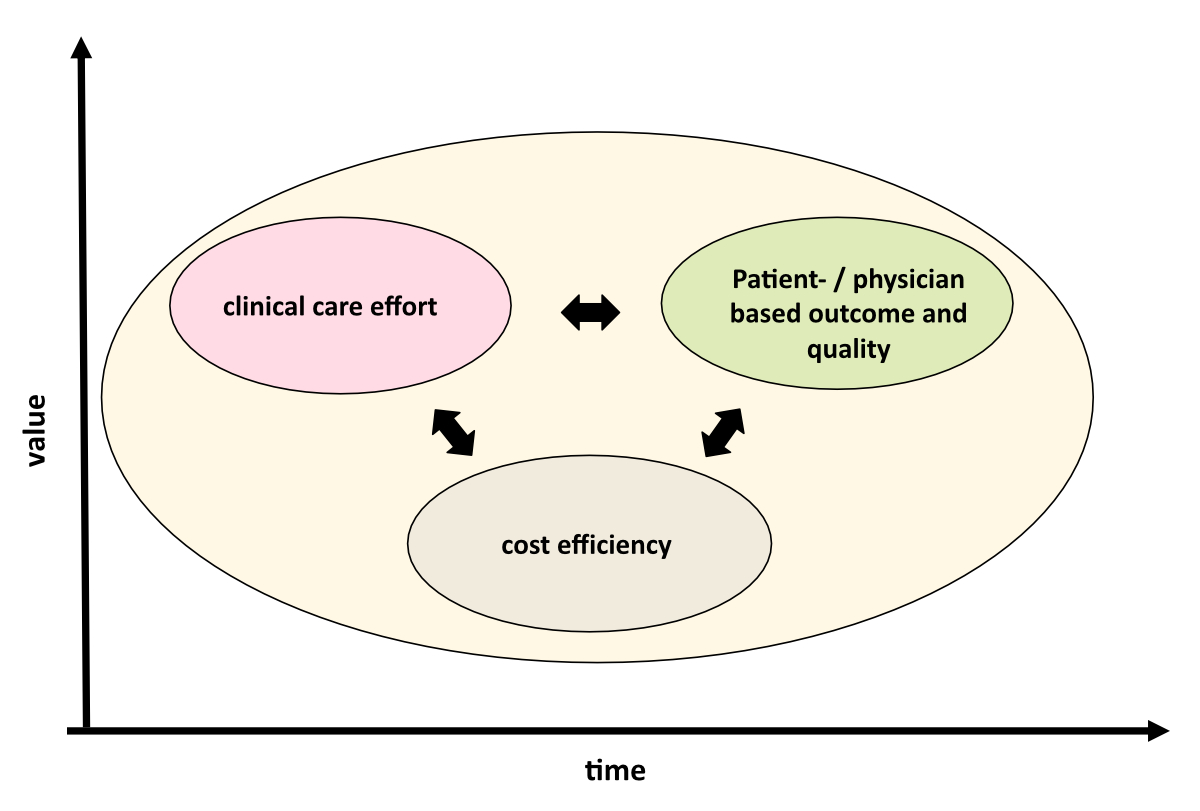
Figure 1The sustainable healthcare triad aligns the clinical effort with outcome and quality, as well as cost efficiency. The goal is to benchmark these parameters over time to establish shared value.
Sarcoma surgery and care are highly transdisciplinary, serving as a model for developing a sustainable healthcare system. The complexity of sarcomas necessitates collaboration across multiple disciplines to achieve optimal tumour removal and local control. The Swiss Sarcoma Network (www.swiss-sarcoma.net) exemplifies the integration of disciplines and institutions, fostering a multi-institutional and transdisciplinary approach rather than a mono-institutional silo system.
Sarcoma surgery is a highly complex procedure influenced by factors such as anatomical location, tumour size and biology. A senior Swiss Sarcoma Network surgeon conducted a 10-year analysis to develop a comprehensive surgical profile that considers all relevant parameters for resections and reconstructions [10]. This spectrum serves as a valuable tool for assessing surgical experience, educating future surgeons and evaluating the complexity and costs of specific interventions. Based on this profile, the Swiss Sarcoma Network introduced the soft-tissue surgery complexity score, which incorporates patient-, tumour biology- and surgery-related factors to determine the complexity of each intervention [11]. This score is particularly important for Porter’s geography model of care, which strives to deliver the appropriate treatment in the optimal geographic location, leading to improved outcomes and cost-effectiveness. Beyond surgery, sarcoma care entails multiple aspects that demand attention. To address this, the Swiss Sarcoma Network collaborated with an international advisory board of experts to define six categories of quality indicators for sarcoma care [12]. These categories encompass patient work-up, multidisciplinary team / sarcoma board management, therapy (including surgery, radiation and systemic therapy), complexity of sarcoma therapy, clinical outcomes and patient-reported outcomes. Evaluating these indicators is vital for sustaining a healthcare ecosystem, as it provides a comprehensive view of patient outcomes and the quality of care, as assessed by physicians.
In value-based healthcare, patient-reported outcome measures (PROMs) play a crucial role in assessing treatment effectiveness and improving outcomes, providing valuable insights beyond clinical metrics [9]. While numerous patient-reported outcome measures exist, only a few have been created for sarcoma surgery [13]. One widely used patient-reported outcome measure is the EQ-5D, which includes five questions on general health dimensions and has been validated for various diseases, including cancer. The Swiss Sarcoma Network has established a reference score of EQ-5D specifically for sarcoma patients and has revealed that the most significant negative predictor of perceived health is the administration of chemotherapy.
Sarcoma surgery and care present challenges because treatments are individualised and multidimensional. To address these challenges, the Swiss Sarcoma Network has developed a novel health-related quality of life (HRQOL) instrument [13]. This survey instrument utilises over 10 personalised generic patient-reported outcome measure questionnaires, allowing patients to electronically complete questionnaires based on their specific treatments and longitudinal follow-up periods. By incorporating a comprehensive set of patient-reported outcome measures, this approach aims to capture the holistic impact of sarcoma treatment on patients’ lives.
Managing healthcare data is a significant challenge in today’s world, but the digital transformation of healthcare practices holds great potential for revolutionising current approaches. Instant access to real-world-time clinical data and automated analyses are crucial, especially in multidisciplinary and multi-institutional settings.
To integrate complex data into daily practice and generate real-world-time evidence, a key strategy is combining the management of multidisciplinary team/sarcoma board conferences (MDT/SB) with the patient registry. By doing so, conflicting issues like surgical margins can be addressed and resolved through a multidisciplinary approach, with data recorded directly in the registry without the need for retrospective data collection.
During MDT/SB, the presenting physician and their team provide patient information, which is associated with the registry. Patients with sarcoma recurrence are automatically presented to the MDT/SB, and their data are stored in the registry. Patients without recurrence undergo regular check-ups and provide electronic patient-reported outcome measures. This system enables real-world-time follow-up of all patients.
The platform used incorporates over 500 parameters and facilitates calculations of quality indicators and simple statistics for direct visualisation. With real-world-time data collection and evidence analytics, predictive modelling becomes possible, ultimately leading to the development of a human-sarcoma digital twin and enabling individualised precision care.
Health services research examines the impact of various factors on healthcare access, quality and costs and on patients' well-being. Utilising an interoperable digital platform with descriptive and inferential statistics enables real-world-time research. This interdisciplinary field investigates how social factors, financing systems, organisational structure, health technologies and personal behaviours affect healthcare. A sarcoma study including all patients undergoing biopsy revealed 55% malignancy in suspicious soft tissue and bone neoplasms [14]. This finding has implications for planning and establishing an integrated practice unit (IPU) to streamline diagnostics. Another analysis compared pathology workups from different institutions, emphasising the importance of reference reviews. Incorrect diagnosis impacted treatment in 12.2% of cases [15]. Consulting reference pathologists reduced time to diagnosis. An ongoing project is evaluating the costs of hospitalisations and surgical interventions across three hospitals and is considering the case mix index, complexity score and outcomes.
Embedding health services research within hospitals is crucial. Affiliation with a medical faculty with health-focused research facilitates these analyses. Leveraging digital platforms and data analysis improves healthcare practices and patient outcomes in real time.
Healthcare organisations face numerous challenges, including labour shortages, cost containment and capital contraction. To address these challenges, the development of an integrated, preventive, transparent, outpatient-based and data-driven healthcare system is necessary. The sustainable healthcare triad, comprising clinical care, physician- and patient-based outcomes and quality, and cost efficiency, plays a vital role in this system. Defining the triad enables the establishment of key performance indicators for sarcoma care and aligns patient and physician perspectives on cost efficiency. The transdisciplinary organisation of sarcoma care, involving multiple disciplines and institutions, serves as a model for building a sustainable healthcare system. Defining the surgical spectrum, with its associated complexity, and the quality of care, using physician- and patient-based metrics, is crucial to this process. By adopting these strategies, healthcare organisations can deliver improved care while optimising efficiency and sustainability.
The healthcare industry must evolve and adapt to overcome challenges like workforce shortages and capital contraction. Digitalisation and electronic health records will play a crucial role. Defining quality of care with physician-based metrics aligns patient and physician views on cost efficiency for a sustainable healthcare system. Embracing and implementing the sustainable healthcare triad is necessary to define the shared value. Further research is needed to explore how the industry can adapt and achieve sustainable healthcare delivery.
A summary of the scientific contributions of the Swiss Sarcoma Network and further literature can be found under this link or QR code:

https://swiss-sarcoma.net/pdf/20230930-SSN_academic_overview.pdf
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Shanafelt T, Kuriakose C. Widespread clinician shortages create a crisis that will take years to resolve. NEJM Catal. 2023 Mar;4(3):CAT.23.0044. 10.1056/CAT.23.0044
2. Scholer M. Scheidegger: wenn wir so weitermachen, fahren wir das System an die Wand. Schweiz Arzteztg. 2017;98(15-16):495–7.
3. Wille N, Gilli Y. Qualität stärken statt Quantität steuern – Teil 1. Schweiz Arzteztg. 2022;103(37):26–8.
4. Wille N, Gilli Y. Wie gelingt Kostendämpfung ohne Versorgungseinbussen? – Teil 1. Schweiz Arzteztg. 2022;103(36):30–2.
5. Marty F. Hört auf, das Gesundheitswesen zu steuern. Schweiz Arzteztg. 2023;103(05):16–9.
6. Meyer PC, Brauchbar M: Trends und Herausforderungen im Gesundheitswesen Schweiz. Ärzteztg 2018; 99(33):1072-5
7. Porter ME, Pabo EA, Lee TH. Redesigning primary care: a strategic vision to improve value by organizing around patients’ needs. Health Aff (Millwood). 2013 Mar;32(3):516–25. 10.1377/hlthaff.2012.0961
8. Fuchs B, Bode B, Studer G, Breitenstein S. Wie entwickelt sich die Sarkomchirurgie? Leading Opinions Orthopädie&Rheumatologie. 2021;1:16–8.
9. Fuchs B, Studer G, Bode B, Wellauer H, Frei A, Theus C, et al.; SwissSarcomaNetwork. Development of a value-based healthcare delivery model for sarcoma patients. Swiss Med Wkly. 2021 Dec;151(5152):w30047. 10.4414/SMW.2021.w30047
10. Theus-Steinmann C, Schelling G, Heesen P, Breitenstein S, Scaglioni MF, Fuchs B. How is the spectrum of sarcoma surgery assessed? Cancers (Basel). 2023 Feb;15(4):1305. 10.3390/cancers15041305
11. Frei A, Scaglioni MF, Giovanoli P, Breitenstein S, Heesen P, Fuchs B; On Behalf Of The Swiss Sarcoma Network. Definition of the surgical case complexity in the treatment of soft tissue tumors of the extremities and trunk. Cancers (Basel). 2022 Mar;14(6):1559. 10.3390/cancers14061559
12. Heesen P, Studer G, Bode B, Windegger H, Staeheli B, Aliu P, et al. Quality of sarcoma care: longitudinal real-time assessment and evidence analytics of quality indicators. Cancers (Basel). 2022 Dec;15(1):47. 10.3390/cancers15010047
13. Mosku N, Heesen P, Christen S, Scaglioni MF, Bode B, Studer G, et al.; Swiss Sarcoma Network. The sarcoma-specific instrument to longitudinally assess health-related outcomes of the routine care cycle. Diagnostics (Basel). 2023 Mar;13(6):1206. 10.3390/diagnostics13061206
14. Mosku N, Heesen P, Studer G, Bode B, Spataro V, Klass ND, et al. Biopsy ratio of suspected to confirmed sarcoma diagnosis. Cancers (Basel). 2022 Mar;14(7):1632. 10.3390/cancers14071632
15. Wellauer H, Studer G, Bode-Lesniewska B, Fuchs B. Time and accuracy to establish the diagnosis of soft tissue tumors: a comparative analysis from the Swiss Sarcoma Network. Sarcoma. 2022 Apr;2022:7949549. 10.1155/2022/7949549