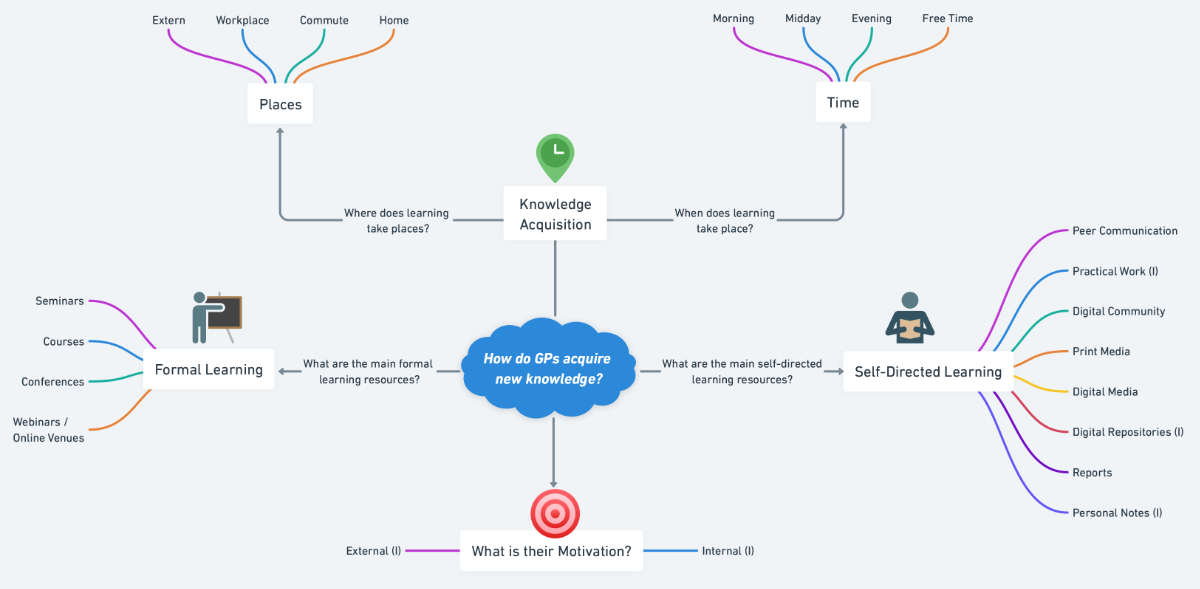
Figure 1Visual synthesis of the findings from research question 1. GP: general practitioner; (I): Inductive categories.
DOI: https://doi.org/https://doi.org/10.57187/s.3436
Self-directed learning (SDL) consists of measures in which learners take responsibility for identifying their own learning needs, formulating their own learning objectives and taking the initiative to find and use appropriate resources to meet these objectives [1]. Recognising the challenge in fostering both students’ and professionals’ abilities for self-directed learning is paramount, as it involves the mobilisation of several key processes such as self-monitoring, self-assessing and self-reflection [2]. Although self-directed learning can imply auxiliary forms like problem-based learning, case-based learning and simulation-based learning [3], it also takes place outside facilitated forms of learning, solely depending on the individuals’ impetus to acquire new knowledge. This acknowledgement not only underlines the importance of self-directed learning as a crucial cornerstone for lifelong learning and mandatory professional development, regulated by the Swiss Medical Profession Act (MedBG) [4, 5], but also sets the stage for exploring the specific self-directed learning activities of general practitioners (GPs) or “family physicians”. Considering their unique setting of working individually or in small teams and that a substantial fraction of them provide primary healthcare services in rural areas, understanding their personal motivation and approach on how to maintain self-directed learning is of utmost interest.
When screening the literature on how GPs acquired new knowledge in the three decades before the COVID-19 pandemic, approaches such as informal problem-based learning, peer communication, textbooks and journals, as well as formal venues such as congresses and seminars, were shown to be the mainstay of their self-directed learning [6–13]. Furthermore, with the emergence of digital repositories, informal digital peer communication and CME obligations, digitally enhanced self-directed learning among general practitioners became more and more common from the 2000s [8, 10, 11, 14, 15].
In recent years, self-directed learning gained importance in medical education since it can add sufficiently to classical approaches in preparing learners for the complex and rapidly changing healthcare environment, in which continuous learning and adaptation are essential [16].
In particular, the COVID-19 pandemic demonstrated a rapid progression in the turnover of medical information [17]. With ever-changing measures of policies and medical knowledge [18, 19], healthcare professionals were urged to find strategies to face this unprecedented scenario. Consecutively, a plethora of articles addressed the pandemic’s impact on the education of medical students, residents and front-line healthcare personnel [20, 21]. Since the frequently used qualifier ‘front-line’ often refers to hospital settings, it remains unclear to what extent the self-directed learning of GPs has been affected by the pandemic.
With the present article, our aim is to explore the self-directed learning activities of GPs in general and to what extent the pandemic influenced their self-directed learning behaviour. The following research questions reflect our objectives:
Research question 1: How do GPs acquire new knowledge?
Research question 2: What impact did the COVID-19 pandemic have on the self-directed learning of GPs?
Research question 3: Which ideas do GPs have about how to optimise their self-directed learning?
This study employs a qualitative research approach with semi-structured interviews. With its phenomenological nature, where a large proportion of insight lies in tacit knowledge of experts, the methods chosen aim to capture an in-depth exploration of the experiences, perceptions and insights of the interviewees at a hermeneutical level [22–25].
Prior to participation, all interviewees were provided with detailed information about the study’s aims, procedures and their rights, including confidentiality and voluntary participation. Written consent was not obtained, as our study does not fall under Article 2, Paragraph 1 (Scope) of the Swiss Federal Act on Research Involving Human Beings (Human Research Act, HRA). The independent Swiss cantonal ethics committee therefore declared that authorisation was unnecessary and deemed the study exempt from full ethical review.
The construction of the interview guide followed Gideon [26], with some modifications to accommodate our qualitative study design.
In the first step, we searched for a suitable conceptual framework. Thus, we reviewed theoretical models on self-directed learning [1, 27–30] and ultimately settled for the “Person, Process and Context (PPC)” model from Hiemstra and Brockett [27] with its three eponymous key components. Within the model, Person contains the individuals’ characteristics like motivation, experience, resilience, self-reflection and self-concept. Process refers to the organisation of learning, including planning, facilitation, technological aspects and evaluation. The Context component clusters environmental aspects such as culture, learning climate, (financial) obligations and political milieu [27]. The PPC model emphasises the equal importance of these three components.
For the development of categories and a structured content analysis, we further made use of Kuckartz’s qualitative content analysis framework [31] as it allows for a mixed deductive-inductive category system, frequently used in qualitative studies. As such, the deductive categories were established from preparatory work (i.e. literature review and team discussion) to be tested against the data collected, while the inductive part allows for the generation of new theories and insights based on the observations made during the interviews.
Starting with a foundation of deductive main and subcategories, these could be adapted and complemented by inductive categories which were discovered throughout the iterations of interview material analysis (table 1).
Table 1Differentiated category system based on deductive and inductive categories.
| Main categories | Probed subcategories | |
| Research question 1: How do general practitioners acquire new knowledge? | ||
| Learning opportunities / Use of media | Formal | Seminars |
| Courses | ||
| Conferences | ||
| Webinars | ||
| Self-directed learning | Peer communication | |
| Practical work (I) | ||
| Digital community | ||
| Print media | ||
| Digital media | ||
| Digital repositories (I) | ||
| Reports | ||
| Personal notes (I) | ||
| Knowledge acquisition places | External | |
| Workplace | ||
| Daily commute (I) | ||
| Home | ||
| Knowledge acquisition time | Morning | |
| Midday | ||
| Evening | ||
| Free time | ||
| Motivation | Internal (I) | |
| External (I) | ||
| Research question 2: What impact did the COVID-19 pandemic have on the self-directed learning of general practitioners? | ||
| Transformation due to COVID-19 | Digital transformation | |
| Shift in practice | ||
| Ambivalent views on digitalisation | ||
| Lack of recognition (I) | ||
| Learning frequency | ||
| Learning location | ||
| Research question 3: What optimisation potentials do general practitioners see for a more successful practice of self-directed learning? | ||
| Experience & optimisation potential | Advancing factors | |
| Impeding factors | ||
| Optimisation potential | ||
(I): Inductive categories.
In the second step, the team drafted raw interview questions in a consensus-driven process, fitting the key concepts. Here, care was taken to ensure that the intended topics were covered (table 1).
In the third step, we revised the questions and checked that no double negations or other potential distractors were used, thereby ensuring that all questions were clearly and unambiguously formulated. Next, the introduction of the interview guide and its sections as well as the logical arrangement of the questions were implemented. Furthermore, to collect additional information that had not yet been discussed and to be able to respond flexibly to the interviewees, follow-up questions to the main questions were considered in advance and noted in the form of short prompts under the main questions.
In the fourth step, we pilot-tested the questions and guide on two physicians at the Institute for Medical Education in Bern. The participants were instructed to indicate whether each question was clear and relevant. The question route was adapted accordingly.
We recruited 18 GPs from a network of student mentors at the medical faculty in Bern [32] via email and an information letter on the planned study. From a list of >700 student mentors in the network, these 18 GPs were suggested by RH using convenience sampling. Ultimately, 16 of the 18 GPs took part in the study. To increase the likelihood of participation, sampling was based on existing personal contacts. Selection criteria included being German-speaking and actively working as a GP either independently or in a group office. The aim was to achieve a cohort with diverse characteristics related to age, sex, office form, location of work and years of experience while ensuring feasibility for in-depth interviews. The interviewer reported saturation to be reached within the sample of 16.
The interviews were conducted between 30 May 2022 and 06 July 2022. All interviewees were managed individually, with 15 of the 16 interviews conducted online using Zoom video conferencing software (Zoom Video Communications Inc., San Jose, CA, USA) and one on-site interview at the respective GP’s office. The interviews lasted between 35 and 45 minutes.
All interviews were imported into Adobe Premiere Pro (Adobe Inc., San Jose, CA, USA) for automatic transcription. The data was then anonymised and transcribed intelligent verbatim following Dresing and Pehls’ transcription rules [33] and then imported into NVIVO (NVIVO by QSR International Ltd., Denver, CO, USA) for the subsequent analysis processes.
According to Kuckartz’s qualitative content analysis framework, the analysis proceeded through six phases [31]
We used memos to record observations and spontaneous ideas to gain an initial overview of the text material and to maintain a rough structure of the categories. Additionally, we recorded remarkable insights for the analysis with the help of annotations.
Based on the reviewed literature, the theoretical background and the research questions, a deductive category system was developed in advance (table 1) .
To achieve a coherent refinement of the data material, free of divergences, it was reviewed multiple times. To become familiar with the material, we first undertook an inductive process of coding the data. In this process, after coding of eight interviews, many similarities and some overlaps in the codes were identified. Therefore, at this point, the line-by-line coding was divided into thematic groupings by two different coders, both final-year students from the Institute of Psychology of the University of Bern. This was done to counteract subjectivity, establish better reliability and to have the possibility to discuss discrepant cases together. The resultant groupings clearly showed that the discussed topics had a high overlap with the previously established deductive category system. The material was then assigned to the main categories and subcategories, as well as to new categories derived from the inductive process. Some categories previously formed in the deductive process were dropped due to lack of mention. Finally, a differentiated category system based on deductive and inductive categories was established (table 1).
In the second coding process, we coded the entire material using the new differentiated category system.
While the primary focus of this study is qualitative, basic descriptive statistics were employed to summarise the demographic information of the participants. This included calculating means and standard deviations (SD) for continuous variables such as age and years of work experience, and frequencies and percentages for categorical variables such as sex, type of practice (individual vs group office) and location of practice (rural vs urban). These measures provide a quantitative overview of the sample characteristics, enhancing the contextual understanding of the qualitative findings.
Sixteen of the eighteen GPs invited to participate in the study accepted. The final sample consisted of 10 female (63%) and 6 male (37%) GPs, with an average age of 48 years (SD: 11.6) and an average work experience of 13 years (SD: 10.6). Five GPs (31.3%) worked in their own office and eleven GPs (68.7%) were employed in a group office, with ten offices located in rural areas and 6 in cities, all across six cantons in the German-speaking part of Switzerland (i.e. Aargau, Bern, Basel-Stadt, Luzern, Wallis, Zürich).
The interviewees showed an overarching utilisation of various learning opportunities, where formal entities such as seminars, courses, conferences and webinars account for the minor part of knowledge acquisition (25%). The majority (75%) takes place through self-directed learning entities like peer communication, being peer-to-peer (p2p) in-house, remote or in the form of quality circles. Furthermore, electronic correspondence, practical work with patients, digital repositories, reading of media and reports, as well as writing, collecting, and reading notes were described self-directed learning opportunities. This is also reflected in the statements regarding its frequency. Twelve interviewees rate informal learning occasions as highly frequent (that is, on most workdays).
“...we really have a culture, where we go to each other’s office at any time for any question or to look at something, or we sit together at the computer and search together for the decisive knowledge. And we do this often.” (B1)
“And in the course of the COVID pandemic, we have also set up a chat where questions can be asked, like ‘How do you do this?’. It is still being used.” (B5)
“..., I use [UpToDate®] mainly when I have patient-specific questions, when I encounter diseases that I simply do not know or do not know enough about, or when I can’t proceed with my normal knowledge, then I look at that actually. And I do that several times a day.” (B3)
All interviewees make use of traditional and digital media, explicitly mentioning that the pandemic has led to a greater use of digital tools and resources. In detail, digital evidence-based platforms such as UpToDate®, medical guidelines, available hybrid professional media like the Swiss Medical Forum or Primary and Hospital Care, textbooks and government websites, such as The Federal Office of Public Health (BAG), were deemed important sources of information.
“If, for example, I have a patient in front of me and I can’t remember how to treat something or what the diagnosis is, then I use the MediX® Guidelines or UpToDate®.” (B12)
“On one hand, there are the weekly journals, ..., such as the Swiss Medical Forum and the Swiss Medical Weekly. They cover many general medical topics. And then there is also Primary Care, which is another journal … and it is especially for general practitioners.” (B13)
Generally, knowledge acquisition takes place in the office, at home, on the daily commute and at external venues, often depending on timeliness and effort.
“In the practice, at home and then of course at quality circles I must say. That’s the most important, and then at congresses as well.” (B5)
“So the professional journals at home or on the train, or otherwise, when I am on the go and in the office of course...” (B8)
“...[in the] office and at home and at on-site training. Journals, when I’m on vacation or when I’m on the train. Then I also read or listen to podcasts sometimes..., depending on the situation.” (B12)
Most commonly, knowledge acquisition takes place throughout the working day, followed by evenings and free-time learning. Morning and midday time slots are used only by a few.
“Or, if I need to know something quickly, then in practice throughout the day.” (B11)
“And then otherwise in the evening, when I have time.” (B14)
“Yes, and also over the weekend. Because during the week, it’s very busy in everyday practice and there’s no time left.” (B5)
“If it’s not urgent, then I’ll discuss it with my colleagues during the lunch break.” (B11)
For many, the motivation for knowledge acquisition comes from personal interest and the desire to provide the best possible service to patients. The interviewees also mention the eagerness to integrate new knowledge into daily practice, and the finding of content that is relevant for their patients and application-orientated, as motivational.
“Yes, because I want to be a good doctor. So, my motivation is to practice good medicine, evidence-based medicine. And yes, that’s why it’s important to me to offer the best possible service to my patients.” (B11)
“You need to have knowledge to treat the patients adequately and you need to acquire this knowledge. This is also my duty, I’m a doctor, I knew this when I learned the profession... And then there is also an aspect of continuing education, which someone would do out of own interest.” (B14)
Figure 1 gives a visual synthesis of the findings from research question 1.
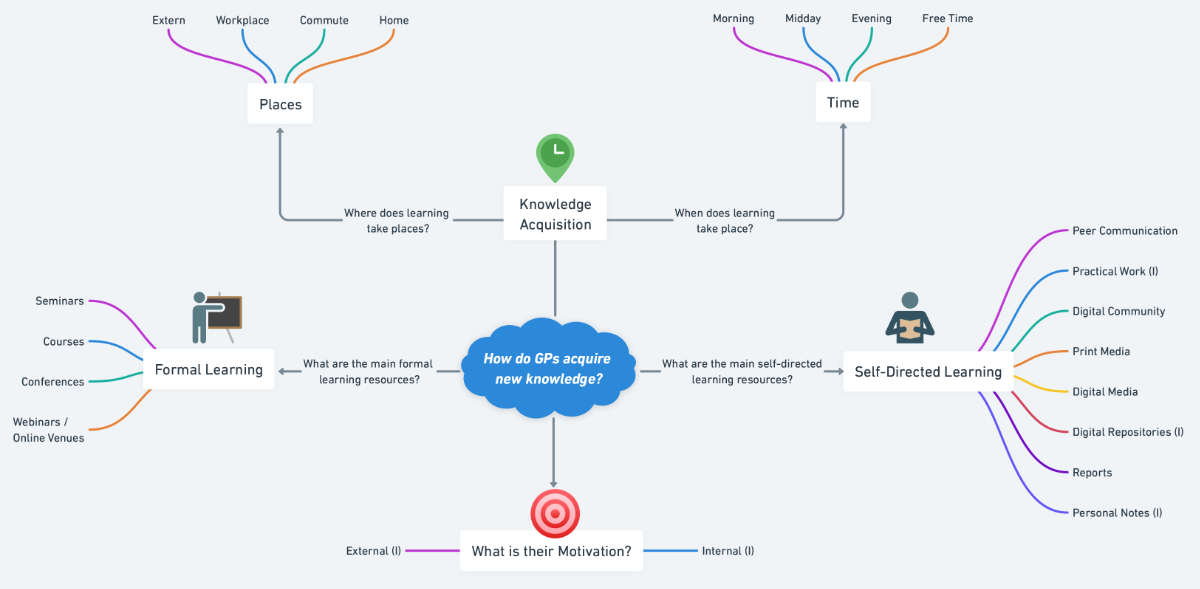
Figure 1Visual synthesis of the findings from research question 1. GP: general practitioner; (I): Inductive categories.
First and foremost, the COVID-19 pandemic has intensified the use of digital tools and digitally mediated education among most respondents.
“So, due to Covid … a lot is now online, which is not so bad. We even set up our quality circle online this year and it works quite well. Many trainings were online, actually, due to Covid, this has become easier.” (B2)
“It has really changed a lot. These Zoom meetings, we never had them before, and a lot has happened within this setting.” (B10)
“Yes, I think it has certainly been an essential driver (for digital media). Firstly due to the pandemic and secondly due to the flood of information, communication was almost only based on [digital] media.” (B11)
During the pandemic, the topics of knowledge acquisition had a strong tendency to focus on COVID-19 and pandemic-related topics, such as mental stress disorders. Here, the support of government agencies such as the BAG and the Cantonal Medical Office was largely perceived as helpful and appreciated.
“Yes, I think, Corona has taken up a lot of space. Suddenly there was nothing else or almost nothing else than this whole Corona story. And especially in the practice and in everyday life. And it always generated a lot of questions, be it from patients or colleagues, so you wanted to be totally up-to-date. Although other topics were still around, they were not as present as they used to be. So the focus completely shifted for two years.” (B7)
“So it was certainly the study of infectious diseases that was in focus or also these long-term forms and mental stress disorders. I think these are all topics that were more prominent. Yes, so that has changed.” (B15)
Although some respondents positively evaluated the increased use of digital aids and online education, considering them efficient and flexible, others preferred personal events and personal exchange in physical presence despite the increased use and availability of online resources and named reasonable issues, impeding full trust in digitalisation.
“It simplified my everyday life and I think it has also become more efficient regarding continuous professional development.” (B12)
“We also held the quality circles online during this pandemic, but that also had a downside; sometimes due to trivial technical issues, like the sound quality being bad and people being inaudible and always getting interrupted and so on. So yes, that was not optimal. And since we’ve been able to meet again, it’s much better.” (B9)
“But what needs to be said is that during the pandemic, no congresses took place and that was very bad for me... When I wanted to start again [after a work break], Corona came and then for two years there was simply nothing.” (B14)
The pandemic also increased the pressure for knowledge acquisition on COVID-19 and the general workload, as expressed at least by some GPs. This was seen negatively on most occasions, especially leaving a Kafkaesque feeling as the term “front-line” was very hospital-focused and primary care physicians felt unrecognised and left out of decision-making.
“So during the pandemic, I got up earlier and read the stuff before office...” (B1)
“Not objective enough, because it was very hospital-focused. The general practitioners didn’t really have a voice. There was no one from the general practitioners involved in the task force. People usually go to the general practitioner first, and there, the general practitioners were actually not represented or hardly represented.” (B13)
“Our everyday practice was heavily changed. We spent countless hours on information work, on additional services, which were neither compensated nor acknowledged.” (B14)
Furthermore, only some GPs mentioned an increased frequency of informal learning / self-directed learning under the pandemic, while the majority of GPs rated the frequency as unchanged.
Most GPs commented on a change with regard to the learning location, with the main change being the cancellation of learning venues in physical presence, which included mainly formal learning venues, but also self-directed learning-based learning opportunities like quality circles.
Figure 2 gives a visual synthesis of the findings from research question 2.
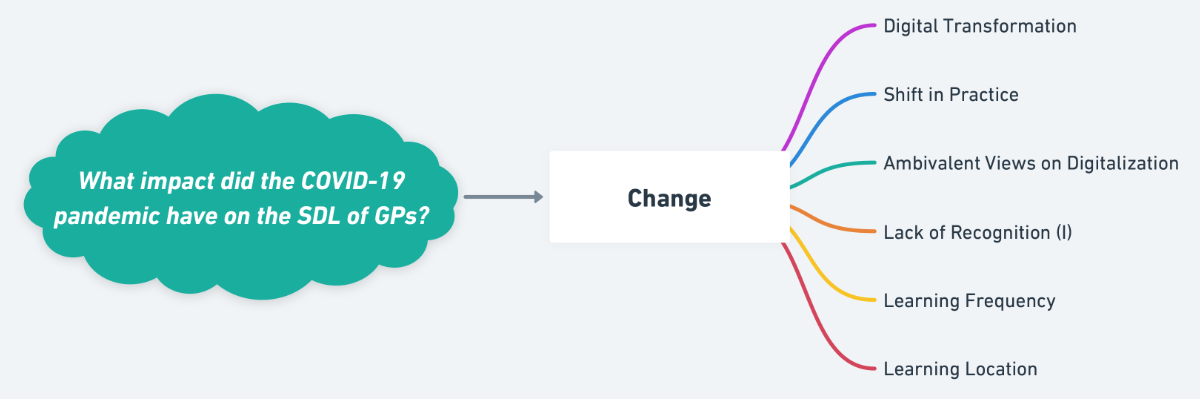
Figure 2Visual synthesis of the findings from research question 2. (I): Inductive categories; SDL: self-directed learning.
GPs reported a plethora of advancing and impeding factors as seen in figure 3. Taking these factors and the gained experience into account as a basis, we asked the GPs to make suggestions on how to optimise their self-directed learning and identified the following four clusters of optimisation potential:
The COVID-19 pandemic has catalysed the use of digital tools and continuing education for the majority of GPs, and many expressed the desire for digital offerings to remain available, to be extended and to be improved, and to integrate new media formats and technologies, such as virtual reality.
“I would advocate for the online options to remain and be expanded because some courses are still not offered online today.” (B12)
“My useful link collection... I found them because colleagues recommended them to me and that might be helpful: a kind of exchange with good tips where you can look something up.” (B14)
“...I wish for new technologies, such as virtual reality, to play a larger role in knowledge transfer or knowledge acquisition. I would be interested if we could somehow make this a bit more modern and contemporary.” (B7)
Most GPs also wish for an even stronger network and more opportunities for exchange with their peers.
“For example, I would deem even more exchange with colleagues beneficial.” (B13)
“And I hope that the exchange remains as lively as it is. I find the feedback from others and their opinions so important, as well as this work with peers, that’s very important to me.” (B14)
Furthermore, the desire for more practice-orientated content and application-orientated transfer of knowledge was frequently expressed.
“Rather, convey the theory in a more application-oriented way like in the US... or convey directly applicable knowledge for service...” (B2)
“More concise training opportunities... This is wishful thinking. More qualitative and less quantitative content, which is supported by professional societies and then you get points. But then it’s not really looked at whether this point is now relevant for me and my practice and my patients.” (B6)
“But the conveyance of knowledge or the theory of something, I can imagine that could somehow become more interactive, livelier and three-dimensional.” (B7)
The GPs also wish for better integration of continuing education into their daily work schedule and a greater emphasis on the importance of lifelong learning. Therefore, the desire for better framework conditions and more flexible training requirements has been mentioned to promote knowledge acquisition.
“Yes, I think one should simply not impose too many restrictions. Not everything should be made obligatory. Instead, we should have a bit more freedom again so that we can choose for ourselves.” (B5)
“...perhaps this is a particular problem for part-time working doctors with families … to accumulate their [CME] points. Because even if they only work 20%, they naturally have to have the same number of points.” (B9)
“It would really be helpful if tools like Zoom and Teams were more supported. For example, there is a video conference in the hospital for one hour once a week on a topic.. . And then I also asked if it would be possible for one to log in remotely, for example. Unfortunately, that was not possible. And I can’t leave for an hour of formal education, otherwise I’d be away for half the day... ...especially in the rural areas, this is important. It’s not the same as in the city.” (B10)
“…especially with the view that more and more people [i.e. parents] are working part-time, is to make shorter, practice-relevant courses and do this online. This way, for example, I could attend such learning opportunities much more flexibly and at the same time manage everything with the kids.” (B11)
Figure 3 gives a visual synthesis of the findings from research question 3.
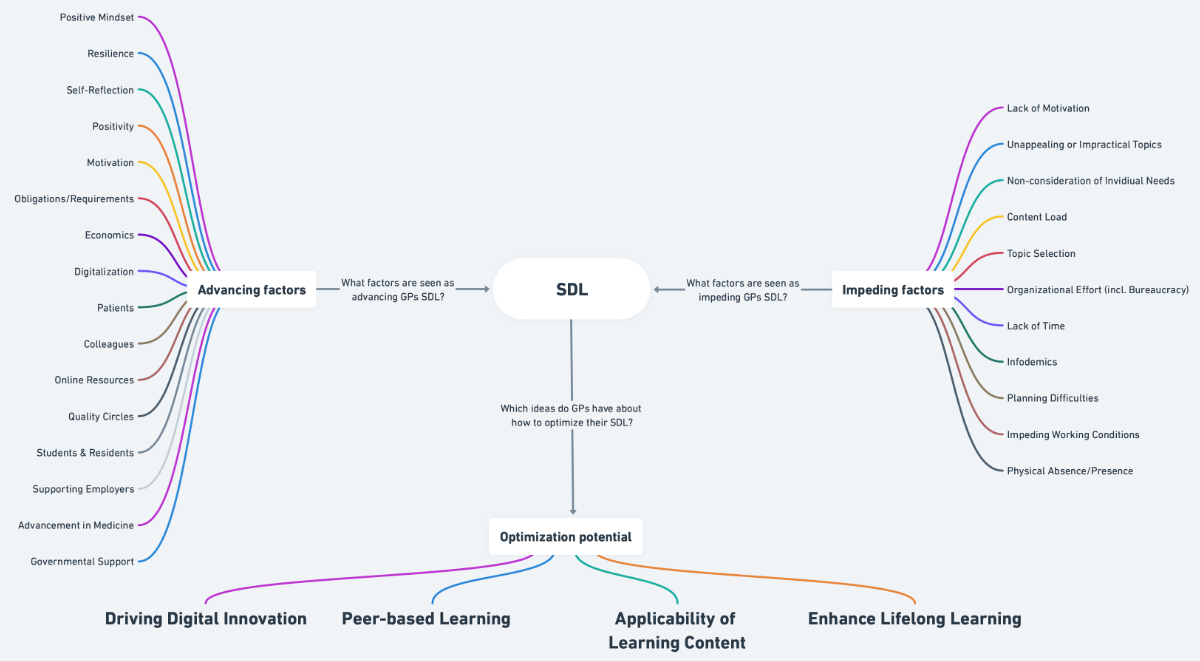
Figure 3Visual synthesis of the findings from research question 3. GP: general practitioner; SDL: self-directed learning.
This qualitative study sought to examine general learning activities and self-directed learning habits of GPs from the German-speaking part of Switzerland by employing a mixed deductive/inductive-based thematic analysis of how new knowledge is acquired, whether this modus operandi was influenced by the COVID-19 pandemic, and how self-directed learning could be optimised in the future.
For the first research question on how GPs acquire new knowledge, we found that with regard to learning opportunities, the participants display a versatile approach towards self-directed learning by employing a mix of formal and informal (SDL) – sometimes hybrid – learning activities. Within the cluster of self-directed learning activities, communication with peers remains the most constant and important informal learning entity for GPs. This finding is consistent with the existing literature, where self-directed learning and especially peer communication also proved to be the main way primary care physicians learn [6–12]. However, in Use of media, a significant shift can be seen over the last 25 years. Around the start of the millennium, when online computing and communication were already established, printed books and journals were still reported as the most important informal learning resources after peer communication, while online bibliographies and platforms were named last [9]. And while we still find use of print media for self-directed learning in our study, it’s mainly referring to journals, while books were now only explicitly mentioned by a quarter of the interviewees. Concurrently, with the momentum of digital transformation gained under the pandemic, online media are now in use by every interviewee. In particular, digital knowledge platforms and conferencing software gained huge popularity, as well as other digital formats like podcasts and video platforms for practical learning. Matching the fundamental idea of targeted problem-based learning in self-directed learning, straightforward, practical knowledge platforms such as the MediX®-Guidelines were often preferred for quick gains in learning, while more-comprehensive and anglophone platforms such as UpToDate® were often deemed inconvenient for such purposes. However, acquiring new knowledge in a timely manner and staying abreast of emerging trends with digital media is considered crucial for patient care and overall professional development by our interviewees. Therefore, even if we exclude recent pandemic changes, a strong technological shift has occurred in the last 25 years, which reflects the information needs of GPs today [16] and highlights the practical necessity for GPs to embrace digital platforms for efficient and immediate access to knowledge, thereby enhancing their capacity for self-directed learning in a rapidly evolving medical landscape.
When asking the interviewees about their motivation to pursue new knowledge, practical work with patients is still the main driver, which is also in accordance with the extant literature [9, 13]. Interestingly enough, in addition to personal preferences and working with residents, motivation to learn and personal development in itself, as well as medical and technological progress, were considered main motivators for staying up-to-date. In this sense, well-written reports from specialists have also been named important informal learning opportunities for quite a few of the interviewees, which is also a long-term motivator for GPs to acquire knowledge [12]. This underlines the practical aspect of motivation in self-directed learning to align learning objectives with clinical practice and personal development goals to sustain engagement and progression.
When inquiring about knowledge acquisition places and time, we found that our interviewees seize upon various locations and time slots adapted to timeliness and effort. Swift sessions of knowledge acquisition, for example, on specific questions in problem-orientated settings, are often looked up instantly in the office in between patients, while in consultation or at lunch break, where the latter was also mentioned in conjunction with social aspects of peer communication. Broader learning goals, like reading up on new therapies or learning about a disease, are often placed in the evening both at work, after office hours, or at home. Furthermore, articles as well as podcasts are also in use, often on the daily commute, depending on time and travel modality. Formal learning entities mentioned in the interviews, namely seminars, courses, conferences and webinars, were widely deemed impractical when only available in physical presence. This accounts especially for short learning venues, attended by GPs from rural areas, which is consistent with the literature [34], while multiday venues are widely appreciated and highly regarded for meeting colleagues and having informal exchanges in physical presence, which is not yet possible in the same manner in solely online venues. Altogether, the diversity in learning locations and times – especially due to the digital realm – highlights the practicality of the integration of self-directed learning into daily life and allows GPs to tailor their learning experiences to fit their individual schedules and immediate needs.
Regarding our second research question on the impact of the COVID-19 pandemic on self-directed learning, we learned that it catalysed a digital transformation among the interviewed GPs, primarily driven by the need to access and communicate rapidly changing medical information. This finding echoes the global trend of accelerated digital transformation in various sectors due to the pandemic [35]. The mentioned benefits of digital knowledge acquisition are manifold: practicability, accessibility and the overall resource-efficient possibility of virtual attendance were reported by the majority of participating GPs. With regard to resource efficiency, research has quantified the reduction of carbon emission in virtual attendance with up to two orders of magnitude lower than for in-person attendance [36]. Furthermore, online educational opportunities are described as a flexible, convenient and suitable trend for “time-poor” GPs [37] and was also widely welcomed in our interviews. Hence, the digital realm inherits the benefits of enhanced accessibility and flexibility of learning resources, making continuous education more feasible for GPs despite time constraints and the dynamic nature of medical knowledge.
Nevertheless, knowledge management under the digital shift has been challenging and inherits ambivalent views on digitalisation. Digitalisation-related concerns included technical difficulties, such as instable or lost connections, and impairment of audiovisual quality in meetings. Interestingly, we did not find a significant correlation between age and use of digital media, while we found in the literature that older GPs were less likely to use online learning, especially for self-education purposes [37]. When divided by the mean age of 48 years, our participants aged over 48 years – who were also the GPs with the most work experience, ranging from 15 to 37 years – showed a general use of digital media for learning, including digital knowledge platforms, guidelines, journals, official authority websites, podcasts, Google and Wikipedia. However, since we did not explicitly quantify data, the frequency of usage might differ, with younger people presumably having more cumulative online time. However, we found that younger GPs also have a strong demand for peer learning, which is in accordance with the literature [38] and their background as digital natives has them well positioned for hybrid or online learning solutions, which include virtual contact with peers, future integration of Artificial Intelligence (AI) and the Internet of Things (IoT) into their self-directed learning. Ultimately, staying up-to-date is necessary as more and more patients also acquire information on the internet as their main source of health-related questions and bring this information into consultations [39, 40]. Addressing the ambivalent views on digitalisation in self-directed learning requires overcoming technical barriers and integrating digital tools that cater to the diverse preferences and technical proficiencies of GPs.
Despite the fact that most GPs recognised the work of the authorities under the pandemic, the sheer amount of information and its half-life have clearly complicated knowledge acquisition and hold potential for a gratification crisis as the interviewees mentioned a lack of recognition of their work on the front line. As filtering and transferring short-lived information to patients was part of the significant increase in workload and front-line burden under the pandemic, some of the interviewees expressed a Kafkaesque feeling about the overall situation, where the use of the “front-line” qualifier was perceived as very hospital-focused and GPs felt unrecognised and left out of decision-making while being on the front line, echoing other studies from around the world [41–43]. Our findings underscore the practical necessity for effective communication and acknowledgment mechanisms from official authorities to support GPs in their self-directed learning efforts, particularly in managing the overload of information and maintaining their morale as well as recognising their pivotal role in patient care.
The interviewed GPs spent a significant proportion of time going into pandemic-related topics and consequently less on non-pandemic-related consultations on acute and chronic disease, which was widely considered negative. This, as well as an also-reported increase in general workload and the aforementioned pandemic-related bureaucracy, was also found in other research [44]. And while this shift and its momentum have their positive aspects, it must not be forgotten that continuous professional development especially of novice GPs needs space for diverse learning on the holistic spectrum of primary care. Undisputedly, rapid response measures and early intervention efforts, such as under the COVID-19 pandemic, belong in this spectrum. Yet, primary care’s mainstay is a much broader spectrum of diseases, clinical decision-making, advanced consultation skills, practice management, leadership and commissioning [45, 46].
Unsurprisingly, under the aforementioned digital shift, we found a consequent decline of formal learning venues in physical presence under COVID-19, and many interviewees praise the possibility of online attendance. However, a frequently mentioned barrier remains the informal aspect of such formal events, and the meeting of colleagues in physical presence is still valued and untouched regardless of digital progress. In this sense, hybrid venues were often seen as the best way forward, to meet everyone’s expectations. In addition to that, in formal venues, physicians tend to focus on content that is of personal interest and relevant to their daily practice, which was also found by other researchers [37]. Therefore, the cultivation of hybrid learning models that maintain the value of face-to-face interactions while leveraging the benefits of digital platforms seems crucial to ensure a comprehensive and engaging learning experience for GPs.
Regarding our third research question on optimisation potentials for more successful self-directed learning practice, participants perceived the COVID-19 pandemic as a catalyst for driving digital innovation, namely the use of digital tools and online continuing education, and many GPs expressed the desire for digital offerings to remain available, to be extended, to be improved and to further integrate new media formats and technologies.
Furthermore, most of the interviewees also wish for an even stronger network and more opportunities for exchange with colleagues in the sense of peer-based learning. In light of this, we see the biggest informal potential in quality circles, which are well-established, organised and accepted learning venues of informal and partly self-imposed formal character that offer many benefits for quality of practice, professional development and psychological wellbeing of primary care physicians [47–51]. Such venues offer an optimal foundation for sustained hybrid solutions on the basis of accessibility (in terms of location and cost) and preference to make way for a maximum participation and peer learning effect. Digitalisation holds myriad possibilities to enhance such peer communication events even further due to peer availability. For planning virtual attendance, it is noteworthy though that initial meetings in physical presence made future virtual attendance even more effective [52]. This underlines the practical implication of connecting digital innovation and quality circles and seizing upon their symbiotic effects for enhancing self-directed learning among GPs.
Regarding mandatory professional development, regulated by the Swiss Medical Profession Act (MedBG) [4, 5], one suggestion from the interviewees was to establish informal self-test opportunities from official authorities that provide individual feedback on where improvement is needed, without being formally judged. Furthermore, to achieve optimal integration into the daily work routine, many interviewees also wish for a better integration of continuing education into everyday work. Therefore, the desire for better framework conditions, less bureaucracy and more-flexible training should be promoted to foster knowledge acquisition in primary care physicians. Context-related challenges such as information overload underscore the need for strategic management of learning resources and appropriate time allocation for self-directed learning. The proposed context optimisation solutions, such as the provision of time quotas for self-directed learning and communication with colleagues, could prove beneficial in overcoming these challenges. These findings place emphasis on creating more-flexible and integrated learning opportunities within the daily routine and highlights the practical significance of aligning self-directed learning with the dynamic workflow of GPs.
Our findings might be limited due to the relatively small sample size and geographic restriction to the German-speaking part of Switzerland. In this regard, approaches towards self-directed learning, the influence of the pandemic as well as the needs and demands for optimising self-directed learning might not give the full picture. However, the literature echoes similar findings to ours on peer group dynamics and clinically relevant learning [38]. Additionally, this study follows a qualitative approach and does not claim to reflect the self-directed learning habits of all GPs, but rather to reflect the opinions of a representative sample. Furthermore, the convenience sampling we used would not be appropriate for a study aiming for generalisability, but represents a valid method in qualitative research for the acquisition of new insights. Therefore, our study provides implications from which further research can proceed. Future studies may explore the impact and potential of emerging digital technologies, including virtual reality and artificial intelligence in self-directed learning among GPs and assess their long-term effectiveness, feasibility and impact on professional development and quality of patient care. Furthermore, a more in-depth investigation on the experiences of GPs across different demographics and contexts could provide a more comprehensive understanding of self-directed learning practices. There may also be a need to further explore the notion of self-directed learning in a post-pandemic world, given the inevitable changes brought about by the pandemic. Understanding how GPs adapt to these challenges can be instrumental in shaping policies and practices for future self-directed learning initiatives also under unforeseen global health events.
The present findings contribute to a better understanding of self-directed learning among GPs, particularly during unprecedented global health challenges. The COVID-19 pandemic has expedited the digital transformation of self-directed learning, with GPs expressing interest in hybrid learning scenarios that balance digital and traditional learning methods with a strong focus on peer-based communication. In this sense, we see the biggest informal potential in the future role of digitally enhanced quality circles as a sustained hybrid solution on the basis of accessibility (in terms of location and cost) and preference to make way for a maximum participation and peer learning effect. Here, digitalisation could be used to enhance peer communication further due to peer availability, e.g. through problem-focused chats among the quality circle members, to seize upon filtered, concise knowledge, based on swarm intelligence. For an optimal entry, we suggest initial meetings in physical presence, as virtual attendance is seen as significantly more effective when done after meeting new people face-to-face. In accordance with the interviewees’ wish for a more practice- and application-orientated transfer of knowledge, we also support the idea of establishing informal self-assessments by official authorities as such can support GPs in setting priorities and finding more adequate formal venues to match their daily practice demands and self-directed learning. Our findings provide useful pointers for optimising learning resources and environments that resonate with the GPs’ learning needs and preferences and underline the urgent need to address the identified barriers and harness the beneficial factors to optimise self-directed learning. It is crucial to evaluate if the GPs themselves should be encouraged to more actively network and exchange information and its sources, or if this also needs to be picked up by official authorities. Our paper suggests both tracks are promising.
We extend our deepest gratitude to the participating general practitioners.
This study did not make use of any public, commercial, or not-for-profit funding.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Knowles M. Self-directed learning: a guide for learners and teachers. New York: Association Press, 1975.
2. Hill JR, Song L, West RE. Social Learning Theory and Web-Based Learning Environments: A Review of Research and Discussion of Implications. Am J Distance Educ. 2009 May;23(2):88–103.
3. Bate E, Hommes J, Duvivier R, Taylor DC. Problem-based learning (PBL): getting the most out of your students - their roles and responsibilities: AMEE Guide No. 84. Med Teach. 2014 Jan;36(1):1–12.
4. Kauffman DM, Mann KV. Teaching and learning in medical education. in Understanding Medical Education, 2013, pp. 7–29. doi: https://doi.org/
5. Bundesgesetz über die universitären Medizinalberufe (Medizinalberufegesetz, MedBG). Internet: https://www.fedlex.admin.ch/eli/cc/2007/537/de.
6. Slotnick HB. How doctors learn: physicians’ self-directed learning episodes. Academic Medicine, vol. 74, no. 10, 1999. https://journals.lww.com/academicmedicine/Fulltext/1999/10000/How_doctors_learn__physicians__self_directed.14.aspx
7. Cervero RM. Place matters in physician practice and learning. Journal of Continuing Education in the Health Professions, vol. 23, 2003. https://journals.lww.com/jcehp/Fulltext/2003/23011/Place_matters_in_physician_practice_and_learning.4.aspx 10.1002/chp.1340230405
8. Westberg EE, Miller RA. The basis for using the Internet to support the information needs of primary care. J Am Med Inform Assoc. 1999;6(1):6–25.
9. Verhoeven AA, Boerma EJ, Meyboom-de Jong B. Use of information sources by family physicians: a literature survey. Bull Med Libr Assoc. 1995 Jan;83(1):85–90.
10. Coumou HC, Meijman FJ. How do primary care physicians seek answers to clinical questions? A literature review. J Med Libr Assoc. 2006 Jan;94(1):55–60.
11. Dorsch JL. Information needs of rural health professionals: a review of the literature. Bull Med Libr Assoc. 2000 Oct;88(4):346–54.
12. Owen PA, Allery LA, Harding KG, Hayes TM. General practitioners’ continuing medical education within and outside their practice. BMJ. 1989 Jul;299(6693):238–40.
13. Stanley I, al-Shehri A, Thomas P. Continuing education for general practice. 1. Experience, competence and the media of self-directed learning for established general practitioners. Br J Gen Pract. 1993 May;43(370):210–4.
14. Clarke MA, Belden JL, Koopman RJ, Steege LM, Moore JL, Canfield SM, et al. Information needs and information-seeking behaviour analysis of primary care physicians and nurses: a literature review. Health Info Libr J. 2013 Sep;30(3):178–90.
15. Vollmar HC, Rieger MA, Butzlaff ME, Ostermann T. General Practitioners’ preferences and use of educational media: a German perspective. BMC Health Serv Res. 2009 Feb;9(1):31.
16. M. S. Knowles, E. F. Holton III, R. A. Swanson, and P. A. Robinson, The Adult Learner. Routledge, 2020. doi: .
17. Verspoor K. The Evolution of Clinical Knowledge During COVID-19: Towards a Global Learning Health System. Yearb Med Inform. 2021 Aug;30(1):176–84.
18. Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020 Jun;20(6):631–3.
19. Williams SN, Armitage CJ, Tampe T, Dienes KA. Public perceptions of non-adherence to pandemic protection measures by self and others: A study of COVID-19 in the United Kingdom. PLoS One. 2021 Oct;16(10):e0258781.
20. Chhablani N, Choudhari SG. Behind the Frontline: A Review on the Impact of COVID-19 Pandemic on Healthcare Workers. Cureus. 2022 Sep;14(9):e29349.
21. Wohlfarth B, Gloor B, Hautz WE. Challenges of students and residents of human medicine in the first four months of the fight against the Covid-19 pandemic - Implications for future waves and scenarios. BMC Med Educ. 2021 Oct;21(1):554.
22. Bogner A, Littig B, Menz W. Introduction: Expert Interviews — An Introduction to a New Methodological Debate. Interviewing Experts. London: Palgrave Macmillan UK; 2009. pp. 1–13.
23. Neubauer BE, Witkop CT, Varpio L. How phenomenology can help us learn from the experiences of others. Perspect Med Educ. 2019 Apr;8(2):90–7.
24. Philipp Mayring. Einführung in die qualitative Sozialforschung. 7th ed. Beltz; 2023.
25. Wagemann C, Goerres A, Siewert MB, Meuser M, Nagel U. Handbuch Methoden der Politikwissenschaft. Wiesbaden: Springer Fachmedien Wiesbaden; 2020.
26. L. Gideon, Handbook of Survey Methodology for the Social Sciences. New York (NY): Springer New York; 2012.
27. Hiemstra R, Brockett R. Reframing the Meaning of Self-Directed Learning: An Updated Model. New Prairie Press, 2012. Accessed: Apr. 27, 2023. [Online]. Available: https://newprairiepress.org/aerc/2012/papers/22/
28. Candy P. Self-Direction for Lifelong Learning. Jossey-Bass; 1991.
29. Murad MH, Coto-Yglesias F, Varkey P, Prokop LJ, Murad AL. The effectiveness of self-directed learning in health professions education: a systematic review. Med Educ. 2010 Nov;44(11):1057–68.
30. Sawatsky AP, Ratelle JT, Bonnes SL, Egginton JS, Beckman TJ. A model of self-directed learning in internal medicine residency: a qualitative study using grounded theory. BMC Med Educ. 2017 Feb;17(1):31.
31. Kuckartz U, Raediker S. Qualitative Inhaltsanalyse. Methoden, Praxis, Computerunterstützung. 5th ed. Beltz; 2022.
32. Trachsel S, Schaufelberger M, Feller S, Küng L, Frey P, Guttormsen Schär S. Evaluation eines neuen Mentoring-Programms für Medizinstudierende in der hausärztlichen Grundversorgung: Erfahrungen von Studierenden und Lehrärzten. GMS Z Med Ausbild., vol. 27(3):Doc42, 2010, [Online]. Available:
33. Dresing T, Pehl T. Praxisbuch Interview, Transkription & Analyse. Anleitungen und Regelsysteme für qualitativ Forschende., vol. 8. Marburg, 2018.
34. Cunningham DE, Ward C, Kyle J, Yeoman L. Learning needs, preferred learning methods and learning challenges of first five general practitioners in NHS Scotland: a qualitative study. BMJ Open. 2021 May;11(5):e044859.
35. Taylor DC, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013 Nov;35(11):e1561–72.
36. Gattrell WT, Barraux A, Comley S, Whaley M, Lander N. The Carbon Costs of In-Person Versus Virtual Medical Conferences for the Pharmaceutical Industry: Lessons from the Coronavirus Pandemic. Pharmaceut Med. 2022 Apr;36(2):131–42.
37. Yee M, Simpson-Young V, Paton R, Zuo Y. How do GPs want to learn in the digital era? Australian Journal for General Practitioners, vol. 43, pp. 399–402, 2014. https://www.racgp.org.au/afp/2014/june/learning-in-the-digital-era
38. How do GPs want to learn in the digital era? Australian Journal for General Practitioners, vol. 43, pp. 399–402, 2014. https://www.racgp.org.au/afp/2014/june/learning-in-the-digital-era
39. Wald HS, Dube CE, Anthony DC. Untangling the Web—the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns. 2007 Nov;68(3):218–24.
40. Marstedt G. Das Internet: Auch Ihr Ratgeber für Gesundheitsfragen? Bertelsmann Stiftung; 2021.
41. Gu A, Willis K, Kay M, Hutt K, Smallwood N. ‘We are largely left out’: workplace and psychosocial experiences of Australian general practitioners during the initial months of the COVID-19 pandemic. Aust J Prim Health. 2023 Feb;29(1):47–55.
42. Cohidon C, El Hakmaoui F, Senn N. The role of general practitioners in managing the COVID-19 pandemic in a private healthcare system. Fam Pract. 2022 Jul;39(4):586–91.
43. Makowski L, Schrader H, Parisi S, Ehlers-Mondorf J, Joos S, Kaduszkiewicz H, et al. German general practitioners’ experiences during the COVID-19 pandemic and how it affected their patient care: A qualitative study. Eur J Gen Pract. 2023 Dec;29(2):2156498.
44. Schrimpf A, Bleckwenn M, Braesigk A. COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave. Healthcare (Basel). 2023 Jan;11(3):320.
45. Taylor C, Parsons J, Sparrow N, Gerada C. The first5 concept. Br J Gen Pract. 2011 Jan;61(582):72–3.
46. Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020 Jun;10(6):e039674.
47. Rohrbasser A, Harris J, Mickan S, Tal K, Wong G. Quality circles for quality improvement in primary health care: their origins, spread, effectiveness and lacunae- A scoping review. PLoS One. 2018 Dec;13(12):e0202616.
48. Beyer M, Gerlach FM, Flies U, Grol R, Król Z, Munck A, et al. The development of quality circles/peer review groups as a method of quality improvement in Europe. Results of a survey in 26 European countries. Fam Pract. 2003 Aug;20(4):443–51.
49. Eliasson G, Mattsson B. From teaching to learning. Experiences of small CME group work in general practice in Sweden. Scand J Prim Health Care. 1999 Dec;17(4):196–200.
50. de Villiers M, Bresick G, Mash B. The value of small group learning: an evaluation of an innovative CPD programme for primary care medical practitioners. Med Educ. 2003 Sep;37(9):815–21.
51. Rohrbasser A, Wong G, Mickan S, Harris J. Understanding how and why quality circles improve standards of practice, enhance professional development and increase psychological well-being of general practitioners: a realist synthesis. BMJ Open. 2022 May;12(5):e058453.
52. Shaw T, Long A, Chopra S, Kerfoot BP. Impact on clinical behavior of face-to-face continuing medical education blended with online spaced education: a randomized controlled trial. J Contin Educ Health Prof. 2011;31(2):103–8.