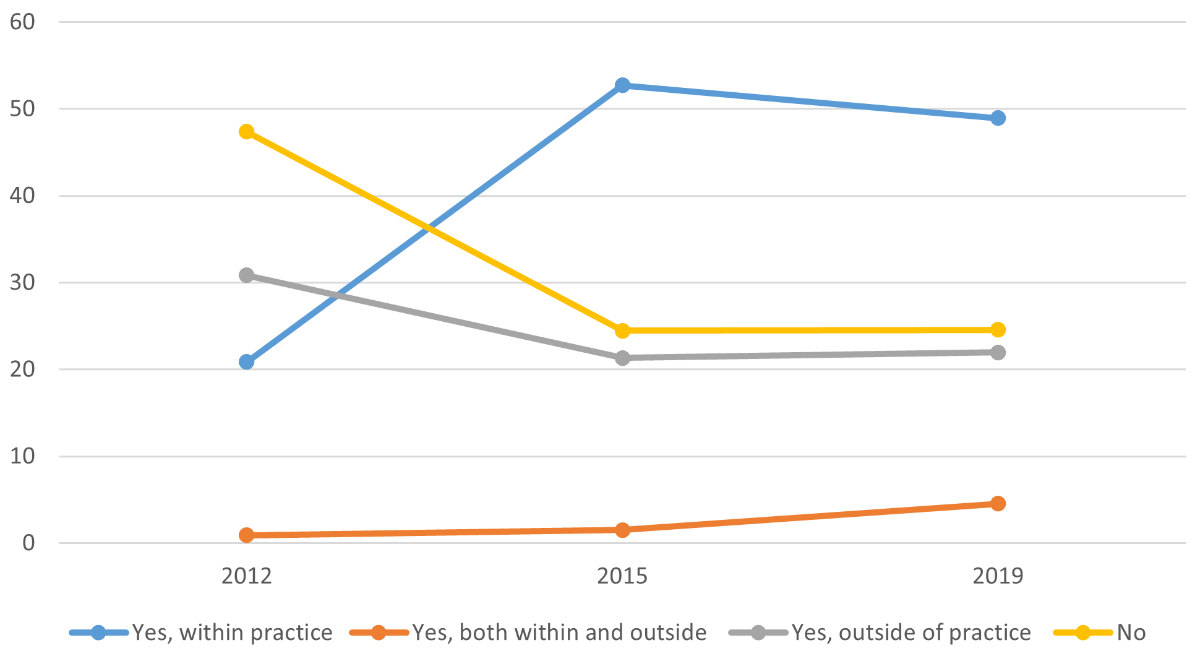
Figure 1Frequencies (in %) of case managers in general practitioner practices between 2012 and 2019, weighted data.
DOI: https://doi.org/https://doi.org/10.57187/s.3425
In the context of longer life expectancy and thus increasing prevalence of chronic illnesses and often multimorbidity, healthcare systems are facing challenges. Indeed, in response to an ageing global population and the desire to keep patients at home while at the same time reducing health costs, Western health systems have relied on the strengthening of primary care [1–4]. In parallel, an evolution of primary care models has emerged: the traditional model exclusively based on the general practitioner has been evolving by integrating other professionals and other functions allowing for better coordination of care for patients [5–7]. These new models of care, focused on multidisciplinary primary healthcare teams and proactive shared care, seem to be particularly relevant, especially for patients with long-term conditions [8].
It is in this context that case managers have emerged in primary care [8, 9]. Case managers are care provider other than the general practitioner (often a nurse) whose mission is mainly to coordinate the care of a patient in relation to one or more pathologies [10, 11]. Case management is defined as “a collaborative process of assessment, planning, facilitation, care coordination, evaluation and advocacy for options and services to meet an individual’s and family’s comprehensive health needs through communication and available resources to promote patient safety, quality of care, and cost-effective outcomes” [12]. It should be noted, however, that case management remains a generic term that has no single definition and represents a range of activities that may vary between different programmes and countries [13]. Furthermore, case management can be distinguished from care management in the care of a chronically ill population. Case management is aimed at a smaller part of the population with so-called “highly complex” health needs requiring personalised care, whereas care management is aimed at lower-risk chronic patients whose care will be more disease- and population-orientated than person-orientated [14, 15].
Literature has shown the effectiveness of case manager interventions. The benefits of such interventions include reductions in emergency department visits and hospital admissions, overall reductions in expenditures and improved patient outcomes such as quality of life and patient satisfaction [11, 16, 17]. Furthermore, it has been shown that they positively affect knowledge, social support and psychosocial beliefs for a variety of patients [18, 19].
The current literature on case management focuses mainly on the potential effects of this practice on the healthcare system (effectiveness, limitations, costs, etc.), as well as on the implementation of projects aimed at integrating case manager settings. However, it is difficult to find literature on this subject exploring the frequency of use in a context of international comparison, and similarly for the evolution of this practice over time. The present study fills this gap, which seems relevant given the effectiveness of this type of practice in the literature and the need for primary care reform more generally.
The aim of this study was to describe the frequency of use of case managers within general practitioner practices in 11 Western countries. In addition, this study will highlight a temporal evolution in the frequency of use of case managers in these countries between 2012 and 2019. Finally, possible associations of this use with other factors related to the characteristics of general practitioners and their practices will be investigated.
The data used comes from the Commonwealth Fund International Health Surveys of Primary Care Physicians conducted in 2012, 2015 and 2019. These are regularly conducted cross-sectional surveys of nationally representative, random samples of general practitioners investigating various domains related to primary care including general practitioners’ preparedness to manage care of patients with complex needs, communicate and coordinate with other specialties and stakeholders in the healthcare system and community, and use of information technology in health [20]. The surveys have been conducted since 2006 in eleven Western countries, namely Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom and the United States [21].
The survey population consisted of a random sample of primary care physicians from private or government lists in all countries except France, where the samples were selected from a nationally representative panel of primary care doctors [21]. As the professions responsible for primary care may vary across countries, experts defined the professionals sampled for each country. General practitioners and family physicians were included in all countries; internists and paediatricians were also included in Germany, Switzerland and the United States [21, 22]. The range of final sample sizes in different countries was 500–2124 in 2012, 502–2905 in 2015 and 500–2569 in 2019, yielding total sample sizes of 9776, 12,049 and 13,200, respectively [22–24]. The response rates by country varied from 20% to 66% in 2012, 19% to 47% in 2015 and 15% to 49% in 2019 [22–24]. Finally, data was weighted for each country to allow the final outcome to be representative of the primary care physician population [22]. Other characteristics and the study protocol of the surveys have already been detailed elsewhere [21, 22, 24–26].
Eligible participants were informed that they were free to decide whether to participate or not.
To ensure comparability between countries, the questionnaire was analysed by experts and adjusted for country-specific wording and translated when necessary [20]. The question investigated here, reported in the 2012, 2015 and 2019 surveys, was “Does your practice use personnel, such as nurses or case managers, to monitor and manage care for patients with chronic conditions that need regular follow-up care?” with possible answers “Yes, use personnel within the practice”, “Yes, use personnel outside the practice”, “Yes, use personnel both within and outside the practice” or “No”. In the 2012 survey, data about this question for Sweden was not available and the responses for France were not exactly the same as those given above. These two countries were therefore not included in our analysis for 2012. Finally, we selected several variables in order to characterise the use of case managers, including general practitioners’ sociodemographic characteristics such as sex (female; male), age (under 35; 35–44; 45–54; 55–64; 65 or older), practice location (city; suburb; small town; rural area; remote area) and size of medical practice described by the number of full-time equivalent (FTE) general practitioners in the practice. Data on practice size (FTE) was not available for Sweden in 2019.
The data was analysed with STATA software v16 (StataCorp LLC, College Station, Texas, USA). We used country-specific sampling weights already available (provided by the Commonwealth Fund) to balance the potential overrepresentation of general practitioners in relation to certain factors (sex, age, region) [20]. The weighting approach has already been described in detail in the methodology reports [22, 24]. First, we obtained descriptive statistics characterising the frequency of response by country. We repeated this for each survey (2012, 2015 and 2019) in order to follow the evolution of frequency over time. We analysed the question with the four possible responses. In addition, we created a binary Yes/No variable for the second part of the analysis, with Yes grouping the responses “Yes, use personnel within the practice” and “Yes, use personnel both within and outside the practice” and No grouping the responses “Yes, use personnel outside the practice” and “No”. This was done to focus on the role of the case manager working within the practice, as it is this practice which is of particular interest to us in this present study and which best fits the definition of case manager. Next, we used the 2019 survey to perform weighted, mixed-effects, multilevel (country/practice) logistic regression, using the country as the random factor. A multilevel model was used to take into account the nested nature of the data (numerous respondents in each country). In addition, using the country as the random factor allows, in a way, to introduce some information (latent variables) about the country’s health system. We studied the frequency of use of case managers (binary variable, defined above) within the practice as the dependent variable, according to the following four variables as independent variables: sex, age, practice location and practice size (FTE). First, we performed a bivariate analysis and then a multivariate analysis. Second, the independent variables were introduced via a manual forward stepwise selection to obtain the final multivariate model.
The “rural area” and “remote area” categories of practice location were combined into a single “rural area” category because of their similarity and the low number of respondents in the “remote area” category (1.2%). FTE is a continuous independent variable that was converted into a categorical one according to its distribution, described in quartiles (Q1 to Q4). The FTE values for each quartile were as follows: Q1 ≤1.2; Q2 1.2–2.5; Q3 2.5–4.5; Q4 ≥4.5.
Each country was responsible for ethical consent according to its own regulations. Local approval for this study was obtained from the ethics review board of each participating country.
The total number of respondents (general practitioners) was 9776 in 2012, 12,049 in 2015 and 13,200 in 2019. The proportion of female respondents increased over time, from 38.8% in 2012 to 45.5% in 2019. Regarding the age of general practitioners, there was an increase in the percentage of younger respondents (<35 years) from 7.7% in 2012 to 10.5% in 2019 as well as in the percentage of older respondents (>65 years) from 6.9% in 2012 to 13.1% in 2019 (table 1).
Table 1Sociodemographic characteristics of general practitioners taking part in the 2012, 2015 and 2019 Commonwealth Fund survey, weighted data.
| Distribution in each country | ||||||||||||||
| 2012 | ||||||||||||||
| n | AU | CA | FR | DE | NL | NZ | NO | SE | CH | GB | US | Total | ||
| Sample size, n | 500 | 2124 | 501 | 909 | 522 | 500 | 869 | 1314 | 1025 | 500 | 1012 | 9776 | ||
| Female sex (0.48% data missing) | 3794 | 37.04% | 40.21% | 33.69% | 37.68% | 39.16% | 45.00% | 36.66% | 52.65% | 30.41% | 38.86% | 37.51% | 38.81% | |
| Age, years (n = 9728, 0.49% data missing) | <35 | 754 | 7.61% | 8.77% | 7.20% | 1.50% | 7.08% | 7.80% | 12.78% | 9.43% | 1.29% | 12.31% | 7.27% | 7.71% |
| 35–44 | 2200 | 24.03% | 23.74% | 20.40% | 35.42% | 28.97% | 29.50% | 22.53% | 20.69% | 18.28% | 30.27% | 24.28% | 22.50% | |
| 45–54 | 3094 | 35.04% | 31.60% | 57.30% | 27.63% | 34.83% | 40.90% | 33.40% | 22.07% | 35.73% | 35.30% | 27.99% | 31.65% | |
| 55–64 | 3009 | 29.54% | 25.29% | 15.10% | 28.31% | 28.62% | 17.80% | 27.16% | 38.93% | 37.08% | 19.40% | 24.37% | 30.78% | |
| >65 | 671 | 3.79% | 10.60% | 0.00% | 7.13% | 0.50% | 4.00% | 4.13% | 8.89% | 7.62% | 2.72% | 16.08% | 6.86% | |
| 2015 | ||||||||||||||
| Sample size, n | 747 | 2284 | 502 | 559 | 618 | 503 | 864 | 2905 | 1065 | 1001 | 1001 | 12,049 | ||
| Female sex (0.27% data missing) | 5324 | 36.99% | 43.85% | 35.00% | 44.27% | 45.27% | 45.00% | 40.04% | 51.50% | 32.94% | 49.07% | 39.86% | 44.19% | |
| Age, years (n = 12,029, 0.17% data missing) | <35 | 1162 | 11.30% | 9.52% | 7.80% | 1.00% | 4.52% | 9.00% | 13.10% | 9.11% | 0.80% | 13.79% | 5.54% | 9.66% |
| 35–44 | 2921 | 28.80% | 22.10% | 15.80% | 35.68% | 28.12% | 29.00% | 31.70% | 26.62% | 18.08% | 30.88% | 20.29% | 24.28% | |
| 45–54 | 3155 | 32.10% | 27.50% | 28.10% | 27.59% | 31.32% | 40.01% | 22.00% | 24.35% | 31.28% | 29.97% | 29.13% | 26.23% | |
| 55–64 | 3561 | 17.30% | 26.24% | 39.00% | 28.59% | 33.33% | 18.00% | 27.00% | 28.12% | 36.36% | 19.16% | 28.83% | 29.60% | |
| >65 | 1230 | 10.50% | 14.52% | 9.30% | 7.12% | 2.71% | 4.00% | 6.20% | 11.81% | 13.49% | 6.20% | 16.13% | 10.23% | |
| 2019 | ||||||||||||||
| Sample size, n | 500 | 2569 | 1287 | 809 | 788 | 503 | 661 | 2411 | 1095 | 1001 | 1576 | 13,200 | ||
| Female sex (0.45% data missing) | 6004 | 45.02% | 45.99% | 37.54% | 45.36% | 52.29% | 55.00% | 43.71% | 51.17% | 40.55% | 46.10% | 44.84% | 45.48% | |
| Age, years (n = 13,153, 0.36% data missing) | <35 | 1391 | 13.91% | 10.96% | 2.97% | 0.81% | 10.05% | 13.12% | 12.81% | 12.45% | 1.70% | 28.74% | 8.06% | 10.54% |
| 35–44 | 3017 | 24.98% | 23.31% | 16.32% | 15.83% | 30.80% | 19.24% | 34.00% | 27.19% | 18.75% | 28.81% | 22.77% | 22.86% | |
| 45–54 | 3172 | 23.49% | 24.85% | 20.79% | 30.73% | 28.63% | 24.24% | 22.51% | 22.89% | 29.20% | 22.23% | 27.22% | 24.03% | |
| 55–64 | 3845 | 23.44% | 25.54% | 41.94% | 35.90% | 28.39% | 31.36% | 21.74% | 24.57% | 32.90% | 14.02% | 24.16% | 29.13% | |
| >65 | 1728 | 14.18% | 15.35% | 17.98% | 16.74% | 2.13% | 12.04% | 8.93% | 12.89% | 17.45% | 6.21% | 17.79% | 13.09% | |
AU: Australia; CA: Canada; FR: France; DE: Germany; NL: Netherlands; NZ: New Zealand; NO: Norway; SE: Sweden; CH: Switzerland; GB: United Kingdom; US: United States.
The overall frequency of general practitioners using a case manager within their practices varied from 20.9% in 2012 to 49.0% in 2019 (figure 1). There was an increase from 2012 to 2015, followed by a stagnation (or even a decrease) from 2015 to 2019. At the same time, the percentage of general practitioners not using case managers in their practices fell from 47.4% in 2012 to 24.5% in 2015 and 24.6% in 2019. In addition, the frequency of using personnel outside the practice also declined, but more slightly.
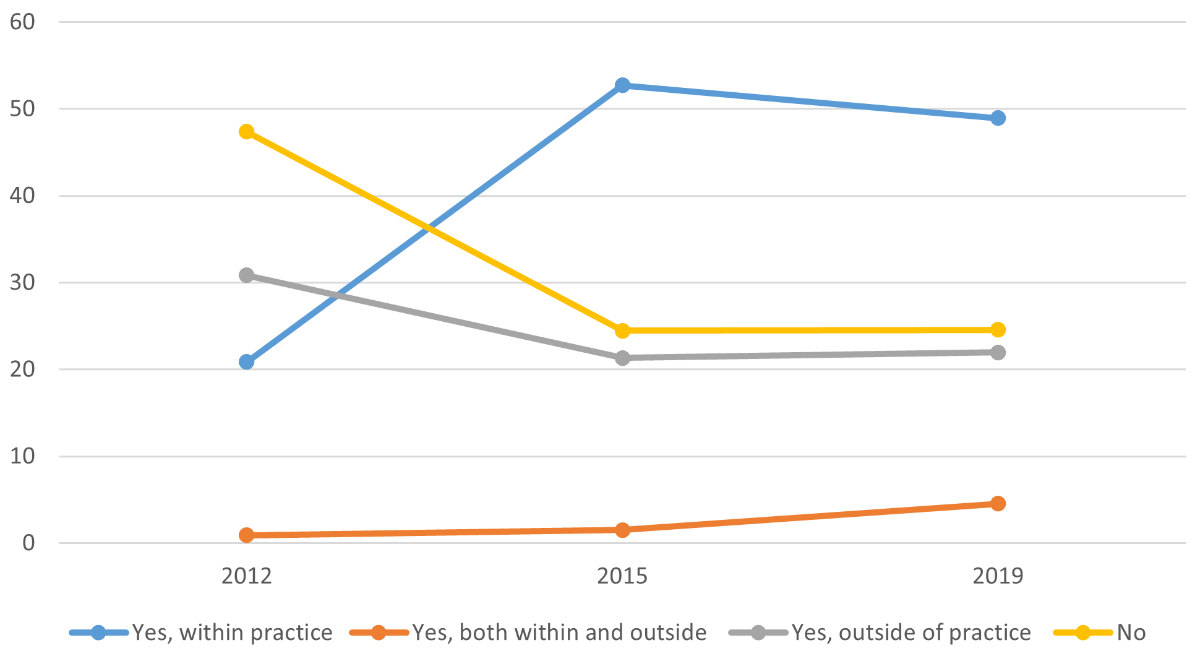
Figure 1Frequencies (in %) of case managers in general practitioner practices between 2012 and 2019, weighted data.
Among the countries surveyed, there were disparities in the frequency of use of case managers within general practitioner practices (figure 2). Australia, the Netherlands, New Zealand, Sweden and the United Kingdom seemed to be frequent users of case managers. The frequencies of practice (“Yes, use personnel within the practice” and “Yes, use personnel both within and outside the practice”) varied from 30.3% (United Kingdom) to 53.5% (Netherlands) in 2012, reaching 64.1% (Netherlands) to 89.5% (United Kingdom) in 2019. Once again, there was a trend towards an increase from 2012 to 2015, followed by stagnation or even a decrease in some countries from 2015 to 2019. In other countries (Canada, France, Germany, Norway, the USA), the frequencies of use of case managers (“Yes, use personnel within the practice” and “Yes, use personnel both within and outside the practice”) varied from 5.7% (Switzerland) to 22.8% (USA) in 2012 to 11.7% (Switzerland) to 52.1% (USA) in 2019. It should be noted that the USA and Canada had similar patterns and that Switzerland and France had similar curves, with the lowest frequencies of case managers. Looking at the temporal evolution, there was an increasing trend in the frequency of use of case managers for all countries except three (Australia, the Netherlands and Norway) which saw their curve decrease from 2015 to 2019.
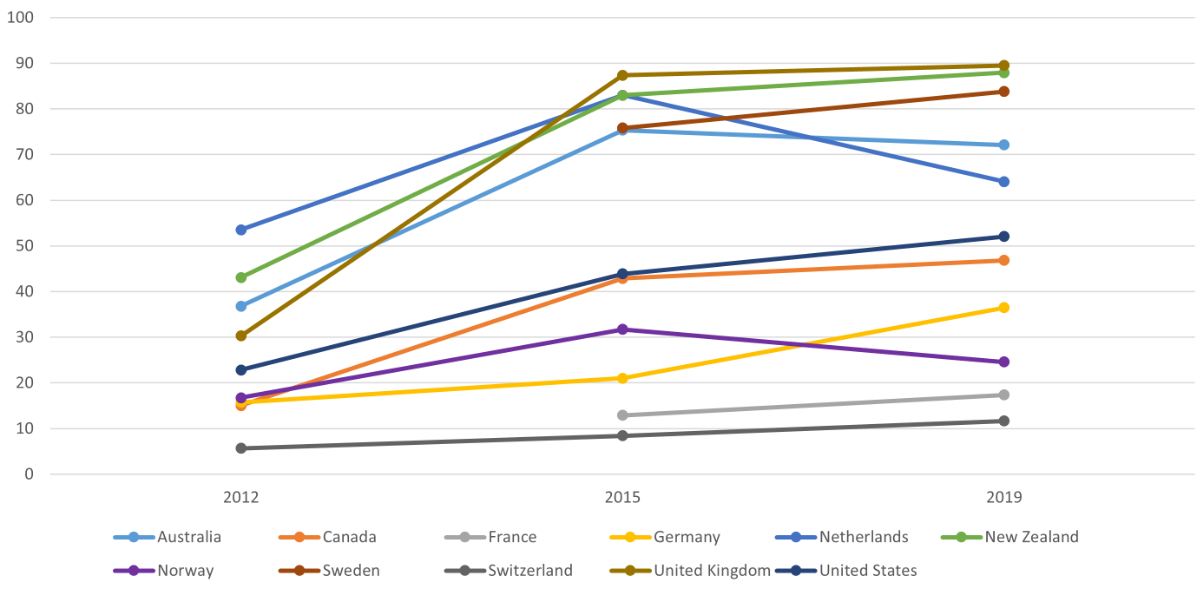
Figure 2Frequencies (in %) of case managers (“Yes, within the practice” and “Yes, both within and outside the practice”) between 2012 and 2019 in 11 Western countries, weighted data.
Regarding the frequency of use of case managers outside the practice (“Yes, use personnel outside the practice”), there was also considerable heterogeneity between the different countries. The frequency varied from 4.7% (Germany) to 62.4% (Switzerland) in 2012 to 4.7% (New Zealand) to 70.3% (France) in 2019, with a temporal trend towards a decrease in frequency. Finally, if we look at the respondents not using a case manager at all inside or outside the practice (“No”), there was also a decrease from 2012 to 2019. In 2019, a majority of respondents used case managers to manage the care of patients with chronic conditions in all countries (except Switzerland).
The multivariate analysis showed a higher frequency of use of case managers in practices located in small towns (odds ratio [OR] 1.4, 95% confidence interval [CI] 1.2–1.7) and in rural areas (OR 1.9, 95% CI 1.5–2.4) compared to the city. The frequency of case managers was higher in larger practices, as shown by comparing practices in the second, third and fourth quartile of FTE employee counts against those in the first quartile (Q2: OR 1.7, 95% CI 1.4–1.9; Q3: OR 2.1, 95% CI 1.6–2.9; Q4: OR 3.8, 95% CI 3.0–4.9). For these two factors (location and FTE), the same trend was found in the single independent variable analysis and in the multivariate analysis (table 2).
Table 2Associations between case managers, practice organisation and general practitioner characteristics; logistic regression (binary variable, 2019).
| Univariate analysis | Multivariate analysis | ||||||
| Characteristics | n | % | OR | 95% CI | OR | 95% CI | |
| Sex (ref: male) | 7054 | 54.06% | |||||
| Female | 5937 | 45.48% | 0.97 | 0.89–1.04 | 0.96 | 0.90–1.03 | |
| Age (ref: ≥65) | 1704 | 13.09% | |||||
| ≤35 | 1378 | 10.54% | 1.60 | 1.15–2.23 | 1.13 | 0.78–1.64 | |
| 35–44 | 2983 | 22.86% | 1.42 | 1.11–1.82 | 1.08 | 0.81–1.42 | |
| 45–54 | 3136 | 24.03% | 1.31 | 1.14–1.51 | 1.09 | 0.94–1.26 | |
| 55–64 | 3801 | 29.13% | 1.33 | 1.13–1.57 | 1.21 | 0.98–1.50 | |
| Location (ref: city) | 5592 | 43.18% | |||||
| Suburb | 2660 | 20.59% | 1.01 | 0.85–1.20 | 0.97 | 0.82–1.14 | |
| Small town | 2756 | 21.28% | 1.40 | 1.14–1.71 | 1.42 | 1.17–1.73 | |
| Rural | 1938 | 14.95% | 1.62 | 1.27–2.07 | 1.89 | 1.48–2.43 | |
| FTE (ref: Q1) | 2537 | 26.05% | |||||
| Q2 | 2393 | 24.59% | 1.67 | 1.45–1.93 | 1.65 | 1.43–1.90 | |
| Q3 | 2446 | 25.05% | 2.11 | 1.55–2.88 | 2.14 | 1.56–2.94 | |
| Q4 | 2371 | 24.31% | 3.69 | 2.88–4.73 | 3.82 | 2.97–4.91 | |
CI: confidence interval; FTE: full-time equivalent; OR: odds ratio; Qx: quartile x.
In the multivariate analysis, the frequency of case manager use did not vary significantly in general practitioners aged <35 years (OR 1.1, 95% CI 0.8–1.6), 35–44 years (OR 1.1, 95% CI 0.8–1.4), 45–54 years (OR 1.1, 95% CI 0.9–1.3) and 55–64 years (OR 1.2, 95% CI 1–1.5) compared to general practitioners aged ≥65 years. The frequency of case managers was not significantly different between female general practitioners (OR 1.0, 95% CI 0.9–1.0) compared to male general practitioners in the multivariate analysis (table 2).
There were large differences in the frequency of use of personnel such as case managers to care for patients with chronic conditions in general practitioner practices between the different countries. The temporal trend was upwards in almost all countries with a strong increase in frequency from 2012 to 2015 and then a stagnation or slight increase / decrease from 2015 to 2019. The temporal evolution between countries varied greatly, with stronger growth in use in some countries and slower growth in others, resulting in larger differences in frequency between countries over time. Some countries (Australia, Netherlands, New Zealand, Sweden, United Kingdom) already had a relatively widespread practice of case management in 2012 (>30% of “Yes”) and saw this frequency increase up to 2019. Other countries such as Switzerland and France had very limited use of such personnel and practices.
The frequency of use of case managers was associated with general practitioner practice characteristics, with a higher OR in rural areas and small town practices compared to practices located in cities and also a higher OR in practices with a higher full-time equivalent (OR Q4 > Q3 > Q2 compared to Q1). The independent variables related to general practitioner characteristics (age and sex) showed weaker associations with case manager use, with no sex or age differences.
Such differences in the use of case management in primary care can be explained by several factors. First of all, the structure of the health system and particularly primary care varies greatly from one country to another [27–29]. We might mention a first group of countries where general practitioners are the entry point to the health system, so-called “gatekeepers” that people are obliged to see in order to access a specialist. These systems, which can be found in Australia, Netherlands, New Zealand and the United Kingdom, are often considered to have strong primary care and seem to correspond to a higher frequency of case managers [27, 29–31]. It can be assumed that as a consequence of gatekeeping, the patient base may be larger, which increases the demands on health care and thus accelerates the need for a transition to more-integrated and multidisciplinary primary care, requiring new types of profiles such as case managers in medical practices. Moreover, in some countries, such new profiles (nurses, case managers) may even embody the gatekeeper function directly [30].
Another model is a more fragmented health system model with no or little gatekeeping, with very traditional primary care models and often based on the general practitioner and medical assistant pair or medical secretary [28, 32]. These countries, like Switzerland and Germany for example, have the lowest case manager frequencies [31, 33]. While these are perhaps the systems that would benefit most, the transition to an integrated care model (e.g. including case managers) is more difficult in more-fragmented care systems with little multidisciplinarity [34, 35]. It is also to be noted that these countries have the highest frequency of use of personnel outside the practice to monitor and manage care for patients with chronic conditions. The present questionnaire does not give us more information about this type of profile, which could correspond to home care nurses or health insurance case managers for example, and which would require further specific research. This use of out-of-practice personnel covers some of the functions assigned to case managers in other countries but illustrates the lack of flexibility and innovation to move away from the traditional model to build multiprofessional practice models incorporating new roles such as case managers [35].
Another possible explanation for the differences in the frequency of case management in primary care relates to health policy and public health. While the previous point on the historical organisation of care sheds light on the disparities in the frequency of use of case managers, this new factor allows us to look more closely at the differences in the temporal evolution. Indeed, countries with reforms and policies that encourage strong primary care workforce development such as Australia, the United Kingdom and the Netherlands are countries that use case management a lot [30, 36]. This is in line with the literature on the development of case management projects, which points to a need for strong guidelines from healthcare administrators and policymakers, in particular to clarify the roles of case managers [37]. This commitment on the part of health policy is country-specific and varies greatly. The temporal evolution of the use of case managers described in the results may partly reflect these differences, with some countries having used case managers within general practitioner practices for a longer period of time and with a sharp increase in frequency and subsequent stagnation once the practice is well established. In Australia, Norway and the Netherlands, there was even a drop between 2015 and 2019, which can be explained by an increase in case managers outside of practice, possibly reflecting the development of new professions or roles in these countries.
The trend towards stagnation or decline in frequency from 2015 to 2019 is less obvious in countries that use few case managers, with a more or less constant but small increase in frequency, which may also reflect public health policy decisions. Indeed, weak health policies or decentralised responsibilities can slow down the implementation of clear policies to strengthen primary care [30]. This is the case for example in Switzerland where public health does not have many direct links with (private) primary care which leads to a lack of communication and collaboration and favours the status quo of primary care models and may therefore slow down the development of initiatives such as the establishment of case managers [33]. This tendency towards inertia in the health system is even more pronounced in rich countries such as Switzerland, whose health system is not yet saturated and has therefore been able to persist despite its limitations and future needs for reform and innovation in primary care in particular [33].
In addition, several elements related to general practitioner practices and their structures can explain the differences in the use of case management. First of all, one can mention the funding of primary care which differs from country to country and which will have an impact on the payment of case managers and thus on the ease (or not) of implementation. Countries with a fee-for-service funding model have more difficulty paying nurses than doctors for the same services [26]. Those countries (Germany, Switzerland) will tend to have less use of case managers [26, 27]. In Switzerland, this difficulty has been underlined in the framework of case manager implementation projects because the primary care financing model is not adapted to this kind of practice [33]. Inversely, other mixed-financing models combining, for example, capitation and fee-for-service seem relevant and more likely to encourage the implementation of case managers [27, 33]. Furthermore, policies also have a role to play here, by providing specific funds to encourage coordinated and multidisciplinary primary care practice or by setting up specific funding systems to encourage case management practice, as is the case to some extent in Australia or New Zealand [26, 27].
Another element that can slow down the implementation of case management at the practice level in some places is the cultural aspect of the distribution of care. Indeed, professionals (especially general practitioners here) defend their turf and sometimes find it difficult to share or delegate certain tasks, which is necessary when working with a case manager [18, 34]. One can imagine that this kind of situation might be linked to a more general practitioner plus medical assistant-centred primary care system and to very liberal and still uncoordinated care systems like those in France or Switzerland [28].
Moreover, the specific characteristics of the practice (number of general practitioners, location, etc.) may also play a role. Again, these factors may reflect the healthcare system in which they operate. Group practices (several general practitioners working there) are places where team-based communication skills are needed, which is an important element in the integration of case managers and can therefore be an environment that favours the development of this type of practice [18]. The results of the present study are consistent with this principle as there were more case managers in group practices with more general practitioners. Location also seems to play a role in the implementation and use of case managers, with a tendency towards greater use of case managers in rural areas and small towns, which could be explained by the increased need in these areas for coordination and management of chronic patients who may not have as easy access to the different actors of the health system as they do in the city. In addition, the lower density of general practitioners in rural areas may encourage other healthcare professionals such as nurses to set up in these regions, to reinforce or even substitute the general practitioners’ functions [36, 37]. In contrast to practice characteristics, personal characteristics related to general practitioners such as sex and age do not seem to have much influence on the frequency of use of case managers, which may reflect the importance of the other factors discussed here (related to health structures and policies notably) in the implementation of primary care models incorporating case managers, compared to personal preferences or characteristics.
Finally, certain resources are necessary for the successful integration of case managers into primary care and these also vary greatly from one country to another. First of all, training needs to be put in place for good development of the practice. Countries where the use of case managers is still confidential, for example Switzerland, need to put in place adequate training to encourage practice and teach the new roles associated with case management [33]. Another resource element that can influence the implementation of this kind of practice is the availability of material adapted to the functions of case managers. This includes health technology tools such as electronic patient records, which can facilitate the implementation of case management and are key tools for coordinated follow-up [18, 33]. The availability and use of this technology varies greatly from country to country and may partly explain why case management is more easily integrated in some places [27].
This study has some limitations. The questionnaires were not answered in the same way in all countries (internet, email or telephone). Although the method is as similar as possible between countries, slight differences in methods are possible and have been described in the methodology reports [21, 22]. In addition, the structure of healthcare systems, and in particular primary care, varies greatly from one country to another, which can complicate comparisons between countries. Adjusting the multivariate analysis by country allows us, in some way, to partly take these variations into account. Response rates vary greatly between countries and were sometimes low [22, 24]. The data was self-reported and therefore possibly subject to reporting bias. Data for the case manager question was not available for France and Sweden in 2012. Moreover, we should point out that using the FTE variable to describe the size of the practice has its limitations because we do not know the exact number of doctors working in the practice but only the total % of work. Finally, it should be remembered that case management does not have a single definition and therefore does not necessarily represent exactly the same activities in each country [15, 24, 25]. The variability in terminology can lead to ambiguity in the role and complicate comparability in different contexts. The question concerning the case manager in the CWF survey does not allow us to differentiate between the professions performing this function (nurse practitioner, home care nurse, social worker, etc.), which would be an interesting topic to explore in future research.
There are also several strengths to this study. The sample size was large, with a significant number of respondents per country. In addition, it had a strong methodology that allowed for international and temporal comparison. Finally, the countries involved were all Western countries with high incomes and similar health needs, also allowing for comparison.
The present study has revealed great disparities in the use of case managers in primary care between the 11 countries surveyed. Case management seems to have become established in several countries, whereas it is struggling to establish itself in others. The frequency of use of case managers appears to be more associated with external factors such as the structure of the health system, the commitment of health policies, the functioning of primary care as well as historical and cultural aspects specific to each country rather than the personal characteristics and choices of the general practitioners. It would thus seem appropriate to build on these elements to set up practices that include case managers, for example by encouraging the implementation of case management projects through health policies, by specifying the roles and objectives of case managers, by defining the most appropriate profession to perform this function, by developing appropriate means of payment to remunerate case managers, by providing more training in collaboration and information sharing and by making available appropriate resources such as health information technology tools that allow for adequate case management practice.
It would be relevant to further study the structural elements facilitating the implementation of case managers, in order to provide clear guidelines to health policies that would allow for a simpler implementation, especially in countries that still make little use of this kind of model despite its benefits and despite the ever-increasing needs for primary care reform.
We would like to thank the Swiss Federal Office of Public Health for making the data available at no cost, and the Commonwealth Fund for collecting and sharing the data, also free of charge.
The data comes from the Commonwealth Fund International Health Policy Survey and has been made available free of charge to all participating countries. We obtained the data for free from the Swiss Federal Office of Public Health. The funding of the present study was supported by Unisanté (Lausanne, Switzerland).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest related to the content of this manuscript was disclosed.
1. Tran HT, Leonard SD. Geriatric Assessment for Primary Care Providers. Prim Care. 2017 Sep;44(3):399–411. 10.1016/j.pop.2017.05.001
2. Ageing [Internet]. [cited 2023 Jan 12]. Available from: https://www.who.int/health-topics/ageing
3. Hassenteufel P, Naiditch M, Schweyer FX. Les réformes de l’organisation des soins primaires : perspectives multi-situées. Avant-propos. Rev Fr Aff Soc. 2020;(1):11–31. 10.3917/rfas.201.0011
4. Bourgueil Y, Ramond-Roquin A, Schweyer FX. 1. Qu’appelle-t-on « soins primaires »? In: Les soins primaires en question(s) [Internet]. Rennes: Presses de l’EHESP; 2021 [cited 2022 Nov 7]. p. 5–13. (Débats Santé Social). Available from: https://www.cairn.info/les-soins-primaires-en-question--9782810908820-p-5.htm
5. Sangaleti C, Schveitzer MC, Peduzzi M, Zoboli EL, Soares CB. Experiences and shared meaning of teamwork and interprofessional collaboration among health care professionals in primary health care settings: a systematic review. JBI Database Syst Rev Implement Reports. 2017 Nov;15(11):2723–88. 10.11124/JBISRIR-2016-003016
6. Morgan S, Pullon S, McKinlay E. Observation of interprofessional collaborative practice in primary care teams: an integrative literature review. Int J Nurs Stud. 2015 Jul;52(7):1217–30. 10.1016/j.ijnurstu.2015.03.008
7. Rawlinson C, Carron T, Cohidon C, Arditi C, Hong QN, Pluye P, et al. An Overview of Reviews on Interprofessional Collaboration in Primary Care: barriers and Facilitators. Int J Integr Care. 2021 Jun;21(2):32. 10.5334/ijic.5589
8. Askerud A, Conder J, Askerud A, Conder J. Patients’ experiences of nurse case management in primary care: a meta-synthesis. Aust J Prim Health. 2017 Oct;23(5):420–8. 10.1071/PY17040
9. Davy C, Bleasel J, Liu H, Tchan M, Ponniah S, Brown A. Effectiveness of chronic care models: opportunities for improving healthcare practice and health outcomes: a systematic review. BMC Health Serv Res. 2015 May;15(1):194. 10.1186/s12913-015-0854-8
10. Tello J, Barbazza E, Yelgezekova Z, Kruse I, Klazinga N, Kringos D. Glossary of Terms : WHO European Primary Health Care Impact Performance and Capacity Tool (PHC-IMPACT). In 2019 [cited 2023 Jan 12]. Available from: https://www.semanticscholar.org/paper/Glossary-of-Terms-%3A-WHO-European-Primary-Health-and-Tello-Barbazza/ae5467b291d3319a2ac532df2e825b0dc341d050#citing-papers
11. Hudon C, Chouinard MC, Pluye P, El Sherif R, Bush PL, Rihoux B, et al. Characteristics of Case Management in Primary Care Associated With Positive Outcomes for Frequent Users of Health Care: A Systematic Review. Ann Fam Med. 2019 Sep;17(5):448–58. 10.1370/afm.2419
12. What Is A. Case Manager | Case Management Society of America [Internet]. [cited 2023 Jan 12]. Available from: https://cmsa.org/who-we-are/what-is-a-case-manager/
13. Ross S, Curry N, Goodwin N. Case Management: What It Is and How It Can Best Be Implemented. King’s Fund; 2011. 32 pp.
14. Barceló A, Luciani S, Agurto I, Ordunez P, Tasca R, Sued O. Improving Chronic Illness Care through Integrated Health Service Delivery Networks. Pan Am Health Organ Wash DC. 2012 Jan 1;
15. Russell M, Roe B, Beech R, Russell W. Service developments for managing people with long-term conditions using case management approaches, an example from the UK. Int J Integr Care. 2009;9(1):e02. 10.5334/ijic.303
16. Hudon C, Chouinard MC, Aubrey-Bassler K, Muhajarine N, Burge F, Bush PL, et al. Case Management in Primary Care for Frequent Users of Health Care Services: A Realist Synthesis. Ann Fam Med. 2020 May;18(3):218–26. 10.1370/afm.2499
17. Malebranche M, Grazioli VS, Kasztura M, Hudon C, Bodenmann P. Case management for frequent emergency department users: no longer a question of if but when, where and how. CJEM. 2021 Jan;23(1):12–4. 10.1007/s43678-020-00024-4
18. Teper MH, Vedel I, Yang XQ, Margo-Dermer E, Hudon C. Understanding Barriers to and Facilitators of Case Management in Primary Care: A Systematic Review and Thematic Synthesis. Ann Fam Med. 2020 Jul;18(4):355–63. 10.1370/afm.2555
19. Ferguson JA, Weinberger M. Case management programs in primary care. J Gen Intern Med. 1998 Feb;13(2):123–6. 10.1046/j.1525-1497.1998.00029.x
20. Cohidon C, Wild P, Senn N. Job stress among GPs: associations with practice organisation in 11 high-income countries. Br J Gen Pract. 2020 Aug;70(698):e657–67. 10.3399/bjgp20X710909
21. Doty MM, Tikkanen R, Shah A, Schneider EC. Primary Care Physicians’ Role In Coordinating Medical And Health-Related Social Needs In Eleven Countries. Health Aff (Millwood). 2020 Jan;39(1):115–23. 10.1377/hlthaff.2019.01088
22. Rapoport R, Czyzewicz E, Manley R. 2019 International Health Policy Survey of Primary Care Doctors. Methodology Report. 2019 [cited 2023 Jan 4]; Available from: https://www.bag.admin.ch/dam/bag/en/dokumente/e-f/forschung/ihp-befragungen-cwf/aerztinnen-und-aerzte-in-der-grundversorgung/2019-methodenbericht-ihpbefragung.pdf.download.pdf/ihp-befragung-2019-methodology-report.pdf
23. Pierson R, Applebaum S. International Health Perspectives 2012: A Survey of Physicians in Eleven Countries. 2012;
24. Rapoport R, Tipan L, Czyzewicz E. 2015 International Health Policy Survey of Primary Care Doctors. Methodology Report. 2015 [cited 2023 Jan 4]; Available from: https://www.bag.admin.ch/dam/bag/de/dokumente/e-f/forschung/ihp-befragungen-cwf/aerztinnen-und-aerzte-in-der-grundversorgung/2015-methodenbericht-ihpbefragung.pdf.download.pdf/2015-ihp-method-report-e.pdf
25. Schoen C, Osborn R, Squires D, Doty M, Rasmussen P, Pierson R, et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff (Millwood). 2012 Dec;31(12):2805–16. 10.1377/hlthaff.2012.0884
26. Osborn R, Moulds D, Schneider EC, Doty MM, Squires D, Sarnak DO. Primary Care Physicians In Ten Countries Report Challenges Caring For Patients With Complex Health Needs. Health Aff (Millwood). 2015 Dec;34(12):2104–12. 10.1377/hlthaff.2015.1018
27. Tikkanen R, Osborn R, Mossialos E, Djordjevic A, Wharton G. International Profiles of Health Care Systems 2020. 2020.
28. Bourgueil Y, Ramond-Roquin A, Schweyer FX. Les soins primaires en question(s). Rennes: Presses de l’EHESP; 2021. 120 p. (Débats Santé Social).
29. Kringos DS, Boerma WG, Hutchinson A, Saltman RB. Building primary care in a changing Europe [Internet]. World Health Organization. Regional Office for Europe; 2015 [cited 2022 Oct 14]. Available from: https://apps.who.int/iris/handle/10665/154350
30. Kringos D, Boerma W, Bourgueil Y, Cartier T, Dedeu T, Hasvold T, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013 Nov;63(616):e742–50. 10.3399/bjgp13X674422
31. van Loenen T, van den Berg MJ, Heinemann S, Baker R, Faber MJ, Westert GP. Trends towards stronger primary care in three western European countries; 2006-2012. BMC Fam Pract. 2016 May;17(1):59. 10.1186/s12875-016-0458-3
32. Jabbarpour Y, Jetty A, Dai M, Magill M, Bazemore A. The Evolving Family Medicine Team. J Am Board Fam Med. 2020;33(4):499–501. 10.3122/jabfm.2020.04.190397
33. Schütz Leuthold M, El-Hakmaoui F, Senn N, Cohidon C. General Practitioner’s Experience of Public-Private Partnerships to Develop Team-Based Care: A Qualitative Study. Int J Public Health. 2023 Nov;68:1606453. 10.3389/ijph.2023.1606453
34. Delnoij D, Klazinga N, Glasgow IK. Integrated care in an international perspective [Internet]. Int J Integr Care. 2002;2(2):e04. [cited 2022 Oct 14] Available from: http://www.ijic.org/articles/10.5334/ijic.62/
35. Cachou De Camaret A, Wild P, Senn N, Cohidon C. The professional composition of general practices in Western countries and associations with their perceived ability to manage patients with chronic conditions. Fam Pract. Forthcoming.
36. Pavlič DR, Sever M, Klemenc-Ketiš Z, Švab I, Vainieri M, Seghieri C, et al. Strength of primary care service delivery: a comparative study of European countries, Australia, New Zealand, and Canada. Prim Health Care Res Dev. 2018 May;19(3):277–87. 10.1017/S1463423617000792
37. Joo JY, Huber DL. Barriers in Case Managers’ Roles: A Qualitative Systematic Review. West J Nurs Res. 2018 Oct;40(10):1522–42. 10.1177/0193945917728689