Physician wellbeing and burnout in emergency medicine
in Switzerland
DOI: https://doi.org/https://doi.org/10.57187/s.3421
Eric P. Heymannabc,
Valerie Romannad,
Rod Limef,
Kristine Van Aarsenf,
Nour Khatibeg,
Thomas C. Sauterach,
Barbara Schildai,
Stefan M. Muellerajk
a Swiss Society of Emergency and Rescue Medicine,
Switzerland
b Department of Emergency Medicine,
Cantonal Hospital of Neuchâtel, Neuchâtel, Switzerland
c Department of Emergency Medicine, Faculty of Medicine, University of Bern, Switzerland
d Department of Emergency Medicine, Tiefenau
Hospital, Bern, Switzerland
e Canadian Association of Emergency
Physicians, Canada
f Department of Paediatric Emergency
Medicine, London Health Sciences Centre, Ontario, Canada
g University of Toronto, Faculty of
Medicine, Toronto, Canada
h Department of Emergency Medicine, Bern
University Hospital, Bern, Switzerland
i Croce verde Bellinzona e di Tre Valli, Bellinzona,
Switzerland
j Department of Anaesthesiology,
Stadtspital, Zurich, Switzerland
k Schutz
& Rettung Zürich, Zürich
Summary
Emergency physicians are the most at-risk medical
specialist group for burnout. Given its consequences for patient care and
physician health and its resulting increased attrition rates, ensuring the
wellbeing of emergency physicians is vital for preserving the integrity of the
safety net for the healthcare system that is emergency medicine. In an effort to
understand the current state of practicing physicians, this study reviews the results
of the first national e-survey on physician wellbeing and burnout in emergency medicine
in Switzerland. Addressed to all emergency physicians between March and April
2023, it received 611 complete responses. More than half of respondents met at least
one criterion for burnout according to the Maslach Burnout Inventory – Human
Services Survey (59.2%) and the Copenhagen Burnout Inventory (54.1%). In
addition, more than half reported symptoms suggestive of mild to severe
depression, with close to 20% screening positively for moderate to severe
depression, nearly 4 times the incidence in the general population, according
to the Patient Health Questionnaire-9. We found that 10.8% of respondents
reported having considered suicide at some point in their career, with nearly
half having considered this in the previous 12 months. The resulting high
attrition rates (40.6% of respondents had considered leaving emergency medicine
because of their working conditions) call into question the sustainability of
the system. Coinciding with trends observed in other international studies on
burnout in emergency medicine, this study reinforces the fact that certain
factors associated with wellbeing are intrinsic to emergency medicine working
conditions.
Introduction
Burnout is defined as an occupational phenomenon
resulting from chronic workplace stress [1]. It is characterised by three dimensions:
an emotional component (feeling of energy depletion or exhaustion), a
depersonalisation component (increased mental distance from one’s job or
feelings of negativism or cynicism related to one’s job) and a personal
accomplishment component (reduced professional efficacy) [2]. Burnout is not a disease
but rather a state, and it is a
risk factor for the development of mental and physical illnesses, such as
depression, hypertension, multiple sclerosis and cancer [3].
Among healthcare professionals, emergency
physicians are the most at-risk specialist group for burnout, with consequences
not only for physician health but also for patient care and the rest of the
healthcare system [4, 5]. Burnout is associated with reduced quality of care,
decreased patient satisfaction and increased medical complication and error
rates, and it leads to reduced productivity, higher staff turnout and attrition, increased
costs and
the eventual closure of emergency departments [6, 7]. In certain countries, up
to 87.9% of emergency physicians are burnt out [8–10].
Clinically, burnout can manifest with a
variety of symptoms, such as irritability, anxiety, insomnia, lack of
concentration and dissatisfaction. It is often recognised at a late stage, when
it has been translated into loss of interest, behavioural problems, reluctance
to accept new obligations or postponement of current obligations, and general
distancing of oneself from the job [11, 12]. If not addressed, burnout can lead
to depression and alcohol and drug abuse [13], which can culminate in suicide, which
is not uncommon among emergency physicians [14]. Often, as a means of escape
from this vicious cycle, emergency physicians choose to leave the profession,
which worsens the situation for remaining physicians [15].
Switzerland has seen an increase in the incidence
of burnout in recent decades across all fields of medicine [16]. The recent
COVID crisis, as well as the post-pandemic increase in patient flow, has led to
an increase in work-related exhaustion [17–20]. No study has yet quantified the
situation in Swiss emergency departments, but with a system currently in
crisis, and calls for reform from both the Swiss Society of Emergency and
Rescue Medicine (SGNOR/SSMUS/SSERM) and emergency physicians throughout the
country, there is a need to understand how wellbeing can be improved to ensure
the preservation of the safety net for the Swiss population that is emergency
medicine.
The following study aimed to review the
current state of wellbeing of emergency physicians in Switzerland and to
identify factors influencing this wellbeing.
Methodology
Survey design
We designed a survey-type observational
study. Eligible study participants were physicians currently practicing in a
Swiss emergency department, regardless of training or experience. The survey,
which was sent to all 1300 members of the SSERM, was translated into German,
French, Italian and English and was also disseminated to non-SSERM members via
a modified snowball recruitment method (as SSERM membership is not mandatory to
practice emergency medicine in Switzerland). To enable this secondary
recruitment method, an explanatory email containing a link to the survey was
sent to the heads of all 104 hospital-based emergency departments in
Switzerland and was intended to be forwarded to residents and staff currently working
in their emergency departments.
The survey was divided into four parts. The
first section consisted of socio-demographic questions. The second section included
Likert scale questions pertaining to the Maslach Burnout Inventory – Health
Services Survey (MBI-HSS) and the Copenhagen Burnout Inventory (CBI), two externally
validated instruments used to measure burnout [21]. The MBI-HSS is the most
widely used scale to measure burnout among human services workers; in the form
of a standardised 22-point questionnaire, it aims to assess three aspects of
burnout: depersonalisation, emotional exhaustion and personal accomplishment.
The Copenhagen Burnout Inventory (CBI) is another commonly used assessment tool;
in the form of a 19-point questionnaire, it also assesses three aspects of burnout:
personal (P-CBI), work-related (WR-CBI) and client-related (CR-CBI – i.e.
patient-related). In addition to the Maslach Burnout Inventory-Health Services
Survey (MBI-HSS) and CBI, the second section of the survey also included Likert
scale questions covering the Patient Health Questionnaire (PHQ-9) to screen for
depression [22]. A third section contained closed questions on career
resilience and on suicidality. Finally, a fourth section focused on the
personal experience of each physician, in the form of free-text questions giving the
opportunity for respondents to express individualised concerns. This
final section was the subject of a secondary analysis, which will not be
covered in detail in this paper.
The survey was open for a duration of 4
weeks, between March 23rd and April 23rd, 2023, with a
reminder email sent out 2 weeks after the survey became available. The link to
the e-survey was distributed by email, and data were collected on the Mind Garden©
platform. All responses were kept anonymous, and incomplete surveys were
excluded. No financial incentives were offered for responses.
The study protocol was approved by the Swiss Society
of Emergency and Rescue Medicine and the Swiss Ethics Committee (BASEC
2022-01519).
Outcomes
The primary outcome measured was the
incidence of burnout among emergency medicine physicians using two scores: the MBI
(cut-offs: depersonalisation ≥10, emotional exhaustion ≥27, personal
accomplishment <34) and CBI (cut-offs: P-CBI, WR-CBI and CR-CBI: ≥50). In addition,
we investigated the incidence of depression (using the PHQ-9),
suicidality and career resilience. As a secondary outcome, we examined whether
age, gender, primary language at work, employment percentage (i.e. part-time),
working hours, number of night shifts, post-graduate experience, specialty,
relationship status and having children had any influence on the incidence of burnout.
Statistical analysis
Burnout scores for the MBI and CBI were calculated according to the
appropriate questionnaire manuals [23, 24]. Standard descriptive statistics
were calculated for demographics. Relationships between meeting the threshold
for burnout on the MBI and CBI and potential risk factors were assessed using
binary logistic regression. As an initial step for the purposeful selection of
model variables, univariate analysis of each potential risk factor versus
meeting the threshold for burnout on any domain on the MBI was analysed. This
was repeated for the outcome of meeting the threshold for burnout on any domain
of the CBI. Variables found to be associated (p-value <0.1) with burnout were
included as predictors in the initial multivariable model to determine which
factors were independently associated with burnout. Backwards stepwise
multivariable logistic regression (Wald removal criterion of 0.1) was used to
determine the predictor variables independently associated with burnout.
Likelihood ratio tests were used to determine the appropriateness of including variables
in the multivariable model. Nagelkerke R2 was used to
determine the variance in burnout explained by the final model. This test was
chosen because it is modified to have a maximum value of 1 which, although it
has limitations, provides greater ease of interpretation than other methods.
All data analyses were performed in SPSS
version 29 (IBM Corp., IBM SPSS Statistics for Windows, Version 29.0. Armonk,
NY: IBM Corp).
Results
Of the 685 completed surveys, 74 were
missing data and thus excluded; 611 responses were therefore included in our analysis.
The majority of respondents were male (321/611, 52.5%), with a median age of 40
years (IQR 32.0–49.0). A substantial proportion
of respondents were married (295/611, 48.3%) with children (324/611, 53%), and the
median duration of practice was 12 years post-graduation (IQR 5.0–21.0).
Socio-demographic variables
Table 1 summarises the socio-demographic
variables identified by our survey.
Table 1Socio-demographic variables.
| Variable |
Results |
| Age |
Median [IQR] |
40.00 [32.0–49.0] |
| Range |
24.0–76.0 |
| Gender, n (%) |
Male |
321 (52.5%) |
| Female |
290 (47.5%) |
| Non-binary |
0 (0%) |
| Relationship status, n (%) |
Single |
121 (19.8%) |
| In a stable relationship |
159 (26.0%) |
| Married |
295 (48.3%) |
| Divorced |
28 (4.6%) |
| Widowed |
2 (0.3%) |
| Other |
6 (1.0%) |
| Partner working as a healthcare
professional, n (%) |
Yes |
256 (41.9%) |
| No |
280 (45.8%) |
| Not applicable |
75 (12.3%) |
| Children, n (%) |
Yes |
324 (53.0%) |
| No |
287 (47.0%) |
| If children, how many |
Median [IQR] |
1.0 [0.0–2.0] |
| Range |
0.0–5.0 |
| If children, age of youngest |
Median [IQR] |
7.0 [2.0–15.0] |
| Range |
0.0–39.0 |
| Primary language at work, n (%) |
French |
218 (35.7%) |
| German |
318 (52.0%) |
| Italian |
75 (12.3%) |
| Other |
0 (0.0%) |
| Employment in % |
Mean (SD) |
86.63% (19.30%) |
| Median [IQR] |
100% [80.0–100%] |
| Range |
0–100% |
| Average hours worked per week |
Mean (SD) |
47.34 (12.08) |
| Median [IQR] |
50.00 [40.0–55.0] |
| Range |
0–100 |
| Average number of night shifts per month
in person (at the hospital) |
Mean (SD) |
3.62 (3.15) |
| Median [IQR] |
4.00 [1.0–5.0] |
| Range |
0.0–25.0 |
| Number of years worked since graduating from
medical school |
Mean (SD) |
13.90 (10.15) |
| Median [IQR] |
12.00 [5.0–21.0] |
| Range |
0–47 |
| Specialty (in training or finished), n
(%) |
Surgery |
39 (6.4%) |
| Anaesthesiology |
175 (28.6%) |
| Internal medicine |
355 (58.1%) |
| Other |
42 (6.9%) |
| Emergency Medicine SSERM / SGNOR / SSMUS, n (%)* |
None |
209 (34.2%) |
| ISP KNM / FAI MUH |
173 (28.3%) |
| FA PKNM / AFC MUP |
141 (23.1%) |
| ISP KNM + FA PKNM / FAI MUH + AFC MUP |
88 (14.4%) |
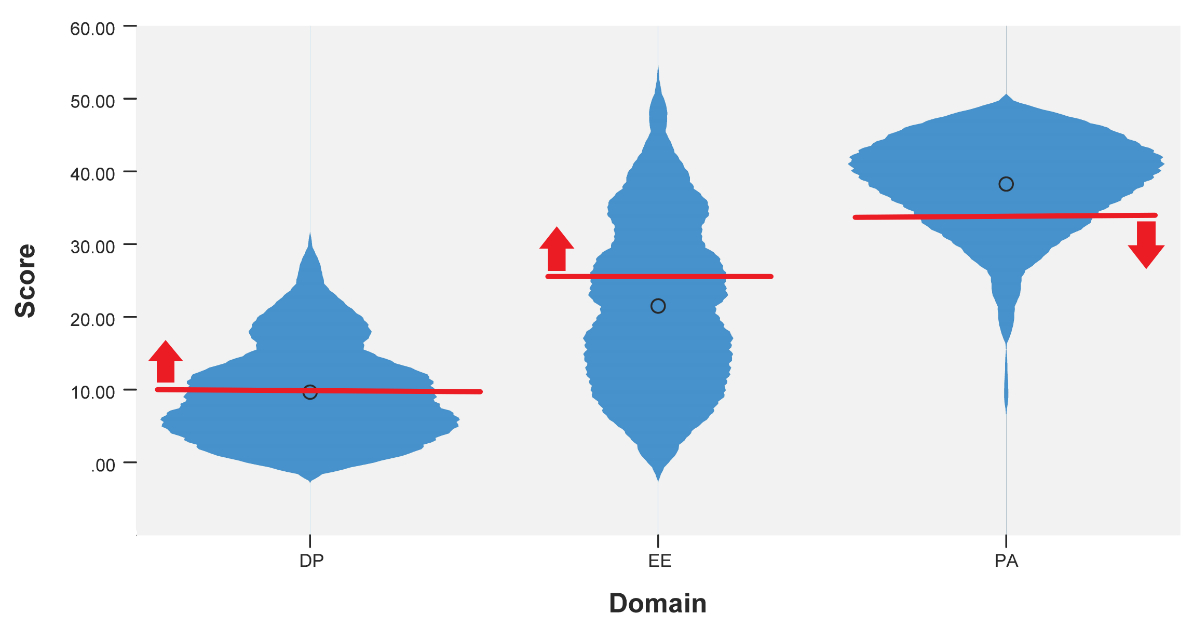
Maslach Burnout Inventory
Of all participants, 362/611 (59.2%) met at
least one of the criteria for burnout according to the Maslach Burnout
Inventory (MBI) 279/611 (45.7%) met the depersonalisation cut-off of ≥10
(median score 9.0 [IQR 5.0–13.0]), 208/611 (34.0%) met the emotional exhaustion
cut-off of ≥27 (median score 21.0 [IQR 13.0–30.0]) and 128/611 (20.9%) met the personal
accomplishment cut-off of <34 (median [IQR] score 39.0 [9.0–48.0]). Figure 1 illustrates
the percentage of participants
meeting each criterion (of the 362 meeting at least one criterion) and figure 2 illustrates
the percentage of participants the MBI burnout criteria, according to each dimension.
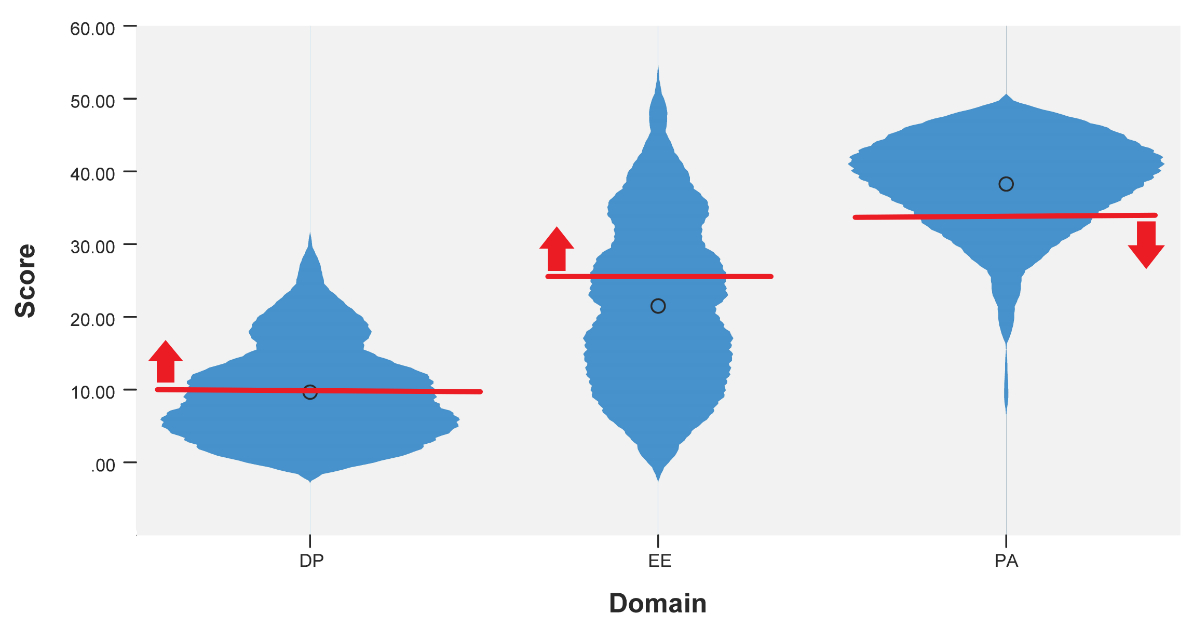
Figure 1Violin plot. Total score by domain of the Maslach
Burnout Inventory (0 = mean score). Red lines indicate the cut-offs for each Maslach
Burnout Inventory domain, with the red arrows indicating those above each
threshold. Black circles indicate median scores.

Figure 2Percentage of participants (n = 362) meeting
the Maslach Burnout Inventory burnout criteria, according to each dimension.
The initial model-building univariate
analyses removed gender and average working hours per week from the model. The
multivariable logistic regression model was run with the remaining predictors,
and the final model correctly classified 68.2% of cases and explained 23.8% of
the variance in burnout. The final multivariable logistic regression model
showed that each additional 1 year increase in age was associated with a 3.5%
decrease in the odds of meeting any MBI burnout threshold, and for each one-unit
increase in the number of in-person night shifts per month a physician was
1.109 times more likely to meet an MBI criterion for burnout. Compared to
physicians who had children, those without children were almost twice as likely
to suffer from burnout (95% CI 1.09–2.76).
Table 2Regression analysis. Outcome was
meeting burnout criteria for any domain of the Maslach Burnout Inventory.
|
Univariate |
Multivariable* |
| Variable |
Odds ratio |
95% confidence interval |
p-value |
Odds ratio |
95% confidence interval |
p-value |
| Age |
0.93 |
0.92–0.95 |
<0.001 |
0.965 |
0.944–0.986 |
0.001 |
| Gender |
Male |
Reference |
|
|
|
| Female |
1.18 |
0.86–1.63 |
0.31 |
| Primary language at work |
French |
reference |
|
|
|
| German |
0.52 |
0.37–0.75 |
<0.001 |
| Italian |
0.66 |
0.38–1.13 |
0.128 |
| Employment in % |
1.01 |
1.00–1.02 |
0.02 |
|
| Average working hours per week |
1.00 |
0.987–1.01 |
0.93 |
|
| Average number of in-person night shifts
per month |
1.18 |
1.11–1.26 |
<0.001 |
1.109 |
1.041–1.180 |
0.001 |
| Number of years worked since graduating from
medical school |
0.93 |
0.92–0.95 |
<0.001 |
|
|
|
| Specialty (in training or finished) |
Surgery |
Reference |
|
|
Reference |
|
|
| Anaesthesiology |
0.44 |
0.21–0.90 |
0.02 |
0.494 |
0.221–1.104 |
0.086 |
| Internal medicine |
1.00 |
0.50–2.00 |
0.99 |
0.928 |
0.429–2.009 |
0.850 |
| Other |
1.79 |
0.68–4.71 |
0.24 |
1.578 |
0.548–4.543 |
0.398 |
| Emergency Medicine SSERM / SGNOR / SSMUS** |
None |
Reference |
|
|
|
|
|
| ISP KNM / FAI MUH |
0.62 |
0.41–0.95 |
0.03 |
|
|
|
| FA PKNM / AFC MUP |
0.37 |
0.24–0.58 |
<0.001 |
|
|
|
| ISP KNM + FA PKNM / FAI MUH + AFC MUP |
0.54 |
0.32–0.91 |
0.02 |
|
|
|
| Relationship status |
Single |
Reference |
|
|
Reference |
|
|
| In a stable relationship |
0.75 |
0.43–1.30 |
0.31 |
1.007 |
0.556–1.825 |
0.982 |
| Married |
0.23 |
0.14–0.38 |
<0.001 |
0.590 |
0.323–1.079 |
0.087 |
| Divorced |
0.33 |
0.14–0.78 |
0.01 |
1.086 |
0.410–2.875 |
0.868 |
| Widowed/other |
0.86 |
0.16–4.52 |
0.86 |
1.866 |
0.323–10.773 |
0.485 |
| Partner working as a healthcare
professional |
Yes |
Reference |
|
|
|
|
|
| No |
1.30 |
0.92–1.83 |
0.13 |
|
|
|
| Not applicable |
2.35 |
1.33–4.15 |
0.003 |
|
|
|
| Children |
Yes |
Reference |
|
|
Reference |
|
|
| No |
3.71 |
2.62–5.24 |
<0.001 |
1.731 |
1.087–2.758 |
0.021 |
Copenhagen Burnout Inventory
Of all participants, 333/611 (54.5%) met at
least one criterion for burnout according to the Copenhagen Burnout Inventory (CBI)
286/611 (46.8%) met the P-CBI cut-off of ≥50 (median score 45.80 [IQR 33.50–58.30]),
254/611 (41.6%) met the WR-CBI cut-off of ≥50 (median score 42.90 [IQR 28.60–57.10])
and 132/611 (21.6.%) met the CR-CBI cut-off of ≥50 (median score 29.20 [IQR 12.50–45.80]).
Furthermore, 102/611 (16.7%) met the criteria for all three domains (Personal, Work-Related
and Client-Related).
The initial model-building univariate
analyses removed average working hours per week and partner working as a
healthcare professional from the model. The multivariable logistic regression
model was run with the remaining predictors, and the final model correctly classified
65.0% of cases and explained 13.1% of the variance in burnout. The final
multivariable logistic regression model showed that each additional one-year
increase in age was associated with a 3.8% decrease in the odds of meeting any CBI
burnout threshold, and for each one-unit increase in the number of in-person
night shifts per month a physician was 1.098 times more likely to meet a CBI
criterion for burnout. Compared to physicians without a SSERM specialty, those
with an interdisciplinary sub-specialty in hospital emergency medicine (ISP KNM /
FAI MUH) were 1.714 times more likely to suffer from
burnout (95% CI 1.050–2.797).
Table 3Regression analysis. Outcome was
meeting burnout criteria for any domain of the Copenhagen Burnout Inventory.
|
Univariate |
Multivariable* |
| Variable |
Odds ratio |
95% confidence interval |
p-value |
Odds ratio |
95% confidence interval |
p-value |
| Age |
0.952 |
0.937–0.967 |
<0.001 |
0.962 |
0.941–0.983 |
<0.001 |
| Gender |
Male |
Reference |
|
|
Reference |
|
|
| Female |
1.70 |
1.23–2.35 |
0.001 |
1.357 |
0.956–1.926 |
0.088 |
| Primary language at work |
French |
Reference |
|
|
|
| German |
0.647 |
0.456–0.918 |
0.015 |
| Italian |
0.730 |
0.430–1.240 |
0.244 |
| Employment in % |
1.008 |
0.999–1.016 |
0.067 |
|
| Average working hours per week |
1.004 |
0.991–1.018 |
0.515 |
|
| Average number of in-person night shifts
per month |
1.144 |
1.076–1.215 |
<0.001 |
1.098 |
1.035–1.165 |
0.002 |
| Number of years worked since graduating from
medical school |
0.950 |
0.935–0.967 |
<0.001 |
|
| Specialty (in training or finished) |
Surgery |
Reference |
|
|
|
| Anaesthesiology |
0.547 |
0.270–1.106 |
0.093 |
| Internal medicine |
0.996 |
0.508–1.950 |
0.990 |
| Other |
0.928 |
0.383–2.244 |
0.867 |
| Emergency Medicine SSERM / SGNOR / SSMUS** |
None |
Reference |
|
|
Reference |
|
|
| ISP KNM / FAI MUH |
0.858 |
0.570–1.290 |
0.461 |
1.714 |
1.050–2.797 |
0.031 |
| FA PKNM / AFC MUP |
0.543 |
0.352–0.836 |
0.006 |
1.018 |
0.620–1.672 |
0.942 |
| ISP KNM + FA PKNM / FAI MUH + AFC MUP |
0.806 |
0.488–1.333 |
0.401 |
1.651 |
0.919–2.967 |
0.093 |
| Relationship status |
Single |
Reference |
|
|
|
| In a stable relationship |
1.210 |
0.735–1.991 |
0.453 |
| Married |
0.456 |
0.295–0.706 |
<0.001 |
| Divorced |
0.495 |
0.216–1.136 |
0.097 |
| Widowed/other |
0.571 |
0.136–2.399 |
0.445 |
| Partner working as a healthcare
professional |
Yes |
Reference |
|
|
|
| No |
1.182 |
0.841–1.661 |
0.336 |
| Not applicable |
1.409 |
0.835–2.377 |
0.199 |
| Children |
Yes |
Reference |
|
|
Reference |
|
0.069 |
| No |
2.28 |
1.644–3.161 |
<0.001 |
1.456 |
0.971–2.184 |
|
Patient Health Questionnaire-9
The median score for the PHQ-9 was 5.00
(IQR 0.0–25.0), with a cut-off of ≤4 indicating minimal depression (and no
recommended treatment) [22, 25]. Of all participants, 331/611 (54.2%)
physicians met the criteria for mild to severe depression, with 220/611 (36.0%)
meeting the criteria for mild depression, 77/611 (12.6%) for moderate depression,
27/611 (4.4%) for moderately severe depression and 7/611 (1.1%) for severe
depression.
Consideration of a career change
A total of 432/611 (70.7%) of respondents
had considered leaving emergency medicine as a result of their working
conditions. Of all participants, 26/611 (4.3%) had considered this once every
shift, 44/611 (7.2%) more than once a shift, 42/611 (6.9%) once a week, 43/611
(7.0%) more than once a month, 93/611 (15.2%) once a month, 60/611 (9.8%) more
than once a year, 77/611 (12.6%) once a year and 47/611 (7.7%) at least once in
their career. In contrast, 179/611 physicians (29.3%) had never considered
leaving their profession.
Consideration of suicide
A total of 66/611 respondents (10.8%) had
considered suicide at some point in their career; of these, 34/611 (5.6%) had
considered this in the previous 12 months.
Discussion
While often accepted as multifactorial,
with the intertwining of personal and professional issues, burnout is an
occupational phenomenon resulting from chronic workplace stress [1]. Our study demonstrates
the repercussions that current working conditions have on physician wellbeing
in emergency departments in Switzerland.
In our survey, 59.2% of respondents met at
least one criterion for burnout according to the MBI-Health Services Survey, and
54.1% met at least one burnout criterion using the CBI. In addition, more than
half exhibited symptoms of mild to severe depression, and close to 20% screened
positive for moderate to severe depression, nearly 4 times the incidence in the
general population [26]. More worryingly, our study also illustrates the ultimate
consequences of these difficult working conditions, with 10.8% of respondents reporting
having considered suicide at some point during their career as an emergency
physician and nearly half having contemplated this in the 12 months prior to
our study. In a profession reluctant to seek help for depression [27, 28] where
suicide is not uncommon [14, 29–32], attention needs to be focused on prevention
by resolving issues that negatively influence wellbeing.
Our findings are comparable to those of
other international studies of burnout in emergency physicians [5, 19]. While certain
issues may be specific to individuals and/or individual countries, the
similarities among studies suggest that there are common issues shared by all emergency
physicians throughout the world and that certain characteristics associated
with burnout are inherent to emergency medicine.
Night shifts, commonly accepted as part of
the responsibilities of an emergency physician, are strenuous and harmful to
their wellbeing [5]. In our study, 36% of respondents reported working ≥5
nights a month. Burnout was also cited as one of the top 10 factors influencing
wellbeing in the free-text portion of our survey, and it increased
significantly with the frequency of night shifts (MBI: OR 1.18, p <0.001; CBI:
OR 1.144, p <0.001).
Working hours were reported as one of the
main issues affecting emergency physician wellbeing in the free-text section of
our survey. Interestingly, the statistical analysis did not show an increase in
burnout when working over 50 hours a week (MBI: OR 1.00, p = 0.93; CBI: OR
1.004, p = 0.515). Similarly, working part time was also not statistically associated
with increased burnout (MBI: OR 1.01, p = 0.02; CBI: OR 1.008, p = 0.067). We suggest
interpreting these results with caution, as the denominator used was that of a 50-hour
week with 10-hour days, which is the standard for all physicians, regardless of
medical specialty, in Switzerland [33]. As suggested by other studies [34–36],
the 50-hour week is in itself not adapted to emergency medicine, as it does not
take into account the strenuous nature and constant (increasing) workflow of emergency
departments. As such, it is our opinion that the 50-hour week is in itself a
risk factor for burnout, and this has been suggested in a recent review of Danish
studies [37]. A comparative analysis between a 50-hour work week and a reduced
work schedule for emergency medicine would thus be pertinent; this might be an
area for reform.
The number of years of practice and age
also seemed to have an effect on burnout. In an inverse relationship, each
additional year of practice decreased the risk of burnout (MBI: OR 0.93, p <0.001;
CBI: OR 0.950, p <0.001), similarly to age (MBI: OR 0.93, p <0.001; CBI:
OR 0.952, p <0.001). This is seemingly counterintuitive, as one would expect
that the more time spent in a strenuous work environment, the higher the
potential for burnout. However, this interpretation does not consider that,
with increasing experience, emergency medicine physicians generally see their
share of night shifts decrease in favour of more traditional daytime hours, and
clinical responsibilities diminish in favour of diverse non-clinical areas, such
as training and emergency department management. Senior physicians are
therefore less likely to be regularly exposed to difficult working conditions,
and thus less likely to burn out, which could explain the statistical results.
Specific to Switzerland, and our study,
language at the place of work was shown to have an influence on burnout, though
this was not statistically significant. French-speaking respondents reported
more burnout than physicians working in German (MBI: OR 0.647, p = 0.015; CBI:
OR 0.52, p <0.001) or Italian (MBI: OR 0.730, p = 0.0244; CBI: OR 0.66, p = 0.128)
areas, in a manner similar to that seen in previous studies in Switzerland [16,
38]. Further analysis is needed, as each region, and often each canton, differs
in the way emergency departments are organised; this includes (but is not
limited to) the type of clinical activity and level of clinical supervision. A follow-up
study to this survey aims to incorporate these specificities as variables to
better understand their influence on wellbeing.
Our study has therefore demonstrated that current
working conditions negatively influence the wellbeing of Swiss emergency
physicians. Reform is therefore vital, not only for the health of emergency
physicians, but also for the continuity of acute care, which is at risk due to
high staff attrition rates, as evidenced by the 40.6% of respondents who reported
considering a change in their career at least once a month. In order to reform
these working conditions, other parameters that are not assessable using Likert
scale questions need to be reviewed. As mentioned previously, our survey
included a free-text section, which offered an opportunity for participants to report
the challenges they faced. As the subject of a separate analysis, we believe
this will help to guide reform and to explain why no other medical specialty
sees such high rates of burnout and staff turnover.
Notably, certain factors extrinsic to working
conditions had an important influence on burnout. Similar to other studies [10,
39–43], female and non-binary physicians reported higher levels of burnout than
their male counterparts (MBI: OR 1.70, p = 0.001; CBI: OR 1.18, p = 0.31) . As
with other studies, this seems to be an independent factor [19, 44–46].
Interestingly, having no children was also a contributing factor (MBI: 2.28, p <0.001;
CBI: 3.71, p <0.001), as was being single, suggesting the importance of
personal resources.
Limitations
While we believe the sample was
representative of the population, the modified snowball approach used to
distribute the survey introduced bias. Given the unknown total sample size and the
infeasibility of estimating the total number of emergency department physicians
in Switzerland, the response rate is difficult to estimate. In addition, the
survivorship bias mentioned during the discussion limited the study to physicians
who are currently practicing. The absence of mandatory membership to the Swiss
Society of Emergency and Rescue Medicine makes surveying those who have already
left difficult and allows the possibility of recollection bias. All of these
issues are due to the absence of a recognised specialist title and dedicated
training pathway.
Conclusion
With over half of survey respondents
meeting at least one criterion for burnout, 20% screening positive for moderate
to severe depression (nearly 4 times the incidence in the general population)
and 10.8% having considered suicide at some point during their career, this is
the first national study to demonstrate that current working conditions are
harmful to the wellbeing of Swiss emergency physicians. In a system in which continuity
is regularly questioned (40.6% of survey respondents reported considering a
change in their career at least once a month), reform is urgently needed. This
study aimed to provide a situational overview and offers insight into what factors
affect wellbeing in emergency medicine. Furthermore, it confirmed certain risk
factors for burnout previously identified in other international studies, such
as night shifts, working hours, seniority, gender and individual resources, and
introduced new factors, such as language of practice. In order to evaluate
trends and better understand some of these aforementioned factors, regular
follow-up studies are required.
Dr med. Eric Heymann
Médecin
Chef Adjoint
Département
des Urgences
Réseau hospitalier neuchâtelois
Rue de la Maladière 45
CH-2000 Neuchâtel
eric.heymann[at]rhne.ch
References
1. WHO. Burn-out an “occupational phenomenon”: International Classification of Diseases
[Internet]. [cited 2023 May 9]. Available from: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
2. Maslach C. Burnout, Psychology of. In: Wright JD, editor. International Encyclopedia
of the Social & Behavioral Sciences. 2nd ed. Oxford: Elsevier; 2015. pp. 929–32. [Internet][
[cited 2023 May 9]], Available from https://www.sciencedirect.com/science/article/pii/B9780080970868260091 10.1016/B978-0-08-097086-8.26009-1
3. Von Känel R. Was der Klinikarzt vom Burnout-Syndrom wissen sollte – Von der gezielten
Fragestellung bis zur Übermittlung der Verdachtsdiagnose. Klin. 2016 Feb;45(01):26–32.
10.1055/s-0041-111192
4. Hodkinson A, Zhou A, Johnson J, Geraghty K, Riley R, Zhou A, et al. Associations of
physician burnout with career engagement and quality of patient care: systematic review
and meta-analysis. BMJ. 2022 Sep;378:e070442. 10.1136/bmj-2022-070442
5. Zhang Q, Mu MC, He Y, Cai ZL, Li ZC. Burnout in emergency medicine physicians: A meta-analysis
and systematic review. Medicine (Baltimore). 2020 Aug;99(32):e21462. 10.1097/MD.0000000000021462
6. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator.
Lancet. 2009 Nov;374(9702):1714–21. 10.1016/S0140-6736(09)61424-0
7. Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence Relating
Health Care Provider Burnout and Quality of Care: A Systematic Review and Meta-analysis.
Ann Intern Med. 2019 Oct;171(8):555–67. 10.7326/M19-1152
8. Wright T, Mughal F, Babatunde OO, Dikomitis L, Mallen CD, Helliwell T. Burnout among
primary health-care professionals in low- and middle-income countries: systematic
review and meta-analysis. Bull World Health Organ. 2022 Jun;100(6):385–401A. 10.2471/BLT.22.288300
9. General Medical Council. National training surveys reports, 2022 summary reports.
Internet: https://www.gmc-uk.org/about/what-we-do-and-why/data-and-research/national-training-surveys-reports
10. Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Wang H, et al. Changes in Burnout
and Satisfaction With Work-Life Integration in Physicians and the General US Working
Population Between 2011 and 2020. Mayo Clin Proc. 2022 Mar;97(3):491–506. 10.1016/j.mayocp.2021.11.021
11. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52(1):397–422.
10.1146/annurev.psych.52.1.397
12. Bauer J, Stamm A, Virnich K, Wissing K, Müller U, Wirsching M, et al. Correlation
between burnout syndrome and psychological and psychosomatic symptoms among teachers.
Int Arch Occup Environ Health. 2006 Mar;79(3):199–204. 10.1007/s00420-005-0050-y
13. Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The Relationship
Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis.
J Gen Intern Med. 2017 Apr;32(4):475–82. 10.1007/s11606-016-3886-9
14. Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, Drop Out, Suicide: Physician
Loss in Emergency Medicine, Part I. West J Emerg Med. 2019 May;20(3):485–94. 10.5811/westjem.2019.4.40970
15. Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences
of physician dissatisfaction. Med Care. 2006 Mar;44(3):234–42. 10.1097/01.mlr.0000199848.17133.9b
16. Arigoni F, Bovier PA, Sappino AP. Trend of burnout among Swiss doctors. Swiss Med
Wkly. 2010 Aug;140:w13070.
17. Zumbrunn B, Stalder O, Limacher A, Ballmer PE, Bassetti S, Battegay E, et al. The
well-being of Swiss general internal medicine residents. Swiss Med Wkly [Internet].
2020 Jun 18 [cited 2022 Nov 21];(23). Available from: https://smw.ch/article/doi/smw.2020.20255 10.4414/smw.2020.20255
18. Al-Gobari M, Shoman Y, Blanc S, Canu IG. Point prevalence of burnout in Switzerland:
a systematic review and meta-analysis. Swiss Med Wkly [Internet]. 2022 Sep 28 [cited
2022 Nov 21];(37). Available from: https://smw.ch/article/doi/smw.2022.w30229 10.4414/SMW.2022.w30229
19. Petrino R, Riesgo LG, Yilmaz B. Burnout in emergency medicine professionals after
2 years of the COVID-19 pandemic: a threat to the healthcare system? Eur J Emerg Med.
2022 Aug;29(4):279–84. 10.1097/MEJ.0000000000000952
20. Douillet D, Caillaud A, Riou J, Miroux P, Thibaud E, Noizet M, et al. Assessment of
physicians’ resilience level during the COVID-19 pandemic. Transl Psychiatry. 2021 May;11(1):283.
10.1038/s41398-021-01395-7
21. Dyrbye LN, Meyers D, Ripp J, Dalal N, Bird SB, Sen S. A Pragmatic Approach for Organizations
to Measure Health Care Professional Well-Being. NAM Perspect [Internet]. 2018 Oct 1
[cited 2023 Oct 31]; Available from: https://nam.edu/a-pragmatic-approach-for-organizations-to-measure-health-care-professional-well-being/ 10.31478/201810b
22. Levis B, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) Collaboration.
Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression:
individual participant data meta-analysis. BMJ. 2019 Apr;365:l1476. 10.1136/bmj.l1476
23. Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach Burnout Inventory
Manual [Internet]. 4th ed. Menlo Park, CA: Mind Garden; [cited 2023 Nov 12]. Available
from: https://www.mindgarden.com/maslach-burnout-inventory-mbi/686-mbi-manual-print.html
24. Det Nationale Forskningscenter for Arbejdsmiljø. Copenhagen Burnout Inventory - CBI
[Internet]. [cited 2023 Nov 12]. Available from: https://nfa.dk/da/Vaerktoejer/Sporgeskemaer/Sporgeskema-til-maaling-af-udbraendthed/Copenhagen-Burnout-Inventory-CBI
25. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity
measure. J Gen Intern Med. 2001 Sep;16(9):606–13. 10.1046/j.1525-1497.2001.016009606.x
26. Kocalevent RD, Hinz A, Brähler E. Standardization of the depression screener patient
health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2013;35(5):551–5.
10.1016/j.genhosppsych.2013.04.006
27. The Lancet. Physician burnout: a global crisis. Lancet. 2019 Jul;394(10193):93. 10.1016/S0140-6736(19)31573-9
28. Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of Burnout on Self-Reported
Patient Care Among Emergency Physicians. West J Emerg Med. 2015 Dec;16(7):996–1001.
10.5811/westjem.2015.9.27945
29. Center C, Davis M, Detre T, Ford DE, Hansbrough W, Hendin H, et al. Confronting depression
and suicide in physicians: a consensus statement. JAMA. 2003 Jun;289(23):3161–6. 10.1001/jama.289.23.3161
30. Dorevitch S, Forst L. The occupational hazards of emergency physicians. Am J Emerg
Med. 2000 May;18(3):300–11. 10.1016/S0735-6757(00)90125-6
31. Goolsby C, Lala V, Gebner R, Dacuyan-Faucher N, Charlton N, Schuler K. Emergency physician
risk of occupational mortality: A scoping review. J Am Coll Emerg Physicians Open.
2021 Oct;2(5):e12554. 10.1002/emp2.12554
32. Lee YK, Lee CC, Chen CC, Wong CH, Su YC. High risk of ‘failure’ among emergency physicians
compared with other specialists: a nationwide cohort study. Emerg Med J. 2013 Aug;30(8):620–2.
10.1136/emermed-2012-201440
33. SECO S d’Etat à l’économie. Aide-mémoire sur l’application de la loi sur le travail
dans les hôpitaux et cliniques [Internet]. [cited 2023 Nov 12]. Available from: https://www.seco.admin.ch/seco/fr/home/Publikationen_Dienstleistungen/Publikationen_und_Formulare/Arbeit/Arbeitsbedingungen/Merkblatter_und_Checklisten/merkblatt-fuer-die-anwendung-des-arbeitsgesetzes-in-krankenansta.html
34. Stowell JR, Vohra TT, Luber SD. Emergency medicine resident clinical hours: a national
survey. J Emerg Med. 2015 Apr;48(4):474–80.e1. 10.1016/j.jemermed.2014.11.005
35. Rischall ML, Chung AS, Tabatabai R, Doty C, Hart D. Emergency Medicine Resident Shift
Work Preferences: A Comparison of Resident Scheduling Preferences and Recommended
Schedule Design for Shift Workers. AEM Educ Train. 2018 Jun;2(3):229–35. 10.1002/aet2.10104
36. Jeanmonod R, Brook C, Winther M, Pathak S, Boyd M. Resident productivity as a function
of emergency department volume, shift time of day, and cumulative time in the emergency
department. Am J Emerg Med. 2009 Mar;27(3):313–9. 10.1016/j.ajem.2008.03.002
37. Zaugg J. Les médecins danois ont trouvé l’équilibre. Bull Med Suisses 2023. Available
from: https://saez.swisshealthweb.ch/fr/article/doi/bms.2023.22195
38. Goehring C, Bouvier Gallacchi M, Künzi B, Bovier P. Psychosocial and professional
characteristics of burnout in Swiss primary care practitioners: a cross-sectional
survey. Swiss Med Wkly. 2005 Feb;135(7-8):101–8. 10.4414/smw.2005.10841
39. Jagsi R, Griffith KA, Jones R, Perumalswami CR, Ubel P, Stewart A. Sexual Harassment
and Discrimination Experiences of Academic Medical Faculty. JAMA. 2016 May;315(19):2120–1.
10.1001/jama.2016.2188
40. Linzer M, Harwood E. Gendered Expectations: Do They Contribute to High Burnout Among
Female Physicians? J Gen Intern Med. 2018 Jun;33(6):963–5. 10.1007/s11606-018-4330-0
41. Hu YY, Ellis RJ, Hewitt DB, Yang AD, Cheung EO, Moskowitz JT, et al. Discrimination,
Abuse, Harassment, and Burnout in Surgical Residency Training. N Engl J Med. 2019 Oct;381(18):1741–52.
10.1056/NEJMsa1903759
42. Templeton K, Bernstein CA, Sukhera J, Nora LM, Newman C, Burstin H, et al. Gender-Based
Differences in Burnout: Issues Faced by Women Physicians. NAM Perspect [Internet].
2019 May 30 [cited 2023 Nov 21]; Available from: https://nam.edu/gender-based-differences-in-burnout-issues-faced-by-women-physicians/
43. Krisen: Vor allem Ärztinnen mit Kindern suchen Hilfe [Internet]. [cited 2023 Nov 21].
Available from: https://www.medinside.ch/post/krisen-vor-allem-aerztinnen-mit-kindern-suchen-hilfe
44. Levine H, Baranchuk N, Li T, Garra G, Nagarajan MS, Garg N. An emergency medicine
physician well-being study focusing on gender differences and years of practice during
the COVID-19 pandemic. Am J Emerg Med. 2022 May;55:84–8. 10.1016/j.ajem.2022.02.055
45. Lin YY, Pan YA, Hsieh YL, Hsieh MH, Chuang YS, Hsu HY, et al. COVID-19 Pandemic Is
Associated with an Adverse Impact on Burnout and Mood Disorder in Healthcare Professionals.
Int J Environ Res Public Health. 2021 Apr;18(7):3654. 10.3390/ijerph18073654
46. Corlade-Andrei M, Măirean C, Nedelea P, Grigorași G, Cimpoeșu D. Burnout Syndrome
among Staff at an Emergency Department during the COVID-19 Pandemic. Healthcare (Basel).
2022 Jan;10(2):258. 10.3390/healthcare10020258