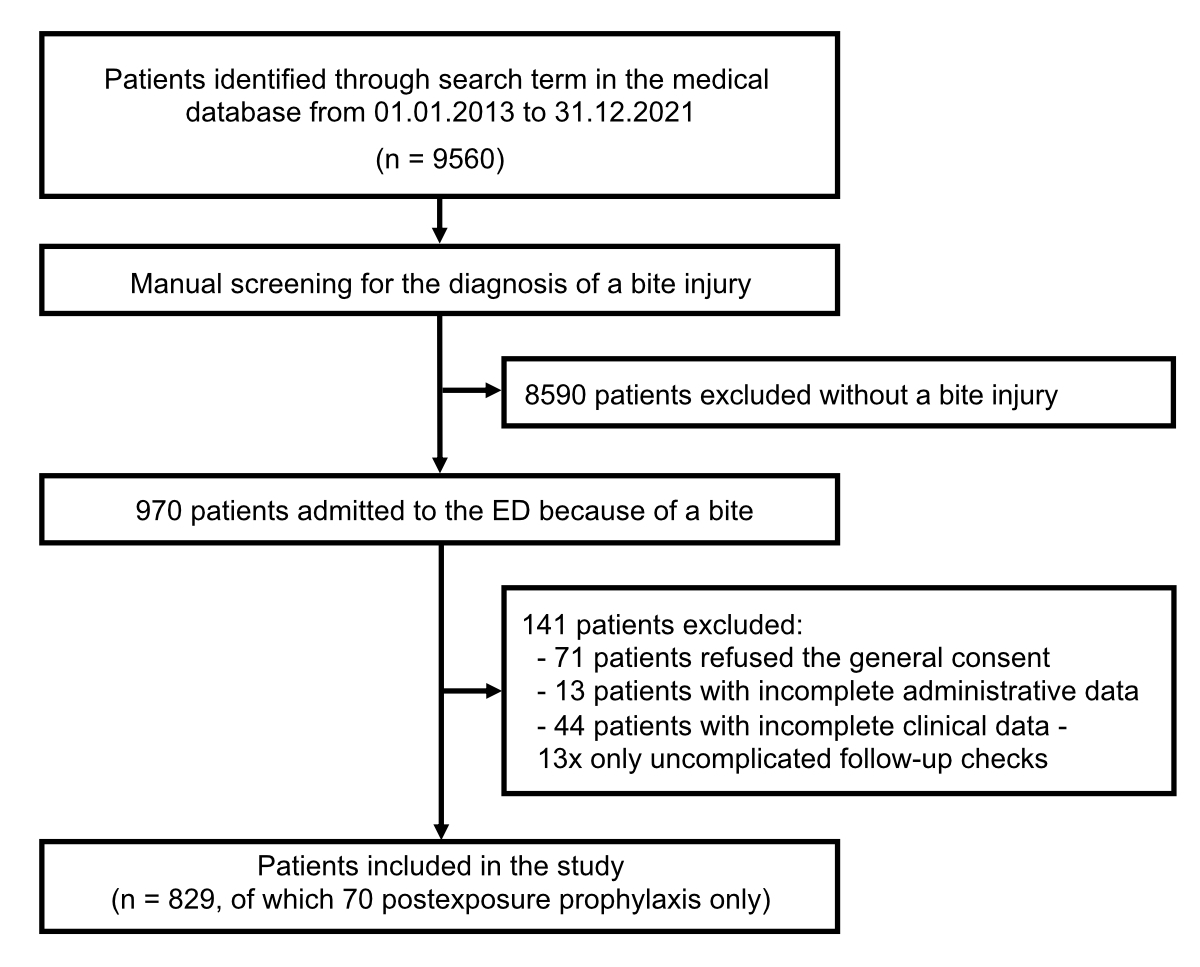
Figure 1Flowchart of the study.
ED: emergency department.
DOI: https://doi.org/https://doi.org/10.57187/smw.2023.40093
Animal and human bite injuries are a significant global health problem [1–3]. The frequency and nature of animal and human bite injuries depend on geographic location, level of industrialisation and cultural factors [4]. Whereas in industrialised countries bite injuries are more likely to result in localised injuries and infections, human rabies remains an important zoonotic disease in many developing countries, especially in Asia and Africa [5].
In the USA, an estimated 50% of people will be bitten by an animal or another person during their lifetime and bite injuries account for 1% of all emergency department visits [3, 6, 7]. According to the literature, dog bites are the most common animal bites (60–80%), followed by cat bites (20–30%) and rodent bites (2–3%) [2, 8–10]. Human bites are the third most common source of bites, accounting for 3.6% to 23% of all bite injuries [1, 11].
Wound characteristics depend on the species, the bite source dentition and the anatomical location of the injury [2]. The most frequent locations are the hands and extremities in 70–80% of cases and the head and neck in 10–30% of cases [4]. Most bite wounds can be treated in the emergency department [1]. Adequate and prompt management with irrigation and removal of necrotic tissue is important in lowering complication risk [1, 12, 13]. The incidence of wound infection is high compared with other traumatic wounds. The relative risk is determined by animal species, site of bite, host factors and local wound care [12]. Human bites can also transmit hepatitis B, hepatitis C and HIV; postexposure prophylaxis should be considered in every human bite [14].
In Switzerland, animal bites are frequent and represent a public health problem of increasing importance due to the steadily growing pet population [15]. The true incidence of bite injuries in general is difficult to determine because not all patients with bite injuries seek medical attention; this is especially common for human bites [2, 12]. In Switzerland, 20 years ago, an annual incidence rate of medical consultations following vertebrate bites and scratches was found to be 325 per 100,000 people [15]. In regard to socioeconomic changes in Switzerland including the growing pet population in recent years, the present study aimed to provide an up-to-date overview of animal and human bite injuries in patients admitted to a tertiary emergency department in Switzerland in terms of demographics, injury patterns and treatment strategies for bite injuries of different sources.
This cross-sectional study was conducted at the Department of Emergency Medicine for Adults of the Inselspital, Bern University Hospital, Switzerland, a tertiary emergency department, from 1 January 2013 to 31 December 2021.
A full-text keyword search was performed on the medical reports of all adult patients (≥16 years) admitted to our emergency department within the given time period using the defined keyword “bite”. The medical reports of the identified consultations were then manually reviewed for an actual human or animal bite injury by two experienced physicians (MK and LM). Patients without a recent bite wound diagnosis, cases with incomplete clinical data in the manual full-text analysis and patients who refused to give general consent for the use of their anonymised data or subsequently withdrew it were excluded from the study. Follow-up consultations after the emergency department visit were not evaluated. Patients who visited the emergency department only for postexposure prophylaxis were analysed separately (postexposure prophylaxis-specific) due to often undocumented bite information in the reports.
The following data were extracted automatically or manually (MK and LM) from the database of the patient management system (E. care; Mesalvo Turnhout BV, Turnhout, Belgium) of the Department of Emergency Medicine for Adults of Bern University Hospital, Switzerland:
The statistical analysis was performed with Stata® 16.1 (StataCorp LLC, College Station, Texas, USA). For the descriptive analysis, the distribution of continuous variables, such as age, were described with the median and interquartile range (IQR) as most continuous variables were not normally distributed. The distribution of categorical data was described with the total number accompanied by the percentages. P values were obtained using the Chi-squared test for categorical variables and the Kruskal-Wallis test for continuous variables; variables with a p value <0.05 were considered significant.
The study was approved by the regional ethics committee of the Canton of Bern, Switzerland (KEK:2019-00628).
From 1 January 2013 to31 December 2021, a total of 9560 out of 407,278 patients referred to our emergency department were identified in the medical database using our search strategy. Ultimately, 829 patients met all inclusion criteria. Of these, 70 (8.4%) patients visited the emergency department only for postexposure prophylaxis treatment and were analysed separately; hence 759 (91.4%) patients were included in the overall study analysis (figure 1).
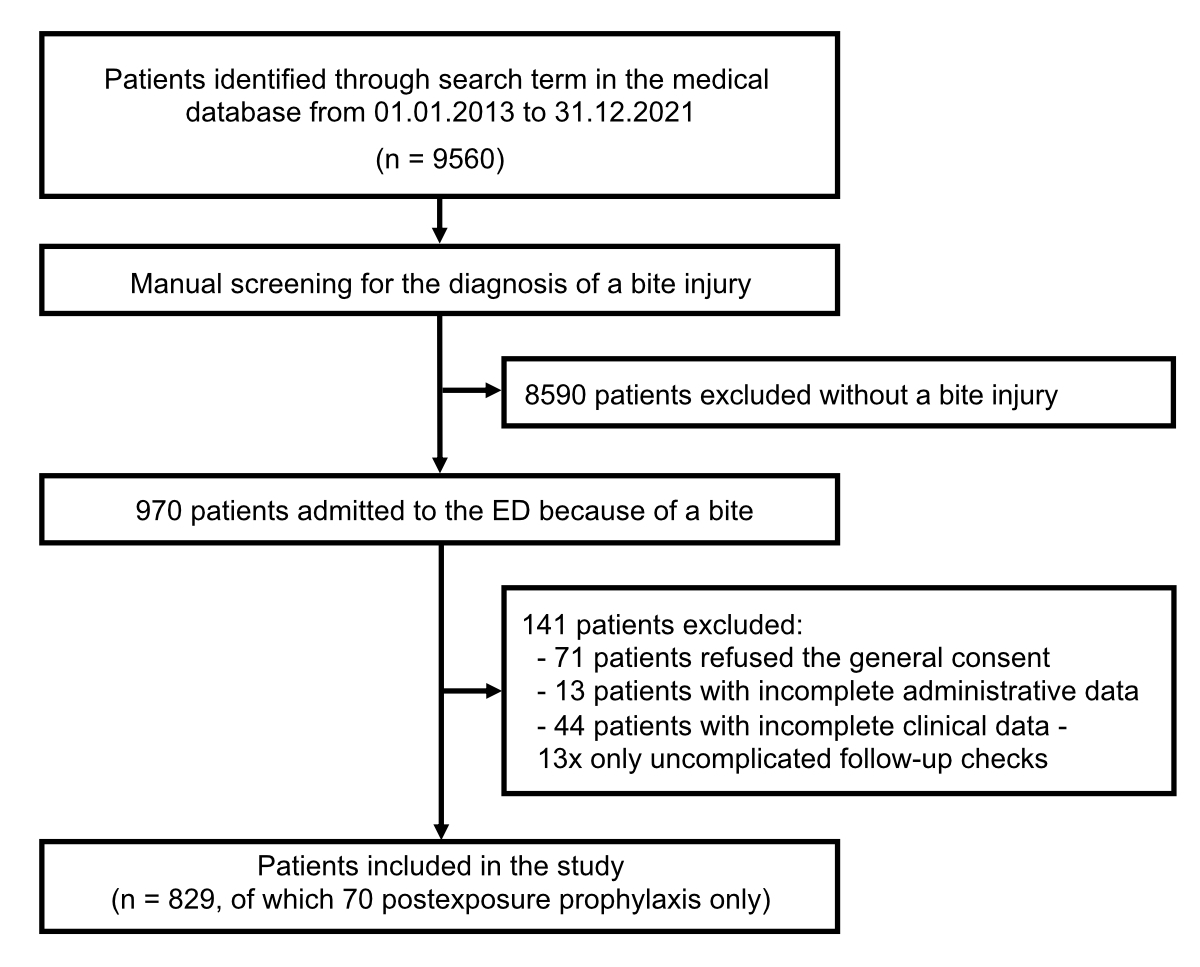
Figure 1Flowchart of the study.
ED: emergency department.
Most patients were bitten by a dog (n = 336, 44.3%), followed by cats (n = 239, 31.5%). Human bites were the third most frequent source of bite injuries (n = 115, 15.2%). Sixty-nine patients (9.1%) were bitten by other animals (table 1).
Table 1Source of bite; n = 759; Patients with consultation for postexposure prophylaxis only are excluded.
| n | (%) | |
| Dog | 336 | (44.3) |
| Cat | 239 | (31.5) |
| Human | 115 | (15.2) |
| Snake | 24 | (3.2) |
| Rat | 14 | (1.8) |
| Horse | 8 | (1.1) |
| Mouse | 6 | (0.7) |
| Bat | 4 | (0.5) |
| Rabbit | 3 | (0.4) |
| Monkey | 2 | (0.3) |
| Fish | 2 | (0.3) |
| Fox | 1 | (0.1) |
| Scorpion | 1 | (0.1) |
| Degu (a rodent) | 1 | (0.1) |
| Marten | 1 | (0.1) |
| Cow | 1 | (0.1) |
| Chicken | 1 | (0.1) |
Overall, the median age was 39 (IQR 27–54) years and 407 (53.6%) patients were female. The 336 dog bites occurred in 174 men (51.8%) and 162 women (48.2%). Cat bite injuries were more than twice as likely to affect women (n = 172, 72.0%) than men (n = 67, 28.0%) and human bites were twice as common in men (n = 79, 68.7%) than in women (n = 36, 31.3%). In total, 400 (52.7%) patients presented to the emergency department within six hours of the bite, among them mainly patients after human bites (n = 93, 80.9%) and dog bites (n = 207, 61.6%). Most patients with cat bites presented to our emergency department >6 hours after the bite (n = 178, 74.5%) (table 2).
Table 2Demographic data for patients with human and animal bite injuries; n = 759; Patients with consultation for postexposure prophylaxis only are excluded.
| All patients | Source of bite | |||||||||||
| Human | Dog | Cat | Other animal | |||||||||
| n = 759 | (%) | n = 115 | (%) | n = 336 | (%) | n = 239 | (%) | n = 69 | (%) | p value | ||
| Sex | Female | 407 | (53.6) | 36 | (31.3) | 162 | (48.2) | 172 | (72.0) | 37 | (53.6) | |
| Male | 352 | (46.4) | 79 | (68.7) | 174 | (51.8) | 67 | (28.0) | 32 | (46.4) | ||
| Age in years, median (IQR) | 39 | (27– 54) | 29 | (22–40) | 40 | (27–55) | 47 | (34–58) | 33 | (26–51) | <0.001 | |
| Age categories, years | 16–25 | 156 | (20.6) | 42 | (36.5) | 71 | (21.1) | 28 | (11.7) | 15 | (21.7) | |
| 26–35 | 173 | (22.8) | 38 | (33.0) | 73 | (21.7) | 39 | (16.3) | 23 | (33.3) | ||
| 36–45 | 129 | (17.0) | 17 | (14.8) | 52 | (15.5) | 50 | (20.9) | 10 | (14.5) | ||
| 46–55 | 130 | (17.1) | 13 | (11.3) | 59 | (17.6) | 49 | (20.5) | 9 | (13.0) | ||
| 56–65 | 91 | (12.0) | 4 | (3.5) | 45 | (13.4) | 36 | (15.1) | 6 | (8.7) | ||
| >65 | 80 | (10.5) | 1 | (0.9) | 36 | (10.7) | 37 | (15.5) | 6 | (8.7) | ||
| Time to consultation, hours | 0–6 | 400 | (52.7) | 93 | (80.9) | 207 | (61.6) | 61 | (25.5) | 39 | (56.5) | |
| 7–24 | 151 | (19.9) | 9 | (7.8) | 43 | (12.8) | 84 | (35.1) | 15 | (21.7) | ||
| 25–48 | 69 | (9.1) | 3 | (2.6) | 23 | (6.8) | 39 | (16.3) | 4 | (5.8) | ||
| >48 | 112 | (14.8) | 4 | (3.5) | 48 | (14.3) | 50 | (20.9) | 10 | (14.5) | ||
| Unknown | 27 | (3.6) | 6 | (5.2) | 15 | (4.5) | 5 | (2.1) | 1 | (1.4) | ||
Face injuries occurred in 19.6% (n = 66) of dog bites, in 13.9% (n = 16) of human bites and in 2.5% (n = 6) of cat bites. Injuries of the arm were found in 25.2% (n = 29) of human bites, in 17.2% (n = 41) of cat bites and in 16.7% (n = 56) of dog bites. Overall, hand injuries were seen most frequently (n = 412, 54.3%) and were mainly inflicted by “other animals” (n = 54, 78.3%) and cats (n = 171, 71.5%). Leg injuries were fourth most common (n = 87, 11.5%) and were most often inflicted by dogs (n = 68, 20.2%). Multiple bite wounds were found in 63 (8.3%) patients.
Most bite injuries (n = 609, 80.2%) were mild (severity grade I). Severe bite injuries (grade II or III) were found mainly in dog bites (n = 95, 28.3%). Signs of infection were found in 34.5% (n = 262) of all patients and ranged from 5.2% (n = 6) after human bites to 73.6% (n = 176) after cat bites (table 3).
Table 3Wound characteristics at presentation; n = 759; Patients with consultation for postexposure prophylaxis only are excluded.
| All patients | Source of bite | p value | |||||||||
| Human | Dog | Cat | Other animal | ||||||||
| n = 759 | (%) | n = 115 | (%) | n = 336 | (%) | n = 239 | (%) | n = 69 | (%) | ||
| Anatomical location of the bite | |||||||||||
| Face (including ears) | 92 | (12.1) | 16 | (13.9) | 66 | (19.6) | 6 | (2.5) | 4 | (5.8) | <0.001 |
| Head and neck | 14 | (1.8) | 4 | (3.5) | 8 | (2.4) | 1 | (0.4) | 1 | (1.4) | 0.174 |
| Arm | 130 | (17.1) | 29 | (25.2) | 56 | (16.7) | 41 | (17.2) | 4 | (5.8) | 0.009 |
| Hand | 412 | (54.3) | 47 | (40.9) | 140 | (41.7) | 171 | (71.5) | 54 | (78.3) | <0.001 |
| Torso | 12 | (1.6) | 7 | (6.1) | 4 | (1.2) | 1 | (0.4) | 0 | (0.0) | <0.001 |
| Leg | 87 | (11.5) | 7 | (6.1) | 68 | (20.2) | 11 | (4.6) | 1 | (1.4) | <0.001 |
| Foot | 14 | (1.8) | 0 | (0.0) | 4 | (1.2) | 5 | (2.1) | 5 | (7.2) | 0.003 |
| Genitals* | 3 | (0.4) | 1 | (0.9) | 2 | (0.6) | 0 | (0.0) | 0 | (0.0) | – |
| Multiple | 63 | (8.3 | 18 | (15.7) | 23 | (6.8) | 22 | (9.2) | 0 | (0.0) | 0.001 |
| Classification according to Rueff** | <0.001 | ||||||||||
| Grade I | 609 | (80.2) | 110 | (95.7) | 240 | (71.4) | 204 | (85.4) | 55 | (79.7) | |
| Grade II | 122 | (16.1) | 4 | (3.5) | 78 | (23.2) | 33 | (13.8) | 7 | (10.1) | |
| Grade III | 22 | (2.9) | 1 | (0.9) | 17 | (5.1) | 0 | (0.0) | 4 | (5.8) | |
| Unknown | 1 | (0.1) | 0 | (0.0) | 1 | (0.3) | 0 | (0.0) | 0 | (0.0) | |
| Signs of infection | 262 | (34.5) | 6 | (5.2) | 63 | (18.8) | 176 | (73.6) | 17 | (24.6) | <0.001 |
* Too few cases to calculate the p value.
** Classification according to Rueff: 0 = no visible lesion; grade I = superficial skin lesion, torn skin, scratched skin, bite canal, crushing injury; grade II = wound extending from the skin to the fascia, muscle or cartilage; grade III = wound with tissue necrosis or tissue loss. Only 5 patients were assessed as grade 0 (2 patients with cat bites and 3 patients with “Other animal” bites).
For the majority of patients, wound treatment was provided in the emergency department (n = 562, 74.0%); one fifth of the patients (n = 164, 21.6%) required treatment in the operating theatre or by a specialist in the polyclinic, e.g. hand surgery or plastic surgery. In the majority of cases, wound treatment was restricted to cleaning measures only (n = 402, 53.0% superficial disinfection; n = 112, 14.8% with additional wound irrigation with sterile water). Simple suturing was performed in 60 (7.9%) patients, complicated suturing in 39 (5.1%) patients. Patients with cat bites needed a wound revision in 41.4% (n = 99) of cases. Half of all patients received prophylactic antibiotics (n = 388, 51.1%), especially for human (n = 79, 68.7%) and dog (n = 218, 64.9%) bites, but only 61 (25.5%) patients with a cat bite. Patients with cat bites often received secondary antibiotics (n = 161, 67.4%). Active immunisation for tetanus prophylaxis was performed in 351 (46.2%) of the patients; 7 (0.9%) patients received active and passive tetanus immunisation; 3 (0.4%) patients received passive tetanus immunisation. For human bites, HIV postexposure prophylaxis was administered in 4 (3.5%) patients and hepatitis B postexposure prophylaxis in 17 (14.8%) patients. For animal bites, active and passive rabies postexposure prophylaxis was performed in 19 (3.0%) patients; active rabies immunisation in 4 (0.6%) patients. The majority of patients could be discharged home after emergency treatment (n = 597, 78.7%); only 162 (21.3%) patients were hospitalised, especially patients with cat bites (n = 89, 37.2%) who required hospitalisation more often than patients with dog bites (n = 55, 16.4%). Five of the 24 patients with a snake bite were treated with antivenom and four of them were hospitalised in the intensive care unit (table 4).
Table 4Treatment of animal and human bite injuries; n = 759; Patients with consultation for postexposure prophylaxis only are excluded.
| All patients | Source of bite | p value | |||||||||
| Human | Dog | Cat | Other animal | ||||||||
| n = 759 | (%) | n = 115 | (%) | n = 336 | (%) | n = 239 | (%) | n = 69 | (%) | ||
| Place of treatment | <0.001 | ||||||||||
| Emergency department | 562 | (74.0) | 114 | (99.1) | 246 | (73.2) | 152 | (63.3) | 50 | (72.5) | |
| Operating theatre or polyclinic | 164 | (21.6) | 1 | (0.9) | 78 | (23.2) | 78 | (32.6) | 7 | (10.1) | |
| Externally performed* | 31 | (4.1) | 0 | (0.0) | 11 | (3.3) | 8 | (3.3) | 12 | (17.4) | |
| Unknown | 2 | (0.3) | 0 | (0.0) | 1 | (0.3) | 1 | (0.4) | 0 | (0.0) | |
| Wound treatment | <0.001 | ||||||||||
| Disinfection only | 402 | (53.0) | 101 | (87.8) | 151 | (44.9) | 99 | (41.4) | 51 | (73.9) | |
| Disinfection and wound irrigation | 112 | (14.8) | 7 | (6.1) | 60 | (17.9) | 38 | (15.9) | 7 | (10.1) | |
| Simple suturing | 60 | (7.9) | 4 | (3.5) | 50 | (14.9) | 2 | (0.8) | 4 | (5.8) | |
| Complex suturing | 39 | (5.1) | 2 | (1.7) | 36 | (10.7) | 0 | (0.0) | 1 | (1.4) | |
| Wound revision | 143 | (18.8) | 0 | (0.0) | 38 | (11.3) | 99 | (41.4) | 6 | (8.7) | |
| Unknown | 3 | (0.4) | 1 | (0.9) | 1 | (0.3) | 1 | (0.4) | 0 | (0.0) | |
| Antibiotic treatment | <0.001 | ||||||||||
| None | 117 | (15.4) | 32 | (27.8) | 51 | (15.2) | 7 | (2.9) | 27 | (39.1) | |
| Prophylactic antibiotics | 388 | (51.1) | 79 | (68.7) | 218 | (64.9) | 61 | (25.5) | 30 | (43.3) | |
| Secondary antibiotics | 236 | (31.1) | 4 | (3.5) | 59 | (17.6) | 161 | (67.4) | 12 | (17.4) | |
| Unknown | 18 | (2.4) | 0 | (0.0) | 8 | (2.4) | 10 | (4.2) | 0 | (0.0) | |
| Tetanus postexposure prophylaxis | <0.001 | ||||||||||
| None | 394 | (51.9) | 64 | (55.7) | 135 | (40.2) | 157 | (65.7) | 38 | (55.1) | |
| Active immunisation | 351 | (46.2) | 47 | (40.9) | 197 | (58.6) | 76 | (31.8) | 31 | (44.8) | |
| Active and passive immunisation | 7 | (0.9) | 2 | (1.7) | 3 | (0.9) | 2 | (0.8) | 0 | (0.0) | |
| Passive immunisation | 3 | (0.4) | 2 | (1.7) | 0 | (0.0) | 1 | (0.4) | 0 | (0.0) | |
| Unknown | 4 | (0.5) | 0 | (0.0) | 1 | (0.3) | 3 | (1.3) | 0 | (0.0) | |
| Rabies postexposure prophylaxis** | |||||||||||
| Active and passive immunisation | 19 | (3.0) | – | – | 9 | (2.7) | 3 | (1.3) | 7 | (10.1) | 0.001 |
| Active immunisation | 4 | (0.6) | – | – | 4 | (1.2) | 0 | (0.0) | 0 | (0.0) | 0.158 |
| HIV / hepatitis B postexposure prophylaxis*** | |||||||||||
| Postexposure prophylaxis for HIV# | 4 | (3.5) | 4 | (3.5) | – | – | – | – | – | – | |
| Postexposure prophylaxis for hepatitis B## | 17 | (14.8) | 17 | (14.8) | – | – | – | – | – | – | |
| Disposition | <0.001 | ||||||||||
| Discharge | 597 | (78.7) | 115 | (100) | 281 | (83.6) | 150 | (62.8) | 51 | (73.9) | |
| Admission | 162 | (21.3) | 0 | (0.0) | 55 | (16.4) | 89 | (37.2) | 18 | (26.1) | |
| Hand surgery | 113 | (14.9) | 0 | (0.0) | 33 | (9.8) | 75 | (31.4) | 5 | (7.2) | |
| Plastic surgery | 13 | (1.7) | 0 | (0.0) | 10 | (3.0) | 2 | (0.8) | 1 | (1.4) | |
| Intensive care### | 6 | (0.8) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 6 | (8.7) | |
| Ophthalmology | 3 | (0.4) | 0 | (0.0) | 2 | (0.6) | 1 | (0.4) | 0 | (0.0) | |
| External hospital | 2 | (0.3) | 0 | (0.0) | 2 | (0.6) | 0 | (0.0) | 0 | (0.0) | |
| Other | 24 | (3.2) | 0 | (0.0) | 7 | (2.1) | 11 | (4.6) | 6 | (8.7) | |
| Unknown | 1 | (0.1) | 0 | (0.0) | 1 | (0.0) | 0 | (0.0) | 0 | (0.0) | |
* Performed externally, e.g. already by the admitting doctor or in the referring hospital.
** The total percentages refer to the total of 644 animal bites. Rabiespostexposure prophylaxis administered after the following “Other animal” bites: bats (4patients), monkey (1), fox (1), marten (1).
*** The total percentages refer to the total of 115 human bites.
# HIV test of the source not performed in 84 patients; HIV test of the source performed in 31 patients; source known to be HIV-positive in 2 patients.
## HBsAb titre known in 20 patients, HBsAb titre obtained in 25 patients; source known to be hepatitis B-positive in 1 patient.
### All patients hospitalised in the intensive care unit were snake bite patients; 5 patients totally were treated with antivenom, 4 of them were treated in the intensive care unit.
Ab: antibody
Bites most frequently occurred during leisure time (n = 609, 80.2%), regardless of the source of the bite. In more than half of all bite categories (n = 453, 59.7%), the animal or person biting was known to the victim. Human bites happened most frequently during acts of aggression (n = 88, 76.5%); in 27 cases (23.5%), the bite occurred under the influence of alcohol or other drugs. The reasons for animal bites were manifold (table 5).
Table 5Context of animal and human bites; n = 759; Patients with consultation for postexposure prophylaxis only are excluded.
| All patients | Source of bite | p value | |||||||||
| Human | Dog | Cat | Other animal | ||||||||
| Context of animal and human bites | n = 759 | (%) | n = 115 | (%) | n = 336 | (%) | n = 239 | (%) | n = 69 | (%) | <0.001 |
| Accident during leisure time | 609 | (80.2) | 85 | (73.9) | 293 | (87.2) | 178 | (74.5) | 53 | (76.8) | |
| Work-related accident | 80 | (10.5) | 27 | (23.5) | 21 | (6.2) | 18 | (7.5) | 14 | (20.3) | |
| Context of accident unclear | 70 | (9.2) | 3 | (2.6) | 22 | (6.5) | 43 | (18.0) | 2 | (2.9) | |
| Relationship to the biter | <0.001 | ||||||||||
| Animal/human known | 453 | (59.7) | 68 | (59.1) | 195 | (58.0) | 153 | (64.0) | 37 | (53.6) | |
| Animal/human unknown | 219 | (28.9) | 38 | (33.0) | 112 | (33.3) | 39 | (16.3) | 30 | (43.5) | |
| Unknown situation | 87 | (11.5) | 9 | (7.8) | 29 | (8.6) | 47 | (19.7) | 2 | (2.9) | |
| Animal bites | 644 | (84.8) | <0.001 | ||||||||
| Attack by an animal | 146 | (22.7) | 146 | (43.5) | 0 | (0.0) | 0 | (0.0) | |||
| Animal in distress (interfering in a fight between two animals included) | 237 | (36.8) | 70 | (20.8) | 125 | (52.3) | 42 | (60.9) | |||
| Veterinary care, feeding, other work with an animal | 69 | (10.7) | 24 | (7.1) | 28 | (11.7) | 17 | (24.6) | |||
| Playing with an animal | 50 | (7.8) | 43 | (12.8) | 7 | (2.9) | 0 | (0.0) | |||
| Bite by a police dog obeying police officer’s command | 4 | (0.6) | 4 | (1.2) | 0 | (0.0) | 0 | (0.0) | |||
| Other / Unknown | 138 | (21.4) | 49 | (14.6) | 79 | (33.1) | 10 | (14.5) | |||
| Human bites | 115 | (15.2) | - | ||||||||
| Influence of alcohol / other drug* | 27 | (23.5) | |||||||||
| Dispute / physical aggression | 88 | (76.5) | |||||||||
| Assisting another person having a seizure | 10 | (8.7) | |||||||||
| Other / Unknown | 17 | (14.8) | |||||||||
*The contextual factor “Alcohol/Other drugs” can be present in addition to any other contextual factors.
Seventy (8.4%) patients presented for postexposure prophylaxis only; this subgroup included, among others, 30 (42.9%) patients who had suffered a dog bite and 24 (34.3%) patients with a bat bite (supplementary table S1).
The median age was 36 (28–44) years. More than half (n = 37, 52.9%) of the patients presented >48 hours after the bite event. Active immunisation for tetanus prophylaxis was performed in 22 (31.4%) patients and 1 (1.4%) patient received a passive tetanus immunisation. Active and passive rabies postexposure prophylaxis was performed in 41 (61.2%) patients, active rabies immunisation in 19 (28.4%) patients and passive immunisation in 2 (3.0%) patients. No patient received HIV or hepatitis B postexposure prophylaxis (supplementary table S2).
In this single-centre study, 829 of 407,278 emergency department patients were evaluated for bite injuries from 2013 to 2021. In line with the literature, dog bites were the most frequent animal bite injuries, followed by cat and human bites [4].
The literature shows that men are more often affected by bite injuries in general; and, specifically, that dog bites are more common in young males; conversely, injuries from cats are significantly more frequent in females and older people [4, 8, 17, 18]. In our present study, the number of female patients overall was higher than male patients due to a high number of cat bites, whereas the number of dog bites was comparable between both sexes. Cat bite injuries were more than twice as likely to affect women, and human bites were more common in men.
Animal bites are mainly caused by pets [19, 20] and often occur in the context of a distressed animal: 50% to 80% of all patients are bitten by a familiar animal [3, 21], up to even 90% in the case of dog bites [1, 8–10]. Our results underline these findings: two thirds of the patients knew the animal and an animal in distress was present in one third of the cases. Bite injuries caused by humans are frequently related to aggressive behaviour, often associated with alcohol and other drugs or during sexual and athletic activities, occupational interventions (e.g. dental) or are self-inflicted [1]. In our present study, in almost two thirds of human bites the source of the bite was known to the victim and in more than 70% of the cases aggression was involved, in almost one quarter alcohol or other drugs.
In line with previous data [17], the arm and hand were by far the most frequently injured body sites. Dog bites led to the most severe primary injuries, whereas the majority of human and cat bites were deemed superficial injuries according to Rueff’s classification.
Surgical debridement with appropriate irrigation can effectively eradicate bacterial flora [22]. Nevertheless, 10–20% of bite wounds become infected, including 30–50% of cat bites, 5–25% of dog bites and 20–25% of human bites [4, 23–26]. Therefore, most experts recommend early prophylactic antibiotic treatment for fresh, deep wounds; injuries in critical body areas such as hands, feet and around joints, the face and genitalia; and for people at increased risk of infection due to immune disorders [3, 4, 25–27]. However, this remains a controversial issue in the literature. Meta-analyses found no evidence for a reduction in infection rates with prophylactic antibiotics, except in hand bite wounds caused by cats and humans [28–30].
In this study, 60% of patients with dog bites and 80% of patients with human bites presented to the emergency department within 6 hours. Two thirds of these patients received prophylactic antibiotic therapy. Consistent with prompt presentation, less than one fifth of dog bite patients and only a few human bite patients showed signs of infection at emergency department presentation. Dogs typically cause crush injuries when they bite [1]; in contrast cat bites result in small puncture wounds that appear harmless on the surface and the true depth of the injury is often underestimated by the patient and the physician [4]. Therefore, cat bites are often considered minor injuries, even though there is a high risk of infection due to deep bacterial inoculation. Initially, many of them might not even be treated medically. As our data show, the majority of patients with cat injuries presented to the trauma centre when complications occurred: over 70% of patients with cat bites presented with a delay of more than six hours after the bite event and showed signs of infection. This is in line with the literature: results from a Belgian study demonstrated that 75% of dog bite patients presented within 24 hours of the attack, while all of the patients injured by cats presented relatively late when infectious complications had developed [12].
The high rate of infections after cat bites is certainly related to the tertiary care role of our emergency department, as many patients are referred for hand or plastic surgery due to complications after bite injuries. Consequently, more than one third of patients were hospitalised after cat bites compared to 16.4% of patients after dog bites, although the initial bite injury by dogs was more often classified as severe. Patients with human bite wounds had only superficial wounds and hospitalisation was not required.
Only 4 of the 115 human bite patients received HIV postexposure prophylaxis and 17 patients received hepatitis B postexposure prophylaxis. This low rate may be due to the fact that the source was known to many patients and the risk of transmission of infectious diseases could be assessed. Nevertheless, careful evaluation of the indication for HIV postexposure prophylaxis, hepatitis B postexposure prophylaxis and hepatitis C infection follow-up is warranted after all human bite injuries.
The strength of this study is the consecutive inclusion of all admissions of animal and human bite injuries in a large emergency department over a 9-year time period. This study has some limitations. As with all retrospective data analyses, we cannot rule out documentation bias or missed patients, despite careful data extraction and analysis. This is a single-centre study and many patients with minor bite injuries are likely to be treated in surrounding hospitals and by general practitioners and are not seen at the tertiary emergency department. In addition, patients presenting primarily for a bite injury and those presenting as a result of a complication following a bite injury were included in this cohort. In view of this and the fact that no follow-up data were collected, no general statements can be made about the association between the source of the bite and the risk of infection in this patient population.
Animal and human bites, although preventable, are common consultations in the emergency department. Dog bites were the most common, followed by cat and human bites. Dog bites were associated with the most severe primary injuries. Patients with dog and human bites often presented primarily to the emergency department, whereas patients with cat bites frequently presented with a delay and signs of infection. In summary, primary and emergency care physicians must be aware of the high risk of infection after bite injuries, especially after cat bites. Surgical debridement in the initial treatment needs to be considered. Prophylactic antibiotic therapy and close follow-up examinations are recommended in most cases.
We thank Sabina Utiger, data manager, for the data extraction from the medical database of the emergency department, Inselspital, Bern.
Author contributions: SE, DAJ, MM, MK, LM, JK designed the study. SE, MK did the literature search. MK, LM, SE carried out data acquisition. MM, SE analysed data. SE, DAJ wrote the first draft of the manuscript. All authors contributed to the interpretation of the data and writing of the manuscript and approved the final version of the manuscript.
This research received no specific grant from any funding agency.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Aziz H, Rhee P, Pandit V, Tang A, Gries L, Joseph B. The current concepts in management of animal (dog, cat, snake, scorpion) and human bite wounds. J Trauma Acute Care Surg. 2015 Mar;78(3):641–8. 10.1097/TA.0000000000000531
2. Dendle C, Looke D. Review article: Animal bites: an update for management with a focus on infections. Emerg Med Australas. 2008 Dec;20(6):458–67.
3. Jaindl M, Oberleitner G, Endler G, Thallinger C, Kovar FM. Management of bite wounds in children and adults-an analysis of over 5000 cases at a level I trauma centre. Wien Klin Wochenschr. 2016 May;128(9-10):367–75. 10.1007/s00508-015-0900-x
4. Rothe K, Tsokos M, Handrick W. Animal and Human Bite Wounds. Dtsch Arztebl Int. 2015 Jun;112(25):433–42.
5. Frey J, Mindekem R, Kessely H, Doumagoum Moto D, Naïssengar S, Zinsstag J, et al. Survey of animal bite injuries and their management for an estimate of human rabies deaths in N’Djaména, Chad. Trop Med Int Health. 2013 Dec;18(12):1555–62. 10.1111/tmi.12202
6. Wiley JF 2nd. Mammalian bites. Review of evaluation and management. Clin Pediatr (Phila). 1990 May;29(5):283–7. 10.1177/000992289002900506
7. Goldstein EJ. Bite wounds and infection. Clin Infect Dis. 1992 Mar;14(3):633–8. 10.1093/clinids/14.3.633
8. Ostanello F, Gherardi A, Caprioli A, La Placa L, Passini A, Prosperi S. Incidence of injuries caused by dogs and cats treated in emergency departments in a major Italian city. Emerg Med J. 2005 Apr;22(4):260–2. 10.1136/emj.2004.014886
9. Morosetti G, Toson M, Piffer C. Lesions caused by animals in the Autonomous Province of South Tyrol in 2010: fact-finding for prevention. Vet Ital. 2013;49(1):37–50.
10. Bregman B, Slavinski S. Using emergency department data to conduct dog and animal bite surveillance in New York City, 2003-2006. Public Health Rep. 2012;127(2):195–201. 10.1177/003335491212700208
11. Tabbara M, Hatzigianni P, Fux C, Zimmermann H, Exadaktylos AK. Human bite wounds: a swiss emergency department experience. Wounds. 2012 Apr;24(4):85–90.
12. Griego RD, Rosen T, Orengo IF, Wolf JE. Dog, cat, and human bites: a review. J Am Acad Dermatol. 1995 Dec;33(6):1019–29. 10.1016/0190-9622(95)90296-1
13. Stefanopoulos PK, Tarantzopoulou AD. Facial bite wounds: management update. Int J Oral Maxillofac Surg. 2005 Jul;34(5):464–72. 10.1016/j.ijom.2005.04.001
14. Conlon HA. Human bites in the classroom: incidence, treatment, and complications. J Sch Nurs. 2007 Aug;23(4):197–201. 10.1177/10598405070230040301
15. Matter HC, Sentinella Arbeitsgemeinschaft. The epidemiology of bite and scratch injuries by vertebrate animals in Switzerland. Eur J Epidemiol. 1998 Jul;14(5):483–90. 10.1023/A:1007460213308
16. Rueff F, Bedacht R, Schury G. [Bite injury. Special situation as to clinical aspects, therapy and course of healing]. Med Welt. 1967 Mar;12:663–8.
17. Ting JW, Yue BY, Tang HH, Rizzitelli A, Shayan R, Raiola F, et al. Emergency department presentations with mammalian bite injuries: risk factors for admission and surgery. Med J Aust. 2016;204(3):114 e1-7. 10.5694/mja15.00653
18. Pfortmueller CA, Efeoglou A, Furrer H, Exadaktylos AK. Dog bite injuries: primary and secondary emergency department presentations—a retrospective cohort study. ScientificWorldJournal. 2013 Sep;2013:393176. 10.1155/2013/393176
19. Freshwater A. Why your housecat’s trite little bite could cause you quite a fright: a study of domestic felines on the occurrence and antibiotic susceptibility of Pasteurella multocida. Zoonoses Public Health. 2008 Oct;55(8-10):507–13. 10.1111/j.1863-2378.2008.01152.x
20. Kennedy SA, Stoll LE, Lauder AS. Human and other mammalian bite injuries of the hand: evaluation and management. J Am Acad Orthop Surg. 2015 Jan;23(1):47–57. 10.5435/JAAOS-23-01-47
21. Benson LS, Edwards SL, Schiff AP, Williams CS, Visotsky JL. Dog and cat bites to the hand: treatment and cost assessment. J Hand Surg Am. 2006 Mar;31(3):468–73. 10.1016/j.jhsa.2005.12.011
22. Pomares G, Huguet S, Dap F, Dautel G. Contaminated wounds: effectiveness of debridement for reducing bacterial load. Hand Surg Rehabil. 2016 Sep;35(4):266–70. 10.1016/j.hansur.2016.06.001
23. Norton C. Animal and human bites. Emerg Nurse. 2008 Oct;16(6):26–9. 10.7748/en2008.10.16.6.26.c6781
24. Brook I. Management of human and animal bite wound infection: an overview. Curr Infect Dis Rep. 2009 Sep;11(5):389–95. 10.1007/s11908-009-0055-x
25. Esposito S, Picciolli I, Semino M, Principi N. Dog and cat bite-associated infections in children. Eur J Clin Microbiol Infect Dis. 2013 Aug;32(8):971–6. 10.1007/s10096-013-1840-x
26. Myers JP. Bite Wound Infections. Curr Infect Dis Rep. 2003 Oct;5(5):416–25. 10.1007/s11908-003-0022-x
27. Stierman KL, Lloyd KM, De Luca-Pytell DM, Phillips LG, Calhoun KH. Treatment and outcome of human bites in the head and neck. Otolaryngol Head Neck Surg. 2003 Jun;128(6):795–801. 10.1016/S0194-59980300254-7
28. Medeiros I, Saconato H. Antibiotic prophylaxis for mammalian bites. Cochrane Database Syst Rev. 2001;(2):CD001738.
29. Rittner AV, Fitzpatrick K, Corfield A. Best evidence topic report. Are antibiotics indicated following human bites? Emerg Med J. 2005 Sep;22(9):654. 10.1136/emj.2005.028662
30. Henton J, Jain A. Cochrane corner: antibiotic prophylaxis for mammalian bites (intervention review). J Hand Surg Eur Vol. 2012 Oct;37(8):804–6. 10.1177/1753193412452204