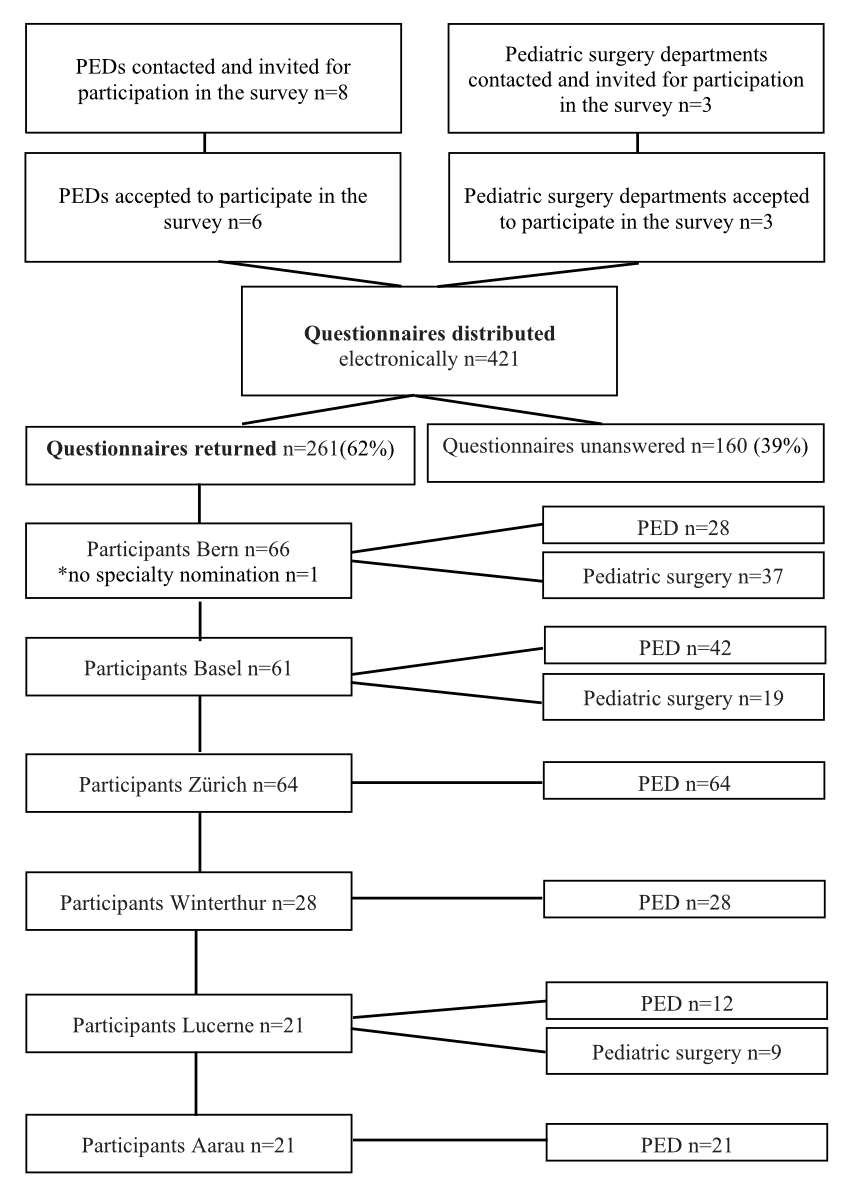
Figure 1 Participant selection chart.
DOI: https://doi.org/10.57187/smw.2023.40017
Prevention and detection of child abuse and family violence is paramount to prevent further harm to children [1–4]. However, despite a legal, ethical, and moral responsibility of health care providers (HCPs) to recognise and report child abuse and neglect (CAN), insufficient levels of awareness and skills among medical and nursing staff working with children often lead to under-detection and under-reporting of victims [1, 5, 6]. Maltreatment of children is a serious global public health concern, with incidence rates at emergency departments (EDs) in the U.S. of 23.1 per 1000 children [7], 30 per 1000 children in the Netherlands [8], 1656 reported cases per 1.74 million children in Switzerland [9], and over 700 annual deaths in children under 15 years of age in the European World Health Organization region [10]. Only 5% of child maltreatment cases are reported to child protection services (CPS) [11]. The number of unknown or unreported cases is likely much higher as most criminal offenses occur within the family, and child victims often are too young to ask for help [6]. Interventions to improve detection rates are heterogenous and include screening tools, mandatory staff education, interdisciplinary child protection team development, standardised documentation, and referral pathways in the ED; however, these interventions are used inconsistently [6]. Although excellent skills are of utmost importance for early detection of child abuse, specific child maltreatment education is not yet a mandatory part of pre- or postgraduate academic curricula in Switzerland and many European countries [12, 13]. With a small investment of time, the confidence in one's ability to detect child maltreatment could be markedly increased [14, 15]. In many cases, paediatric emergency departments (PEDs) and paediatric surgery departments are the first place of contact with the health care system for child abuse victims and their parents or caregivers.
There is a knowledge gap regarding provider-reported barriers and facilitators to detecting and reporting child abuse in PED and paediatric surgery settings in Switzerland. Evidence in the current literature mostly stems from nurses, family/paediatric nursing practitioners, midwives, or physicians working with children in general EDs. The published evidence stems from survey studies (n = 185, Israel [16]; n = 182, U.S. [17]), self-reported data collection methods (n = 145, Saudi Arabia [18]), literature reviews [1, 19], or semi-structured interviews (n = 29, U.S. [20]).
We aimed to examine nurses’ and physicians’ beliefs regarding the obstacles and enablers to recognising and reporting child abuse in Swiss PEDs and on paediatric surgical wards using an online survey. We hypothesised that our results, in a culturally different setting, without mandatory child protection education, would vary from previous studies [16, 20]. Based on our results, we aimed to create a recognition aid tool to facilitate and improve the detection and reporting of child abuse.
An observational, cross-sectional, multicentre, survey-based study was conducted in three tertiary PEDs (Bern, Basel, Zurich), three rural PEDs (Winterthur, Lucerne, Aarau), and three tertiary paediatric surgery departments (Bern, Basel, Lucerne) in German-speaking Switzerland.
For the selection of potential participants, the department heads of eight paediatric institutions (with a PED and/or paediatric surgery department) in German-speaking Switzerland were approached for participation in the survey. Once the participation of the department was confirmed, a departmental E-mail contact list for nursing and medical staff was obtained from the department secretary for electronic distribution of the survey. Participation in the survey was encouraged and promoted by MB through on-site presentations of the study purpose and electronic information sent together with the survey.
To calculate the sample size, we estimated the size of the entire population of nursing and medical staff working in PEDs and paediatric surgery departments in the German-speaking part of Switzerland (approximately 255 physicians and 510 nurses). We then selected a convenience sample using a non-probability design (due to the declined participation in the survey of a subset of institutions) to achieve a final sample size of 382, representing approximately 50% of the relevant population. A total of 421 nurses (except from Lucerne paediatric surgery department) and physicians employed by the participating institutions were surveyed via an online questionnaire between February 1, 2017, and August 31, 2017 (figure 1).
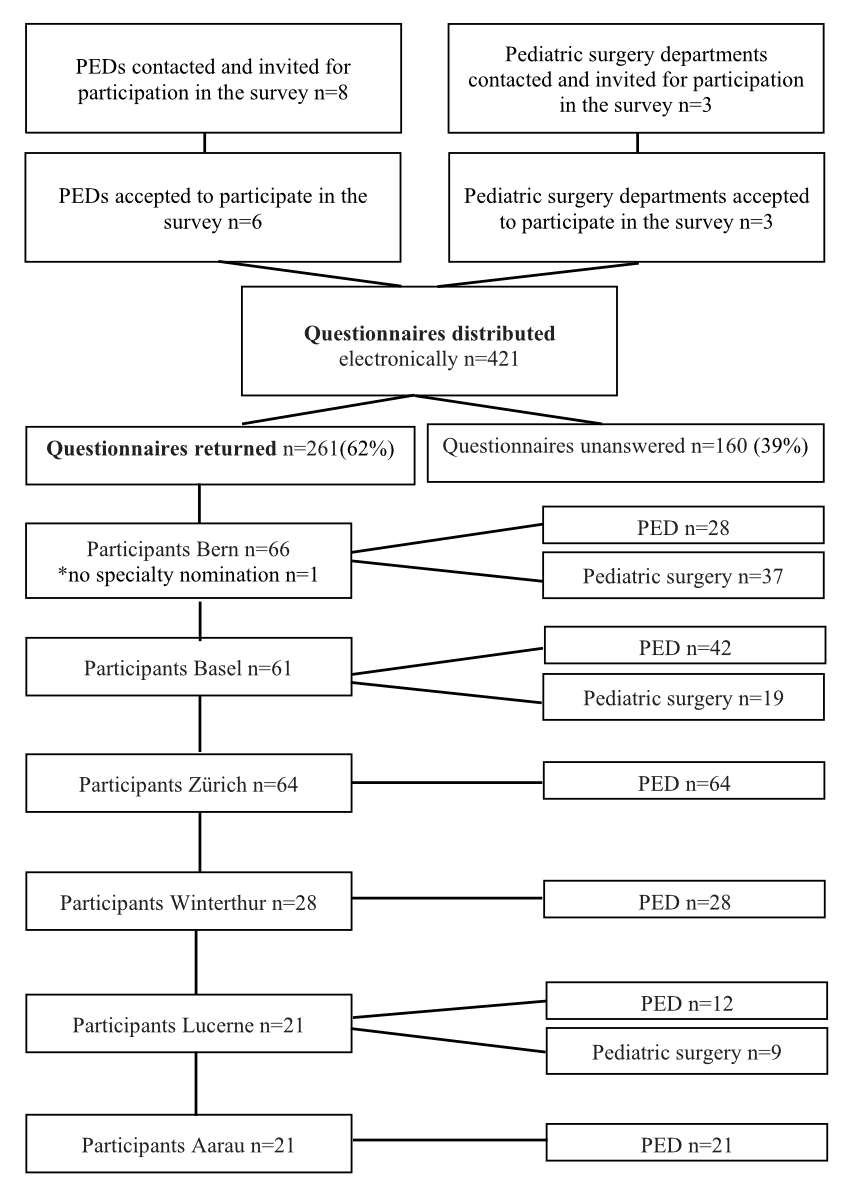
Figure 1 Participant selection chart.
A survey that measures nurses’ and physicians’ difficulties and enablers to recognising and reporting child abuse in our setting was not readily available; therefore, we decided to create our own survey that was applicable to our setting.
We modified the Delphi technique to establish a structured questionnaire exploring nurses’ and physicians’ difficulties and enablers to recognising and reporting child abuse. A two-round feedback process was used to capture the collective opinion of suitable experts [21].
RML drafted the first version of the questionnaire based on the literature, expert knowledge, and expert discussions. The first draft was composed of closed-end, drop-down questions including the answer option “other” where participants could provide an answer in their own words if none of the other options applied, multiple choice questions, yes-or-no questions in part with an open-ended answer option, and Likert scale questions with 1 representing “extremely/very” (e.g., competent), 2 “rather” (e.g., competent), 3 “neither” (e.g., competent nor incompetent, neutral), 4 “rather” (e.g., incompetent), and 5 “extremely/very” (incompetent). All feedback rounds were conducted iteratively through consultation and feedback. In the first round, recourse was taken to feedback from a group of experts (two senior PED nurses, one PED consultant, one consultant paediatric surgeon and member of CPS at the University Hospital, Inselspital Bern). To collect the experts’ feedback, we used open-ended questions with the scope of prioritising the most relevant survey questions and topics for recognition of child abuse.
All the participating stakeholders were invited by e-mail to complete the questionnaire. They were asked to comment on the content, comprehensibility, grammar/spelling, completeness, and relevance of the survey items to suggest changes or decide whether the items should be included in the final competence list. This also included checking that the survey did not contain confusing, leading, nested, or double-barrelled questions. The face validity of the survey was established during the first feedback round, where experts read the questionnaire and evaluated whether the questions effectively captured the topic under investigation. After completing the first round, the facilitator (RML) read all the answers to the open-ended questions, edited, merged similar answers/suggestions, and grouped them into categories to compile the second-round questionnaire. In the second feedback round, the edited version was pilot tested by four population-based participants who were invited by E-mail. The pilot data from their answers in this edited version was checked for consistency with the questions. Items included in the questionnaire were again re-piloted, and final edits were made based on the answers received. At the end of the second round, consensus was reached, resulting in the final 19-item version of the survey. The survey covers the following domains: recognition of CAN, reporting of CAN, support resources, confidence in recognition and approaching the child and the family, and child abuse education. The original questionnaire was written in German (available from the authors upon request) and was translated to English for the purpose of publication (table 1). The final online version was again pilot tested for ease of completion and technical functioning by MB to confirm its comprehensibility and the usefulness of the response options.
Table 1Questionnaire “Nurses’ and physicians’ difficulties and enablers to recognising and reporting child abuse.”
| No | Question | Response options |
| 1 | What is your gender? | Female |
| Male | ||
| 2 | How old are you (in years)? | <20 |
| 20–30 | ||
| 31–40 | ||
| 41–50 | ||
| 51–60 | ||
| >60 | ||
| 3 | What is your level of training? | Medical student |
| Medical trainee | ||
| With specialist certificate | ||
| Without specialist certificate | ||
| Consultant | ||
| With specialist certificate | ||
| Without specialist certificate | ||
| Senior Consultant | ||
| Medical director/head of department | ||
| Nursing assistant | ||
| Health care assistant (German FaGe*) in training | ||
| Health care assistant (German FaGe*) | ||
| Nursing student | ||
| Registered nurse | ||
| Other (please describe) | ||
| 4 | In which department do you work? | Paediatric emergency department (PED) |
| Paediatric surgery department | ||
| 5 | How long have you been working in the PED and/or in paediatric surgery department? | <1 year |
| 1–3 years | ||
| >3 years | ||
| 6 | What forms of child abuse have you encountered (at and outside the workplace)? (Multiple answers possible) | Physical abuse |
| Emotional abuse | ||
| Sexual abuse | ||
| Neglect (emotional and/or physical) | ||
| Munchhausen by proxy | ||
| None | ||
| 7 | How confident do you feel about recognising child abuse in the PED or in the paediatric surgery department? | Very confident |
| Rather confident | ||
| Neither confident nor unconfident | ||
| Rather unconfident | ||
| Very unconfident | ||
| 8 | If you chose “rather unconfident” or “very unconfident” in Question 7, why did you choose this answer? (Multiple answers possible) | Lack of experience |
| Respect for taboo topic | ||
| Difficulty to distinguish between accidental and non-accidental events | ||
| Other (please describe) | ||
| 9 | In your clinical role, when do you report a suspicion of child abuse? (Multiple answers possible) | When I am sure that child abuse is the correct diagnosis |
| When I suspect child maltreatment | ||
| When I am considering child abuse as a possible diagnosis | ||
| Other (please describe) | ||
| 10 | What do you do if you suspect child abuse? (Multiple answers possible) | I inform a colleague who is at the same level of training as myself |
| I inform the consultant on call | ||
| I inform the child protection services of my hospital | ||
| 11 | Do you know whether there are child protection services at your hospital? | Yes |
| No | ||
| 12 | How often have you suspected a case of child abuse in the PED or on the surgical ward in the last 12 months? | Never |
| Once | ||
| Twice | ||
| Three times | ||
| Four times | ||
| Other (please describe) | ||
| 13 | How often have you suspectedand reported a case of child abuse in the PED or on the surgical ward in the last 12 months? | Never |
| Once | ||
| Twice | ||
| Three times | ||
| Four times | ||
| Other (please describe) | ||
| 14 | If you did not report all your suspected cases, what was the reason? (Multiple answers possible) | Uncertainty of whether it was really child abuse |
| Lack of time for reporting | ||
| Uncertainty of whether my report has any consequences or leads to investigation | ||
| Protection of the child and their family | ||
| I felt that it is not my responsibility | ||
| I forgot to report | ||
| Other (please describe) | ||
| 15 | What made you report a suspicion of child abuse? (Multiple answers possible) | Discovery of physical injuries (e.g., stocking-like scalding patterns, injuries to back and buttocks) |
| Ambiguous history (e.g., injury cannot be explained by the psychomotor development of the child, different statements by different relatives/caregivers) | ||
| Expressed suspicion of a parent/relative | ||
| Suspicious behaviour of the child | ||
| Suspicious behaviour of a parent/caregiver | ||
| Repeated hospital presentations with suspicious injuries, history, or behaviour | ||
| Referral with suspicion of child abuse | ||
| Other (please describe) | ||
| 16 | If you suspected child abuse, how competent did you feel addressing the child/parents/relatives with the suspicion? | Extremely competent |
| Rather competent | ||
| Neither competent nor incompetent | ||
| Rather incompetent | ||
| Extremely incompetent | ||
| 17 | Would you like to know more about how to recognise child abuse? | Yes |
| No | ||
| If yes, which format would you prefer? (Multiple answers possible) | ||
| Leaflet | ||
| Staff education | ||
| E-learning programme | ||
| Other (please describe) | ||
| 18 | Would you like to have access to a standardised questionnaire and/or documentation form as a support for dealing with suspected child abuse the next time you are confronted with a suspicious situation? | Yes |
| No | ||
| 19 | Do you have ideas/proposals for the improvement of detection and/or reporting of child abuse in the PED or on the surgical ward? | Yes (please specify here) |
| No |
FaGe* = Fachangestellte/r Gesundheit = Nursing assistant profession in Switzerland, usually subordinated to qualified nursing professionals.
The survey was anonymous. We used the online tool SurveyMonkey® (SurveyMonkey Inc., San Mateo, California, USA) [22] for electronic distribution of the questionnaire. Both fully and partially completed surveys were included for analysis.
Primary outcome: Frequency (in absolute numbers and percentage) of obstacles and enablers to recognising and reporting child abuse over a 12-month period.
Secondary outcomes:a) Number of suspected versus reported child abuse cases over the last 12 months, b) frequency of drivers for and action taken when reporting child abuse, c) level of confidence in the communication with the family, d) interest in gaining more knowledge about child abuse, and e) interest in the availability of standardised questions and documentation forms when encountering child abuse on a 5-point Likert scale, respectively (c-e).
SPSS 25 and Excel were used for data analysis. Categorical variables are presented as frequencies and percentages. The Chi-squared test was used to determine whether there were statistically significant differences between the observed frequencies in various categorical variables or participants. Statistical significance was defined as p <0.05. Missing, conflicting, or ambiguous answers were coded as missing data. Analysis of the available data was performed to minimise bias from missing data. In the tables, we report solely valid percentages, (i.e., each reported analysis is accompanied by the actual number of subjects included in that analysis). Participants with a missing value for each question did not contribute to the analysis of that question. Ambiguous and conflicting answers were excluded from the analysis and were treated as missing data.
We performed qualitative analysis of this small set of qualitative data using content analysis. The data from the participants’ descriptions in their own words were categorised into consistent groups (e.g., “someone else reported it” and “it was already reported”) and were accounted for in tables (e.g., table 5) or summarised in the explanatory text following the tables.
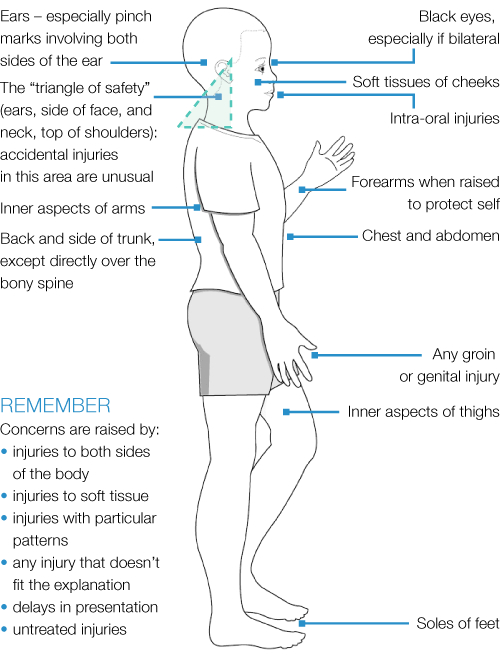
We aimed to design a comprehensive decision aid pocket card to support staff in the detection of child abuse in the ED. MB and RML drafted the first version of this tool containing six parts that were based on validated tools or published evidence. Experts from the CPS at Astrid Lindgren’s Children’s Hospital, Sweden were invited by e-mail to review the first draft and comment on the content, comprehensibility, grammar/spelling, completeness, and relevance of the survey items to suggest changes or decide whether the items should be included in the final version. After reception of the review comments, the facilitator (RML) reviewed the comments, edited, merged similar answers/suggestions, and compiled the current version. Consensus was reached on all items except for the “Typical locations for accidental and non-accidental injuries’ item, which the authors decided not to replace with the other suggested items (e.g., TEN-4-FACESp, a validated tool to help screen children under 4 years of age with bruising to differentiate accidental from non-accidental injury [23]). The final version of the tool comprised six parts (see appendix): 1) six screening questions adapted from the validated ESCAPE instrument [24] to be used in case of suspected CAN or for the implementation of a general screening in the ED, 2) alarming clinical/behavioural findings of abuse/neglect within the context of the history [25], 3) child and 4) family factors that increase vulnerability to CAN, 5) typical locations for accidental and non-accidental injuries [26], and 6) suggested consensus and experience-based example questions for approaching the child and their family for suspected child abuse. We found this especially useful to respond to the expressed (emotional) challenge of approaching the child and their family in case of suspected CAN and to facilitate a possible entry point for the conversation that could save a life. TEN-4-FACESp is listed and referenced as an additional resource for use in children under 4 years of age [23]. Written permission was obtained for reproduction of the “Typical locations for accidental and non-accidental injuries” figure from the original authors. We encourage users to insert the contact details of local CPS and a link to the local hospital CAN reporting policy, as this may vary widely between hospitals.
The Ethics Committee of the Children's Hospital, Inselspital, waived ethical approval for this type of survey study. A study protocol was not required for this study and was not prepared.
Overall, 261/421 employees from paediatric emergency medicine and paediatric surgery departments of six different hospitals returned the survey (62% response rate) (figure 1). All questionnaires were included for analysis whether fully or partially completed: completed, n = 200 (76.6%); incomplete, n = 61 (of which two-thirds [n = 40] only had 1–2 missing answers, n = 3 had 3, n = 2 had 4, n = 1 had 8, n = 7 had 10, n = 6 had 11, and n = 2 had 14 missing answers). The data presented in this paper represent the results from the pilot survey on our intended respondents (n = 261). Participant demographics are described in table 2. The participants were mostly females (n = 202/254, 79.5%); they included registered nurses (n = 150/256, 58.6%) and medical trainees without specialist certificate (n = 45/257, 17.5%).
Table 2Participant demographics.
| Overall respondents n (%) | Paediatric emergency department (PED)* n (%) | Paediatric surgery* n (%) | |
| Hospital | n = 261/261 (100) | n = 195/260 (75) | n = 65/260 (25) |
| Bern (University hospital) | 66/261 (25.3) | 28/195 (14.4) | 37/65 (56.9) |
| Basel (University hospital) | 61/261 (23.4) | 42/195 (21.5) | 19/65 (29.2) |
| Zurich (University hospital) | 64/261 (24.5) | 64/195 (32.8) | 0/65 (0) |
| Winterthur (Teaching hospital) | 28/261 (10.7) | 28/195 (14.4) | 0/65 (0) |
| Lucerne (Teaching hospital) | 21/261 (8.0) | 12/195 (6.2) | 9/65 (13.8) |
| Aarau (Teaching hospital) | 21/261 (8.0) | 21/195 (10.7) | 0/65 (0) |
| Gender, n (%) | n = 254/261 (97.3) | n = 191/195 (97.9) | n = 62/65 (95.4) |
| Female | 202/254 (79.5) | 157/191 (82.2) | 45/62 (72.6) |
| Male | 52/254 (20.5) | 34/191 (17.8) | 17/62 (27.4) |
| Missing | 7/261 | 4/195 | 3/65 |
| Age, n (%) | n = 255/261 (97.7) | n = 192/195 (98.5) | n = 62/65 (95.4) |
| <20 years | 4/255 (1.6) | 1/192 (0.5) | 3/62 (4.8) |
| 20–30 years | 74/255 (29) | 53/192 (27.6) | 21/62 (33.9) |
| 30–40 years | 90/255 (35.3) | 77/192 (40.1) | 12/62 (19.4) |
| 41–50 years | 54/255 (21.2) | 39/192 (20.3) | 15/62 (24.2) |
| 51–60 years | 22/255 (8.6) | 16/192 (8.3) | 6/62 (9.7) |
| >60 years | 11/255 (4.3) | 6/192 (3.1) | 5/62 (8.1) |
| Missing | 6/261 | 3/195 | 3/65 |
| Professional group, n (%) | n = 256/261 (98.1) | n = 192/195 (98.5) | n = 64/65 (98.5) |
| Nurse | 150/256 (58.6) | 113/192 (58.9) | 37/64 (57.8) |
| Physician | 106/256 (41.4) | 79/192 (41.1) | 27/64 (42.2) |
| Registered psychologist | 1/256 (0.4) | ||
| Missing | 4/261 | 3/195 | 1/65 |
| Level of training, n (%) | n = 257/261 (98.5) | n = 192/195 (98.5) | n = 64/65 (98.5) |
| Medical profession | |||
| Medical student | 1/257 (0.4) | 1/192 (0.5) | 0/64 (0) |
| Medical trainee without specialist certificate | 45/257 (17.5) | 33/192 (17.2) | 12/64 (18.8) |
| Medical trainee with specialist certificate | 6/257 (2.3) | 5/192 (2.6) | 1/64 (1.6) |
| Junior consultant without specialist certificate | 5/257 (1.9) | 3/192 (1.6) | 2/64 (3.1) |
| Consultant with specialist certificate | 37/257 (14.4) | 30/192 (15.6) | 7/64 (10.9) |
| Senior consultant | 10/257 (3.9) | 6/192 (3.1) | 4/64 (6.25) |
| Medical director/head of department | 2/257 (0.8) | 1/192 (0.5) | 1/64 (1.6) |
| Nursing profession | |||
| Nursing assistant | 3/257 (1.2) | 0/192 (0) | 3/64 (4.7) |
| Nursing student | 1/257 (0.4) | 1/192 (0.5) | 0/64 (0) |
| Registered nurse | 140/257 (54.5) | 109/192 (56.8) | 31/64 (48.4) |
| Health care assistant** student | 1/257 (0.4) | 0/192 (0) | 1/64 (1.6) |
| Health care assistant** | 5/257 (1.9) | 3/192 (1.6) | 2/64 (3.1) |
| Other profession | |||
| Registered psychologist | 1/257 (0.4) | ||
| Missing | 4/261 | 3/195 | 1/65 |
| Work experience, n (%) | n = 260/261 (99.6) | n = 195/195 (100) | n = 65/65 (100) |
| <1 year | 53/260 (20.4) | 44/195 (22.6) | 9/65 (13.8) |
| 1–3 years | 59/260 (22.7) | 48/195 (24.6) | 11/65 (16.9) |
| >3 years | 148/260 (56.9) | 103/195 (52.8) | 45/65 (69.2) |
| Missing (psychologist participant) | 1/261 | 0/195 | 0/65 |
| Previous confrontation with child abuse at or outside work (multiple answers were possible) | n = 250/261 (95.8) | n = 190/195 (97.4) | n = 59/65 (90.8) |
| Physical abuse | 235/250 (94) | 183/190 (96.3) | 52/59 (88.1) |
| Neglect | 216/250 (86.4) | 167190 (87.9) | 49/59 (83.1) |
| Emotional abuse | 169/250 (67.6) | 137/190 (72.1) | 32/59 (54.2) |
| Sexual abuse | 153/250 (61.2) | 134190 (70.5) | 19/59 (32.2) |
| Munchhausen by proxy syndrome | 115/250 (46) | 91/190 (47.9) | 24/59 (40.7) |
| None | 11/261 (4.2) | 5/195 (2.6) | 6/65 (9.2) |
| Missing (psychologist participant) | 1/261 | 0/195 | 0/65 |
PED = Paediatric emergency department. * Missing specialty nomination n = 1, ** FaGe (German: Fachangestellte/r Gesundheit) is a nursing assistant profession in Switzerland, usually subordinated to qualified nursing professionals.
In this sample, 82.9% (203/245) of participants suspected CAN during the 12-month period investigated in this survey (total answers n = 245, missing n = 15) (table 3), and 95.8% (n = 250/261) had been previously confronted with a child abuse case (table 2). Although this sub-sample did not include all participants, it allowed us to obtain sufficient valid data.
PED staff (n = 153/188, 81.4%) more frequently reported child abuse than paediatric surgeons (n = 32/57, 56.1%) (p = 0.0001); likewise, paediatric surgeons (n = 25/57, 43.9%) “never reported” child abuse significantly more often than paediatric emergency physicians (n = 35/188, 18.6%) (p = 0.0001) (figure 2).
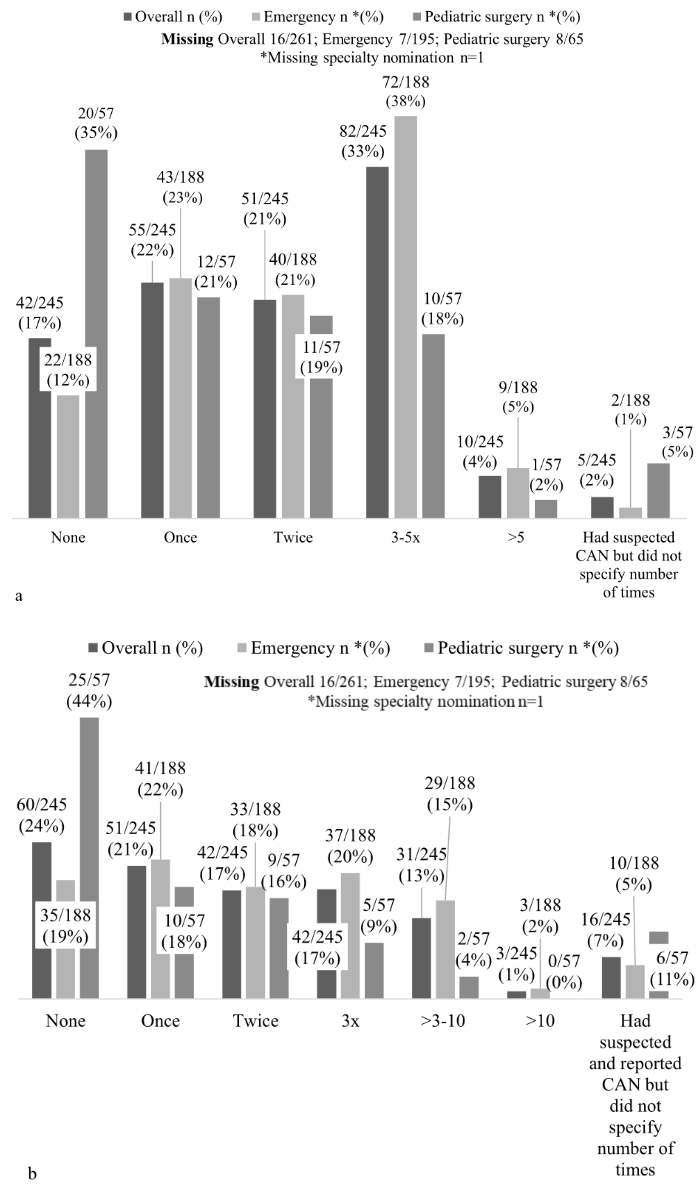
Figure 2 Overall suspected and reported child abuse and neglect and by profession (paediatric emergency and paediatric surgery).
* Missing specialty nomination n = 1
Interestingly, we found a discrepancy between the number of suspicions and reports of CAN in 44/245 (18%) respondents, with a preponderance of suspicions (on average 2.9 suspected versus 1.1 reported cases) and various acknowledged reasons for not reporting a suspicion; the most common rationale being uncertainty as to whether child abuse was the correct diagnosis (n = 21/44, 47.7%) (figure 2).
Table 3Number of suspected child abuse cases over the last 12 months and reasons for not reporting suspected child abuse.
| Occasions of suspecting but not reporting child abuse over the last 12 months (n = 44) | n (%) |
| Once | 13/44 (29.5) |
| Twice | 15/44 (28.9) |
| Three times | 4/44 (8.9) |
| Four times | 6/44 (13.3) |
| Five times or more | 6/44 (13.3) |
| Reasons for not reporting child abuse cases, indicated by respondents who suspected more cases than they reported (n = 44) | n (%) |
| Uncertainty of whether child abuse was the correct diagnosis | 21/42 (50) |
| Not my task/someone else reported it | 9/42 (21.4) |
| Reported to the senior consultant, who decided differently/unsure whether it was subsequently reported | 5/42 (11.9) |
| Uncertainty of whether the report has any consequences/causes investigation | 4/42 (9.5) |
| Lack of time | 3/42 (7.1) |
| Missing | 2/44 |
| Hypothetical reasons for not reporting child abuse cases, indicated by those who reported all their suspicions; more than one answer was possible (n = 80) | n (%) |
| Uncertainty of whether child abuse was the correct diagnosis | 58/76 (76.3) |
| Lack of time | 4/76 (5.3) |
| Concern about potential consequences for the patient or the staff | 5/76 (6.6) |
| Not my task/someone else reported it | 28/76 (36.8) |
| Parental protection | 2/76 (2.6) |
| Forgotten to report | 2/76 (2.6) |
| Missing | 4/80 |
Considering the reasons for not reporting suspected child abuse (table 3), we can assume that in a further 11/44 cases, the suspicion was eventually reported (e.g., “someone else reported it”, “it was already reported”, or “reported to the consultant”). One response was excluded from the analysis as the ratio of suspected and reported to suspected cases was inappropriate, most likely due to misunderstanding of the question (the respondent stated that she had reported all her suspicions in the end). The characteristics of the remaining 33/245 (13.5%) respondents with diverging answers are detailed in table 4. Significantly more females than males (p = 0.039) and significantly more nurses than physicians (p = 0.005) indicated higher numbers of CAN suspicions than reports. Likewise, staff with longer work experience were less likely to report initially suspected CAN than staff with less work experience (p = 0.008). Furthermore, CAN was reported more often at university hospitals (n = 184/100 respondents) than smaller teaching hospitals (n = 168/100 respondents). The average number of reported cases per person ranged from 1.3 to 2.5 in the different hospitals.
Table 4Characteristics of participants with a discrepancy in the number of suspected versus reported child abuse cases.
| Characteristics (n = 33) | n (%) | ||
| Sex | Male | 2/32 (6.3) | p = 0.039 |
| Female | 30/32 (93.8) | ||
| Missing | 1/33 | ||
| Profession | Health care assistant | 2/33 (6.1) | p = 0.005 |
| Registered nurse | 25/33 (75.8) | ||
| Physician | 6/33 (18.2) (junior medical trainee without specialist certificate: n = 2; junior medical trainee with specialist certificate: n = 1; consultant without specialist certificate: n = 1; consultant with specialist certificate: n = 2) | ||
| Age (years) | <20 | 0/33 (0) | p = 0.452 |
| 20–30 | 12/33 (36.4) | ||
| 31–40 | 13/33 (39.4) | ||
| 41–50 | 3/33 (9.1) | ||
| 51–60 | 4/33 (12.1) | ||
| >60 | 1/33 (3.0) | ||
| Work experience (years) | <1 | 1/33 (3.0) | p = 0.008 |
| 1–3 | 13/33 (39.4) | ||
| >3 | 19/33 (57.6) | ||
| Discipline | Emergency | 26/33 (78.8) | p = 0.798 |
| Surgical ward | 7/33 (21.2) | ||
Triggers to report a suspicion of child abuse are depicted in figure 3.
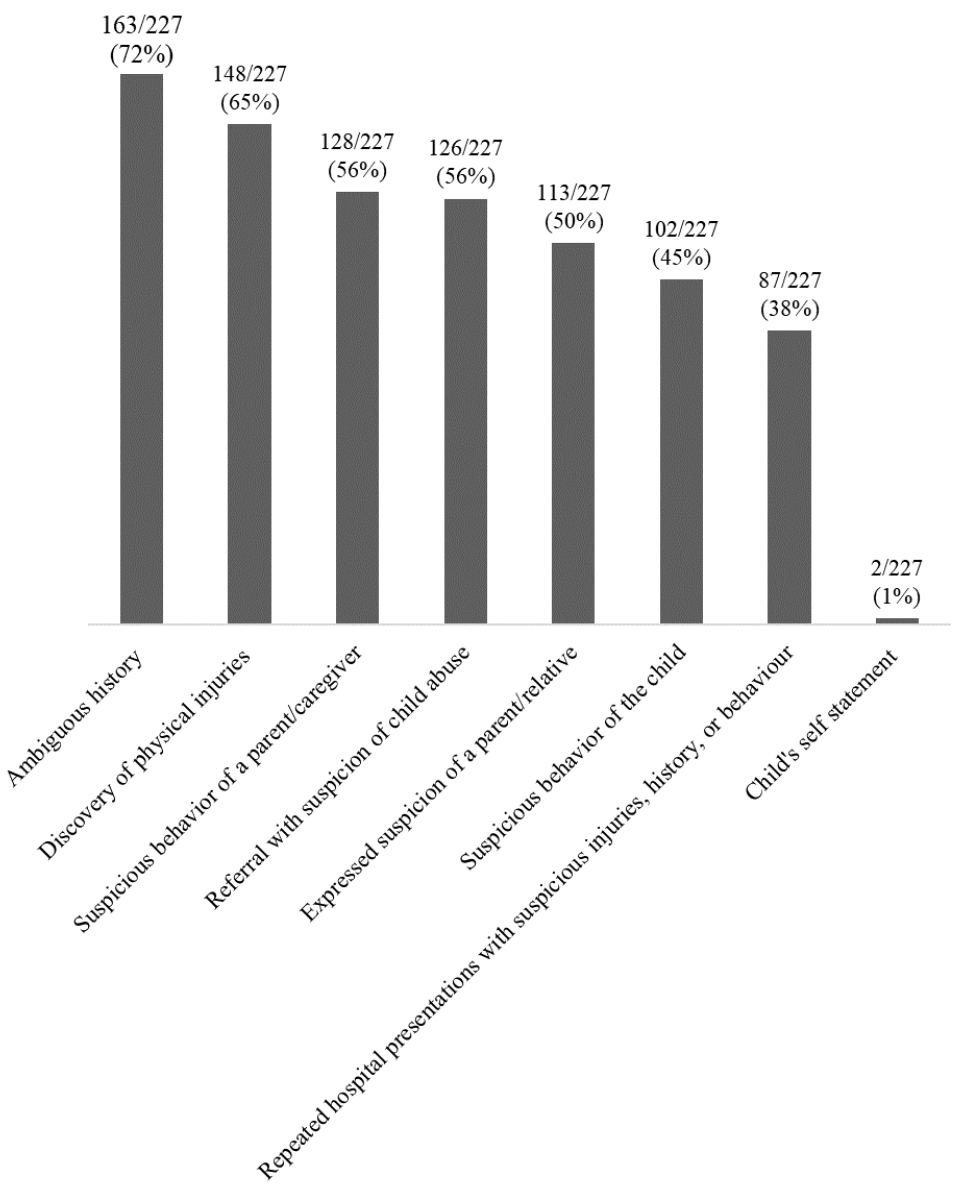
Figure 3 Triggers for paediatric emergency or paediatric surgery staff to report suspected child abuse (more than one answer was possible, so the percentages do not sum up to 100).
Self-reported barriers and enablers for the recognition and reporting of CAN, person informed about the suspected child abuse, and preferred educational tools for child abuse education are listed in table 5.
Table 5Self-reported barriers and enablers of the detection and reporting of child abuse, the person informed about the suspected child abuse, and the preferred educational tool for child abuse education.
| Barriers to the recognition of CAN (n = 64) (question 8) | n (%) | |
| Lack of exposure/experience | 34/64 (53.1) | |
| Difficulty distinguishing between accidental and non-accidental events | 26/64 (40.6) | |
| Respect for a taboo topic | 3/64 (4.7) | |
| Lack of transparency of the reporting process | 1/64 (1.6) | |
| Missing | 5/69 | |
| Obstacles to reporting CAN (n = 80) | ||
| Doubts about the diagnosis | 58/80 (72.5) | |
| Feeling unaccountable for notification | 28/80 (35) | |
| Uncertainty of whether reporting has any consequence | 5/80 (6.25) | |
| Lack of time | 4/80 (5) | |
| Forgetting to report | 2/80 (2.5) | |
| Parental protection | 2/80 (2.5) | |
| Unspecific answer | 4/80 (5) | |
| Enablersfor the of CAN (n = 245/261) (question 9) | n (%) | |
| Suspicion of child maltreatment | 127/245 (51.8) | |
| Child abuse was a differential diagnosis | 115/245 (46.9) | |
| Certainty about the diagnosis | 3/245 (1.2) | |
| Self-reported enablers for the of CAN (n = 53/261) (open-ended question 19) | n (%) | |
| Mandatory child protection (refresher) courses | 16/52 (30.7) | |
| Encouragement of low thresholds to express and report suspicions | 7/52 (13.5) | |
| Implementation of clearly defined clinical practice guideline for the reporting of child abuse for medical and nursing staff, including but not limited to: | Catalogue of questions and standardised documentation form to be used in case of suspicion | 6/52 (11.5) |
| Flowcharts | 3/52 (5.8) | |
| Mandatory full-body examination and documentation in case of suspicion | 1/52 (1.9) | |
| Standardised handling of suspicions expressed by team members regardless of hierarchical position | 2/52 (3.8) | |
| Improvement of child protection services resources: | Implementation of a 24/7 on-call roster for child protection services | 4/52 (7.7) |
| Mandatory feedback by child protection services to the reporting staff member for each case for training purposes | 2/52 (3.8) | |
| Standardised involvement of child protection services for specific diagnoses (e.g., fractures incompatible with developmental age) | 1/52 (1.9) | |
| Teaching facilitated by forensic medicine and psychology specialtiesImplementation of complementary forensic nursing training | 3/52 (5.8)2/52 (3.8) | |
| “For your information” alert in the medical record for representing patients | 1/52 (1.9) | |
| Mandatory skill training, including communication training, for new employees | 1/52 (1.9) | |
| Simplification of procedure routine for reporting child abuse | 1/52 (1.9) | |
| Implementation of informational leaflets for patients and their families | 1/52 (1.9) | |
| Consultation with other hospitals in cases of suspected child maltreatment | 1/52 (1.9) | |
| Missing | 1/53 | |
| Person informed about the suspected child abuse (question 10) | n (%) | |
| Consultant | 169/245 (68.9) | |
| Peer colleague at the same level of training | 19/245 (7.8) | |
| Hospital's child protection services (CPS) | 57/245 (23.3) | |
| Preferred educational tool for child abuse education (question 17) | n (%) | |
| Continued professional education in child abuse for staff | 199/225 (88.4) | |
| E-learning programmes | 70/225 (31.1) | |
| Leaflets | 48/225 (21.3) | |
| Other | 10/225 (4.4) | |
The self-reported levels of confidence in recognising child abuse and competency in addressing the child/parents/relatives with the suspicion of child abuse are described in figure 4. There was no significant differences between the professional affiliation and described level of confidence in recognising child abuse (p = 0.237).
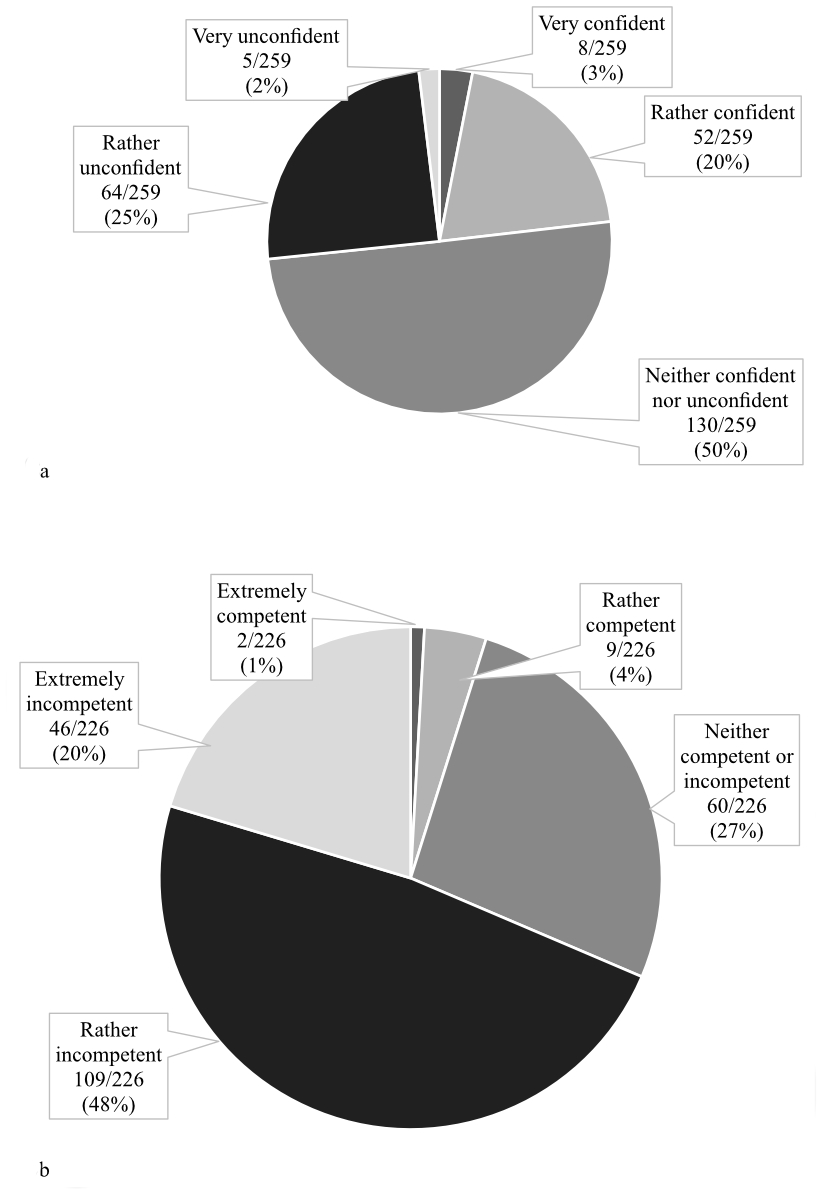
Figure 4 a: Self-reported level of confidence in recognising child abuse on a 5-point Likert rating scale. b: Self-reported level of competency in addressing the child/parents/relatives with the suspicion of child abuse on a 5-point Likert rating scale.
Nearly all participants (n = 241/244, 98.8%) knew whether there was an acting CPS in their hospital but expressed an interest to know more about how to recognise child abuse (n = 226/242, 93.4%). Regarding the interest in receiving more child abuse education (table 5), there was no significant difference between hospitals (p = 0.251), sex (p = 0.060), work experience (p = 0.358), age (p = 0.147), specialty (paediatric emergency medicine or paediatric surgery) (p = 0.38), and profession (p = 0.34) or between nursing (p = 0.859), medical (p = 0.193) and nursing assistant (FaGe) level of training (p = 0.062). Three-quarters (n = 185/243, 76.1%) of the participants stated that they were interested in having access to a standardised questionnaire and/or documentation form supporting the management of suspected child abuse.
Based on the reported enablers for the detection and reporting of child maltreatment (table 5), a CAN detection aid tool was created featuring risk factors for child abuse (clinical, history, socio-economic factors), screening questions for staff [24], sample questions for facilitated communication with child abuse victims and their families, and a graphical representation of typical locations of accidental and non-accidental injuries in children [26]. We suggest that other resources be added individually (e.g., contact details of the hospital CPS, linkto the local child abuse referral pathway, and relevant local web sites).
Detecting and reporting child abuse in the ED to prevent further harm!
A “no” answer to any of the following questions should trigger collection of more information and prompt notification of the child protection services.
Abuse:
Neglect:
Abuse/neglect:
Family findings:
Socio-economic factors
Family factors that increase the risk of recurring child abuse
Typical features of accidental and non-accidental injuries are shown in figures 5 and 6.
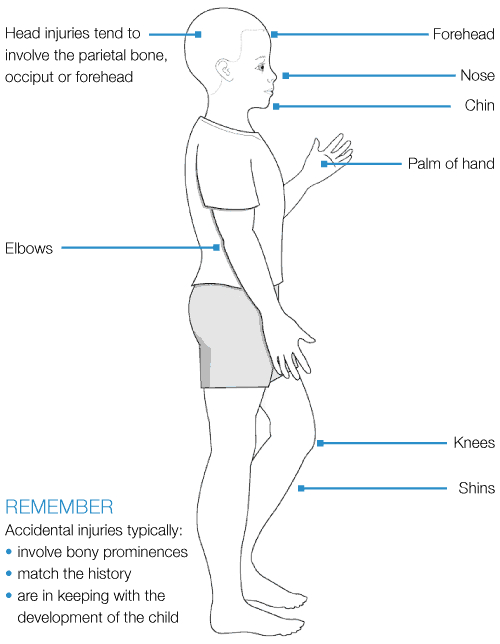
Figure 5 Typical features of accidental injuries. Reproduced with permission from: Harris J, Sidebotham P, Welbury R, et al. Child protection and the dental team: an introduction to safeguarding children in dental practice. COPDEND: Sheffield, 2006-13,https://bda.org/childprotection/Recognising/Pages/Physical.aspx.
We recommend the TEN-4-FACESp tool as an additional, validated resource for use in children under 4 years of age [23].
Preparation of the conversation: Use non-leading, open-ended questions in a quiet and private atmosphere, avoid discussing stressful topics in the presence of the child, listen without condemning, and describe your findings as objectively as possible (e.g., size and colour of haematoma instead of estimated age).
Introduction: “We routinely ask standard questions with this type of injury and may notify child protection services, if appropriate”, “We routinely involve child protection services with this kind of injury at this age”.
Example questions (child/adolescent):
You may insert here: Contact details of local child protection services, link to hospital child abuse and neglect reporting policy.
To the best of our knowledge, this is the first survey on the barriers to detecting and reporting child maltreatment in the PED and paediatric surgery department in Switzerland. This study highlights several significant self-reported obstacles and enablers of the detection and reporting of CAN. The largest hurdles were insufficient knowledge about and lack of confidence in detecting the signs and symptoms of child abuse, reporting to CPS, and interprofessional (e.g., belonging to the professional group nursing) and medical hierarchical structures.
The main emerging self-reported enablers to detecting and reporting CAN according to our survey results included more and regular child abuse education, clinical practice guidelines for CAN reporting and identification (e.g., a catalogue of questions and a standardised documentation form to be used in case of suspicion), and encouragement of lower thresholds to express and report CAN that bypass hierarchical and interprofessional barriers.
Our findings confirm the previously described barriers and enablers for detecting and reporting CAN in other settings, which have been consistent over the past decades [1, 16–20]. Alarmingly, strategies to maximise recognition and reporting of CAN by HCPs working in EDs have been insufficiently implemented.
Emerging barriers to recognising child abuse from past studies include inadequate knowledge, experience and awareness, failure to recognise the signs and symptoms of abuse during a child’s presentation, lack of confidence, inadequate CAN assessment tools or omission of essential questions from such tools [27], biased provider views about education, family structure or employment status [28], and lack of ongoing contact with the family [1, 17, 20]. The earlier published enablers for the detection of CAN included real-time case discussion with peers/supervisors, more child abuse education, objection to child abuse, and professional and personal accountability and responsibility [16, 19].
Previously elaborated barriers to reporting child maltreatment included failure to recognise the signs and symptoms of maltreatment, lack of confidence, inadequate education/ignorance, knowledge, and experience with the reporting process, a lack of guidelines [29], reporting infrastructure deficits, loyalty to the family or fear of causing harm to the child or their family [19], reluctance to involve legal bodies, biased provider views, lack of follow-up of reported cases, fear of negative consequences of reporting (e.g., testifying in court [20], or litigating with retaliating family members [29]), and previous negative experiences with CAN reporting [18]. In contrast, enablers for reporting CAN were real-time case discussion with peers or supervisors, the belief that it was in the patient’s best interest to report in case of suspicion [1, 20, 31], specific CAN reporting laws [18, 32], reporters’ own parental status (i.e., inclination to report increased with the number of own children) [16], and longer work experience [33]. This contrasts with the findings of our study, where the percentage of respondents not reporting a proportion of their initial CAN suspicions was higher among staff with longer work experience compared with those with <3 years of work experience (table 4). However, this may reflect a more thorough reconsideration of the CAN diagnosis in this group.
Only 1/4 (23.2%) respondents felt “very confident” or “rather confident” in recognising child abuse, and nearly all (93.4%) expressed an interest in increasing their knowledge about the recognition of child abuse. Likewise, only every twentieth participant felt extremely competent (n = 2/226, 0.9%) or rather competent (n = 9/226, 3.9%) in addressing the child/parents/relatives with the suspicion.
In line with our results, this need for more knowledge and education has been elaborated in a previous survey-based European study [13]. Child maltreatment education was mandatory in just over one-half (n = 16/29) of the participating countries and for approximately one-third of ED nursing (31.9%) and medical (36.2%) staff; 71.9% of respondents from 28 countries expressed the need for more training, and one-half (51.9%) of European hospitals providing treatment for children were insufficiently equipped to recognise child maltreatment in the ED [13]. Despite the availability of international guidelines (e.g., NICE or AWMF guidelines for the management of child maltreatment [34, 35]) and persistently high numbers of reported child abuse cases in Switzerland [9] and abroad [5, 10], child protection training is not yet mandatory in Switzerland and many European countries. Consequently, the main enablers of the recognition and reporting of child maltreatment reported in this survey included mandatory skill training, including communication training for new employees, regular refresher courses, and the need for encouragement of staff and lower thresholds to actively express and report suspicions (table 5). It has been recommended that such education should cover the recognition of child abuse based on child risk factors, clinical examination findings, parental risk factors (e.g., severe psychiatric problems, substance abuse or domestic violence), and steps for handling CAN, including awareness of CPS and sensitive communication with the child and their parents [14, 15, 36, 37].
Almost three-quarters (82.9%) of HCPs suspected child abuse once (22.9%) or twice (20.8%) in the past 12 months (figure 2); all but 30/245 (12.2%) subsequently reported their suspicions. In line with previous findings [13], the number of suspected cases was positively correlated with the level of care provided at the institution (tertiary versus teaching hospital); therefore, university hospitals seemed to be better equipped for the recognition of CAN.
In this study, more than 1 in 10 (12.2%) suspected child maltreatment cases were not reported or followed up, potentially leading to adverse outcomes for these children. When examining the reasons for waiving notification in these cases, uncertainty of whether child abuse was the correct diagnosis (47.7%) and lack of feeling responsible (20.5%) were the most common underlying rationales for not acting in these cases, followed by uncertainty of whether reporting has any consequences (9.1%) and opposing assessments by hierarchically superior staff (11.4%) (table 3). Interestingly, there were significantly more suspected but not reported cases reported by female than male health care workers (p = 0.039) and by nurses than physicians (p = 0.005). This behaviour has been described previously and is attributed to institutional task allocation and greater confidence among medical staff [16]. Potential obstacles for nursing and junior medical staff for reporting suspected child maltreatment cases may be a lack of education and a consequent lack of confidence, hierarchical structures with high thresholds to express concerns, and the local reporting system infrastructure (table 5). Likewise, PED staff reported CAN significantly more often than paediatric surgery staff. However, this may be explained by a participant bias, in which many inpatient cases were already reported by the first point of contact in the ED and were subsequently admitted to the surgical ward.
There is an urgent need to implement intervention strategies (e.g., a legal obligation to implement mandatory child protection education for nursing and medical students or postgraduate trainees beyond the basic academic curriculumin Switzerland and abroad), develop cognitive aids to meet the needs of HCPs in the ED, implement validated screening tools, improve the reporting system infrastructure, ensure the supply of resources and support (e.g., funding, time), implement CAN reporting laws, and advocate for gender and interprofessional equity [19].
Only every twentieth survey participant felt extremely competent (0.9%) or rather competent (3.9%) in addressing the child/parents/relatives with the suspicion of child abuse. These findings highlight the need to extensively cover communication training, not only for the delicate task of confronting the family with a suspicion (using pre-formulated expressions such as “Reporting children with this type of injury is routine in our institution”) but also for conveying one’s suspicion to the final decision maker using established teamwork items, such as “speaking up” [38]. Self-reported potential drivers for and action taken when reporting child abuse include the need for clinical practice guidelines, including a catalogue of pre-formulated questions and a standardised documentation form to be used in case of suspicion, and standardisation of the detection and reporting process, regardless of hierarchical position (e.g., flowcharts and mandatory full body examination documentation) (table 5). In addition, more effective teamwork with feedback from Allied Health (CPS) and instruction by forensic medicine was mentioned as potential areas of improvement. There was an interest in having access to a standardised questionnaire and/or documentation form supporting the management of suspected child abuse among three-quarters of participants (76.1%). EDs with a hospital policy/clinical practice guidelines on the management of child abuse scored higher in the detection of both child and parental risk factors than institutions without these policies/guidelines in place [13].
Strategies to increase the detection of child abuse in EDs to prevent devastating outcomes have been previously described, including checklists, the development of new screening tools [6, 24, 39–42], testing of existing tools for their usefulness [15, 43], implementation of staff training [15, 31, 44], and automatic involvement of CPS at certain defined diagnoses [45]. Checklists covering the indicators of risk for CAN have been previously shown to increase the rate of suspected but not confirmed cases of child maltreatment, the awareness of CAN, and the documentation of suspected cases [5]. Earlier studies have highlighted the three- (0.3% versus 0.1%) to fivefold higher detection rate (0.5% versus 0.1%) of child maltreatment in the ED when a local checklist or validated screening tool (e.g., ESCAPE instrument, currently the screening tool with the highest empiric level [3]) was used, respectively, as compared with not using screening tools [39]. Furthermore, the use of this screening tool led to improved documentation and a higher level of awareness of child abuse, which in turn may help prevent further harm to children at risk for maltreatment. However, ESCAPE did not screen for sexual and emotional CAN and might therefore not be feasible for reliable detection of all types of child maltreatment in the PED [3]. Similar screening questions are used in other screening tools, such as in the SPUTOVAMO-R2 [46]. At the time of this study, no validated screening tools were used at our institutions. Likewise, only 28.6% of 29 surveyed European EDs used a validated (SPUVAMO, ESCAPE) or local, non-validated screening tool [13]. In this survey, we did not investigate the need for a local or validated screening tool; however, previous investigations reported a high level of acceptance among HCPs for the introduction of an early detection measure/screening tool to facilitate the recognition of domestic violence and the increased risk for child abuse, although its concrete form remains controversial [12]. It has been suggested that screening tools should cover both child risk factors (clinical findings and medical history red flags) and parental risk factors that significantly increase the risk of suffering child abuse (e.g., domestic violence, drug/substance abuse, and severe mental health problems) [13]. Automatic involvement of CPS for children under 1 year of age presenting with high-risk injuries did not lead to increased child abuse detection rates [45].
In this survey, nearly all (98.8%) respondents knew whether an acting CPS existed in their institution. This contrasts other studies, where only one-third of participants stated that they had a local child maltreatment team at their institution [13].
Secondary preventive measures have been described, including the co-examination of siblings of suspected/confirmed child abuse or family violence victims [47], screening adult patients in the ED to identify potential children at risk for maltreatment [13, 34, 40] and vice versa, and universal intimate partner violence assessment or screening for parental risk factors, including domestic violence in the PED [48]. In addition to the parental risk factors/conditions (parental substance dependence, mental illness, domestic violence), chronic illness of the child has been associated with the increased occurrence of child abuse [2, 25, 27, 49]. One study examined the efficiency of child abuse detection by screening for parental risk factors in adult EDs using the Hague protocol. The study found a large increase in child protection notifications after the introduction of the protocol [40]. The same protocol was tested in a pilot study in Switzerland but lacked statistically significant statements due to the small sample size [50].
We acknowledge certain limitations to this survey-based study.
First, we modified the Delphi process to conduct expert feedback rounds to develop the questionnaire used in this survey. Following the comprehensive Delphi design might have increased the quality of the survey and the survey data. Furthermore, the pilot test (feedback round 2) was conducted on a very small sample (n = 4); it has been suggested to pilot test a survey on at least 30–60 population-based participants [51]. We did not perform principal components analysis or assess the internal consistency of questions loading onto the same factor. Doing so would have improved the survey structure by removing a maximum of potential internal inconsistency of questions and minimising ambiguous or missing answers and maximising answers to open-ended questions, thereby increasing the internal validity of this study.
Second, recruitment of participants was performed using a non-probability design due to a subset of institutions declining participation in the survey. This may have introduced selection bias into the sample and results. Furthermore, only institutions from German-speaking Switzerland were approached for participation in the survey, potentially introducing selection bias. Including institutions in French- or Italian-speaking Switzerland would have allowed for a more accurate representation of results.
Third, we acknowledge that the missing data in our study may have reduced the precision of desired survey data. The percentage of missing data from this survey may limit the generalisability of our results. The percentage of missing values may be related to the quality of the study and the quality of the collected data. The quality of this study can be improved by formal validation of the pilot survey; this includes reliability and validity testing, which was not conducted. Validation of this instrument will improve internal consistency, test-retest, interrater reliability, content and construct validity, and ultimately the power and generalisability of the results [52]. We included 61 (23.4%) incompletely answered surveys in our analysis; however, in two-thirds of the incomplete surveys, only one or two answers were missing. This might have introduced a non-response bias and could be explained by a lack of time, interest, comprehension, or interruption in the answering process. Likewise, the nursing staff of Lucerne hospital declined participation in the survey, and more ED than paediatric surgery medical and nursing staff were surveyed. The external validity of the study may therefore be compromised; our results may lack power, may not be generalisable to the real world and may need to be repeated with a more balanced sample.
Fourth, we recognise a potential social-desirability bias in which behaviour that will be viewed favourably by others might have been over-reported regarding a subset of questions (7–11 and 13–16). To minimise social-desirability bias and interference with the interpretation of average tendencies, the survey was conducted entirely anonymously, and participants were informed of the purpose and importance of the survey (i.e., to improve future management of CAN).
Fifth, we did not investigate whether tertiary and rural hospitals complied with international guidelines (e.g., NICE [34]), whether they had implemented child protection policies/clinical practice guidelines, or whether regular child protection training was held and which aspects were covered. Detailed knowledge of this data may allow educational areas of need to be identified and action to be taken to counteract potential educational gaps. Furthermore, this data would allow researchers to draw conclusions on whether regular child protection training is associated with higher self confidence in the detection and reporting of child maltreatment. Finally, the use or interest in the use of a child abuse screening tool was not investigated.
Finally, our aid tool underwent an informal feedback process but is not yet formally validated.
Several significant self-reported barriers to detecting and reporting child maltreatment in the PED emerged from this survey that were consistent with previously reported issues from other health care settings, the most significant being insufficient knowledge about and lack of confidence in detecting the signs and symptoms of child abuse. Despite consistently similar results over the past decades, the need remains urgent for intervention strategies, such as a legal obligation to implement mandatory child protection education for nursing and medical students or postgraduate trainees during general paediatrics, paediatric surgery and paediatric emergency medicine specialty training beyond the basic academic curriculumin Switzerland and abroad, the availability of cognitive aid tools to meet the needs of HCPs in the ED, and implementation of validated screening tools. We have devised a proposed cognitive aid tool for use and adaption according to local routines to maximise the recognition, referral, and management of child abuse cases in paediatric care (available as a separate file for download at https://doi.org/10.57187/smw.2023.40017). Both this pilot survey and the cognitive aid tool need to be formally validated in future studies prior to their use in international research and clinical work to reduce the risk of more devastating outcomes in children.
All study data are available upon request from the first author.
The authors would like to thank Dr. Viktoria Dixon and the CPS team at Astrid Lindgren’s Children´s hospital, Karolinska University Hospital Solna, Stockholm, Sweden for their critical review of the cognitive aid tool.
No funding was obtained for the conduction of this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Savell S.Child sexual abuse: are health care providers looking the other way? J Forensic Nurs. 2005;1(2):78–81.
2. Hornor G.Child maltreatment: screening and anticipatory guidance. J Pediatr Health Care.2013;27(4):242–50.
3. Hoft M,Haddad L.Screening Children for Abuse and Neglect: A Review of the Literature. J Forensic Nurs. 2017;13(1):26–34.
4. Kuang X,Aratani Y,Li G.Association between emergency department utilization and the risk of child maltreatment in young children. Inj Epidemiol. 2018 Dec;5(1):46.
5. Louwers EC,Affourtit MJ,Moll HA,de Koning HJ,Korfage IJ.Screening for child abuse at emergency departments: a systematic review. Arch Dis Child.2010 Mar;95(3):214–8.
6. Jordan KS,Moore-Nadler M.Children at risk of maltreatment: identification and intervention in the emergency department.Adv Emerg Nurs J.2014;36(1):97–106.
7. Bar-on ME, Zanga JR. Child abuse: a model for the use of structured clinical forms. Pediatrics. 1996 Sep;98(3 Pt 1):429-33.
8.Lenneke A.van Ijzendoorn R, Bakermans-Kranenburg M, Pannebakker FD, Vogels T, Euser S. De Nationale Prevalentiestudie Mishandeling van kinderen en jeugdigen (npm-2005). Leiden: LUMC; 2007.
9. Harms Huser D. “Nationale Kinderschutzstatistik 2021.”https://www.paediatrieschweiz.ch/nationale-kinderschutzstatistik-2021
10. “European status report on preventing child maltreatment.”2018 https://www.euro.who.int/__data/assets/pdf_file/0017/381140/wh12-ecm-rep-eng.pdf
11. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009 Jan; 373(9657):68–81.
12. Krüger P, Lätsch D, Voll P, Völksen S. Übersicht und evidenzbasierte Erkenntnisse zu Massnahmen der Früherkennung innerfamiliärer Gewalt bzw. Kindeswohlgefährdungen Bern: BSV. Beiträge zur sozialen Sicherheit; Forschungsbericht Nr. 1/18.2018 www.bsv.admin.ch > Publikation & Service > Forschung und Evaluation > Forschungsberichte.
13. Hoedeman F, Puiman PJ, Smits AW, Dekker MI, Diderich-Lolkes de Beer H, Laribi S, et al. Recognition of child maltreatment in emergency departments in Europe: should we do better? PLoS One.2021 Feb;16(2):e0246361.
14. Smeekens AE, Broekhuijsen-van Henten DM, Sittig JS, Russel IM, ten Cate OT, Turner NM, et al. Successful e-learning programme on the detection of child abuse in emergency departments: a randomised controlled trial.Arch Dis Child.2011 Apr;96(4):330–4.
15. Carson SM. Implementation of a Comprehensive Program to Improve Child Physical Abuse Screening and Detection in the Emergency Department.J Emerg Nurs.2018 Nov;44(6):576–81.
16. Ben Natan M Faour C, Naamhah S, Grinberg K, Klein-Kremer A. Factors affecting medical and nursing staff reporting of child abuse.Int Nurs Rev.2012 Sep;59(3):331–7.
17. Barlow S, Freeborn D, Cole B, Williams M. Advanced practice nurse barriers to child maltreatment.APSAC Adv.2012.
18. Elarousy W, Abed S. Barriers that inhibit reporting suspected cases of child abuse and neglect among nurses in a public hospital, Jeddah, Saudi Arabia.East Mediterr Health J.2019 Aug;25(6):413–21.
19. Wilson IA, Lee J. Barriers and Facilitators Associated With Child Abuse and Neglect Reporting Among Child Care Professionals: A Systematic Review.J Psychosoc Nurs Ment Health Serv.2021 Jun;59(6):14–22.
20. Tiyyagura G, Gawel M, Koziel JR, Asnes A, Bechtel K. Barriers and Facilitators to Detecting Child Abuse and Neglect in General Emergency Departments.Ann Emerg Med.2015 Nov;66(5):447–54.
21. de Villiers MR, de Villiers PJ, Kent AP. The Delphi technique in health sciences education research.Med Teach.2005 Nov;27(7):639–43.
22. “Survey monkey,” https://www.surveymonkey.com/welcome/sem/?program
23. Pierce MC, Kaczor K, Lorenz DJ, Bertocci G, Fingarson AK, Makoroff K, et al. Validation of a Clinical Decision Rule to Predict Abuse in Young Children Based on Bruising Characteristics.JAMA Netw Open.2021 Apr;4(4):e215832.
24. Louwers EC, Korfage IJ, Affourtit MJ, Ruige M, van den Elzen AP, de Koning HJ, et al. Accuracy of a screening instrument to identify potential child abuse in emergency departments [A]. Child Abuse Negl.2014 Jul;38(7):1275–81.
25. Lips U, Wopman M, Jud A, Falta R. Kindsmisshandlung - Kindesschutz Leitfaden zu Früherfassung und Vorgehen in der Praxis.2020 https://www.kinderschutz.ch/angebote/herunterladen-bestellen/leitfaden-kindsmisshandlung
26. Harris J, Sidebotham P, Welbury R. Child protection and the dental team: an introduction to safeguarding children in dental practice. COPDEND: Sheffield, 2006-13. https://bda.org/childprotection/Recognising/Pages/Physical.aspx.https://bda.org/childprotection/Recognising/Pages/Physical.aspx
27. Diderich HM, Verkerk PH, Oudesluys-Murphy AM, Dechesne M, Buitendijk SE, Fekkes M. Missed cases in the detection of child abuse based on parental characteristics in the emergency department (the Hague Protocol).J Emerg Nurs.2015 Jan;41(1):65–8.
28. Cowley LE, Maguire S, Farewell DM, Quinn-Scoggins HD, Flynn MO, Kemp AM. Factors influencing child protection professionals’ decision-making and multidisciplinary collaboration in suspected abusive head trauma cases: A qualitative study.Child Abuse Negl.2018 Aug;82:178–91.
29. Davidov DM, Jack SM, Frost SS, Coben JH. Mandatory reporting in the context of home visitation programs: intimate partner violence and children’s exposure to intimate partner violence.Violence Against Women.2012 May;18(5):595–610.
30. Leite JT, Beserra MA, Scatena L, Silva LM, Ferriani M. Coping with domestic violence against children and adolescents from the perspective of primary care nurses.Rev Gaúcha Enferm.2016 Jun;37(2):e55796.
31. Jordan KS, MacKay P, Woods SJ. Child Maltreatment: Optimizing Recognition and Reporting by School Nurses.NASN Sch Nurse.2017 May;32(3):192–9.
32. Mathews B, Lee XJ, Norman RE. Impact of a new mandatory reporting law on reporting and identification of child sexual abuse: A seven year time trend analysis. Child Abuse Negl. 2016 Jun;56:62–79.
33. Rolim AC, Moreira GA, Gondim SM, Paz SS, Vieira LJ. Factors associated with reporting of abuse against children and adolescents by nurses within Primary Health Care. Rev Lat Am Enfermagem. 2014;22(6):1048–55.
34. The National Institute for Health and Care Excellence (NICE). Child abuse and neglect 2017. https://www.nice.org.uk/guidance/ng76/resources/child-abuse-and-neglect-pdf-1837637587141.,2017.
35. AWFM Kinderschutz Leitlinie. https://www.awmf.org/uploads/tx_szleitlinien/027-069m_S3_Kindesmisshandlung-missbrauch-vernachlaessigung-Kinderschutzleitlinie_2019-02_01.pdf
36. Louwers EC, Korfage IJ, Affourtit MJ, De Koning HJ, Moll HA. Facilitators and barriers to screening for child abuse in the emergency department.BMC Pediatr.2012 Oct;12(1):167.
37. Milani GP, Vianello FA, Cantoni B, Agostoni C, Fossali EF. New program for identification of child maltreatment in emergency department: preliminary data.Ital J Pediatr. 2016 Jul;42(1):66.
38. Eppich W.“Speaking Up” for Patient Safety in the Pediatric Emergency Department.Clin Pediatr Emerg Med. 2015 Jun;16(2):83–9.
39. Louwers EC, Korfage IJ, Affourtit MJ, Scheewe DJ, van de Merwe MH, Vooijs-Moulaert AF, et al. Effects of systematic screening and detection of child abuse in emergency departments.Pediatrics.2012 Sep;130(3):457–64.
40. Diderich HM, Fekkes M, Verkerk PH, Pannebakker FD, Velderman MK, Sorensen PJ, et al. A new protocol for screening adults presenting with their own medical problems at the Emergency Department to identify children at high risk for maltreatment. Child Abuse Negl.2013 Dec;37(12):1122–31.
41. Paek SH, Jung JH, Kwak YH, Kim DK, Ryu JM, Noh H, et al. Development of screening tool for child abuse in the korean emergency department: using modified Delphi study. Medicine (Baltimore).2018 Dec;97(51):e13724.
42. Dudas L, Petrohoy G, Esernio-Jenssen D, Lansenderfer C, Stirparo J, Dunstan M, et al. Every child, every time: hospital-wide child abuse screening increases awareness and state reporting. Pediatr Surg Int.2019 Jul;35(7):773–8.
43. Rumball-Smith J, Fromkin J, Rosenthal B, Shane D, Skrbin J, Bimber T, et al. Implementation of routine electronic health record-based child abuse screening in General Emergency Departments. Child Abuse Negl.2018 Nov;85:58–67.
44. Ansari S, Boyle A. Emergency department-based interventions for women suffering domestic abuse: a critical literature review. Eur J Emerg Med. 2017 Feb;24(1):13-18. doi: 10.1097/MEJ.0000000000000416.
45. Powers E,Tiyyagura G,Asnes AG,Leventhal JM,Moles R,Christison-Lagay E,et al. Early Involvement of the Child Protection Team in the Care of Injured Infants in a Pediatric Emergency Department.J Emerg Med.2019 Jun;56(6):592–600.
46. Schouten MC, van Stel HF, Verheij TJ, Houben ML, Russel IM, Nieuwenhuis EE, et al. The Value of a Checklist for Child Abuse in Out-of-Hours Primary Care: To Screen or Not to Screen. PLoS One.2017 Jan;12(1):e0165641.
47. Lindberg DM, Shapiro RA, Laskey AL, Pallin DJ, Blood EA, Berger RP; ExSTRA Investigators.Prevalence of abusive injuries in siblings and household contacts of physically abused children. Pediatrics.2012 Aug;130(2):193–201.
48. Litzau M, Denise Dowd M, Stallbaumer-Rouyer J, Miller MK, Randell KA. Universal Intimate-Partner Violence Assessment in the Pediatric Emergency Department and Urgent Care Setting: A Retrospective Review. Pediatr. Emerg Care. vol. Publish Ahead of Print, Jan. 2019, doi:.https://journals.lww.com/00006565-900000000-98257
49. Mulder TM, Kuiper KC, van der Put CE, Stams GJ, Assink M. Risk factors for child neglect: A meta-analytic review. Child Abuse Negl.2018 Mar;77:198–210.
50. Staubli G, Sager R, Schreen C, Eis D, Schmid S, Jud A. Screening von Patienten auf der Erwachsenennotfallstation bezüglich Kindswohlgefördung (SPEK). Nov. 20,2018 https://docplayer.org/109588767-Screening-von-patienten-auf-erwachsenennotfallstationen-bezueglich-kindswohlgefaehrdung-spek.html
51. Perneger TV, Courvoisier DS, Hudelson PM, Gayet-Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res.2015 Jan;24(1):147–51.
52. Groenwold RH, Dekkers OM. Missing data: the impact of what is not there. Eur J Endocrinol.2020 Oct;183(4):E7–9.
53. Louwers EC, Korfage IJ, Affourtit MJ, Ruige M, van den Elzen AP, de Koning HJ, et al. Accuracy of a screening instrument to identify potential child abuse in emergency departments. Child Abuse Negl.2014 Jul;38(7):1275–81.
54. Lips U, Wopman M, Jud A, Falta R. Kindsmisshandlung - Kindesschutz Leitfaden zu Früherfassung und Vorgehen in der Praxis. 2020 https://www.kinderschutz.ch/angebote/herunterladen-bestellen/leitfaden-kindsmisshandlung
55. Pierce MC, et al. Validation of a Clinical Decision Rule to Predict Abuse in Young Children Based on Bruising Characteristics. JAMA Netw. Open, vol. 4, no. 4, p. e215832,Apr. 2021, doi:.https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2778559