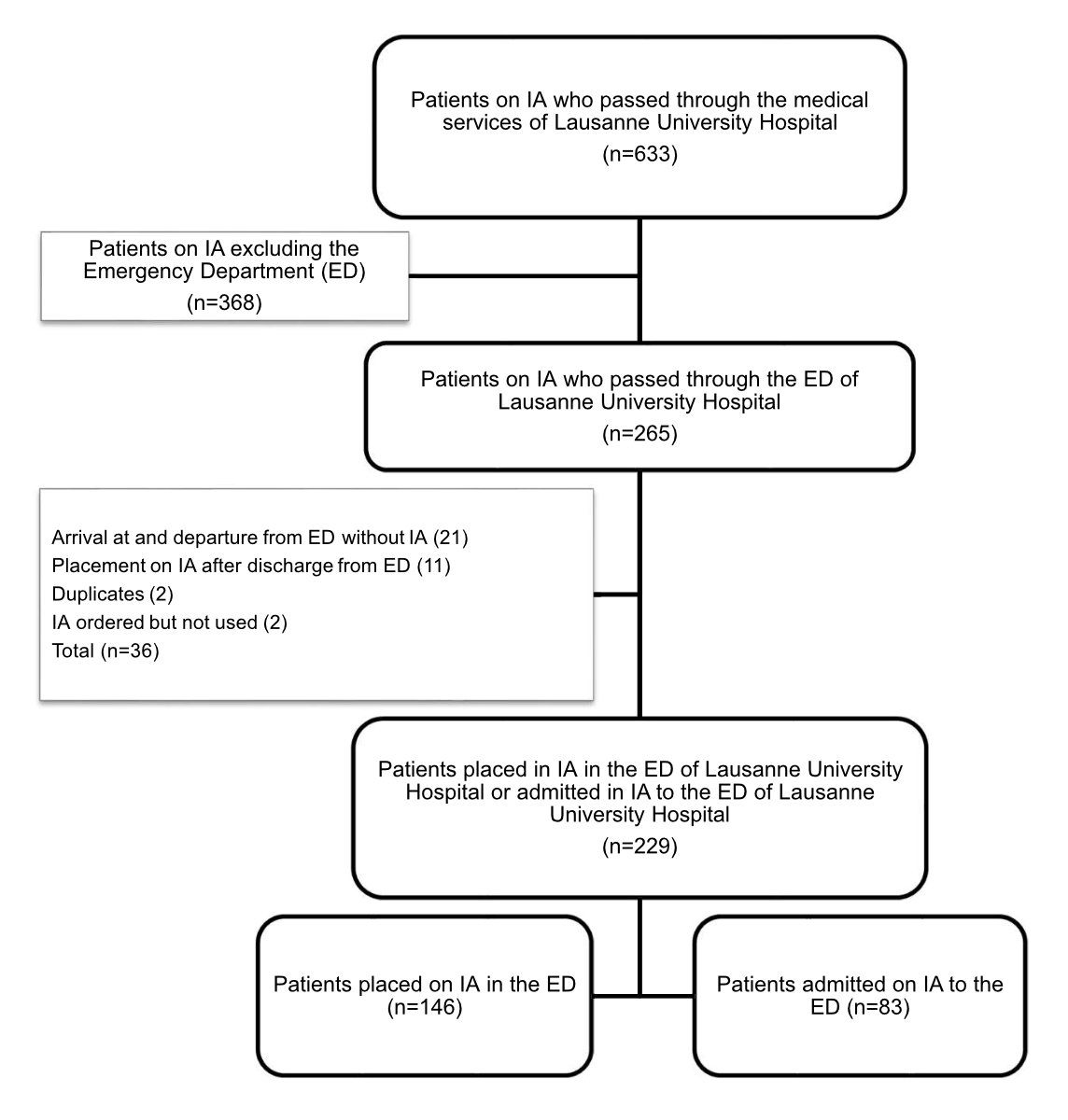
Figure 1 Flowchart: patients on involuntary admission included in the study.
DOI: https://doi.org/https://doi.org/10.57187/smw.2023.40063
Taking care of patients against their will when they are incapable of discernment represents a significant stake, both from a biopsychosocial and a legal point of view. Nevertheless, physicians may in specific situations, impose care and hospitalisation on a patient. This possibility confers on physicians the right to deprive someone of his or her liberty, an extremely strong measure that only judicial and police bodies are generally authorised to order. The involuntary admission is a measure of protection of the individual provided by the law, which makes it possible to place or retain a person against his or her will in an appropriate institution (hospital, sheltered accommodation, or home for senior citizens) when their medico-social situation requires it and when outpatient or inpatient alternatives have failed or cannot be carried out [1]. The goal of this measure is to protect patients from themselves and to provide them with the help and care they need [1]. Only people with mental disorders or a mental disability or who are in a state of serious neglect may be committed on involuntary admission, insofar as the required treatment cannot be provided in any other way [1, 2]. The involuntary admission must thus be proportionate and stopped as soon as the conditions for placement are no longer met [1].
In Switzerland, involuntary admissions are regulated by Article 426 of the Swiss Civil Code and at a cantonal level by public health laws. Involuntary hospitalisation can be ordered by the guardianship authority, called the Adult Protection Authority (APA), or by authorised doctors [1]. In the canton of Vaud, only primary care physicians, physicians on call (including prehospital emergency physicians), paediatricians, psychiatrists or child psychiatrists, and delegated physicians of the Department of Health and Social Action are authorised to pronounce an involuntary admission [3]. For each involuntary admission, a dedicated form must be completed and when the decision is re-evaluated, a follow-up form must also be completed to inform either the continuation of the involuntary admission or its termination. In the canton of Vaud, each involuntary admission is registered in the Register of Protection Measures, created in 2013 [4]. This register reveals that the number of involuntary admissions pronounced by the medical profession has increased sharply over the period 2013-2017, whereas those emanating from the APA has decreased [5]. The involuntary admission rates in the canton of Vaud are among the highest in Switzerland and are also extremely high when compared with data available from other Western countries [4, 6]. The objective of this study was to describe patients involuntary admitted to the emergency department of Lausanne University Hospital on involuntary admission, in terms of age, gender, emergency department length of stay, motive for involuntary admission, diagnosis, whether or not the involuntary admission was confirmed after the emergency department, destination at emergency department discharge.
This retrospective, observational, and monocentric study included patients 18 years and older admitted on involuntary admission to the emergency department of Lausanne University Hospital from January 1, 2018, to December 31, 2018. Lausanne University Hospital is a public university hospital that provides primary care for the 300,000 inhabitants of the Lausanne area, as well as tertiary care for Western Switzerland (about 1.5 million population area). The emergency department at Lausanne University Hospital receives approximately 60,000 adult patients per year. Patients for whom an involuntary admission has been pronounced in the Lausanne area, either in the context of requiring hospitalisation at Lausanne University Hospital, or with a request for a somatic assessment before transfer to the Department of Psychiatry, are admitted to the emergency department.
The patients were identified by the Cantonal Medical Office of Vaud. Emergency department length of stay and the destination of patients on discharge from the emergency department were extracted from the emergency department patient flow database (Gyroflux©). Discharge letters and involuntary admission were extracted from the electronic archiving software (Archimed©). These extractions made it possible to collect the following data: age, gender, assessment applicant, origin and reason for recourse to the placement measure, use of psychoactive substances, length of stay in the emergency department, destination, and diagnosis at emergency department discharge. These data were then coded and stored by using the REDCap® program (Vanderbilt University, Nashville, Tennessee). Only the principal investigators had access to the files of this coded database.
The main objective of this study was to describe patients admitted to the emergency department with an involuntary admission from January 1, 2018, to December 31, 2018, in terms of age (calculated at the time of admission in the emergency department), gender, emergency department length of stay, motive for involuntary admission (mental disorders, mental disability or state of serious neglect), diagnosis, whether or not the involuntary admission was confirmed after the emergency department because a reassessment of the involuntary admission indication is made in the emergency department by an emergency physician and/or a psychiatrist in order to define whether forced hospitalisation should be ordered, and destination at emergency department discharge.
The results were expressed as means and standard deviations for quantitative variables with a normal distribution and as median and interquartile range for non-normally distributed data. Qualitative data were expressed by using counts and percentages. All analyses were performed with Stata 16.0 (StataCorp LP, College Station, Texas).
This study was approved by the Swiss Ethics Committee on research involving humans (CER-VD) at Lausanne on March 25, 2020 (project-ID 2019-02452).
The Cantonal Medical Office of Vaud identified 633 cases of involuntary admission admitted to or issued from Lausanne University Hospital for the study period. From this list, 265 situations mentioned the emergency department. After analysis of these 265 patients, only 229 were considered for this study, the others not meeting the decision criteria for placement on involuntary admission in the emergency department and/or for admission on involuntary admission to the emergency department (figure 1). Among the patients on involuntary admission who were identified in the perimeter of the emergency department in 2018, a total of 83 were admitted on involuntary admission. This represents an incidence of 1.4 of 1000 emergency department admissions.
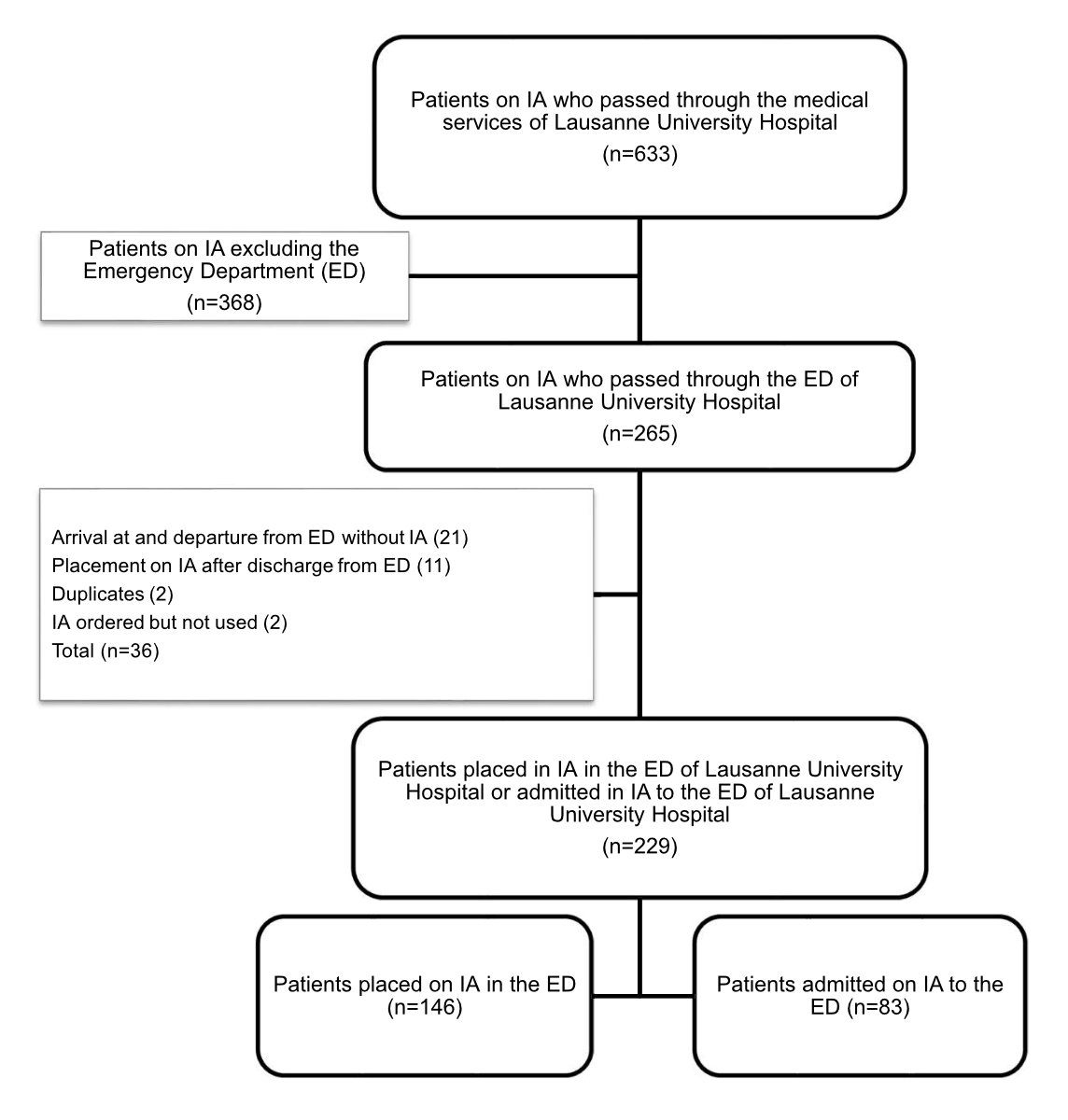
Figure 1 Flowchart: patients on involuntary admission included in the study.
These patients had a mean age of 55 years (±20) (figure 2) and were predominantly male (58%, n = 48). Involuntary admissions were ordered mainly by an on-call physician (n = 38), an attending physician (n = 26), a psychiatrist (n = 5), or the APA (n = 3). The origins of the requests for involuntary admission are listed in table 1. Patients came principally from their home (61%) or had been brought in by the police after being found in the public domain (20%). Institutions (home for senior citizens, sheltered accommodation, boarding house) represented the third most frequent source, with 13% of patients. Other patients came from prisons (3%) and hospitals (3%). Regarding the documentation of involuntary admission, the initial form was available in the hospital electronic files in 47% of cases (n = 39). For patients with an available form (n = 39), most of the reasons given for involuntary hospitalisation were mental disorders (74%, n = 29). A serious state of neglect was invoked in 23% (n = 9) of situations. Lastly, mental deficiency was cited for 10% of people being put on involuntary admission. In four situations, a combination of these three reasons was stated for the same placement on involuntary admission (two reasons in three cases, three reasons in one case). In 64% (n = 25) of these involuntary admissions, the file mentioned that relatives and legal/therapeutic representatives, or both, had been made aware of the decision.
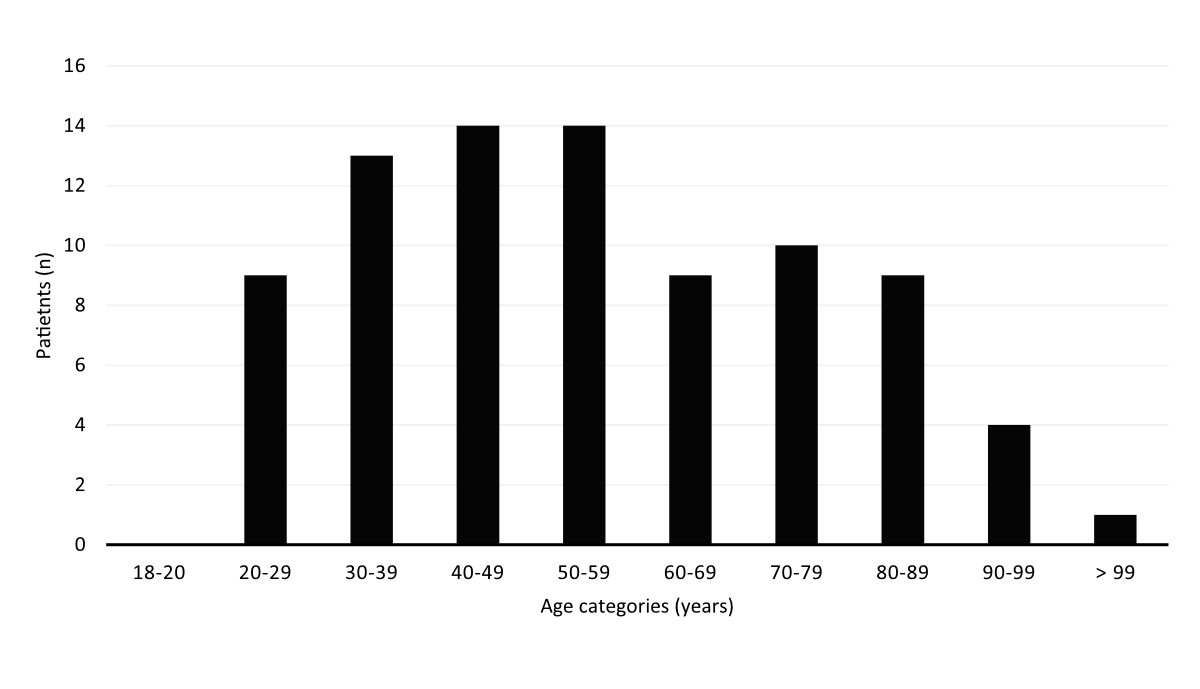
Figure 2 Distribution of patients by age category.
Table 1Sources of evaluation requests for placement on involuntary admission (n = 83).
| Requestor of evaluation | Patients admitted on involuntary admission to the emergency department | |
| n | % | |
| Relative or guardian | 13 | 15.7% |
| Police | 24 | 28.9% |
| Institution (home for senior citizens, sheltered accommodation, boarding house) | 8 | 9.6% |
| Prison service | 2 | 2.4% |
| Medico-social centre | 3 | 3.6% |
| Attending physician | 11 | 13.3% |
| Other | 12 | 14.5% |
| Not specified | 10 | 12% |
The involuntary admission follow-up form was present in the hospital chart in 52% of cases (n = 43). The reasons for the 40 missing follow-up forms were as follows: absence of a written follow-up form (n = 5); patients who went to the somatic emergency department on referral from the psychiatric emergency department only for a clinical examination before returning to the psychiatric emergency department (n = 31); use of the wrong form for patients (n = 2); a patient on involuntary admission who ran away from his place of hospitalisation, was found by the police, and brought back to the emergency department before being sent back to the hospital accommodating him without the involuntary admission measure being modified (n = 1); and a patient who had been the subject of an invalid involuntary admission placement for geographical reasons, who was then transferred to his state of residence to be evaluated there (n = 1).
Involuntary admission was confirmed for 28 patients (34%) and discontinued for 22 patients (27%) among the 83 admitted to the emergency department on involuntary admission. Indeed, among the 83 involuntary admissions, there is no documentation of the reassessment of the measure for 33 patients (39%). The median length of stay and destination after the emergency department for the discontinued or confirmed involuntary admissions are listed in table 2. The median emergency department length of stay for involuntary admissions was between 9 and 16 hours (table 2). In comparison, the median length of stay in the emergency department for all patients in 2018 was 5.8 hours. In 25% of these situations, the use of a restraint method, whether physical or chemical, was documented (n = 17). However, the number of restraint measures used in the emergency department is likely to be underestimated due to incomplete documentation [7].
Table 2Median length of stay and destination of patients admitted on involuntary admission to the emergency department (n = 83).
| n | % | Length of stay (hours), median (IQR) | Destination | n | % | Length of stay (hours), median (IQR) | |
| Discontinued involuntary admission | 22 | 27 | 16 (8–19) | Return home | 14 | 64 | 14 (7–17) |
| Voluntary admission to another establishment | 4 | 18 | 24 (11–32) | ||||
| Implementation of outpatient measures | 1 | 4 | 17 | ||||
| Other | 3 | 14 | 23 (5–30) | ||||
| Confirmed involuntary admission | 28 | 34 | 9 (6–20) | Transfer on involuntary admission to another establishment | 27 | 96 | 9 (6–20) |
| Maintain the on involuntary admission in the establishment | 1 | 4 | 10 | ||||
| N/A | 33 | 39 | 9 (6–22) | N/A | N/A | N/A | N/A |
The two etiological diagnoses most often described were psychiatric: on the one hand, a group comprising schizophrenia, schizotypal, and delusional disorders (F20-F29, 34%), and, on the other, a group with mental and behavioural disorders due to psychoactive substance use (F10-F19, 24%). A complete description of the classification of involuntary admissions by diagnosis for patients in the emergency department is given in table 3. The presence of a psychoactive substance at emergency department admission was diagnosed in more than half of the patients. Alcohol was the most frequently found substance (table 4).
Table 3Diagnosis retained for patients admitted on involuntary admission to the emergency department.
| Diagnoses (ICD-10) | N (%) | Gender (M : F) | Age, years, mean ± SD | Length of stay, hours, median (IQR) |
| Schizophrenia, schizotypal, and delusional disorders (F20-F29) | 24 (29.0%) | 1.6 : 1 | 41 ±19 | 10 (7–18) |
| Mood (affective) disorders (F30-F39) | 7 (8.4%) | 1.3 : 1 | 45 ±16 | 9 (7–21) |
| Mental and behavioural disorders due to psychoactive substance use (F10-F19) | 20 (24.1%) | 1.2 : 1 | 49 ±16 | 18 (8–22) |
| Organic, including symptomatic, mental disorders (F00-F09) | 19 (22.9%) | 1 : 1.1 | 72 ±15 | 9 (6–18) |
| Disorders of adult personality and behaviour (F60-F69) | 5 (6.0%) | 1.5 : 1 | 48 ±20 | 7 (6–22) |
| 1st attempted suicide, without an associated diagnosis | 2 (2.4%) | 1 : 1 | 35 ±8 | 10 (6–13) |
| Behavioural syndromes associated with physiological disturbances and physical factors (F50-59) | 3 (3.6%) | 2 : 1 | 45 ±7 | 22 (22–26) |
| Unspecified mental disorder (F99) | 3 (3.6%) | male only | 66 ±14 | 13 (9–14) |
Table 4Psychoactive substances consumed (n = 83).
| n | % | |
| Psychoactive substances consumed | 36 | 53.7% |
| – Alcohol* | 29 | 43.3% |
| – Benzodiazepines | 4 | 6% |
| – Antidepressants | 2 | 6% |
| – Analgesics | 2 | 3% |
| – Cannabis | 6 | 9% |
| – Cocaine | 3 | 4.5% |
* Mean ethanolaemia (if measured): 53 (±32) mmol/l
A total of 83 patients were admitted on involuntary admission to the emergency department in 2018. Most were male (58%, n = 48). This gender predominance is found in various studies [6, 8, 9]. Mental disorders were the main reason cited for involuntary hospitalisation. This observation is consistent with the results published by the Groupe de travail (GT) Population PAFA of the canton of Vaud for 2014 [4]. The diagnosis of “schizophrenia, schizotypal and delusional disorders (F20-F29)” was most frequently reported among all involuntary admission forms studied (n = 24). This finding is also similar to that reported in the literature, with a clear predominance of psychotic disorders in involuntarily admitted patients [6, 8–11]. The second most frequently made diagnosis was “mental and behavioural disorders due to psychoactive substance use (F10-F19)” (n = 20), closely followed by “organic, including symptomatic, mental disorders (F00-F09)” (n = 19), reflecting a certain heterogeneity in the reasons for resorting to an involuntary admission. Police were the most frequent applicant for emergency department admitted patients on involuntary admission. The predominance of these two diagnostic categories could explain why the police were mainly at the origin of the request for involuntary hospitalisation. Involuntary admission patients had acute alcoholic intoxication more than half the time. It appears that, faced with intoxicated and non-collaborating patients, potentially in psychomotor agitation in the public domain or at their home and refusing a transfer to the emergency department, paramedics on site called police and asked for an involuntary admission to legitimise the use of coercion. In these conditions, physicians used involuntary admission to force people to go to the emergency department. In the same way, involuntary admission was used by primary care physicians or by on-call doctors to coerce confused or demented older adults who refused urgent medical treatment to consult an emergency department. This led to a significant proportion of involuntary admission measures being pronounced because of a serious state of neglect, which affected one in four patients admitted to the emergency department on involuntary admission. A serious state of neglect has been defined by the Swiss Federal Court as a state of decline that is no longer reconcilable with human dignity (ATF 128 III 14). Among the nine people who arrived at the emergency department on involuntary admission as a result of a serious state of neglect, more than half (55.5%) presented “mental and behavioural disorders due to psychoactive substance use (F10-F19)”. The involuntary admission measure was discontinued in 50% (2/4) of people with this type of mental disorder. Because of the small number of individuals concerned, it is difficult to draw conclusions from these results, but it is nevertheless interesting to note the subjective aspect of this notion of “serious state of neglect”, the assessment of which does not always seem to be the same between relatives and guardians, on-call or attending doctors, and emergency department physicians or psychiatrists. The results obtained show a certain solitude of the doctor on duty and a lack of means to deal with patients in a situation of acute alcoholic intoxication or in a context of “serious state of neglect”, refusing hospitalisation. Faced with situations for which the outpatient network can no longer offer solutions, primary care physicians do not have many options other than pronouncing an involuntary admission measure, sometimes encouraged by the police for reasons of responsibility, particularly for individuals under the influence of psychoactive substances. Among the people admitted under a placement measure in the emergency department, a proportion of involuntary admission was discontinued (27%). However, the limitation of this result should be noted because we do not have information on the reassessment of involuntary admission in 39% of cases (n = 33). The assessment in the emergency department, therefore, made it possible in several cases to set up support measures after having carried out a broad multidisciplinary and multi-professional assessment, generally including the outpatient network and the patient’s entourage, which is obviously not feasible in the prehospital field in the current context. However, the local implementation of models of mental health care, such as crisis resolution teams [12] or open dialogue interventions [13], would provide specialised support to primary care physicians or on-call doctors in the community, helping to keep patients in their environment and avoiding some admissions to the emergency department on involuntary admission [14].
Thus, the emergency department plays the role of a filter and of being a “neutral” place in allowing a biopsychosocial reassessment of the situation. Although the emergency department is at the interface of civilian life, liberal medicine, and hospital, this role of the filter being assumed de facto by the emergency department, for lack of another structure, can be questioned. The growing, sustained, and almost permanent activity of the emergency department does not always allow sufficient time to dedicate to the reassessment of complex situations with high stakes. The use of involuntary admission to admit patients to the emergency department is therefore questionable, representing a real risk of inappropriate use for reasons of convenience or lack of an adequate alternative.
Among the patients admitted on involuntary admission, differences were observed between individuals whose involuntary admission measure was stopped and those whose involuntary admission measure was confirmed in the emergency department. Most of the discontinued involuntary admissions involved women (57.1%). Patients whose involuntary admission was finally lifted had a longer emergency department length of stay than those for whom involuntary admission was confirmed. This difference in emergency department length of stay reflects the need for an in-depth and more complete somatic and psychiatric assessment for patients for whom involuntary admission is discontinued, as well as the time necessary to organise alternative care measures, which includes conducting a reassessment several times, organising outpatient follow-up, surveying the patient’s medical and personal entourage, and waiting for a voluntary hospitalisation bed [15]. Overall, emergency department physicians judged that involuntary admission could be discontinued in one-third of the situations. Discontinued involuntary admissions after an emergency department assessment concerned 25% of patients diagnosed with “schizophrenia, schizotypal and delusional disorders (F20-F29)” and more than 33% of people diagnosed with “organic, including symptomatic, mental disorders (F00-F09)”. In this last group of patients, the average age was 70 years. It is, therefore, legitimate to wonder whether the use of an involuntary admission measure in older adults is sometimes excessive and unjustified. This could also suggest misuse of this measure and fall within the framework of elder mistreatment, according to the definition given by the World Health Organization [16]. It should also be noted that a high proportion of involuntary admissions were discontinued in patients admitted on involuntary admission in the context of “mental and behavioural disorders due to psychoactive substance use (F10-F19)”. In fact, the emergency department physicians discontinued more than half of the involuntary admission measures (58.8%) for these patients, who were admitted to the emergency department mostly because of acute alcoholic intoxication. Here, too, this result shows the sometimes inappropriate use of involuntary admission and, above all, illustrates the lack of a simple and short-term alternative to this measure of constraint. One of the elements that could explain the high proportion of involuntary admissions being discontinued in people with organic mental disorders or dependence on psychoactive substances is the possibility that the emergency department offers a somatic and psychiatric assessment 24/7. In addition, after a period of observation in the emergency department, patients are no longer under the influence of alcohol, which benefits their assessment. They often no longer present a clinical condition that justifies treatment in a hospital environment.
Often the involuntary admissions were not fully documented. Although the main information (context of medical assessment, reason for resorting to it, patient’s destination) was in most cases provided, the indications related to the presence of a guardian, legal representative, therapeutic representative, and living will, as well as communication of the measure to relatives and of a voluntary hospitalisation proposal, were only occasionally recorded. In addition, there was no reassessment of the involuntary admission indication in 50% of the cases for which the involuntary admission defined the emergency department as the patient’s destination. The traceability of this potentially serious decision is suboptimal, and the process of documentation and transmission of information must be strengthened. The ability to carry out precise monitoring of the use of involuntary hospitalisation by the office in charge is therefore limited by the quality of the documentation and the transmission of information by the physician who decides on an involuntary admission, its lifting, or its continuation.
To our knowledge, this is the first study concerning the analysis of patients admitted to a university hospital emergency department on involuntary admission. This made it possible to highlight various categories of patients and reasons for resorting to these measures. Our study also sheds light on the gaps in the documentation of the forms, which limits their traceability. The main limitation of this work is the incomplete quality of the data available because of the retrospective design. Therefore, part of the results could be obtained for only a small number of people and may not be representative of all the patients concerned.
Near a third of patients admitted on involuntary admission saw this measure discontinued after their assessment in the emergency department.
One of the uses of involuntary admission is to force patients to be examined by an emergency physician or even a psychiatrist. On-call and primary care physicians seemed to lack the time or resources to set up alternatives to emergency department admissions on involuntary admission, especially in situations in which the involuntary admission was discontinued after an emergency department assessment. The strong demand for the police to obtain an involuntary admission before taking a patient under coercion to the hospital also illustrates the absence of a specific form that allows the involuntary admission of a patient to the emergency department for a somatic and psychiatric evaluation. The desire of primary care physicians to use a legal form to document the decision obliges them to pronounce an involuntary admission for which the conditions described by the law are not always met and could, in some situations, constitute inappropriate use of involuntary admission under the law. A simple document requiring the patient to be admitted to the emergency department, attesting to the patient’s inability to discern, and the imperative need to carry out a somatic and psychiatric evaluation to decide whether an involuntary admission will be indicated or not could be an alternative in these situations.
This study was financed by the Department of Emergency Medicine of the Lausanne University Hospital (CHUV)
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Placement à des fins d’assistance (art. 426 à 439 CC) | État de Vaud [cited 2019 Sep 9]. Available from: https://www.vd.ch/themes/justice/curatelles-et-tutelles/autres-mesures-de-protection/placement-a-des-fins-dassistance-plafa/
2. Coercive measures in medecine. Swiss Academy of Medical Sciences (SAMS); 2015 [cited 2019 Sep 9]. Available from: https://www.samw.ch/fr/Publications/Directives.html
3. Boubaker K . Directives du Médecin cantonal à l’intention des médecins vaudois concernant les placements à des fins d’assistance (PLAFA) y inclus 1) la procédure pour maintenir une personne entrée de son plein gré 2) les mesures ambulatoires (MA). Service de la santé publique - Département de la santé et de l’action sociale; 2018. [cited 2019 Sep 9]. Available from: https://www.vd.ch/fileadmin/user_upload/themes/sante/Professionnels/PLAFA/PLAFA_directive_MedecinsCantonal_Revision_V02.10.2018.pdf
4. Monnat M , Morandi S , Masson A , Midili V , Stadelmann S , Vicario CG . Population PLAFA : Aspects épidémiologiques et statistiques : Rapport final. Lausanne: Etat de Vaud; 2016. p. 71 [cited 2019 Sep 9]. Available from https://www.vd.ch/fileadmin/user_upload/themes/etat_droit/tutelles_curatelles/Actualit%C3%A9s/PLAFA_RapportFinal_GTPopulation.pdf
5. Nicollier M . Les médecins multiplient les placements forcés. 24Heures. 08.16.2017 [cited 2019 Sep 10]. Available from: https://www.24heures.ch/vaud-regions/medecins-multiplient-placements-forces/story/10813128
6. Silva B , Golay P , Morandi S . Factors associated with involuntary hospitalisation for psychiatric patients in Switzerland: a retrospective study. BMC Psychiatry. 2018 Dec;18(1):401. https://doi.org/10.1186/s12888-018-1966-6
7. Beysard N , Yersin B , Carron PN . Mechanical restraint in an emergency department: a consecutive series of 593 cases. Intern Emerg Med. 2018 Jun;13(4):575–83. https://doi.org/10.1007/s11739-017-1697-6
8. Hotzy F , Moetteli S , Theodoridou A , Schneeberger AR , Seifritz E , Hoff P , et al. Clinical course and prevalence of coercive measures: an observational study among involuntarily hospitalised psychiatric patients. Swiss Med Wkly. 2018 Apr;148:w14616.
9. Placements en établissement psychiatrique à des fins d’assistance | OBSAN [cited 2019 Sep 6]. Available from: https://www.obsan.admin.ch/fr/publications/placements-en-etablissement-psychiatrique-des-fins-dassistance
10. Schmitz-Buhl M , Gairing SK , Rietz C , Häussermann P , Zielasek J , Gouzoulis-Mayfrank E . A retrospective analysis of determinants of involuntary psychiatric in-patient treatment. BMC Psychiatry. 2019 Apr;19(1):127. https://doi.org/10.1186/s12888-019-2096-5
11. Salize HJ , Dressing H . Epidemiology of involuntary placement of mentally ill people across the European Union. Br J Psychiatry. 2004 Feb;184(2):163–8. https://doi.org/10.1192/bjp.184.2.163
12. Stulz N , Wyder L , Maeck L , Hilpert M , Lerzer H , Zander E , et al. Home treatment for acute mental healthcare: randomised controlled trial. Br J Psychiatry. 2020 Jun;216(6):323–30. https://doi.org/10.1192/bjp.2019.31
13. Freeman AM , Tribe RH , Stott JC , Pilling S . Open Dialogue: A Review of the Evidence. Psychiatr Serv. 2019 Jan;70(1):46–59. https://doi.org/10.1176/appi.ps.201800236
14. Moetteli S , Heinrich R , Jaeger M , Amodio C , Roehmer J , Maatz A , et al. Psychiatric Emergencies in the Community: characteristics and Outcome in Switzerland. Adm Policy Ment Health. 2021 Nov;48(6):1055–64. https://doi.org/10.1007/s10488-021-01117-7
15. Maniaci MJ , Lachner C , Vadeboncoeur TF , Hodge DO , Dawson NL , Rummans TA , et al. Involuntary patient length-of-stay at a suburban emergency department. Am J Emerg Med. 2020 Mar;38(3):534–8. https://doi.org/10.1016/j.ajem.2019.05.045
16. Sethi D . Weltgesundheitsorganisation, éditeurs. European report on preventing elder maltreatment. Copenhagen: World Health Organization, Regional Office for Europe; 2011. p. 86.