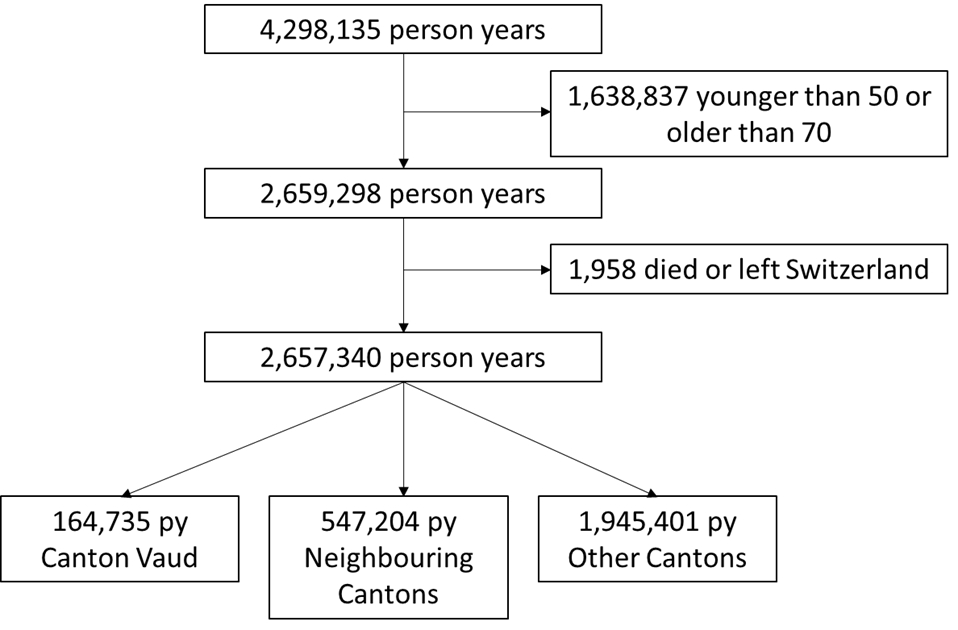
Figure S1 Exclusions.
DOI: https://doi.org/10.57187/smw.2023.40054
In Switzerland, colorectal cancer is the third most common cancer in men and the second most common in women [1, 2]. Colorectal cancer screening reduces mortality and, to a lesser extent, incidence by detecting and removing early-stage adenocarcinomas and adenomatous polyps [2, 3]. The US Preventive Task Force [4] and the European Panel [5] recommend screening for patients aged 50 to 75 years with either colonoscopy every 10 years or a faecal occult blood test every 1–2 years [6]. Several studies have shown the benefits of colorectal cancer screening (lower mortality and incidence of colorectal cancer and cost-effectiveness) [2, 3, 7], and European guidelines recommend organised screening programmes to ensure quality and equality. Such programmes already exist in many countries [8].
In Switzerland, the colorectal cancer screening prevalence before the implementation of organised programmes had increased from 33% in 2007 to 48% in 2017, mostly due to the growing use of opportunistic colonoscopy [9]. Colorectal cancer testing rates in Switzerland are higher among those with private insurance coverage and low-deductible health plans, suggesting that reimbursement of tests might increase colorectal cancer screening rates [6]. In July 2013, the Swiss Federal Department of Home Affairs authorised the reimbursement by insurance of colorectal cancer screening for people aged 50 to 69, with a deductible for screening tests [7, 10]. Switzerland has no national programme; each of the 26 cantons acts autonomously and chooses the organisational modalities that suit it [11].
In Switzerland, the canton of Uri implemented the first colorectal cancer screening programme in 2014 [12], but canton Vaud began the first organised programme in Switzerland in 2015 (in compliance with World Health Organization criteria), with invitations mailed from 2016. The target population included all people residing in Vaud, aged 50 to 69 years, who were not considered at high risk for colorectal cancer (i.e. without symptoms, family history or previous advanced neoplasia) [7, 13]. Citizens can choose between the faecal immunochemical test (FIT, a type of faecal occult blood test) every two years or colonoscopy every 10 years [7]. GPs are the gateway to this screening programme because they provide advice for an informed decision about screening tests, prescriptions for FIT and referrals for colonoscopies. Several other cantons have since launched programmes, including Jura, Neuchâtel and Geneva in 2019, as well as Valais and Fribourg in 2020. The impact of the Vaud programme on colonoscopy and faecal occult blood test testing rates is not known because Vaud does not have universal health records with the screening status of all individuals. In Vaud, as throughout Switzerland, high rates of opportunistic screening existed before the implementation of the screening programme, making isolating its effect more difficult [9].
We aimed to track colorectal cancer testing rates after the implementation of the 2013 federal law and the organised screening programme in 2015 using data from a large health insurance company (CSS) in Switzerland. We hypothesised that the earlier implementation of a screening programme (in Vaud) would be associated with greater increases in overall colorectal cancer testing rates than in neighbouring cantons (without screening programmes) and the rest of Switzerland, especially faecal occult blood test testing. We also estimated the proportion of people up to date with screening in 2018, hypothesising that the proportion would be higher in a canton with a screening programme in addition to opportunistic screening.
We conducted yearly cross-sectional analyses of a cohort of CSS health insurance enrollees. Ethics approval was not required under the Swiss Human Research Act because all data were retrospective and irreversibly anonymised [14].
Our methods were similar to those of Bissig et al. [15]. We analysed the claims data of CSS, which covers around 16% of the Swiss population and 10% of Vaud, from 2010 to 2018. CSS covers approximately 1.7 million insured persons in Switzerland, including around 85,000 in Vaud [16]. The data were extracted by the CSS Institute for Empirical Health Economics, an independent research centre of CSS. They are not available for public sharing because, under Swiss law, the publication of fully anonymised insurance claim data is restricted. The data can be obtained by contacting the CSS Institute and signing a data protection declaration guaranteeing data protection. We analysed the data from all insurees, divided into three groups: (1) Vaud (VD); (2) the four neighbouring cantons (Geneva [GE], Neuchâtel [NE], Fribourg [FR] and Valais [VS]); and (3) the rest of Switzerland.
We included all faecal occult blood tests and colonoscopies performed between 2010 and 2018, stratified by group. We analysed the testing rate yearly and completed the analysis by comparing tests performed within and outside the screening programme in Vaud. We grouped people who received an faecal occult blood test and a colonoscopy in the same calendar year in the faecal occult blood test category because positive faecal occult blood tests are usually followed by a diagnostic colonoscopy and no clinical indication exists for an faecal occult blood test after a colonoscopy. We had no information about the reasons for performing colonoscopies and included all colonoscopies independently of the indication (not only for screening). Since sigmoidoscopies are rare in Switzerland, we classified them as colonoscopies [17, 18].
We used the Swiss analysis list for laboratory measures to identify billed faecal occult blood tests. Billing is no different for guaiac-based and immunochemical faecal occult blood test in the analysis list, so both were classed as faecal occult blood tests. We used Swiss ambulatory procedure codes (TARMED) to identify colonoscopies, sigmoidoscopies and recto-sigmoidoscopies. Billing data do not include test indications (screening or diagnostic), but since 2015, tests performed within organised programmes have been billed with special codes. All codes are listed in the appendix (table S1). We had no data on tests performed in hospitals, but inpatient colonoscopies represent less than 10% of all colonoscopies.
Patients without colonoscopy or faecal occult blood test data were assumed to not have undergone these tests.
We collected demographic data (birth date, death date, gender, postal code) from CSS standard insurance data. We used a list from the Federal Statistics Office to convert postal codes to canton and urban status (urban, intermediate or rural). For each year, we extracted from the CSS dataset the participant’s deductible (in Swiss Francs, CHF) and health plan (free physician choice, family physician as gatekeeper, health maintenance organisation [HMO] or telemedicine).Health insurance data does not include clinical diagnoses. Since pharmacy-based cost groups identify the medications used to treat chronic diseases, these served as a proxy for chronic disease; we extracted the number of pharmacy-based cost groups for each enrolee [19–21]. Most covariates had no missing data because basic demographic data is obligatory to enrol in insurance and the insurance type was available for all participants; pharmacy-based cost group information was likely missing, but those without a prescription medication were assumed not to have the related comorbidity.
We used descriptive statistics to characterise the enrollees in each study year and the proportion of people who had (a) any test for colorectal cancer, (b) faecal occult blood test and (c) colonoscopy each year, from 2010 to 2018, stratifying by geographical area (Vaud vs neighbouring cantons vs the rest of Switzerland). Patients with family physician, telemedicine or HMO insurance model plans were classed as managed care. We compared the characteristics of those who had an faecal occult blood test within and outside the Vaud screening programme in 2018. We did not perform the same comparison for those with a colonoscopy in 2018 because we did not know the indication for colonoscopies done outside the programme (screening, surveillance or diagnostic).
Testing rates are the proportion of those insured who had a colonoscopy or faecal occult blood test during that calendar year. To analyse yearly colorectal cancer testing rates, we defined (a) any testing for colorectal cancer as insurees with a bill for at least one test (faecal occult blood test, colonoscopy or sigmoidoscopy) in that calendar year. We defined (b) faecal occult blood test as those who claimed bills for one or more faecal occult blood tests with or without a colonoscopy. We defined (c) colonoscopy as those who had a colonoscopy or sigmoidoscopy and no faecal occult blood test in that calendar year. As mentioned above, faecal occult blood test and colonoscopy performed within the same year were most likely due to a positive faecal occult blood test followed by diagnostic colonoscopy, such that the initial choice of test was faecal occult blood test. We fitted two multinomial logistic regression models, the first for overall testing rates and the second to compare yearly testing rates by method, both adjusted for sociodemographic factors and comorbidities.
For analyses that computed the proportions of insurees in 2018 who had been tested for colorectal cancer at the recommended intervals, we restricted the dataset to those continuously insured from 2010 to 2018 and tracked insurees backwards to identify bills for faecal occult blood tests in 2018 or 2017 or any colonoscopy between 2010 and 2018. We computed these for each geographical region. Insurees were (a) up to date with any testing for colorectal cancer if they had had at least one colonoscopy in 2010–2018 or any faecal occult blood test in 2017–2018. They were (b) up to date with faecal occult blood test if they were billed for one or more faecal occult blood tests in 2017–2018, with or without a colonoscopy. They were (c) up to date with colonoscopy if they had undergone any colonoscopy in 2010–2018 and no faecal occult blood test in 2017–2018. Data were extracted from the Swiss Health Survey for comparison, using the methods described in a recent publication [12].
The threshold for statistical significance for all analyses was p <0.05. We used Stata software for all statistical analyses. All code is available on request.
For the yearly cross-sectional analyses, we included those aged 50–69 on the last day of the year who were continuously insured in the same basic insurance by CSS for ≥11 months that year. We excluded participants who died or moved during the study year.
We performed an additional analysis of the proportion of participants up to date with testing in 2018, defined as having had a colonoscopy within the last 9 years (not 10 years given limited data) or an faecal occult blood test within the last 2 years. We further restricted the dataset to individuals aged 59–69 years in 2018 who were continuously insured by CSS between 2010 and 2018 (to ensure a 9-year look-back period). We compared insurees living in Vaud to those living in neighbouring cantons with similar inclusion criteria.
We included data from between 288,288 and 323,230 insurees aged 50–69 annually, between 2010 and 2018 (exclusions detailed in figure S1 in the appendix). Table 1 describes the characteristics of the included population in Vaud, neighbouring cantons and the rest of Switzerland, every 4 calendar years (2010–2014–2018). There was consistently a slight majority of women, and the proportion of younger patients (aged 50–59) increased with time. The proportion of participants with managed-care insurance more than doubled in 8 years in all areas. The proportion of participants with a chronic health condition (pharmacy-based cost group ≥1) decreased slightly. Persistent differences existed between Vaud and other cantons, including a higher proportion of women and people aged 50–59 years in Vaud.
Table 1Characteristics of the included population (aged 50–69 years) in Vaud (VD), neighbouring cantons and the rest of Switzerland, every 4 calendar years (2010–2018); CSS database. Exclusion criteria: moved, died or changed insurance during each calendar year. Comparison cantons: neighbouring cantons (NB): Geneva, Neuchâtel, Fribourg and Valais; RS: the rest of Switzerland.
| 2010 | 2014 | 2018 | |||||||||
| VD | NB | RS | VD | NB | RS | VD | NB | RS | |||
| Population (n) | 20,921 | 64,076 | 203,231 | 18,482 | 61,615 | 213,294 | 17,492 | 62,203 | 243,535 | ||
| Gender | Female | % | 54.1 | 51.4 | 50.8 | 54.3 | 51.4 | 50.4 | 54.1 | 51.5 | 50.1 |
| (95% CI) | (53.5–54.8) | (51.1–51.8) | (50.6–51.0) | (53.6–55.0) | (51.0–51.8) | (50.2–50.6) | (53.4–54.9) | (51.1–51.9) | (49.9–50.3) | ||
| Age | 50–59 years | % | 52.1 | 54.2 | 56.3 | 55.4 | 56.8 | 57.4 | 57.3 | 58.2 | 58.6 |
| (95% CI) | (51.4–52.8) | (53.8–54.6) | (56.1–56.5) | (54.7–56.2) | (56.4–57.2) | (57.1–57.6) | (56.6–58.1) | (57.8–58.6) | (58.4–58.7) | ||
| 60–69 years | % | 47.9 | 45.8 | 43.7 | 44.6 | 43.2 | 42.7 | 42.7 | 41.8 | 41.5 | |
| (95% CI) | (47.2–48.6) | (45.4–46.2) | (43.5–43.9) | (43.9–45.3) | (42.8–43.6) | (42.4–42.9) | (42.0–43.4) | (41.4–42.2) | (41.3–41.6) | ||
| Urban status * | Urban | % | 63.6 | 51.73 | 57.7 | 61.6 | 48.9 | 56.8 | 59.3 | 47.6 | 56.3 |
| (95% CI) | (63.0–64.3) | (51.3–52.1) | (57.4–57.9) | (60.9–62.3) | (48.5–49.3) | (56.6–57.0) | (58.6–60.0) | (47.2–48.0) | (56.1–56.5) | ||
| Intermediate | % | 18.8 | 26.1 | 22 | 19.35 | 27.09 | 22.5 | 20.8 | 27.5 | 22.9 | |
| (95% CI) | (18.3–19.3) | (25.8–26.4) | (21.8–22.2) | (18.8–19.9) | (26.7–27.4) | (22.3–22.7) | (20.2–21.4) | (27.1–27.8) | (22.7–23.0) | ||
| Rural | % | 17.6 | 22.2 | 20.4 | 19.1 | 24 | 20.7 | 19.9 | 24.9 | 20.8 | |
| (95% CI) | (17.1–18.1) | (21.9–22.5) | (20.2–20.5) | (18.5–19.6) | (23.7–24.4) | (20.5–20.9) | (19.4– 20.5) | (24.6–25.3) | (20.7–21.0) | ||
| Managed care | Yes** | % | 25 | 24.6 | 36.7 | 43.7 | 42.75 | 52.2 | 56.2 | 55.4 | 65 |
| (95% CI) | (24.4–25.6) | (24.2–24.9) | (36.4–36.9) | (43.0–44.4) | (42.4–43.1) | (51.9–52.4) | (55.5–57.0) | (55.0–55.8) | (64.9–65.2) | ||
| Pharmacy-based cost group | ≥1*** | % | 48.4 | 47.2 | 38.7 | 45.3 | 45.6 | 38.9 | 43.5 | 44.4 | 37 |
| (95% CI) | (47.7–49.1) | (46.8–47.6) | (38.5–38.9) | (44.6–46.0) | (45.2–46.0) | (38.7–39.1) | (42.8–44.2) | (44.0–44.8) | (36.8–37.1) | ||
CSS: a Swiss health insurer; HMO: health maintenance organisation; VD: canton Vaud.
* Determined using the postal code and a list from the Federal Statistical Office of Switzerland.
** Managed care includes family physician, HMO and telemedicine insurance models.
*** Pharmacy-based cost group; method to assess chronic health conditions based on information about medication (≥1: chronic health condition).
Table 2 and figure S2 in the appendix show the evolution of the colorectal cancer testing rate (proportion of insurees who underwent a colonoscopy or faecal occult blood test each year) between 2010 and 2018 by (A) overall testing rates, (B) faecal occult blood test and (C) colonoscopy. The absolute increase in (A) overall testing rates was +4.0% in Vaud, 3.2% in the neighbouring cantons and 1.2% in the rest of Switzerland. The absolute testing rate for (B) faecal occult blood test increased, primarily between 2016 and 2018, by 1.2% in Vaud and 0.9% in the neighbouring cantons, but it decreased by 1.6% in the rest of Switzerland. Testing in the Vaud programme began in 2016, and by 2018, 1.7% of participants in Vaud had an faecal occult blood test within the programme. For(C) colonoscopy data, the absolute increase was 2.9% in Vaud, 2.3% in neighbouring cantons, and 2.7% in the rest of Switzerland (from 4.3% to 7.1%). The number of colonoscopies performed in the screening programme more than doubled from 2016 to 2018 (from 0.6% to 2.0%). In Vaud, 40% of faecal occult blood tests and 26% of colonoscopies in 2018 occurred in the screening programme.
Table 2Change in colorectal cancer testing (% of insurees tested each year), presented as overall testing rates (any test for colorectal cancer), faecal occult blood test and colonoscopy, in those aged 50–69 in Vaud, neighbouring cantons and the rest of Switzerland, between 2010 and 2018. The organised screening programme began at the end of 2015 in Vaud. CSS database years 2010 to 2018. Exclusion criteria: moved, died or changed insurance during each year.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | ||
| VD | N pop | 20,921 | 19,257 | 17,823 | 18,202 | 18,482 | 17,989 | 17,447 | 17,122 | 17,492 |
| Neighbours* | N pop | 64,076 | 59,259 | 58,347 | 60,036 | 61,615 | 60,745 | 60,426 | 60,497 | 62,203 |
| The rest of Switzerland | N pop | 203,231 | 199,556 | 199,888 | 206,086 | 213,294 | 218,030 | 228,012 | 233,769 | 243,535 |
| Overall testing rates | ||||||||||
| Vaud | % | 7.6 | 8.3 | 7.6 | 7.8 | 8.6 | 8.3 | 9.5 | 10.4 | 11.6 |
| (95% CI) | (7.2–8.0) | (7.9–8.7) | (7.2–8.0) | (7.4–8.2) | (8.2–9.0) | (7.9–8.7) | (9.1–10.0) | (9.9–10.9) | (11.2–12.1) | |
| Neighbours | % | 6.1 | 6.0 | 6.1 | 6.2 | 7.0 | 6.9 | 8.7 | 8.7 | 9.3 |
| (95% CI) | (6.0–6.3 ) | (5.8–6.2) | (5.9–6.3) | (6.0–6.4) | (6.8–7.2) | (6.7–7.1) | (8.5–9.0) | (8.5–9.0) | (9.1–9.5) | |
| The rest of Switzerland | % | 7.4 | 7.7 | 7.6 | 7.6 | 8.0 | 7.9 | 8.7 | 8.2 | 8.6 |
| (95% CI) | (7.3–7.5) | (7.6–7.8) | (7.5–7.8) | (7.5–7.7) | (7.9–8.1) | (7.8–8.0) | (8.6–8.9) | (8.1–8.3) | (8.4–8.7) | |
| Faecal occult blood test only or faecal occult blood test and colonoscopy | ||||||||||
| Vaud overall | % | 2.9 | 3.3 | 2.6 | 2.6 | 2.5 | 2.4 | 2.8 | 3.4 | 4.1 |
| (CI) | (2.7–3.2) | (3.0–3.5) | (2.4–2.8) | (2.4–2.9) | (2.3–2.7) | (2.2–2.6) | (2.6–3.1) | (3.2–3.7) | (3.8–4.4) | |
| Vaud in program** | % | – | – | – | – | – | – | 0.7 | 1.3 | 1.7 |
| (CI) | (0.5–0.8) | (1.1–1.5) | (1.5–1.9) | |||||||
| Vaud outside program*** | % | – | – | – | – | – | – | 2.2 | 2.2 | 2.5 |
| (CI) | (2.0–2.4) | (1.9–2.4) | (2.2–2.7) | |||||||
| Neighbours overall | % | 1.7 | 1.6 | 1.5 | 1.4 | 1.5 | 1.5 | 2.2 | 2.2 | 2.6 |
| (CI) | (1.6–1.8) | (1.5–1.7) | (1.4–1.6) | (1.3–1.5) | (1.4–1.6) | (1.5–1.7) | (2.1–2.3) | (2.0–2.3) | (2.4–2.7) | |
| The rest of Switzerland overall | % | 3.1 (3.0–3.2) | 2.8 (2.8–2.9) | 2.6 (2.5–2.7) | 2.3 (2.2–2.3) | 2.0 (2.0–2.1) | 1.8 (1.7–1.9) | 1.8 (1.7–1.8) | 1.6 (1.5–1.6) | 1.5 (1.5–1.6) |
| (CI) | ||||||||||
| Colonoscopy only for any indication | ||||||||||
| Vaud overall | % | 4.7 | 5.0 | 5.0 | 5.2 | 6.1 | 5.9 | 6.7 | 7.0 | 7.5 |
| (CI) | (4.4–5.0) | (4.7–5.3) | (4.7–5.3) | (4.9–5.5) | (5.8–6.5) | (5.6–6.3) | (6.3–7.1) | (6.6–7.4) | (7.1–7.9) | |
| Vaud in program** | % | – | – | – | – | – | 0.0 | 0.6 | 1.0 | 2.0 |
| (CI) | (0.0–0.1) | (0.5–0.7) | (0.9–1.2) | (1.8–2.2) | ||||||
| Vaud outside program*** | % | – | – | – | – | – | 5.9 | 6.1 | 6.0 | 5.5 |
| (CI) | (5.5–6.2) | (5.8–6.5) | (5.6–6.3) | (5.2–5.9) | ||||||
| Neighbours overall | % | 4.4 | 4.4 | 4.6 | 4.8 | 5.5 | 5.4 | 6.5 | 6.6 | 6.7 |
| (CI) | (4.3–4.6) | (4.2–4.6) | (4.4–4.8) | (4.7–5.0) | (1.4–1.6) | (5.2–5.6) | (6.3–6.7) | (6.4–6.8) | (6.5–6.9) | |
| The rest of Switzerland overall | % | 4.3 | 4.8 | 5.0 | 5.3 | 6.0 | 6.1 | 7.0 | 6.7 | 7.1 |
| (CI) | (4.2–4.4) | (4.7–4.9) | (4.9–5.1) | (5.2–5.4) | (5.8–6.1) | (6.0–6.2) | (6.9–7.1) | (6.6–6.8) | (6.9–7.2) | |
CSS: a Swiss health insurer
* Includes neighbouring cantons: Geneva (GE), Neuchâtel (NE), Fribourg (FR) and Valais (VS).
** In programme = people who were included in the programme and did not have to pay deductible and co-pay. After 2015, this testing was billed using a specific code.
*** Inside/outside the programme was only distinguishable from 2015 (for colonoscopy) and from 2016 (for faecal occult blood test/both), before which it was billed under the same code for insurance
Table 3 shows a comparison between the distribution of faecal occult blood tests inside and outside the screening programme by sociodemographic characteristics in 2018 in Vaud. During that year, 785 patients were screened, of whom 307 were in the screening programme. Participants in the programme were younger, had fewer comorbidities and were more likely to have a high-deductible health plan than those tested outside the programme.
Table 3Comparison of the proportion of faecal occult blood tests inside and outside the Vaud screening program, for insurees aged 50–69 years in 2018. CSS database. Statistical comparisons used the chi-squared test.
| Faecal occult blood test or both | |||||
| Outside | n = 478 | Inside | n = 307 | p | |
| Gender % (CI) | 0.950 | ||||
| Female | 57 (52–61) | 272 | 57 (51–63) | 174 | |
| Male | 43 (39–48) | 206 | 43 (38–49) | 133 | |
| Deductible_cat* % (CI) | 0.001 | ||||
| Low | 76 (72–80) | 363 | 66 (60–71) | 201 | |
| High | 24 (20–28) | 115 | 35 (29–40) | 106 | |
| Pharmacy-based cost group** % (CI) | 0.003 | ||||
| 0 | 41 (36–45) | 195 | 52 (46–58) | 159 | |
| >1 | 59 (55–64) | 283 | 48 (43–54) | 148 | |
| Age % (CI) | 0.039 | ||||
| 50–54 years | 20 (16–24) | 95 | 22 (17–27) | 66 | |
| 55–59 years | 29 (25–34) | 140 | 34 (29–40) | 104 | |
| 60–64 years | 21 (17–25) | 99 | 24 (19–29) | 73 | |
| 65–69 years | 30 (26–35) | 144 | 21 (16–26) | 64 | |
| Urban status*** % (CI) | 0.014 | ||||
| Urban | 54 (50–59) | 260 | 57 (52–63) | 176 | |
| Intermediate | 29 (25–33) | 137 | 20 (16–25) | 62 | |
| Rural | 17 (14–21) | 81 | 23 (18–28) | 69 | |
CSS: a Swiss health insurer
* Deductible categories (low: 300 or 500 CHF; high: 1,000 or 2,500 CHF).
** Pharmacy-based cost group; method to assess chronic health conditions based on information about medication (≥1: chronic health condition).
*** Determined using the postal code and a list from the Federal Statistical Office of Switzerland.
Table 4 presents the odds ratio (OR) of being tested for colorectal cancer in each calendar year between 2011 and 2018 compared to 2010. After multivariate adjustment, we found that people in Vaud were more likely to be tested for colorectal cancer than in neighbouring cantons using any test (overall OR 1.27, 95% CI 1.24–1.30), faecal occult blood test (OR 1.87, 95% CI 1.79–1.96) or colonoscopy (OR 1.09, 95% CI 1.06–1.12). The faecal occult blood test and colonoscopy testing rates increased more after 2016 than before this year. A test for interaction between year and canton (“time x cantons”) was slightly less than 1, suggesting that although screening rates in Vaud were higher throughout the period, the increase in the rate in Vaud after 2016 was less than that of neighbouring cantons (OR 0.95, 95% CI 0.91–0.99). We performed two sensitivity analyses: first, we compared Vaud to all the rest of Switzerland, which gave a positive interaction term, suggesting that the rate of increase in Vaud was greater after the implementation of the programme (table S2 in the appendix). Second, we excluded Geneva from the list of neighbouring cantons (because of an intervention in GP practices there) and obtained similar results (not shown).
Table 4Odds ratio of being tested for colorectal cancer within each calendar year (2011–2018) for 50–69-year-old insurees, in (A) any test for colorectal cancer (faecal occult blood test or colonoscopy)*, (B) faecal occult blood test** or (C) colonoscopy**, in canton Vaud compared to neighbouring cantons before and after the launch of the Vaud organised screening programme in 2015. CSS database.
| (A) Testing overall* | (B) faecal occult blood test** | (C) Colonoscopy only** | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Canton of residence | Neighbouring cantons1 | 1 | 1 | 1 | |||
| Vaud | 1.27 | 1.24–1.30 | 1.87 | 1.79–1.96 | 1.09 | 1.06–1.12 | |
| Time x cantons interaction2 | 0.95 | 0.91–0.99 | 0.86 | 0.80–0.92 | 0.99 | 0.94–1.03 | |
| Sex | Female | 1 | 1 | 1 | |||
| Male | 1.05 | 1.03–1.07 | 0.98 | 0.95–1.01 | 1.07 | 1.05–1.09 | |
| Age | 50–59 years | 1 | 1 | 1 | |||
| 60–69 years | 1.23 | 1.21–1.25 | 1.34 | 1.29–1.38 | 1.19 | 1.17–1.22 | |
| Area of residence | Urban | 1 | 1 | 1 | |||
| Intermediate | 1.05 | 1.03–1.07 | 1.56 | 1.50–1.62 | 0.91 | 0.89–0.93 | |
| Rural | 0.90 | 0.88–0.92 | 1.31 | 1.26–1.37 | 0.78 | 0.76–0.81 | |
| Comorbidities | No pharmacy-based cost group groups | 1 | 1 | 1 | |||
| Pharmacy-based cost group groups n ≥1 | 1.71 | 1.68–1.74 | 1.66 | 1.60–1.72 | 1.72 | 1.69–1.76 | |
| Insurance type | No managed-care model | 1 | 1 | 1 | |||
| Managed-care model3 | 1.05 | 1.03–1.07 | 1.06 | 1.02–1.09 | 1.05 | 1.03–1.07 | |
| Year | 2010 | 1 | 1 | 1 | |||
| 2011 | 1.01 | 1.0–1.1 | 1.02 | 0.95–1.09 | 1.02 | 0.97–1.07 | |
| 2012 | 1.01 | 1.0–1.1 | 0.91 | 0.84–0.98 | 1.05 | 1.00–1.10 | |
| 2013 | 1.03 | 1.0–1.1 | 0.85 | 0.79–0.92 | 1.11 | 1.05–1.16 | |
| 2014 | 1.17 | 1.1–1.2 | 0.92 | 0.85–0.99 | 1.28 | 1.23–1.34 | |
| 2015 | 1.14 | 1.1–1.2 | 0.91 | 0.84–0.97 | 1.25 | 1.20–1.31 | |
| 2016 | 1.46 | 1.4–1.5 | 1.32 | 1.23–1.42 | 1.53 | 1.46–1.60 | |
| 2017 | 1.49 | 1.4–1.6 | 1.37 | 1.27–1.47 | 1.56 | 1.49–1.63 | |
| 2018 | 1.64 | 1.6–1.7 | 1.65 | 1.54–1.76 | 1.64 | 1.57–1.71 | |
CSS: a Swiss health insurer; OR: odds ratio.
* OR of being tested for faecal occult blood test or colonoscopy versus no test for each calendar year.
Results from multivariate-adjusted logistic regression model adjusted for sex, age, pharmacy-based cost group category, managed-care model, year considered, canton Vaud vs neighbouring cantons. Interaction term added testing the interaction between periods before the organised screening programme (years 2011–2014 vs 2015–2018) and canton Vaud vs neighbouring cantons.
** OR of being tested by faecal occult blood test only (or faecal occult blood test and colonoscopy) or colonoscopy only vs no test for each calendar year.
Results from multivariate-adjusted multinomial model adjusted for sex, age, pharmacy-based cost group category, managed-care model, year considered, canton Vaud vs neighbouring cantons. Interaction term added testing the interaction between periods before the organised screening programme (years 2011–2014 vs 2015–2018) and canton Vaud vs neighbouring cantons.
1 Comparison cantons: Geneva (GE), Fribourg (FR), Neuchâtel (NE), Valais (VS).
2 Interaction between time (2010–2012 versus 2015–2018) and location (Vaud).
3 The following models were considered managed-care: HMO, telemedicine, family physician.
In Vaud in 2018, we found that 49.1% of the insurees were up to date with colorectal cancer testing (table S3 in the appendix), compared to 42% in neighbouring cantons.
Using data from a large insurance company, we found that the overall colorectal cancer testing increased substantially throughout Switzerland between 2010 and 2018 in the context of a new reimbursement law for colorectal cancer screening tests. The screening rates were consistently higher in Vaud than in neighbouring cantons, with greater absolute increases after the introduction of a screening programme in 2015. By 2018, 40% of faecal occult blood tests and 26% of colonoscopies in Vaud occurred in the screening program, including a greater proportion of younger patients with high-deductible health plans.
Our findings are consistent with recent studies showing a steady increase in colorectal cancer screening rates in Switzerland. A similar study used CSS claims data in canton Uri, which was the first Swiss canton to implement a screening programme, in 2014. It found an increase in colorectal cancer screening rates of 2.1%, from 8.7% to 10.8% [15], a lower magnitude than observed in our results (versus +4% in Vaud). The 4% absolute increase over 10 years included a 3% increase in the 4 years after implementing the programme, which was a 35% relative increase. This increase is similar to that seen after the implementation of a screening programme in Ontario, Canada, in 2008, also in the context of significant opportunistic screening [22]. In Vaud in 2018, we found that 49% of people with CSS insurance were up to date with colorectal cancer testing. In 2017, a cross-sectional data collection from the Swiss Sentinel Surveillance Network showed that 45% of patients had been tested for colorectal cancer within the recommended intervals [23]. The European Commission set a colorectal cancer screening rate of 45% in the average-risk population as an acceptable goal, along with a desirable rate of 65% [24]. In Germany, the USA and the UK, the proportion of the eligible population up to date with colorectal cancer testing varied between 60% and 67% between 2013 and 2016 [25–27]. Our study supports the previous statement that the reimbursement of colorectal cancer screening tests could increase testing rates [6].
Previous studies have shown a clear socioeconomic gradient in colorectal cancer testing in Switzerland, with lower screening by younger citizens with high-deductible health plans [6, 12]. We found that those participating in the screening programme were younger and healthier and had higher-deductible plans than those tested outside the programme. These findings confirm the hypothesis that a screening programme could reach a different portion of the population, potentially increasing the proportion of patients who are tested [28]. These early encouraging results support the push by the Swiss Cancer League to implement organised programmes in as many cantons as possible.
Despite a growing proportion of screening tests in Vaud occurring within the screening program, the rate of the increase of testing was not greater in Vaud than in the neighbouring cantons without a screening programme. This contrasts with the difference between Uri and its neighbours after the implementation of the Uri programme [15]. One explanation is the slow roll-out of mailings to the general population by the Vaud programme, planned to take 7 years. Another possibility is the substantial increase in faecal occult blood test use in neighbouring cantons, a trend not observed in the German-speaking part of Switzerland. The decrease in faecal occult blood test use in German-speaking cantons occurred despite the PharmaSuisse campaign that distributed FITs in pharmacies throughout Switzerland [29]. This could be due to a “spill-over effect” from starting a programme in Vaud to the other French-speaking cantons (i.e. more media attention, diffusion via medical publications).
Our study has several strengths. First, we used a large dataset going back to 2010, giving sufficient statistical precision for subgroup analyses. Second, datasets from health insurance are updated every year, more rapidly showing change than those from the quinquennial Swiss Health Interview Survey. Third, insurance data capture screening use both within and outside the organised screening programme, which is very important in the context of ongoing opportunistic screening.
Our study also has several limitations. First, the dataset comes from a single large health insurer (CSS) covering around 16% of the Swiss population and only 10% of the canton Vaud. This insurance covers a greater proportion of the population in central Swiss cantons than in Vaud, and it may be chosen by different sectors of the population, as evidenced by differences between groups at the same time points in table 1 [16]. However, the higher screening rates seen in Vaud persisted after adjustment for several confounders. Controlling for confounding, such as physician practice patterns, may nonetheless be unmeasured or incomplete. Second, the dataset includes colorectal cancer screening tests performed between 2010 and 2018, regardless of the indication (i.e. for symptoms, surveillance or screening). Third, greater weight is probably given to colonoscopies because not all faecal occult blood tests were collected; we can assume that not all tests are submitted for insurance reimbursement and that every pathological faecal occult blood test leads to a diagnostic colonoscopy. Moreover, many people certainly had repeated testing between 2010 and 2018 and are thus overrepresented in the primary analysis. However, in table S2, we created a longitudinal cohort and obtained similar results. Fourth, some neighbouring cantons implemented projects to increase screening before organised programmes, which may mask the effect of the organised programme in Vaud. Therefore, we repeated a sensitivity analysis without Geneva and found the same results. Fifth, other factors could have played a role in the increase in screening tests since 2010, beyond the 2013 federal law and the new screening programme. These include ongoing sensitisation campaigns about colorectal cancer screening, healthcare system and provider factors (clinician recommendation), and psychosocial factors (e.g. related to knowledge about colorectal cancer and screening, risk perception, and perceived barriers and benefits) [30]. However, we have no reason to believe that these factors differently impacted the different regions considered in our study. Finally, we did not publish a protocol before beginning the analysis, though our analytical approach was chosen a priori based on recent work by Bissig et al. [15].
This study confirmed the overall increase in colorectal cancer screening rates since 2010 in Switzerland, with larger increases in Vaud, where the first organised colorectal cancer screening programme was implemented. The testing rates also increased in neighbouring cantons, possibly reflecting changes in testing patterns by general practitioners or testing use in the community, but with smaller increases than in Vaud. Our results suggest that the Vaud programme reached a different subpopulation (with high-deductible health plans, 50–59 years old, and with fewer comorbidities) compared to those being tested outside the programme (opportunistic screening). Taken together, these findings support a greater implementation of organised programmes in Switzerland. Future research should examine the impact of organisational differences between programmes and easier access to faecal occult blood test on testing rates.
This work was supported by the funds from the Swiss Cancer Research Foundation, Health Services Research (HSR-4366-11-2017) and the Swiss National Science Foundation, National Research Program 74 (NFP74 407440_167519) “Smarter Health Care”. Dr Kevin Selby received salary support from the Leenaards Foundation. The funders had no role in the design or conduct of the study, in the collection, management, analysis, or interpretation of data, or in the preparation, review, or approval of the manuscript.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Office Fédéral de la Statistique (OFS) . Le cancer en Suisse, rapport 2021. Available from: https://www.bfs.admin.ch/news/fr/2021-0245
2. Bulliard JL , Ducros C , Levi F . Dépistage organisé du cancer colorectal: défis et enjeux pour un essai pilote en Suisse. Rev Med Suisse. 2012 Jul;8(348):1464–7.
3. von Karsa L , Patnick J , Segnan N , Atkin W , Halloran S , Lansdorp-Vogelaar I , et al.; European Colorectal Cancer Screening Guidelines Working Group . European guidelines for quality assurance in colorectal cancer screening and diagnosis: overview and introduction to the full supplement publication. Endoscopy. 2013;45(1):51–9.
4. Davidson KW , Barry MJ , Mangione CM , Cabana M , Caughey AB , Davis EM , et al.; US Preventive Services Task Force . Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021 May;325(19):1965–77. https://doi.org/10.1001/jama.2021.6238
5. Arditi C , Peytremann-Bridevaux I , Burnand B , Eckardt VF , Bytzer P , Agréus L , et al.; EPAGE II Study Group . Appropriateness of colonoscopy in Europe (EPAGE II). Screening for colorectal cancer. Endoscopy. 2009 Mar;41(3):200–8. https://doi.org/10.1055/s-0028-1119626
6. Braun AL , Kässner A , Syrogiannouli L , Selby K , Bulliard JL , Martin Y , et al. Association between colorectal cancer testing and insurance type: Evidence from the Swiss Health Interview Survey 2012. Prev Med Rep. 2020 May;19:101111. https://doi.org/10.1016/j.pmedr.2020.101111
7. Auer R , et al. Programme cantonal vaudois de dépistage du cancer colorectal: information et décision partagée., Revue médicale suisse, vol. 11, no. 2209-15, 2015.
8. Basu P , et al. Status of implementation and organization of cancer screening in The European Union Member States—Summary results from the second European screening report, vol. 142, no. 1, pp. 44-56, 2018. https://doi.org/10.1002/ijc.31043
9. R. Schneider et al. Ten-year changes in colorectal cancer screening in Switzerland: the Swiss Health Interview Survey 2007, 2012 and 2017. Primary and Hospital Care 2021;21(Suppl.11). Poster presentation in SSMIG congress, 2021.
10. Département fédéral de l'intérieur. Ordonnance du DFI sur les prestations dans l'assurance obligatoire des soins en cas de maladie. 1995 (Etat le 1er février 2021).
11. Stratégies nationales contre le cancer. Les standards nationaux de qualité pour le dépistage du cancer colorectal en Suisse. Personnes asymptomatiques sans risque élevé. In: Standards de qualité pour le dépistage du cancer colorectal en Suisse, 2020.
12. Schneider R , Näpflin M , Syrogiannouli L , Bissig S , Tal K , Bulliard JL , et al. Change in Colorectal Cancer Tests Submitted for Reimbursement in Switzerland 2012-2018: Evidence from Claims Data of a Large Insurance. Int J Public Health. 2021 Oct;66:1604073. https://doi.org/10.3389/ijph.2021.1604073
13. Ligue contre le cancer. Le cancer du côlon et du rectum. Carcinome colorectal. Informations de la Ligue contre le cancer pour les personnes touchées et leurs proches. 2e édition revue et augmentée, 2015.
14. Swiss Confderation (2011). Federal Act on Research involving Human Beings. https://www.fedlex.admin.ch/eli/cc/2013/617/en
15. Bissig S , Syrogiannouli L , Schneider R , Tal K , Selby K , Del Giovane C , et al. Change in colorectal cancer (CRC) testing rates associated with the introduction of the first organized screening program in canton Uri, Switzerland: evidence from insurance claims data analyses from 2010 to 2018. Prev Med Rep. 2022 Jun;28:101851. https://doi.org/10.1016/j.pmedr.2022.101851
16. CSS assurance. Rapport de gestion 2019. Groupe CSS Rapport de gestion, 2019, p. 13.
17. Fischer R , Collet TH , Zeller A , Zimmerli L , Gaspoz JM , Giraudon K , et al. Obesity and overweight associated with lower rates of colorectal cancer screening in Switzerland. Eur J Cancer Prev. 2013 Sep;22(5):425–30. https://doi.org/10.1097/CEJ.0b013e32835f3b87
18. Marbet UA , Bauerfeind P , Brunner J , Dorta G , Valloton JJ , Delcò F . Colonoscopy is the preferred colorectal cancer screening method in a population-based program. Endoscopy. 2008 Aug;40(8):650–5. https://doi.org/10.1055/s-2008-1077350
19. Lamers LM . Pharmacy costs groups: a risk-adjuster for capitation payments based on the use of prescribed drugs. Med Care. 1999 Aug;37(8):824–30. https://doi.org/10.1097/00005650-199908000-00012
20. Lamers LM , van Vliet RC . The Pharmacy-based Cost Group model: validating and adjusting the classification of medications for chronic conditions to the Dutch situation. Health Policy. 2004 Apr;68(1):113–21. https://doi.org/10.1016/j.healthpol.2003.09.001
22. Lamers LM , Vliet RC . Health-based risk adjustment Improving the pharmacy-based cost group model to reduce gaming possibilities. Eur J Health Econ. 2003;4(2):107–14. https://doi.org/10.1007/s10198-002-0159-9
23. Cancer Care Ontario . Ontario Cancer Screening Performance. Report 2016. Toronto: Cancer Care Ontario; 2016.
24. Braun AL , et al. Variation in colorectal cancer testing between primary care physicians: a cross-sectional study in Switzerland, vol. 64, no. 7, pp. 1075-1083, 2019.
24. Segnan JP . L von Karsa , European Guidelines for Quality Assurance in Colorectal cancer screening and diagnosis - first edition. European comission, 2010.
25. Chen C , Stock C , Jansen L , Chang-Claude J , Hoffmeister M , Brenner H . Trends in colonoscopy and fecal occult blood test use after the introduction of dual screening offers in Germany: results from a large population-based study, 2003-2016. Prev Med. 2019 Jun;123:333–40. https://doi.org/10.1016/j.ypmed.2019.03.048
26. DeGroff A , Sharma K , Satsangi A , Kenney K , Joseph D , Ross K , et al. Increasing Colorectal Cancer Screening in Health Care Systems Using Evidence-Based Interventions. Prev Chronic Dis. 2018 Aug;15:E100. https://doi.org/10.5888/pcd15.180029
27. Cardoso R , Guo F , Heisser T , Hoffmeister M , Brenner H . Utilisation of colorectal cancer screening tests in european countries by type of screening offer: results from the european health interview survey. Cancers (Basel). 2020 May;12(6):1409. https://doi.org/10.3390/cancers12061409
28. Selby K , Jensen CD , Levin TR , Lee JK , Schottinger JE , Zhao WK , et al. Program Components and Results From an Organized Colorectal Cancer Screening Program Using Annual Fecal Immunochemical Testing. Clin Gastroenterol Hepatol. 2022 Jan;20(1):145–52. https://doi.org/10.1016/j.cgh.2020.09.042
29. PharmaSuisse . (2019). Analyse de la prestation «Dépistage du cancer du côlon» réalisée par les pharmacies affiliées à pharmaSuisse. https://www.pharmasuisse.org/data/docs/fr/20985/190320-Datenerhebung-Darmkrebsvorsorge-2018.pdf?v=1.0
30. Gimeno García AZ . Factors influencing colorectal cancer screening participation. Gastroenterol Res Pract. 2012;2012:483417. https://doi.org/10.1155/2012/483417
Table S1Extracted colorectal cancer testing billing codes.
| Catalog | Code | Description |
| TARMED | 19.06 | Colonoscopy |
| TARMED | 19.07 | Sigmoidoscopy |
| Tarif code | 0001.1220.002 | Colonoscopy with biopsy program Vaud |
| Tarif code | 0001.1221.002 | Colonoscopy-only program Vaud |
| Tarif code | 0001.1222.002 | Colonoscopy with polypectomy program Vaud |
| AL | 1583.00 | Occult blood |
| AL | 1583.01 | Occult blood |
| Tarif code | 0001.1234.001 | faecal occult blood test in program UR |
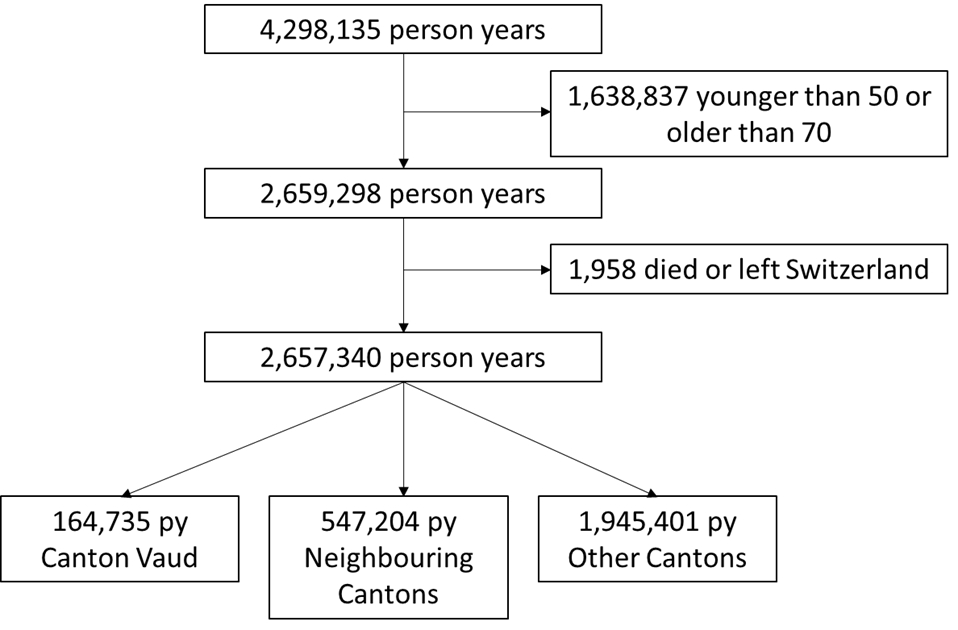
Figure S1 Exclusions.
Table S2Odds ratio of being tested for colorectal cancer within each calendar year (2011–2018) for 50–69-year old insures, in (A) Any test for colorectal cancer (faecal occult blood test or colonoscopy)*, B) faecal occult blood test** or C) colonoscopy)**; in canton Vaud compared to neighbouring cantons & the rest of Switzerland (i.e. all other cantons) before and after the launch of the Vaud organized screening program in 2015. CSS database.
| Testing overall* | Faecal occult blood test** | Colonoscopy only** | |||||
| OR | 95% CI | OR | 95 % CI | OR | 95% CI | ||
| Canton of residence | Rest of Switzerland1 | 1 | 1 | 1 | |||
| Vaud | 1.05 | 1.03–1.08 | 1.18 | 1.14–1.23 | 1.00 | 0.98–1.02 | |
| Time x cantons interaction2 | 1.16 | 1.12–1.20 | 1.67 | 1.57–1.77 | 1.03 | 0.98–1.08 | |
| Sex | Female | 1 | 1 | 1 | |||
| Male | 1.09 | 1.08–1.10 | 1.15 | 1.13–1.17 | 1.07 | 1.06–1.08 | |
| Age | 50–59 years | 1 | 1 | 1 | |||
| 60–69 years | 1.26 | 1.25–1.27 | 1.41 | 1.38–1.43 | 1.21 | 1.20–1.22 | |
| Area of residence | Urban | 1 | 1 | 1 | |||
| – Intermediate | 1.00 | 0.99–1.01 | 1.06 | 1.04–1.08 | 0.98 | 0.97–0.99 | |
| – Rural | 0.88 | 0.87–0.89 | 0.96 | 0.94–0.98 | 0.86 | 0.85–0.87 | |
| Comorbidities | No pharmacy-based cost groups | 1 | 1 | 1 | |||
| Pharmacy-based cost group s n≥1 | 1.71 | 1.69–1.72 | 1.63 | 1.60–1.66 | 1.74 | 1.72–1.76 | |
| Insurance type | No managed care model | 1 | 1 | 1 | |||
| Managed care model3 | 1.01 | 1.00–1.02 | 1.03 | 1.01–1.05 | 0.99 | 0.99–1.01 | |
| Year | 2010 | 1 | 1 | 1 | |||
| 2011 | 1.03 | 1.01–1.06 | 0.95 | 0.92–0.98 | 1.09 | 1.06–1.12 | |
| 2012 | 1.03 | 1.01–1.05 | 0.87 | 0.84–0.90 | 1.13 | 1.10–1.16 | |
| 2013 | 1.03 | 1.01–1.05 | 0.76 | 0.74–0.79 | 1.20 | 1.17–1.23 | |
| 2014 | 1.11 | 1.09–1.14 | 0.72 | 0.70–0.75 | 1.36 | 1.33–1.39 | |
| 2015 | 1.10 | 1.08–1.12 | 0.66 | 0.63–0.68 | 1.38 | 1.35–1.41 | |
| 2016 | 1.26 | 1.24–1.29 | 0.69 | 0.67–0.72 | 1.62 | 1.58–1.66 | |
| 2017 | 1.21 | 1.19–1.23 | 0.64 | 0.62–0.66 | 1.57 | 1.53– 1.60 | |
| 2018 | 1.28 | 1.26–1.31 | 0.67 | 0.65–0.70 | 1.67 | 1.63–1.71 | |
* OR of being tested for faecal occult blood test or colonoscopy versus no test for each calendar year.
Results from multivariate adjusted logistic regression model adjusted for sex, age, pharmacy-based cost group categories, managed care model, Year considered, Canton Vaud vs the other neighbouring cantons. Interaction term added testing the interaction between period before the organized screening program (years 2011-2014 vs 2015–2018) and canton Vaud vs the other cantons.
** OR of being tested for faecal occult blood test only (or faecal occult blood test and colonoscopy) or colonoscopy only versus no test for each calendar year.
Results from multivariate adjusted multinomial model adjusted for sex, age, pharmacy-based cost group categories, managed care model, Year considered, Canton Vaud vs the other neighbouring cantons. Interaction term added testing the interaction between period before the organized screening program (years 2011–2014 vs 2015–2018) and canton Vaud vs the other cantons.
1: Comparison cantons: Geneva (GE), Fribourg (FR), Neuchâtel (NE), Valais (VS); 2: Interaction between time (2010–2012 versus 2015–2018) and location (Vaud); 3: following models considered “Managed Care”: HMO, Telemedicine, family physician
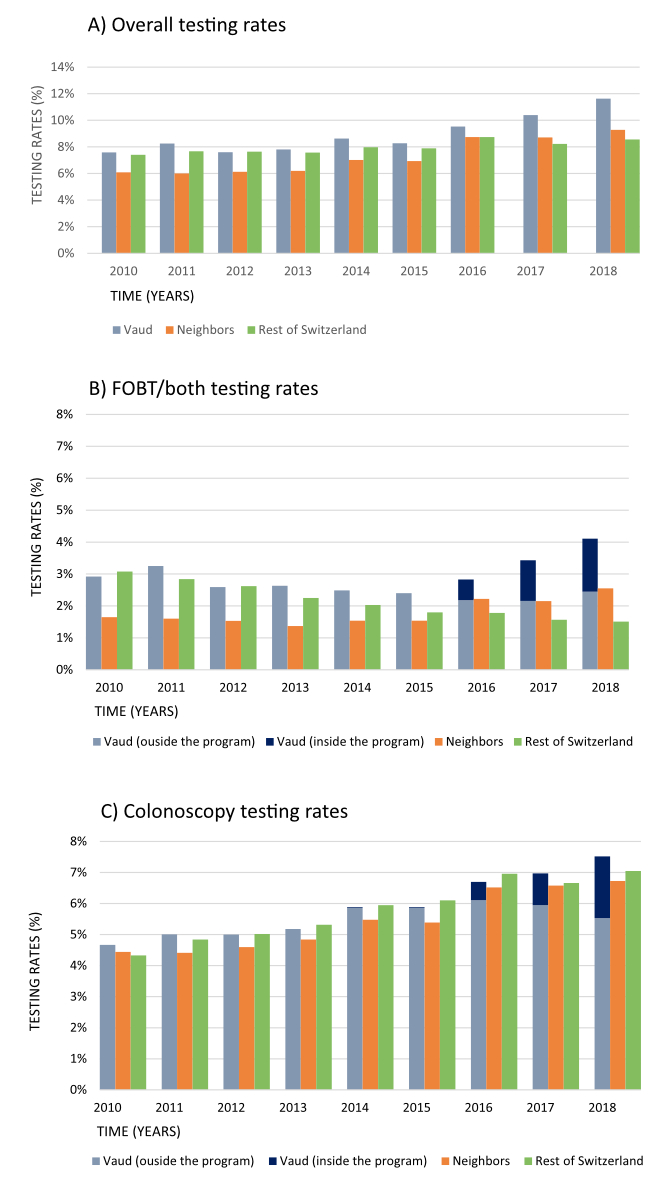
Figure S2 Change in colorectal cancer testing (% of insures tested each year) presented as: A) overall testing rates (any test for colorectal cancer), B) faecal occult blood test; and C) colonoscopy in those aged 50–69 in Vaud, neighbouring cantons and the rest of Switzerland, between 2010 and 2018. The organized screening program for colorectal cancer began in 2015 in Vaud. CSS database years 2010 to 2018.
Table S3Proportion of population up to date with testing (colonoscopy within last 9 years or faecal occult blood test within last 2 years) in SHS+ population in 2017 and CSS population in 2018 respectively, aged 59 to 69 for Vaud and neighbouring cantons; SHS database 2017 and CSS database 2018 *
| Testing overall* | Faecal occult blood test** | Colonoscopy*** | ||||
| Vaud | Neighbours | Vaud | Neighbours | Vaud | Neighbours | |
| Percentage in CSS dataset 2018 [% (CI)] | 49.1 (47.4–50.6) | 41.6 (40.9–42.4) | 11.7 (10.7–12.6) | 7.6 (7.2–8.0) | 41.1 (39.6–42.5) | 36.9 (36.1–37.6) |
| N tested / N total | 2222/4523 | 6584/15818 | 527/4523 | 1205/15818 | 1858/4523 | 5835/15818 |
| Percentage in SHS* dataset 2017 [ % (CI)} | 53.1 (46.6–59.5) | 50.6 (46.3–54,9) | 12.9 (9.1–17.8) | 15.1 (12.2–18.5) | 41.0 (34.8–47.5) | 35.7 (31.6–39.9) |
| N tested/ N total ** | 143/266 | 303/602 | 34/266 | 87/602 | 109/266 | 216/602 |
* Any colorectal cancer test in recommended interval (faecal occult blood test in last 2 years or colonoscopy in last 10 years)
** faecal occult blood test only in last 2 years or faecal occult blood test in last 2 years and colonoscopy in last 10 years
*** Colonoscopy in last 10 years and no faecal occult blood test in last 2 year