Parental willingness to have children vaccinated against COVID-19 in Geneva, Switzerland: a cross-sectional population-based study
DOI: https://doi.org/10.57187/smw.2023.40049
Hélène
Bayssona, Nick
Pullena, Carlos
de Mestrala, Claire
Semaania, Francesco
Pennacchioa, María-Eugenia
Zaballaa, Arnaud G.
L’Huillierb, Elsa
Lorthea, Idris
Guessousc d, Silvia
Stringhiniace, the Specchio-COVID19 study group***
a Unit of
Population Epidemiology, Division of Primary Care Medicine, Geneva University
Hospitals, Geneva, Switzerland
b Pediatric
Infectious Diseases Unit, Geneva University Hospitals and Faculty of Medicine,
Geneva, Switzerland
c Department
of Health and Community Medicine, Faculty of Medicine, University of Geneva,
Geneva, Switzerland
d Division
and Department of Primary Care Medicine, Geneva University Hospitals, Geneva,
Switzerland
e University
Center for General Medicine and Public Health, University of Lausanne,
Lausanne, Switzerland
*, ** These first authors and last
authors, respectively, contributed equally to this work
*** Members are listed at the end
Hélène Baysson, MD
Unit of Population
Epidemiology
Geneva University Hospitals
CH-1200 Geneva
helene.baysson[at]unige.ch
Summary
OBJECTIVE: We aimed to examine factors associated with parental
willingness to vaccinate their children against COVID-19.
METHODS: We surveyed adults included in a digital longitudinal cohort study
composed of participants in previous SARS-CoV-2 serosurveys conducted in
Geneva, Switzerland. In February 2022, an online questionnaire collected
information on COVID-19 vaccination acceptance, parental willingness to
vaccinate their children aged ≥5 years and reasons for vaccination preference. We
used multivariable logistic regression to assess the demographic, socioeconomic
and health-related factors associated with being vaccinated and with parental
intention to vaccinate their children.
RESULTS: We included 1,383 participants (56.8% women; 69.3% aged 35–49
years). Parental willingness to vaccinate their children increased markedly
with the child’s age: 84.0%, 60.9% and 21.2%, respectively, for parents of
adolescents aged 16–17 years, 12–15 years and 5–12 years. For all child age
groups, unvaccinated parents more frequently indicated not intending to
vaccinate their children than vaccinated parents. Refusal to vaccine children
was associated with having a secondary education (1.73; 1.18–2.47) relative to
a tertiary education and with middle (1.75; 1.18–2.60) and low (1.96; 1.20–3.22)
household income relative to high income. Refusal to vaccine their children was
also associated with only having children aged 12–15 years (3.08; 1.61–5.91), aged
5–11 years (19.77; 10.27–38.05), or in multiple age groups (6.05; 3.22–11.37),
relative to only having children aged 16–17 years.
CONCLUSION: Willingness to vaccinate children was high for parents of adolescents
aged 16–17 years but decreased significantly with decreasing child age.
Unvaccinated, socioeconomically disadvantaged parents and those with younger
children were less likely to be willing to vaccinate their children. These
results are important for vaccination programs and developing communication
strategies to reach vaccine-hesitant groups, both in the context of COVID-19 and
in the prevention of other diseases and future pandemics.
Introduction
Vaccination
against COVID-19 has proven efficacy to reduce transmission, limit disease severity,
and prevent hospitalisations and post-COVID syndrome, including in children as
young as five years [1–4]. Mass vaccination in Switzerland began on 23 December
2020, with priority given to individuals aged 65 years and older, those with chronic
diseases deemed ‘particularly vulnerable to COVID-19’ and health workers.
Subsequently, vaccination eligibility progressively extended to include all
persons aged ≥16 years (May 2021), children aged ≥12 years (June 2021) and
children aged ≥5 years (December 2021) [5]. Since vaccines became available,
public and scientific debate has been ongoing on the need for and relevance of
vaccinating children, whereas the vaccination of adolescents is strongly
recommended and generally accepted [6–8]. Although the disease burden
(infection severity and short-term effects) in children and adolescents has
been relatively low, when infected with SARS-CoV-2, they can transmit the virus
to others [9]. Children and adolescents with COVID-19 have a low risk of
multisystemic inflammatory syndrome [10] and a low to moderate risk of long
COVID [11–13], but they may face educational disruptions, social isolation and
poor wellbeing [14–16]. Available vaccination data highlight the safety of the
COVID-19 vaccination among children and adolescents [3, 17, 18]. In
Switzerland, COVID-19 vaccination is recommended for children and adolescents
to protect them from severe forms of COVID-19 and post-COVID syndrome [2, 19]. It
is also highly recommended for children and adolescents with a chronic illness
and those who are in close contact with others at high risk, such as people
with a weakened immune system [20]. In addition, from a public health
perspective, vaccination among children and adolescents will de facto increase
general vaccination coverage and potentially reduce viral circulation in the
population.
Worldwide,
parental willingness to vaccinate their children for common childhood diseases
varies greatly across populations, often depending on psychosocial,
sociocultural, socioeconomic and political factors [21–23]. Understanding the factors
associated with parental willingness to vaccinate children is important for
tailoring vaccination campaigns with the objective of an overall vaccination
increase. Among adults, COVID-19 vaccine acceptance has evolved since the
beginning of the pandemic as a function of its evolution and the establishment
of containment measures [24–26].
As the pandemic continues,
with new variants driving new waves of transmission, and the immune landscape in
the population shows decreasing immune protection against emerging variants, vaccination
will continue to play a key role in minimising infections, protecting health care
workers and vulnerable patients and preventing overburdening health care
systems. Monitoring the level of vaccination acceptance in the population,
including among children and adolescents, is essential for this. This study aimed
to examine parental willingness to have children vaccinated against COVID-19
and explored potentially related sociodemographic factors.
Methods
Study design, setting
and sample
This study was
embedded in the longitudinal digital cohort study Specchio-COVID19. The cohort
was launched in December 2020 to follow the participants of COVID-19 serosurveys
conducted in the canton of Geneva, Switzerland. Its main objective is to monitor
COVID-19-related symptoms, SARS-CoV-2 seroconversion, and the overall impact of
the pandemic on several dimensions of health and socioeconomic factors for at
least 2 years [27]. The participants were randomly selected from the general population
at three time points: for the first serosurvey, April–June 2020, participants aged
20–75 years were enrolled from a previous general health survey (Bus Santé) representative
of the population of Geneva [25]; for the second and third serosurveys (November–December
2020 and June–July 2021), participants were recruited from random
samples provided by the Federal Statistics Office of individuals living in
Geneva aged 0–64 years [29, 30].
Following
participation in one of these serosurveys, participants were invited to join
the Specchio-COVID19 cohort study, consisting of periodic online questionnaires
and potential serological follow-up [31]. Upon registration, an initial
questionnaire collected sociodemographic and lifestyle characteristics and general
health-related information. Self-reported SARS-CoV-2 infections and vaccination
status were updated through monthly questionnaires. The vaccination questionnaire
designed for this study was sent out to participants on 15 February 2022, five weeks
after vaccination became available for children aged ≥5 years. Responses up to 13
March 2022 were included in the analysis. Data on the age, sex and education
distribution in the overall population of the canton of Geneva were obtained
from the Cantonal Office of Statistics of Geneva [32].
Data collected in the
COVID-19 vaccination questionnaire
For all
participants, the questionnaire collected information regarding COVID-19 vaccination
status, acceptance and perceived utility of vaccination in children. For those
with children aged 5–17 years, supplementary questions collected information about
their willingness to have their children vaccinated against COVID-19 and their reasons
for or against this.
The demographic and
socioeconomic variables were categorised as follows: education as primary (compulsory
education or no formal education), secondary (apprenticeships, secondary school
and specialised schools) and tertiary education (university degree, higher
professional education and doctorates); income, according to household
composition-specific categories from cantonal household income statistics [33],
as low (below the first quartile of the general population), middle (between
the first and third quartiles) and high (above the third quartile), considering
both self-reported household income and household composition (living alone
with or without children, in a relationship with or without children, or in a
shared apartment with other adults) from the baseline questionnaire; birth
country as Switzerland, other high-income country, and low- or middle-income
country; employee status as employee, independent, unemployed, retired and
other economically inactive; having a chronic disease as yes/no; household
composition as alone, single with children, with partner and children, and
living with others but not children; smoking status was current, former and
never. We categorised having children into four age-based groups: only 5–11
years, only 12–15 years, only 16–17 years, and mixed ages.
As an outcome, vaccination
status was defined as yes/no according to the question “Have you received at
least one dose of the COVID-19 vaccine?” Intention to vaccinate
children was defined as “intend to or already vaccinated”, “do not know” and “not intending
to”.
Statistical analysis
In descriptive
statistics, we reported the number and percentage for categorical variables and
the median and interquartile range (IQR) for continuous variables. We used
logistic regression to assess the association of demographic, socioeconomic and
health-related factors with COVID-19 vaccination status. Logistic regression
models were run for all the following variables, adjusting for sex and age:
education, household income, employment status, household composition, having a
chronic disease and smoking status. For each variable, we also ran
multivariable logistic regressions adjusting for age, sex, education (n = 1
missing) and income (n = 3 missing; n = 790 unknown/unwilling to respond and
excluded from analyses). A multinomial regression model was used to assess the
relationship between the predictor variables (age, sex, education, income,
child’s age group) and the willingness of parents to have their children
vaccinated. All regression models were
complete case analyses. Odds
ratios (ORs) and 95% confidence intervals (95% CIs) were calculated through the
exponentiation of estimated coefficients. Statistical significance was taken at
the level of p<0.05 a priori. All analyses were conducted using R
4.1.1 (R Foundation for Statistical Computing, Vienna, Austria), distributed
under the GNU General Public License. The code used in the regression analyses is available
at https://github.com/UEP-HUG/2022-vacc-opinion-public.
Ethical considerations
All participants
of the Specchio-COVID19 longitudinal study provided informed and written
consent upon enrolment in the study. Ethical approval for the study was obtained
from the Cantonal Research Ethics Commission of Geneva, Switzerland (project
number 2020-00881). The protocol of the overarching study (Specchio-COVID19)
has been published elsewhere [31].
Results
Sample characteristics
Of the 6,816 individuals
invited, 4,275 chose to participate (62.7% overall response rate; see
supplementary Table 1), of whom 1,383 participants (1/3 of the total sample)
were parents of children aged 5–17 years and constituted our analytical sample.
Among these, 69.3% were aged 35–49 years, and 56.8% were women. Most
participants were professionally active (88.2%), had completed tertiary
education (73.6%) and reported a middle household income (51.3%; table 1).
Among participants with children aged 16–17 years, 87.0% reported that their
children were already vaccinated. This decreased to 65.5% among those with
children aged 12–15 years and 8.7% among participants with children aged 5–11
years. For a description of the overall sample and a comparison to the general
population of Geneva, see supplementary tables 2–4. For an overview of
sociodemographic factors associated with vaccination status in the overall
sample, see supplementary tables 5–6.
Table 1Sociodemographic and health-related characteristics of
the study participants.
|
Sociodemographic characteristics
1
|
Participants with children aged 5–17
years, n (%)
|
|
N
|
1383
|
| Sex |
Female |
785 (56.8) |
| Male |
592 (42.8) |
| Other |
6 (0.4) |
| Age category, years |
18–34 |
49 (3.5) |
| 35–49 |
958 (69.3) |
| 50–64 |
364 (26.3) |
| ≥65 |
12 (0.9) |
| Birth country |
Switzerland |
744 (55.4) |
| Other high-income country |
442 (33.0) |
| Low-income country |
155 (11.6) |
| Employment status |
Employee |
1098 (79.4) |
| Independent |
122 (8.8) |
| Unemployed |
41 (3.0) |
| Retired |
17 (1.2) |
| Other economically inactive |
105 (7.6) |
| Education |
Primary |
39 (2.8) |
| Secondary |
324 (23.4) |
| Tertiary |
1017 (73.6) |
| Other |
2 (0.1) |
| Household income2
|
High |
224 (16.2) |
| Middle |
709 (51.3) |
| Low |
237 (17.2) |
| Don’t know/don’t wish to answer |
211 (15.3) |
| Chronic disease (parent) |
Yes |
282 (20,4) |
| No |
1101 (79.6) |
| Household composition |
Alone |
15 (1.1) |
| Single parent with children |
149 (10.8) |
| With partner and children |
1187 (85.9) |
| Living with others but no children |
31 (2.2) |
| Smoking status |
Current smoker |
210 (15.2) |
| Former smoker |
408 (29.5) |
| Never smoker |
764 (55.3) |
| Having children |
Only children 5–11 |
530 (38.3) |
| Only children 12–15 |
238 (17.2) |
| Only children 16–17 |
177 (12.8) |
| Children of mixed age groups |
438 (31.7) |
| Having children already vaccinated3
|
Only children 5–11 |
46 (8.7) |
| Only children 12–15 |
156 (65.5) |
| Only children16–17 |
154 (87.0) |
| Children of mixed age groups |
278 (63.5) |
Willingness of parents
to have children vaccinated against COVID-19
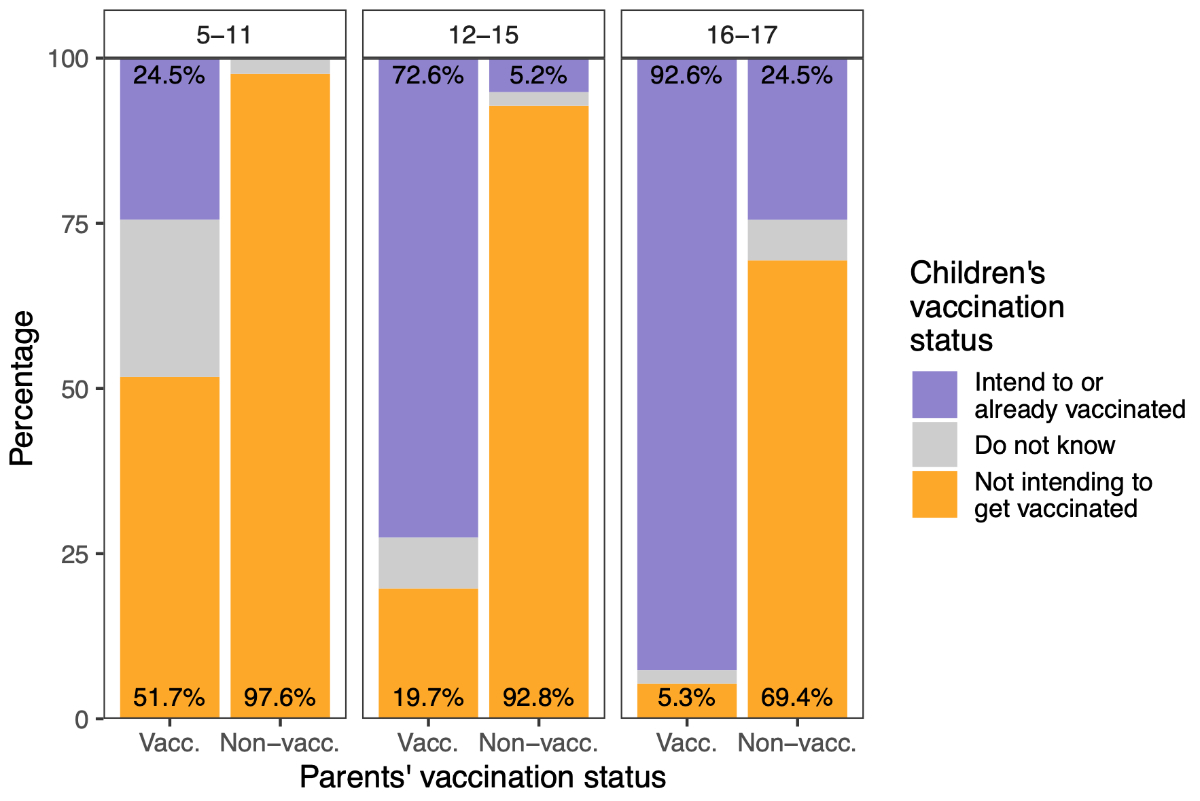
Parental intention
to vaccinate their children differed considerably according to their children’s
age group (with a marked decrease in younger age groups) and their own
vaccination status (figure 1, supplementary table 7). Overall, 13.4% of parents
with adolescents aged 16–17 years indicated no intention to vaccinate them,
2.6% indicated being undecided and 84.0% indicated their children had already
received the vaccine. Among parents of children aged 12–15 years, 31.0%
indicated having no intention to vaccinate their children, 7.0% indicated being
undecided and 60.9% indicated having already vaccinated their children. Among
parents with children aged 5–11 years, 59.6% indicated having no intention to
vaccinate them, 20.9% indicated not knowing yet and 21.2% indicated having
already vaccinated their children or intending to (supplementary table 7). For
all child age groups, unvaccinated parents indicated not intending to vaccinate
their children more frequently than vaccinated parents did (figure 1).
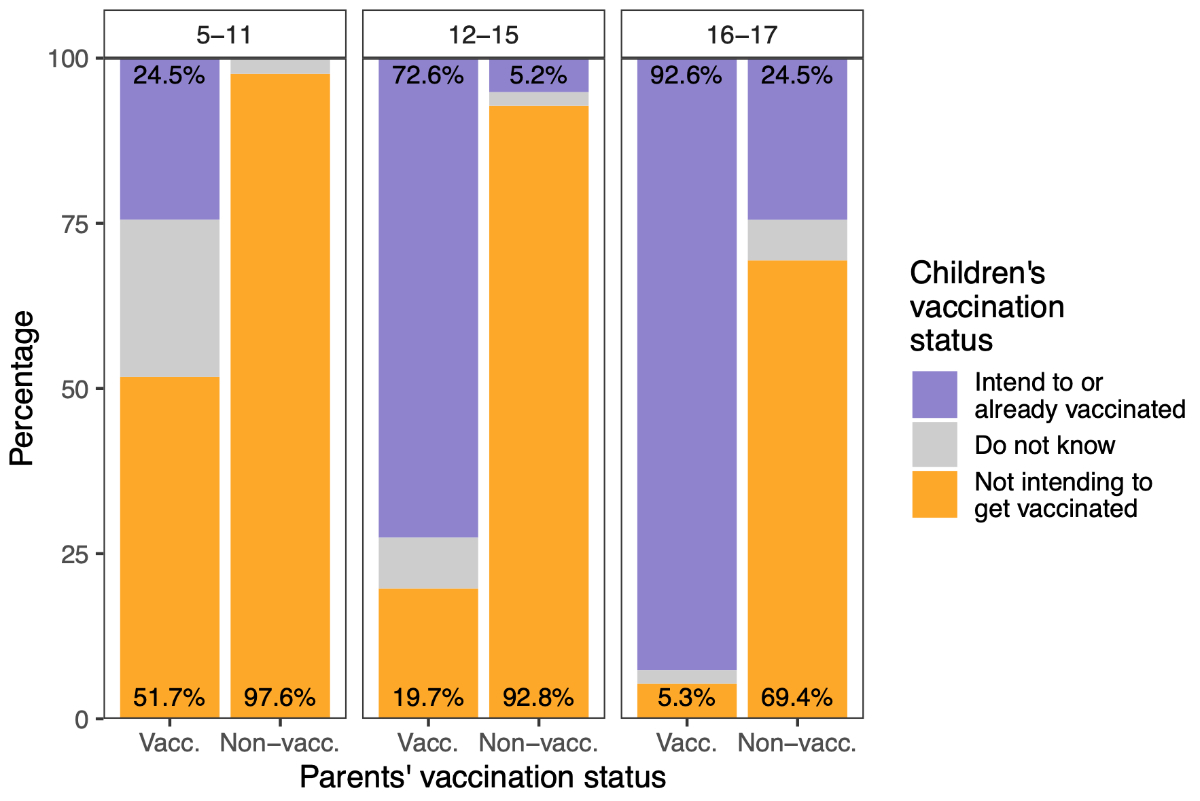
Figure 1 Parental intention to vaccinate children by age
group and own vaccination status.
Parental vaccination status
is positively associated with their intention to have their children vaccinated,
across all age groups, though this association was weakest for the 5–11 years
age group. “Vacc.” means parents having received at least one vaccine dose (those
with at least one child aged 5–11 n = 705; 12–15 n = 548; 16–17 n = 339), and
“Non-vacc.” refers to non-vaccinated parents (5–11 n = 126; 12–15 n = 97; 16–17
n = 48). If a parent has children in more than one age group, they are counted
twice in the figure.
Sociodemographic
factors associated with parental intention to vaccinate children against
COVID-19
In comparison with
those willing to have their children vaccinated, regardless of age, parents
with secondary or primary education, and those with middle or low household
income levels, had greater odds of refusing COVID-19 vaccination for their
children or deciding differently depending on the child’s age (table 2). No
association existed with the parent’s sex, whereas being a younger parent was
associated with willingness to have children vaccinated, whatever their age
(table 2).
Compared with
parents who had children only in the 16–17 years age group, parents with
children only in the 12–15 years age group had three times greater odds of
refusing to have their children vaccinated (3.08; 1.61–5.91); parents with
children only in the 5–11 years age group had almost 20 times greater odds of
refusing to have their children vaccinated (19.8; 10.3–38.1).
Table 2. Association between sociodemographic factors and
parental intention to vaccinate children.
Estimates (odds ratio and 95% confidence interval) are from
multinomial logistic regression, mutually adjusted for all variables presented
in this table. Reference categories are female sex, tertiary educational level,
high household income, and having children in only the 16–17 years age group.
The analytical sample for complete case multinomial model was n = 1,162.
| |
Parental intention to have their children vaccinated
a
|
|
Depends on child’s age
b
vs always
|
Never
c
vs always
|
|
OR (95% CI)
|
p-value
|
OR (95% CI)
|
p-value
|
| Age, years |
0.96 (0.93–0.99) |
0.01 |
0.96 (0.93–0.98) |
0.001 |
| Sex |
Female |
1.00 (ref.) |
|
1.00 (ref.) |
|
| Male |
1.15 (0.80–1.64) |
0.45 |
0.90 (0.66–1.23) |
0.52 |
| Education level |
Tertiary |
1.00 (ref.) |
|
1.00 (ref.) |
|
| Secondary |
1.24 (0.79–1.95) |
0.35 |
1.71(1.18–2.47) |
0.004 |
| Primary |
2.56 (0.88–7.44) |
0.08 |
1.21 (0.42–3.46) |
0.73 |
| Household income |
High |
1.00 (ref.) |
|
1.00 (ref.) |
|
| Middle |
1.52 (0.97–2.37) |
0.07 |
1.75 (1.18–2.60) |
0.005 |
| Low |
1.60 (0.90–2.85) |
0.11 |
1.96 (1.20–3.22) |
0.008 |
| Children’s age group |
16–17 years only |
1.00 (ref.) |
|
1.00 (ref.) |
|
| 12–15 years only |
2.46 (0.86–7.02) |
0.09 |
3.08 (1.61–5.91) |
0.001 |
| 5–11 years only |
19.4 (7.22–52.14) |
<0.001 |
19.77 (10.27–38.05) |
<0.001 |
| Multipled
|
17.3 (6.73–44.68) |
<0.001 |
6.05 (3.22–11.37) |
<0.001 |
Reasons for parental
intention for or against vaccinating children
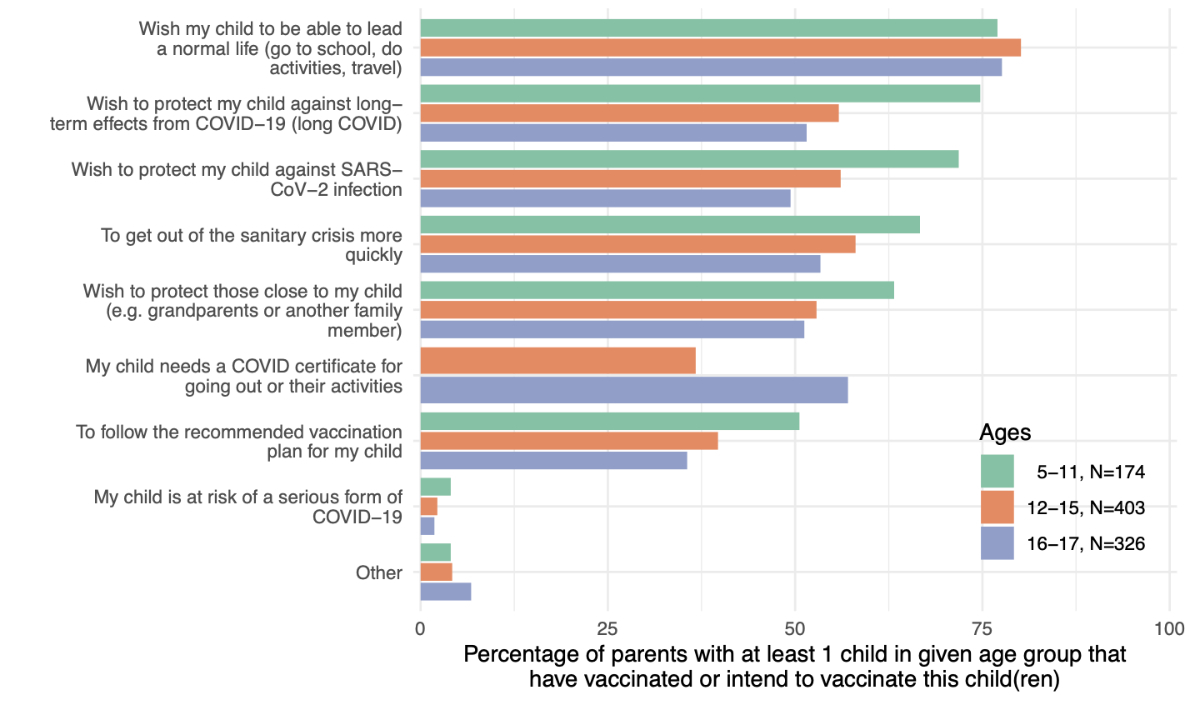
Among parents in favour
of vaccinating their children, the most frequently chosen reason was “wish my
child to be able to lead a normal life (go to school, do activities, travel,
etc.)”, reported by more than three quarters of parents, regardless of their
child’s age group (figure 2). The other most reported reasons varied in
frequency according to the child’s age group. For instance, the intention to
vaccinate children to protect them against long COVID symptoms was reported by
51.5% of parents with children aged 16–17 years, 55.8% of parents with children
aged 12–15 years and 74.7% of parents with children aged 5–11 years. Similarly,
protection against SARS-CoV-2 infection was reported as a reason by 49.4%,
56.1% and 71.8% of parents with children aged 16–17 years, 12–15 years and 5–11
years, respectively. With a similar frequency according to the child’s age
group, over half of the parents also reported “to get out of the public
health crisis more quickly” and “wish to protect those
close to my child (grandparents or other family members)” as reasons
for vaccinating their children (figure 2).
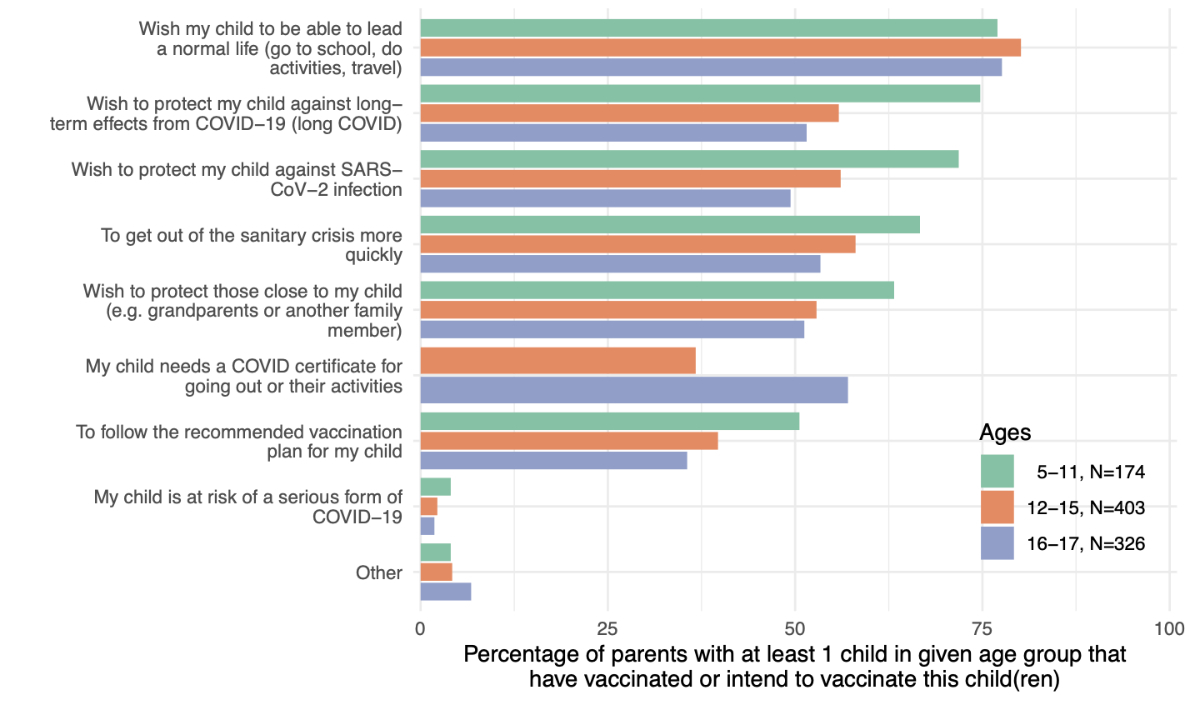
Figure 2 Reasons for deciding or wanting to vaccinate
children.
Parents of children in the given age groups were asked their reasons for
deciding or intending to vaccinate their children. Multiple choices were
possible. Parents of children aged 5–11 years were not asked about the need for
a COVID certificate because this age group did not require one for any
activities in Switzerland.
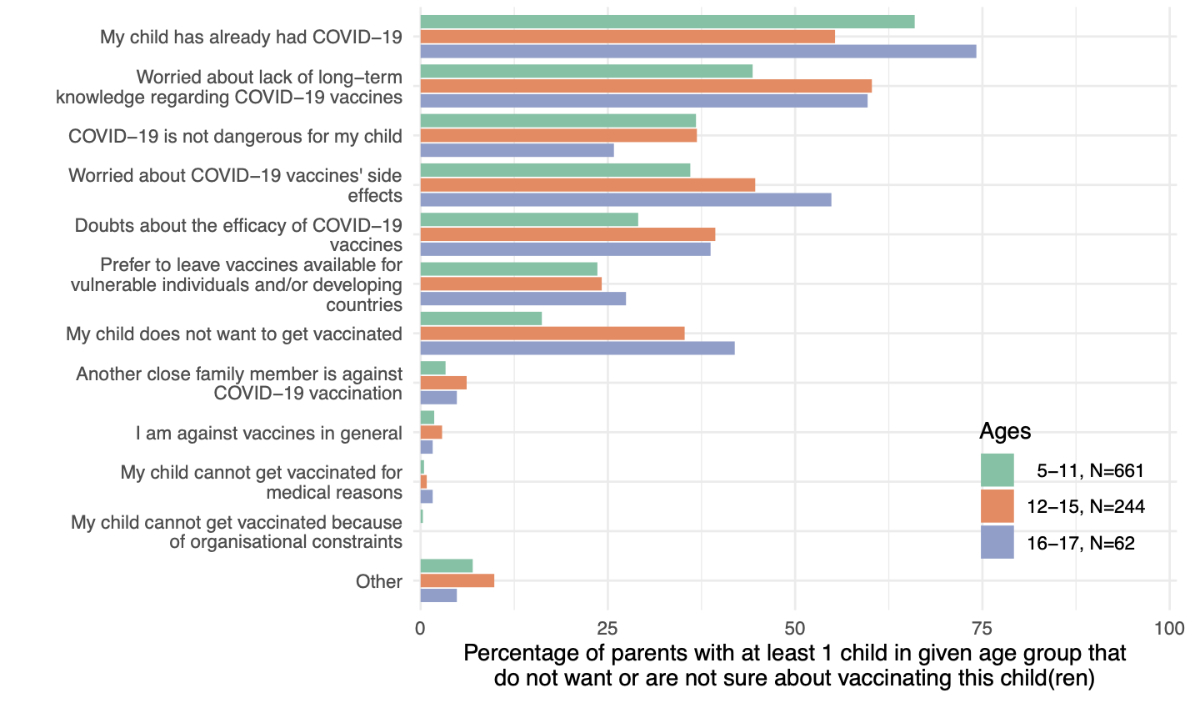
Among parents not intending
to vaccinate their children, “my child has already had COVID-19” was
reported by 74.2%, 55.3% and 66.0% of those with children aged 16–17 years, 12–15
years and 5–11 years, respectively (figure 3). A “worry about lack of
long-term knowledge regarding COVID-19 vaccines” was reported by 59.7%,
60.2% and 44.3% of parents with children aged 16–17 years, 12–15 years and 5–11
years, respectively. A “worry about COVID-19 vaccines’ side effects” was
reported by 54.8%, 44.7% and 36.0% of parents with children aged 16–17 years, 12–15
years and 5–11 years, respectively. “My child does not want to get vaccinated” was
reported by 41.9%, 35.2% and 16.2% of parents with children aged 16–17 years, 12–15
years and 5–11 years, respectively. Very few participants reported being
against vaccines in general (figure 3).
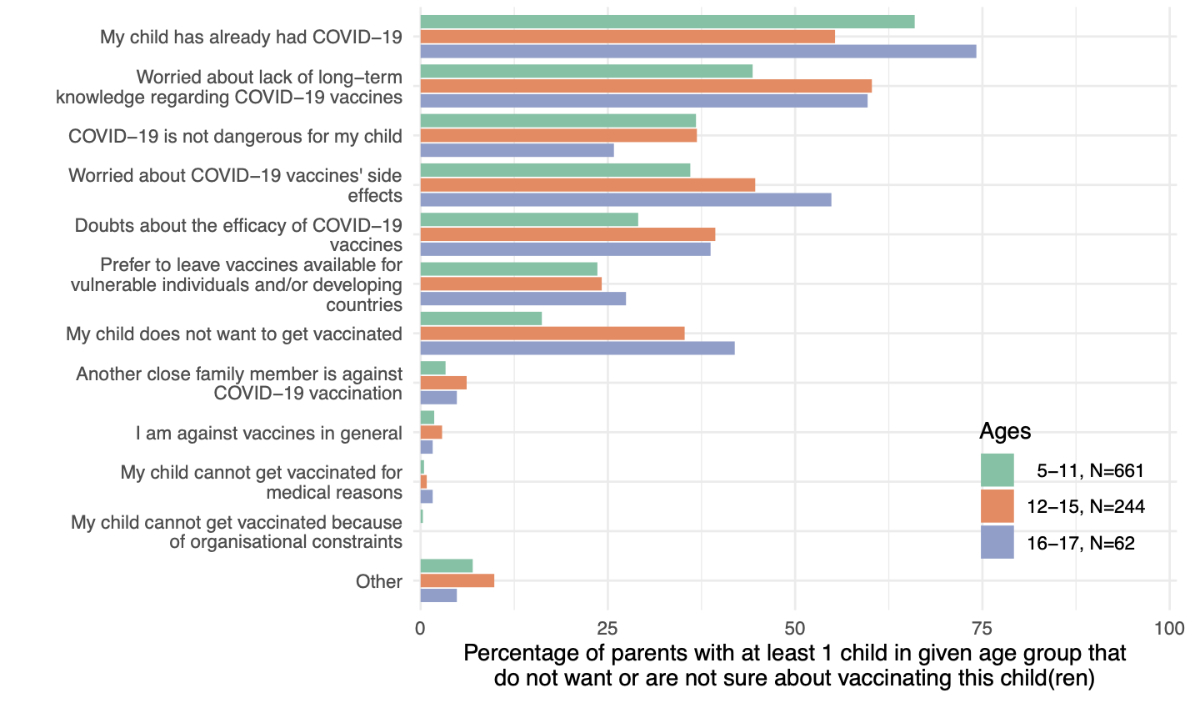
Figure 3 Reasons for deciding not to vaccinate children.
Parents of children in the given age groups were asked their reasons for not
wanting to vaccinate or not being sure about vaccinating their children.
Multiple choices were possible.
Discussion
To our knowledge,
this is the first population-based study in Switzerland to assess parental
willingness to have their children vaccinated against COVID-19 since vaccination
was officially approved for children and adolescents. Our study began 5 to 8 weeks
after vaccination became available to all children aged ≥5 years. We found that
parental willingness to have their children vaccinated differed considerably
according to their children’s age and their own vaccination status.
A recent meta-analysis
of 44 studies worldwide, most of which were conducted before vaccination was
approved for children and adolescents, found that parental intention to
vaccinate their children was 60.1% overall, although it ranged from 25.6% in
Saudi Arabia to 92.2% in Zambia [8]. This meta-analysis also found that,
overall, 22.9% of participants intended not to vaccinate their children, and 25.8%
were unsure [8].
In our previous
cross-sectional vaccination survey, conducted before vaccination was available for
children, we showed that less than
half of parents (45.6%) intended to have their children vaccinated in the
canton of Geneva. The gradient in intention increased with children’s age from 38.6% for children aged 6–10 years to 55.9% for children aged 16–18 years
[24]. In a sample of Swiss German-speaking parents, 58.7% reported their
intention to have their children vaccinated. However, this result might be
overestimated because parents were recruited at a vaccination centre [34].
These new findings
reflect those of international studies conducted since vaccination was approved
for children aged 12 years and older. A Canadian study found that around 90% of
parents had already vaccinated or were very likely to vaccinate their children
aged 12–17 years, whereas more than half were willing to vaccinate their
younger children (0–11 years) [35]. In the US, a study found that around two thirds
of parents had already vaccinated or intended to vaccinate their children aged
12–17 years, and 60% intended to vaccinate their children aged 5–11 years [36].
In both studies, similarly to our findings, parents were significantly more
likely to vaccinate their children if they were themselves vaccinated [35, 36].
Our findings are also
in line with those of previous studies showing that parental willingness to
vaccinate their children decreased progressively with the age of the child,
from 84.0% for parents of children aged 16–17 years to 19.5% for parents of
children aged 5–11 years [8, 34–36]. However, in the studies from the US and
Canada, these decreases were not as pronounced as in our findings [35, 36].
The COVID
certificate was established for adolescents aged 16 years or above in
Switzerland, and for those aged 12 years or above in neighbouring France, which
likely explains why around three quarters of parents reported choosing to
vaccinate their children so they could “lead a normal life”. Similar
to reports regarding willingness to vaccinate children against other diseases, we
found that perceived vaccine safety was an important determinant of acceptance [37,
38]. In addition, in Switzerland, vaccination is not recommended for children
who have already had COVID, which likely explains this reason being the most
frequently reported among parents not intending to vaccinate their children.
As reported in
other countries, we found that higher parental education and household income
levels were associated with a higher likelihood of vaccinating children. Although
we found no association with the parent’s sex, previous studies reported that fathers
were more likely to intend to vaccinate their children, with mothers more
concerned about the potential undesirable side effects [8, 34–36]. This lack of
association may be because women were overrepresented in our sample.
Parental hesitancy
to vaccinate their children against COVID-19 appears to be higher compared with
other recommended vaccines, although our study did not consider vaccine
hesitancy for children aged <5 years. For instance, a recent nationwide
survey in Switzerland found that 26% of parents were vaccine-hesitant regarding
the official recommendations for polio–pertussis–tetanus and measles vaccines
during the first year of life [39, 40]. Notably, our results showed that even
among parents not intending to vaccinate their children against COVID-19, only
a small proportion (<5%) reported being against vaccines in general.
Implications for
public health policies
As the pandemic enters
new phases, with newly emerging virus variants driving new waves and exerting
variable pressure on health systems, maintaining and reinforcing prevention
strategies remains important, particularly including the vaccination of
children and adolescents. Information campaigns must still emphasise that even
though vaccines’ effectiveness in preventing infections can decrease over time
and with the emergence of new variants of concern, they still confer a high
level of protection against severe COVID-19, hospitalisation and death [2, 4]. Vaccination
of children and adolescents remains an essential component of the prevention of
severe COVID-19 and hospitalisation, as well as preventing long COVID and psychosocial
and educational difficulties. As such, given the decreased willingness to
vaccinate younger children, vaccination programs must frame their outreach
message, particularly for socioeconomically disadvantaged parents, who are less
likely to vaccinate their children. Identifying specific groups with the lowest
level of acceptance of further COVID-19 vaccination is essential for effective
science and public health communication, building general trust in vaccines and
tackling socioeconomic inequalities. This will, in turn, strengthen other
vaccination campaigns and prepare for future pandemics.
Strengths and
limitations
The main strengths
of this study are its population-based sample and the inclusion of data on
sociodemographic and health-related characteristics, which allowed analysis of COVID-19
vaccination acceptance according to these factors. Importantly, participants
were interviewed 6–10 weeks after vaccination was approved for children aged ≥5
years, which enabled their opinions to be based on real-life conditions instead
of hypothetical vaccination of their children.
Several limitations
of our study should be acknowledged. Although the participation rate in this
study was relatively high, generalisation of the results presented here
requires caution because our sample is not completely representative of the
general adult population of the canton of Geneva. Our participants were older
and had a higher level of education than the general adult population – a
common characteristic of epidemiological population-based studies [41]. Participation
required French literacy, internet access and digital literacy, potentially
excluding part of the general population. Some other factors that may impact vaccination
acceptance were not investigated, such as religious or political views, social
network influence, and other indicators of socioeconomic conditions that are
likely to influence individual perceptions and behaviour. Parents’
decisions regarding vaccination can also be influenced by their health care
providers. In addition,
especially for children and adolescents, we do not know about the presence of chronic
diseases, which can impact the willingness of parents to have them vaccinated.
Conclusion
Parental
willingness to vaccinate their children was high for adolescents aged 16–17
years, but it decreased considerably for younger adolescents and was markedly
lower among unvaccinated parents. Underprivileged socioeconomic conditions were
associated with being unvaccinated among adults and not intending to vaccinate
their children. Given the proven efficacy of COVID-19 vaccines in preventing
severe disease and hospitalisation, our results should be considered in
designing future vaccination hesitancy research and in the communication and
outreach strategies of vaccination programs targeting vaccine-hesitant groups.
Data availability
statement
Coded study data
that underlie the results reported in this article can be made available to the
scientific community after deidentification and upon submission of a data
request application to the investigators’ board via the corresponding author.
The protocol of the overarching study (Specchio-COVID19) can be found at
https://bmjopen.bmj.com/content/12/1/e055515.
Acknowledgements
We thank all the participants, without whom this study would
not have been possible.
Authors’ contributions: HB, SS and IG designed the study. HB and SS designed the
questionnaire for the survey. MEZ, CS and FP were involved in participant
recruitment and implementation of the survey. NP conducted statistical analyses
of the data. HB and CdM drafted the manuscript. EL and ALH reviewed the
manuscript. All authors participated in the analysis interpretation and reviewed
and approved the final manuscript.
Specchio-COVID19 study group: Specchio-COVID19
study group: Isabelle Arm-Vernez, Andrew S Azman, Fatim Ba, Oumar Ba, Delphine
Bachmann, Jean-François Balavoine, Baysson H, Michael Balavoine, Hélène
Baysson, Lison Beigbeder, Julie Berthelot, Patrick Bleich, Gaëlle Bryand
Rumley, François Chappuis, Prune Collombet, Delphine Courvoisier, Alain Cudet,
Carlos de Mestral Vargas, Paola D’Ippolito, Richard Dubos, Roxane Dumont,
Isabella Eckerle, Nacira El Merjani, Antoine Flahault, Natalie Francioli,
Marion Frangville, Idris Guessous, Séverine Harnal, Samia Hurst, Laurent
Kaiser, Omar Kherad, Julien Lamour, Pierre Lescuyer, François L’Huissier,
Fanny-Blanche Lombard, Andrea Jutta Loizeau, Elsa Lorthe, Chantal Martinez,
Lucie Ménard, Lakshmi Menon, Ludovic Metral-Boffod, Benjamin Meyer, Alexandre
Moulin, Mayssam Nehme, Natacha Noël, Francesco Pennacchio, Javier Perez-Saez,
Giovanni Piumatti, Didier Pittet, Jane Portier, Klara M Posfay-Barbe, Géraldine
Poulain, Caroline Pugin, Nick Pullen, Zo Francia Randrianandrasana, Aude
Richard, Viviane Richard, Frederic Rinaldi, Jessica Rizzo, Khadija Samir,
Claire Semaani, Silvia Stringhini, Stéphanie Testini, Didier Trono, Guillemette
Violot, Nicolas Vuilleumier, Ania Wisniak, Sabine Yerly, María-Eugenia Zaballa.
References
1. Klein NP, Stockwell MS, Demarco M, Gaglani M, Kharbanda AB, Irving SA, et al. Effectiveness of COVID-19 Pfizer-BioNTech BNT162b2 mRNA Vaccination in Preventing COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Nonimmunocompromised Children and Adolescents Aged 5-17 Years - VISION Network, 10 States, April 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022 Mar;71(9):352–8. https://doi.org/10.15585/mmwr.mm7109e3 PMID:35239634
2. Dorabawila V, Hoefer D, Bauer UE, Bassett MT, Lutterloh E, Rosenberg ES. Effectiveness of the BNT162b2 vaccine among children 5-11 and 12-17 years in New York after the Emergence of the Omicron Variant. medRxiv. Published online January 1, 2022:2022.02.25.22271454. https://doi.org/10.1101/2022.02.25.22271454.
3. Walter EB, Talaat KR, Sabharwal C, Gurtman A, Lockhart S, Paulsen GC, et al.; C4591007 Clinical Trial Group. Evaluation of the BNT162b2 Covid-19 Vaccine in Children 5 to 11 Years of Age. N Engl J Med. 2022 Jan;386(1):35–46. https://doi.org/10.1056/NEJMoa2116298 PMID:34752019
4. Nordström P, Ballin M, Nordström A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: a retrospective, total population cohort study in Sweden. Lancet. 2022 Feb;399(10327):814–23. https://doi.org/10.1016/S0140-6736(22)00089-7 PMID:35131043
5. General Health Directorate of Canton of Geneva. Vaccination in Geneva: numbers and campaign. ge.ch. Accessed July 1, 2022. https://www.ge.ch/en/node/23804
8. Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: A systematic review and meta-analysis. Prev Med. 2022 Apr;157:106994. https://doi.org/10.1016/j.ypmed.2022.106994 PMID:35183597
10. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MB, et al.; Overcoming COVID-19 Investigators; CDC COVID-19 Response Team. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020 Jul;383(4):334–46. https://doi.org/10.1056/NEJMoa2021680 PMID:32598831
11. Buonsenso D, Munblit D, De Rose C, et al. Preliminary evidence on long COVID in children. Acta Paediatr Oslo Nor 1992. 2021;110(7):2208-2211. https://doi.org/10.1111/apa.15870.
14. Colvin MK, Reesman J, Glen T. The impact of COVID-19 related educational disruption on children and adolescents: an interim data summary and commentary on ten considerations for neuropsychological practice. Clin Neuropsychol. 2022 Jan;36(1):45–71. https://doi.org/10.1080/13854046.2021.1970230 PMID:34495815
16. Richard V, Dumont R, Lorthe E, Baysson H, Zaballa ME, Barbe RP, et al.; Specchio-COVID19 Group. COVID-19-Related School Disruptions and Well-Being of Children and Adolescents in Geneva. J Paediatr Child Health. 2022 May;58(5):937–9. https://doi.org/10.1111/jpc.15973 PMID:35411686
19. Zambrano LD, Newhams MM, Olson SM, Halasa NB, Price AM, Boom JA, et al.; Overcoming COVID-19 Investigators. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA Vaccination Against Multisystem Inflammatory Syndrome in Children Among Persons Aged 12-18 Years - United States, July-December 2021. MMWR Morb Mortal Wkly Rep. 2022 Jan;71(2):52–8. https://doi.org/10.15585/mmwr.mm7102e1 PMID:35025852
24. Wisniak A, Baysson H, Pullen N, Nehme M, Pennacchio F, Zaballa ME, et al.; Specchio-COVID19 study group. COVID-19 vaccination acceptance in the canton of Geneva: a cross-sectional population-based study. Swiss Med Wkly. 2021 Dec;151(4950):w30080. https://doi.org/10.4414/SMW.2021.w30080 PMID:34908389
25. Nehme M, Baysson H, Pullen N, Wisniak A, Pennacchio F, Zaballa ME, et al.; Specchio-COVID19 study group. Perceptions of vaccination certificates among the general population in Geneva, Switzerland. Swiss Med Wkly. 2021 Nov;151(47):w30079. https://doi.org/10.4414/SMW.2021.w30079 PMID:34846113
27. Baysson H, Pennachio F, Wisniak A, Zabella ME, Pullen N, Collombet P, et al.; Specchio-COVID19 study group. Specchio-COVID19 cohort study: a longitudinal follow-up of SARS-CoV-2 serosurvey participants in the canton of Geneva, Switzerland. BMJ Open. 2022 Jan;12(1):e055515. https://doi.org/10.1136/bmjopen-2021-055515 PMID:35105645
29. Stringhini S, Zaballa ME, Perez-Saez J, Pullen N, de Mestral C, Picazio A, et al.; Specchio-COVID19 Study Group. Seroprevalence of anti-SARS-CoV-2 antibodies after the second pandemic peak. Lancet Infect Dis. 2021 May;21(5):600–1. https://doi.org/10.1016/S1473-3099(21)00054-2 PMID:33539733
30. Stringhini S, Zaballa ME, Pullen N, Perez-Saez J, de Mestral C, Loizeau AJ, et al.; Specchio-COVID19 study group. Seroprevalence of anti-SARS-CoV-2 antibodies 6 months into the vaccination campaign in Geneva, Switzerland, 1 June to 7 July 2021. Euro Surveill. 2021 Oct;26(43):2100830. https://doi.org/10.2807/1560-7917.ES.2021.26.43.2100830 PMID:34713799
31. Baysson H, Pennacchio F, Wisniak A, et al. The Specchio-COVID19 study cohort: a web-based prospective study of SARS-CoV-2 serosurveys participants in the canton of Geneva (Switzerland). Submitted. Published online June 2021.
32. Office Cantonal des Statistiques (OCSTAT). Statistiques cantonales - République et canton de Genève. Accessed September 8, 2021. https://www.ge.ch/statistique/
33. Office Cantonal des Statistiques (OCSTAT). T 20.02.7.01 - Statistique cantonale du revenu et de la fortune des ménages - Quantiles du revenu annuel brut des ménages selon le type de ménage en 2015-2017 - Canton de Genève. Published online December 11, 2020.
34. Wagner A, Liberatore F, Schmelzer S, Dratva J. Confident and altruistic - parents’ motives to vaccinate their children against COVID-19: a cross-sectional online survey in a Swiss vaccination centre. Swiss Med Wkly. 2022 Mar;152(11):w30156. https://doi.org/10.4414/SMW.2022.w30156 PMID:35315342
38. Kempe A, Saville AW, Albertin C, Zimet G, Breck A, Helmkamp L, et al. Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics. 2020 Jul;146(1):e20193852. https://doi.org/10.1542/peds.2019-3852 PMID:32540985
40. Deml MJ, Buhl A, Huber BM, Burton-Jeangros C, Tarr PE. Trust, affect, and choice in parents’ vaccination decision-making and health-care provider selection in Switzerland. Sociol Health Illn. 2022 Jan;44(1):41–58. https://doi.org/10.1111/1467-9566.13388 PMID:34747500
41. Reinikainen J, Tolonen H, Borodulin K, Härkänen T, Jousilahti P, Karvanen J, et al. Participation rates by educational levels have diverged during 25 years in Finnish health examination surveys. Eur J Public Health. 2018 Apr;28(2):237–43. https://doi.org/10.1093/eurpub/ckx151 PMID:29036286
Appendix: Supplementary tables and
figures
The appendix is available in the pdf version of the article.