Long-term
mortality effects of century crises: A warning from the past for the decades
after COVID-19?
DOI: https://doi.org/https://doi.org/10.57187/smw.2023.40057
Anthropometrics & Historical Epidemiology Research Group, Institute of Evolutionary Medicine, University of Zurich, Zurich, Switzerland
Almost 3 years have passed since the first
coronavirus disease 2019 (COVID-19) case was reported in Switzerland in spring
2020. A recent study has shown that COVID-19 has reached historic proportions
as a crisis for Switzerland that has not been seen since 1918 [1]. In the last
3 years, numerous studies have been published on the short-term impacts of
COVID-19, including the risk associated with COVID-19 infection during
pregnancy and its impact on neonates [2–6]. All these studies have highlighted
important direct or indirect effects of COVID-19 that occur during or shortly
after infection. However, the long-term effects of the COVID-19 pandemic in the
decades to come cannot be studied yet. This applies especially to the effects
of in-utero exposure of current birth cohorts later in adulthood. Questions
regarding the long-term health effects of maternal COVID-19 infection on
offspring remain unanswered.
We must analyse history to understand how
past crises affected in-utero exposure and long-term health consequences. Only
a look back into history can reveal that such crises can have long-term
effects. For example, the “Spanish flu” is the first well-documented crisis in
Switzerland for which an in-utero exposed birth cohort can be studied across
its lifespan. The “foetal origin hypothesis”, proposed by Barker [7, 8], argued
that foetal malnutrition caused by hunger, infections, and stress can have
lasting effects on future health. Based on this hypothesis in addition to
studies using data from the 1918 pandemic, there is already evidence that poor
foetal health may increase the risk developing various health issues, such as
cardiovascular disease, hypertension, diabetes, and kidney problems, which lead
to an increased risk of mortality [9–12].
In the last 200 years, Switzerland has been
impacted by several severe crises despite the fact that the two world wars had
less of an impact on Switzerland than other countries. In 1817, countless
people died in Switzerland in the last large hunger crisis [13]. According to
the historical literature, hundreds of pregnant women were undernourished,
which led to prenatal malnutrition. In 1918/1919 and towards the end of World
War 1, the Spanish flu struck Switzerland at a time when scarce supplies were
having an increasing impact on the nutritional and health status of the
population [14]. Experts believe that at least one-half of the population was
infected by the influenza virus during the 1918 pandemic, especially younger
adults, including many young pregnant women [15]. Increased rates of preterm
birth, still birth, and low-birth-weight neonates were observed as immediate
impacts of the Spanish flu on pregnant women [16–18]. Modern medical literature states that suboptimal
intrauterine conditions resulting from maternal malnutrition, hypoxia,
psychological stress, or even mild exposure to an infectious disease can have
lasting effects on foetal development and are often associated with reduced
birth weight [19]. Therefore, if
we consider the severe health crisis years in Switzerland over the last 200
years, how was the in-utero exposure of birth cohorts at that time associated
with health and all-cause mortality later in life?
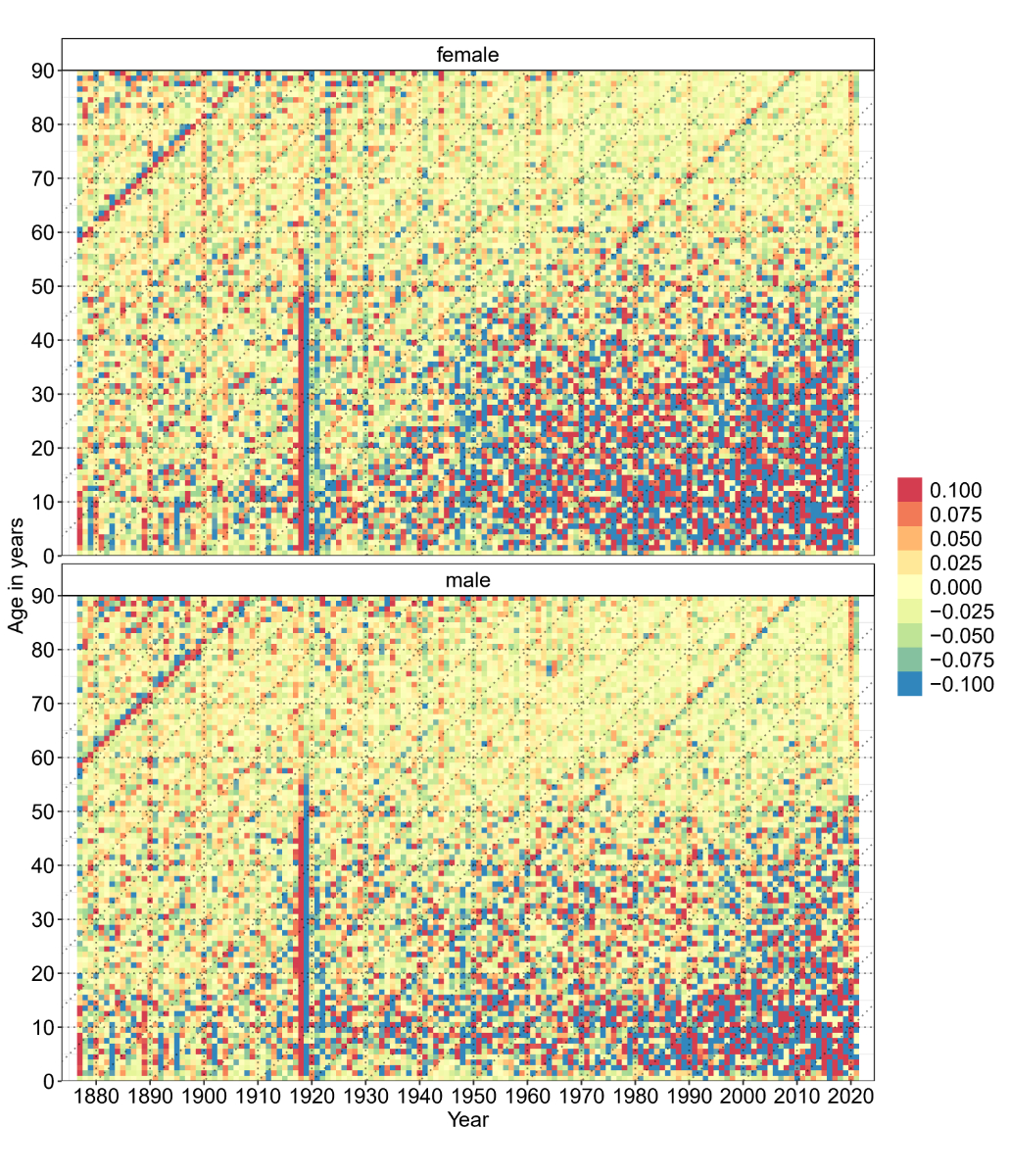
To emphasise the powerful effects of
in-utero exposure on long-term mortality in Switzerland, I adapted the Lexis
surface plots recently published by Jones et al. for England and Wales from
1910 to 2010 [20]. The Lexis surface plot was applied for the first time on
Swiss data from 1876 to 2021 (figure 1) and showed the annual change in
age-specific mortality. To calculate these changes, Swiss mortality and
population data from 1876 to 2021 were obtained from the Human Mortality
Database [21]. The figure shows the data categorised by sex. The x-axis
represents the year of mortality, and the y-axis represents the age of the
persons in the respective year. Orange and red
represent an increase in mortality compared with the previous year, while blue
and green represent decreased mortality.
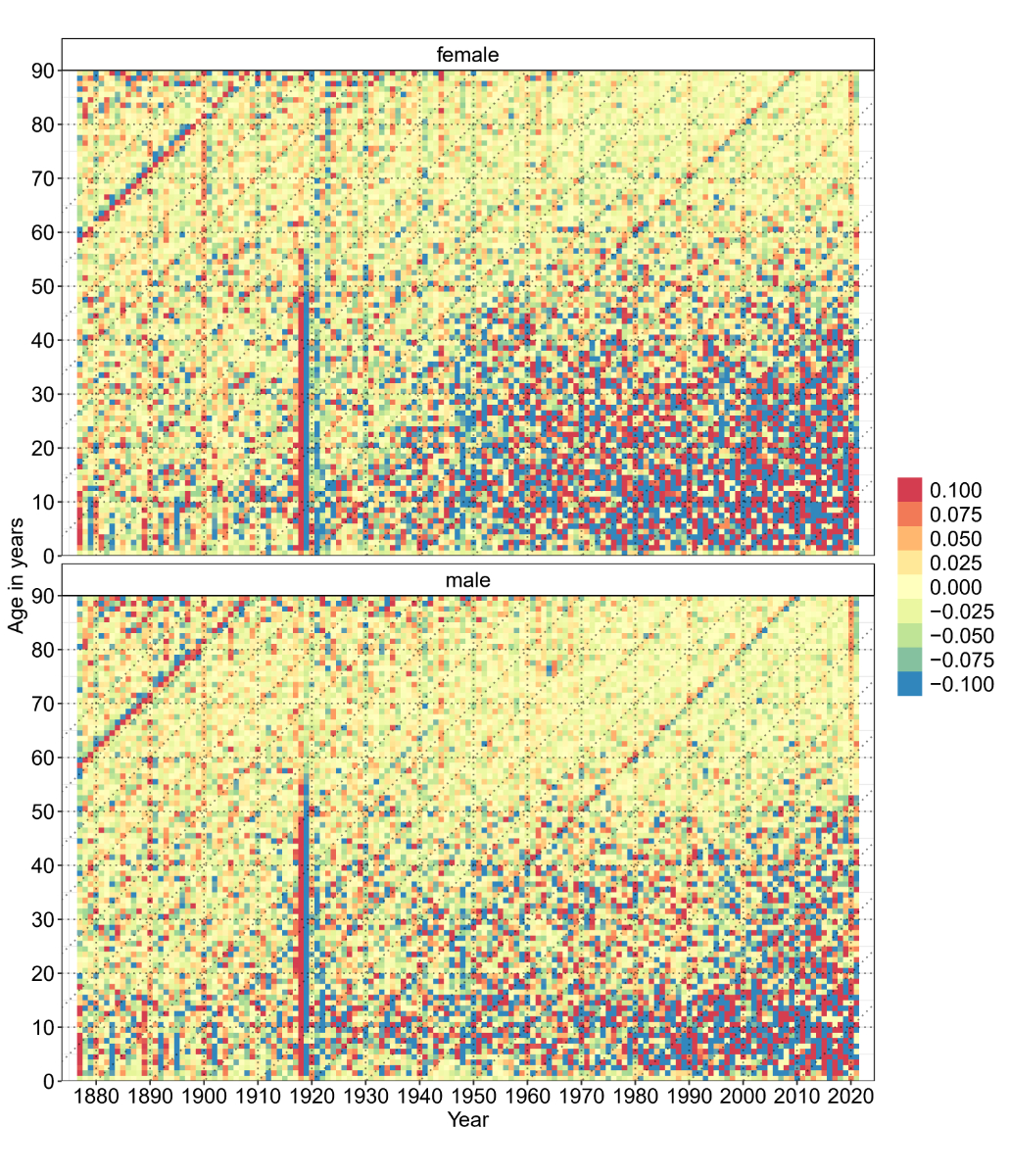
Figure 1 Lexis surface plot (adapted to Swiss data from Jones et al. [20]) for annual change in
age-specific mortality. Orange and red represent an increase in mortality
compared with the previous year, while blue and green represent decreased
mortality. Vertical lines represent period effects, while diagonal lines
represent cohort effects.
First, we studied the vertical lines. A closer look at the year 1918 reveals a red vertical bar for men and women up to
the age of 50 years. This reflects the high mortality of young adults due to
the Spanish flu. In 2020, the first year of the COVID-19 pandemic, an orange
bar is visible from age 70 years and older, indicating a higher mortality for
older people in 2020 compared with 2019. The differences are not as large as in
the case of the Spanish flu, where the bar is dark red; however, an increased
mortality is still visible, more so in males than females.
To identify the effects on birth cohorts,
the diagonal lines were considered. Each diagonal line corresponds to a birth
cohort and the corresponding mortality effect later in life. The first
prominent red diagonal line is visible from 1877 to 1908; it starts in 1877 at
59 years of age and increases to 90 years in 1908. This line represents the
birth cohort of 1818, which was exposed in utero to the last severe hunger
crisis in Switzerland in 1817. Across all years and ages, this birth cohort has
higher mortality compared with earlier and later cohorts. Unfortunately, we
cannot follow this birth cohort across all ages because Swiss data before 1877
is lacking.
The next visible diagonal line represents
the birth cohort of 1919 (in-utero exposure during the end of World War 1 and
the Spanish flu). This diagonal line is especially prominent from the 1970s,
when the birth cohort was aged 51 years and older. For males, the line is even
clearly visible from 1919 onwards. This underlines the higher mortality risk of
the 1919 birth cohort, especially from the age of 50 years. It remains unclear
which causes of death were more prevalent in the 1919 birth cohort as compared
to those of prior and following years. However, modern medical literature
states that adverse neonatal health is associated with increased risk for type
2 diabetes, hypertension, and coronary heart diseases in later life [9], with the latter being associated
with the greatest increased risk of mortality [22].
The red and blue points in figure 1 from
the 1950s onwards, for ages up to 40 years, should not be interpreted. At those
ages, mortality was very low due to the small sample size; therefore, the
variance is large, as a minimal number of deaths leads to larger differences in
the annual change in mortality.
Even if it is only visual and descriptive,
this first small adaptation of a recently published method to analyse Swiss
data clearly shows the impact of in-utero exposure to severe health crises in
the past, not only in the immediate crisis year, but also on the long-term
mortality of the affected birth cohorts, even decades later.
Whether we will see similar patterns in the
following decades for the 2020/2021 birth cohort is uncertain at this time. The
only certainty is that many pregnant women were exposed to COVID-19 during the
pandemic, and we do not yet know how this will affect the 2020/2021 birth cohort
in adulthood and later life, even if the course of infection in the mothers was
mild. However, the increased mortality of the 1918 and 1919 birth cohorts later
in life should make us vigilant and remind us to monitor the birth cohorts of
2020/2021 in the future.
Acknowledgements
The author thanks Kaspar Staub, Frank
Rühli, Nicole Bender, Joël Floris, Marcel Zwahlen and Olivia Keiser for support
and previous collaborations.
Dr. Katarina Matthes
Institute of Evolutionary Medicine
University of Zurich
Winterthurerstrasse 190
CH-8057 Zurich
katarina.matthes[at]iem.uzh.ch
References
1.
Staub K
,
Panczak R
,
Matthes KL
,
Floris J
,
Berlin C
,
Junker C
, et al.
Historically High Excess Mortality During the COVID-19 Pandemic in Switzerland, Sweden, and Spain. Ann Intern Med. 2022 Apr;175(4):523–32. https://doi.org/10.7326/M21-3824
2.
Kotlar B
,
Gerson E
,
Petrillo S
,
Langer A
,
Tiemeier H
. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 2021 Jan;18(1):10. https://doi.org/10.1186/s12978-021-01070-6
3.
Villar J
,
Ariff S
,
Gunier RB
,
Thiruvengadam R
,
Rauch S
,
Kholin A
, et al.
Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021 Aug;175(8):817–26. https://doi.org/10.1001/jamapediatrics.2021.1050
4.
Lambelet V
,
Ceulemans M
,
Nordeng H
,
Favre G
,
Horsch A
,
Stojanov M
, et al.
Impact of the COVID-19 pandemic on Swiss pregnant and breastfeeding women - a cross-sectional study covering the first pandemic wave. Swiss Med Wkly. 2021 Sep;151(3738):w30009. https://doi.org/10.4414/smw.2021.w30009
5.
Radan AP
,
Baud D
,
Favre G
,
Papadia A
,
Surbek D
,
Baumann M
, et al.
Low placental weight and altered metabolic scaling after severe acute respiratory syndrome coronavirus type 2 infection during pregnancy: a prospective multicentric study. Clin Microbiol Infect. 2022 May;28(5):718–22. https://doi.org/10.1016/j.cmi.2022.02.003
6.
McClymont E
,
Albert AY
,
Alton GD
,
Boucoiran I
,
Castillo E
,
Fell DB
, et al.; CANCOVID-Preg Team
. Association of SARS-CoV-2 Infection During Pregnancy With Maternal and Perinatal Outcomes. JAMA. 2022 May;327(20):1983–91. https://doi.org/10.1001/jama.2022.5906
7.
Barker DJ
. The fetal and infant origins of adult disease. BMJ. 1990 Nov;301(6761):1111. https://doi.org/10.1136/bmj.301.6761.1111
8.
Barker DJ
. Fetal origins of coronary heart disease. BMJ. 1995 Jul;311(6998):171–4. https://doi.org/10.1136/bmj.311.6998.171
9.
Almond D
,
Mazumder B
. The 1918 Influenza Pandemic and Subsequent Health Outcomes: An Analysis of SIPP Data. Am Econ Rev. 2005 May;95(2):258–62. https://doi.org/10.1257/000282805774669943
10.
Lin MJ
,
Liu EM
. Does in utero exposure to Illness matter? The 1918 influenza epidemic in Taiwan as a natural experiment. J Health Econ. 2014 Sep;37(1):152–63. https://doi.org/10.1016/j.jhealeco.2014.05.004
11.
Myrskylä M
,
Mehta NK
,
Chang VW
. Early life exposure to the 1918 influenza pandemic and old-age mortality by cause of death. Am J Public Health. 2013 Jul;103(7):e83–90. https://doi.org/10.2105/AJPH.2012.301060
12.
Garthwaite C.
The Effect of In-Utero Conditions on Long Term Health: Evidence from the 1918 Spanish Flu Pandemic. 2008.
13.
Krämer D
. Menschen grasten nun mit dem Vieh. Basel: Schwabe; 2015.
14.
Staub K
. Der vermessene menschliche Körper als Spiegel der Ernährungs- und Gesundheitsverhältnisse am Ende des Ersten Weltkrieges. In:
Pfister C
,
Segesser D
,
Krämer D
, editors
. Woche für Woche neue Preisaufschläge. Nahrungsmittel-, Energie- und Ressourcenkonflikte in der Schweiz des Ersten Weltkrieges. Basel: Schwabe; 2016. pp. 285–308.
15.
Sonderegger C
,
Tscherrig A
. Die Grippepandemie 1918-1919 in der Schweiz. In:
Krämer D
,
Pfister CS
, editors
. Woche für Woche neue Preisaufschläge» Nahrungsmittel-, Energie- und Ressourcenkonflikte in der Schweiz des Ersten Weltkrieges. Basel: Schwabe. 2016.
16.
Helgertz J
,
Bengtsson T
. The Long-Lasting Influenza: The Impact of Fetal Stress During the 1918 Influenza Pandemic on Socioeconomic Attainment and Health in Sweden, 1968-2012. Demography. 2019 Aug;56(4):1389–425. https://doi.org/10.1007/s13524-019-00799-x
17.
Butie C
,
Matthes KL
,
Hösli I
,
Floris J
,
Staub K
. Impact of World War 1 on placenta weight, birth weight and other anthropometric parameters of neonatal health. Placenta. 2020 Oct;100:150–8. https://doi.org/10.1016/j.placenta.2020.07.003
18.
Bloom-Feshbach K
,
Simonsen L
,
Viboud C
,
Mølbak K
,
Miller MA
,
Gottfredsson M
, et al.
Natality decline and miscarriages associated with the 1918 influenza pandemic: the Scandinavian and United States experiences. J Infect Dis. 2011 Oct;204(8):1157–64. https://doi.org/10.1093/infdis/jir510
19.
Plagemann A
,
Harder T
,
Schellong K
,
Schulz S
,
Stupin JH
. Early postnatal life as a critical time window for determination of long-term metabolic health. Best Pract Res Clin Endocrinol Metab. 2012 Oct;26(5):641–53. https://doi.org/10.1016/j.beem.2012.03.008
20.
Jones PM
,
Minton J
,
Bell A
. Methods for disentangling period and cohort changes in mortality risk over the twentieth century: comparing graphical and modelling approaches [Internet]. Qual Quant. 2022;(Aug):1–21. https://doi.org/10.1007/s11135-022-01498-3
21.
Human Mortality Database
. Available from: https://www.mortality.org/
22.
Azambuja MI
. Spanish flu and early 20th-century expansion of a coronary heart disease-prone subpopulation. Tex Heart Inst J. 2004;31(1):14–21.