Long-term development of assisted suicide in Switzerland: analysis of a 20-year experience (1999–2018)
DOI: https://doi.org/10.57187/smw.2023.40010
Giacomo
Montagnaab, Christoph
Junkerc, Constanze
Elfgende, Andres R.
Schneebergerfgh, Uwe
Güthdi
aBreast Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, USA
bBreast Centre, University of Basel, Switzerland
cFederal Statistical Office, Neuchâtel, Switzerland
dBreast Centre Zurich, Switzerland
eFaculty of Medicine, University of Witten/Herdecke, Witten, Germany
fPsychiatric Services Grisons, Chur, Switzerland
gPsychiatric Hospital, University of Zurich, Switzerland
hAlbert Einstein College of Medicine, New York, USA
iFaculty of Medicine, University of Basel, Switzerland
Summary
AIMS OF THE STUDY: The legalisation of assisted suicide is one of the most debated topics in the field of medical ethics worldwide. In countries in which assisted suicide is not legal, public discussions about its approval also encompass considerations of the long-term consequences that such legalisation would bring, for example, how many people will use this option, from what conditions would they be suffering, would there be differences between male and female assisted suicide and which developments and trends could be expected if there were to be a marked increase of cases of assisted suicide over time?
METHODS: In order to answer these questions, we present the development of assisted suicide in Switzerland over a 20-year period (1999–2018; 8738 cases) using data from the Swiss Federal Statistical Office.
RESULTS: During the observation period, the number of assisted suicides rose significantly: when four 5-year periods (1999–2003, 2004–2008, 2009–2013, 2014–2018) were analysed, the number of assisted suicide cases doubled over each period compared with the preceding one (Χ = 206.7, 270.4 and 897.4; p <0.001). The percentage of assisted suicides among all deaths rose from 0.2% (1999–2003; n = 582) to 1.5% (2014–2018: n = 4820). The majority of people who chose assisted suicide were elderly, with increasing age over time (median age in 1999–2003: 74.5 years vs 2014–2018: 80 years), and with a predominance of women (57.2% vs 42.8%). The most common underlying condition for assisted suicide was cancer (n = 3580, 41.0% of all assisted suicides). Over time, assisted suicide increased similarly for all underlying conditions; however, the proportion in each disease group remained unchanged.
CONCLUSIONS: It is a matter of one’s viewpoint whether the rise of assisted suicide cases should be considered alarming or not. These figures reflect an interesting social development but still do not appear to represent a mass phenomenon.
Introduction
The legalisation of medical aid in dying is one of the most debated topics in the field of medical ethics worldwide [1–5]. There is a small but increasing number of countries where this is legal under certain circumstances, including Switzerland, the Netherlands, Belgium, Luxembourg, Austria, Spain, Colombia, Canada, some US states (California, Colorado, Hawaii, Maine, Montana, New Jersey, New Mexico, Oregon, Washington state, Vermont and Washington D.C.), New Zealand and the six Australian states (New South Wales, Queensland, South Australia, Tasmania, Victoria und Western Australia) [6–10].
In countries where assisted dying is not yet legal, there are ongoing intensive, and often controversial debates on this topic, in particular on assisted suicide. Public discussions about its approval not only include fundamental ethical matters. The public decision-makers who decide whether this should be allowed in their countries might wonder what would happen if they did allow it [11–13]. One might ask, with legalisation, what long-term consequences will it bring? The primary focus of our work was to provide relevant data and information regarding the historical context of assisted suicide in Switzerland, and create a foundation for this discussion by answering the following questions:
- How many people will use this option? What will be the ratio of assisted suicides to all deaths?
- How quickly and with what dynamics will there be an increase in the number of expected cases?
- From what conditions will the persons be suffering who choose assisted suicide?
- Would there be differences between male and female assisted suicides?
- How old are patients who select this path?
- Which developments and trends could be expected if there were to be a marked increase in assisted suicide cases over time? Are there shifts in sociodemographic factors or underlying disease, for example will more younger people choose this path over time, or will certain illnesses become quantitatively more dominant?
In order to address these questions, empirical data from Switzerland provides valuable data for this discussion. Switzerland is the country where assisted suicide has been legal the longest. Important aspects of the Swiss model, which need to be considered when interpreting data from Switzerland, are summarised in table 1 [14, 15]. Since assisted suicide in Switzerland is not only not illegal, but also widely socially accepted, relatively freely available and performed with a defined procedure, these data can be useful for countries that debate whether or not to permit assisted dying in the form of assisted suicide but would not go so far as to legalise active euthanasia. From an ethical viewpoint, there are substantial differences between the two practices. In assisted suicide, the role of the doctor consists of prescribing the lethal dose of a certain drug. The critical point is that patients, voluntarily wishing to die, must carry out the final act of the procedure themselves [16]. In active euthanasia, the physician also administers the lethal drug. Opponents of this practice argue that precisely this active role in the process of dying violates the essence of medicine and might undermine irreversibly the patients' and society’s trust in the moral integrity of the medical profession [17].
The differences between assisted suicide and active euthanasia, however, appear not to be an issue of a purely ethical nature. Data from countries in which both practices are allowed (e.g., the Netherlands and Belgium) show that euthanasia occurs much more frequently and represents more than 95% of hastened deaths. A possible explanation is that euthanasia would lower the psychological threshold for requesting assisted dying. This would also explain the substantial and continuing rise of assisted deaths in these countries (euthanasia is quickly approaching 5% of all deaths in the Netherlands) compared with countries in which only assisted suicide is permitted [1, 2].
The present study is a continuation of the previous work published by Steck et al. [18, 19], which was based on 3941 assisted suicide cases in Switzerland over a 12-year period [19]. By using the data that were recorded in the Swiss National Cohort, they were able to demonstrate that socioeconomic factors associated with assisted suicide (e.g., female gender, higher education, having no religious affiliation, no living children, residing in an urban/peri-urban area and in a neighbourhood with a higher socioeconomic index) remained stable over time. In contrast to their study, we report the most recent development and included a higher number of assisted suicide cases: with 8738 cases over a 20-year period, we share our analysis of the longest period and highest number of cases ever reported on assisted suicide in the medical literature.
Linguistic aspects: A conscious and sensitive use of language related to the topic “medical aid in dying / assisted dying / assisted suicide / euthanasia” is absolutely required. We know that in the USA the language has evolved in a way that currently the term “medical aid in dying” instead of “assisted suicide” is preferred. Not to use the term “suicide” recognises the fact that the practice of medical aid in dying is distinct from the behaviour that has been traditionally and ordinarily described as “suicide” and people who seek medical aid in dying due to an incurable and life-ending illnesses might feel deeply offended when the medical practice is referred to as “suicide” [20]. We appreciate this approach. However, the term “medical aid in dying” is a comparably neutral term and can only be understood within the framework of and in accordance with the applicable provisions of the local law. In the USA and Switzerland medical aid in dying requires the patient to be able to take the medication themselves, and euthanasia is illegal. By contrast, in Belgium and the Netherlands “medical aid in dying” practically means “euthanasia.” In order to clearly define the aim and the scope of our work, we chose not to use the neutral term “medical aid in dying“, but instead the more specific term “assisted suicide” which corresponds with the terminology used in Switzerland (table 1).
Table 1The Swiss model of assisted suicide (AS): distinctive legal and social aspects [14, 15, 28].
|
1. The country has a long history of legal AS.
|
Neither the legal code nor professional bodies in Switzerland take measures against doctors who participate in AS in accordance with applicable laws. |
| Swiss Criminal Code (Strafgesetzbuch) [36] |
Direct active euthanasia is a criminal offence according to the Articles 111 (“Intentional homicide”), 113 (“Manslaughter”) and 114 (“Homicide at the request of the victim”). |
| According to the Article 115 which entered into force in 1942, AS is only illegal in cases where it is carried out “for selfish motives”. |
| The Swiss model of AS arose in the 1980s with this background of comparatively open legal regulation. |
| Swiss courts place considerable weight on the autonomous responsibility of the doctor in respect of his or her practical actions in participating in AS. |
| Swiss Academy of Medical Sciences (SAMS) Guidelines* (Version 2013) [33] |
According to the SAMS, it is still considered to be a matter of principle that assisting suicide is not a part of medical practice because it contradicts the goals of medicine. However, should a doctor assist as a matter of personal conscience in a suicide, this is possible under certain and clearly defined conditions: |
| – The patient’s illness justifies the assumption that the end of life is near or can be expected to be near. |
| – Alternative options for assistance have been discussed and, where desired, implemented. |
| – The capability of making decisions has been established. |
| – The wish for death is the result of serious consideration without external pressure and is enduring, the assessment from an independent third party, who is not necessarily a doctor. |
| – The desire for suicide does not arise from a mental health problem. |
| – Several consultations have taken place between doctor and patient. |
| – Alternative therapies have been discussed and/or implemented. |
| – The evaluating doctor possesses an appropriate specialist knowledge of the underlying disease. |
| – The prescribing doctor must not be the only one to certify mental competence. |
| – Relatives should be involved where possible. |
|
2. Social developments which are comparable with other modern Western societies
|
An ageing society where life expectancy is high (in 2018, the life expectancy was 85.4 years for women, and 81.7 years for men) and chronic conditions are the leading cause of death [24, 25]. |
| An increasingly secular society, in which religious convictions play an ever smaller role in personal lifestyle decisions. |
|
3. High-quality palliative care
|
The growth of AS in Switzerland is not due to a lack of palliative care. There is an extensive network of palliative care teams in specialised care centers, hospices and outpatient facilities. |
|
4. The high level of social acceptance for AS from both the general public and the medical fraternity arises out of a national tradition in which the autonomy of the individual is esteemed
|
General public: a referendum that was held in the most populated canton (Canton Zurich) in May 2011, which was intended to put an end to the current practice ("Stop Assisted Suicide") was rejected by 84% of the vote [37]. |
| Medical fraternity: a majority of Swiss doctors currently agree with AS. In a survey of 1318 doctors, 77% responded that under certain conditions AS would be acceptable [38]. |
| The high level of social acceptance for AS has left its traces in the everyday language. It has become common to hear people who are suffering from serious illnesses express themselves very openly on the subject of AS (“… and if necessary, I’ll go to EXIT.” A further common expression is: “I don’t want to take assisted suicide, but it is a comfort to know that it is there should I need it …“). |
|
5. The organisations for assisted dying …
|
… play an important role in the public perception of AS. These organisations champion the right to assisted death and promote this in the form of accompanied suicide. |
|
6. The sequence of events in an AS is clearly defined
|
There is a tried and tested interaction between the three participants in the act: |
| – the patient wishing to die; |
| – the physician who prescribes the lethal drug after careful assessment of the underlying disease and the ‘capacity of judgement’ of the patient; |
| – the organisations for assisted dying which accompany the act of suicide. |
| The patient must freely request the help of the association, must submit a physician’s medical certificate mentioning the diagnosis. A support assistant, who is not necessarily a physician, then pays them a visit, to verify the actual wish to die. Then either the attending physician or a physician of the association will issue the prescription for obtaining the lethal substance. A support assistant will come on the day of the suicide with the substance, which will be ingested by the patient himself/herself. A report is then filled in at this time for the attention of the authorities. |
|
7. Reliable data
|
After death all cases of AS must be reported to the appropriate police agency as an "extraordinary death". As a result of this reporting obligation the Swiss Federal Office for Statistics is able to deliver reliable information about the situations that bring people to avail themselves of AS. |
Material and methods
Data source
The Swiss Cause of Death Statistics are based on medical cause listed on the death certificates. Diagnoses are recorded based on the International Classification of Diseases (ICD-10) and are collected by the Federal Statistical Office (FSO) according to the rules defined by the World Health Organization (WHO) [21]. All collected data are treated anonymously and strictly confidentially, and are subject to the provisions of the Federal Data Protection Act of 19 June 1992 (SR 235.1) [22]. Publications on the Cause of Death Statistics refer to persons who are a resident in Switzerland, i.e. on the permanent resident population regardless of nationality and place of death.
Since the end of the 1990s, the FSO has received isolated notifications of assisted suicide. As the ICD-10 does not have any code for assisted suicide, in the beginning these cases were classified as suicide by poisoning. Since 2009, assisted suicide has been logged consistently with code X61.8 as concomitant cause of death. In all cases, the illness or disease leading to the suffering was coded as underlying cause of death [21]. In this sense, assisted suicide is usually the last resort taken at the end of a serious disease [21].
For this study, we analysed all death cases in Switzerland between 1999 and 2018; in this 20-year period 1,261,923 people died (table 2). Typical for an ageing Western population, the median age at death was high (82 years; men 78 years, women 85 years) and chronic conditions and cancer diseases were the leading causes of death (e.g., cancer: age-standardised rate for men: 29.3% of all causes of death; women: 22.2%) [23, 24]. Women had a higher life expectancy than men (in 2018 85.4 years vs 81.7); an increase of life expectancy was observed both in women (in 2000: 82.6 years) and more pronounced in men (in 2000: 76.9 years) [25].
Table 2Death cases in Switzerland (1999–2018) with particular consideration of assisted suicide (AS) as cause of death.
|
Time period
|
Entire period 1999–2018
|
1999–2003
|
2004–2008
|
2009–2013
|
2014–2018
|
|
All death cases (men and women)
|
1,261,923 |
311,097 |
303,909 |
316,350 |
330,567 |
| Median age at death |
82 |
80 |
81 |
82 |
83 |
|
Cause of death: AS (% of all causes)
|
8738 |
582 (0.2) |
1161 (0.4) |
2175 (0.7) |
4820 (1.5) |
| Chi-square statistic (p-value) |
|
|
206.7 (p <0.001) |
270.4 (p <0.001) |
897.4 (p <0.001) |
| Median age at death |
78 |
75 |
76 |
78 |
80 |
| Men |
All male death cases
|
609,701 |
150,725 |
146,929 |
152,365 |
159,682 |
| Median age at death |
78 |
77 |
78 |
79 |
80 |
|
Cause of death: AS (% of all causes)
|
3737 |
244 (0.2) |
514 (0.4) |
922 (0.6) |
2057 (1.3) |
| % increase compared with the previous period |
|
|
+110.7% |
+79.4% |
+123.1% |
| Chi-square statistic (p-value) |
|
|
103.5 (p <0.001) |
102.1 (p <0.001) |
387.7 (p <0.001) |
| Median age at death |
77 |
74 |
76 |
76 |
78 |
| Women |
All female death cases |
652,222 |
160,372 |
156,980 |
163,985 |
170,885 |
| Median age at death |
85 |
84 |
84 |
85 |
86 |
|
Cause of death: AS (% of all causes)
|
5001 |
338 (0.2) |
647 (0.4) |
1253 (0.8) |
2763 (1.6) |
| % increase compared with the previous period |
|
|
+91.4% |
+93.6% |
+120.5% |
| Chi-square statistic (p-value) |
|
|
103.9 (p <0.001) |
168.8 (p <0.001) |
513.6 (p <0.001) |
| Median age at death |
79 |
76 |
76 |
79 |
81 |
Statistical analysis
Chi-square tests were used to demonstrate the significant increase in assisted suicide cases over time, and to compare the most frequent underlying condition in men and women. A p-value <0.05 was considered significant. Statistical analyses were performed with the Statistical Package for the Social Sciences (IBM® SPSS® Statistics, Version 21, IBM Corp., Armonk, New York).
Results
Assisted suicide in Switzerland: a significant increase over time
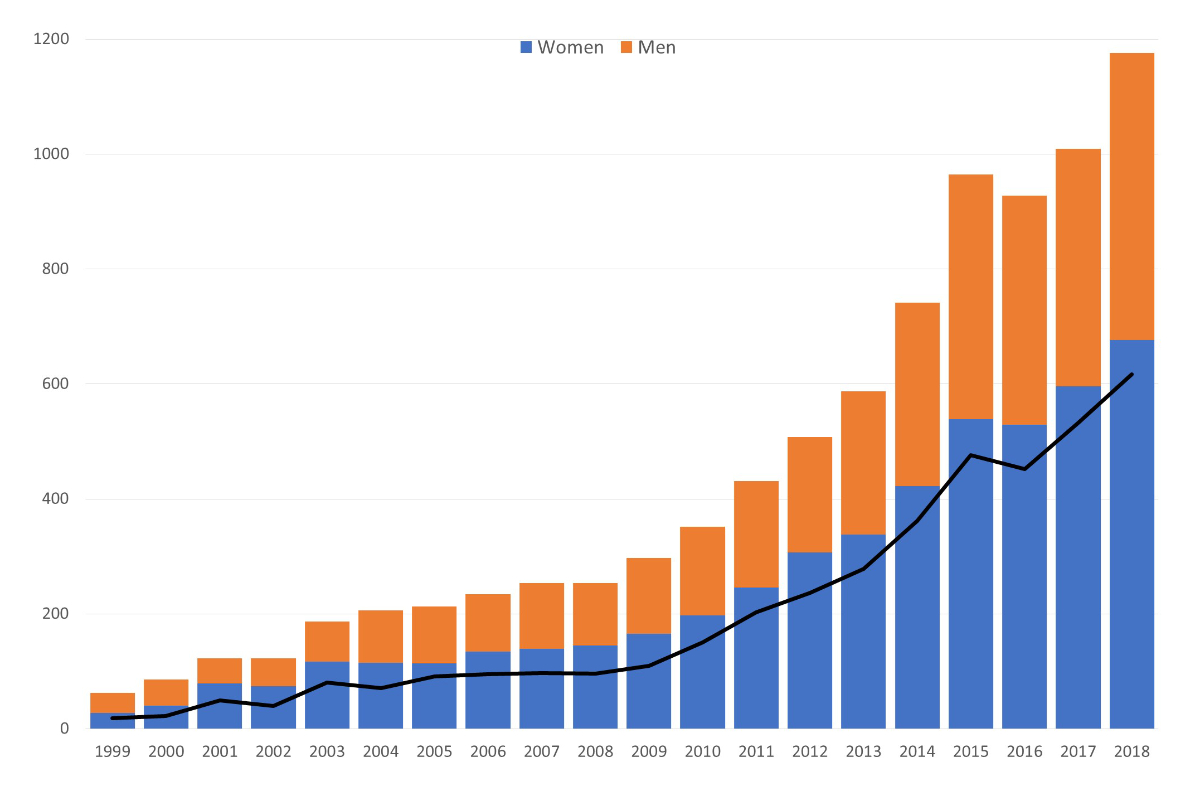
Between 1999 and 2018, a total of 8738 cases of assisted suicide were registered among Swiss residents. During the observation period the annual number of assisted suicides rose substantially (fig. 1). At the beginning of our observation period in 1999 the number was 63. In 2004 the 200 mark was exceeded (n = 206), in 2012 the 500 mark (n = 508) and in 2017 the 1000 mark (n = 1007) were surpassed. For the purposes of the representation of the development of assisted suicide during the whole observation period of 20 years, we have selected four 5-year-intervals to analyse further. The individual time intervals contain similar numbers of assisted suicide (1999–2003 range 63–187; 2004–2008 range 206–254; 2009–2013 range 297–587; 2014–2018 range 742–1176). Table 2 demonstrates that there was a significant increase in assisted suicide cases in all of the above mentioned 5-year time periods compared with the respective preceding period, in women and men alike. In general, the total cases somewhat doubled for every respective period. In the most current period, there was a further marked rise in assisted suicide (an increase of more than 120% compared with the preceding period): in total approximately 55% of all assisted suicide cases in the 20-year observation occurred in this 5-year period. Thus, it appeared to be particularly important to represent this marked trend separately from the preceding years. During the observation period, the crude ratio of assisted suicide to all death cases rose from 0.2% in 1999–2003 to 1.5% in 2014–2018 (table 2). In 2018, the number of annual suicides reached its highest point ever, at 1176 cases, making up 1.8% of all death cases.
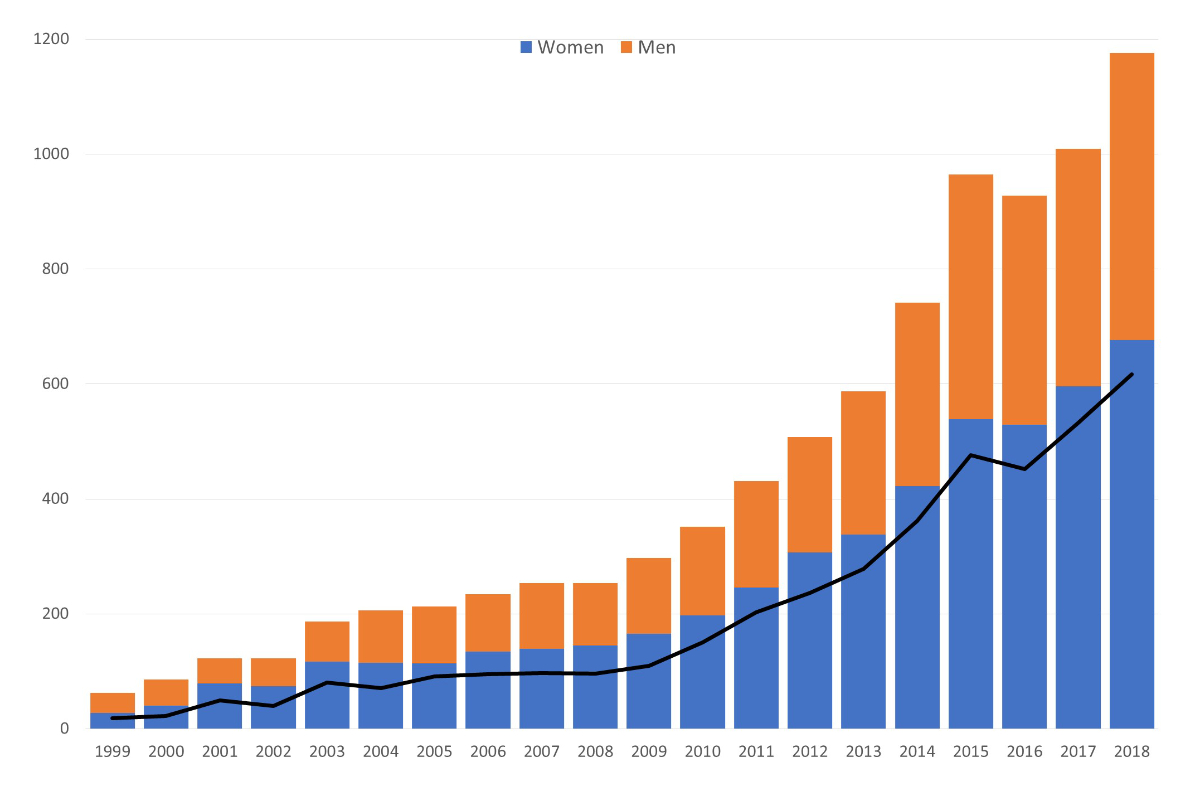
Figure 1 Assisted suicide in Switzerland 1999–2018: sex and advanced age (≥80 years at time of death) distribution.
Sex: There was a stable predominance of women over the four defined time intervals: 1999–2003: 58.1%; 2004–2008: 55.7%; 2009–2013: 57.6%; 2014–2018: 57.3%.
Advanced age, i.e. persons ≥80 years at time of assisted suicide (black line): 1999–2003: 36.4% (♀ 39.6%; ♂ 32.0%); 2004–2008: 39.1% (♀ 40.6%; ♂ 37.1%); 2009–2013: 45.0% (♀ 49.0%; ♂ 39.5%); 2014–2018: 50.6% (♀ 54.0%; ♂ 46.1%).
Age and sex
Assisted suicide was generally chosen by older people (median age at death 78 years). In the two most current observation periods (from 2009–2018), 48.9% of persons who chose assisted suicide were 80 years or older. In this 10-year period, only 24 persons were under 36; this corresponds to only 0.3% of assisted suicide cases. Over time, the median age at death increased more for persons who chose assisted suicide (1999–2003 vs 2014–2018: +5.5 years) than for the total population (1999–2003 vs 2014–2018: +3 years). There was a stable predominance of women (57.2%; ranges over the four observation periods: 55.7–58.1%; fig. 1), who, at the time of the suicide, were approximately two years older than men (79 years vs 77 years).
Underlying diseases
The most common underlying condition for assisted suicide was cancer (n = 3,580, 41.0%; table 3). Comparison between genders (table 4) shows that cancer was more likely to be the most underlying condition in men than in women (48.8% vs 35.2%; chi-square statistic = 163.6, p <0.001). The second leading cause for assisted suicide was neurodegenerative diseases (13.0%), a further 10.9% suffered from a cardiovascular disease and 9.2% from a musculoskeletal disorder (table 3). The proportion of cases in which a malignant disease was the reason for the assisted suicide remained stable over the four defined time intervals (39.2%, 40.8%, 42.3%, and 40.6%); a similar stable distribution over time was also displayed by other underlying conditions.
Table 3 shows the distribution of assisted suicide by the underlying condition, focusing on the most common types of cancer (those with ≥250 assisted suicide cases): lung, breast, prostate, colorectal, and pancreatic cancer. Over time, assisted suicide increased for all cancer types. However, the proportion of cases of assisted suicide within the various cancer types remained unchanged over time (as did the distribution of the underlying diseases in the total group of assisted suicides). There was a continuous rise in the percentage of cancer-related assisted suicides in comparison with all cases of cancer-related death: 0.3% in the first study interval (1999–2003) vs 2.3% in the last (2014–2018).
Table 3Assisted suicide (AS) cases in Switzerland (1999–2018): distribution of underlying diseases.
|
Time period
|
Entire period 1999–2018
|
1999–2003
|
2004–2008
|
2009–2013
|
2014–2018
|
|
All cases with AS
|
8738 |
582 |
1161 |
2175 |
4820 |
| Median age of death (5th to 95th percentile) |
78 (52–93) |
75 (43–91) |
76 (50–92) |
78 (52–93) |
80 (55–94) |
|
Underlying disease reported:
|
|
1. Cancer (%)
|
3580 (41.0) |
228 (39.2) |
474 (40.8) |
920 (42.3) |
1958 (40.6) |
| Median age at death (5th to 95th percentile) |
74 (51–90) |
71 (47–88) |
71 (48–88) |
74 (52–91) |
75 (53–91) |
| 1.1 Lung |
508 (5.8) |
34 (5.8) |
60 (5.2) |
131 (6.0) |
283 (5.9) |
| 1.2 Colorectal |
387 (4.4) |
22 (3.8) |
49 (4.2) |
99 (4.6) |
217 (4.5) |
| 1.3 Breast |
386 (4.4) |
29 (5.0) |
51 (4.4) |
100 (4.6) |
206 (4.3) |
| 1.4 Prostate |
367 (4.2) |
22 (3.8) |
56 (4.8) |
93 (4.3) |
196 (4.1) |
| 1.5 Pancreas |
270 (3.1) |
9 (1.5) |
39 (3.4) |
61 (2.8) |
161 (3.3) |
| 1.6 Other malignant diseases |
1662 (19.0) |
112 (19.3) |
219 (18.8) |
436 (20.0) |
895 (18.6) |
|
|
2. Other diseases (%)
|
4730 (54.1) |
282 (48.4) |
556 (47.9) |
1174 (54.0) |
2718 (56.4) |
| Median age of death (5th to 95th percentile) |
81 (53–94) |
76 (39–92) |
78 (48–93) |
80 (50–94) |
82 (56–94) |
|
|
2.1 Neurodegenerative diseases
|
1134 (13.0) |
86 (14.8) |
135 (11.6) |
316 (14.5) |
597 (12.4) |
| Median age at death (5th to 95th percentile) |
73 (47–90) |
66 (36–89) |
69 (44–88) |
71 (44–88) |
75 (53–90) |
| 2.1.1 Parkinson’s disease |
245 (2.8) |
16 (2.8) |
25 (2.1) |
66 (3.0) |
138 (2.9) |
| 2.1.2 Amyotrophic lateral sclerosis |
227 (2.6) |
16 (2.8) |
35 (3.0) |
68 (3.1) |
108 (2.2) |
| 2.1.3 Multiple sclerosis |
189 (2.2) |
22 (3.8) |
33 (2.8) |
58 (2.7) |
76 (1.6) |
| 2.1.4 Dementia |
56 (0.6) |
2 (0.3) |
3 (0.3) |
16 (0.7) |
35 (0.7) |
| 2.1.5 Other neurodegenerative diseases |
417 (4.8) |
30 (5.1) |
39 (3.4) |
108 (5.0) |
240 (5.0) |
|
|
2.2 Cardiovascular diseases
|
949 (10.9) |
49 (8.4) |
90 (7.8) |
237 (10.9) |
573 (11.9) |
| Median age at death (5th to 95th percentile) |
85 (66–95) |
86 (73–96) |
84 (70–94) |
84 (64–94) |
86 (66–96) |
|
|
2.3 Musculoskeletal diseases*
|
803 (9.2) |
37 (6.3) |
61 (5.3) |
195 (9.0) |
510 (10.6) |
| Median age at death (5th to 95th percentile) |
85 (67–94) |
82 (55–95) |
83 (63–94) |
84 (67–95) |
86 (70–94) |
|
|
2.4 Mental disorders
|
409 (4.7) |
37 (6.3) |
44 (3.8) |
90 (4.1) |
238 (4.9) |
| Median age at death (5th to 95th percentile) |
77 (42–93) |
75 (29–93) |
78 (44–94) |
74 (36–91) |
80 (45–93) |
|
|
2.5 Lung diseases
|
375 (4.3) |
14 (2.4) |
35 (3.0) |
99 (4.6) |
227 (4.7) |
| Median age at death (5th to 95th percentile) |
77 (61–91) |
77 (50–89) |
77 (55–88) |
77 (61–91) |
79 (46–93) |
|
|
2.6 Infectious diseases
|
62 (0.7) |
12 (2.1) |
13 (1.1) |
14 (0.6) |
23 (0.5) |
| Median age at death (5th to 95th percentile) |
65 (39–87) |
44 (32–97) |
58 (39–81) |
74 (50–90) |
72 (52–88) |
|
|
2.7 Other disorders
|
998 (11.4) |
47 (8.1) |
178 (15.3) |
223 (10.3) |
550 (11.4) |
| Median age at death (5th to 95th percentile) |
84 (55–96) |
75 (35–89) |
79 (51–94) |
83 (58–94) |
86 (62–96) |
|
|
3. Unknown
|
428 (4.9) |
72 (12.4) |
131 (11.3) |
81 (3.7) |
144 (3.0) |
| Median age at death (5th to 95th percentile) |
83 (59–94) |
84 (54–94) |
81 (57–94) |
86 (63–95) |
85 (63–94) |
Table 4Assisted suicide (AS) cases in Switzerland (1999–2018): distribution of sexes.
|
Women, n = 5001 (57.2%)
|
Men, n = 3737 (42.8%)
|
| Median age of death (5th to 95th percentile) |
79 (53–93) |
77 (51–93) |
|
| Cancer was reported as underlying disease (%) |
1758 (35.2) * |
822 (48.8) * |
| Median age at death (5th to 95th percentile) |
73 (51–90) |
75 (51–90) |
|
| Other diseases (%) |
2969 (59.3) |
1761 (47.1) |
| Median age of death (5th to 95th percentile) |
82 (53–94) |
79 (51–94) |
|
| Unknown |
274 (5.5) |
154 (4.1) |
| Median age at death (5th to 95th percentile) |
85 (62–94) |
82 (54–94) |
One unique disease with a particular high percentage of assisted suicide
Amyotrophic lateral sclerosis (ALS) is a comparatively rare progressive neurodegenerative disorder (3465 death cases in the 20 year-period between 1999 and 2018 represent just 0.27% of all death cases in Switzerland; the 227 cases of ALS-related assisted suicide accounted for only 2.6% of all assisted suicides). Over time, the percentages of ALS-related assisted suicide in comparison with all cases of ALS-related death were at any time during the study period 8–10-fold higher than the corresponding crude ratios from all other death cases (1999–2003: percentage of assisted suicide from all death cases: 0.2% vs percentage from ALS-related assisted suicide to all ALS-related death cases: 2.4%; corresponding data for the period 2004–2008: 0.4% vs 4.3%; 2009–2013: 0.7% vs 7.1%; 2014–2018: 1.5% vs 10.7%). As expected, there was an increase in the number of ALS-related assisted suicides over time; however, this rise preceded the general trend; the percentage of ALS-related assisted suicides in relation to all assisted suicide cases remained stable (1999–2003 2.8% vs 2014–2018 2.2%).
Discussion
Underlying diseases
During the 20-year period of the study, no particular disease group became predominantly associated with assisted suicide. The proportion of assisted suicides in each disease group remained roughly the same (minor shifts among non-cancer-related underlying diseases can be explained by a more accurate data collection; in fact, the percentage of cases categorised with “unknown” as a reason for assisted suicide decreased over the study period, with 12% from 1999 to 2008 vs 3–4% between 2009 and 2018). This stable development, which is in line with data reported by Steck et al. [19], is somewhat surprising as one might expect, as a result of the exchange of information between patients or relatives in various internet forums and self-help groups, a trend might emerge in assisted suicide for a particular disease. There is, however, no evidence of such a development. The stable distribution of assisted suicide among various diseases could be interpreted as an indication that the process in the terminal phase of the various illnesses is essentially similar. There seems to be no disease in which the terminal phase is notoriously so symptomatically forbidding or agonising that patients more frequently or prematurely turn to assisted suicide [24].
At first glance, amyotrophic lateral sclerosis holds a special position. There hardly seems to be any other disease where the terminal phase is so notoriously agonising (it is a rapidly progressive disease as the patient becomes totally paralysed, with many patients feeling they are imprisoned in their own body living in fear of chocking to death with full consciousness). In fact, the percentage of assisted suicide for this disease was over time approximately 8–10-fold higher than that of other diseases. However, the rise in the number of ALS-related assisted suicide cases over the 20-year study period corresponds to the general rise of assisted suicide cases, and the percentages of ALS-related assisted suicides compared with the total number of assisted suicide cases remained stable over time (ranging from 2.2–3.1%). Furthermore, due to this comparatively small number of cases (only 2.6% of all assisted suicide cases), ALS-related assisted suicides are, at least from a quantitative point of view, practically negligible.
Age and sex / the slippery slope hypothesis
In Switzerland the vast majority of people who chose to end their lives with assisted suicide were elderly persons. This is reassuring to those who fear that the legalisation and the increase in use of assisted suicide may lead to a growing number of young people choosing this option. The opposite is in fact true: the median ages increased over the study period.
It is noteworthy that the majority of individuals who chose assisted suicide were women. This is in marked contrast to the “classical” suicide in which males take their own lives at nearly four times the rate of females and represent more than 70% of all suicides in Switzerland [21]. One could hypothesise that the preponderance of women committing assisted suicide may be related to the choice of method: it is well known that men use more violent methods of suicide (in Switzerland the most frequent methods for male suicide are hanging and shooting) while women tend to end life prematurely by poisoning [21].
The higher proportion of women and the higher median age at time of assisted suicide, might also reflect different gender-specific sociodemographic factors. Elderly men may have younger partners who can provide the care and support they need; however, this is often not the case for elderly women, who, by having a higher life expectancy, are often widowed or have even older partners unable to provide the care they need. Current data of the Swiss FSO supports this hypothesis. In 2018, among people aged ≥80 years (accounting for 5.2% of the permanent resident population), 62% were women. Whereas 66% of the men aged ≥80 years were still married, only 26% of women in the same group were married. Similarly, in this population 59% of the women and 23% of the men were widowed. Additionally, of the 3% private households with a married couple in which at least one of the spouses was 80 years of age or older, in 74% of cases, the husband was older than the wife (average age difference of five years) [26].
The higher age of people who chose assisted suicide, in particular in non-cancer disease groups (the median age in the most current time interval was 82 years) may partially be explained by the fact that the largest Swiss organisation for assisted dying, “EXIT”, has proposed in recent years an easier access to “old age suicide” [27]. This implies that the option of assisted suicide should also be possible for an elderly person who may not necessarily be suffering from a fatal disease but who, because of the sum of his or her current or expected complaints and ailments (multimorbidity with reduction of bodily functions, decreasing sensory capacity and performance deficits), the lack of perspectives and the disappearance of life-long friends and family members, finds his or her quality of life seriously reduced.
The particular Swiss cultural context in which assisted suicide enjoys a high level of social acceptance [28], might also be mirrored in a comparably low percentage of cancer-associated assisted suicides. Although cancer was still the most common underlying disease for assisted suicide in Switzerland, the percentage of cancer patients within the total group of people who chose assisted suicide was only 40%, which is significantly lower than that in other countries in which 70–80% of assisted dying cases relate to cancer diseases [6, 29–31]. It is obvious that many people in Switzerland, in particular the elderly, choose to assert their freedom to take the option of assisted dying for reasons other than the “classical” fatal disease, cancer.
This development alarms the critics of assisted suicide who warn that after its legalisation, the safeguards put in place for these practices will quickly be bypassed and a broadening of the medical indications for assisted suicide will lead to an uncontrolled extension to people who are not terminally ill or do not suffer from severe symptoms or conditions. This “slippery slope effect” refers to a situation in which an innovation, once introduced, develops its own possibly unstoppable momentum to extend beyond its initial boundaries. For the advocates of the principle that assisted suicide should be performed only in cases in which patients suffer from a terminal illness and/or experience unbearable and uncontrollable pain, the legalisation of “old age suicide” is a step too far. They fear a development in which the next slip down the slope takes in the vulnerable elderly who, whether from the viewpoint of the state and/or that of the family, now perform no useful social function [6, 32]. In this situation they can be pressured into wishing to dispose of themselves as they are perceived as a liability for those around them.
Differing standpoints regarding “old age suicide” are reflected in the current discussions that are taking place within the professional bodies of Swiss medicine. The guidelines of the Swiss Academy of Medical Sciences (SAMS) regarding physician-assisted suicide have changed over time from categorical rejection to a more flexible position in 2004 (and in a revised version in 2013 [33], table 1). The Swiss Medical Association, Foederatio Medicorum Helveticorum (FMH), has up to now taken up every change of the SAMS guidelines in its medical practice regulations. The guidelines thus became obligatory for all members of the FMH. The most current SAMS guideline “Management of dying and death”, passed in 2018, extended the indications for assisted suicide appreciably and replaced the former terminal illness requirement (“The patient’s illness justifies the assumption that the end of life is near or can be expected to be near” [33]) with a revised condition that “the symptoms of disease and/or functional impairments are a source of intolerable suffering for the patient” [34]. These revised guidelines, however, were initially still rejected by the FMH (the first SAMS guideline in 20 years which was not taken up in the professional code). The decision was taken on the grounds that the precondition of “unbearable suffering” for assisted suicide was an undefined legal concept which would lead to a great degree of legal uncertainty [35]. In May 2022, a further revised version of the SAMS
guideline was adopted by the FMH in the Professional Code of Conduct. The
criterion formulated for the first time in 2018 that “intolerable
suffering” is sufficient for granting euthanasia remained untouched.
Limitations
There are some methodological weaknesses that affect the complete and correct identification of assisted suicide in Switzerland (e.g., lack of a central obligatory registry for assisted suicide, cases may be missed or not reported appropriately, death certificates might be an error-prone source for information about the underlying disease), which must be considered in the interpretation of our data. For more detailed information on these points, we refer to the excellent overview given by Steck and colleagues [19].
Conclusion
Our analysis of the 20-year experience with assisted suicide in Switzerland demonstrates that for every 5-year subperiod the number of assisted suicide cases doubled compared with the preceding 5-year period. During the most current time period from 2014–2018, assisted suicide comprised of 1.5% of all death cases. It is a matter of one’s viewpoint whether this rise should be considered alarming or not. These figures reflect an interesting social development but still do not appear to represent a mass phenomenon. However, the current rates could be just a snapshot of the progression to an even greater expansion of assisted suicide in the future.
Some contents of the manuscript have been presented in part as an invited lecture at the European School of Oncology (ESO) / European Society for Medical Oncology (ESMO) Advanced Breast Cancer Fifth International Consensus Conference (ABC5), Lisbon, November 2019.
Acknowledgments
We thank the Federal Statistical Office (FSO) for providing mortality and census data and for the support that made this study possible. The authors thank Georg Bosshard, Richard Law, and Shaun McMillan for their intellectual input. Thanks are due to Andreas Schötzau for statistical advice.
Author contributions: All authors meet the journal’s criteria for authorship and agree to be accountable for all aspects of the work. They have directly participated in the planning, execution, or analysis of the study. They have read and approved the final version submitted.
Uwe Güth, MD
Breast Centre Zurich
Seefeldstrasse 214
CH-8008 Zurich
uwe.gueth[at]unibas.ch
References
1.
Borasio GD,
Jox RJ,
Gamondi C.
Regulation of assisted suicide limits the number of assisted deaths. Lancet. 2019 Mar;393(10175):982–3. https://doi.org/10.1016/S0140-6736(18)32554-6
2.
Gamondi C,
Borasio GD,
Limoni C,
Preston N,
Payne S.
Legalisation of assisted suicide: a safeguard to euthanasia? Lancet. 2014 Jul;384(9938):127. https://doi.org/10.1016/S0140-6736(14)61154-5
3.
Lo B.
Beyond Legalization - Dilemmas Physicians Confront Regarding Aid in Dying. N Engl J Med. 2018 May;378(22):2060–2. https://doi.org/10.1056/NEJMp1802218
4.
McPherson A.
Dying and choosing. Lancet. 2009 Oct;374(9698):1325. https://doi.org/10.1016/S0140-6736(09)61814-6
5.
Snyder Sulmasy L,
Mueller PS,
Ethics P
; Ethics, Professionalism and Human Rights Committee of the American College of Physicians. Ethics and the Legalization of Physician-Assisted Suicide: An American College of Physicians Position Paper. Ann Intern Med. 2017 Oct;167(8):576–8. https://doi.org/10.7326/M17-0938
6.
Emanuel EJ,
Onwuteaka-Philipsen BD,
Urwin JW,
Cohen J.
Attitudes and Practices of Euthanasia and Physician-Assisted Suicide in the United States, Canada, and Europe. JAMA. 2016 Jul;316(1):79–90. https://doi.org/10.1001/jama.2016.8499
7. Parliament of Victoria. Voluntary Assisted Dying. Available at: https://www.parliament.vic.gov.au/publications/research-papers/download/36-research-papers/13834-voluntary-assisted-dying-bill-2017. Accessed 22.10.2021.
8.
Death With Dignity. Available at: https://www.deathwithdignity.org. Accessed 22.10.2021.
9.
Wikipedia. Asssited suicide. Available at: https://en.wikipedia.org/wiki/Assisted_suicide. Accessed 20.10.2021.
10.
Rada AG.
Spain will become the sixth country worldwide to allow euthanasia and assisted suicide. BMJ. 2021 Jan;372(147):n147. https://doi.org/10.1136/bmj.n147
11.
Porter K,
Warburton KG.
Physicians’ views on current legislation around euthanasia and assisted suicide: Results of surveys commissioned by the Royal College of Physicians. Future Healthc J. 2018 Feb;5(1):30–4. https://doi.org/10.7861/futurehosp.5-1-30
12.
Crumley ET,
Sheppard C,
Bowden C,
Nelson G.
Canadian French and English newspapers’ portrayals of physicians’ role and medical assistance in dying (MAiD) from 1972 to 2016: a qualitative textual analysis. BMJ Open. 2019 May;9(4):e020369. https://doi.org/10.1136/bmjopen-2017-020369
13.
Sperling SK.
Oregon’s Death With Dignity Act. JAMA Oncol. 2018 May;4(5):747–8. https://doi.org/10.1001/jamaoncol.2017.5302
14.
Ziegler SJ,
Bosshard G.
Role of non-governmental organisations in physician assisted suicide. BMJ. 2007 Feb;334(7588):295–8. https://doi.org/10.1136/bmj.39100.417072.BE
15.
Bartsch C,
Landolt K,
Ristic A,
Reisch T,
Ajdacic-Gross V.
Assisted Suicide in Switzerland: An Analysis of Death Records From Swiss Institutes of Forensic Medicine. Dtsch Arztebl Int. 2019 Aug;116(33-34):545–52.
16.
Bosshard G,
Jermini D,
Eisenhart D,
Bär W.
Assisted suicide bordering on active euthanasia. Int J Legal Med. 2003 Apr;117(2):106–8. https://doi.org/10.1007/s00414-002-0346-3
17.
Sprung CL,
Somerville MA,
Radbruch L,
Collet NS,
Duttge G,
Piva JP, et al.
Physician-Assisted Suicide and Euthanasia: Emerging Issues From a Global Perspective. J Palliat Care. 2018 Oct;33(4):197–203. https://doi.org/10.1177/0825859718777325
18.
Steck N,
Junker C,
Maessen M,
Reisch T,
Zwahlen M,
Egger M
; Swiss National Cohort. Suicide assisted by right-to-die associations: a population based cohort study. Int J Epidemiol. 2014 Apr;43(2):614–22. https://doi.org/10.1093/ije/dyu010
19.
Steck N,
Junker C,
Zwahlen M
; Swiss National Cohort. Increase in assisted suicide in Switzerland: did the socioeconomic predictors change? Results from the Swiss National Cohort. BMJ Open. 2018 Apr;8(4):e020992. https://doi.org/10.1136/bmjopen-2017-020992
20. Compassion and Choices. Medical Aid In Dying Is Not Assisted Suicide, Suicide or Euthanasia. Available at: https://compassionandchoices.org/resource/assisted-suicide/. Accessed 02.07.2021, 2021.
21.
Federal Statistical Office (FSO). Cause of death statistics. Assisted Suicide and suicide in Switzerland. Available at: https://www.bfs.admin.ch/bfs/de/home/statistiken/kataloge-datenbanken/publikationen.assetdetail.3902308.html. Published 2016. Accessed 20.10.2021.
22.
The Federal Assembly of the Swiss Confederation. Federal Act on Data Protection. Available at: https://www.admin.ch/opc/en/classified-compilation/19920153/index.html. Accessed 20.10.2021.
23.
Montagna G,
Junker C,
Elfgen C,
Schneeberger AR,
Güth U.
Assisted suicide in patients with cancer. ESMO Open. 2022 Feb;7(1):100349. https://doi.org/10.1016/j.esmoop.2021.100349
24.
Federal Statistical Office. (FSO. Death and its main causes in Switzerland, 2018. Availabe at: https://www.bfs.admin.ch/bfs/en/home/statistics/health/state-health/mortality-causes-death/specific.gnpdetail.2021-0541.html. Published 2021. Accessed 26.04.2022.
25.
Federal Statistical Office. (FSO. Life expectancy in Switzerland, 2000-2020. Available at: https://www.bfs.admin.ch/bfs/en/home/statistics/population/births-deaths/life-expectancy.assetdetail.18845607.html. Published 2021. Accessed 26.04.2022.
26.
Federal Statistical Office (FSO). Structural Survey. Population and Households Statistics. Available at: https://www.bfs.admin.ch/bfs/en/home/statistics/population/surveys/statpop.html Published 2016. Accessed 20.10.2021.
27.
EXIT. Der Altersfreitod ist mehrheitsfähig. Available at: https://exit.ch/artikel/der-altersfreitod-ist-mehrheitsfaehig/. Published 2014. Accessed 20.10.2021.
28.
Burkhardt S,
La Harpe R.
Debates about assisted suicide in Switzerland. Am J Forensic Med Pathol. 2012 Dec;33(4):410–3. https://doi.org/10.1097/PAF.0b013e318273b83f
29.
Onwuteaka-Philipsen BD,
Brinkman-Stoppelenburg A,
Penning C,
de Jong-Krul GJ,
van Delden JJ,
van der Heide A.
Trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-sectional survey. Lancet. 2012 Sep;380(9845):908–15. https://doi.org/10.1016/S0140-6736(12)61034-4
30.
Chambaere K,
Vander Stichele R,
Mortier F,
Cohen J,
Deliens L.
Recent trends in euthanasia and other end-of-life practices in Belgium. N Engl J Med. 2015 Mar;372(12):1179–81. https://doi.org/10.1056/NEJMc1414527
31.
Hedberg K,
New C.
Oregon’s Death With Dignity Act: 20 Years of Experience to Inform the Debate. Ann Intern Med. 2017 Oct;167(8):579–83. https://doi.org/10.7326/M17-2300
32.
Sulmasy DP,
Finlay I,
Fitzgerald F,
Foley K,
Payne R,
Siegler M.
Physician-Assisted Suicide: Why Neutrality by Organized Medicine Is Neither Neutral Nor Appropriate. J Gen Intern Med. 2018 Aug;33(8):1394–9. https://doi.org/10.1007/s11606-018-4424-8
33.
Swiss Academy of Medical Sciences. Care of patients in the end of life. Available at: https://www.samw.ch/en/Ethics/Topics-A-to-Z/Dying-and-death/Background-dying-and-death.html. Published 2013. Accessed 20.10.2021.
34.
Swiss Academy of Medical Sciences. Management of dying and death. Available at: https://www.samw.ch/en/Ethics/Topics-A-to-Z/Dying-and-death.html. Published 2018. Accessed 20.10.2021.
35.
FMH-Swiss Medical Association. Stellungnahme der FMH zu den SAMW-Richtlinien «Umgang mit Sterben und Tod». Available at: https://www.fmh.ch/_service/suche.cfm#q=Assistierte%20Suizidbeihilfe. Published 2018. Accessed 20.10.2021.
36.
The Federal Assembly of the Swiss Confederation. Swiss Criminal Code of 21 December 1937. Available at: https://www.admin.ch/opc/en/classified-compilation/19370083/index.html#id-ni1-ni2. Accessed 20.10.2021.
37.
Canton of Zurich. Wahlen & Abstimmungen. Available at: https://wahlen-abstimmungen.zh.ch/internet/justiz_inneres/wahlen-abstimmungen/de/abstimmungen/abstimmungsarchiv.html?tag=15.05.2011. Published 2011. Accessed 20.10.2021.
38.
Brauer S,
Bolliger C,
Strub JD.
Swiss physicians’ attitudes to assisted suicide: A qualitative and quantitative empirical study. Swiss Med Wkly. 2015 May;145:w14142. https://doi.org/10.4414/smw.2015.14142