
Figure 1 Number of operations divided by different types of hip arthroplasty and gender from 1969 to 2019 at 5-year intervals.
DOI: https://doi.org/10.57187/smw.2023.40047
Prosthetic hip replacement is one of the most successful operations, with a cumulative 20-year revision rate for osteoarthritis of less than 10% [1]. It is not surprising that total hip arthroplasty has been called “the operation of the century” by Learmonth et al. [2].
In the Kantonsspital St. Gallen, the first prosthetic hip joint in continental Europe was implanted on February 9 in 1961 by the chief orthopaedic surgeon Maurice Edmond Müller, who was co-founder of the Arbeitsgemeinschaft für Osteosynthesefragen (AO) and a pioneer in the field of orthopaedic surgery. In 2002, he was honoured by the International Society of Orthopaedic Surgery and Traumatology (SICO) with the title “Orthopaedic Surgeon of the Century” [3]. His successor Bernhard Georg Weber developed, in addition to a classification of ankle fractures, a novel hip prosthesis system introducing prosthetic heads with three different neck lengths [4]. In this historical context we can refer to data of early hip replacements at our institution.
In Switzerland, prosthetic hip joint replacements have been systematically recorded in the Swiss Implant Registry (SIRIS) since September 1, 2012 [5]. Other comparable prosthesis registers have been collecting data for a longer period of time [1, 6]. For example, the Swedish Hip Arthroplasty Registry was started in 1979 [6]. However, even earlier hip joint replacements at the Kantonsspital St. Gallen were recorded in handwritten operating theatre journals, which contain some of the oldest documented data on hip arthroplasty procedures in Switzerland. These data provide new information on trends in patient characteristics and surgeon caseloads in hip arthroplasty over 50 years in Switzerland.
The aim of this study was to investigate the demographic changes of hip arthroplasty patients over a period of 50 years (1969 to 2019) recorded at 5-year intervals at the Kantonsspital St. Gallen. The focus of this study is the medical history in relation to general population demographic changes over the last 50 years.
The present study was conducted at the Department of Orthopaedic Surgery and Traumatology of the Musculoskeletal System of the Kantonsspital St. Gallen. Today, around 5,000 general orthopaedic surgical procedures are performed annually in three operating theatres. The hospital’s service area mainly includes the population of the canton of St. Gallen as well as the population of neighbouring cantons (in particular Appenzell Ausser- and Innerhoden and Thurgau). This 50-year retrospective exploratory study included patients who received an artificial hip joint replacement (total hip arthroplasty primary, revision or hemiarthroplasty) at the Kantonsspital St. Gallen between January 1, 1969 and December 31, 2019. Every fifth year was included, which resulted in a 5-year sampling rate over the observation period.
The operating theatre journals used for this retrospective explorative study were handwritten until 1999 and digital from 2004 to 2019 (integrated in the hospital data management system). The journal for the years 1972 to 1978 could not be found in the archives, therefore in all tables the first period was 10 years (1969–1979), but from 1979 onwards the data at 5-year intervals were available. The following data were collected: age, sex, place of residence, side of the operated hip, name of main surgeon, type of hip arthroplasty. The surgeons’ names from 2004 and 2009 were no longer accessible for data exports due to changes in the information system. Demographic data from 1969 to 2019 are public and could be downloaded from the Swiss Federal Statistical Office (SFSO) [7].All data was linked to one dataset in an Excel spreadsheet.Data extraction was performed by the first author D. F.
The operation protocols from 1969 contain the year of birth of the patients. To determine the age, the year of birth was subtracted from the year of surgery. In the operation protocols from 1979 to 1999, patient data including the exact date of birth and operation date were recorded, which made it possible to calculate the patients’ age. However, the date of birth was not always legible. In these cases, it could be determined using the social insurance number (AHV number) that contains encoded patient’s name, gender and date of birth [8]. For patients operated on from 2004 to 2019, age was calculated exactly using the specified date of birth and date of operation.
The gender was determined based on the name. If a name was not clearly gender-specific, gender was assigned using the AHV number. We recorded the respective canton as place of residence. The municipality served as the basis for determining the canton, since often only the municipality of residence was noted in the records. For foreign patients, the appropriate country was recorded. The place of residence for patients operated from 2004 to 2019 could be found in the clinical information system of the Kantonsspital St. Gallen.
For the statistical analysis and data visualization IBM® SPSS® version 27 and Microsoft Excel [9, 10] were used and graphics processed with Gimp version 2.10.30 [11]. We applied descriptive statistics to evaluate changes in age and sex distribution, place of residence and caseload per surgeon. Caseload was defined as the number of operations per surgeon per year. A distinction was made between high-volume (>50), medium-volume (15–50) and low-volume (1–14) surgeons. Patients’ age distribution was evaluated separately for men and women and divided by type of hip arthroplasty (total hip arthroplasty primary, revision or hemiarthroplasty) as well as gender distribution. For comparison, Mann-Whitney U-test and binomial test were used. A p-value less than 0.05 was defined as significant. The Mann-Whitney U-test was applied to elaborate whether men and women differed in age for different types of hip arthroplasty. The binomial test was used to examine whether one type of hip arthroplasty was used more frequently on a particular side (H1 is proportion ≠ 0.5) and whether men and women differed in the number of joint replacements according to the type of hip arthroplasty (H1 is proportion ≠ 0.5 as the sex ratio has been close to 50% in Switzerland over the years [7]). A linear regression model was used to assess the association between the median age of patients included in the study with residence in Switzerland and the life expectancy of the Swiss population according to gender and type of hip arthroplasty.
This study was approved by Ethikkomission Ostschweiz (BASEC Nr. Req_2021-01008). According to HFG Art. 2 Abs. 2 lit. c, our research is not subject to the Humanforschungsgesetz. Informed consent was not necessary.
The sample comprised 2,963 records from patients, of which 1,318 were men and 1,608 women. The gender was recorded as “indifferent” in 37 cases because it could not be assigned with sufficient certainty. Records for 11 patients could not be assigned to any prosthesis type. The age of 8 patients was unclear. These records were not included in the corresponding statistical analyses.
Change in number of operations
Overall, significantly more women than men underwent primary total hip arthroplasty (n = 1,156 vs 1,018, p = 0.003) and hemiarthroplasty (n = 241 vs 72, p <0.001). The number of women and men were comparable in the total revision arthroplasty group (n = 206 vs 223, p = 0.440).
The results for the individual years can be seen in figure 1, which shows the number of operations per year according to gender and type of hip arthroplasty and whether men and women differ significantly in this respect.
We calculated the number of operations per year for the patients most at risk (defined as 50–89 yr.). From 1969 to 2019 we obtained the following values at 5-year intervals in ascending order: n = 293, 243, 305, 258, 230, 293, 271, 265, 259, and 253. The Swiss population most at risk (50–89 y) increased from 1,632,442 to 3,333,105 persons between 1969 and 2019.

Figure 1 Number of operations divided by different types of hip arthroplasty and gender from 1969 to 2019 at 5-year intervals.
Overall, women were significantly older than men, irrespective of whether they received primary total hip arthroplasty (1,152 women and 1,017 men, median age = 70 yr. vs 66 yr., p25 = 61 yr. vs 58 yr., p75 = 77 yr. vs 73 yr., p <0.001), hemiarthroplasty (241 women and 72 men, median age = 84 yr. vs 78.5 yr., p25 = 78 yr. vs 71 yr., p75 = 89 yr. vs 85 yr., p <0.001) or total revision arthroplasty (206 women and 223 men, median age = 71 yr. vs 70 yr., p25 = 64.25 yr. vs 63 yr., p75 = 78 yr. vs 75 yr., p = 0.036).
Looking at the individual years separately, the following results are found: women were significantly older in the primary total hip arthroplasty group in 1984, 1994, 1999, 2004 and 2019; in the total revision arthroplasty group in 1989 and 1999; and in the hemiarthroplasty group in 1984, 1989 and 1994. Figure 2 shows the annual age distribution subdivided by age and type of hip arthroplasty.

Figure 2 Age of patients according to type of hip arthroplasty and gender from 1969 to 2019 at 5-year intervals.
Using linear regression, we examined the relationship between median age of patients for each year and the corresponding life expectancy of Swiss citizens as published for the year. The coefficients of correlation are calculated for subgroups (type of hip arthroplasty and gender). The best correlation was found in the group of women with primary total hip arthroplasty (r = 0.875). The linear regression relationships and correlation coefficients for the subgroups are shown in figure 3.
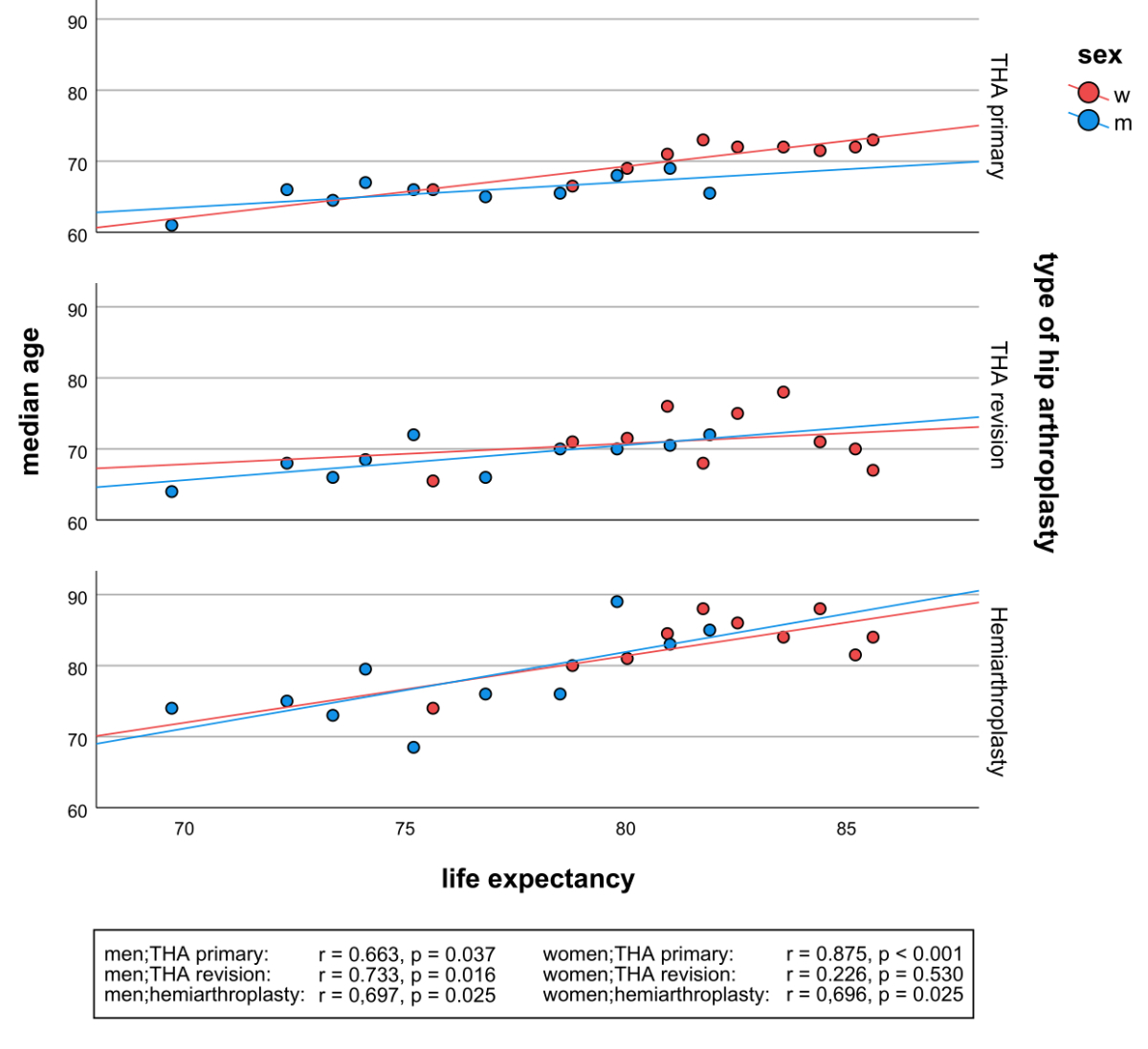
Figure 3 Linear regression relation between life expectancy of Swiss population & median age of patients included in the study according to different types of hip arthroplasty and gender from 1969 to 2019 at 5-year intervals.
No significant difference in side distribution was demonstrated in the primary total hip arthroplasty (1,073 right vs 987 left, p = 0.061), total revision arthroplasty (200 right vs 200 left, p = 1.000) and hemiarthroplasty (129 right vs 145 left, p = 0.365) groups.
Figure 4 illustrates the number of patients with artificial hip joint replacements (total, revision or hemiprostheses) operated on by high- (>50), medium- (15–50) and low-volume (1–14) surgeons per 100 from 1969 to 2019. During the period 1969–1999, fewer than 50 percent of patients were operated on by a high-volume surgeon. Today, the majority (>50%) have surgery by high-volume surgeons.

Figure 4 Number of patients with artificial hip joint replacement (total, revision, or hemiprosthesis) operated on by a high (>50), medium (15-50), and low (1-14) volume surgeon per 100 from 1969-2019 at 10-year intervals

Figure 5 Place of residence of patients with artificial hip joint replacements (total, revision, or hemiprostheses) in the Kantonsspital St.Gallen from 1969 to 2019 at 5-year intervals
The first hip prosthesis registry was started in Sweden in 1979 and older studies regarding hip prosthetics have described age and gender distribution [6, 12–14]. However, this study is the first to present the change of patient characteristics in hip arthroplasty over a period of 50 years and provides new information on surgeon caseloads per year in a single institution. As the SIRIS implant registry was only introduced in Switzerland in 2012 [15], the demographic information of this study closes information gaps.
The fact that for all types of hip arthroplasty women are older than men can partly be explained by the higher life expectancy of women. In particular, the rising median age of women with primary total hip replacements can be very well justified by the increasing life expectancy over the last 50 years (Fig. 3).
The median age of patients who received hemiprostheses is considerably higher than of patients with total hip arthroplasty (primary and revision). The reason for this is probably the predominant use of hemiarthroplasty to treat fractures in elderly patients. These figures are consistent with results published in the SIRIS implant registry [15].
Compared to 1969, patients are older for all types of prosthetic hip replacements at present (e.g., 2019). Although there is some variation with lower median age appearing in some of the years, a trend toward rising median age is evident looking at the whole period observed from 1969 to 2019. Considering the possibility of a continuing long term trend, the relevance of older age being associated with higher perioperative mortality and being a risk factor for adverse events, such as prosthesis dislocation, periprosthetic fracture, infection, arrhythmia, postoperative delirium, etc. after hip arthroplasty must be noted [16–24]. Statements and trend analyses over short periods of time are difficult and limited due to the 5-year intervals of this study. According to SIRIS, the mean age of the patients who received total arthroplasty increased by around 1 year each between the periods 2012 to 2014 and 2019 (men 66.3 yr. to 67.1 yr.; women 69.9 yr. to 70.8 yr.). The mean age in the total revision arthroplasty group (men 68.9 yr. to 70.8 yr., women 71.7 yr. to 73.5 yr.) increased by about two years, which indicates a short-term rising trend [15]. Our study shows that this trend was present before the initiation of the SIRIS registry, and that the increasing age in hip arthroplasty reflects the demographic changes. Thus, our study does not support repetitively postulated statements that the indication for prosthetic hip replacements is extended to younger age groups. Similar trends are shown in the data from Rochester, USA. Although a relatively steady increase in incidence for total hip arthroplasty was observed between 1969 and 2008 in the younger age groups (0–49, 50–59, 60–69 years), the largest overall increase in incidence was observed in the 70–79 years age group. In particular, from 2001–2004 onwards, there was a clear trend towards extending the indication for hip replacement to older age groups (especially 70–79 and 80–110-year-olds) [25].
From 1969 to 2019 significantly more primary total hip prostheses were implanted in women than in men (55.0% vs 45.0%). Considering individual years, however, the women to men ratio partly differed by several percentage points (e.g., 61.6% female proportion in 1969 vs 45.1% in 2014). More recent data from Switzerland show that the gender proportion of patients who received primary total hip arthroplasty has been relatively constant over the last few years (women 53%, men 47%). The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) has been providing comparable data since 2003 [15, 26]. No significant differences were found in the total revision arthroplasty group in any year, which is also reflected in SIRIS data with an almost balanced sex ratio [15]. Significantly fewer men than women received hemiprostheses between 1969 and 2019. With the exception of 2014, the proportion of women was always higher than 66.6%, but varied strongly above this level (e.g., 66.67% in 1969, 92.31% in 1994). This big difference is most likely attributable to the higher incidence of osteoporotic hip fractures in women [27–29].
Interestingly, the number of operations performed per year on patients aged 50–89 remains relatively constant in the range between n = 230 to 305. The Swiss population most at risk (50–89 y) increased from 1,632,442 to 3,333,105 persons, i.e. over 100%, between 1969 and 2019 [7]. The pioneering role of the Kantonsspital St. Gallen which at that time offered the new procedure of hip arthroplasty almost exclusively could be one of the reasons for the comparatively high numbers of operations in the early years (e. g., more operations were performed in 1969 than in 2019).
Our data show a tendency towards more total primary hip replacements being implanted on the right side (52.1% right, 47.9% left). However, this difference was not significant. Further non-significant differences were found for the total revision arthroplasty (49.9% right, 50.1% left) and the hemiarthroplasty group (47.1% right, 52.9% left). Data from the 2005 annual report of the “Danish Hip Alloplasty Register” show a higher proportion of hip replacements on the right in primary (53.1%) and revision (52.1%) surgeries [30].
Whereas during the period 1969–1999, fewer than 50 percent of patients were operated on by a high-volume surgeon (more than 50 replacements per year), today, the majority have surgery by high-volume surgeons. The reasons for this are probably the increasing subspecialisation of orthopaedic surgeons, especially in a central hospital. The trend in hip arthroplasty towards high-volume surgeons is also evident in the USA: a study examining the development of caseloads in hip and knee arthroplasty in the United States between 1990 and 2004 concludes that in particular the caseload of the top 5% of primary THA and TKA surgeons has increased [31].
Caseloads are a quality assurance parameter. In the canton of Zurich, for example, 15 prosthesis implantations per year are required for a surgeon to get approval for primary prostheses [32]. Patients treated by surgeons with high annual caseloads have lower mortality and lower revision rates [33, 34]. However, a prescription by law of the number of caseloads leads to competition within the hospital and the consecutive selection of surgeons. The question of how many hip surgeries a surgeon must perform to meet certain quality standards is still not clear and must be discussed further.
Regarding municipality, most patients came from the canton of St. Gallen, followed by neighbouring cantons, while other cantons and foreign countries were sparsely represented in most of the years. However, in 1969, most patients came from abroad, of which 77% were from Germany. We explain this by the close geographic location of Germany to Switzerland and the exclusive availability of hip arthroplasty at the Kantonsspital St. Gallen at that time.
Due to paper-based data, the quality of our dataset may be limited. The sample size was generally small in the total revision arthroplasty and hemiarthroplasty group. This may limit the validity of results from statistical tests. The linear regression performed does not take into account the presence of possible confounding factors such as improvement in anaesthesia. Because this is a single-centre study, the results may not be projected to the whole of Switzerland or to countries with a different population structure.
Demographic changes of patients undergoing total hip replacement reflect the overall demographic changes in the Swiss population. Over the last 50 years, the indication for prosthetic hip replacements has not been extended to younger age groups. However, the caseload in hip arthroplasty has changed over the last 50 years towards high-volume surgeons.
The authors received no specific funding for this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) . Hip, Knee & Shoulder Arthroplasty: 2021 Annual Report, Adelaide; AOA, 2021: 1-432. Available at: https://aoanjrr.sahmri.com/annual-reports-2021
2. Learmonth ID , Young C , Rorabeck C . The operation of the century: total hip replacement. Lancet. 2007 Oct;370(9597):1508–19. https://doi.org/10.1016/s0140-6736(07)60457-7 https://doi.org/10.1016/S0140-6736(07)60457-7
3. Schatzker J . Maurice Edmond Müller. His Own Words. AO Found; 2018.>
4. Weißer . Christoph. Chirurgenlexikon: 2000 Persönlichkeiten aus der Geschichte der Chirurgie. Berlin, Heidelberg, New York: Springer-Verlag; 2019. https://doi.org/10.1007/978-3-662-59238-0
5. Röder C , Staub L , Heller R . Bericht über 1. Erfassungsjahr 2012 des SIRIS Registers. 2013. Available at: https://www.spitalinfo.ch/fileadmin/documents/anq/20/20131022_Bericht_Erfassungsjahr2012_SIRIS_Registers_de_final.pdf
6. Kärrholm J . The Swedish Hip Arthroplasty Register (www.shpr.se). Acta Orthop. 2010 Feb;81(1):3–4. https://doi.org/10.3109/17453671003635918
7. Bevölkerung | Bundesamt für Statistik [Internet]. [cited 2021 Dec 21]. Available at: https://www.bfs.admin.ch/bfs/de/home/statistiken/bevoelkerung.html
8. AHV-Nummer . Infos zur neuen AHV-Nummer und zur alten AHVNummer [Internet]. [cited 2021 Dec 22]. Available at: https://www.ahvnummer.ch/aufbau-alt.htm
9. SPSS Statistics - Schweiz | IBM [Internet]. [cited 2021 Dec 22]. Available at: https://www.ibm.com/ch-de/products/spss-statistics
10. Microsoft . Microsoft Excel, Tabellenkalkulationssoftware | Microsoft 365 [Internet]. [cited 2021 Dec 22]. Available at: https://www.microsoft.com/de-ch/microsoft-365/excel
11. GIMP - GNU Image Manipulation Program [Internet]. [cited 2021 Dec 23]. Available at: https://static.gimp.org/
12. Kaplan, C. J. Posterior approach to the hip joint in prosthetic replacement. South African Medical Journal, 1961, 35. Jg., Nr. 22, S. 441-444.
13. Charnley, J. O. H. N. ; Follacci, F. M. ; Hammond, B. T. The long-term reaction of bone to self-curing acrylic cement. The Journal of Bone and Joint Surgery. British volume, 1968, 50. Jg., Nr. 4, S. 822-829. Available at: https://doi.org/https://doi.org/10.1302/0301-620X.50B4.822.
14. Morscher EW , Dick W , Kernen V . Cementless fixation of polyethylene acetabular component in total hip arthroplasty. Arch Orthop Trauma Surg (1978). 1982;99(4):223-230. Available at: https://doi.org/https://doi.org/10.1007/bf00381397. https://doi.org/10.1007/BF00381397
15. Zdravkovic V , Beck M , Brand C , Christen B. Swiss National Hip & Knee Joint Registry - Report 2020 - Annual Report of the SIRIS Registry, Hip & Knee, 2012 – 2019. 2020.
16. Koenig K , Huddleston JI 3rd , Huddleston H , Maloney WJ , Goodman SB . Advanced age and comorbidity increase the risk for adverse events after revision total hip arthroplasty. J Arthroplasty. 2012 Aug;27(7):1402–1407.e1. https://doi.org/10.1016/j.arth.2011.11.013
17. Huddleston JI , Wang Y , Uquillas C , Herndon JH , Maloney WJ . Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012 Feb;470(2):490–6. https://doi.org/10.1007/s11999-011-1967-y
18. Ogino D , Kawaji H , Konttinen L , Lehto M , Rantanen P , Malmivaara A , et al. Total hip replacement in patients eighty years of age and older. J Bone Joint Surg Am. 2008 Sep;90(9):1884–90. https://doi.org/10.2106/jbjs.g.00147 https://doi.org/10.2106/JBJS.G.00147
19. Murphy BP , Dowsey MM , Choong PF . The Impact of Advanced Age on the Outcomes of Primary Total Hip and Knee Arthroplasty for Osteoarthritis: A Systematic Review. JBJS Rev. 2018 Feb;6(2):e6. https://doi.org/10.2106/jbjs.rvw.17.00077 https://doi.org/10.2106/JBJS.RVW.17.00077
20. Fang M , Noiseux N , Linson E , Cram P . The Effect of Advancing Age on Total Joint Replacement Outcomes. Geriatr Orthop Surg Rehabil. 2015 Sep;6(3):173–9. https://doi.org/10.1177/2151458515583515
21. Ezquerra-Herrando L , Seral-García B , Quilez MP , Pérez MA , Albareda-Albareda J . Instability of total hip replacement: A clinical study and determination of its risk factors. Rev Esp Cir Ortop Traumatol. 2015;59(4):287–94. https://doi.org/10.1016/j.recot.2014.12.004 https://doi.org/10.1016/j.recote.2015.04.010
22. Karachalios T , Komnos G , Koutalos A. Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev. 2018;3(5):232-239. Published 2018 May 21. Available at: https://doi.org/https://doi.org/10.1302/2058-5241.3.170068.
23. Bovonratwet P , Malpani R , Ottesen TD , Tyagi V , Ondeck NT , Rubin LE , et al. Aseptic revision total hip arthroplasty in the elderly : quantifying the risks for patients over 80 years old. Bone Joint J. 2018 Feb;100-B(2):143–51. https://doi.org/10.1302/0301-620x.100b2.bjj-2017-0895.r1 https://doi.org/10.1302/0301-620X.100B2.BJJ-2017-0895.R1
24. Xiao QX , Liu Q , Deng R , Gao ZW , Zhang Y . Postoperative cognitive dysfunction in elderly patients undergoing hip arthroplasty. Psychogeriatrics. 2020 Jul;20(4):501–9. https://doi.org/10.1111/psyg.12516
25. Singh JA , Vessely MB , Harmsen WS , Schleck CD , Melton LJ 3rd , Kurland RL , et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969-2008. Mayo Clin Proc. 2010 Oct;85(10):898–904. https://doi.org/10.4065/mcp.2010.0115
26. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) . Revision of Hip and Knee Arthroplasty: Supplementary Report in Hip, Knee & Shoulder Arthroplasty: 2021 Annual Report, AOA, Adelaide; 2021: 1-25.
27. Mazzucchelli Esteban R , Pérez-Fernández E , Crespí-Villarías N , et al. Trends in osteoporotic hip fracture epidemiology over a 17-year period in a Spanish population: Alcorcón 1999. Arch Osteoporos. 2017;12(1):84. Published. 2015;2017(Sep):27. https://doi.org/10.1007/s11657-017-0376-6
28. Guzon-Illescas O , Perez Fernandez E , Crespí Villarias N , et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14(1):203. Published 2019 Jul 4. Available at: https://doi.org/https://doi.org/10.1186/s13018-019-1226-6.
29. Brauer CA , Coca-Perraillon M , Cutler DM , Rosen AB . Incidence and mortality of hip fractures in the United States. JAMA. 2009 Oct;302(14):1573–9. https://doi.org/10.1001/jama.2009.1462
30. The Danish Hip Arthroplasty Register (DHR), National Annual Report . 2005.
31. Kurtz SM , Ong KL , Schmier J , Zhao K , Mowat F , Lau E . Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009 Feb;24(2):195–203. https://doi.org/10.1016/j.arth.2007.11.015
32. Kanton Zürich G . Weitergehende leistungsspezifische Anforderungen und Erläuterungen Akutsomatik (Version 2020.1; gültig ab 1. Januar 2020). 2020 [cited 2022 Mar 6]; Available from: www.smob.ch/guide_lines/RichtlinienzurBehandlungvonUebergewichtderSMOB.9.11.2010x.pdf
33. Katz JN , Losina E , Barrett J , Phillips CB , Mahomed NN , Lew RA , et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001 Nov;83(11):1622–9. https://doi.org/10.2106/00004623-200111000-00002
34. Losina E , Barrett J , Mahomed NN , Baron JA , Katz JN . Early failures of total hip replacement: effect of surgeon volume. Arthritis Rheum. 2004 Apr;50(4):1338–43. https://doi.org/10.1002/art.20148