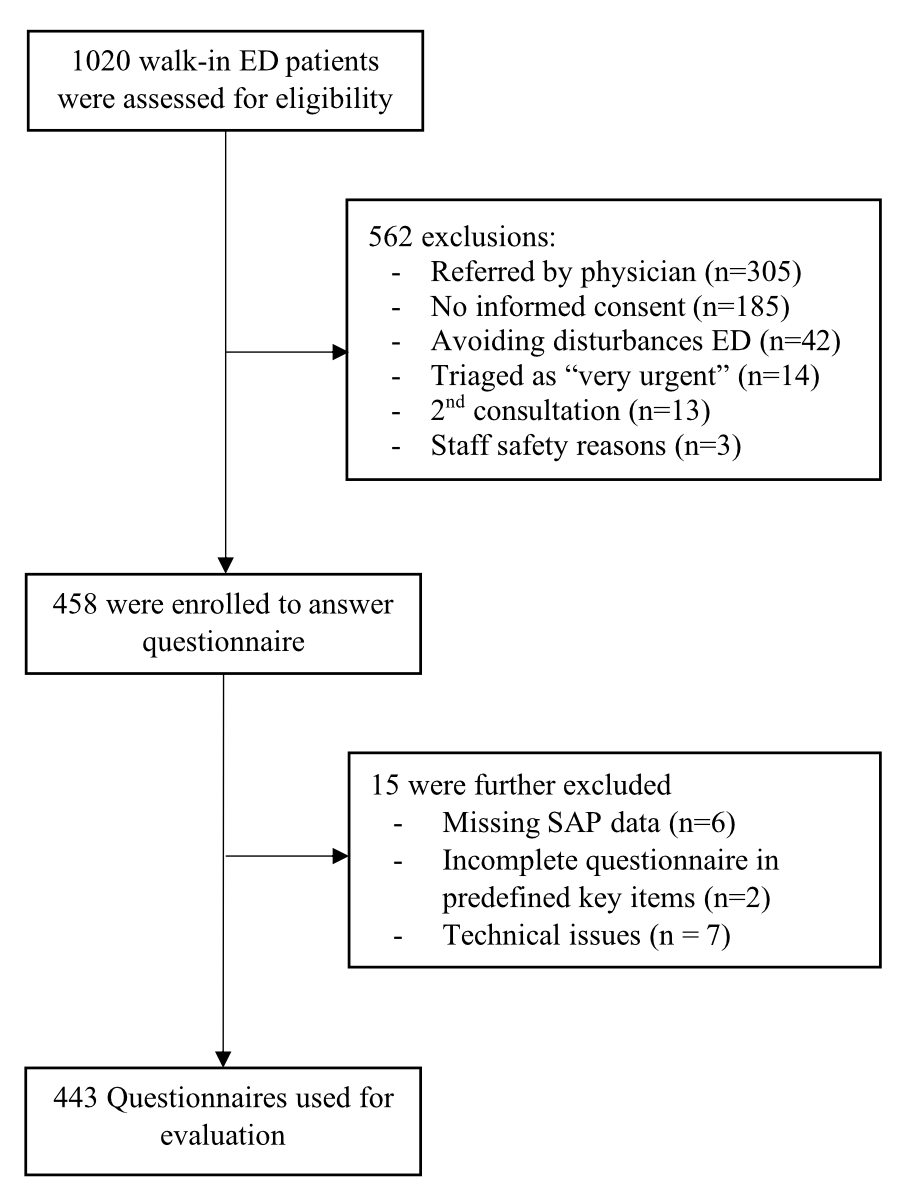
Figure 1 Flowchart of the study.
DOI: https://doi.org/10.57187/smw.2023.40027
Medical care for patients who are not physically present [1] gained worldwide importance during the pandemic [2] when face-to-face consultations have been avoided [3]. In Switzerland, a decrease in emergency department (ED) consultations of 24.9% to 42.5% was noted during the first months of 2020 compared with 2019 [4]. The demand for telehealth services increased significantly at the beginning of the pandemic [5]. Virtual telehealth platforms were successfully and quickly built and scaled up, for example in New York, where 17,000 patients, 50% of whom planned an ED visit for their mostly COVID-19-related symptoms, used a platform prior to their consultation. Only 2.5% of these needed physical consultations in the ED [6]. In Switzerland, various telehealth applications were used in the COVID-19 context: machine learning was successfully used to develop a COVID-19 severity assessment tool (COSA) [7]; online forward triage tools were used to decide whether testing for SARS-CoV-2 is indicated [8], or whether children were allowed to go to school or day care [9,10]. Telehealth was used for triage and follow-up of patients with suspected or confirmed COVID-19 [11,12]. As of 2022, 72% of the members of The New England Journal of Medicine Catalyst Insights Council stated that telehealth had improved or greatly improved patient health in their organisation [1]. Telehealth has become mainstream in care delivery.
It is, however, unclear how COVID-19 has changed the frequency of telehealth use, and also how telehealth is used before ED consultation in Switzerland. We aimed to investigate (i) the frequency and parameters of telehealth use among patients at the emergency department of a Swiss University (ED) two years into the pandemic, and (ii) to compare the results with a sample before the pandemic [13], in order to gain insights into the changes in telehealth use. Furthermore, we (iii) explored the influence of the COVID-19 pandemic on the use of and attitude to telehealth, as reported by the patients.
A consecutive convenience sample of Emergency Department (ED) patients was obtained in 30 shifts from 8–29 July 2021. Patients consulting the ED were consecutively screened and included according to the criteria below. Within this period, the government had already started lifting COVID-19 restrictions. Public events were allowed, with a limit of 100 people indoors and 300 people outdoors. For private gatherings, the limits were 30 and 50 people, respectively. Restaurants were again allowed to serve guests indoors, but specific restrictions still applied. Working from home was regarded as a recommendation rather than requirement for businesses that carried out weekly testing. Amateur sports and cultural activities were opened and vaccinated or recovered persons no longer had to quarantine [14].
A survey obtained from October to December 2019 was used as a pre-pandemic comparison [13] and will be called the “baseline survey” throughout the article. To ensure comparability, the study design of the baseline study was adopted for the update study. Most of the questions remained unchanged, and questions regarding COVID-19 were added. This 2021 update is designated as the “COVIDsurvey”. “COVID-19” is used as term for the disease or the pandemic whenever it is not related to either of the surveys. Both surveys were conducted in the same ED setting in Bern University Hospital (Inselspital), where around 50,000 patients are treated per year [15]. The same inclusion and exclusion criteria were used and data collection was supervised by the same survey team. As there was no difference in telehealth use during night shifts vs day shifts in the baseline survey [13], we decided to conduct the COVID survey during daytime only. Patients were included if they were able to give informed consent and had chosen to consult the ED by themselves. More details on the inclusion and exclusion criteria are presented in figure 1. A sample size of 308 patients in each group was calculated to be sufficient to detect a 10% increase in telehealth use, with an alpha error of 0.05 and power of 0.8. Thus, we decided to aim for at least 417 valid questionnaires, as in the baseline survey.
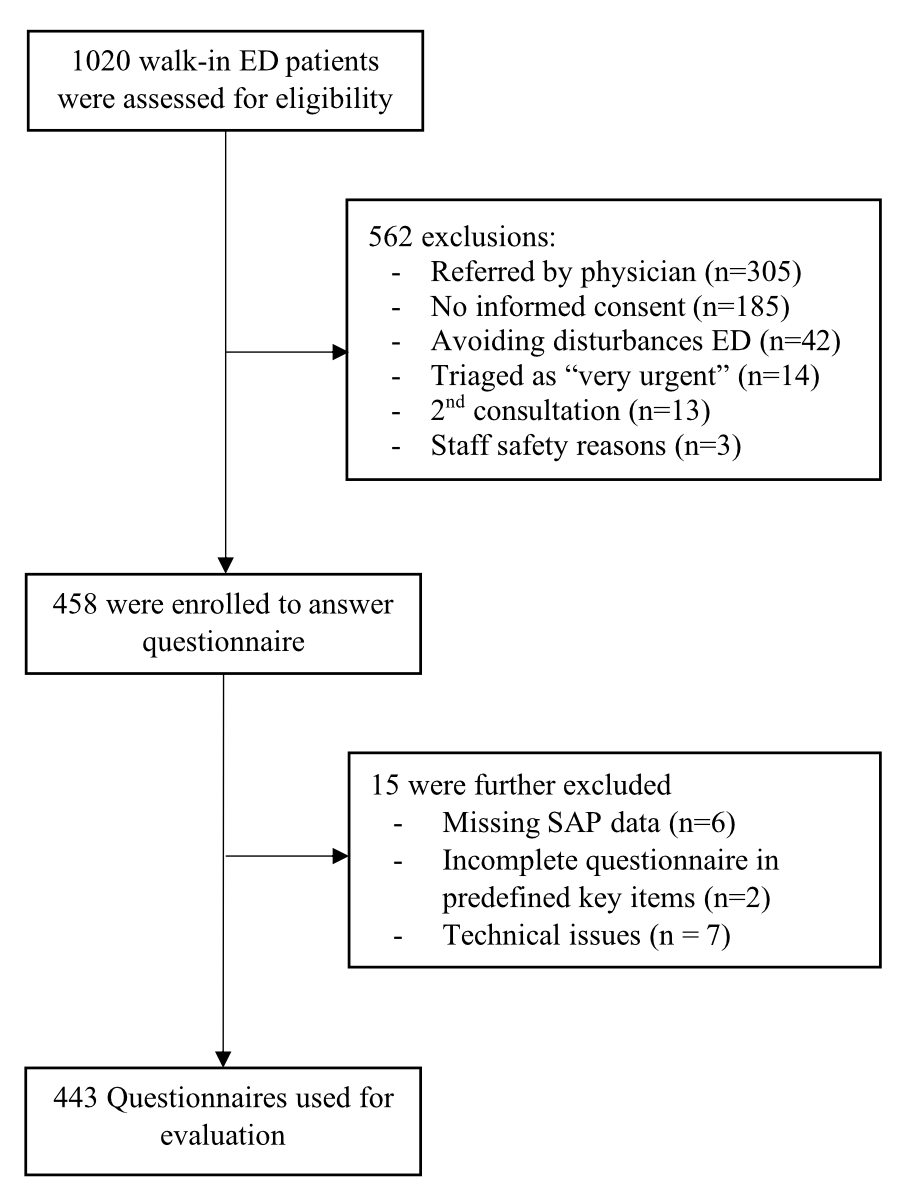
Figure 1 Flowchart of the study.
The study was a repeated cross-sectional study with prospective data collection among the adult walk-in population of a tertiary care ED in Switzerland. The study team involved in the patient survey consisted of one medical student (EA) and one medical doctor (LP), who were instructed and supervised by senior researchers (AM/TCS). LP, AM and TCS were also involved in the baseline survey, to assure consistency in data collection. More details on data collection are provided in the publication of the baseline survey [13].
Trained nurses made a triage at ED presentation according to the Swiss Emergency Triage Scale [16]. Patient and consultation characteristics were extracted from the electronic patient records.
Definition of the term “telehealth”: For our surveys, we defined telehealth as the use of any kind of remote communication technology by the patient prior to ED presentation. This is based on the definition by the US National Institutes of Health (NIH) [17]. In this definition, we included telephone calls to health professionals and to relatives, as well as internet searches by the patient and the use of health applications.
Primary outcome: The primary outcome was the difference in frequency of telehealth use between the two surveys.
Secondary outcomes: Secondary outcomes were characteristics of telehealth users and comparison of users versus non-users in the COVID survey, influence of the pandemic on telehealth use reported by the patients, and comparison of baseline and COVID survey data. The survey questions can be found in the appendix.
Statistical analysis was performed in the same way for the two surveys [13]. For data analysis, we used Stata® MP 16 (StataCorp, The College Station, Texas, USA). We present descriptive analysis of categorical variables as absolute numbers and percentages. The distribution of the continuous variable “age” was described with median and interquartile range (IQR), as this variable was not normally distributed. We compared categorical variables with the chi-square test, age distributions with the Wilcoxon rank sum tests. A p-value <0.05 was considered significant, 0.05 <p <0.1 a trend.
Our study is registered with the Ethics Committee of Canton Bern, Switzerland (Req 2019-00635). Consent was obtained from each patient. No patient treatment was delayed or otherwise affected by the study.
During the study period, 1020 ED walk-in patients were screened for eligibility. A breakdown of the reasons for exclusion (n = 577) is presented in the study flowchart (fig. 1).
A total of 443 patients were included in our study and their complete questionnaires were evaluated. Baseline characteristics of all COVID survey participants are presented in table 1.
Table 1Baseline characteristics of COVID survey participants.
| COVID survey patients | |
| Demographic data, n (%) | 443 (100) |
| Age (years), median (IQR) | 43 (30–60) |
| Gender female, n (%) | 226 (51.0) |
| Education, n (%) | 441 (100) |
| Tertiary | 147 (33.3) |
| Secondary | 223 (50.6) |
| Obligatory | 65 (14.7) |
| No formal education | 6 (1.4) |
| Language, n (%) | 437 (100) |
| German | 395 (90.4) |
| French | 15 (3.4) |
| Italian | 6 (1.4) |
| English | 9 (2.1) |
| Other | 12 (2.8) |
| Triage urgency, n (%) | 443 (100) |
| Urgent conditions | 90 (20.3) |
| Semi-urgent | 322 (72.7) |
| Non urgent | 31 (7.0) |
IQR: interquartile range
The results of the baseline survey have already been published [13] and are therefore not described in detail. Tables 2 and 3 present a comparison of patients with and without telehealth use in the COVID survey and patient perspectives on how telehealth use has changed during the pandemic. To give an impression of how telehealth use changed over time, table 4 gives an overview of changes in perceived usefulness and adherence to recommendations. There was no difference between the groups of patients in the baseline survey and those in the COVID survey with respect to age (p = 0.623), gender (p = 0.199) or triage category (p = 0.455).
In the COVID survey, we found a 6.4% increase in telehealth use, as 50.3% of the patients (n = 223) had used telehealth prior to ED consultation, compared to 43.9% (n = 183) in the baseline survey (p = 0.058).
The COVID survey revealed that 54.9% (n = 124) of all women and 45.6% (n = 99) of all men used telehealth (p = 0.052). No significant differences regarding age or education were demonstrated (table 2). The most commonly used telehealth service was a telephone call to the treating physician (31.1%, n = 69) and other physicians (19.8%, n = 44). Overall, 28.8% (n = 64) of patients employed internet search and 16.7% (n = 37) patients called a telehealth provider. No patient used a health application or a symptom checker. In our sample, 16.6% (n = 37) patients were obliged to use telehealth by their insurance policy, compared with 7.7% (n = 14) in 2019.
Table 2Comparison of patients with and without telehealth use in COVID survey.
| All patients | Telehealth used | Telehealth not used | p -value | |
| Demographic data | 443 (100) | 223 (50.3) | 220 (49.7) | |
| Age (years), median (IQR) | 43 (30–60) | 41 (30–59) | 46 (30–61) | 0.347 |
| Gender female, n (%) | 226 (51.1) | 124 (54.9) | 102 (45.1) | 0.052 |
| Education, n (%) | 441 (100) | 221 (50.1) | 220 (49.9) | 0.512 |
| Tertiary | 147 (33.3) | 81 (55.1) | 66 (44.9) | |
| Secondary | 223 (50.6) | 105 (47.1) | 118 (52.9) | |
| Obligatory | 65 (14.7) | 32 (49.2) | 33 (50.8) | |
| No formal education | 6 (1.4) | 3 (50) | 3 (50) | |
| Trauma, n (%) | 102 (23.0) | 35 (34.3) | 67 (65.7) | <0.001 |
| Hospital admission, n (%) | 64 (14.5) | 38 (59.4) | 26 (40.6) | 0.174 |
IQR: interquartile range
In the COVID survey, 12.2% (n = 54) used telehealth for the first time during the current pandemic; 18.3% (n = 80) stated that their attitude towards telehealth had become more positive since the pandemic and 2.3% (n = 10) developed a more negative opinion. The percentage of patients who used telehealth for the first time during the pandemic depended significantly on their levels of education (p = 0.016). Patients with only obligatory schooling or no formal education reported their first telehealth use during the pandemic in 20.0% (n = 13) and 33.3% (n = 2) of cases, respectively. However, 24.6% of patients (n = 16) with only obligatory schooling and 60% of patients (n = 3) with no formal education reported that they would not continue to use telehealth after the pandemic, compared with 6.8% (n = 10) of patients with tertiary education and 19.8% (n = 44) of patients with secondary education. Of the retired patients, 32.1% (n = 26) stated that they would not use telehealth after the pandemic, compared with 8% to 12% of the employed, self-employed, homemakers, and students.
Table 3Influence of the COVID–19 pandemic on telehealth use. First use during pandemic n = 442, plan to use after pandemic n = 440.
| All patients | Age 18 – 24 | Age 25 – 44 | Age 45 – 64 | Age >64 | p-value | |
| First use of telehealth during pandemic, n (%) | 54 (12.2) | 6 (11.1) | 25 (46.3) | 10 (18.5) | 13 (24.1) | 0.232 |
| Change in opinion during pandemic, n (%) | 438 (100) | 62 (14.2) | 167 (38.1) | 125 (28.5) | 84 (19.2) | 0.247 |
| – Positive | 80 (18.3) | 9 (11.3) | 39 (48.8) | 20 (25.0) | 12 (15.0) | |
| – Negative | 10 (2.3) | 3 (30.0) | 4 (40.0) | 1 (10.0) | 2 (20.0) | |
| – No change | 348 (79.5) | 50 (14.4) | 124 (35.6) | 104 (29.9) | 70 (20.1) | |
| Plan to use after pandemic, n (%) | 367 (83.4) | 54 (14.7) | 149 (40.6) | 97 (26.4) | 67 (18.3) | 0.040 |
Perceived usefulness of telehealth was significantly increased in the COVID survey compared with the baseline survey (very useful 69.1%, n = 154 vs 44.0%, n = 80; p <0.001). For further details, see table 4. There was a significant increase in adherence to the telehealth recommendation with respect to urgency of treatment, from 78.0% (n = 131) to 90.4% (n = 150), p = 0.002 (table 4). Significantly more patients were obliged by the insurance to use telehealth (16.6% COVID survey vs 7.7% baseline survey; p = 0.007).
Table 4Comparison of baseline and COVID survey data. Usefulness of telehealth n = 405, Adherence to recommendation n = 333 For this table, data from the published baseline survey were included.
| All patients | Baseline | COVID survey | p-value | |
| Telehealth used, n (%) | 406 (47.2) | 183 (43.9) | 223 (50.3) | 0.058 |
| Usefulness of telehealth, n (%) | 405 (100) | 182 (100) | 223 (100) | <0.001 |
| – 0 (not useful at all) | 16 (4.0) | 12 (6.6) | 4 (1.8) | |
| – 1 | 8 (2.0) | 8 (4.4) | 0 | |
| – 2 | 24 (5.9) | 14 (7.7) | 10 (4.5) | |
| – 3 | 47 (11.6) | 29 (15.9) | 18 (8.1) | |
| – 4 | 76 (18.8) | 39 (21.4) | 37 (16.6) | |
| – 5 (very useful) | 234 (57.8) | 80 (44.0) | 154 (69.1) | |
| Adhered to recommendation, n (%) | 280 (84.1) | 131 (78.0) | 149 (90.3) | 0.002 |
The results demonstrated a trend to an increase in telehealth use; 6.4% more patients used telehealth compared with the baseline survey (p = 0.058), with a predominant increase in female users. There is evidence from pre-pandemic times that shows more telehealth use by men [18], also demonstrated in our baseline survey. In contrast to this, women expressed greater satisfaction with telehealth use [19] during the pandemic. It might be speculated that woman relied more heavily on telehealth, as they had to perform more housework and childcare during the pandemic, as a result of school closures and lockdowns. The complex effects and correlations between COVID-19 measures and their effects on family structure were demonstrated in another study [20]. Adherence to telehealth recommendations and perceived usefulness increased in the COVID survey. This might be partly because patients sometimes had no choice as to whether or not to adhere to the regulations of the COVID-19 Act [21] or due to reduced access to healthcare. A lack of basic requirements for participation in digitised everyday life [22], as well as insufficient infrastructure, are barriers to telehealth use, as has been described [23]. It has been reported that socioeconomic and age-related differences remain important even in the context of COVID-19 [24]. In the COVID survey, retired patients and those with low levels of education stated that they used telehealth during the pandemic for the first time and that they were satisfied with the recommendations. In contrast, however, these patients indicated they would stop using telehealth once COVID-19 was no longer relevant. Socioeconomic impacts on telehealth use were further explored in a qualitative evaluation [20]. The increase in telehealth use in a setting of low resources might also be caused by insurance models with mandatory telehealth use, as these are less expensive than the traditional models.
For the group of retired patients, it can be assumed that their use of telehealth during COVID-19 is related to their desire for risk reduction through less exposure, and therefore they may want to return to their original usage subsequently. Typical advantages of telehealth treatment, such as time- and location-independent therapy, may not be as relevant for retired people as for other population groups. Qualitative evaluations are necessary to further evaluate these findings. Effort is needed to make digital advantages accessible to everyone.
The main strength of this study is that we had the opportunity to compare telehealth use among the ED population before and during the COVID-19 pandemic, as the prior assessment dates were from December 2019 and were performed before the first COVID-19 case in Switzerland had been detected.
To ensure comparability, the COVID survey was conducted similarly to the baseline survey, so that strengths and limitations are similar. The study team filled out the questionnaires together with the patients, so that there were few dropouts or insufficiently answered questionnaires. On the other hand, this is also a potential source of bias if patients want to provide convenient or desired responses for the investigator, especially in the self-reported section for telehealth triage category. The multiple-choice character questions cannot fully represent everything the patients might be interested in telling us about their experiences and further qualitative studies are necessary, for example to explore the reasons for non-use of telehealth. Patients who consulted a telehealth service and found adequate treatment for their complaints are not represented. However, the aim of our study was to provide an overview of change in telehealth use in the ED population due to COVID-19. Again, our study includes only walk-in patients, thus leading to a selection bias. The median age of our population was similar to that of walk-in patients elsewhere [25]. External validity of this study is limited as it is a single-centre study conducted in one region of Switzerland only. Excluding some patients due to language barriers might have introduced a bias in our study sample. Our definition of telehealth including telephone calls is very broad. For future investigations it might be favourable to use a more precise wording. Our first question to the patients was whether they did or not use telehealth. For future research, we might ask initially “What type of telehealth do you use?”. This could help to ensure that we do not miss any use-cases.
Although COVID-19 has increased telehealth use in many populations worldwide we could only find a trend to increased use by Swiss emergency department patients. First-time users of telehealth were predominantly less educated, and inclusion of these user groups may not be sustainable, as was indicated by the patients. COVID-19 led to greater adherence to telehealth recommendations and higher perceived usefulness. When offering telehealth, the needs of all patient groups must be considered, in order to ensure that telehealth provides the greatest benefit with lower barriers to use. Further research is needed to evaluate whether and how patients who do not present to the ER use telehealth.
Triage nurses and administrative staff of our ED front desk contributed significantly to the study by providing workspace and friendly support for the study team.
No external funding
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed. TCS holds an endowed professorship for emergency telemedicine at the University of Bern, funded by the Touring Club of Switzerland. The funder had no influence on the focus of research in emergency telemedicine in general or specifically on the decision to publish or on the content of the present manuscript.
1. Hollander J, Sharma R. Telemedicine Is Mainstream Care Delivery. NEJM Catalyst 2022;3:CAT.22.0176. https://doi.org/10.1056/CAT.22.0176
2. Xu S, Glenn S, Sy L, Qian L, Hong V, Ryan DS, et al. Impact of the COVID-19 Pandemic on Health Care Utilization in a Large Integrated Health Care System: Retrospective Cohort Study. J Med Internet Res. 2021 Apr;23(4):e26558. https://doi.org/10.2196/26558
3. Dudevich A, Frood J. Impact of the COVID-19 Pandemic on Health System Use in Canada. Healthc Q. 2021 Jul;24(2):12–4. https://doi.org/10.12927/hcq.2021.26552
4. Hautz WE, Sauter TC, Exadakytlos AK, Krummrey G, Schauber S, Müller M. Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality – a retrospective study from a Swiss university hospital. Swiss Med Wkly. 2020 Aug;150(3334):w20331. https://doi.org/10.4414/smw.2020.20331
5. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020 Jun;27(6):957–62. https://doi.org/10.1093/jamia/ocaa067
6. Koziatek CA, Rubin A, Lakdawala V, Lee DC, Swartz J, Auld E, et al. Assessing the Impact of a Rapidly Scaled Virtual Urgent Care in New York City During the COVID-19 Pandemic. J Emerg Med. 2020 Oct;59(4):610–8. https://doi.org/10.1016/j.jemermed.2020.06.041
7. Schöning V, Liakoni E, Baumgartner C, Exadaktylos AK, Hautz WE, Atkinson A, et al. Development and validation of a prognostic COVID-19 severity assessment (COSA) score and machine learning models for patient triage at a tertiary hospital. J Transl Med. 2021 Feb;19(1):56. https://doi.org/10.1186/s12967-021-02720-w
8. Hautz WE, Exadaktylos A, Sauter TC. Online forward triage during the COVID-19 outbreak. Emerg Med J. 2021 Feb;38(2):106–8. https://doi.org/10.1136/emermed-2020-209792
9. Starvaggi C, Travaglini N, Aebi C, Romano F, Steiner I, Sauter TC, et al. www.coronabambini.ch: Development and usage of an online decision support tool for pediatric COVID-testing in Switzerland. JMIR Preprints. 25/02/2022:37538.
10. Michel J, Mettler A, Starvaggi C, Travaglini N, Aebi C, Keitel K, et al. The Utility of a Pediatric COVID-19 Online Forward Triage Tool in Switzerland. Front Public Health. 2022 Jul;10:902072. https://doi.org/10.3389/fpubh.2022.902072
11. Lin CH, Tseng WP, Wu JL, Tay J, Cheng MT, Ong HN, et al. A Double Triage and Telemedicine Protocol to Optimize Infection Control in an Emergency Department in Taiwan During the COVID-19 Pandemic: Retrospective Feasibility Study. J Med Internet Res. 2020 Jun;22(6):e20586. https://doi.org/10.2196/20586
12. Percheron Vendeuvre L, Lecygne C, Jeannot JG, Spahni S, Mazouri-Karker S. [Telemedicine in the era of COVID-19: a revolution? The experience of the University Hospitals of Geneva]. Rev Med Suisse. 2020 Sep;16(706):1695–8. https://doi.org/10.53738/REVMED.2020.16.706.1695
13. Mettler AC, Piazza L, Michel J, Müller M, Exadaktylos AK, Hautz WE, et al. Use of telehealth and outcomes before a visit to the emergency department: a cross-sectional study on walk-in patients in Switzerland. Swiss Med Wkly. 2021 Jul;151(2930):w20543. https://doi.org/10.4414/smw.2021.20543
14. Coronavirus: Fourth round of lifting restrictions from Monday goes further than originally planned. https://www.admin.ch/gov/en/start/documentation/media-releases.msg-id-83697.html
15. Bern IG. 3010. Zahlen und Fakten. http://www.notfallzentrum.insel.ch/de/ueber-uns/ueber-die-klinik/zahlen-und-fakten/
16. Rutschmann OT, et al. Reliability of the revised Swiss Emergency Triage Scale: a computer simulation study. Eur J Emerg Med. 2018 Aug;25(4):264–9. https://doi.org/10.1097/MEJ.0000000000000449
17. Telehealth. National Institutes of Health. https://www.nibib.nih.gov/science-education/science-topics/telehealth
18. Khatun F, Heywood AE, Hanifi SM, Rahman MS, Ray PK, Liaw ST, et al. Gender differentials in readiness and use of mHealth services in a rural area of Bangladesh. BMC Health Serv Res. 2017 Aug;17(1):573. https://doi.org/10.1186/s12913-017-2523-6
19. Dopelt K, Avni N, Haimov-Sadikov Y, Golan I, Davidovitch N. Telemedicine and eHealth Literacy in the Era of COVID-19: A Cross-Sectional Study in a Peripheral Clinic in Israel. Int J Environ Res Public Health. 2021 Sep;18(18):9556. https://doi.org/10.3390/ijerph18189556
20. Michel J, Mettler A, Müller M, Hautz WE, Sauter TC. A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study. Int J Environ Res Public Health. 2022 Apr;19(9):5184. https://doi.org/10.3390/ijerph19095184
21. Federal Act on the Statutory Principles for Federal Council Ordinances on Combating the COVID-19 Epidemic. 818.102 (2020).
22. Kazevman G, Mercado M, Hulme J, Somers A. Prescribing Phones to Address Health Equity Needs in the COVID-19 Era: the PHONE-CONNECT Program. J Med Internet Res. 2021 Apr;23(4):e23914. https://doi.org/10.2196/23914
23. Alvarez-Risco A, Del-Aguila-Arcentales S, Yáñez JA. Telemedicine in Peru as a Result of the COVID-19 Pandemic: Perspective from a Country with Limited Internet Access. Am J Trop Med Hyg. 2021 May;105(1):6–11. https://doi.org/10.4269/ajtmh.21-0255
24. Weber E, Miller SJ, Astha V, Janevic T, Benn E. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020 Dec;27(12):1949–54. https://doi.org/10.1093/jamia/ocaa216
25. Hysenbegasi M, Hubloue I, Vanobberghen R, Kartounian J, Devroey D. Evolution over 11 years of the characteristics of walk-in patients at the emergency department of a university hospital in Brussels. J Med Life. 2019;12(1):34–42. https://doi.org/10.25122/jml-2018-0053
The appendix is available for download as a separate PDF file in the online version of this article (https://doi.org/10.57187/smw.2023.40027).