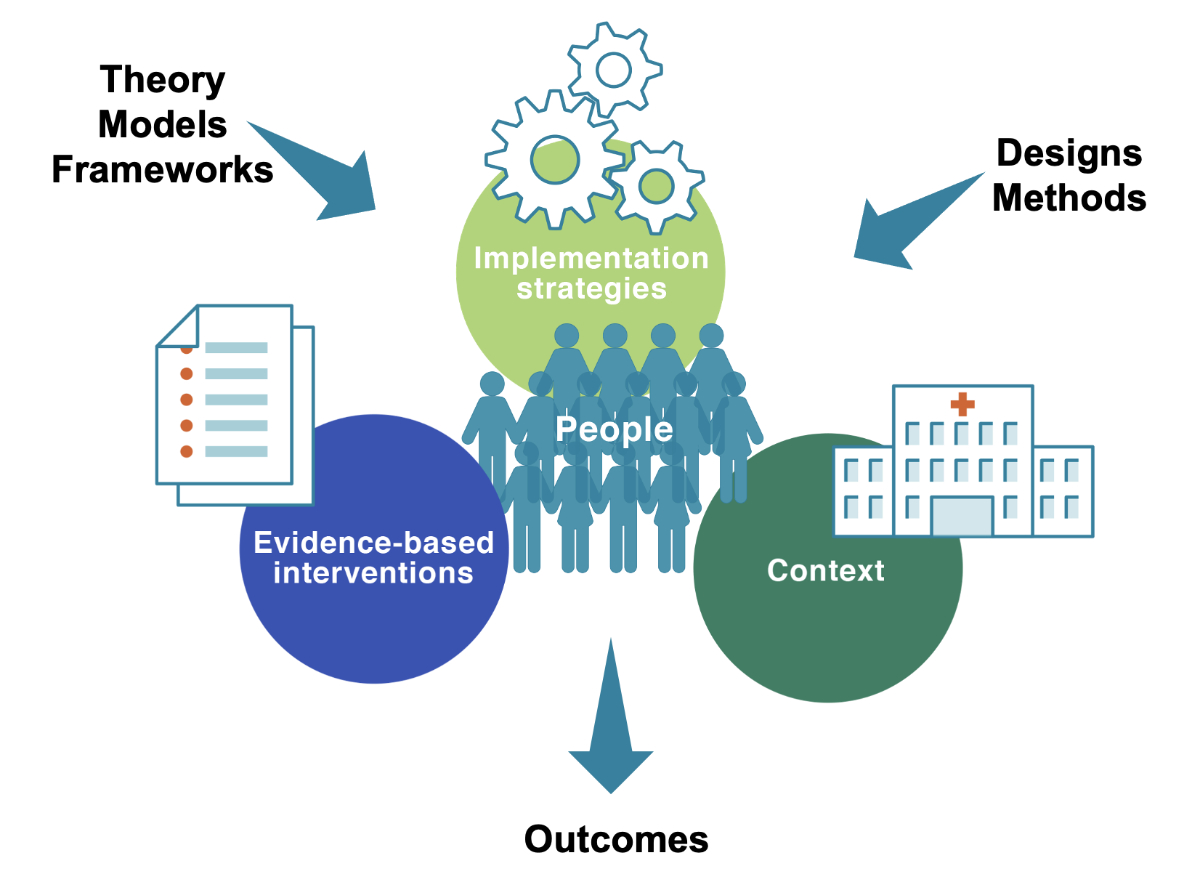
Figure 1 Core elements in implementation science.
DOI: https://doi.org/10.57187/smw.2022.40021
Despite continuous efforts to promote the use of research findings in routine healthcare, progress usually takes a long time. Currently, evidence reaches the practice of physicians, nurses, or allied health practitioners with a time lag of up to 15 years [1], preventing patients and the public from receiving the best possible care.
As a response to this problem, the discipline of implementation science has emerged, both internationally and in Switzerland. Implementation science is the scientific study of methods to enable the systematic integration of research findings and evidence-based practices into care delivery – and the de-integration of low-value care [2]. Implementation science represents a distinct scientific discipline dedicated to finding solutions for narrowing the "know-do" gap in healthcare, decreasing the 15-year lag problem, and improving services for the benefit of patients and their families. In particular, implementation science enables the explanation of clinical interventions’ effectiveness, or lack thereof, and examines their applicability in real-world settings.
Developing implementation science into a strong research discipline is particularly promising in the context of the Swiss health system. Switzerland is a multi-lingual, multi-cultural country with a highly decentralised political structure. Institutions at the federal, cantonal, and municipal levels share responsibilities for planning, delivering, and financing healthcare services while operating under the influence of direct democracy [3]. Switzerland's 26 cantons have considerable power when designing and delivering healthcare services, leading to variations in how services are prioritised, implemented, and sustained. Furthermore, the principle of subsidiarity – stipulating that policy issues be managed at the lowest possible level of government – leads to considerable involvement of non-governmental actors in delivering healthcare services [4].
The consequences of this complex system for delivering healthcare services include difficulties in implementing effective interventions [5] and de-implementing low-value care [6], steadily growing healthcare costs [7], and challenges in removing persistent healthcare disparities [8]. In 2021, these problems contributed to the formation of the Swiss Federal Quality Commission (FQC) aimed at improving the quality of Swiss healthcare, with a focus on better integrating the patient perspective.
Building on cyclical and participatory principles, implementation science is well suited for this complex Swiss system. In collaboration with healthcare professionals, implementation science supports the translation of knowledge generated in science into concrete improvements in practice. Further strengthening the translational research cycle, implementation science also inspires novel scientific investigations based on the insights gained at the intersection of research and practice. Implementation science draws from a rich theoretical foundation for understanding, designing, and evaluating complex implementation processes and their multilevel contextual interactions. Studying implementation in routine healthcare settings focuses on four core elements (figure 1):
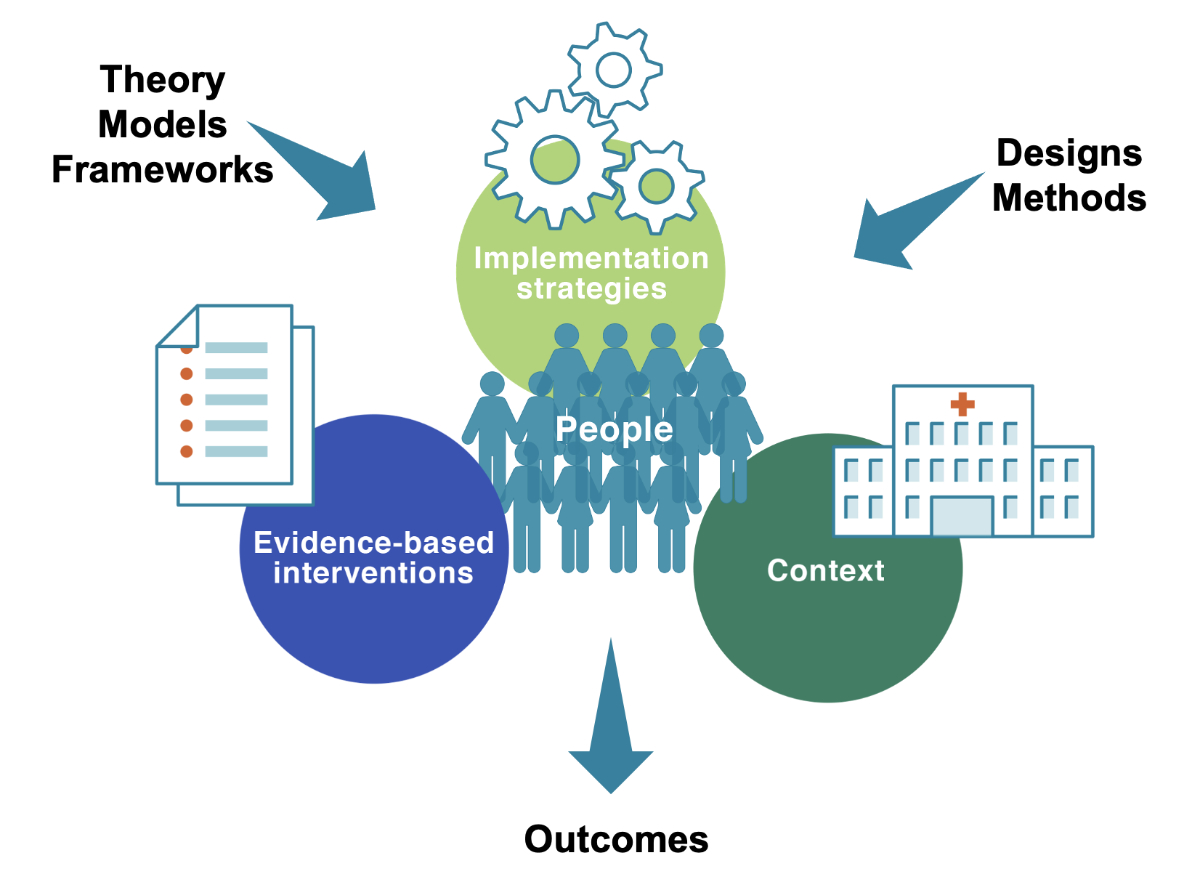
Figure 1 Core elements in implementation science.
Following its inception in the late 1990s, there has been a striking rise of implementation science as a scientific discipline. This progress is evident in the development of implementation science terminology and a broad range of foundational implementation science concepts, frameworks, and theories. More recently, empirical implementation science studies using innovative, hybrid study designs with a dual focus on effectiveness and implementation are being prioritised to evaluate how implementation processes influence the translation of clinical interventions into concrete improvements in patient care, and how these processes can be optimised for the benefit of healthcare professionals and patients [2].
Implementation science offers novel research concepts, methods, and designs to examine and solve wicked problems in Swiss healthcare. This requires meticulous attention to the systematic planning, preparation, support, and improvement of implementing interventions. Rather than insufficient knowledge about “what works,” a central barrier to improving the health and well-being of patients and citizens is the still limited awareness of, knowledge about, and capacity for quality implementation in routine service settings. This is necessary for the timely, effective, and efficient use of evidence in practice.
While Swiss scientists have displayed an interest in implementation science for some time, its visibility as a distinct field of inquiry in Switzerland was significantly advanced through the founding of IMPACT, the Swiss Implementation Science Network, in October 2019 [9]. A year later, the Institute for Implementation Science in Health Care (IfIS) was established at the Faculty of Medicine of the University of Zurich, representing the first institutionalised implementation science infrastructure in Switzerland. In their recent White Paper on Clinical Research, the Swiss Academy of Medical Sciences emphasises implementation science as a central tool in building a "learning healthcare system", which is identified as one of seven goals necessary for Swiss clinical research to significantly impact patient care.
These developments are promising since Switzerland’s diverse geographical, cultural, and cantonal conditions – in a form that is rarely seen in other countries – make it possible to examine and compare implementation variation based on factors such as language, culture, policy, politics, funding, or stakeholder community composition. For example, the parallel implementation of the same antibiotic stewardship program in hospitals in the cantons of Geneva and Graubünden will likely lead to different insights and outcomes because French influences and urban conditions characterise Geneva, whereas Italian and German culture dominates rural Graubünden. These cultural differences could affect policies, organisational cultures, educational standards, and other contextual factors influencing program implementation. Utilising these unique characteristics as part of cross-cantonal research on how to best implement effective interventions under varying conditions, tailor healthcare services to different contexts, or monitor implementation progress over time, requires infrastructure similar to that represented by IfIS.
The development of implementation science in Switzerland has only just begun. Further steps must be taken to build and nourish a stable Swiss implementation science infrastructure. As shown in figure 2, which is based on a research capacity-building framework [10], such infrastructure has sufficient capacity to 1) educate future generations of implementation scientists, 2) conduct rigorous implementation research and advance the science of implementation, 3) effectively disseminate research findings, and 4) support healthcare organisations and systems in integrating effective implementation practice into daily routines.
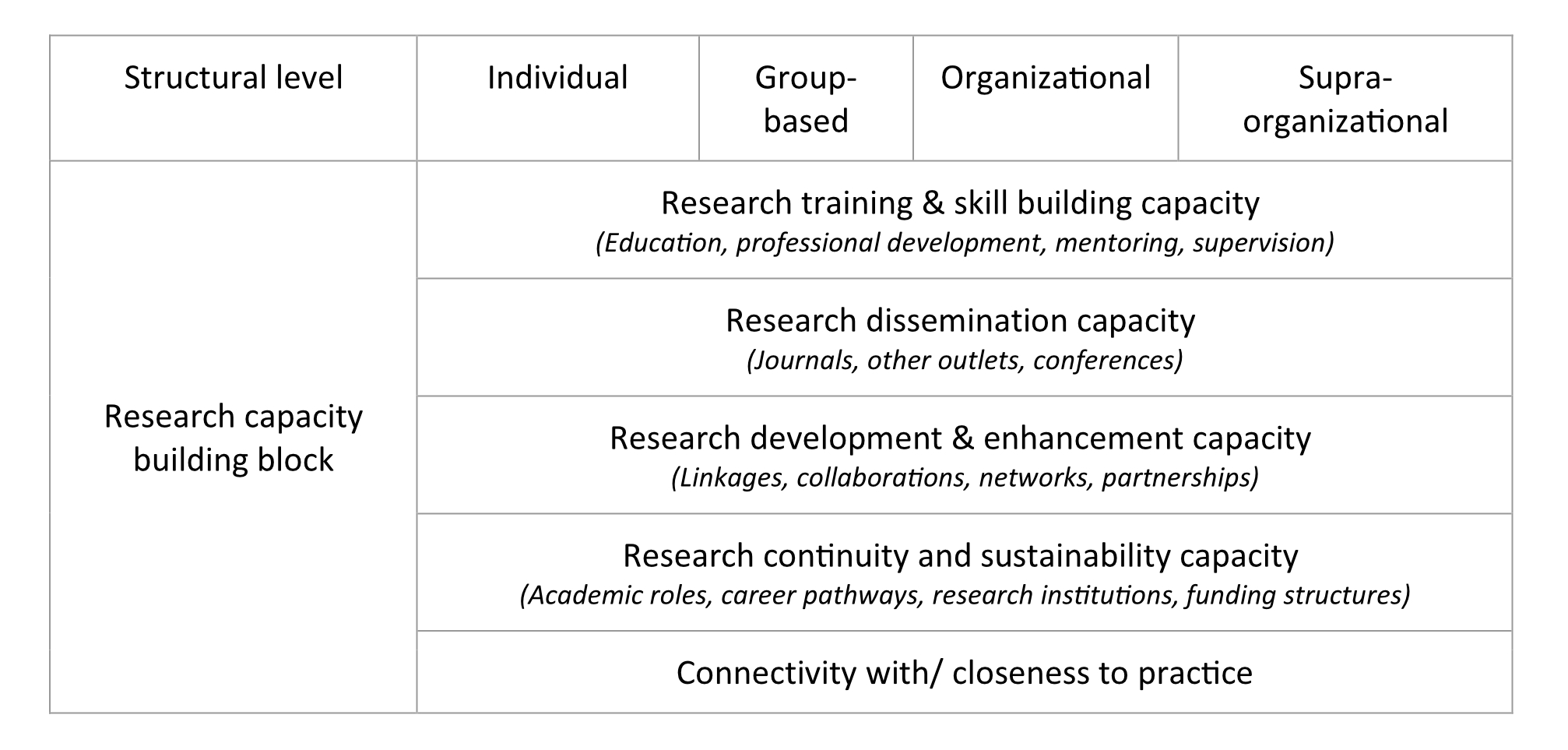
Figure 2 The building blocks of research capacity (adapted based on Cooke J. A framework to evaluate research capacity building in health care. BMC Fam Pract. 2005;6(1):44 [10]).
The further development of implementation science in Switzerland calls for:
Cultivating implementation science in Switzerland using this approach will help build stronger ties between clinical and implementation researchers, sensitise healthcare organisations and their clinicians to the importance of implementation to their services and practices, and enhance the reach of effective interventions among patients and the public. It is time to seize this unique opportunity.
Kathrin Blum; Laura Caci; Paola Daniore; Felix Gille; Christina Haag; Janna Hastings; Tobias Kowatsch, Pashalis Naoumis; Emanuela Nyantakyi; Saskia Oesch; Kimon Papadopoulos; Marco Riguzzi; Jana Sedlakova; Chloé Sieber; Mina Stanikić; Qendresa Thaqi; Andrea Thesenvitz; Eva Thürlimann; Lotte Verweij; Federica Zavattaro.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Khan S, Chambers D, Neta G. Revisiting time to translation: implementation of evidence-based practices (EBPs) in cancer control. Cancer Causes Control. 2021 Mar;32(3):221–30. https://doi.org/https://doi.org/10.1007/s10552-020-01376-z
2. Albers B, Shlonsky A, Mildon R. En Route to Implementation Science 3.0. Implementation Science 3.0. Cham: Springer Nature; 2020. pp. 1–38. https://doi.org/https://doi.org/10.1007/978-3-030-03874-8
3. de Pietro C, Camenzind P, Sturny I, Crivelli L, Edwards-Garavoglia S, Spranger A, et al. Switzerland - Health system review. European Observatory on Health Systems and Policies; 2015.
4. Ladner A, Soguel N, Emery Y, Weerts S, Nahrath S. Swiss Public Administration - Making the State Work Successfully. palgrave macmillan; 2019.
5. Birrenbach T, Kraehenmann S, Perrig M, Berendonk C, Huwendiek S. Physicians’ attitudes toward, use of, and perceived barriers to clinical guidelines: a survey among Swiss physicians. Adv Med Educ Pract. 2016 Dec;7:673–80. https://doi.org/https://doi.org/10.2147/amep.s115149
6. Neuner-Jehle S. Prävention von Fehl- und Überversorgung: was kann der praktizierende Arzt dazu beitragen? Ther Umsch. 2021;78(2):111–7. https://doi.org/https://doi.org/10.1024/0040-5930/a001246
7. Eggli Y, Stadelmann P, Piaget-Rossel R, Marti J. Heterogeneity in The drivers of health expenditures financed by health insurance in a fragmented health system: the case of Switzerland. Health Policy. 2019 Dec;123(12):1275–81. https://doi.org/https://doi.org/10.1016/j.healthpol.2019.10.010
8. Riou J, Panczak R, Althaus CL, Junker C, Perisa D, Schneider K, et al. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: a population-based analysis. Lancet Public Health. 2021 Sep;6(9):e683–91. https://doi.org/https://doi.org/10.1016/s2468-2667(21)00160-2 https://doi.org/https://doi.org/10.1016/S2468-2667(21)00160-2
9. Dhaini SR, Mielke J, Brunkert T, Wyss K, Utzinger J, De Geest S. Swiss Implementation Science Network (IMPACT): A Crucial Building Block to Strengthen the Swiss Research Pipeline for Real-World Translation. Int J Public Health. 2021 Apr;66:1604081. https://doi.org/https://doi.org/10.3389/ijph.2021.1604081
10. Cooke J. A framework to evaluate research capacity building in health care. BMC Fam Pract. 2005 Oct;6(1):44. https://doi.org/https://doi.org/10.1186/1471-2296-6-44